- Department of Cardiovascular Medicine, The Second Affiliated Hospital of Nanchang University, Nanchang, Jiangxi, China
Objective: We aimed to investigate the predictive value of the CT findings combined with serum potassium levels for primary aldosteronism (PA) subtype diagnosis, with a particular interest in sex differences.
Methods: In this retrospective study, we eventually included 482 PA patients who underwent successful adrenal venous sampling (AVS) and had available data. We diagnosed the subjects as having either unilateral (n = 289) or bilateral PA (n = 193) based on AVS. We analyzed the concordance rate between AVS and adrenal CT combined with serum potassium and performed a logistic regression analysis to assess the prevalence of unilateral PA on AVS.
Results: The total diagnostic concordance rate between CT findings and AVS was 51.5% (248/482). The prevalence of hypokalemia in men and women was 47.96% (129/269) and 40.85% (87/213), respectively. The occurrence of unilateral lesions on CT and hypokalemia was significantly associated with an increased prevalence of unilateral PA [odds ratio (OR) 1.537; 95% confidence interval (CI) 1.364–1.731; p < 0.001]. In male participants, G2 (bilateral lesion on CT and normokalemia), G3 (unilateral lesion on CT and normokalemia), G4 (bilateral normal on CT and hypokalemia), G5 (bilateral lesion on CT and hypokalemia), and G6 (unilateral lesion on CT and hypokalemia) were significantly increased for the prevalence of unilateral PA on AVS (G2: OR 4.620, 95% CI 1.408–15.153; G3: OR 6.275, 95% CI 2.490–15.814; G4: OR 3.793, 95% CI 1.191–12.082; G5: OR 16.476, 95% CI 4.531–59.905; G6: OR 20.101, 95% CI 7.481–54.009; all p < 0.05), compared with G1 (patients with bilateral normal on CT and normokalemia). However, among female participants, we found an increased likelihood for unilateral PA in patients with unilateral lesions on CT and hypokalemia alone (OR 10.266, 95% CI 3.602–29.259, p < 0.001), while no associations were found in other groups (all p > 0.05). Sex had a significant effect on modifying the relationship between unilateral PA and the combination of CT findings and serum potassium (p for interaction <0.001).
Conclusion: In conclusion, our results indicated that CT findings combined with serum potassium levels have a great value for predicting the subtype of PA and are stronger in men.
Introduction
Primary aldosteronism (PA) is a frequent cause of secondary hypertension due to autonomous aldosterone secretion by the adrenal glands. The prevalence of PA in hypertensive patients is reportedly 3.2%–12.7% in primary care centers and 1%–29.8% in referral centers (1). Patients with PA have a higher prevalence of various target organ damage and cardiovascular complications such as stroke, microalbuminuria, left ventricular hypertrophy, myocardial infarction, atrial fibrillation, and heart failure than those with essential hypertension (2–4). Aldosterone-producing adenoma (APA) and idiopathic hyperaldosteronism (IHA) are the most frequent forms of PA, accounting for 30% and 60% of all cases, respectively (5). A differential diagnosis between these subtypes is a crucial step in diagnosis and choice of treatment, as most patients with APA are surgically curable, while patients with IHA require lifelong treatment with mineralocorticoid receptor (MR) antagonists (6).
Although adrenal venous sampling (AVS) is recommended as the gold standard method for classifying subtypes by the current guidelines (6, 7); this approach is invasive, costly, technically challenging, and limited to specialized centers (8, 9). Therefore, a simpler non-invasive method for subtype classification is needed. Adrenal computed tomography (CT) is a widely used imaging technique in most centers and is more convenient and inexpensive than AVS. The current guidelines recommend that all patients with PA undergo adrenal CT to exclude adrenocortical carcinoma and severing as the initial study for subtype testing. Nevertheless, previous studies have shown that the diagnostic accuracy of adrenal CT for subtype classifying is not sufficient compared with AVS (10–12). Based on clinical variables, several prediction models have been reported to distinguish among differing subtypes for use instead of AVS (13–19). Although the studies incorporated different clinical parameters, CT findings and serum potassium served as shared predictors for subtype diagnosis of PA patients. A recent study proposed graded recommendation strength of AVS indication based on the probability of unilateral hyperaldosteronism on AVS determined by CT findings and serum potassium (12). However, it is not clear whether there was a significant difference in the association between the subtype of PA and the combination of CT findings and serum potassium between male and female populations.
In this study, we aimed to investigate the predictive value of the CT findings combined with serum potassium levels for subtype diagnosis, with a particular interest in sex differences.
Methods
Study participants
Our study included 482 PA patients with available data on clinical characteristics, biochemistry, CT findings, and successful AVS from November 2017 to October 2021 at the Second Affiliated Hospital of Nanchang University. The diagnostic procedures for PA followed the Endocrine Society Clinical Practice Guidelines (6) and the Expert Consensus on the Diagnosis and Treatment of Primary Aldosteronism in China (7) and were described in detail in our previous study (20). The Medical Research Ethics Committee of the Second Affiliated Hospital of Nanchang University reviewed and approved the study and waived the need for informed consent.
The inclusion criteria of this study were as follows: a) patient aged between 18 and 75 years, b) confirmed diagnosis of PA, c) AVS was bilaterally successful, and d) availability of data on clinical characteristics, biochemistry, and CT findings. Patients with other forms of secondary hypertension, such as renal artery stenosis, hyperthyrea, Cushing’s syndrome, or pheochromocytoma, were excluded.
Diagnosis criteria for PA
Case detection of PA was performed using plasma aldosterone concentration (PAC) to plasma renin activity (PRA) ratio (ARR). Before the screening test, diuretics and mineralocorticoid receptor antagonists were withdrawn for at least 4 weeks, and dihydropyridine calcium channel blockers, angiotensin-converting enzyme inhibitors, angiotensin II receptor blockers, and β-adrenergic receptor blockers were discontinued for at least 2 weeks. Antihypertensive medications were replaced by non-dihydropyridine calcium channel blockers (verapamil slow-release) and/or α-adrenergic receptor blockers (terazosin hydrochloride) for uncontrolled hypertension, and patients were required to monitor blood pressure periodically. Blood samples for PRA and PAC were collected at 7 a.m. after the patients had been upright for 2 hours. The screening test was considered positive when the ARR > 30 (ng/dl)/(ng/ml/h) coupled with PAC >15 ng/dl. For patients with positive screening tests, the captopril challenge test (CCT) or saline infusion test (SIT) was performed to further confirm the diagnosis of PA. When the aldosterone suppression rate was less than 30% or PAC was greater than 11 ng/dl after 2 hours of oral administration of 50 mg captopril, CCT was regarded as positive. The cutoff value for SIT was PAC > 10 ng/dl after infusion of 2L 0.9% saline over 4 hours in the seated position (6, 7).
Serum potassium levels
Hypokalemia was defined as a serum potassium level of <3.5 mmol/L in the available potassium data during hospitalization.
CT imaging
All the patients were examined with thin-slice adrenal CT (GE Co., Chicago, IL, USA). In the absence of AVS outcomes, the adrenal CT images were individually evaluated by two experienced radiologists. A panel discussion serves to settle disagreements between the two radiologists. The CT findings were classified into bilateral normal, unilateral lesion, and bilateral lesion. The adrenal gland’s normal appearance (the thickness of the adrenal gland was <10 mm) on both sides was described as the bilateral normal of CT findings. Unilateral adrenal lesion of CT findings was defined as unilateral adenoma, nodule, or hyperplasia without abnormal appearance on the contralateral glands.
AVS procedure and subtype diagnosis
The bilaterally simultaneous catheterization AVS without adrenocorticotropic hormone (ACTH) stimulation was performed in all patients according to the current guidelines (8). The right adrenal vein (RAV) and left adrenal vein (LAV) were catheterized through the percutaneous right forearm vein approach and femoral vein approach under fluoroscopic guidance, respectively, and successful catheterization was confirmed by slow injection of a small amount of contrast medium. Blood samples were simultaneously collected from the bilateral adrenal veins, and then inferior vena cava (IVC) samples were taken as a control. Adrenal vein cannulation was regarded as successful if the selectivity index (SI) was >2, as the ratio of cortisol concentration of the adrenal vein to the IVC. The lateralization index (LI) was defined as the ratio of aldosterone to cortisol ratio on the dominant side to the non-dominant side. The criterion used for unilateral hyperaldosteronism was LI greater than 2.
Assay methods
Assay methods were described in our previous study (20). PAC (ng/dl) and PRA (ng/ml/h) were determined by chemiluminescence immunoassay (CLIA) following the manufacturer’s instruction (Maglumi 4000 plus, Sinbe Co., Ltd., Shenzhen, China). Plasma cortisol concentration (PCC) (μg/dl) was measured by CLIA following the manufacturer’s instruction (ADVIA Centaur XP, Siemens Co., Munich, Germany).
Statistical analysis
IBM SPSS Statistic version 23.0 (SPSS Inc., Chicago, IL, USA) was performed in the whole statistical analysis. Normally distributed continuous variables are reported as means ± standard deviations (SDs) and analyzed by unpaired t-test. Continuous variables with a skewed distribution are expressed as medians with interquartile range (IQR) and analyzed by the Mann–Whitney U-tests. Categorical variables are presented as absolute numbers with percentages and analyzed by χ2 test or Fisher’s exact tests. The population characteristics were compared among patients with unilateral and bilateral PA by sex classification. CT findings (unilateral lesion, bilateral lesion, and bilateral normal on CT) and serum potassium (hypokalemia and normokalemia) were investigated in the subtype diagnosis of PA determined by AVS. Multivariate logistic regression analysis was used to assess the odds ratios (ORs) and 95% confidence interval (CI) of the association between unilateral PA and the combination of CT findings and serum potassium in different sexes. Patients with bilateral normal CT and normokalemia were defined as the reference group. Three models were constructed for regression analysis: Model 1 was adjusted for none; Model 2 was adjusted for age, sex (only for the overall population), body mass index (BMI; kg/m2), diabetes, estimated glomerular filtration rate (eGFR; ml/min/1.73 m2), systolic blood pressure (SBP; mmHg), and diastolic blood pressure (DBP; mmHg). Model 3 was adjusted for all covariables in Model 2 and adjusted for total cholesterol (TC; mmol/L), triglyceride (TG; mmol/L), high-density lipoprotein (HDL; mmol/L), low-density lipoprotein (LDL; mmol/L), fasting plasma glucose (FPG; mmol/L), glycosylated hemoglobin (HbA1c; mmol/L), and homocysteine (Hcy, mmol/L). Furthermore, the interactions of the association between unilateral PA and the combination of CT findings and serum potassium with age (<60 vs. ≥60 years), BMI (<24 vs. ≥24 kg/m2), eGFR (<90 vs. ≥90 ml/min/1.73 m2), and diabetes (yes vs. no) in different sex were evaluated by interaction test. p < 0.05 (two-tailed) was defined as a statistically significant difference.
Results
Baseline characteristics of study participants
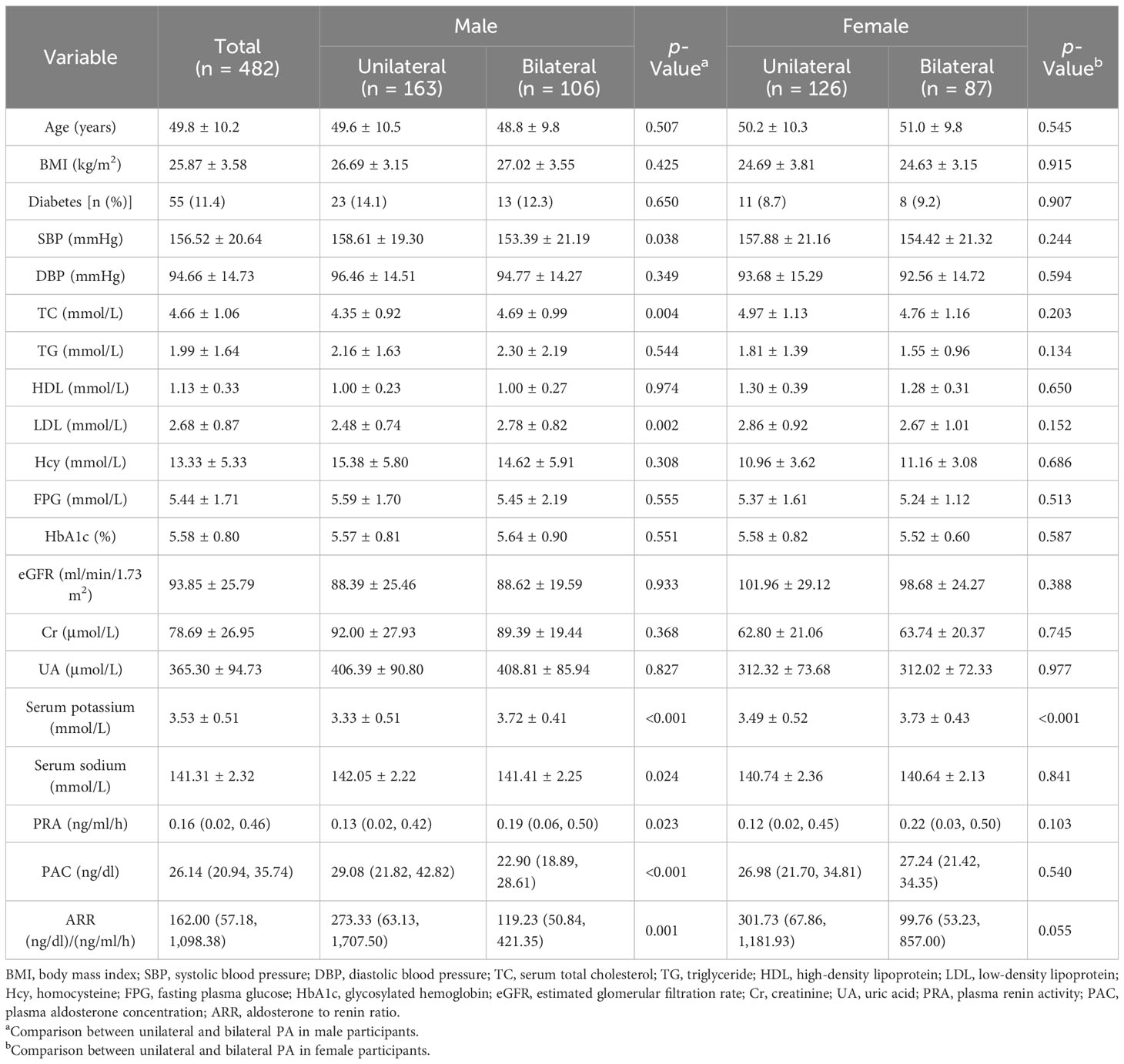
A total of 482 PA patients with successful AVS were included in this study (average age 49.8 ± 10.2 years; 55.81% males). Among the participants, 289 (59.96%) were unilateral PA patients. The average age and the prevalence of hypokalemia in 269 male participants were 49.3 ± 10.2 years and 47.96% (129/269), respectively. The average age and the prevalence of hypokalemia in 213 female participants were 50.5 ± 10.1 years and 40.85% (87/213), respectively. The prevalence of unilateral PA in male and female participants was 60.59% (163/269) and 59.15% (126/213), respectively.
The distributions of study population baseline characteristics according to the subtype of PA among male and female participants are presented in Table 1. In the male group, the unilateral PA patients had higher values for SBP, serum sodium, PAC, and ARR and lower values for TC, LDL, serum potassium, and PRA, compared to bilateral PA patients. Female participants with unilateral PA had lower serum potassium levels compared with bilateral PA. However, no significant differences were found in SBP, TC, LDL, PRA, PAC, ARR, and serum sodium in female participants among unilateral and bilateral PA patients.
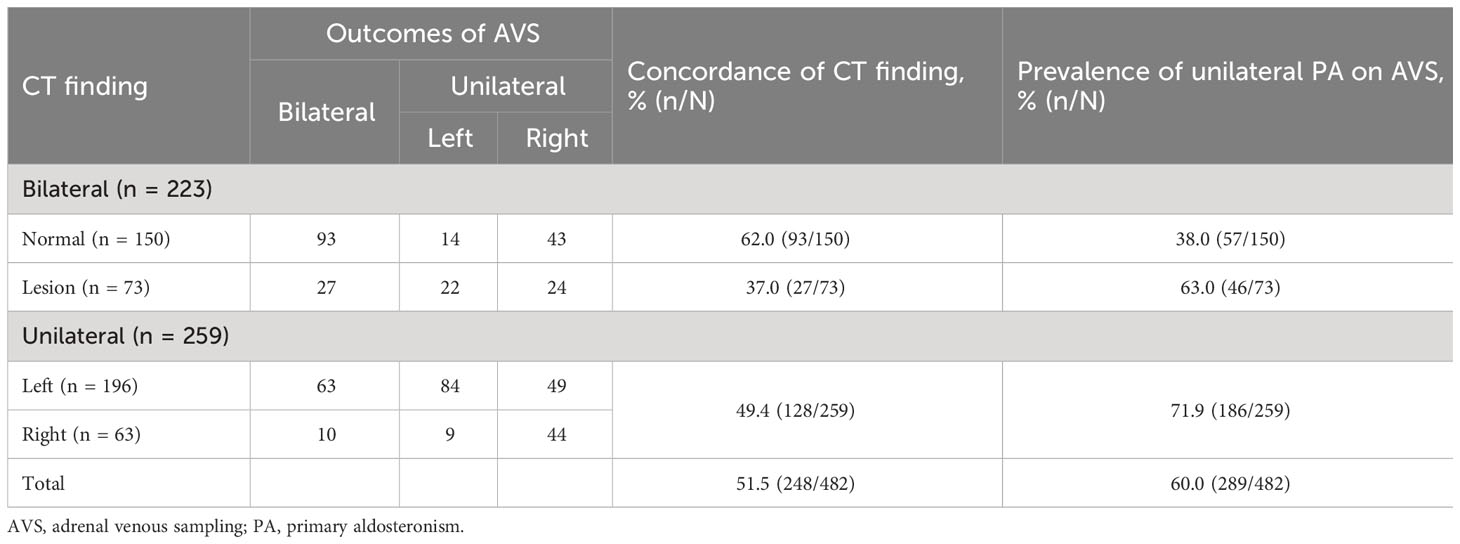
Diagnostic concordance rate between CT findings and AVS
The proportion of bilateral normal, bilateral lesion, and unilateral lesion on adrenal CT findings was 31.1% (150/482), 15.1% (73/482), and 53.7% (259/482), respectively. The diagnostic concordance rate between AVS and bilateral normal, bilateral lesion, and unilateral lesion on adrenal CT findings was 62.0% (93/150), 37.0% (27/73), and 49.4% (128/259), respectively. Although adrenal CT was recommended as the initial study for subtype testing, the overall diagnostic concordance rate of CT findings was 51.5% (248/482). Moreover, approximately 38.0% (57/150) of patients with bilateral normal CT showed unilateral PA on AVS. In addition, 22.4% (58/259) of patients with unilateral lesion on CT performed exhibited hyperaldosteronism in the contralateral adrenal gland on AVS (Table 2).
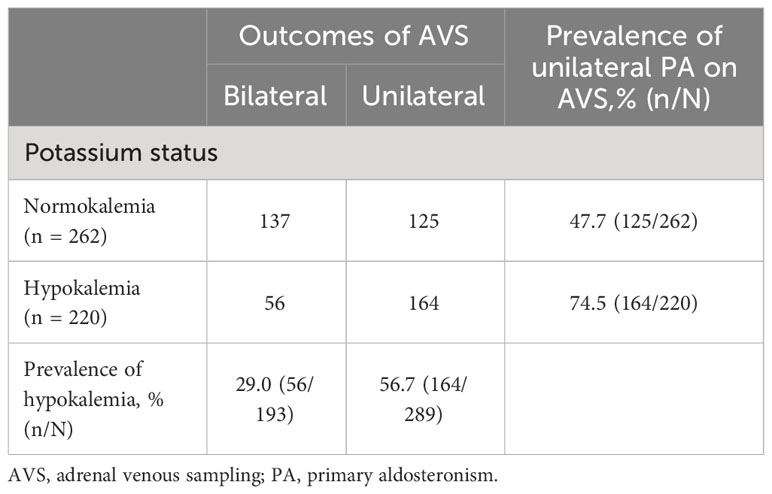
Serum potassium levels in patients with different AVS outcomes
The prevalence of hypokalemia was 56.7% (164/289) in patients with unilateral PA on AVS but was 29.0% (56/193) in patients with bilateral PA on AVS. Furthermore, the prevalence of unilateral PA on AVS was 74.5% in patients with hypokalemia. Serum potassium levels were correlated with the subtype diagnosis of PA (p < 0.001) (Table 3).
Association between unilateral hyperaldosteronism and the combination of CT findings and serum potassium
The results of the multivariate logistic regression analysis are shown in Table 4. Overall, there was a significant association between unilateral PA and the combination of CT findings and serum potassium (p < 0.001). Compared with those in G1 (patients with bilateral normal on CT and normokalemia), the adjusted odds ratios for unilateral PA on AVS in G2 (a bilateral lesion on CT and normokalemia), G3 (unilateral lesion on CT and normokalemia), G4 (bilateral normal on CT and hypokalemia), G5 (bilateral lesion on CT and hypokalemia), and G6 (unilateral lesion on CT and hypokalemia) were 2.423 (95% CI: 1.079, 5.443), 3.289 (95% CI: 1.810, 5.975), 2.646 (95% CI: 1.220, 5.742), 5.767 (95% CI: 2.224, 14.952), and 10.258 (95% CI: 5.355, 19.653), respectively (all p < 0.05). In the stratified analysis, we found that the association of unilateral PA on AVS with the combination of CT findings and serum potassium was stronger in male participants, compared with female participants. In male participants, G2, G3, G4, G5, and G6 were significantly increased for the prevalence of unilateral PA on AVS (G2: OR 4.620, 95% CI 1.408–15.153; G3: OR 6.275, 95% CI 2.490–15.814; G4: OR 3.793, 95% CI 1.191–12.082; G5: OR 16.476, 95% CI 4.531–59.905; G6: OR 20.101, 95% CI 7.481–54.009; all p < 0.05), compared with G1. However, among female participants, we found an increased likelihood for unilateral PA in patients with unilateral lesions on CT and hypokalemia alone (OR 10.266, 95% CI 3.602–29.259, p < 0.001), while no associations were found in other groups (all p > 0.05). Sex had a significant effect on modifying the relationship between unilateral PA and the combination of CT findings and serum potassium (p for interaction <0.001).

Table 4 The odds ratio for unilateral PA on AVS by categorizing the combination of CT findings and serum potassium levels.
Subgroup analysis
In the stratified analyses, none of the variables, including age, BMI, eGFR, and diabetes, significantly modified the association between the prevalence of unilateral PA and the combination of CT findings and serum potassium among male and female participants (all p for interaction >0.05) (Figure 1).
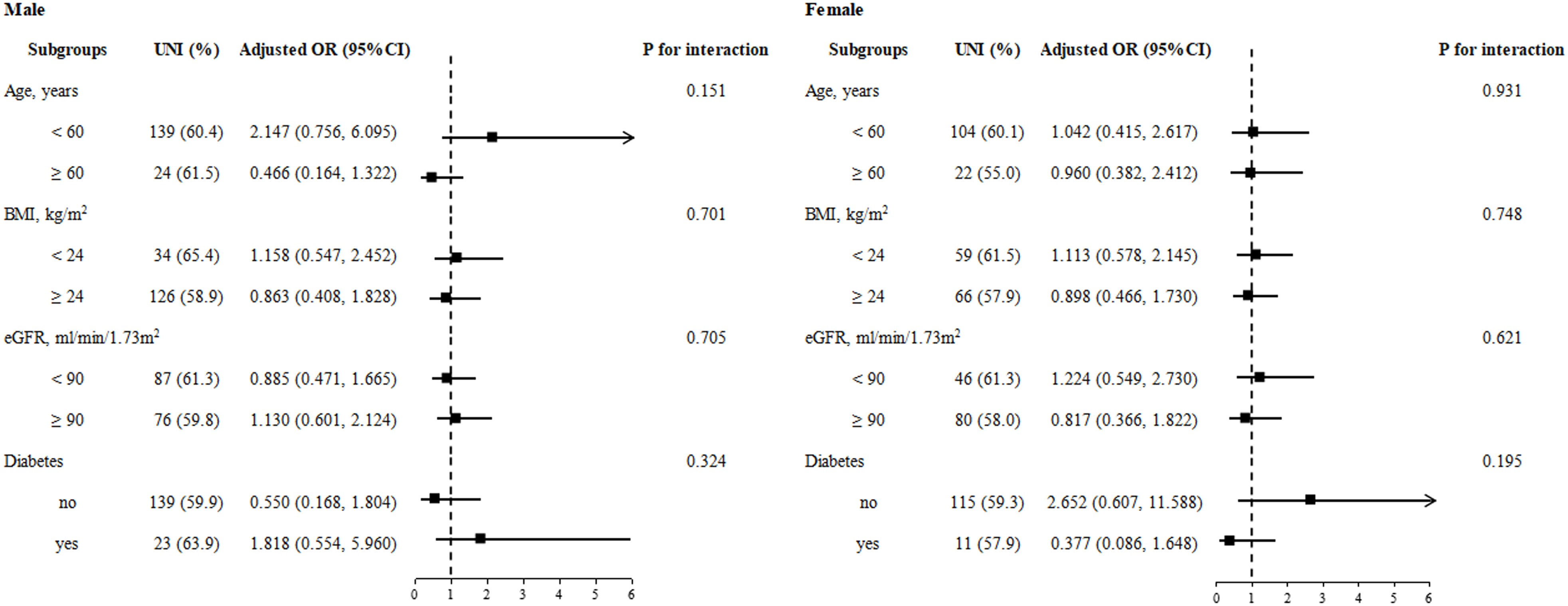
Figure 1 Stratified analyses by potential modifiers of the association between the combination of CT findings and serum potassium and unilateral PA by sex. Adjusted for age, BMI, diabetes, eGFR, SBP, DBP, TC, TG, HDL, LDL, FBG, HbA1c, and Hcy, if not be stratified.
Discussion
Our study confirmed that the combination of CT findings and serum potassium has a great value for predicting the subtype of PA. The occurrence of unilateral lesions on CT and hypokalemia is significantly associated with an increased prevalence of unilateral PA. Moreover, we found that the association of subtype on AVS with the combination of CT findings and serum potassium was stronger in male participants, compared with female participants.
Primary aldosteronism is the most common but largely unrecognized cause of secondary hypertension (21). Unilateral adrenalectomy can normalize aldosterone excess, cure or improve hypertension, and prevent target organ damage in patients with unilateral PA, while bilateral disease is treated with MR antagonist (6, 7). Hence, distinguishing unilateral and bilateral PA is critical for selecting the most appropriate treatment. In the present study, the overall diagnostic concordance rate between CT findings and AVS outcomes was 51.5%, which is similar to previous studies (10–12). Although the current guidelines recommend using adrenal CT severing as the initial study for subtype testing, the specificity of CT findings could not be sufficient to allow surgical decision-making without AVS evidence. Indeed, we found that 38.0% (57/150) of patients with bilateral normal CT showed unilateral PA on AVS, while 22.4% (58/259) of patients with unilateral lesion on CT exhibited unilateral hyperaldosteronism in the contralateral adrenal gland. Research has revealed that thin-section high-resolution CT omits 27 cases of aldosterone-producing microadenoma among 69 cases of APA adrenal because CT cannot detect an adrenal mass less than 6 mm in diameter (22). Meanwhile, non-functioning adenoma is not unusual in PA patients (23, 24). It is indicated that AVS is necessary before surgery to avoid unnecessary or inappropriate surgery. The current guidelines recommend AVS as the gold standard test to lateralize the source of excessive aldosterone secretion. However, AVS is a high-cost, technically difficult, and invasive procedure and has a risk of complications such as adrenal vein rupture, hemorrhage, and thromboembolism (8). Considering the high prevalence of PA, subtype classification based on safe, inexpensive, and reliable methods is very important. Several models have been developed to predict PA subtypes based on clinical findings and with high specificity (13–19). The most widely accepted and classical model was the Küpers prediction score, which suggested that AVS could be omitted in patients with a typical Conn’s adenoma plus serum potassium <3.5 mmol/L or eGFR ≥ 100 ml/min/1.73 m2. In subjects with a score of at least 5, this criterion had a specificity of 100% (95% CI, 91%–100%) and a sensitivity of 53% (95% CI, 38%–68%) to predict a lateralized AVS (13). However, subsequent research showed the Küpers prediction score was not suitable for elderly and Chinese patients (19, 25). Since failure to correctly predict unilateral PA will result in inappropriate or unnecessary adrenalectomy, it seems more reasonable to develop a prediction model to identify patients with bilateral PA that could spare AVS. Kocjan et al. (14) first established a scoring system based on the combined criterion of serum potassium ≥3.5 mmol/L, post-SIT aldosterone <18 ng/dl, and either no or bilateral tumor found on CT imaging to predict bilateral PA, which saved an estimated 16% of the patients from unnecessary AVS. Xiao et al. (18) developed and validated a nomogram that was able to predict the probability of IHA based on BMI, serum potassium, and CT findings, and the specificity reached 100% when the threshold increased to a probability of 90%. Although the above studies incorporated different clinical indicators, CT findings and serum potassium served as shared predictors for subtype diagnosis of PA patients. Recent research showed that the prevalence of unilateral PA on AVS in patients with unilateral disease on CT with hypokalemia, unilateral disease on CT with normokalemia, bilateral normal on CT with hypokalemia, and bilateral normal on CT with normokalemia was 70.6%, 38.1%, 23.8%, and 6.2%, respectively (12). Our study further demonstrates the value of this prediction score for identifying patients who should undergo AVS before surgery by showing that patients with unilateral lesions on CT and hypokalemia had a high likelihood of lateralization on AVS.
Notably, we found that sex can modify the relationship between the subtype of PA and the combination of CT findings and serum potassium. The presence of abnormality on CT and hypokalemia was significantly associated with an increased incidence of unilateral PA among male participants, but not stably in female participants. Previous studies have shown the relationship between sex and the subtype distribution of PA, but the conclusions of these studies have been controversial. A number of studies reported that women had a higher incidence of bilateral PA (14, 16, 17, 26). In contrast, the literature indicated that the proportion of male participants was significantly higher in patients with IHA compared with those with APA (18). However, possible mechanisms for the positive or negative relationship were not mentioned in the literature. Meanwhile, several previous studies did not observe a difference between men and women in the subtype distribution in AVS (13, 15, 27), which is consistent with our current finding. These conflicting results might be attributed to the different definitions of PA subtype and interpretation of AVS in the above studies and the wide variation of study populations in different regions.
There is limited information available about how sex influences serum potassium and adrenal CT results in PA patients. Consistent with the present study, Akasaka et al. (26) found that the incidence of hypokalemia was higher in men. Although there was no difference between men and women with unilateral PA in PAC, we found that male patients with unilateral PA had lower serum potassium levels than female patients. In order to accurately predict the probability of APA in patients with unilateral adrenal nodules, He et al. (28) included men as a positive indicator for a nomogram. Taken together, compared with female patients, male patients with unilateral PA have more obvious clinical features; therefore, the positive correlation between unilateral PA and the combination of CT findings and serum potassium is more significant in men. Research based on the Japan Primary Aldosteronism Study indicated that sex may have a clinically significant impact on the distribution of subtypes differently among the generations, even if it is not a definitive factor in determining the age at the onset of PA for each subtype (26). Moreover, a study demonstrated that women had a higher prevalence of KCNJ5 mutations, which are present in 39.3% of APA patients (29). Furthermore, female sex is associated with poorer renal outcomes in patients receiving spironolactone for bilateral PA (30). Although the possible mechanism is unclear, sex differences should be considered when applying CT findings combined with serum potassium to predict subtypes of PA.
Limitations
There are several limitations to this study. The study was conducted only on a specific population. Our results might not be generalizable to other patient cohorts. In addition, the retrospective nature of the study limited its usefulness. Although our study included more participants compared to most previous studies, prospective studies are still needed to confirm and validate the current results. The PA subtype was based on the outcomes of bilaterally simultaneous catheterization AVS without ACTH stimulation in this study. The criterion used for unilateral hyperaldosteronism was LI > 2. Although this criterion is the most commonly used threshold recommended by current guidelines, the lateralization of AVS is not completely consistent with the subtype of PA. Thus, the subtype diagnosis of PA should be revised by the results of postoperative histological examination and treatment outcomes.
Conclusion
In conclusion, we found that the association of subtype on AVS with the combination of CT findings and serum potassium was stronger in male participants, compared with female participants.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by The Medical Research Ethics Committee of The Second Affiliate Hospital of Nanchang University. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
YW: Conceptualization, Writing – original draft, Writing – review & editing. ZW: Data curation, Methodology, Writing – review & editing. JR: Data curation, Methodology, Writing – review & editing. HH: Data curation, Methodology, Writing – review & editing. ZC: Data curation, Methodology, Writing – review & editing. CH: Data curation, Methodology, Writing – review & editing. QP: Data curation, Methodology, Writing – review & editing. PL: Conceptualization, Funding acquisition, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. The present study was supported by the National Natural Science Foundation of China (grant nos. 81860058, 81560079) and Special funds for guiding local scientific and technological development by the central government of China (grant no. S2019CXSFG0016).
Acknowledgments
We acknowledge the members of the Department of Cardiovascular Medicine of the Second Affiliated Hospital of Nanchang University who participated in the screening of patients with secondary hypertension and performed AVS. We also thank all the study participants.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Kayser SC, Dekkers T, Groenewoud HJ, van der Wilt GJ, Carel Bakx J, van der Wel MC, et al. Study heterogeneity and estimation of prevalence of primary aldosteronism: a systematic review and meta-regression analysis. J Clin Endocrinol Metab (2016) 101(7):2826–35. doi: 10.1210/jc.2016-1472
2. Ohno Y, Sone M, Inagaki N, Yamasaki T, Ogawa O, Takeda Y, et al. Prevalence of cardiovascular disease and its risk factors in primary aldosteronism: a multicenter study in Japan. Hypertension (2018) 71(3):530–7. doi: 10.1161/HYPERTENSIONAHA.117.10263
3. Monticone S, Burrello J, Tizzani D, Bertello C, Viola A, Buffolo F, et al. Prevalence and clinical manifestations of primary aldosteronism encountered in primary care practice. J Am Coll Cardiol (2017) 69(14):1811–20. doi: 10.1016/j.jacc.2017.01.052
4. Monticone S, D'Ascenzo F, Moretti C, Williams TA, Veglio F, Gaita F, et al. Cardiovascular events and target organ damage in primary aldosteronism compared with essential hypertension: a systematic review and meta-analysis. Lancet Diabetes Endocrinol (2018) 6(1):41–50. doi: 10.1016/S2213-8587(17)30319-4
5. Young WJ. Diagnosis and treatment of primary aldosteronism: practical clinical perspectives. J Intern Med (2019) 285(2):126–48. doi: 10.1111/joim.12831
6. Funder JW, Carey RM, Mantero F, Murad MH, Reincke M, Shibata H, et al. The management of primary aldosteronism: case detection, diagnosis, and treatment: an endocrine society clinical practice guideline. J Clin Endocrinol Metab (2016) 101(5):1889–916. doi: 10.1210/jc.2015-4061
7. Endocrinology Branch of Chinese Medical Association, Expert consensus on the diagnosis and treatment of primary aldosteronism (2020 edition). Chin J Endocrinol Metab (2020) 36(9):727–36. doi: 10.3760/cma.j.cn311282-20200615-00444
8. Rossi GP, Auchus RJ, Brown M, Lenders JW, Naruse M, Plouin PF, et al. An expert consensus statement on use of adrenal vein sampling for the subtyping of primary aldosteronism. Hypertension (2014) 63(1):151–60. doi: 10.1161/HYPERTENSIONAHA.113.02097
9. Daunt N. Adrenal vein sampling: how to make it quick, easy, and successful. Radiographics (2005) 25:S143–58. doi: 10.1148/rg.25si055514
10. Young WF, Stanson AW, Thompson GB, Grant CS, Farley DR, van Heerden JA. Role for adrenal venous sampling in primary aldosteronism. Surgery (2004) 136(6):1227–35. doi: 10.1016/j.surg.2004.06.051
11. Lim V, Guo Q, Grant CS, Thompson GB, Richards ML, Farley DR, et al. Accuracy of adrenal imaging and adrenal venous sampling in predicting surgical cure of primary aldosteronism. J Clin Endocrinol Metab (2014) 99(8):2712–9. doi: 10.1210/jc.2013-4146
12. Umakoshi H, Tsuiki M, Takeda Y, Kurihara I, Itoh H, Katabami T, et al. Significance of computed tomography and serum potassium in predicting subtype diagnosis of primary aldosteronism. J Clin Endocrinol Metab (2018) 103(3):900–8. doi: 10.1210/jc.2017-01774
13. Kupers EM, Amar L, Raynaud A, Plouin PF, Steichen O. A clinical prediction score to diagnose unilateral primary aldosteronism. J Clin Endocrinol Metab (2012) 97(10):3530–7. doi: 10.1210/jc.2012-1917
14. Kocjan T, Janez A, Stankovic M, Vidmar G, Jensterle M. A new clinical prediction criterion accurately determines A subset of patients with bilateral primary aldosteronism before adrenal venous sampling. Endocr Pract (2016) 22(5):587–94. doi: 10.4158/EP15982.OR
15. Kobayashi H, Haketa A, Ueno T, Ikeda Y, Hatanaka Y, Tanaka S, et al. Scoring system for the diagnosis of bilateral primary aldosteronism in the outpatient setting before adrenal venous sampling. Clin Endocrinol (Oxf) (2017) 86(4):467–72. doi: 10.1111/cen.13278
16. Kobayashi H, Abe M, Soma M, Takeda Y, Kurihara I, Itoh H, et al. Development and validation of subtype prediction scores for the workup of primary aldosteronism. J Hypertens (2018) 36(11):2269–76. doi: 10.1097/HJH.0000000000001855
17. Kamemura K, Wada N, Ichijo T, Matsuda Y, Fujii Y, Kai T, et al. Significance of adrenal computed tomography in predicting laterality and indicating adrenal vein sampling in primary aldosteronism. J Hum Hypertension (2017) 31(3):195–9. doi: 10.1038/jhh.2016.61
18. Xiao L, Jiang Y, Zhang C, Jiang L, Zhou W, Su T, et al. A novel clinical nomogram to predict bilateral hyperaldosteronism in Chinese patients with primary aldosteronism. Clin Endocrinol (Oxf) (2019) 90(6):781–8. doi: 10.1111/cen.13962
19. Zhang Y, Niu W, Zheng F, Zhang H, Zhou W, Shen Z, et al. Identifying unilateral disease in Chinese patients with primary aldosteronism by using a modified prediction score. J Hypertens (2017) 35(12):2486–92. doi: 10.1097/HJH.0000000000001488
20. Wu Y, Wu Z, Hu H, Rao J, Hu C, Peng Q, et al. Significance of computed tomography combined with postural stimulation test in predicting laterality of primary aldosteronism. BMC Endocr Disord (2023) 23(1):32. doi: 10.1186/s12902-023-01281-x
21. Brown JM, Siddiqui M, Calhoun DA, Carey RM, Hopkins PN, Williams GH, et al. The unrecognized prevalence of primary aldosteronism: A cross-sectional study. Ann Intern Med (2020) 173(1):10–20. doi: 10.7326/M20-0065
22. Omura M, Sasano H, Saito J, Yamaguchi K, Kakuta Y, Nishikawa T. Clinical characteristics of aldosterone-producing microadenoma, macroadenoma, and idiopathic hyperaldosteronism in 93 patients with primary aldosteronism. Hypertens Res (2006) 29(11):883–9. doi: 10.1291/hypres.29.883
23. Vakkalanka S, Zhao A, Samannodi M. Primary hyperaldosteronism: a case of unilateral adrenal hyperplasia with contralateral incidentaloma. BMJ Case Rep (2016) 2016:bcr2016216209. doi: 10.1136/bcr-2016-216209
24. Das G, Taylor PN, Tabasum A, Rao Bondugulapati LN, Parker D, Baglioni P, et al. Resistant hypertension with adrenal nodule: are we removing the right gland? Endocrinol Diabetes Metab Case Rep 2015 (2015) p:150063. doi: 10.1530/EDM-15-0063
25. Riester A, Fischer E, Degenhart C, Reiser MF, Bidlingmaier M, Beuschlein F, et al. Age below 40 or a recently proposed clinical prediction score cannot bypass adrenal venous sampling in primary aldosteronism. J Clin Endocrinol Metab (2014) 99(6):E1035–9. doi: 10.1210/jc.2013-3789
26. Akasaka H, Yamamoto K, Rakugi H, Nagasawa M, Nakamaru R, Ichijo T, et al. Sex difference in the association between subtype distribution and age at diagnosis in patients with primary aldosteronism. Hypertension (2019) 74(2):368–74. doi: 10.1161/HYPERTENSIONAHA.119.13006
27. Nanba K, Tsuiki M, Nakao K, Nanba A, Usui T, Tagami T, et al. A subtype prediction score for primary aldosteronism. J Hum Hypertens (2014) 28(12):716–20. doi: 10.1038/jhh.2014.20
28. He K, Zhang ZT, Wang ZH, Wang Y, Wang YX, Zhang HZ, et al. A clinical-radiomic nomogram based on unenhanced computed tomography for predicting the risk of aldosterone-producing adenoma. Front Oncol (2021) 11:634879. doi: 10.3389/fonc.2021.634879
29. Williams TA, Monticone S, Schack VR, Stindl J, Burrello J, Buffolo F, et al. Somatic ATP1A1, ATP2B3, and KCNJ5 mutations in aldosterone-producing adenomas. Hypertension (2014) 63(1):188–95. doi: 10.1161/HYPERTENSIONAHA.113.01733
Keywords: primary aldosteronism, subtype diagnosis, computed tomography, serum potassium, sex differences
Citation: Wu Y, Wu Z, Rao J, Hu H, Chen Z, Hu C, Peng Q and Li P (2023) Sex modifies the predictive value of computed tomography combined with serum potassium for primary aldosteronism subtype diagnosis. Front. Endocrinol. 14:1266961. doi: 10.3389/fendo.2023.1266961
Received: 25 July 2023; Accepted: 30 October 2023;
Published: 16 November 2023.
Edited by:
Valentina Morelli, Istituto Auxologico Italiano, ItalyReviewed by:
Krzysztof Cezary Lewandowski, Medical University of Lodz, PolandElisa Sconfienza, University of Turin, Italy
Copyright © 2023 Wu, Wu, Rao, Hu, Chen, Hu, Peng and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ping Li, bGlwaW5nc3lkbmV5QDE2My5jb20=
 Yingxing Wu
Yingxing Wu Zuxiang Wu
Zuxiang Wu Huan Hu
Huan Hu Zhiqiang Chen
Zhiqiang Chen Chenkai Hu
Chenkai Hu Ping Li
Ping Li