- Department of Endocrinology and Metabolism, Institute of Endocrine, National Health Commission (NHC) Key Laboratory of Diagnosis and Treatment of Thyroid Diseases, The First Hospital of China Medical University, Shenyang, China
Introduction: Subclinical hypothyroidism (SCH) is a common endocrine disorder characterized by elevated thyroid-stimulating hormone (TSH) levels and normal free thyroxine (FT4) levels. The overdiagnosis and overtreatment of SCH in elderly patients have become concerns as TSH levels naturally increase with age. Studies have shown that many elderly patients with SCH can recover without treatment, and the administration of levothyroxine (L-T4) does not improve their prognosis. Therefore, It is necessary to establish age-specific reference ranges for TSH in elderly individuals to aid in clinical decision-making and prevent overdiagnosis.
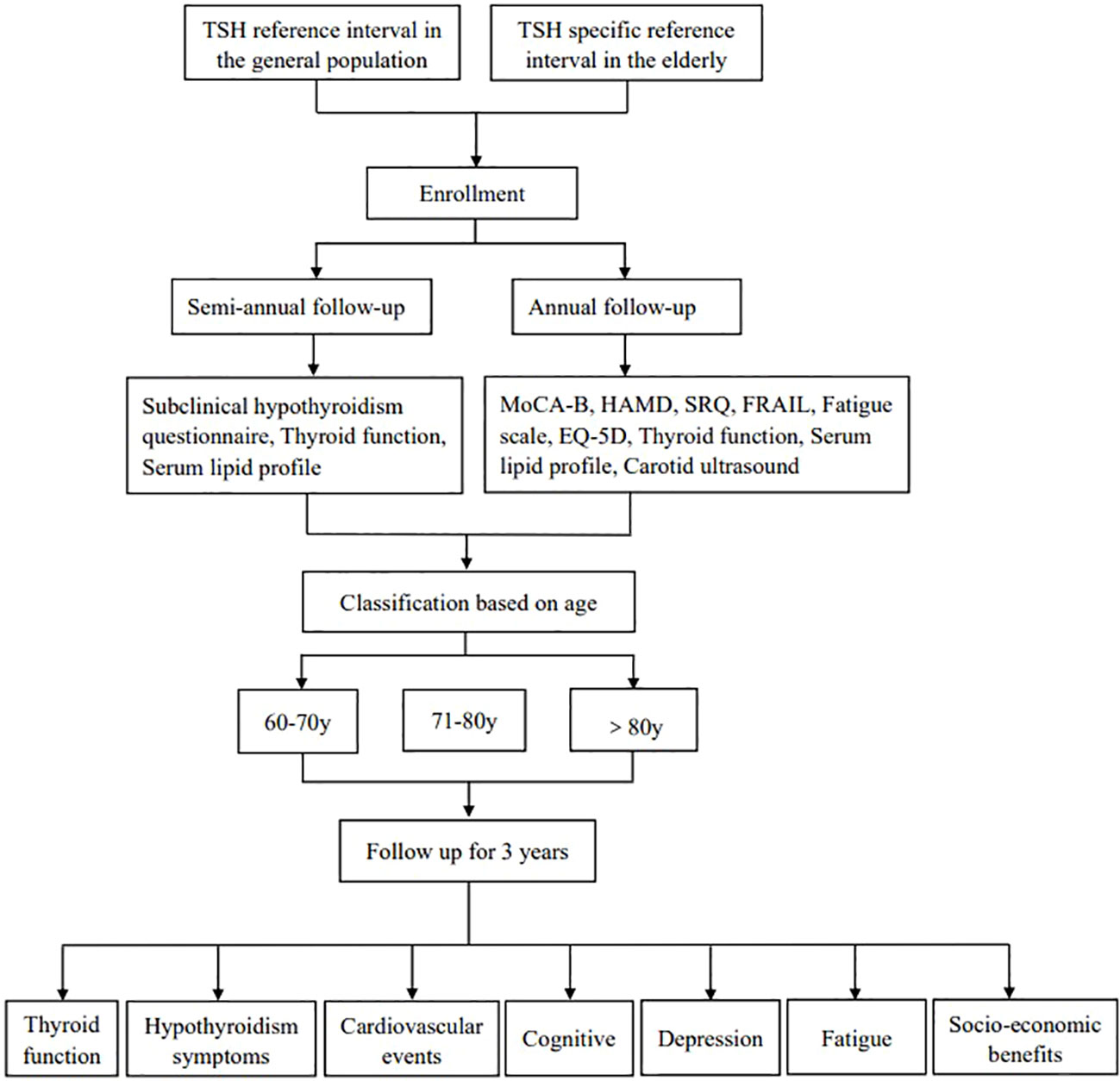
Methods: This is a multicenter prospective study that focuses on Chinese elderly patients with SCH who have TSH levels below 10 mU/L. After obtaining the informed consent of the patients, their initial diagnosis information will be registered, and they will be asked to fill out questionnaires such as the Montreal Cognitive Assessment-Basic (MoCA-B), Hamilton Depression Scale (HAMD), Hypothyroidism Symptom Questionnaire (SRQ), frail scale(FRAIL), fatigue scale, and EQ-5D. In addition, thyroid function tests, blood lipid analysis, carotid artery ultrasound, and thyroid ultrasound examinations will be conducted. Patients will also be grouped according to FT4 levels, the changes in FT4 and its relationship with TSH can also be described. For patients over 80 years old, a decrease in FT4 will be used as an endpoint event, while for patients between 60-80 years old, TSH levels greater than or equal to 10mIU/L or a decline in FT4 will be used as the endpoint event. The TSH reference intervals of the general and elderly populations will be used to calculate medical costs associated with multiple follow-ups of patients, and a social-economic analysis will also be conducted.
Discussion: This study will prospectively observe elderly patients with SCH who are screened using both age-specific and non-age-specific TSH reference ranges for the elderly population. We will compare the results of elderly patients diagnosed with SCH using different reference ranges and analyze their association with FT4 to identify meaningful SCH patients and reduce over diagnosis and over treatment of elderly SCH.
Ethics: The Medical Science Research Ethics Committee of the First Affiliated Hospital of China Medical University approved this study (ID: AF-SOP-07-1.1-01). The results will be published in an open-access journal.
Clinical trial registration: https://www.chictr.org.cn/, identifier ChiCTR2300070831.
Introduction
Subclinical hypothyroidism (SCH) is characterized by elevated serum thyroid-stimulating hormone (TSH) and normal thyroid hormone levels (1). As TSH is considered a good indicator of thyroid function, the diagnosis of SCH is primarily based on TSH levels. However, this can lead to overdiagnosis and overtreatment in elderly patients with SCH, as their TSH levels may naturally increase with age without indicating an underlying thyroid dysfunction (2).
Many studies have found that the incidence rate of SCH increases significantly with age (3, 4), which suggests that we need to consider the impact of aging on the hypothalamic-pituitary-thyroid (HPT) axis. For example, aging may weaken the circadian rhythm of TSH and reduce its responsiveness (5). According to the cross-sectional National Health and Nutrition Examination Survey (NHANES) III, the average TSH of adults aged 80 is 69% higher than that of adults aged 20 (6, 7). Data from Scottish, and Australia also confirm that TSH level increases with age (8–10). Our previous epidemiological survey in ten cities indicated that the prevalence of SCH in people over 65 years old was 19.87% according to the current TSH reference interval, but when the age-specific TSH reference range was used, the prevalence decreased to 3.3% (3). Although the mechanism is unclear, the increase in TSH in the elderly may be a normal phenomenon associated with aging. When the current diagnostic criteria are used, many elderly patients with no clinical significance will be diagnosed.
Prospective research on the natural outcome of the elderly indicated the above problem. In 2004, a study from Spain followed up 107 elderly patients with SCH over 55 years of age for 6 years (11), and the proportion of patients’ disease progression, maintenance, and recovery were 26.8%, 35.8%, and 37.4% respectively, that is, only a few patients had significant progress. In 2012, an American study conducted a 4-year follow-up of 459 elderly patients with SCH over 65 years old and found that 56% of the patients were in the state of SCH maintenance in the second and fourth years of follow-up (12). In addition, the remission rate of TPOAb-negative patients is significantly higher than that of TPOAb-positive patients. In 2017, a Chinese study conducted a 3-year follow-up of 505 patients with SCH over the age of 40 and found that only 3.4% had progressed, while 43.8% were in maintenance, and 49.7% returned to normal (13). It was also believed that TPOAb, TSH levels, creatinine, and total cholesterol levels were related to different outcomes of SCH. That is, many elderly patients with SCH may have stable or even recovery of their condition without any intervention, while only a few of them have progressed and need treatment, which suggests that using the current unified TSH reference interval of the entire population to diagnose SCH in the elderly may lead to overdiagnosis and overtreatment. To avoid this, it is recommended to establish age-specific TSH reference ranges for the elderly to better identify those who may require treatment. This approach can help prevent unnecessary interventions in patients with SCH and reduce potential adverse effects of overtreatment.
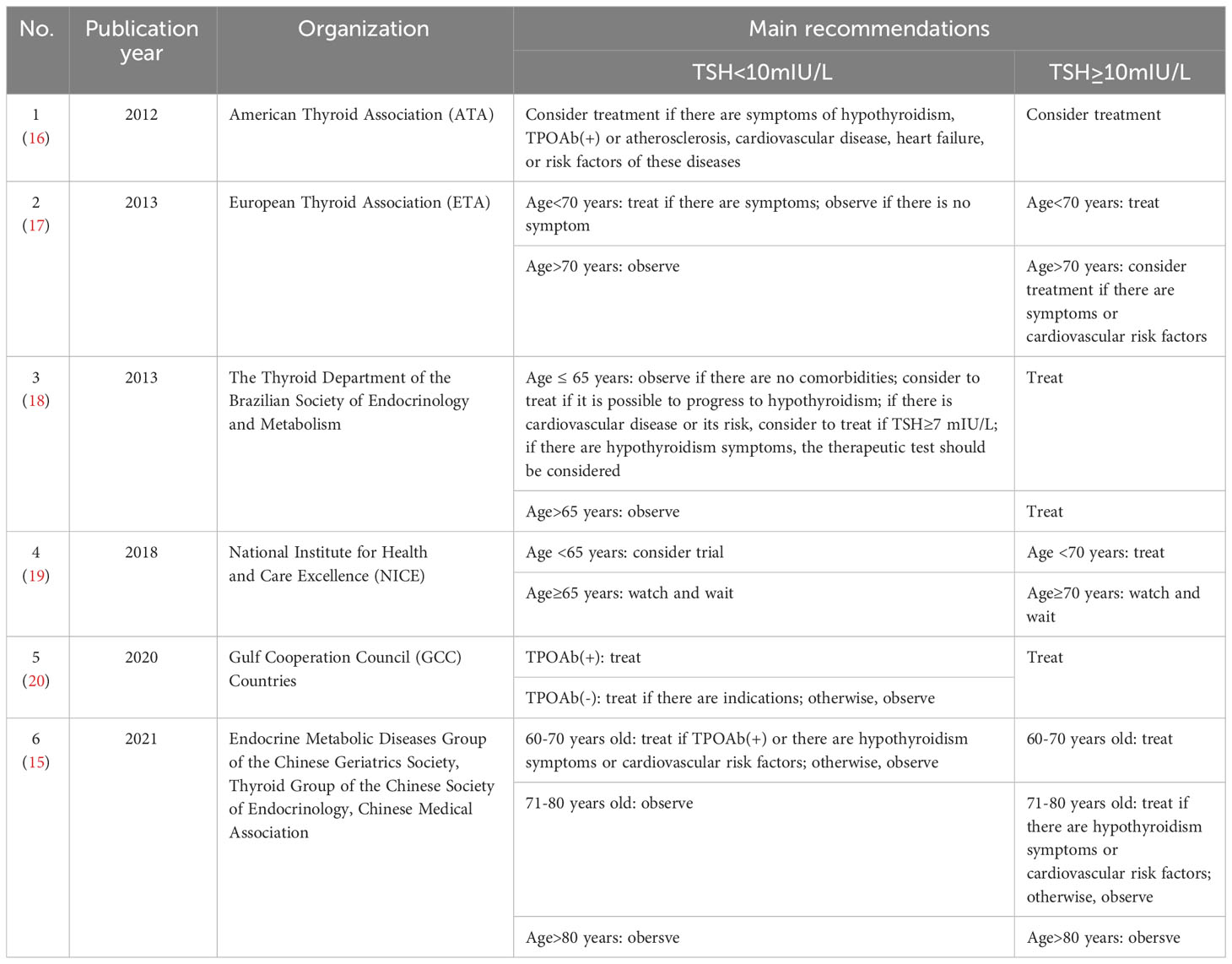
In recent years, there has been increasing attention from experts worldwide toward the management of SCH in elderly patients. Many countries have started to revise their guidelines accordingly to provide more tailored recommendations for the screening, diagnosis, and treatment of SCH in the elderly. In 2020, the French expert consensus proposed that individualized treatment should be adopted for elderly patients with SCH (14). In 2021, experts from China also advocated jointly determining whether treatment is needed according to age, TSH level, symptoms, cardiovascular risk factors, etc (15). The guidelines of other regions are listed in Table 1. These guidelines have great differences and lack reliable epidemiological research support, which is also one of the purposes of our prospective research.
In the process of SCH, we need to consider the adverse outcomes of cardiovascular and cognitive functions. The thyroid hormone is closely related to the cardiovascular system and plays a key role in the regulation of cardiac muscle cell inotropic and chronotropic effects (21, 22). SCH is generally considered a risk factor for cardiovascular disease and cardiovascular-related death events. At present, some studies have shown that the prediction of cardiovascular disease and mortality in elderly patients with SCH should be based on age and TSH level (23–26). The prognosis of the elderly is good, and TSH>10mU/L is often associated with the occurrence of cardiovascular diseases, which need further confirmation. For cognitive function, the thyroid hormone plays a key role in brain development and maturation, so abnormal thyroid function and hormone secretion may affect the neuropsychiatric system (27). Although thyroid function examination is usually performed in patients with cognitive impairment or depression, the relationship between SCH and neurological and psychological functions is still unclear. However, previous research suggested that SCH in the elderly has nothing to do with cognitive decline or dementia events, so it may not be necessary to conduct SCH screening in the elderly with cognitive decline (28–30). It is noteworthy that some studies have found that elderly patients with SCH may be prone to depression, but the results are inconsistent (31–33). Therefore, our research will focus on the cardiovascular disease and depression of patients.
Methods
Research type
This study adopts the methodological strategy of the cohort study in analytical epidemiology to carry out various data collection, diagnostic test analysis around the gold standard and the test data of diagnostic subjects, and economic analysis.
Research objectives and main results
The goal of this study is to prospectively follow up on elderly patients with SCH who are diagnosed using age-specific TSH reference intervals and non-age-specific TSH reference intervals, which aims to establish TSH reference intervals for different age groups to improve the diagnosis and management of SCH in the elderly. The main outcomes being assessed include thyroid function, hypothyroidism-related symptoms, cardiovascular events, cognition, depression, and fatigue, as well as economic and social benefits analysis. The above information will help make informed decisions about the best course of treatment for elderly patients with SCH.
Study population
We are conducting a prospectively observational study on patients over 60 years of age diagnosed with SCH. The study was conducted in the First Affiliated Hospital of China Medical University and the West China Hospital of Sichuan University. Patients will be included from December 2022 to December 2023, and the follow-up data will be collected until December 2025.
Inclusion criteria and exclusion criteria
Inclusion criteria:
Elderly patients with SCH will be included according to the elderly and the general population-specific reference ranges, respectively.
(1) Inpatients and/or outpatients aged≥60 years.
(2) The levels of free triiodothyronine(FT3) and FT4 are within the normal range.
(3) TSH is greater than the upper limit of the normal reference range (old standard) and less than the upper limit of the normal reference range (new standard).
Exclusion criteria:
(1) Does not meet the inclusion criteria, does not sign the consent form, or participates involuntarily.
(2) Exit halfway due to various reasons.
(3) Unable to cooperate with the project team to complete all inspection contents.
(4) Other factors leading to TSH increase. 1) increased TSH caused by measurement errors; 2) convalescence stage of the euthyroid sick syndrome; 3) central hypothyroidism; 4) renal insufficiency; 5) lack of glucocorticoids; 6) the recovery stage of thyroid function in subacute thyroiditis; 7) having taken amiodarone or lithium; 8) other interfering factors.
Public involvement
All patients will participate in the study voluntarily and sign an informed consent form. This study will be based on patient and public participation. We will complete the questionnaire by asking patients questions and promoting medical knowledge by establishing good relationships with patients.
Study follow-up assessments
When a patient has FT4 levels below the lower limit of the normal reference range during follow-up, follow-up is terminated and thyroid hormone replacement therapy will be initiated. For patients aged 60 to 70 years, start treatment when TSH≥10mIU/L. For patients aged 71 to 80 years, treatment begins when TSH≥10 mIU/L and is accompanied by symptoms of hypothyroidism. Normal value reference ranges will be established based on the TSH levels of 120 normal elderly individuals over 60. Elderly SCH patients screened according to the TSH reference interval in the normal population and the elderly population will be followed up every 6 months, including the subclinical hypothyroidism questionnaire, the Montreal Cognitive Assessment-Basic (MoCA-B), Hamilton Depression Scale (HAMD), Hypothyroidism Symptom Questionnaire (SRQ), frail scale(FRAIL), fatigue scale, EQ-5D, thyroid function, blood lipid analysis, carotid color ultrasound, and thyroid ultrasound. The estimated sample size is 438. Patients diagnosed with different TSH reference intervals will be compared for cognitive function, depression scores, hypothyroidism, fatigue severity, carotid atherosclerosis, lipid profile, and cardiocerebrovascular complications. Besides, TSH reference intervals will be applied to calculate medical costs and evaluate the economic benefits of multiple follow-ups of patients with SCH. The research design can be seen in Figure 1.
The scoring breakdown of MoCA-B is as follows: visuospatial and executive functioning: 5 points; animal naming: 3 points; attention: 6 points; language: 3 points; abstraction: 2 points; delayed recall (short-term memory): 5 points; orientation: 6 points; education level: 1 point is added to the score if they have 12 years or less of formal education. A total score of 26 or greater is within the normal range. Using HAMD to assess the degree of depression: 10-13 mild; 14-17 mild to moderate; >17 moderate to severe. The FRAIL consists of five questions with a score of 0-5 (0: for the best state, 5: for the worst state), 3-5 for frailty, 1-2 for pre-frailty, and 0 for physical fitness.
Research quality control
The collection of questionnaire information and the biological specimen will be conducted by doctors, nurses, or investigators with work experience. Data management and quality control will be carried out for data entry, export, storage, and other aspects. Concerning the quality control of biological samples, the collection, pretreatment, transfer, freezing, and other related processes will be carried out in strict accordance with the relevant Standard Operation Procedure standards. At the same time, random inspection will be carried out on all kinds of work from sample collection to detection to ensure sample quality.
The testing and laboratory processing units are the Laboratory of the First Affiliated Hospital of China Medical University and the West China Hospital, Sichuan University. This study will strictly follow the hospital’s laboratory processing approval process for filing and operation.
Concerning data management and security, all kinds of data in this study will be uniformly saved, and all members, temporary employees, and students will sign a confidentiality agreement.
Data analysis
We will calculate age-specific TSH reference intervals based on the obtained data, analyze the natural outcomes, the occurrence of cardiovascular events, cognitive status, depression, and fatigue of elderly patients with SCH diagnosed under different reference intervals, and conduct economic analysis.
Continuous data will be expressed as mean ± standard deviation or median with a range of quartiles. Classification data will be expressed in numbers with percentages. Cox proportional risk model will be used to evaluate survival results. The variables measured several times during the follow-up period will be compared with the paired t-test according to the clinical management used. The significance level will be set to 0.05, and R software, prodlim, and Cairo software will be used to analyze the data.
Limitations
Due to the significant variability in TSH levels, we cannot guarantee whether the diagnosis of patients has been affected by the fluctuations in TSH. We can only strive to have patients undergo two repeated measurements whenever possible, and make an effort to select the same time point for testing. Considering the significance of T4, we plan to establish a diagnostic indicator that combines both T4 and TSH.
Discussion
The specific TSH reference interval of elderly patients with SCH and its management deserve attention (34). In recent years, experts have recognized that the management of elderly patients with SCH needs to follow the principle of individualization (35), and much current research indicated that L-T4 has not shown any improvement in the treatment of cardiovascular disease mortality, cognitive function, depression, fatigue, hypothyroidism and other symptoms of elderly patients (36–40), which make us consider that the reference range of TSH for the elderly needs to be revised. Distinguishing from the reference interval of TSH for the whole population will effectively identify the truly meaningful patients with SCH, avoid over-diagnosis and save social resources.
To confirm its necessity and establish an age-specific TSH reference interval, we conducted this prospective study of the natural outcomes of elderly patients with SCH diagnosed by different reference ranges of TSH. In addition, the economic benefits will also be evaluated. In a word, our study will facilitate the accurate discrimination of high-risk patients in future clinical diagnosis and treatment, and avoid overdiagnosis and overtreatment.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material. Further inquiries can be directed to the corresponding author.
Author contributions
XZ is the first author of this study. XT is the corresponding author supervising this work. XZ drafted the manuscript. YL provided major technical support. JJ, HW, BZ and SW assisted in the literature review. ZS and WT checked the manuscript. All authors contributed to the article and approved the submitted version.
Funding
This study was supported by the National Key Technologies R&D Program provided by Ministry of Science and Technology of the People’s Republic of China (Project Grant # 2022YFC3602300, Sub-project Grant # 2022YFC3602303).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
SCH, Subclinical hypothyroidism; TSH, Thyroid-stimulating hormone; HPT, Hypothalamic-pituitary-thyroid; FT4, Free thyroxine; L-T4, Levothyroxine; MoCA-B, Montreal Cognitive Assessment-Basic; HAMD, Hamilton Depression Scale; SRQ, Hypothyroidism Symptom Questionnaire, FRAIL, Frail scale.
References
1. Biondi B, Cappola AR, Cooper DS. Subclinical hypothyroidism: A review. JAMA (2019) 322(2):153–60. doi: 10.1001/jama.2019.9052
2. Hershman JM, Beck-Peccoz P. Discoveries around the hypothalamic-pituitary-thyroid axis. Thyroid (2023) 33(7):785–90. doi: 10.1089/thy.2022.0258
3. Zhai X, Zhang L, Chen L, Lian X, Liu C, Shi B, et al. An age-specific serum thyrotropin reference range for the diagnosis of thyroid diseases in older adults: A cross-sectional survey in China. Thyroid (2018) 28(12):1571–9. doi: 10.1089/thy.2017.0715
4. Li Y, Teng D, Ba J, Chen B, Du J, He L, et al. Efficacy and safety of long-term universal salt iodization on thyroid disorders: epidemiological evidence from 31 provinces of Mainland China. Thyroid (2020) 30(4):568–79. doi: 10.1089/thy.2019.0067
5. Mammen JS. Interpreting elevated TSH in older adults. Curr Opin Endocr Metab Res (2019) 5:68–73. doi: 10.1016/j.coemr.2019.04.001
6. Hollowell JG, Staehling NW, Flanders WD, Hannon WH, Gunter EW, Spencer CA, et al. Serum TSH, T4, and thyroid antibodies in the United States population (1988 to 1994): national health and nutrition examination survey (NHANES III). J Clin Endocrinol Metab (2002) 87(2):489–99. doi: 10.1210/jcem.87.2.8182
7. Surks MI, Hollowell JG. Age-specific distribution of serum thyrotropin and antithyroid antibodies in the US population: implications for the prevalence of subclinical hypothyroidism. J Clin Endocrinol Metab (2007) 92(12):4575–82. doi: 10.1210/jc.2007-1499
8. Vadiveloo T, Donnan PT, Murphy MJ, Leese GP. Age- and gender-specific TSH reference intervals in people with no obvious thyroid disease in Tayside, Scotland: the Thyroid Epidemiology, Audit, and Research Study (TEARS). J Clin Endocrinol Metab (2013) 98(3):1147–53. doi: 10.1210/jc.2012-3191
9. Hadlow NC, Rothacker KM, Wardrop R, Brown SJ, Lim EM, Walsh JP. The relationship between TSH and free T(4) in a large population is complex and nonlinear and differs by age and sex. J Clin Endocrinol Metab (2013) 98(7):2936–43. doi: 10.1210/jc.2012-4223
10. Yeap BB, Manning L, Chubb SAP, Hankey GJ, Golledge J, Almeida OP, et al. Reference ranges for thyroid-stimulating hormone and free thyroxine in older men: results from the health in men study. J Gerontol A Biol Sci Med Sci (2016) 72(3):444–9. doi: 10.1093/gerona/glw132
11. Diez JJ, Iglesias P. Spontaneous subclinical hypothyroidism in patients older than 55 years: an analysis of natural course and risk factors for the development of overt thyroid failure. J Clin Endocrinol Metab (2004) 89(10):4890–7. doi: 10.1210/jc.2003-032061
12. Somwaru LL, Rariy CM, Arnold AM, Cappola AR. The natural history of subclinical hypothyroidism in the elderly: the cardiovascular health study. J Clin Endocrinol Metab (2012) 97(6):1962–9. doi: 10.1210/jc.2011-3047
13. Li X, Zhen D, Zhao M, Liu L, Guan Q, Zhang H, et al. Natural history of mild subclinical hypothyroidism in a middle-aged and elderly Chinese population: a prospective study. Endocr J (2017) 64(4):437–47. doi: 10.1507/endocrj.EJ16-0549
14. Goichot B, Raverot V, Klein M, Vija Racaru L, Abeillon-Du Payrat J, Lairez O, et al. Management of thyroid dysfunctions in the elderly. French Endocr Soc consensus statement 2019 Long version Ann Endocrinol (Paris) (2020) 81(2-3):89–100. doi: 10.1016/j.ando.2020.04.010
15. Liu Y, Shan Z; Endocrine Metabolic Diseases Group of the Chinese Geriatrics Society; Thyroid Group of the Chinese Society of Endocrinology, Chinese Medical Association. Expert consensus on diagnosis and treatment for elderly with thyroid diseases in China. Aging Med (Milton) (2021) 4(2):70–92. doi: 10.1002/agm2.12165
16. Garber JR CR, Gharib H, Hennessey JV, Klein I, Mechanick JI, Pessah-Pollack R, et al. Clinical practice guidelines for hypothyroidism in adults: cosponsored by the American Association of Clinical Endocrinologists and the American Thyroid Association. Endocr Pract (2012) 18(6):988–1028. doi: 10.4158/EP12280
17. Pearce SH, Brabant G, Duntas LH, Monzani F, Peeters RP, Razvi S, et al. ETA guideline: management of subclinical hypothyroidism. Eur Thyroid J (2013) 2(4):215–28. doi: 10.1159/000356507
18. Sgarbi JA, Maciel LMZ, Mazeto GMFS, Vaisman M, Montenegro RM,, Ward LS. The Brazilian consensus for the clinical approach and treatment of subclinical hypothyroidism in adults: recommendations of the thyroid Department of the Brazilian Society of Endocrinology and Metabolism. Arq Bras Endocrinol Metab (2013) 57(3):166–83. doi: 10.1590/s0004-27302013000300003
19. Excellence. NIfHaC. Clinical Knowlegde Summaries. Subclinical hypothyroidism (non-pregnant) (2019). Available at: https://cksniceorguk/hypothyroidism#!scenario:1.
20. Alzahrani AS, Al Mourad M, Hafez K, Almaghamsy AM, Alamri FA, Al Juhani NR, et al. Diagnosis and management of hypothyroidism in gulf cooperation council (GCC) countries. Adv Ther (2020) 37(7):3097–111. doi: 10.1007/s12325-020-01382-2
21. Ochs N AR, Bauer DC, Nanchen D, Gussekloo J, Cornuz J, Rodondi N. Meta-analysis: subclinical thyroid dysfunction and the risk for coronary heart disease and mortality. Ann Intern Med (2008) 148(11):832–45. doi: 10.7326/0003-4819-148-11-200806030-00225
22. Rodondi N, den Elzen W, Bauer DC, Cappola AR, Razvi S, JP W, Gusseklo J, et al. Subclinical hypothyroidism and the risk of coronary heart disease and mortality. JAMA (2010) 304(12):1365–74. doi: 10.1001/jama.2010.1361
23. Nanchen D, Gussekloo J, Westendorp RG, Stott DJ, Jukema JW, Trompet S, et al. Subclinical thyroid dysfunction and the risk of heart failure in older persons at high cardiovascular risk. J Clin Endocrinol Metab (2012) 97(3):852–61. doi: 10.1210/jc.2011-1978
24. Gencer B, Collet TH, Virgini V, Bauer DC, Gussekloo J, Cappola AR, et al. Subclinical thyroid dysfunction and the risk of heart failure events: an individual participant data analysis from 6 prospective cohorts. Circulation (2012) 126(9):1040–9. doi: 10.1161/CIRCULATIONAHA.112.096024
25. Thayakaran R, Adderley NJ, Sainsbury C, Torlinska B, Boelaert K, Sumilo D, et al. Thyroid replacement therapy, thyroid stimulating hormone concentrations, and long term health outcomes in patients with hypothyroidism: longitudinal study. BMJ (2019) 366:l4892. doi: 10.1136/bmj.l4892
26. Groothof D, Flores-Guerrero JL, Nolte IM, Bouma HR, Gruppen EG, Bano A, et al. Thyroid function and risk of all-cause and cardiovascular mortality: a prospective population-based cohort study. Endocrine (2021) 71(2):385–96. doi: 10.1007/s12020-020-02397-z
27. Przybylak M, Grabowski J, Bidzan L. Cognitive functions and thyroid hormones secretion disorders. Psychiatr Pol (2021) 55(2):309–21. doi: 10.12740/PP/112470
28. Pasqualetti G, Pagano G, Rengo G, Ferrara N, Monzani F. Subclinical hypothyroidism and cognitive impairment: systematic review and meta-analysis. J Clin Endocrinol Metab (2015) 100(11):4240–8. doi: 10.1210/jc.2015-2046
29. Akintola AA, Jansen SW, van Bodegom D, van der Grond J, Westendorp RG, de Craen AJ, et al. Subclinical hypothyroidism and cognitive function in people over 60 years: a systematic review and meta-analysis. Front Aging Neurosci (2015) 7:150. doi: 10.3389/fnagi.2015.00150
30. van Vliet NA, van Heemst D, Almeida OP, Asvold BO, Aubert CE, Bae JB, et al. Association of thyroid dysfunction with cognitive function: an individual participant data analysis. JAMA Intern Med (2021) 181(11):1440–50. doi: 10.1001/jamainternmed.2021.5078
31. Blum MR, Wijsman LW, Virgini VS, Bauer DC, den Elzen WP, Jukema JW, et al. Subclinical thyroid dysfunction and depressive symptoms among the elderly: A prospective cohort study. Neuroendocrinology (2016) 103(3-4):291–9. doi: 10.1159/000437387
32. Tang R, Wang J, Yang L, Ding X, Zhong Y, Pan J, et al. Subclinical hypothyroidism and depression: A systematic review and meta-analysis. Front Endocrinol (2019) 10:340. doi: 10.3389/fendo.2019.00340
33. Loh HH, Lim LL, Yee A, Loh HS. Association between subclinical hypothyroidism and depression: an updated systematic review and meta-analysis. BMC Psychiatry (2019) 19(1):12. doi: 10.1186/s12888-018-2006-2
34. Raverot V, Bonjour M, Abeillon du Payrat J, Perrin P, Roucher-Boulez F, Lasolle H, et al. Age- and sex-specific TSH upper-limit reference intervals in the general french population: there is a need to adjust our actual practices. J Clin Med (2020) 9(3):792. doi: 10.3390/jcm9030792
35. Cook R, Fortescue-Webb D, Taft R, Centre ND. Repeat thyroid function tests for healthy older people are not needed. BMJ (2019) 364:l805. doi: 10.1136/bmj.l805
36. Stott DJ, Rodondi N, Kearney PM, Ford I, Westendorp RGJ, Mooijaart SP, et al. Thyroid hormone therapy for older adults with subclinical hypothyroidism. N Engl J Med (2017) 376(26):2534–44. doi: 10.1056/NEJMoa1603825
37. Stuber MJ, Moutzouri E, Feller M, Del Giovane C, Bauer DC, Blum MR, et al. Effect of thyroid hormone therapy on fatigability in older adults with subclinical hypothyroidism: A nested study within a randomized placebo-controlled trial. J Gerontol A Biol Sci Med Sci (2020) 75(9):e89–94. doi: 10.1093/gerona/glaa123
38. de Montmollin M, Feller M, Beglinger S, McConnachie A, Aujesky D, Collet TH, et al. L-thyroxine therapy for older adults with subclinical hypothyroidism and hypothyroid symptoms: secondary analysis of a randomized trial. Ann Intern Med (2020) 172(11):709–16. doi: 10.7326/M19-3193
39. Gonzalez Rodriguez E, Stuber M, Del Giovane C, Feller M, Collet TH, Lowe AL, et al. Skeletal effects of levothyroxine for subclinical hypothyroidism in older adults: A TRUST randomized trial nested study. J Clin Endocrinol Metab (2020) 105(1):dgz058. doi: 10.1210/clinem/dgz058
Keywords: subclinical hypothyroidism (SCH), TSH, natural outcomes, study protocol, reference intervals
Citation: Zhang X, Li Y, Jin J, Wang H, Zhao B, Wang S, Shan Z, Teng W and Teng X (2023) The different outcomes in the elderly with subclinical hypothyroidism diagnosed by age-specific and non-age-specific TSH reference intervals: a prospectively observational study protocol. Front. Endocrinol. 14:1242110. doi: 10.3389/fendo.2023.1242110
Received: 18 June 2023; Accepted: 19 September 2023;
Published: 15 November 2023.
Edited by:
Paolo Miccoli, University of Pisa, ItalyReviewed by:
Stephen Fitzgerald, Royal Adelaide Hospital, AustraliaAna Valea, Iuliu Hatieganu University of Medicine and Pharmacy, Romania
Copyright © 2023 Zhang, Li, Jin, Wang, Zhao, Wang, Shan, Teng and Teng. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xiaochun Teng, dGVuZ3hpYW9jaHVuQDEyNi5jb20=
 Xueqi Zhang
Xueqi Zhang Yang Li
Yang Li Jing Jin
Jing Jin Weiping Teng
Weiping Teng Xiaochun Teng
Xiaochun Teng