
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Endocrinol. , 24 April 2023
Sec. Reproduction
Volume 14 - 2023 | https://doi.org/10.3389/fendo.2023.1153289
This article is part of the Research Topic Advances in Research on Aging in Female Infertility and Pathologic Pregnancy View all 13 articles
 Mohd Zahoor ul haq Shah1*
Mohd Zahoor ul haq Shah1* Vinoy kumar Shrivastva1
Vinoy kumar Shrivastva1 Manzoor Ahmad Mir2
Manzoor Ahmad Mir2 Wajid Mohammad Sheikh3
Wajid Mohammad Sheikh3 Mohd Ashraf Ganie4
Mohd Ashraf Ganie4 Gulzar Ahmed Rather5
Gulzar Ahmed Rather5 Majid Shafi6
Majid Shafi6 Showkeen Muzamil Bashir3*
Showkeen Muzamil Bashir3* Mohammad Azam Ansari7
Mohammad Azam Ansari7 Meneerah A. Al-Jafary8
Meneerah A. Al-Jafary8 Mohammad H. Al-Qahtani9
Mohammad H. Al-Qahtani9 Abdalelgadir Musa Homeida10
Abdalelgadir Musa Homeida10 Ebtesam A. Al-Suhaimi8*
Ebtesam A. Al-Suhaimi8*Introduction: Polycystic Ovary syndrome (PCOS) affects the health of many women around the world. Apart from fundamental metabolic problems connected to PCOS, focus of our study is on the role of quercetin on genes relevant to steroidogenesis and folliculogenesis.
Methods: Eighteen mature parkes strain mice (4-5 weeks old) weighing 18–21 g were randomly divided into three groups of six each as follows: Group I serves as the control and was given water and a regular chow diet ad lib for 66 days; group II was given oral gavage administration of letrozole (LETZ) (6 mg/kg bw) for 21 days to induce PCOS and was left untreated for 45 days; For three weeks, Group III received oral gavage dose of LETZ (6 mg/kg), after which it received Quercetin (QUER) (125 mg/kg bw orally daily) for 45 days.
Results: In our study we observed that mice with PCOS had irregular estrous cycle with increased LH/FSH ratio, decreased estrogen level and decline in expression of Kitl, Bmp1, Cyp11a1, Cyp19a1, Ar, lhr, Fshr and Esr1 in ovary. Moreover, we observed increase in the expression of CYP17a1, as well as increase in cholesterol, triglycerides, testosterone, vascular endothelial growth factor VEGF and insulin levels. All these changes were reversed after the administration of quercetin in PCOS mice.
Discussion: Quercetin treatment reversed the molecular, functional and morphological abnormalities brought on due to letrozole in pathological and physiological setting, particularly the issues of reproduction connected to PCOS. Quercetin doesn’t act locally only but it acts systematically as it works on Pituitary (LH/FSH)- Ovary (gonad hormones) axis. the Side effects of Quercetin have to be targeted in future researches. Quercetin may act as a promising candidate for medical management of human PCOS.
Polycystic Ovary syndrome (PCOS) affects the health of many women around the world. Patients with PCOS are typically females in their reproductive years that have one or more of the following conditions: (A) obesity; (B) an irregular estrus cycle (C) sub/infertility or (D) hirsutism. Ovarian dysfunction, cysts in ovaries, and hyperandrogenism are some of its diagnostic markers. Despite the lack of a clear aetiology, it appears an imbalance of hormones, particularly elevated testosterone level, as well as insulin resistance (IR), can be taken into account (1–3). Patients with PCOS who have infertility are frequently upset about their inability to get pregnant. The hypothalamic-pituitary-ovarian axis is hypothesized to be impacted by the environment and genetics in around three and a half of PCOS patients who have elevated androgen levels (4). One of the intraovarian steroidogenesis abnormalities that are hypothesized to lead to ovarian failure in PCOS is a decrease in activity of aromatase enzyme, causing an imbalance of hormones, hyperandrogenism, and excess androgens within the ovaries leading to polycystic ovaries could be anticipated from decreased activity of the enzyme aromatase, which determines production rate of production of estrogen from androgen (5, 6).
As was already mentioned, a significant factor in PCOS is hyperandrogenism (7). In ovarian follicle granulosa cells, aromatase (Cyp19a1) changes testosterone (Testo) into oestrogen. As a way to create a model of PCOS having similar features of women with PCOS, we administered letrozole (LETZ) to female mice. LETZ is a non-steroidal inhibitor of aromatase which results in accumulation of androgen by decreasing the activity of aromatase, thereby lowers production of estrogen (8, 9).
Today, a variety of techniques are employed to combat PCOS and promote ovulation. However, a number of serious side effects, such as arthritis and joint or muscular pain have been observed (10). Consequently, natural medicines having no or few side effect are becoming more and more popular. A flavonoid molecule called quercetin (QUER) has biological properties that include, controlling blood lipid levels, controlling blood sugar and scavenging oxygen free radicals. Its molecular formula is C15H10O7, and its chemical name is 4h-1-benzopyran-4-one, 2-(3,4-dihydroxy phenyl), 3,5,7-trihydroxy-flavone. According to recent research, quercetin can boost healthy ovarian follicle development, restore healthy anatomy of ovary, as well as enhance histology of uterus. It’s effects are comparable to those of metformin (11). According to reports, QUER lowers level of LH, and testo in PCOS patients (12). According to the most recent studies, quercetin can impact ovarian development and possesses estrogen-like effects (13) Researchers also discovered that quercetin can reduce insulin resistance, treat hyperinsulinemia, lower blood sugar levels, and block the expression of androgens (14). It has been observed that Oral QUER supplementation was effective in improving the adiponectin-mediated insulin resistance and hormonal profile of women with PCOS. It has been noted that taking oral QUER supplements helped women with PCOS with their adiponectin-mediated insulin resistance and hormonal profile (15). It has been demonstrated that quercetin lowers ovarian Bax and raises Bcl-2 protein abundance in PCOS rodents. Our findings suggest that QUER may increase oestrogen concentration, ovarian aromatase protein content, folliculogenesis, and decrease atresia by attenuating hyperandrogenism in PCOS rats. Q is as effective as metformin in reducing hyperandrogenism by lowering free Testosterone level and improving hypothalamic-pituitary-ovarian axis function. (16)
However, despite the fact that some researches have looked at the connection between QUER and PCOS, however they solely looked into impact of QUER on common signs of PCOS. Apart from fundamental metabolic problems connected to PCOS, focus of our study is on the role of quercetin on genes relevant to steroidogenesis and folliculogenesis.
Sun Pharma Company and Sigma Aldrich were used to obtain the drugs letrozole and quercetin, respectively. The ELISA kits (ELK Biotechnology Wuhan, China) were bought from Clementia Biotech, New Delhi, India for the hormonal analysis. Analytical-grade chemicals were used in addition during the investigation.
Eighteen mature parkes strain mice (Age: 4-5 weeks) weighing 18-21 g were procured from Jeeva life sciences Hyderabad, mice having unrestricted access to water as well as food, and we gave them two weeks to acclimatize the environment. Following the acclimation period of two weeks, the animals were randomly into three groups of six each as follows: Group I serves as the control and was given water and a regular chow diet ad lib for 66 days; group II was given oral gavage administration of letrozole (LETZ) (6 mg/kg bw) (3) for 21 days to induce PCOS and was left untreated for 45 days; For three weeks, Group III received oral gavage dose of LETZ (6 mg/kg), after which it received Quercetin (QUER) (125 mg/kg bw orally daily) for 45 days. We kept mice under normal ambient temperature (22-25˚C), relative humidity of (55-60) and twelve hours of dark and light cycles respectively. A 50 mg/kg intraperitoneal dose of sodium pentobarbital was used to anaesthetize the mice and by puncturing the retro-orbital venous sinus, blood samples from all the mice were obtained at 66th day of the experiment, and serum was obtained which was then used to analyse hormones and biochemistry. A cervical dislocation was then used to kill the mice. The body had its ovaries removed and adipose tissues were cleansed for further biochemical and gene expression studies. The ethical committee of institution (Barkatullah University Bhopal) gave their consent under 1885/GO/Re/S/CPCSEA/IAEC/BU/21 to all experimental protocols.
Using easily accessible kits, triglycerides (TG) and total cholesterol (TC) were colorimetrically measured (Meril Diagnostics, Gujrat, India). Indirect measurements of low-density lipoprotein and very low-density lipoprotein were made while using Friedewald’s equation.
Friedwald Equation: LDL = TC – HDL − (TG/5). VLDL= VLDL = TG/5 (17).
The 67th day of the trial saw the collection of blood via retro-orbital venous sinus puncture. A centrifugation process was used to separate the serum, which was then put in storage until it was needed. The Enzyme-linked- Immunosorbent Assay ELISA kits that were used were obtained from ELK biotechnology, Wuhan, China, (CAT. numbers: ELK 368, ELK4808, ELK8407) and were built on the competitive inhibition enzyme immunoassay methodology. The kits’ microtiter plate already has a specific protein pre-coated on it. An anti-testosterone, anti-LH, anti-FSH, and anti-oestrogen antibody biotin-conjugated was added to the appropriate microplate wells once the addition was made of standards or samples. The TMB substrate solution was then added to each microplate well, followed by the addition of an avidin-horseradish peroxidase (HRP) conjugate, which was then incubated for 45 minutes. The enzyme substrate reaction was stopped using the kits’ stop solution, and the colour shift was detected using an ELISA reader that operates at a wavelength of 450 ± 10 nm.
The sandwich-ELISA method was used in the ELISA kit purchased from Elabscience Biotechnology Inc., (Wuhan, Hubei, P.R.C., China; CAT. No: E-EL-H0111; intra and inter –CV are <10%) This kit came with a micro ELISA plate (MEP) that was already coated with a vascular endothelial growth factor-specific antibody (VEGF). The wells of MEP comprised the particular antibody additionally to norms or examples. Then serial injections of an Avidin-Horseradish Peroxidase (HRP) solution and biotin - conjugated antibodies unique to VEGF were produced into each microplate well. The free bits were removed during washing. Each well received a dose of the substrate solution. Colour blue was only visible in the wells containing VEGF, biotinylated detecting antibody, and Avidin-HRP conjugate. Stop solution is added to stop the enzyme-substrate reaction was halted and the colour changed to yellow. At 450 nm, the optical density (OD) was measured using an ELISA reader. The OD value and VEGF levels are linearly correlated. Based on the OD of the data in respect to the conventional curves, the amount of VEGF present for each sample may be determined.
Total RNA was extracted using Invitrogen’s TRI Reagent, and 1µg of total RNA was used to create cDNA, both in accordance with the manufacturer’s instructions (Invitrogen). The RT-PCR was performed using SYBR green and real-time PCR. To calculate the mRNA values, a standard curve for every gene’s related expression level was developed. The SDS software was used to determine the threshold cycle (CT) of each sample and average CT was calculated for triplicate. Moreover Δ CT for each target gene was calculated by subtracting Δ CT for β-actin from average CT of the target gene of the sample. Table 1 lists the primers and internal controls that were employed, with additional data.
Ovarian tissue was fixated in 10% formol-saline for 24 hrs, dried, covered with paraffin, and sections were cut at a thickness of 5 microns for hematoxylin and eosin (H & E) stains. Motic microscope was used to examine and evaluate the sections (18).
A one-way analysis of variance as well as a post hoc evaluation utilizing Tukey’s multiple comparison tests was utilized to decide the parameters’ importance by using Graph Pad Prism version 9.3. Significance levels of 0.05, 0.01 and 0.001 accordingly have been used to indicate the statistically important, highly remarkable, and extremely significant level.
Letrozole (LTZ) delivery in this trial caused a substantial rise in blood insulin levels (p 0.001) against healthy controls, and we also discovered a significant fall in insulin in the PCOS group receiving QUER in comparison to the PCOS group not receiving treatment (Figure 1).
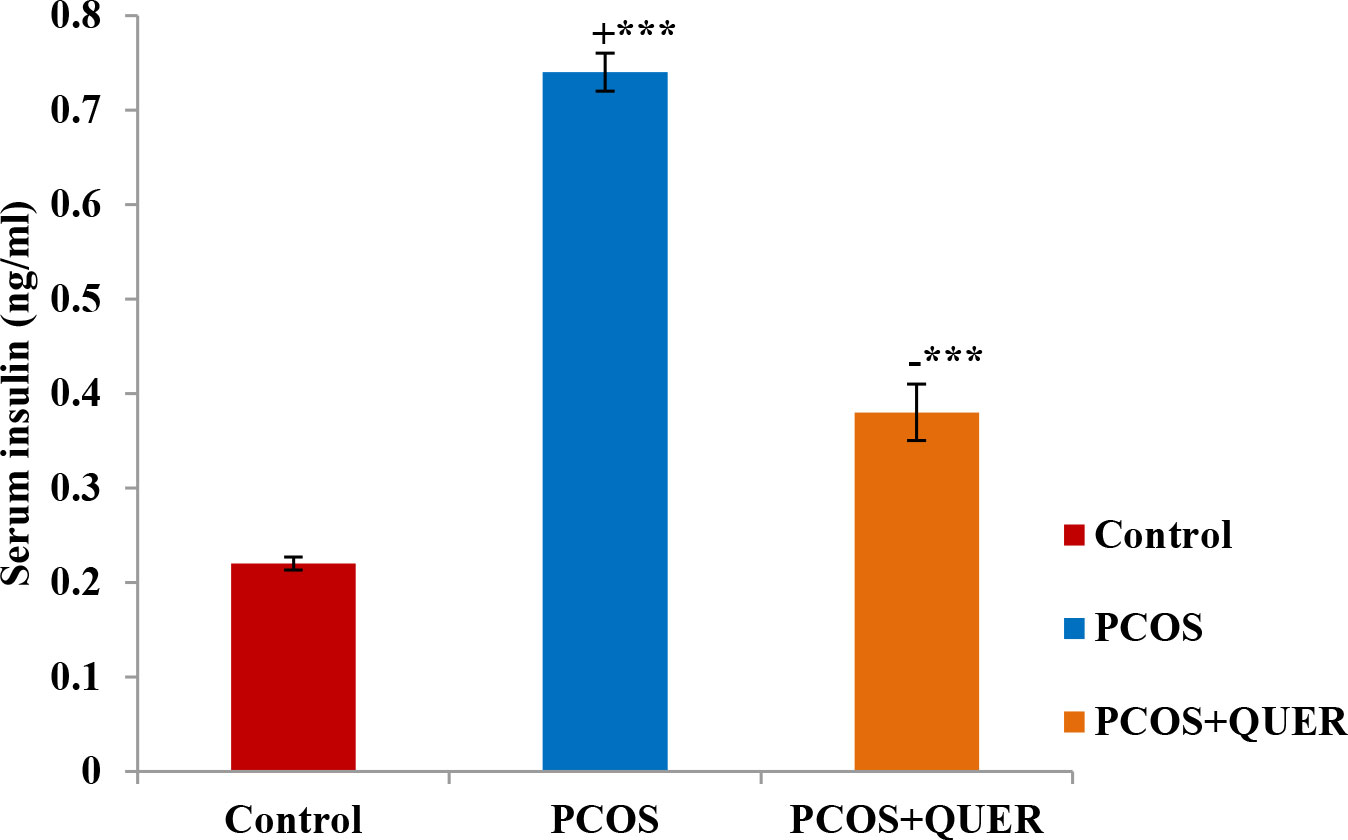
Figure 1 Effect of QUER on Serum insulin in mice with PCOS: With n=6 per group, all values are expressed as means with standard errors: Control: saline solution at 0.9%: PCOS (6 mg/kg of LETZ); PCOS+ QUER (6 mg/kg of LETZ and 125 mg/kg of QUER); += Control versus PCOS; -= PCOS versus PCOS+QUER; ***p 0.001.
The estrouscyclicity of the LETZ-induced PCOS mice was abnormal, and we saw a persistent diestrus condition that led to longer diestrous cycles than in the normal control mice. However, the estrous cycle was regularized after taking QUER, which returned the cycle duration to normal (Table 2).
When compared to the normal control mice, we saw that LETZ-induced PCOS mice had significantly higher levels of TG and cholesterol (P<0.001). In contrast, we saw that the PCOS group that received QUER had significantly lower levels of TG and cholesterol (P<0.001).
We found that, in contrast normal control group, LETZ induced PCOS mice had significantly elevated levels of blood testosterone and LH : FSH ratio and significantly lower serum estrogen and FSH levels. However, QUER treatment significantly reduced (p<0.001) the testosterone as well as LH : FSH levels in PCOS mice, while increasing (p<0.01) the levels of estrogen and FSH compared with the PCOS group that isn’t receiving treatment (Figure 2).
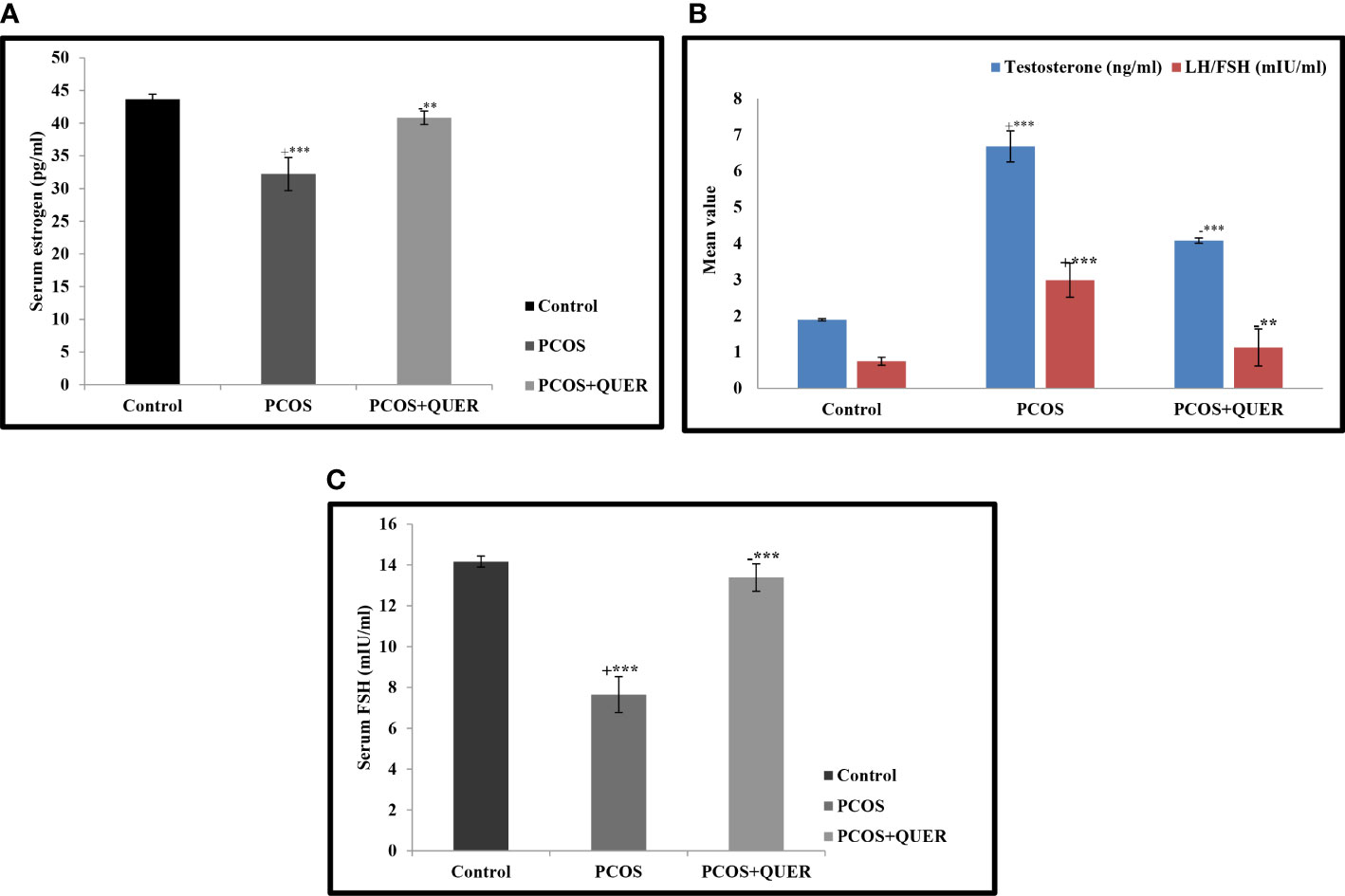
Figure 2 (A) Effect of QUER on Serum estrogen in mice with PCOS With n=6 per group, all values are expressed as means with standard errors: Control: saline solution at 0.9%: PCOS (6 mg/kg of LETZ); PCOS+ QUER (6 mg/kg of LETZ and 125 mg/kg of QUER); += Control versus PCOS; -= PCOS versus PCOS+QUER; ***p 0.001, **p 0.01 (B) Effect of QUER on LH/FSH and testosterone in PCOS mice. With n=6 per group, all values are expressed as means with standard errors: Control: saline solution at 0.9%: PCOS (6 mg/kg of LETZ); PCOS+ QUER (6 mg/kg of LETZ and 125 mg/kg of QUER); += Control versus PCOS; -= PCOS versus PCOS+QUER; ***p 0.001, **p 0.01. (C) Effect of QUER on serum FSH in PCOS mice. With n=6 per group, all values are expressed as means with standard errors: Control: saline solution at 0.9%: PCOS (6 mg/kg of LETZ); PCOS+ QUER (6 mg/kg of LETZ and 125 mg/kg of QUER); += Control versus PCOS; -= PCOS versus PCOS+QUER; ***p 0.001.
This study’s findings demonstrated that when letrozole was administered, VEGF levels significantly increased (p<0.001) when compared to the normal mice. However, in contrast to the LETZ-induced PCOS group, we noticed a significant (P<0.001) drop in VEGF levels in the group that received LETZ + QUER (Figure 3).
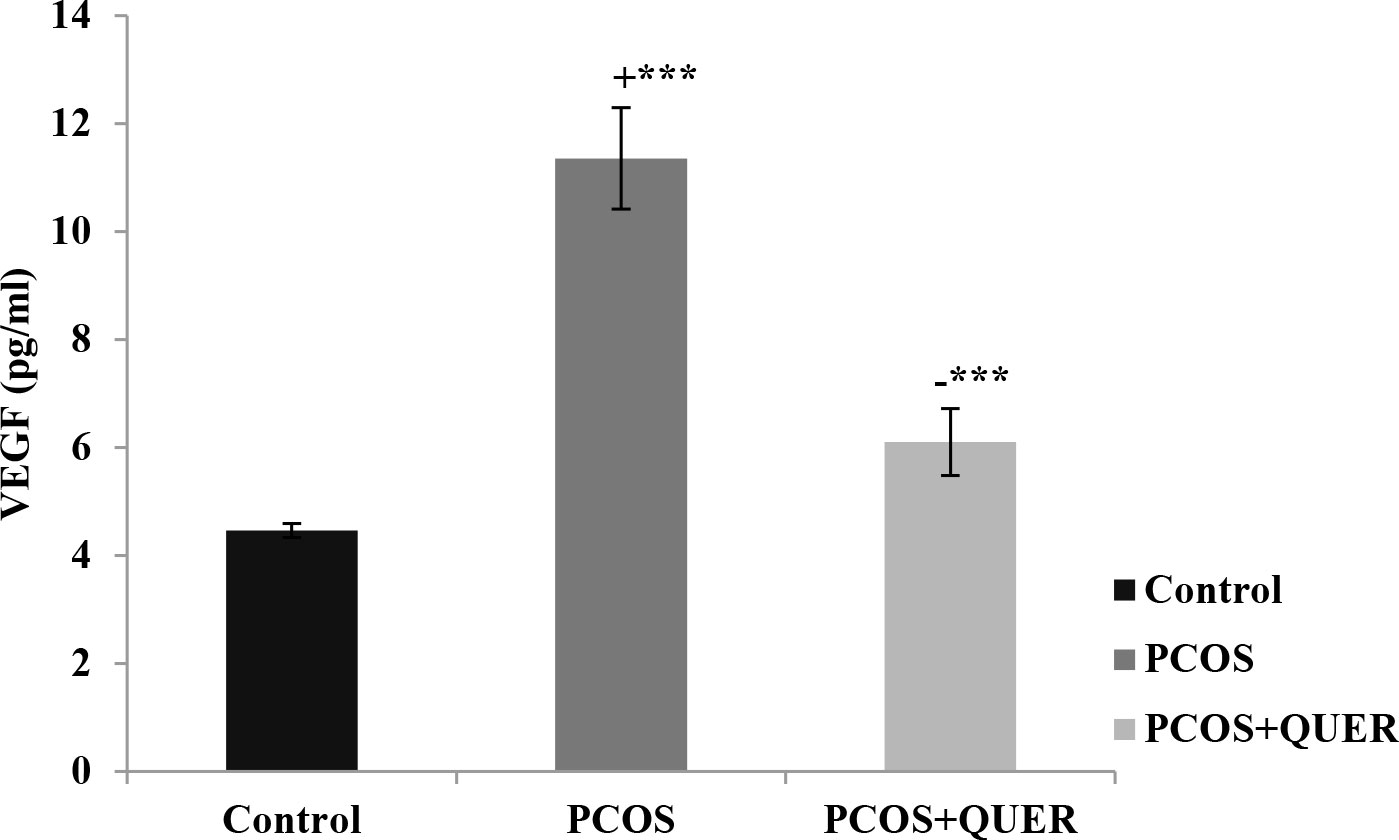
Figure 3 Effect of QUER on plasma VEGF in PCOS mice. With n=6 per group, all values are expressed as means with standard errors: Control: saline solution at 0.9%: PCOS (6 mg/kg of LETZ); PCOS+ QUER (6 mg/kg of LETZ and 125 mg/kg of QUER); += Control versus PCOS; -= PCOS versus PCOS+QUER; ***p 0.001.
Our findings demonstrated that, in comparison to the usual control, the expressions of KITL and Bmp1 significantly decreased after LETZ treatment (p<0.001). The group that received LETZ + QUER, however, had levels that were importantly higher (p<0.05) in contrast to the mice with PCOS induced by letrozole (Figure 4).
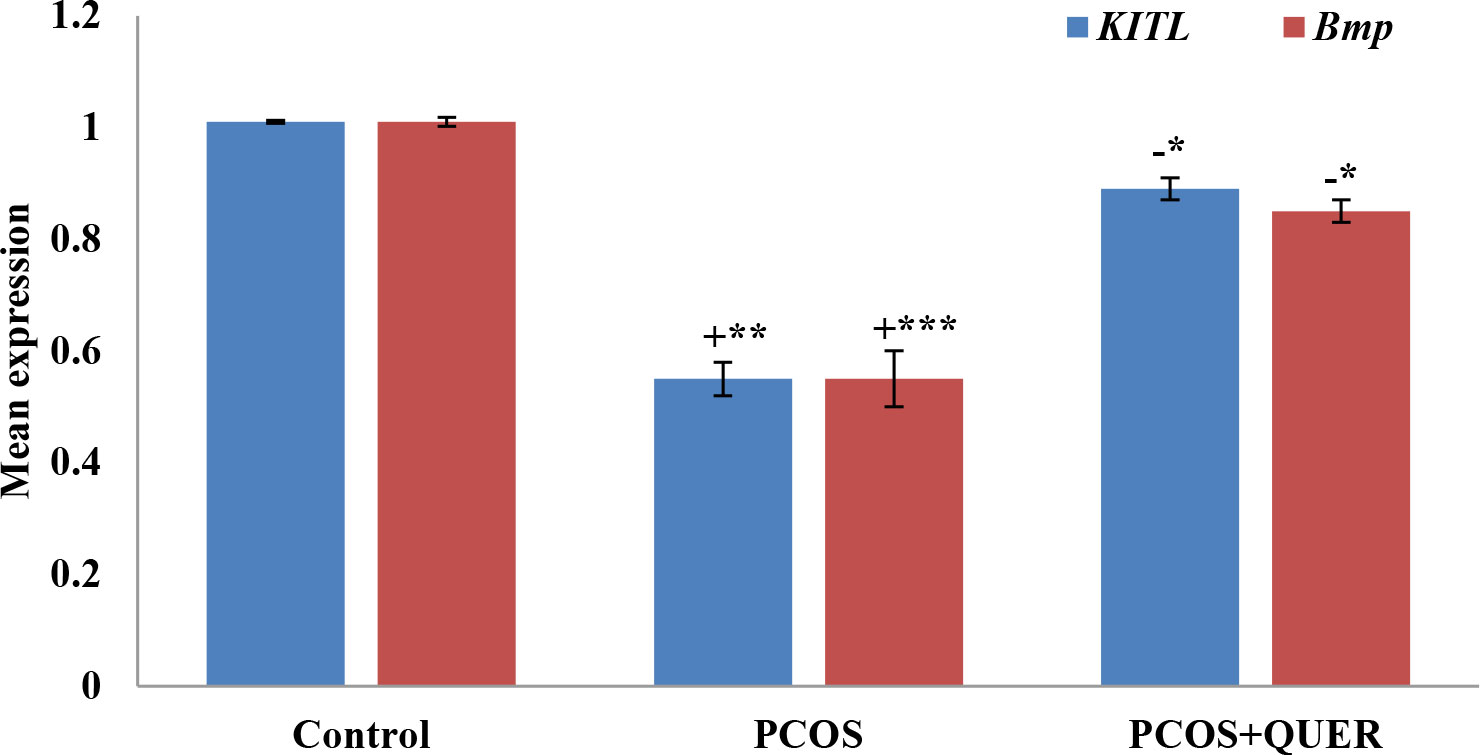
Figure 4 Effect of QUER on KITL and Bmp1 in mice with polycystic ovary syndrome: With n=6 per group, all values are expressed as means with standard errors: Control: saline solution at 0.9%: PCOS (6 mg/kg of LETZ); PCOS+ QUER (6 mg/kg of LETZ and 125 mg/kg of QUER); += Control versus PCOS; -= PCOS versus PCOS+QUER; ***p 0.001, **p 0.01, *P<0.05.
The findings demonstrated that mice with PCOS induced by LETZ had considerably increased levels of CYP17a1 expression and low levels of CYP19a1 and CYP11a1 than control mice. CYP17a1 expression in LETZ + QUER group, however, were significantly lower with the increase in CYP19a1 and CYP11a1 (p<0.01) than mice with LTZ induced PCOS (Figure 5).
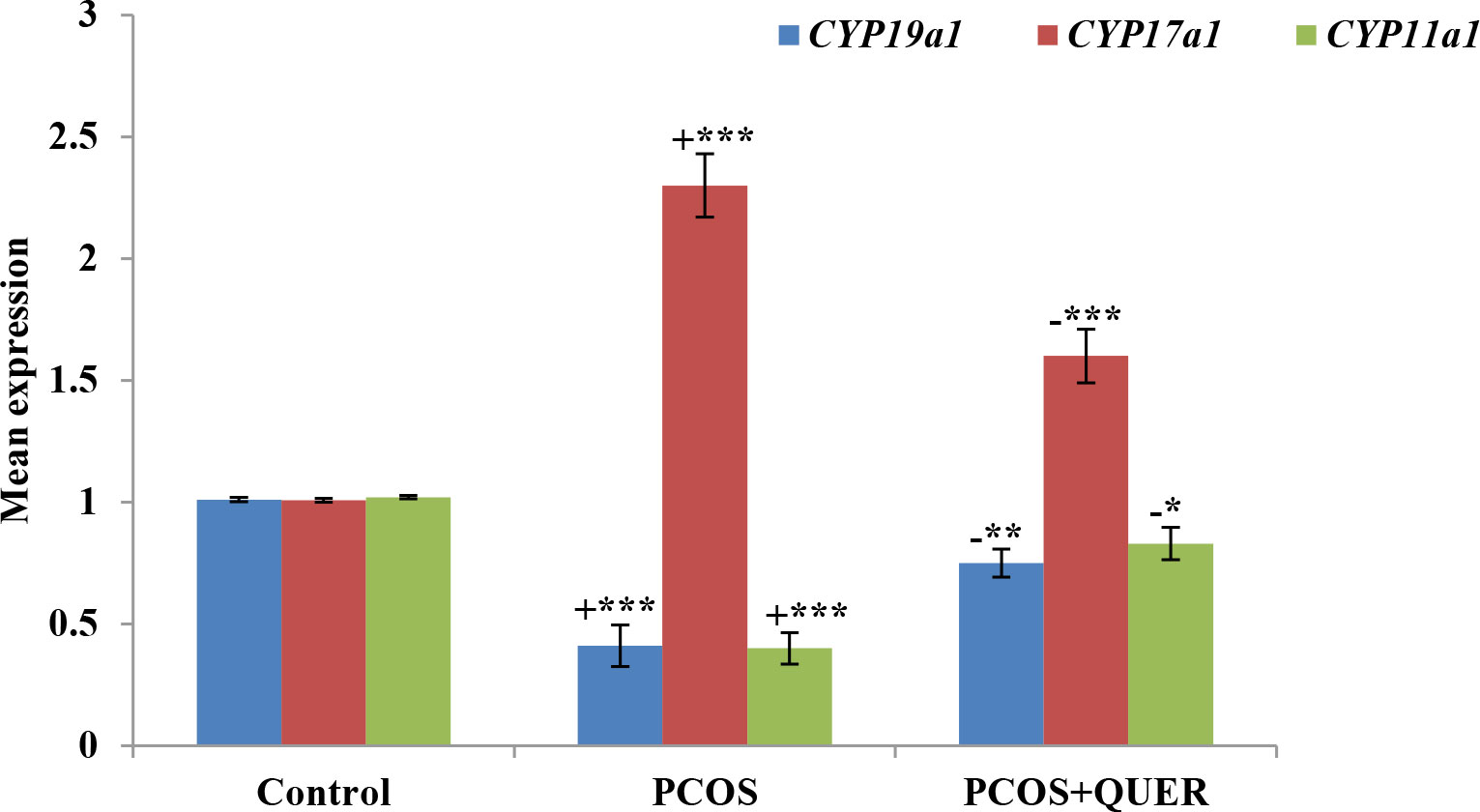
Figure 5 Effects of QUER on CYP19A1, CYP17A1 & CYP11a1 in mice with PCOS. With n=6 per group, all values are expressed as means with standard errors: Control: saline solution at 0.9%: PCOS (6 mg/kg of LETZ); PCOS+ QUER (6 mg/kg of LETZ and 125 mg/kg of QUER); += Control versus PCOS; -= PCOS versus PCOS+QUER; *p<0.05, **p<0.01, ***p<0.001.
The findings demonstrated that Ar, lhr, esr1, and fshr expressions significantly decreased mice with PCOS induced by LETZ (p<0.001). However, we saw a substantial reduction (p<0.01) in the levels of Ar, lhr, esr1, and fshr in the LETZ + QUER group in contrast to the PCOS group subjected to LETZ (Figure 6).
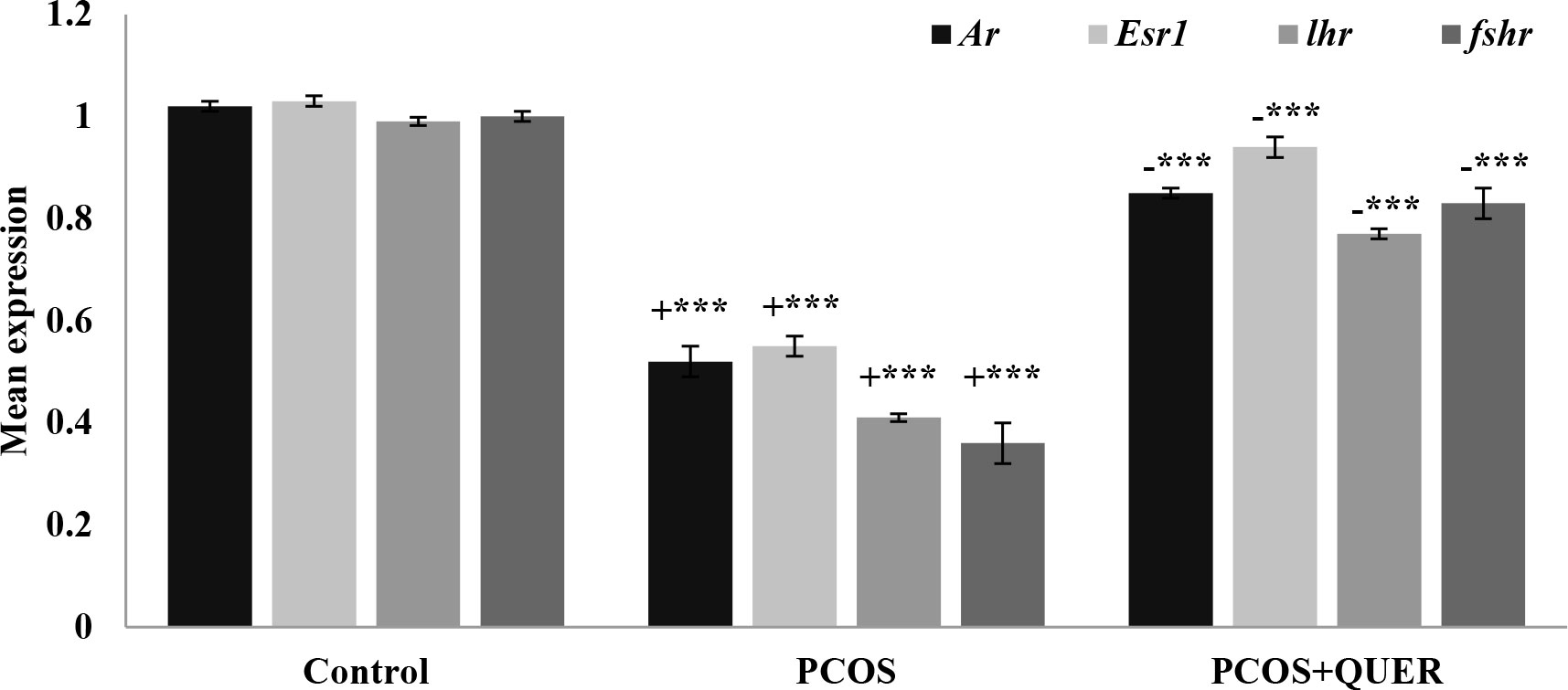
Figure 6 Effects of QUER treatment on Ar, Esr1, lhr and fshr in mice with PCOS. With n=6 per group, all values are expressed as means with standard errors: Control: saline solution at 0.9%: PCOS (6 mg/kg of LETZ); PCOS+ QUER (6 mg/kg of LETZ and 125 mg/kg of QUER); += Control versus PCOS; -= PCOS versus PCOS+QUER; ***p 0.001.
Contrary to the normal control, we saw that letrozole treatment caused the corpus luteum to degenerate, producing more cystic follicles and no ovum. We saw a drop in cystic follicles and a regeneration of the corpus luteum and ovum in the group that underwent oral gavage treatment with LETZ+QUER in contrast to the mice with LETZ induced PCOS (Figure 7).
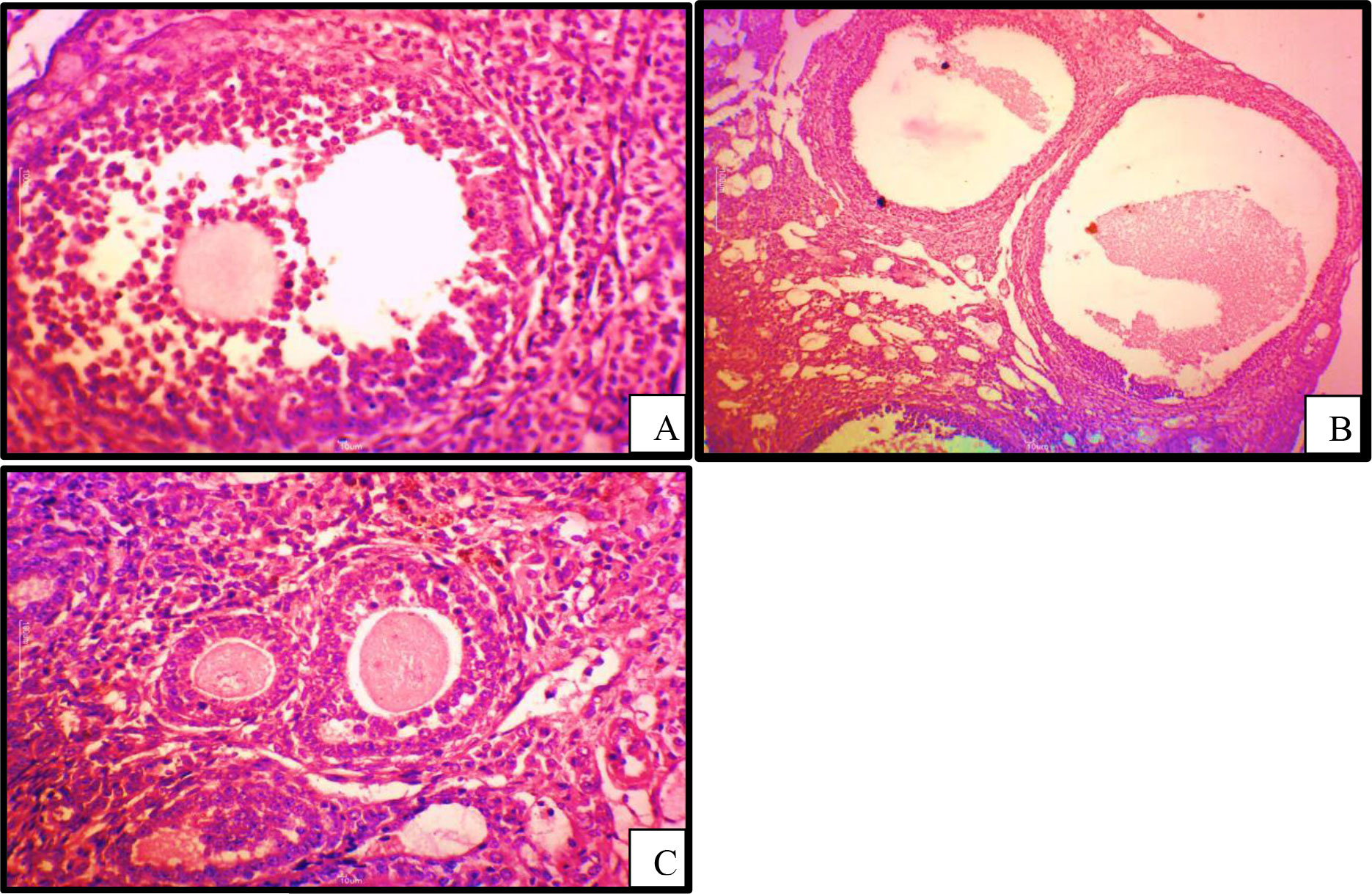
Figure 7 Photomicrographs of histological sections of ovary (H&E, magnificent x50): (A) PCOS; showing cystic follicles with degeneration of ovum (B) control; showing healthy follicle and ovum (C) PCOS treated with QUER; showing regenerated ovum with absence of cystic follicles.
We show here that quercetin (QUER) therapy is linked to anti-androgenic and anti- angiogenesis effects in the mouse ovary using a mice model of PCOS. We further show that the prolonged advantage of QUER improves ovarian function by increasing the control of genes involved to steroidogenesis and folliculogenesis. We demonstrate how QUER alters the functional, molecular, and morphological abnormalities caused by letrozole in pathological and physiological settings, particularly the problems with reproduction associated with PCOS, by regulating steroidogenesis and folliculogenesis in addition to regulating hormone receptors. The estrous cycle is known to cause changes in the hormones that control the activity of the ovaries, including follicle maturation (19). Prolonged estrus cycle with a continuous dioestrus phase was seen in our PCOS mice model, but the deficiencies were alleviated by giving the mice QUER. The PCOS rats also showed an extended diestrus phase and an irregular estrus cycle (20).
Other than type 2 diabetes, which has been previously established, women with polycystic ovarian syndrome also exhibit IR, impaired glucose tolerance, and obesity (14, 21). Result from this supported earlier research in that LETZ-induced PCOS in mice led toward increased levels of insulin, a sign of insulin resistance, a critical feature of metabolic disorders (MD’S) (14, 22). Additionally, previous studies have also shown that adiposity is exacerbated by IR which is a major contributing risk factor for obesity in metabolic and associated disorders (23, 24). Additionally, we discovered in this study that QUER treatment resulted in a considerable drop in blood insulin levels in PCOS mice, suggesting a potential function for QUER in the treatment of insulin resistance. Patients with PCOS experience hyperandrogenism as well as hyperinsulinemia, which causes adipocytes to increase catecholamine-induced lipolysis, which then results in increased serum free fatty acid levels and dyslipidemia (25). Due to the increased production of free fatty acids by the liver, TG levels in the blood are increased (3). In this work, we discovered that letrozole-treated mice had higher TC and TG levels than the control group. However, the levels significantly dropped after QUER treatment.
Pathological, physiological, and developmental angiogenesis all depend on the angiogenic factor VEGF. Oxidative stress initiates an inflammatory state that, within a feedback cycle, results in both insulin resistance and hyperandrogenism (26). According to reports, PCOS women release more VEGF (27). The mechanism is explained by the fact that the VEGF promoter region contains sites where the androgen receptor (AR) binds. When androgens bind to these locations, the VEGF gene is triggered (28). Additionally, blood of women with PCOS has lower levels of soluble VEGF receptors, which increases the bioavailability of VEGF, as shown by (29). These outcomes are in agreement with the higher VEGF levels seen in this study in the letrozole group, Furthermore VEGF levels were decreased when mice treated with quercetin.
We observed serum hormone levels to confirm the impact of quercetin on hormonal alterations. The most consistent hormonal characteristic of PCOS-affected rats is increased serum levels of androgen and LH/FSH (6), and reduced oestrogen were also noted in PCOS-afflicted mice (18). In this investigation, in contrast to levels in PCOS-afflicted mice, quercetin decreased serum LH/FSH concentration. LH levels above normal and elevated LH and FSH ratio may be used as indicators of PCO among females (30). In addition, quercetin treatment in mice with PCOS significantly reduced serum testosterone levels. PCOS illnesses may benefit from the decreasing of these elevated testosterone levels, since it has already been shown that a high androgen level contributes to aetiology of PCOS (5, 31). Contrary to testosterone, LETZ-treated mice had lower serum oestrogen levels, and the decline was associated with mid or early-follicular growth as well as creation of morphology of follicles in ovary (32). The most successful treatments for atypical symptoms linked to female reproductive illnesses are hormones and chemicals; however, these treatments come with a number of side effects, including uterine haemorrhage, and hyperplasia (33, 34). Such findings imply, quercetin might be an effective medication in treating hormonal imbalances brought on by PCOS. Lower steroid hormone levels in the ovary are correlated with higher numbers of developing follicle’s and different their shapes (35).
Kitl and Bmp1 were used in our work to investigate the ovarian follicle components, and histological investigation was also carried out. In PCOS mice ovaries, the mRNA expression of Kitl and Bmp1, are declined; and the decline reversed after QUER injection. Histological examination revealed that the PCOS-afflicted mice similarly had many cysts, small follicles, and thin granulosa cell layers. In the past, letrozole-induced follicular dysfunction was also seen, including atretic and large cysts with few granulosa cells (35). Quercetin appears to be involved in the regulation of different parameters linked to follicular development in the ovary because treatment with the drug returned ovarian follicles and its other components in the present investigation, toward normal range.
Quercetin treatment in the current study raised expression of CYP19a1 in ovary of PCOS-affected mice. Past research has shown that PCOS women have defective aromatase activity, and CYP19a1 is essential for the normal advancement of the estrous or menstrual phases in PCOS rats (5). Contrarily, reduced aromatase activity in PCOS causes disturbances in oestrogen as well as androgeen generation (36). Here it is demonstrated that mice with PCOS had decreased aromatase activity, which is congruent with the CYP19a1 and CYP11a1 mRNA levels. On the other hand, the PCOS plus QUER mice had their aromatase activity restored because CYP19a1 and CYP11a1 was highly expressed. Our results on CYP17A1 expression disagreed with Shah and Patel (37) who reported that quercetin owns useful impact in PCOS via suppressing PI3K that as a result of a reduction in CYP17A1 gene expression which critically plays function in steroidogenesis process in ovary. Additionally, the mRNA levels of Ar and Esr1 were lowered; however, in our work, quercetin therapy corrected this downregulation in mice with PCOS. Ar and Esr1 transcripts are shown to serve a function of proliferation in folllicular growth (38, 39) and elevated Ar levels could facilitate granulosa cell proliferation and differentiation (40). Additionally, quercetin treatment brought back to normal the transcriptional levels of Fshr and Lhr that had been changed in the ovaries of PCOS mice. Fshr moderately controls follicle growth during the baseline follicle growth phase by working in synergy with other stimulating substances like androgens (41). Lhr is also present on theca and granulosa cell surfaces, and Lhr levels have an impact on ovulation, the development of the corpus lutum, also on synthesis of additional steroids’ such as oestrogen, androgen and progesterone (42). Such findings led us to discover cystic degeneration of the corpus luteum and follicles in PCOS-affected animals. It’s interesting to note that the quercetin helped to slow down the degradation of ovarian follicle development by regenerating the corpus luteum and eliminating cystic follicles. It could be said that quercetinmarkedly reversing ovary physiological functions and regularity of estrous cycle. All these functions have been done via acting of quercetinon pituitary- ovary axis because of reversing normal ration of LH/FSH the main gonadotropic hormones.
Our results agree markedly with PourteymourFardTabrizi et al., (12) and Chen et al., (43) who reviewed Quercetin effects and concluded that it can recover disturbance of ovulation, decrease testosterone and Insulin resistance, adjust metabolism of lipid, ameliorate function of vascular endotheliaum and control intestinal microbiota, that all helps significantly in PCOS’ treatment. Quercetin a bio-flavonoid compound, presents in the glycosylies in vegetables and fruits. Although Quercetin analogs have antioxidant effect attributed to the amount of free “OH” groups in its composition, but Quercetin shows essential hydrophobicity (13). This may cause the recovering effect of Quercetin on PCOS mice in our study. Quercetin medical advantages are attributed to flavanols which serve as ant-inflammatory, antivirus and antioxidative stress, which are considered as three main elements that threaten the health and cause diseases, (12, 17).
It is observed that quercetin impacted positively by recovering in the PCOS in different levels: 1) systematically indicated by insulin and lipid profile. 2) Organ level as shown by reserving the ovary histology. 3) Molecular level: it regulated related genes expression and hormones in ovary cells as shown in Figure 8.
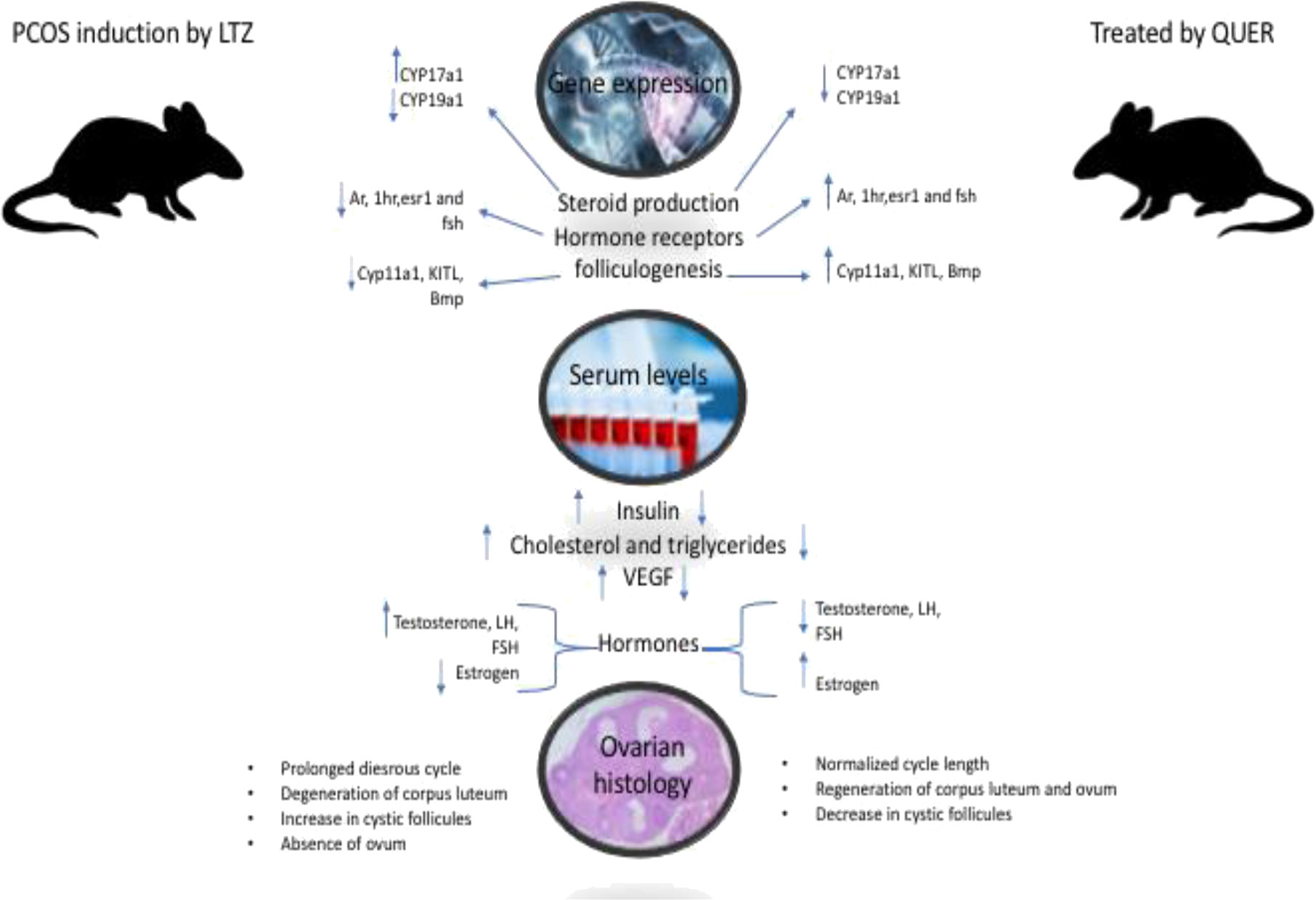
Figure 8 Shows the effect of quercetin on the tested animals in term of Genes expression that control ovary functions. It is observed that quercetin impacted positively by recovering in the PCOS in the ovary by regulating genes expression listed here and restoring hormones and lipid profile.
This study was designed to illustrate recovering effect of quercetin PCOS induced in mice model. It has proven that quercetin administration reversed experimentally abnormalities in PCOS induced by letrozole. It can speculated that PCOS has modulating- effects on regulatory genes of steroidogenesis and folliculogenesis that leading to the pathophysiological changes include (disturbance in gonadotropin as a result of related gene dysregulation, which followed by regression of ovarian follicles. Interestingly, the study has found that quercetin prevented the degradation of ovarian follicle by regenerating the corpus luteum and eliminating cystic follicles which reset the estrous cycle. The curing action of quercetin on ovary has been seen by recovering gonadotropic and gonads steroids with their physiological functions and regularity of cycle. This indicated markedly that Pituitary- ovary axis was the target of quercetin effect as it reversed normal levels and rations of LH/FSH the main gonadotropic hormones. It worth to mention that quercetin has positively treated PCOS syndrome through different biological aspects: 1) metabolic path: systematically indicated by insulin and lipid profile. 2) histological level as shown by reserving the ovary tissue structure and components. 3) Molecular level: it regulated genes expression listed above. 4) through endocrine mechanism as seen in pituitary and ovary hormones. It could be concluded that quercetin has systematic, histological and molecular improving effects on PCOC. Further research is needed to investigate safety of quercetin on body functions and organs
The original contributions presented in the study are included in the article/supplementary material. Further inquiries can be directed to the corresponding authors.
The animal study was reviewed and approved by Institutional ethical committee Barkatullah University Bhopal, India.
MZS: Conceptualization, Data curation, Software, Validation, Visualization, Writing-Review and editing, writing original draft, investigation, resources, analysis, Methodology; VS: Methodology, Project adminstration, Supervision, review and editing. MAM: Conceptualization, Methodology, Software, Review and editing; WMS, MAG, GAR, MS, SMB, MAA, MHA, AMH and EAA: Review and editing; MAA, MHA, AMH and EAA: Resources, Funding acquisition. EAA contributed in Scientific editing and revising the manuscript.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Ul Haq Shah MZ, Soni M, Shrivastava VK, Mir MA, Muzamil S. Gallic Acid reverses ovarian disturbances in mice with letrozole-induced PCOS via modulating adipo R1 expression. Toxicol Rep (2022) 9:1938–49. doi: 10.1016/j.toxrep.2022.10.009
2. Bremer AA. Polycystic ovary syndrome in the pediatric population. Metab Syndr Relat Disord (2010) 8:375–94. doi: 10.1089/met.2010.0039
3. Ul haq Shah MZ, Shrivastava V, Mir MA. Metformin treatment ameliorates endocrine-metabolic disturbances in letrozole-induced PCOS mice model by modulating adiponectin status. Obes Med Res (2022) 31:100392. doi: 10.1016/j.obmed.2022.100392
4. Codner E, Escobar-Morreale HF. Clinical review: hyperandrogenism and polycystic ovary syndrome in women with type 1 diabetes mellitus. J Clin Endocrinol Metab (2007) 92:1209–16. doi: 10.1210/jc.2006-2641
5. Kafali H, Iriadam M, Ozardali I, Demir N. Letrozole-induced polycystic ovaries in the rat: a new model for cystic ovarian disease. Arch Med Res (2004) 35:103–8. doi: 10.1016/j.arcmed.2003.10.005
6. Wang MX, Yin Q, Xu X. A rat model of polycystic ovary syndrome with insulin resistance induced by letrozole combined with high fat diet. Med Sci Monitor Int Med J Exp Clin Res (2020) 26:e922136. doi: 10.12659/MSM.922136
7. Abbott DH, Barnett DK, Bruns CM, Dumesic DA. Androgen excess fetal programming of female reproduction: a developmental aetiology for polycystic ovary syndrome hum. Reprod Update (2005) 11:357–74. doi: 10.1093/humupd/dmi013
8. Daneasa A, Cucolas C, Lenghel LM, Olteanu D, Orasan R, Filip GA. Letrozole vsestradiolvalerate induced PCOS in rats: glycemic, oxidative and inflammatory status assessment. Reproduction (2016) 151:401–9. doi: 10.1530/REP-15-0352
9. Chen T, Jia F, Yu Y, Zhang W, Wang C, Zhu S, et al. Potential role of quercetin in polycystic ovary syndrome and its complications: a review. Molecules (2022) 27(14):4476. doi: 10.3390/molecules27144476
10. Badawy A, Elnashar A. Treatment options for polycystic ovary syndrome. Int J Womens Health (2011) 3:25–35. doi: 10.2147/IJWH.S11304
11. Neisy A, Zal F, Seghatoleslam A, Alaee S. Amelioration by quercetin of insulin resistance and uterine GLUT4 and ERα gene expression in rats with polycystic ovary syndrome (PCOS). Reprod Fertil Dev (2019) 31(2):315–23. doi: 10.1071/RD18222
12. PourteymourFardTabrizi F, Hajizadeh-Sharafabad F, Vaezi M, Jafari-Vayghan H, Alizadeh M, Maleki V. Quercetin and polycystic ovary syndrome, current evidence and future directions: a systematic review. J Ovarian Res (2020) 13(1):11. doi: 10.1186/s13048-020-0616-z
13. Shu X, Hu XJ, Zhou SY, Xu CL, Qiu QQ, Nie SP, et al. Yao xuexuebao. ActapharmaceuticaSinica (2011) 46(9):1051–7.
14. Zheng S, Chen Y, Ma M, Li M. Mechanism of quercetin on the improvement of ovulation disorder and regulation of ovarian CNP/NPR2 in PCOS model rats. J Formosan Med Assoc Taiwan Yizhi (2022) 121(6):1081–92. doi: 10.1016/j.jfma.2021.08.015
15. Rezvan N, Moini A, Janani L, Mohammad K, Saedisomeolia A, Nourbakhsh M, et al. Effects of quercetin on adiponectin-mediated insulin sensitivity in polycystic ovary syndrome: a randomized placebo-controlled double-blind clinical trial. Horm Metab Res (2017) 49(2):115–21. doi: 10.1055/s-0042-118705
16. Mahmoud AA, Elfiky AM, Abo-Zeid FS. The anti-androgenic effect of quercetin on hyperandrogenism and ovarian dysfunction induced in a dehydroepiandrosterone rat model of polycystic ovary syndrome. Steroids (2022) 177:108936. doi: 10.1016/j.steroids.2021.108936
17. Soni M, Shah M, Shrivastava VK. The hypoglycemic and anti-hyperlipidemic activity of vitamin c in di(2-ethylhexyl) phthalate-induced toxicity in female mice, mus musculus. Comp Clin Pathol (2023). doi: 10.1007/s00580-023-03466-1
18. Shah M, Shrivastava VK. Turmeric extract alleviates endocrine-metabolic disturbances in letrozole-induced PCOS by increasing adiponectin circulation: a comparison with metformin. Metab Open (2021) 13:100160. doi: 10.1016/j.metop.2021.100160
19. Sun J, Jin C, Wu H, Zhao J, Cui Y, Liu H, et al. Effects of electroacupuncture on ovarian P450arom, P450c17alpha and mRNA expression induced by letrozole in PCOS rats. PloS One (2013) 8:e79382. doi: 10.1371/journal.pone.0079382
20. Soumya V, Muzib YI, Venkatesh P. A novel method of extraction of bamboo seed oil (BambusabambosDruce) and its promising effect on metabolic symptoms of experimentally induced polycystic ovarian disease. Indian J Pharmacol (2016) 48(2):162–7. doi: 10.4103/0253-7613.178833
21. Joham AE, Teede HJ, Ranasinha S, Zoungas S, Boyle J. Prevalence of infertility and use of fertility treatment in women with polycystic ovary syndrome: data from a large community-based cohort study. J Womens Health (Larchmt) (2015) 24(4):299–307. doi: 10.1089/jwh.2014.5000
22. Cussons AJ, Watts GF, Burke V, Shaw JE, Zimmet PZ, Stuckey BG. Cardiometabolic risk in polycystic ovary syndrome: a comparison of different approaches to defining the metabolic syndrome. Hum Reprod (2008) 23(10):2352–8. doi: 10.1093/humrep/den263
23. Stanhope KL, Schwarz JM, Keim NL, Griffen SC, Bremer AA, Graham JL, et al. Consuming fructose-sweetened, not glucose-sweetened, beverages increases visceral adiposity and lipids and decreases insulin sensitivity in overweight/obese humans. J Clin Invest (2009) 119(5):1322–34. doi: 10.1172/JCI37385
24. Shah MZ, Shrivastava VK. Ameliorative effects of quercetin on endocrine and metabolic abnormalities associated with experimentally induced polycystic ovary syndrome in mice. Comp Clin Pathol (2023), 32–1. doi: 10.1007/s00580-023-03446-5
25. Diamanti-Kandarakis E, Papavassiliou AG, Kandarakis SA, Chrousos GP. Pathophysiology and types of dyslipidemia in PCOS. Trends Endocrinol Metabol: TEM (2007) 18(7):280–5. doi: 10.1016/j.tem.2007.07.004
26. El-bahya AAZ, Radwanb RA, Gadc MZ, Abdel SM. A closer insight into the role of vitamin d in polycystic ovary syndrome (Pcos). Glob J Pharmaceu Sci (2018) 6(4). doi: 10.19080/GJPPS.2018.06.555692
27. Artini PG, Ruggiero M, ParisenToldin MR, Monteleone P, Monti M, Cela V, et al. Vascular endothelial growth factor and its soluble receptor in patients with polycystic ovary syndrome undergoing IVF, hum. Fertil (2009) 12(1):40–4. doi: 10.1080/14647270802621358
28. Eisermann K, Broderick CJ, Bazarov A, Moazam MM, Fraizer GC. Androgen up-regulates vascular endothelial growth factor expression in prostate cancer cells via an Sp1 binding site, mol. Cancer (2013) 12:(1). doi: 10.1186/1476-4598-12-7
29. Almawi WY, Gammoh E, Malalla ZH, Al-Madhi SA. Analysis of VEGFA variants and changes in VEGF levels underscores the contribution of VEGF to polycystic ovary syndrome. PloS One (2016) 11(11):e0165636. doi: 10.1371/journal.pone.0165636
30. Saadia Z. Follicle stimulating hormone (LH: FSH) ratio in polycystic ovary syndrome (PCOS) - obese vs. non- obese women. Med Arch (Sarajevo Bosnia Herzegovina) (2020) 74(4):289–93. doi: 10.5455/medarh.2020.74.289-293
31. Abbott DH, Dumesic DA, Franks S. Developmental origin of polycystic ovary syndrome - a hypothesis. J Endocrinol (2002) 174:1–5. doi: 10.1677/joe.0.1740001
32. Dewailly D, Robin G, Peigne M, Decanter C, Pigny P, CatteauJonard S. Interactions between androgens, FSH, anti-mullerian hormone and estradiol during folliculogenesis in the human normal and polycystic ovary. Hum Reprod Update (2016) 22:709–24. doi: 10.1093/humupd/dmw027
33. Hidaka T, Yonezawa R, Saito S. Kami-shoyo-san, kampo (Japanese traditional medicine), is effective for climacteric syndrome, especially in hormone-replacement-therapy-resistant patients who strongly complain of psychological symptoms. J Obstet Gynaecol Res (2013) 39:223–8. doi: 10.1111/j.1447-0756.2012.01936.x
34. Yang H, Kim HJ, Pyun BJ, Lee HW. Licorice ethanol extract improves symptoms of polycytic ovary syndrome in letrozole-induced female rats. Integr Med Res (2018) 7:264–70. doi: 10.1016/j.imr.2018.05.003
35. Baravalle C, Salvetti NR, Mira GA, Pezzone N, Ortega HH. Microscopic characterization of follicular structures in letrozoleinduced polycystic ovarian syndrome in the rat. Arch Med Res (2006) 37:830–9. doi: 10.1016/j.arcmed.2006.04.006\
36. Chen J, Shen S, Tan Y, Xia D, Xia Y, Cao Y, et al. The correlation of aromatase activity and obesity in women with or without polycystic ovary syndrome. J Ovarian Res (2015) 8:11. doi: 10.1186/s13048-015-0139-1
37. Shah KN, Patel SS. Phosphatidylinositide 3-kinase inhibition: a new potential target for the treatment of polycystic ovarian syndrome. Pharm Biol (2016) 54(6):975–83. doi: 10.3109/13880209.2015.1091482
38. Hammes SR. Androgens regulate ovarian follicular development by increasing follicle stimulating hormone receptor and microRNA-125b expression. Proc Natl Acad Sci United States America (2014) 111(8):3008–13. doi: 10.1073/pnas.1318978111
39. Chauvin S, Cohen-Tannoudji J, Guigon ,CJ. EstradiolSignaling at the heart of folliculogenesis: its potential deregulation in human ovarian pathologies. Int J Mol Sci (2022) 23(1):512. doi: 10.3390/ijms23010512
40. Hasegawa T, Kamada Y, Hosoya T, Fujita S, Nishiyama Y, Iwata N, et al. A regulatory role of androgen in ovarian steroidogenesis by rat granulosa cells. J Steroid Biochem Mol Biol (2017) 172:160–5. doi: 10.1016/j.jsbmb.2017.07.002
41. George JW, Dille EA, Heckert LL. Current concepts of follicle-stimulating hormone receptor gene regulation. Biol Reprod (2011) 84(1):7–17. doi: 10.1095/biolreprod.110.085043
42. Edson MA, Nagaraja AK, Matzuk MM. The mammalian ovary from genesis to revelation.Endocr. Rev (2009) 30:624–712. doi: 10.1210/er.2009-0012
Keywords: PCOS (polycystic ovarian syndrome), steroidogenesis, folliculogenesis, quercetin, VEGF
Citation: Shah MZuh, Shrivastva Vk, Mir MA, Sheikh WM, Ganie MA, Rather GA, Shafi M, Bashir SM, Ansari MA, Al-Jafary MA, Al-Qahtani MH, Homeida AM and Al-Suhaimi EA (2023) Effect of quercetin on steroidogenesis and folliculogenesis in ovary of mice with experimentally-induced polycystic ovarian syndrome. Front. Endocrinol. 14:1153289. doi: 10.3389/fendo.2023.1153289
Received: 30 January 2023; Accepted: 07 April 2023;
Published: 24 April 2023.
Edited by:
Bin Liu, Jinan University, ChinaReviewed by:
Vikas Kumar Roy, Mizoram University, IndiaCopyright © 2023 Shah, Shrivastva, Mir, Sheikh, Ganie, Rather, Shafi, Bashir, Ansari, Al-Jafary, Al-Qahtani, Homeida and Al-Suhaimi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mohd Zahoor ul haq Shah, c2Nob2xhcmVuZG9jcmlub2xvZ3lAZ21haWwuY29t; Showkeen Muzamil Bashir, c2hvd2tlZW5Ac2t1YXN0a2FzaG1pci5hYy5pbg==; Ebtesam A. Al-Suhaimi, ZWFsc3VoYWltaUBpYXUuZWR1LnNh
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.