
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Endocrinol. , 12 July 2023
Sec. Cancer Endocrinology
Volume 14 - 2023 | https://doi.org/10.3389/fendo.2023.1187825
This article is part of the Research Topic Predictors for the Aggressiveness of Papillary Thyroid Carcinoma View all 11 articles
Objective: The lymph node posterior to the right recurrent laryngeal nerve (LN-prRLN) is a crucial component of the central lymph nodes (LNs). We aimed to evaluate multimodal predictive factors of LN-prRLN metastasis in patients with papillary thyroid carcinomas (PTCs), including the clinical data, pathologic data, and preoperative sonographic characteristics of PTCs.
Methods: A total of 403 diagnosed PTC patients who underwent unilateral, sub-total, or total thyroidectomy with central neck dissection were enrolled in this retrospective study. The clinical data, pathologic data, conventional ultrasound (US) and contrast-enhanced ultrasound (CEUS) characteristics of PTCs were collected and evaluated for predicting LN-prRLN metastasis.
Results: In this study, 96 PTC patients with LN-prRLN metastasis and 307 PTC patients without LN-prRLN metastasis were included. Univariate analysis demonstrated that PTC patients with LN-prRLN metastasis more often had younger age, larger size, multifocal cancers, A/T < 1, well-margins, microcalcification, petal-like calcification, internal vascularity, centripetal perfusion pattern and surrounding ring enhancement. Multivariate logistic regression analysis revealed that the CEUS centripetal perfusion pattern, central LN detected by ultrasound and LN-arRLN metastasis were independent characteristics for predicting LN-prRLN metastasis in PTC patients.
Conclusion: According to our research, it is essential for clinicians to thoroughly dissect central LNs, particularly LN-prRLNs.
PTCs are one of the most prevalent thyroid cancer histological subtypes, with rising incidence and substantial lymph node metastatic rates (1, 2). According to studies, PTC lymph node metastasis cases range from 20% to 90% of total PTC cases, with central lymph node (level VI) metastasis constituting the majority of cases (3). Thyroidectomy and lymph node dissection are the two basic treatments for PTCs (4). Prelaryngeal LNs, pretracheal LNs, left paratracheal LNs, and right paratracheal LNs are the four groups that typically make up cervical central LNs. Due to the anatomical variations of the recurrent laryngeal nerves on both sides, the right paratracheal LNs are divided into those that are anterior to the right recurrent laryngeal nerve (LN-arRLN) and those that are posterior to the right recurrent laryngeal nerve (LN-prRLN) (5, 6).
Due to the difficult surgical technique and the high rate of complications as a result of the deep position with confined exposure, some researchers contend that routine LN-prRLN removal is not necessary. Furthermore, it can be difficult to assess metastases before surgery, and even experienced surgeons are likely to ignore this location. However, the LN-prRLN metastasis rate in PTC patients has been reported to be as high as 2.7–30.4% (3, 5, 7). The first surgical treatment strategy for LN-prRLN is crucial for the patient’s prognosis. Inadequate cervical LN dissection may increase the risk of recurrence and complications due to repeated operations, so some researchers have suggested routine removal of LN-prRLNs to maximize treatment success (8). These disagreements demonstrate that LN-prRLN merits consideration and additional study. Hence, it is critical to appropriately estimate the probability of LN-prRLN metastasis, which could aid in determining the scope of surgery and lowering the recurrence rates.
Some studies have reported the clinicopathologic risk factors for LN-prRLN metastasis for PTCs. Zhang et al. reported that tumor size larger than 1 cm, multifocality, and extrathyroidal extension were independent predictors of LN-prRLN metastasis in right-sided PTC (3). Zhou et al. proved that tumor size larger than 1. 5cm, extrathyroidal extension, and LN-arRLN metastasis were independent predictors of LN-prRLN metastasis in cN0 PTC (5). However, the research solely included clinicopathologic features, limiting their clinical application; thus, the preoperative sonographic features of primary tumors are essential for evaluating the risk factors for LN-prRLN metastasis in PTCs. US is an incredibly sensitive tool for evaluating initial PTC lesions, providing ultrasonographic signs of PTCs that can be utilized to predict cervical LN metastases in PTC patients and offer a basis for the selection of surgical techniques (9, 10). Unfortunately, few similar studies have been conducted in LN-prRLN metastasis (11).
CEUS, which provides more information about vascularity than conventional US, could reveal the thyroid nodule’s microvasculature and increase the diagnostic accuracy of thyroid nodules (12, 13). Our previous studies found that preoperative CEUS characteristics could offer help in predicting central lymph node metastasis in PTCs with coexistent Hashimoto’s thyroiditis and identifying malignant cervical LNs from benign cervical LNs (14–16).
By analyzing the preoperative US characteristics of PTCs and the postoperative pathological data in 403 PTC patients, this study seeks to identify potential predictors for the preoperative clinical evaluation of LN-prRLN metastases.
The study was approved by the Ethical Committee of the Second Xiangya Hospital of Central South University in China and performed in accordance with the Declaration of Helsinki for human study. The requirement of informed consent from human subjects was waived by IRBs due to the retrospective nature of the review of images acquired for clinical diagnostic purposes. From May 2021 to August 2022, 1253 consecutive patients with thyroid nodules who received conventional US and CEUS examinations were prospectively enrolled in this single-center study. The inclusion criteria were as follows: (i) patients with thyroid nodules who underwent conventional US and CEUS examinations and (ii) pathological examination confirming PTCs after surgery. Patients with the following criteria were excluded: (i) a history of neck surgery or neck radiotherapy; (ii) central cervical lymph node dissection not performed; and (iii) LN-prRLN without clear pathological diagnosis. The final diagnosis of malignant thyroid nodules and metastatic lymph nodes was confirmed by histopathology after surgery. For patients with multifocal PTCs, the largest one was selected for CEUS examination. Finally, 403 PTC patients (96 patients with LN-prRLN metastasis and 307 patients without LN-prRLN metastasis proven by pathological examination) were included in this study. In addition, TSH, thyroid peroxidase antibody (A-TPO), and thyroglobulin antibody (A-TG) levels were evaluated in all patients within one week before surgery.
A GE E11 US scanner with a 3-12L (3-12 MHz) linear array transducer or Siemens Acuson S3000 US scanner with a 9L4 (4–9 MHz) linear array transducer was used for conventional US and CEUS examination. All examinations were performed by operators with more than ten years of experience in thyroid ultrasound diagnosis and five years of experience in performing CEUS examinations. Two other investigators with 5 years of experience in thyroid ultrasound diagnosis analyzed the US images independently. Disagreements were solved by consensus. Two-milliliters of SonoVue (Bracco, Italy) or 0.4 mL of Sonozoid (GE, USA) was injected intravenously, followed by a saline flush of 5 mL. Thyroid nodule imaging lasted at least 30 seconds.
Conventional US features of the thyroid nodules were classified as follows (13): shape (taller than wide, A/T >1; or wider than tall, A/T< 1); margins (well-defined or ill-defined); echogenicity (marked hypo-, hypo-, iso- or hyper-echoic); calcification (no calcification, microcalcification<1 mm in diameter, macrocalcification >1 mm in diameter); petal-like calcification (defined as microcalcification displayed around the thyroid nodule like a petal) (17) and internal vascularity (present or absent).
The following categories describe the thyroid nodules’ CEUS characteristics (14): enhancement type (hyper-, iso- or hypo-enhancement); enhancement uniformity (heterogeneous or homogeneous enhancement); perfusion pattern (centripetal perfusion, the perfusion of microbubbles from the periphery to the center; centrifugal perfusion, the perfusion of microbubbles from the center to the periphery); and surrounding ring enhancement (presence or absence).
Three surgical options (unilateral, sub-total, or total thyroidectomy with central neck dissection) are available, according to the Chinese Thyroid Association’s guidelines. The procedure was chosen based on the surgeon’s desire and a comprehensive analysis of the patient’s condition. Prelaryngeal LN, pretracheal LN, left paratracheal LN, LN-arRLN, and LN-prRLN were the five subgroups of the central LNs and sent for individual pathological evaluation. If the lateral cervical LNs were diagnosed as metastatic LNs from PTCs, lateral cervical lymph node dissection was performed.
The histopathological results after surgery were used as the only reference standard for the final diagnosis of malignant thyroid nodules and metastatic lymph nodes.
The statistical analysis was carried out using SPSS version 21.0. (SPSS, Chicago, IL, USA). The mean and standard deviation (SD) of continuous data were displayed, and they were compared using an independent t test. Categorical data were evaluated using the chi-square test and are shown as percentages. To evaluate multimodal factors and their independent associations with LN-prRLN metastasis, binary logistic regression was performed. P < 0.05 was used to evaluate whether differences were statistically significant.
This study comprised a total of 403 PTC patients, including 307 individuals without LN-prRLN metastasis and 96 patients with LN-prRLN metastasis. Table 1 displays the clinical and pathologic characteristics of the patients. Among the 403 patients with PTCs, the mean age was 41.69 ± 12.01 years (range 18-73 years), 57.8% (233/403) were younger than 45 years, and 75.4% (304/403) were female patients. The mean tumor size was 12.56 ± 8.65 mm (range 2–51 mm). In total, 32.3% (130/403) of patients had Hashimoto’s thyroiditis, 46.2% (186/403) had multifocal PTCs, 51.9% (209/403) had lesions in the right lobe, 9.9% (40/403) had lesions in the left lobe, 2.5% (10/403) had lesions in the isthmus, and 35.7% (144/403) had lesions in the bilateral lobe. Level VI lymph nodes were detected in 176 (43.7%) patients on preoperative conventional US examination. Sub-total and total thyroidectomy with central neck dissection were performed in 367 (91.1%) patients, and unilateral thyroidectomy with central neck dissection was performed in 36 (8.9%). Histopathological examination showed that the rates of left paratracheal LN, prelaryngeal LN, pretracheal LN, LN-arRLN, LN-prRLN and lateral LN metastasis were 28.5% (115/403), 13.2% (53/403), 30.0% (121/403), 36.0% (145/403), 23.8% (96/403) and 24.6% (99/403), respectively. In addition, among patients without any other cervical lymph node metastasis, the rate of LN-prRLN metastasis was 8.2% (8/96). Transient and permanent hypoparathyroidism were noted in 55 (13.6%) and 2 (0.5%) patients, respectively. Voice change developed in 10 (2.5%) patients, but all patients recovered during follow-up, and no patient had consistent dysfunction with vocal cord paralysis.
The univariate analysis of predictors for LN-prRLN is reported in Table 2. The average age of PTC patients with or without LN-prRLN metastasis was 36.65 ± 12.19 years (range: 18-71 years) or 43.27 ± 11.52 years (range: 18-73 years), respectively. Seventy-two (75.0%) patients with LN-prRLN metastasis were younger than 45 years, and 161 (52.4%) patients without LN-prRLN metastasis were younger than 45 years (p = 0.000), showing that the patients with LN-prRLN metastasis were more inclined to be younger. The mean diameters of PTCs with or without LN-prRLN metastasis were 18.23 ± 10.94 mm (range: 3-51 mm) and 10.79 ± 6.93 mm (range: 2-42 mm), respectively, showing that the former had considerably higher mean diameters than the latter (p = 0.000). A size > 10 mm was present in 68 (70.8%) of the patients with LN-prRLN metastasis and 110 (35.8%) of the patients without LN-prRLN metastasis (p = 0.000). Multifocal malignancies were present in 53 (55.2%) individuals with LN-prRLN metastases and in 133 (43.3%) patients without this occurrence (p = 0.041). Only the largest PTC was selected in patients with multifocal PTCs. LN-prRLN metastasis did not appear to be correlated with any other variables (all p>0.05).
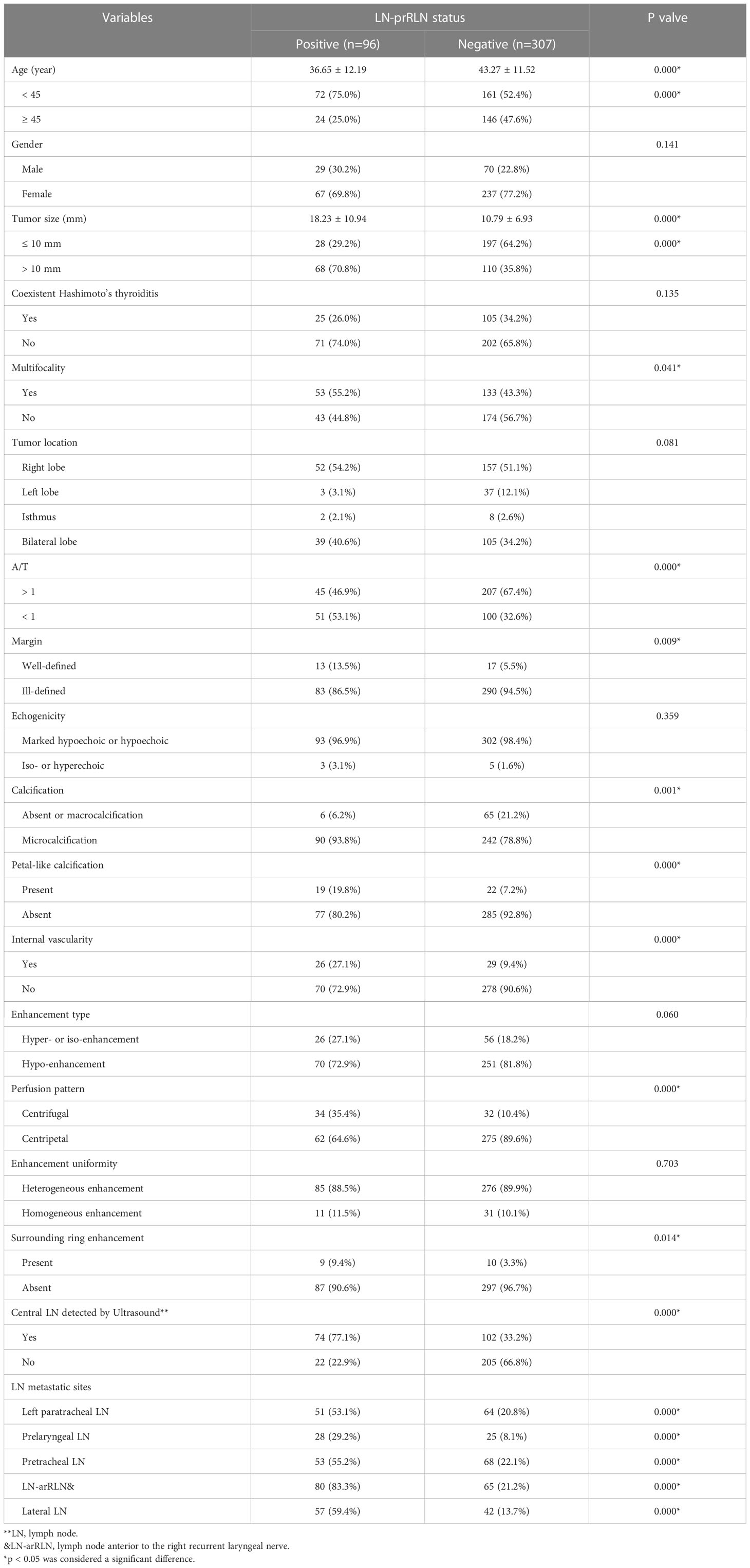
Table 2 Univariate analysis of predictor for lymph node posterior to the right recurrent nerve metastasis (LN-prRLN).
Compared with PTCs without LN-prRLN metastasis, PTCs with LN-prRLN metastasis had more A/T < 1 and well-defined margins, microcalcification, petal-like calcification and internal vascularity on conventional US images. For CEUS images, the PTCs with LN-prRLN metastasis showed a more centrifugal perfusion pattern and the presence of surrounding ring enhancement than the PTCs without LN-prRLN metastasis (Figures 1, 2).
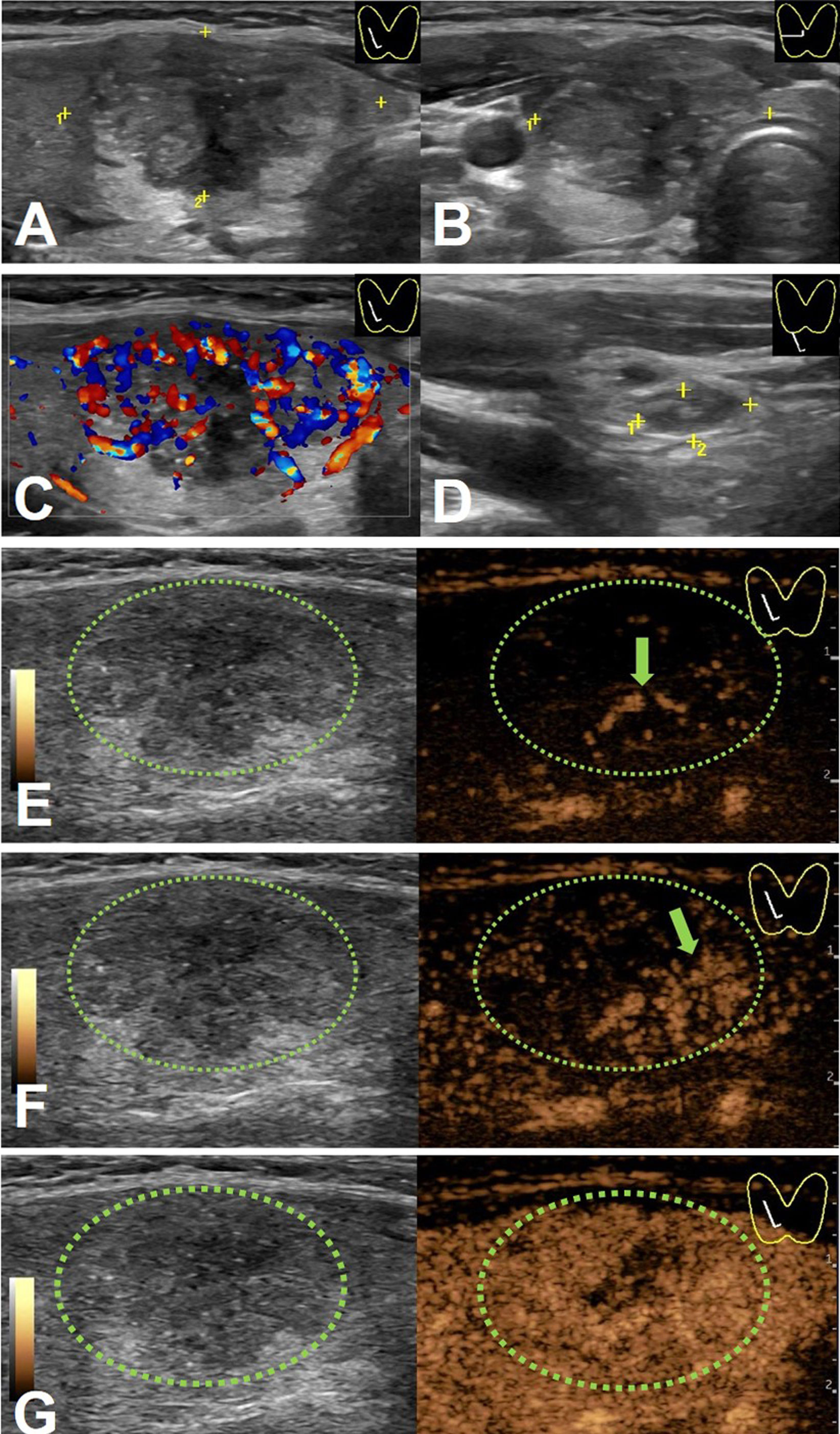
Figure 1 An 18-y-old female PTC patient with LN-prRLN metastasis. Initial longitudinal scan (A) and transverse scan (B) showing a 30-mm thyroid nodule with hypo-echogenicity, ill-defined margins, and petal calcification. (C) Doppler image revealing abundant signals in the nodule. (D) A level VI lymph node (yellow cross) identified on conventional US. (E) CEUS image 6 s after injection of contrast-enhanced agent, the thyroid nodule enhanced from the center to the periphery (green arrow). (F) CEUS image 7 s after injection of contrast-enhanced agent, the thyroid nodule showed heterogeneous enhancement (green arrow). (G) CEUS image 8 s after injection of contrast-enhanced agent, the thyroid nodule showed heterogeneous iso-enhancement.
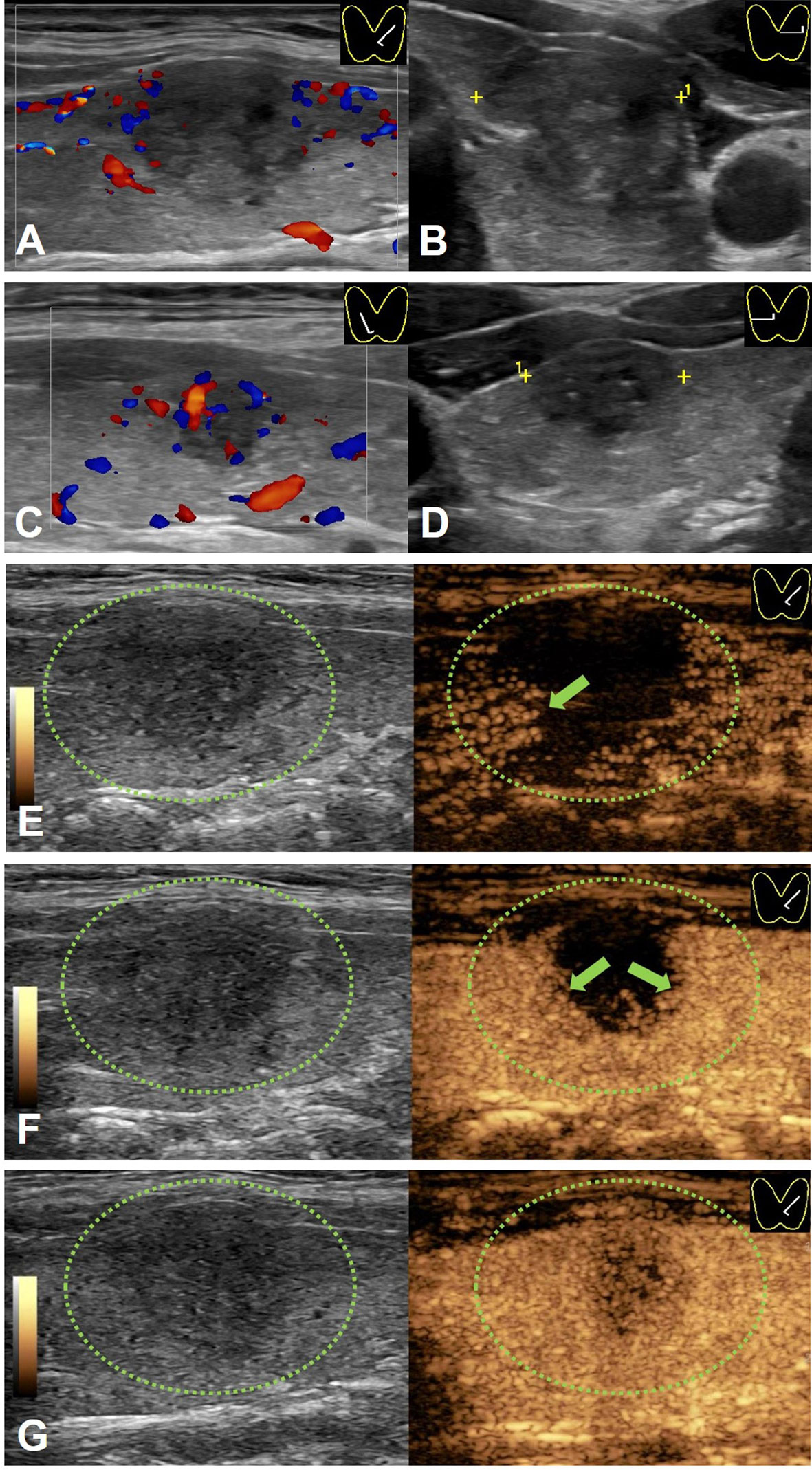
Figure 2 A 41-y-old male PTC patient without LN-prRLN metastasis. (A) Longitudinal Doppler image and (B) transverse scan image showing a 17-mm thyroid nodule with hypo-echogenicity, ill-defined margins, microcalcification and poor signals in the nodule in the left lobe. (C) Longitudinal Doppler image and (D) transverse scan image showing a 11-mm thyroid nodule with hypo-echogenicity, ill-defined margins, microcalcification and few signals in the nodule in the right lobe. (E) CEUS image 10 s after injection of contrast-enhanced agent, the thyroid nodule enhanced from the periphery to the center (green arrow). (F) CEUS image 12 s after injection of contrast-enhanced agent, the thyroid nodule showed heterogeneous enhancement (green arrow). (G) CEUS image 14 s after injection of contrast-enhanced agent, the thyroid nodule showed heterogeneous hypo-enhancement.
Level VI lymph nodes were detected in 74 (77.1%) patients in the PTC with LN-prRLN metastasis group compared with 102 (33.2%) patients in the PTC without LN-prRLN metastasis group on preoperative conventional US examination. In addition, all metastatic rates of left paratracheal LNs, prelaryngeal LNs, pretracheal LNs, LN-arRLNs, LN-prRLNs and lateral LNs were higher than those of the PTCs without LN-prRLN metastasis group on histopathological examination.
All of the statistically significant factors (p < 0.05) underwent multivariate logistic regression analysis. The outcomes showed that the CEUS centrifugal perfusion pattern (B= 1.314, OR = 3.720, 95% CI = 1.808-7.654, p=0.000), central LN detected by ultrasound (B= 1.027, OR = 2.792, 95% CI = 1.440-5.415, p=0.002), and LN-arRLN metastasis (B =0.753, OR =2.123, 95% CI = 1.083-4.163, p=0.028) were independent characteristics for predicting LN-prRLN metastasis (Table 3).
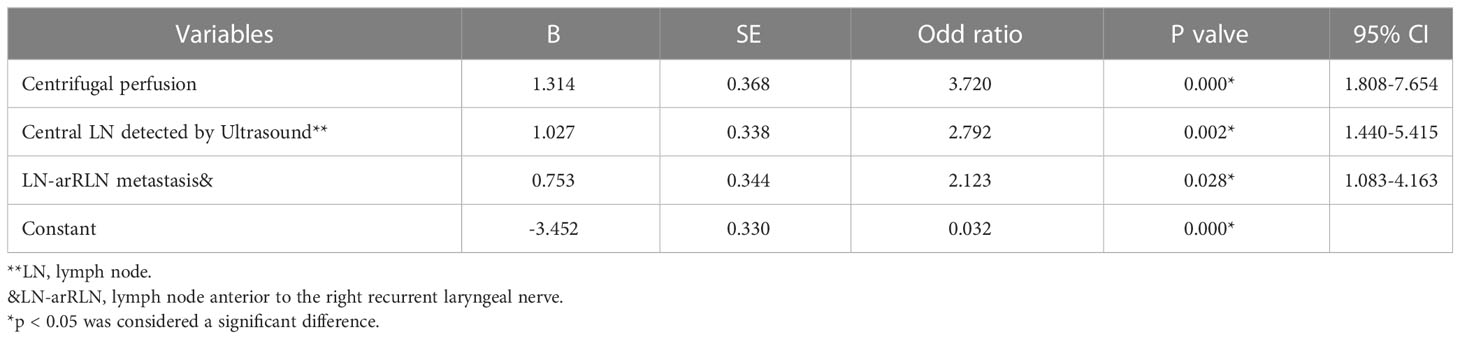
Table 3 Multivariate analysis of the predictors of lymph node posterior to the right recurrent laryngeal nerve metastasis (LN-prRLN).
Currently, there is still controversy about whether to dissect the LN-prRLN in the absence of certain LNs that are positive. Dissection of the LN-prRLN requires patience and experience and could lead to nerve damage and parathyroid injury, affecting the patient’s quality of life (18). According to some researchers, PTCs are a kind of tumor; hence, LN-prRLN dissection is not needed, thus reducing surgical risks to patients after surgery. Hypoparathyroidism and vocal cord paralysis were the two serious complications after thyroid surgery. Transient and permanent hypoparathyroidism occurred in 4.1-51.9% and 0-1.1% of patients, respectively (6, 18–20). Postoperative voice change was found in 4.9-7.4% of patients, while consistent voice change with vocal cord immobility was found in 0-4.0% of patients (6, 18–20).
Although PTCs have a favorable prognosis, other scholars contend that the central LNs are the most frequent sites for lymph node metastasis with a high incidence of 13.7%-72.2% (14, 16, 21). Thorough initial dissection with simultaneous dissection of the LN-prRLN is essential to reduce local recurrence and metastasis and avoid significant complication rates by secondary surgery. Secondary thyroid surgery is difficult for young and inexperienced surgeons, but even skilled and experienced surgeons can have difficulty in mapping the recurrent laryngeal nerve and preventing inadvertent recurrent laryngeal nerve injury, particularly in nonanatomical fields with many scars from the first operations (22, 23). In accordance with the recommendations of the American Thyroid Association (ATA), cervical LNs should be evaluated using preoperative neck US to determine the surgical approach, particularly for lymph node dissection (4). However, conventional US only has a sensitivity of less than 30% for central LNs (24, 25). The risk factors for LN-prRLN metastases in PTCs must be identified for surgeons to choose the best surgical procedures. The variables that predict LN-prRLN metastases in PTC patients, however, are not well known.
Univariate analysis in this study demonstrated that age < 45 years was a clinical risk factor related to LN-prRLN metastasis in PTC patients, demonstrating that patients with LN-prRLN metastasis were more likely to be young people, which was consistent with other previous studies (11, 26). In addition, tumor size > 10 mm was also a clinical risk factor associated with LN-prRLN metastasis, indicating that tumor size was closely linked to an elevated risk of LN-prRLN metastasis, which was also consistent with other previous reports (11, 19).
Recent studies have shown that US characteristics could help predict cervical central LN metastasis in PTC patients (9, 10, 27). Xu et al. reported that a virtual touch tissue imaging area ratio >1, abnormal cervical LNs, microcalcification and multiple nodules were risk factors for the prediction of cervical central LN metastasis in PTC patients (10). Liu et al. found that microcalcification, resistance index >0.7 and multiple nodules have predictive value in central LN metastasis of PTCs (27). However, few studies have been reported for LN-prRLN metastasis prediction by ultrasonographic features. In this study, we found that multiple nodules, calcification, petal-like calcification and internal vascularity were significantly associated with LN-prRLN metastasis in PTC patients. However, the suspicious ultrasonographic features for malignant thyroid nodules, including a taller-than-wider shape (A/T <1) and an ill-defined margin were protective factors for LN-prRLN metastasis in PTC patients, which may contribute to the tumor size of thyroid nodules. The smaller thyroid nodules in PTC patients without LN-prRLN metastasis were more likely to have an ill-defined margin and a taller-than-wider shape of PTCs, which was also reported in our previous study on PTCs with HT patients with coexisting central LN metastasis (14).
Compared to color Doppler technology, the accuracy of thyroid nodule diagnosis may improve with the use of CEUS, which can detect more tumor microvessels. However, to the best of our knowledge, these CEUS parameters for predicting LN-prRLN metastasis in PTC patients have not been explored to date. In our study, we found that the centrifugal perfusion pattern and presence of surrounding ring enhancement were significantly associated with LN-prRLN metastasis in PTC patients. Multivariate analysis demonstrated that the centrifugal perfusion pattern was one of the independent characteristics for the presence of LN-prRLN metastasis.
Although central LNs have a low display rate on preoperative conventional US examination, the present study found central LNs in 176 (43.7%) patients. Moreover, the display rate of central LNs in the PTC with LN-prRLN metastasis group was as high as 77.1%, which was significantly higher than that of 33.2% in PTC without LN-prRLN metastasis group. Multivariate analysis demonstrated that central LN detected by US was another independent characteristic for the prediction of LN-prRLN metastasis, indicating that the centrifugal perfusion pattern on CEUS and central LN detected by US could serve as preoperative factors for predicting LN-prRLN metastasis. In addition, all histopathological metastatic rates of left paratracheal LNs, prelaryngeal LNs, pretracheal LNs, LN-arRLNs, LN-prRLNs and lateral LNs were significantly higher than those of PTCs without LN-prRLN metastasis. In this study, individuals who had LN-arRLN metastases had a nearly fourfold increased probability of LN-prRLN metastasis than patients who did not. According to the multivariate analysis, LN-arRLN metastasis in PTC patients was a significant risk factor for LN-prRLN metastasis, suggesting that the LN-arRLN compartment may be used intraoperatively to predict LN-prRLN metastasis.
According to the findings of univariate and multivariate analyses, the centrifugal perfusion pattern on CEUS, central LN detected by US, and LN-arRLN metastasis were independent predictors of LN-prRLN metastasis in these patients. In that case, suggesting that the LN-prRLN should be removed with thorough neck dissection to prevent metastasis.
There are several limitations to our study. First, it was a single institutional retrospective analysis, hence the findings may not have been applicable to other PTC patient populations. Second, selection bias was also present. To further explain these findings, a large-scale prospective multicenter investigation is needed.
In summary, complete central LN dissection should be taken into consideration given the rate of LN-prRLN metastasis and the challenges and complications of reoperation. Centrifugal perfusion patterns on CEUS, central LN detected by US and LN-arRLN metastasis are helpful in predicting metastasis to LN-prRLNs. Thus, preoperative conventional US and CEUS may serve as useful tools in predicting LN-prRLN metastasis in PTC patients.
The original contributions presented in the study are included in the article/supplementary material. Further inquiries can be directed to the corresponding author.
The studies involving human participants were reviewed and approved by the Ethics Committee of Second Xiangya Hospital, Central South University, China. The patients/participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
CN contributed to the conception and design of the work. YG participated to data analysis and manuscript writing. ZZ, KT, YX, RZ and QP participated to data collection and patients’ follow-up. All authors contributed to the article and approved the submitted version.
This project was funded by the National Natural Science Foundation of China (81974267), the Science and Technology Innovation Program of Hunan Province (2021RC3033), the Hunan Provincial Natural Science Foundation of China (2022JJ30827 and 2022JJ30806) and Natural Science Foundation of Hunan Provincial Health Commission (A202309026329).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Lim H, Devesa SS, Sosa JA, Check D, Kitahara CM. Trends in thyroid cancer incidence and mortality in the United States, 1974-2013. JAMA (2017) 317(13):1338–48. doi: 10.1001/jama.2017.2719
2. Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin (2021) 71(3):209–49. doi: 10.3322/caac.21660
3. Eun YG, Lee YC, Kwon KH. Predictive factors of contralateral paratracheal lymph node metastasis in papillary thyroid cancer: prospective multicenter study. Otolaryngol Head Neck Surg (2014) 150(2):210–5. doi: 10.1177/0194599813514726
4. Haugen BR, Alexander EK, Bible KC, Doherty GM, Mandel SJ, Nikiforov YE, et al. 2015 American Thyroid association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: the American thyroid association guidelines task force on thyroid nodules and differentiated thyroid cancer. Thyroid (2016) 26(1):1–133. doi: 10.1089/thy.2015.0020
5. Zhou M, Duan Y, Ye B, Wang Y, Li H, Wu Y, et al. Pattern and predictive factors of metastasis in lymph nodes posterior to the right recurrent laryngeal nerve in papillary thyroid carcinoma. Front Endocrinol (Lausanne) (2022) 13:914946. doi: 10.3389/fendo.2022.914946
6. Zhang S, Zhang R, Wang C, Gong W, Zheng C, Fang Q, et al. Unnecessity of routine dissection of right central lymph nodes in cN0 papillary thyroid carcinoma located at the left thyroid lobe. Front Oncol (2021) 11:685708. doi: 10.3389/fonc.2021.685708
7. Chang H, Yoo RN, Kim SM, Kim BW, Lee YS, Lee SC, et al. The clinical significance of the right para-oesophageal lymph nodes in papillary thyroid cancer. Yonsei Med J (2015) 56(6):1632–7. doi: 10.3349/ymj.2015.56.6.1632
8. Liu C, Xiao C, Chen J, Li X, Feng Z, Gao Q, et al. Risk factor analysis for predicting cervical lymph node metastasis in papillary thyroid carcinoma: a study of 966 patients. BMC Cancer (2019) 19(1):622. doi: 10.1186/s12885-019-5835-6
9. Chen J, Li XL, Zhao CK, Wang D, Wang Q, Li MX, et al. Conventional ultrasound, immunohistochemical factors and BRAF(V600E) mutation in predicting central cervical lymph node metastasis of papillary thyroid carcinoma. Ultrasound Med Biol (2018) 44(11):2296–306. doi: 10.1016/j.ultrasmedbio.2018.06.020
10. Xu JM, Xu XH, Xu HX, Zhang YF, Guo LH, Liu LN, et al. Prediction of cervical lymph node metastasis in patients with papillary thyroid cancer using combined conventional ultrasound, strain elastography, and acoustic radiation force impulse (ARFI) elastography. Eur Radiol (2016) 26(8):2611–22. doi: 10.1007/s00330-015-4088-2
11. Zou M, Wang YH, Dong YF, Lai XJ, Li JC. Clinical and sonographic features for the preoperative prediction of lymph nodes posterior to the right recurrent laryngeal nerve metastasis in patients with papillary thyroid carcinoma. J Endocrinol Invest (2020) 43(10):1511–7. doi: 10.1007/s40618-020-01238-0
12. Gao L, Xi X, Gao Q, Tang J, Yang X, Zhu S, et al. Blood-rich enhancement in ultrasonography predicts worse prognosis in patients with papillary thyroid cancer. Front Oncol (2021) 10:546378. doi: 10.3389/fonc.2020.546378
13. Peng Q, Niu C, Zhang M, Chen S. Sonographic characteristics of papillary thyroid carcinoma with coexistent hashimoto's thyroiditis: conventional ultrasound, acoustic radiation force impulse imaging and contrast-enhanced ultrasound. Ultrasound Med Biol (2019) 45(2):471–80. doi: 10.1016/j.ultrasmedbio.2018.10.020
14. Chen S, Niu C, Peng Q, Tang K. Sonographic characteristics of papillary thyroid carcinoma with coexistent hashimoto's thyroiditis in the preoperative prediction of central lymph node metastasis. Front Endocrinol (Lausanne) (2021) 12:556851. doi: 10.3389/fendo.2021.556851
15. Fang F, Gong Y, Liao L, Ye F, Zuo Z, Li X, et al. Value of contrast-enhanced ultrasound for evaluation of cervical lymph node metastasis in papillary thyroid carcinoma. Front Endocrinol (2022) 13:812475. doi: 10.3389/fendo.2022.812475
16. Ye F, Gong Y, Tang K, Xu Y, Zhang R, Chen S, et al. Contrast-enhanced ultrasound characteristics of preoperative central cervical lymph node metastasis in papillary thyroid carcinoma. Front Endocrinol (2022) 13:941905. doi: 10.3389/fendo.2022.941905
17. Peng Q, Zhang Q, Chen S, Niu C. Petal-like calcifications in thyroid nodules on ultrasonography: a rare morphologic characteristic of calcification associated with aggressive biological behavior. Front Endocrinol (Lausanne) (2020) 11:271. doi: 10.3389/fendo.2020.00271
18. Du W, Fang Q, Zhang X, Dai L. Metastasis of cN0 papillary thyroid carcinoma of the isthmus to the lymph node posterior to the right recurrent laryngeal nerve. Front Endocrinol (Lausanne) (2021) 12:677986. doi: 10.3389/fendo.2021.677986
19. Liu Z, Sun M, Xiao Y, Yang J, Zhang T, Zhao Y. Predictors of metastasis to lymph nodes posterior to the right recurrent laryngeal nerve in differentiated thyroid carcinoma: a prospective study. Asian J Surg (2017) 40(4):270–7. doi: 10.1016/j.asjsur.2015.12.003
20. Yuan J, Li J, Chen X, Zhong Z, Chen Z, Yin Y, et al. Predictors of lymph nodes posterior to the right recurrent laryngeal nerve metastasis in patients with papillary thyroid carcinoma: a retrospective study. Med (Baltimore) (2017) 96(35):e7908. doi: 10.1097/MD.0000000000007908
21. Medas F, Canu GL, Cappellacci F, Boi F, Lai ML, Erdas E, et al. Predictive factors of lymph node metastasis in patients with papillary microcarcinoma of the thyroid: retrospective analysis on 293 cases. Front Endocrinol (Lausanne) (2020) 11:551. doi: 10.3389/fendo.2020.00551
22. Wojtczak B, Sutkowski K, Kaliszewski K, Barczynski M, Bolanowski M. Thyroid reoperation using intraoperative neuromonitoring. Endocrine (2017) 58(3):458–66. doi: 10.1007/s12020-017-1443-x
23. Pai SI, Tufano RP. Reoperation for recurrent/persistent well-differentiated thyroid cancer. Otolaryngol Clin North Am (2010) 43(2):353–63. doi: 10.1016/j.otc.2010.02.004
24. Khokhar MT, Day KM, Sangal RB, Ahmedli NN, Pisharodi LR, Beland MD, et al. Preoperative high-resolution ultrasound for the assessment of malignant central compartment lymph nodes in papillary thyroid cancer. Thyroid (2015) 25(12):1351–4. doi: 10.1089/thy.2015.0176
25. Hwang HS, Orloff LA. Efficacy of preoperative neck ultrasound in the detection of cervical lymph node metastasis from thyroid cancer. Laryngoscope (2011) 121(3):487–91. doi: 10.1002/lary.21227
26. Sun J, Jiang Q, Wang X, Liu W, Wang X. Nomogram for preoperative estimation of cervical lymph node metastasis risk in papillary thyroid microcarcinoma. Front Endocrinol (Lausanne) (2021) 12:613974. doi: 10.3389/fendo.2021.613974
Keywords: contrast-enhanced ultrasound (CEUS), conventional Ultrasound, central cervical lymph node metastasis, papillary thyroid carcinomas (PTCs), lymph nodes posterior to the right recurrent laryngeal nerve metastasis
Citation: Gong Y, Zuo Z, Tang K, Xu Y, Zhang R, Peng Q and Niu C (2023) Multimodal predictive factors of metastasis in lymph nodes posterior to the right recurrent laryngeal nerve in papillary thyroid carcinoma. Front. Endocrinol. 14:1187825. doi: 10.3389/fendo.2023.1187825
Received: 16 March 2023; Accepted: 27 June 2023;
Published: 12 July 2023.
Edited by:
Eleonora Lori, Sapienza University of Rome, ItalyReviewed by:
Giovanni Succo, San Giovanni Bosco Hospital, ItalyCopyright © 2023 Gong, Zuo, Tang, Xu, Zhang, Peng and Niu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Chengcheng Niu, bml1Y2hlbmdjaGVuZ0Bjc3UuZWR1LmNu
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.