
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
EDITORIAL article
Front. Endocrinol. , 11 May 2023
Sec. Clinical Diabetes
Volume 14 - 2023 | https://doi.org/10.3389/fendo.2023.1214479
This article is part of the Research Topic Prediabetes: New Insights on the Diagnosis, Risk Stratification, Comorbidites, Cardiovascular Disease, Microvascular Complications, and Treatment View all 7 articles
Editorial on the Research Topic
Prediabetes: new insights on the diagnosis, risk stratification, comorbidites, cardiovascular disease, microvascular complications, and treatment
Prediabetes is a highly prevalent condition affecting more than one-third of adults in the US and more than one-fifth in Europe (1, 2). In addition to the well-known increased risk of progression to diabetes, prediabetes is also associated with an increased risk of cardiovascular complications (3). The focus on mechanisms and interventions to reduce the risk of cardio-renal complications in prediabetes is markedly less than that on preventing diabetes (3). More research is needed to better characterize new markers of microvascular and macrovascular risk in prediabetes and to develop new interventions to minimize this risk. In the Research Topic “Prediabetes: New Insights on Diagnosis, Risk Stratification, Comorbidities, Cardiovascular Disease, Microvascular Complications, and Treatment” the authors have made significant contributions to the field of prediabetes (Shu et al., Wang et al., Cloro et al., Wang et al., Zhu et al., Wang et al.) (Figure 1).
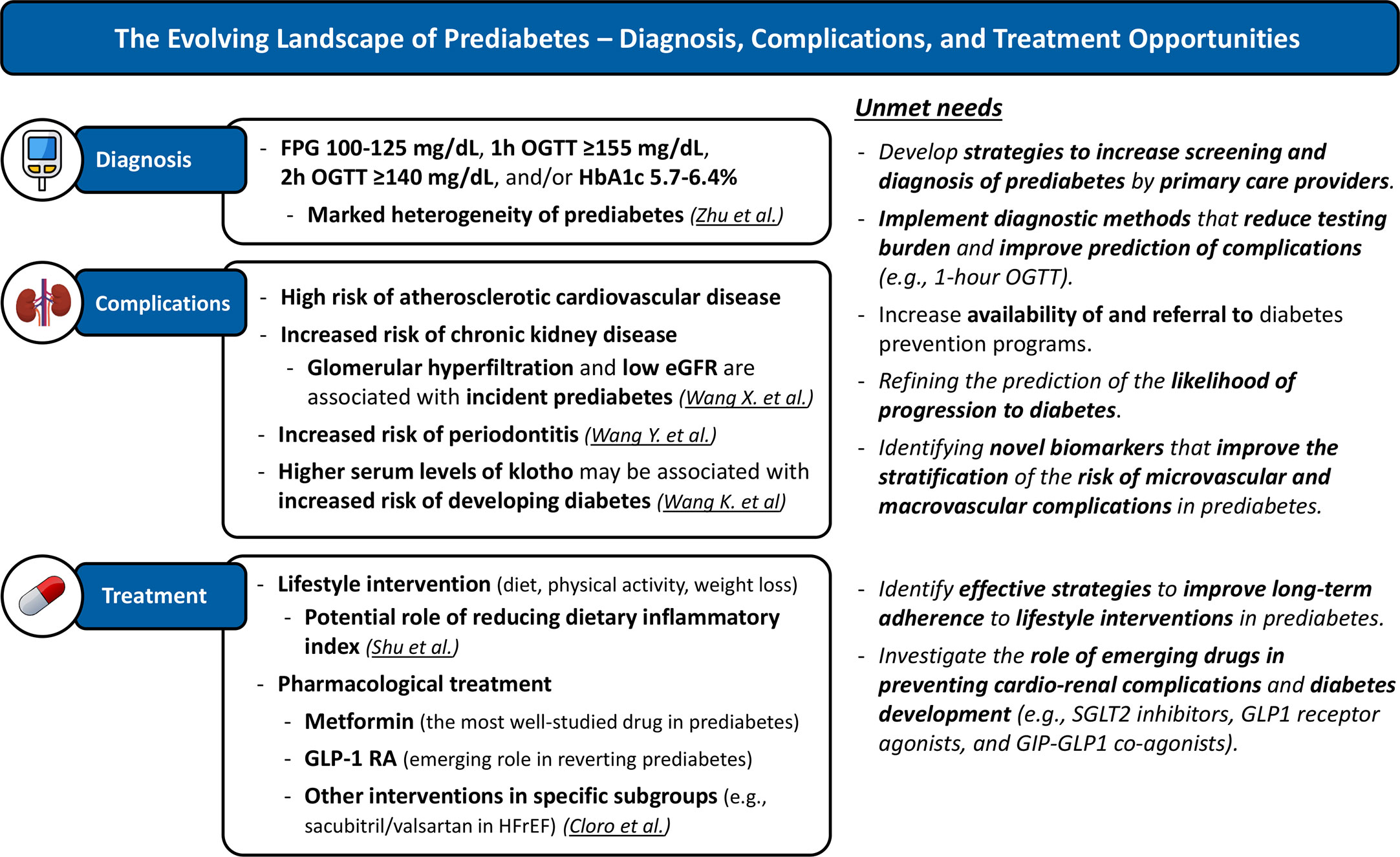
Figure 1 The Evolving Landscape of Prediabetes – Diagnosis, Complications, and Treatment Opportunities. Current knowledge and unmet needs. Underlined text highlights contributions made by articles published in the special topic “Prediabetes: New Insights on Diagnosis, Risk Stratification, Comorbidities, Cardiovascular Disease, Microvascular Complications, and Treatment”. eGFR, estimated glomerular filtration rate; FPG, fasting plasma glucose; GLP-1 RA, GLP-1 receptor agonists; HFrEF, heart failure with reduced ejection fraction; OGTT, oral glucose tolerance test; SGLT2i, SGLT2 inhibitors.
Zhu et al. conducted a population-based longitudinal study to identify factors correlated with targeted prevention of prediabetes. This study provides several relevant conclusions. First, consistent with previous reports (Wang et al.), there was a minimal overlap between the different definitions of prediabetes; only about 10% of participants with prediabetes met all three ADA (American Diabetes Association) criteria for prediabetes. Second, adiposity and obesity-related parameters were significantly associated with prediabetes, which further reinforces the central role of obesity for the development of glycemic dysfunction. Lastly, this study revealed interesting patterns in the distribution of prediabetes criteria in the Chinese population studied. Men were more likely to have impaired fasting glucose (IFG), while women were more likely to have impaired glucose tolerance (IGT). Additionally, different anthropometric parameters may be associated with different prediabetes criteria. Overall, these results emphasize the heterogeneity of prediabetes and highlight the need for targeted interventions in the diagnosis and treatment of prediabetes.
Shu et al. investigated the role of the dietary inflammatory index in prediabetes and insulin resistance among American adults. Their findings suggest that a pro-inflammatory diet, such as diets rich in processed meats (e.g., bacon) refined carbohydrates (e.g., white bread) or sugar-sweetened beverages, is associated with higher fasting plasma glucose (FPG), fasting serum insulin, and HOMA-IR, and consequently increases the odds of prediabetes and insulin resistance. These results suggest that dietary interventions focused on reducing the dietary inflammatory index may configure a novel approach for the prevention of glycemic disorders.
While the association of diabetes with microvascular and macrovascular complications is well known, less well known is the relationship of these complications with prediabetes. However, a growing body of evidence suggests that prediabetes is associated with an increased risk of both microvascular and macrovascular complications (4). Wang et al. in this special issue explored the association between estimated glomerular filtration rate (eGFR) and incident IFG in the Chinese population with normal FPG at baseline. They showed an association between reduced renal function and increased glomerular perfusion with an increased risk of developing IFG. This study illustrates that glomerular hyperfiltration may be a common manifestation of kidney dysfunction with recent progression from normoglycemia to prediabetes.
Wang et al., evaluated the association between serum levels of Klotho (a membrane protein originally described to possess anti-aging properties) and the prevalence of diabetes among adults in the United States. They found a nonlinear and positive association between serum Klotho levels and the prevalence of diabetes. Given the potential role of the Klotho and FGF23 signaling pathways on cardiovascular and renal function (5, 6), further studies evaluating the role of Klotho across the continuum of glycemic dysfunction may offer new approaches to prevent cardio-renal complications in both prediabetes and diabetes.
One of the most overlooked complications of hyperglycemia is periodontitis (7). Wang et al. used a Mendelian randomization approach to investigate the causal relationship between fasting glucose and periodontitis. Their findings confirm previous observations (7) and provide additional evidence to support a causal effect of hyperglycemia on periodontitis. This study underscores the importance of prevention, early detection, and timely treatment of periodontitis in patients with prediabetes and diabetes.
Cloro et al. assessed the effects of sacubitril/valsartan, a combined angiotensin receptor blocker and inhibitor of neprilysin (an enzyme that degrades several vasoactive peptides, including natriuretic peptides), on glycemic and metabolic parameters, insulin resistance, and echocardiographic parameters in patients with prediabetes and heart failure with reduced ejection fraction (HFrEF). Their results suggest that sacubitril/valsartan improves metabolic control and insulin resistance in this population. These results are consistent with a meta-analysis that demonstrated the efficacy of angiotensin-converting enzyme inhibitors or angiotensin II receptor blockers in reducing the risk of new-onset type 2 diabetes (8). The increase in natriuretic peptides with neprilysin inhibition may further promote insulin sensitivity and improve glycemic control (9), as elegantly discussed in the paper by Cloro et al. Further studies should evaluate if neprilysin inhibition could have a role in preventing or treating prediabetes in individuals without heart failure.
Prediabetes research has much to uncover (Figure 1). Future studies should focus on: 1) creating effective strategies to increase screening and identification of prediabetes by primary care providers; 2) increasing availability of and referral to diabetes prevention programs (10); 3) introducing diagnostic methods that decrease testing burden and improve prediction of progression to type 2 diabetes, complications and mortality (e.g., 1-hour OGTT) (11); 4) refining stratification of the risk of cardio-renal complications and likelihood of progression to diabetes; and 5) understanding the role of emerging drugs in preventing cardiovascular complications and diabetes development (e.g., SGLT2 inhibitors, GLP-1 receptor agonists, and GLP-1/GIP- dual agonists). We encourage researchers to prioritize studies on prediabetes, as interventions in this phase may yield greater long-term health benefits compared to those with more advanced stages of glycemic dysfunction.
All authors listed have made a substantial, direct, and intellectual contribution to the work and approved it for publication.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Davidson KW, Barry MJ, Mangione CM, Cabana M, Caughey AB, Davis EM, et al. Screening for prediabetes and type 2 diabetes: US preventive services task force recommendation statement. Jama (2021) 326(8):736–43. doi: 10.1001/jama.2021.12531
2. Eades CE, France EF, Evans JM. Prevalence of impaired glucose regulation in Europe: a meta-analysis. Eur J Public Health (2016) 26(4):699–706. doi: 10.1093/eurpub/ckw085
3. Neves JS, Newman C, Bostrom JA, Buysschaert M, Newman JD, Medina JL, et al. Management of dyslipidemia and atherosclerotic cardiovascular risk in prediabetes. Diabetes Res Clin Pract (2022) 190:109980. doi: 10.1016/j.diabres.2022.109980
4. Gujral UP, Jagannathan R, He S, Huang M, Staimez LR, Wei J, et al. Association between varying cut-points of intermediate hyperglycemia and risk of mortality, cardiovascular events and chronic kidney disease: a systematic review and meta-analysis. BMJ Open Diabetes Res Care (2021) 9(1). doi: 10.1136/bmjdrc-2020-001776
6. Mendonça L, Bigotte Vieira M, Neves JS. Association of combined fractional excretion of phosphate and FGF23 with heart failure and cardiovascular events in moderate and advanced renal disease. J Nephrol. (2023) 36(1):55–67. doi: 10.1007/s40620-022-01358-1
7. Sanz M, Ceriello A, Buysschaert M, Chapple I, Demmer RT, Graziani F, et al. Scientific evidence on the links between periodontal diseases and diabetes: consensus report and guidelines of the joint workshop on periodontal diseases and diabetes by the international diabetes federation and the European federation of periodontology. J Clin Periodontol (2018) 45(2):138–49. doi: 10.1111/jcpe.12808
8. Nazarzadeh M, Bidel Z, Canoy D, Copland E, Wamil M, Majert J, et al. Blood pressure lowering and risk of new-onset type 2 diabetes: an individual participant data meta-analysis. Lancet (London England). (2021) 398(10313):1803–10. doi: 10.1016/s0140-6736(21)01920-6
9. Esser N, Zraika S. Neprilysin inhibition: a new therapeutic option for type 2 diabetes? Diabetologia (2019) 62(7):1113–22. doi: 10.1007/s00125-019-4889-y
10. Golovaty I, Ritchie ND, Tuomilehto J, Mohan V, Ali MK, Gregg EW, et al. Two decades of diabetes prevention efforts: a call to innovate and revitalize our approach to lifestyle change. Diabetes Res Clin Pract (2023) 198:110195. doi: 10.1016/j.diabres.2022.110195
Keywords: prediabetes, impaired glucose tolerance, impaired fasting glucose, cardiovascular disease, microvascular complications
Citation: Neves JS, Buysschaert M and Bergman M (2023) Editorial: Prediabetes: new insights on the diagnosis, risk stratification, comorbidites, cardiovascular disease, microvascular complications, and treatment. Front. Endocrinol. 14:1214479. doi: 10.3389/fendo.2023.1214479
Received: 29 April 2023; Accepted: 04 May 2023;
Published: 11 May 2023.
Edited and Reviewed by:
Åke Sjöholm, Gävle Hospital, SwedenCopyright © 2023 Neves, Buysschaert and Bergman. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: João Sérgio Neves, anNuZXZlc0BtZWQudXAucHQ=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.