- 1Department of Sports Medicine, Huashan Hospital, Fudan University, Shanghai, China
- 2Department of Gastroenterology and Hepatology, Tianjin Medical University General Hospital, Tianjin, China
- 3Chronic Disease Epidemiology Laboratory, Pennington Biomedical Research Center, Baton Rouge, LA, United States
Editorial on the Research Topic
Exercise, diabetes and metabolic-associated fatty liver disease
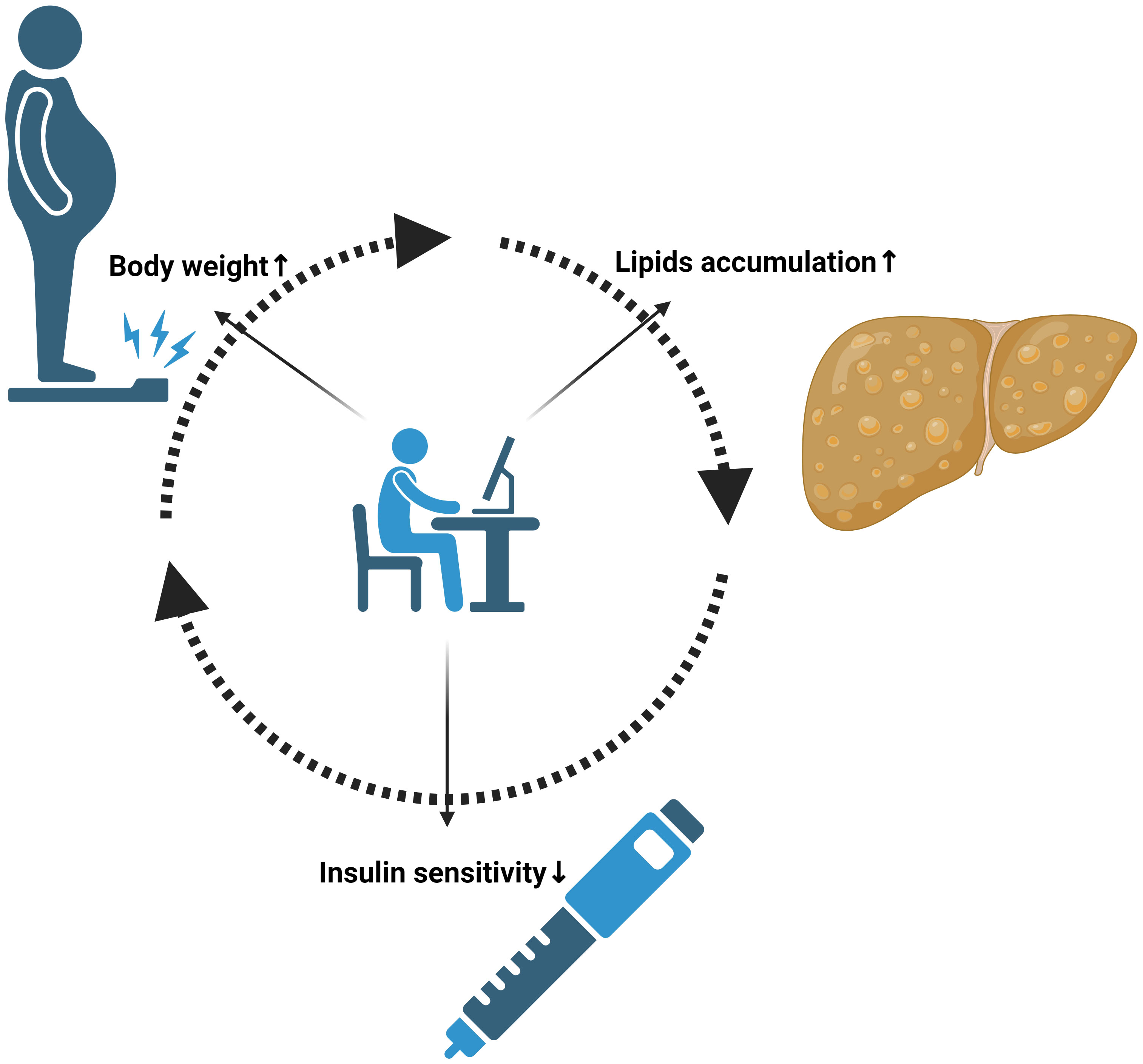
The interplay between lifestyle, metabolic health, and chronic diseases has become increasingly relevant in our modern health landscape (1). The prevalence of sedentary behaviors, alongside dietary excesses, has led to a surge in metabolic disorders, including diabetes and metabolic-associated steatotic liver disease (MASLD) [previously known as metabolic-associated fatty liver disease (MAFLD)] (2). These conditions, often linked and overlapping, present not only a health crisis for individuals but also a challenge for global healthcare systems. Diabetes, a major public health issue, is intricately connected to lifestyle choices. Its management and prevention are heavily influenced by physical activity and diet, necessitating a deeper understanding of these relationships. Similarly, MASLD, previously known as non-alcoholic fatty liver disease (NAFLD), has emerged as the most common liver disorder worldwide. It is closely associated with metabolic syndromes such as obesity and insulin resistance, conditions that are often precursors or companions of diabetes and future cardiovascular diseases (Figure 1) (3, 4).
Exercise, a cornerstone of diabetes management, has also been recognized for its role in improving liver health. Physical activity, interacted with genetic susceptibility, influences glucose metabolism, insulin sensitivity, and overall metabolic function, thus playing a crucial role in managing and preventing conditions like diabetes and MASLD (5–8). However, the nuances of this relationship – the type, intensity, and duration of exercise that are most beneficial – are areas of ongoing research. Moreover, the intersection of these conditions with other comorbidities, such as cardiovascular diseases and osteoarthritis, adds layers of complexity to their management. This underscores the need for a multidisciplinary approach that considers the multifaceted nature of these diseases.
In this Research Topic, we bring together six articles that provide valuable insights into the complex relationships between exercise, diabetes, and MAFLD. Each article addresses a different aspect of this triad, contributing to a comprehensive narrative that enhances our understanding and guides future research and clinical practices.
The first article by Lei et al. explores the association between metabolic dysfunction-associated fatty liver disease and an increased risk of subclinical carotid atherosclerosis in China. This study adds to the growing body of evidence linking MAFLD with cardiovascular risks. The second article by Chai et al. reinforces the Research Topic’s overarching theme with a systematic review and meta-analysis on the effects of lifestyle interventions in adults with MAFLD. This study solidifies the role of non-pharmacological approaches in managing this condition. Shifting focus to pharmacological interventions, the third article by Kongmalai et al. presents a systematic review and network meta-analysis of randomized controlled trials on new anti-diabetic agents for treating NAFLD. This study highlights the emerging therapeutic options bridging diabetes and liver disease treatment. The fourth article introduces an innovative approach to knee osteoarthritis rehabilitation in patients with MASLD, comparing blood flow restriction training with traditional weight-bearing exercises. This multicenter randomized controlled trial offers new insights into managing MASLD-associated comorbidities. The fifth study by Vágvölgyi et al. explores the benefits of a three-month physical training program, revealing improvements in cardiovascular autonomic functions in patients with metabolic syndrome, with and without diabetes. This pilot study paves the way for future research into exercise regimes for these patients. Our last article by Bennasar-Veny et al. provides a comprehensive analysis of physical activity’s impact on glycemic control in individuals with prediabetes. This systematic review and meta-analysis emphasize the critical role of exercise in the early intervention stages of diabetes.
Together, these articles illuminate the intricate interdependencies between physical activity, metabolic health, and chronic disease management. They collectively emphasize the importance of an integrated approach to treatment and prevention, combining lifestyle interventions with medical management. This Research Topic serves as a crucial resource for clinicians, researchers, and policymakers, advocating for informed, multifaceted strategies to combat the growing challenges of diabetes and MASLD/MAFLD in the context of modern lifestyles.
Author contributions
YaS: Writing – original draft. CS: Writing – review & editing. GH: Conceptualization, Writing – review & editing. YuS: Writing – original draft.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article.GH was partially supported by the grant from the National Institute of General Medical Sciences (U54GM104940).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Khemka S, Reddy A, Garcia RI, Jacobs M, Reddy RP, Roghani AK, et al. Role of diet and exercise in aging, Alzheimer’s disease, and other chronic diseases. Ageing Res Rev (2023) 91:102091. doi: 10.1016/j.arr.2023.102091
2. Rinella ME, Lazarus JV, Ratziu V, Francque SM, Sanyal AJ, Kanwal F, et al. A multisociety Delphi consensus statement on new fatty liver disease nomenclature. J Hepatol (2023). doi: 10.1016/j.jhep.2023.06.003
3. Sheka AC, Adeyi O, Thompson J, Hameed B, Crawford PA, Ikramuddin S. Nonalcoholic steatohepatitis: A review. Jama (2020) 323(12):1175–83. doi: 10.1001/jama.2020.2298
4. Shen Y, Hu T, Tan H, Xu Y, Wang Y, Ma X, et al. Insight to the association among fibroblast growth factor 21, non-alcoholic fatty liver disease and cardiovascular outcomes: A population-based study. Cytokine (2023) 170:156318. doi: 10.1016/j.cyto.2023.156318
5. Colosimo S, Mitra SK, Chaudhury T, Marchesini G. Insulin resistance and metabolic flexibility as drivers of liver and cardiac disease in T2DM. Diabetes Res Clin Pract (2023) 206:111016. doi: 10.1016/j.diabres.2023.111016
6. Wronka M, Krzemińska J, Młynarska E, Rysz J, Franczyk B. The influence of lifestyle and treatment on oxidative stress and inflammation in diabetes. Int J Mol Sci (2022) 23(24):15743. doi: 10.3390/ijms232415743
7. Chen Y, Liu H, Wang L, Zhou T, Liang Z, Li W, et al. Lifestyle intervention modifies the effect of the MC4R genotype on changes in insulin resistance among women with prior gestational diabetes: Tianjin Gestational Diabetes Mellitus Prevention Program. Am J Clin Nutr (2019) 110(3):750–8. doi: 10.1093/ajcn/nqz121
Keywords: exercise, diabetes, fatty liver, metabolic syndrome, editorial
Citation: Sun Y, Sun C, Hu G and Shen Y (2023) Editorial: Exercise, diabetes and metabolic-associated fatty liver disease. Front. Endocrinol. 14:1347458. doi: 10.3389/fendo.2023.1347458
Received: 30 November 2023; Accepted: 01 December 2023;
Published: 19 December 2023.
Edited and Reviewed by:
Åke Sjöholm, Gävle Hospital, SwedenCopyright © 2023 Sun, Sun, Hu and Shen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yun Shen, yun.shen@pbrc.edu; Gang Hu, gang.hu@pbrc.edu
 Yang Sun
Yang Sun