- 1Institute of Metabolic Diseases, Guang’ anmen Hospital, China Academy of Chinese Medical Sciences, Beijing, China
- 2Beijing University of Chinese Medicine, Beijing, China
Aims/hypothesis: Through a comprehensive analysis of the clinical randomized controlled trials of traditional Chinese medicine (TCM) combined with conventional western medicine (CWM) in treating type 2 diabetes(T2DM) in the past ten years, the clinical efficacy and safety of different TCMs combined with CWM were explored. This study aimed to provide specific suggestions for clinical guidance on treating T2DM.
Methods: A literature search was conducted in CNKI, WanFang, VIP, CBM, PubMed, Embase, and Web of Science. The search time was limited from 2010 to the present time. The literature type was a controlled clinical trial study of TCM combined with CWM intervention in treating T2DM. The outcome indices of the efficacy evaluation included fasting blood glucose (FBG), 2-hour postprandial blood glucose (2hPG), glycosylated hemoglobin (HbA1c), adverse reactions, and clinical efficacy. Stata 15 and RevMan 5.4 software were used to conduct a network meta-analysis and a traditional meta-analysis.
Results: The results showed that shenqi jiangtang granule combined with sulfonylurea, shenqi jiangtang granules combined with metformin and jinlida granules combined with insulin had significant effects on reductions in FBG, 2hPG and clinical efficacy compared with western medicines alone, which included fasting blood glucose [MD=-2.17, 95%CI=(-2.50, -1.85)], blood sugar at 2 hours after a meal [MD=-1.94, 95%CI=(-2.23, -1.65)], and clinical curative effect [OR= 1.73, 95%CI=(0.59, 2.87)].
Conclusions: TCM combined with CWM has a very significant effect on treating T2DM compared with CWM alone. According to the network meta-analysis, the best intervention measures of different TCMs for different outcome indicators were obtained.
Systematic review registration: identifier 42022350372.
1 Introduction
Diabetes is a complex metabolic disease. The prevalence of diabetes has been increasing in recent years, and it has become the ninth leading cause of death throughout the world. This disease is a major public health problem affecting the entire world. Long-term exposure to a hyperglycemic environment in patients with diabetes can lead to abnormalities in various immune cells, thus negatively affecting multiple organs and leading to many common complications (1). The improper management of diabetes metabolism can also lead to serious long-term complications, including retinopathy, kidney disease, neuropathy, and cardiovascular disease, thus leading to significantly increased mortality. In 2019, the International Diabetes Federation reported that the number of people with diabetes is estimated at 463 million and will increase to 700 million by 2045 (2). Many risk factors and biological processes have been shown to contribute to the development of type 2 diabetes(T2DM), including hyperglycemia, hyperinsulinemia, insulin resistance, lipid accumulation, inflammation, oxidative stress, and adipokines (3). In addition, T2DM is caused by insulin resistance (IR), which leads to an increased demand for insulin in peripheral tissues and resulting in β-cell function failure. The core of the disease course is the impaired function of islet β-cells. However, there is a question as to how to improve the impaired function of islet β-cells and avoid the risk factors for T2DM.
The use of antidiabetic drugs is an ideal treatment method in clinical practice. Nevertheless, many drugs may lead to hypoglycemia, body fluid retention, cardiovascular disease, and other adverse reactions. However, there is a question as to how to choose the most effective treatment method exhibiting the most minor negative reactions. Currently, commonly used drugs for the treatment of diabetes include biguanides (metformin), sulfonylureas (SHD), dipeptidyl peptidase 4 inhibitors (DPP-IV), α-glucosidase inhibitors (AGI), and insulin (RI), among other drugs. According to the clinical efficacy, these drugs have very significant hypoglycemic effects. Some drugs, such as glucagon-like peptide-1 receptor agonist (GLP-1), can also reduce cardiovascular death and stroke in clinical diabetic patients, thus showing a perfect clinical effect. Drugs such as empagliflozin or liraglutide also reduce all-cause and cardiovascular mortality (4). With the development of traditional Chinese medicine (TCM), the clinical application of TCM combined with conventional western medicine (CWM) in treating T2DM is increasingly extensive. For example, studies have found that TCM can regulate the intestinal flora and improve glucose metabolism in patients with T2DM (5); moreover, the intestinal flora is essential for maintaining host health, and an increasing number of studies have been conducted on the treatment of diseases by targeting the intestinal flora with TCM, which fully demonstrates the advantages of TCM in this scenario. As characterized by syndrome differentiation and with a focus on symptom improvement, TCM has apparent benefits in the treatment of T2DM and its complications. TCM is characterized by multiple links, approaches, and targets in the prevention and treatment of diabetes, which is the advantage of TCM syndrome differentiation (6). TCM combined with CWM can reduce the risk of adverse reactions caused by a single treatment, such as gastrointestinal and hypoglycemia reactions. This study conducted a network meta-analysis on the intervention of TCM combined with CWM in T2DM, to explore the efficacy and safety ranking of the current treatment of T2DM, for guiding the optimal clinical treatment measures.
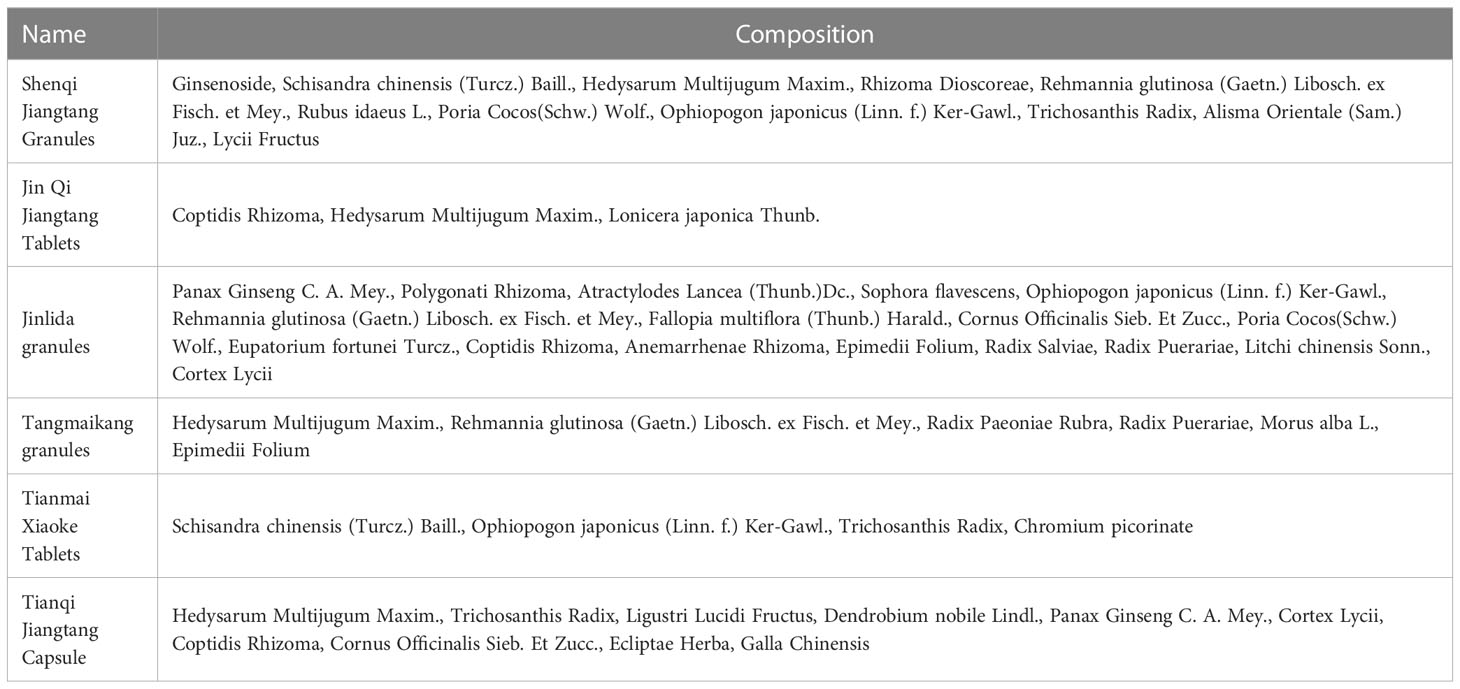
The intervention measures that were included in this study included shenqi jiangtang granules (SQJT), jinqi jiangtang tablets (JQJT), jinlida granules (JLD), tangmaikang granules (TMK), tianmai xiaoke tablets (TMXKP), tianqi jiangtang capsules (TQJT) and CWM intervention. The included TCM is recommended according to China’s Guidelines for the Prevention and Treatment of Type 2 Diabetes (2020 Edition). The selection of TCM has been unanimously agreed upon by clinical experts, and it is the medicine that possesses a significant effect on the treatment of T2DM. Due to the fact that it was approved by the State Food and Drug Administration in 1995, SQJT has successively entered the National Essential Medicine list and the National Medical Insurance List, and it has also won the National Torch project. A considerable amount of research data has been accumulated in the past 20 years. JQJT was approved by the Ministry of Health of the People’s Republic of China on August 19, 1992, and it won the third prize in science and technology progress in 1993. Moreover, JLD, which was launched in 2019, is an innovative TCM developed under the guidance of collateral disease theory and has a significant clinical market. The TCM included in this study has a mature basis for early clinical application, and has good effects on the treatment of T2DM. The specific ingredients of TCM are shown in Table 1. Traditional Western drugs included biguanides (metformin), sulfonylureas (SHD), dipeptidyl peptidase 4 inhibitors (DPP-IV), α-glucosidase inhibitors (AGI), insulin (RI), and glucagon-like peptide-1 receptor agonists (GLP-1). This study aimed to conduct a paired meta-analysis of head-to-head randomized controlled trials (RCTs) that were included in significant databases, followed by a network meta-analysis based on direct and indirect comparisons of standard controls (conventional western medicines). Currently, the indirect treatment of different TCMs combined with CWM is relatively small in clinical practice. In this study, a network meta-analysis was used to conduct direct and indirect analyses of the intervention of different TCMs combined with CWM to explore the optimal therapeutic means for the clinical treatment of T2DM.
2 Methods
2.1 Literature search
This network meta-analysis was conducted according to the PRISMA Extended Statement, and it was performed step-by-step in strict accordance with the PRISMA Checklist. This study has been registered on the International Prospective Register for Systems Evaluation (PROSPERO) website as CRD number 42022350372.
The literature search time of this study ranged from January 2010 to October 2022. The literature search was conducted by searching the CNKI, WanFang, VIP, CBM, PubMed, Embase, and Web of Science databases and was screened according to the inclusion and exclusion criteria. The primary screening direction was a randomized controlled trial (RCT) of TCM combined with CWM in the treatment of T2DM. The included TCMs included SQJT, JQJT, JLD, TMK, TQJT, and TMXKP. In addition, the included CWMs were as follows: sulfonylureas (SHD), biguanides (metformin), dipeptidyl peptidase-4, α-glucosidase inhibitors (DPP-IV), alpha-glucosidase inhibitors (AGI), insulin (RI), and glucagon-like peptide-1 (GLP-1),which were uniformly divided into the category of CWM. Two researchers independently conducted a literature search, and the Chinese database used “Shenqi Jiangtang Granules”, “Jinqi Jiangtang tablets”, “Jinlida granules”, “Tangmaikang granules”, “Tianqi Jiangtang capsules”, “Tianmai Xiaoke tablets”, “Conventional Western medicine”, “Type 2 diabetes mellitus”, for the literature search. English databases under “shenqi jiangtang”, “jinqi jiangtang”, “jinlida”, “tangmaikang”, “tianqi jiangtang”, “tianmai xiaoke”, and “diabetes”, were retrieved in the form of subject words + free words. Two researchers independently conducted a literature search. After selecting the weight, some types of literature were screened according to the title and abstract. Finally, the final selection was performed according to the reading of the full text to obtain the final included literature.
2.2 Criteria for inclusion
The included research criteria were as follows. (1) Research on the treatment of T2DM with TCM combined with CWM that met the requirements of this paper, with traditional Chinese medicine including SQJT, JQJT, JLD, TMK, TQJT, and TMXKP and conventional Western medicine including SHD, metformin, DPP-IV, AGI, RI, and GLP-1. (2) Randomized controlled clinical trials (RCTs). (3) The intervention time being at least 2 months. (4) The included literature including at least one outcome indicator required by this study. (5) Adults with T2DM (≥18 years old). (6) Research data in the literature that was able to be obtained through public platforms.
2.3 Exclusion criteria
The exclusion criteria for this study were as follows: (1) the publication was an animal experiment, an academic conference, a paper, or a nonrandomized controlled trial (RCT). (2) TCM and CWM that did not meet the requirements of the study. (3) literature published as an abstract only. (4) a sole focus on laboratory findings that were not RCTs, reviews, or reports. (5) repeated publications of literature. (6) the literature with complete data that could not be obtained after contacting the author.
2.4 Data extraction and quality assessment
Two researchers independently extracted the data of the included literature and assessed the bias risk of the included literature. Data extraction was performed according to the Excel table, which was prepared in advance. The extraction contents of the table was comprised of the author of the included literature, publication year, intervention group, age, sex, course of the disease, the total number of included studies, the grouping method of the clinical studies, whether the blind method was implemented, outcome indicators, intervention and follow-up times, specific measures of intervention, and the value of the outcome indicators, among other contents. If there was a dispute, a third researcher discussed it with the other researchers. We conducted a risk assessment of the included studies by using the Cochrane ROB Bias risk assessment tool that was used to assess the RCTs. The risk levels were high, medium, and low risk, and the literature was independently evaluated by two investigators by using the same standardized methodology. The risk of bias in the included literature was evaluated by considering randomization, assignment concealment, whether participants and researchers were blinded, the blind evaluation of outcome indicators, and selective reporting.
2.5 Outcomes
According to the consensus of clinical experts and previous experience, we selected FBG, 2hPG, HbA1c, clinical efficacy, and incidence of adverse reactions as important outcome indicators to evaluate the effectiveness of TCM combined with CWM in the intervention of T2DM.
2.6 Statistical analysis
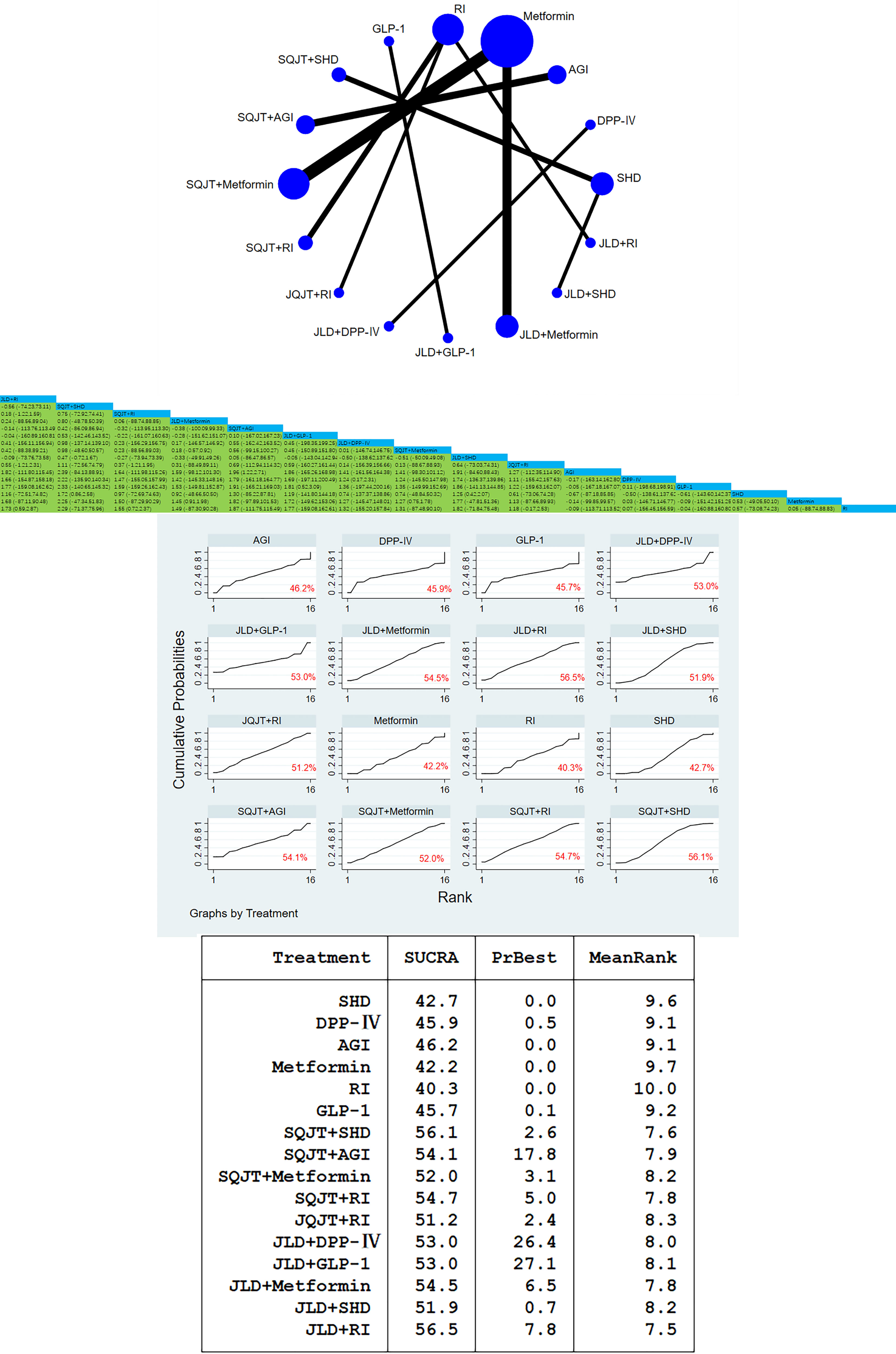
In this study, a combination of traditional meta-analysis and network meta-analysis was used to analyze the included literature. Traditional meta-analysis aims to explore the efficacy of direct interventions of different TCMs combined with CWM in the treatment of T2DM. In contrast, network meta-analysis is an overall comparison of various intervention measures; specifically, direct and indirect comparisons. We combined RevMan 5.4 software and Stata15 software package “net meta” to analyze the literature, wherein we used the I2 index to evaluate the heterogeneity among the studies and hypothesized homogeneity. For binary variables, the OR index was used. For continuous variables, the MD index was used. Moreover, we used 95% confidence intervals (CIs) to determine the clinical effect of the included study. We performed a frequency network meta-analysis by using Stata software to analyze indirect comparisons between different interventions. The probability of an intervention being the safest and most effective was estimated by using the area under cumulative ranking, and the relative ranking probability of different interventions was displayed. The effect values and 95%CIs of pair-to-pair comparisons between the interventions were clearly expressed by using league tables, and the inconsistencies of the results were confirmed using the node-splitting method and Bayes P value. However, inconsistencies could not be assessed because the network meta-analysis did not close the loop. Furthermore, a sensitivity analysis was used to determine the risk of bias in the included studies. According to the differences among the literature included in the intensive reading, the similarity hypothesis was formulated. Via the various statistical analyses, the different effects of intervention measures and clinical efficacy were completely analyzed.
3 Results
3.1 The process of literature retrieval and the primary research characteristics of the included literature
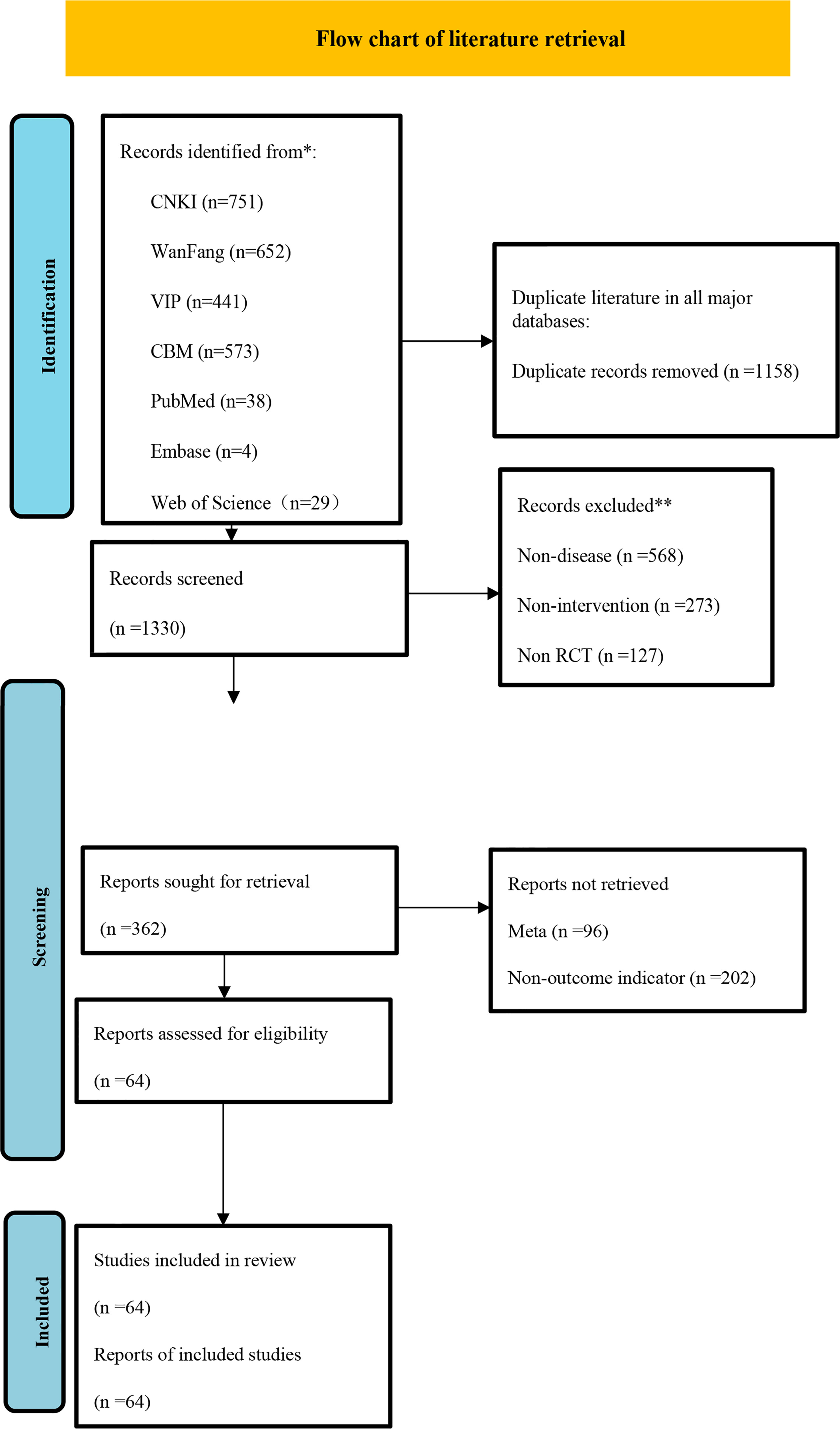
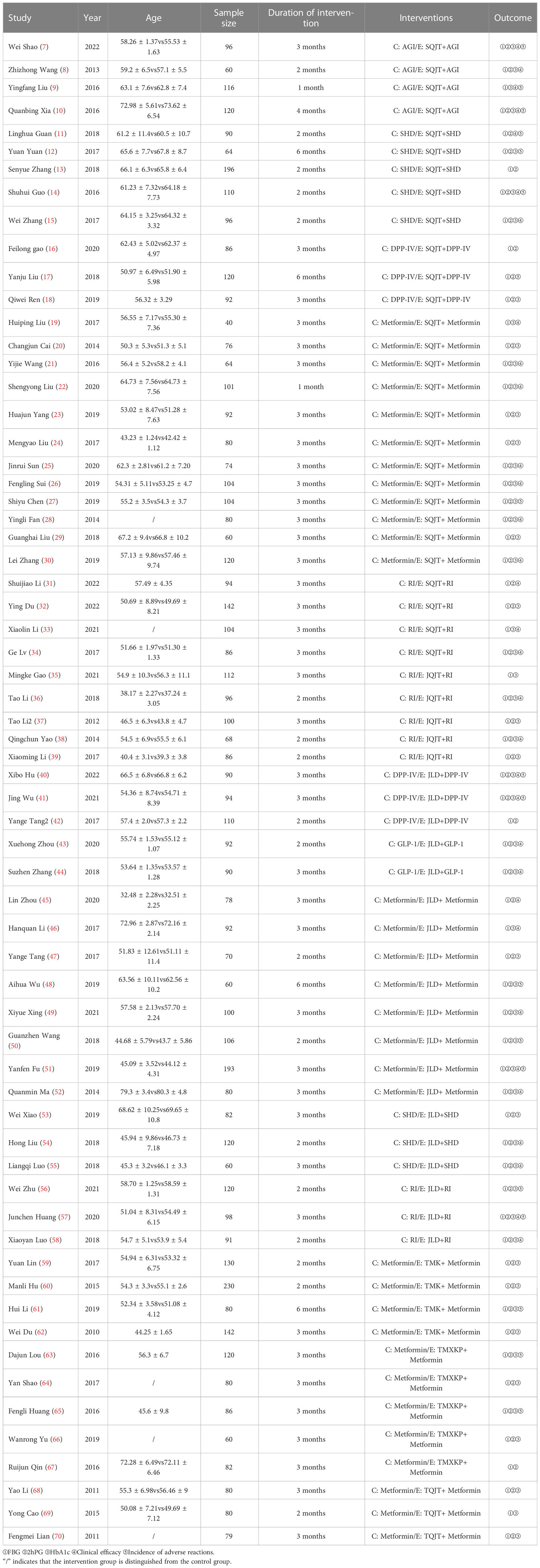
After literature retrieval in various major databases according to strict exclusion criteria, 64 studies were finally included. Two researchers independently extracted the included literature according to Excel tables. The flow charts and essential characteristics of the included literature are shown in Figure 1 and Table 2 respectively.
3.2 Risk of bias in included studies
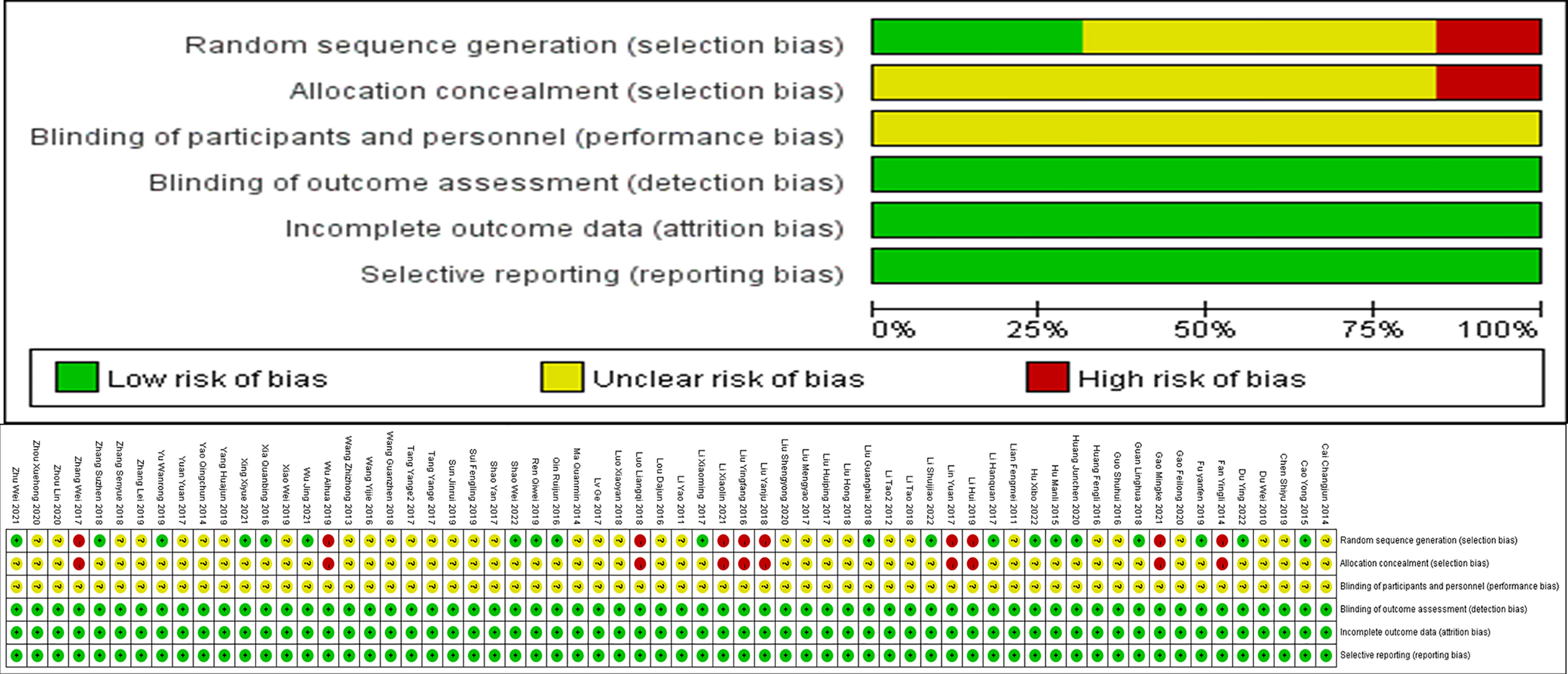
This study conducted a detailed assessment of the risk of bias using Cochrane assessment methods. Random sequence generation, Allocation concealment, Blinding of participants and personnel, Blinding of outcome assessment, Incomplete outcome data, and Selective reporting were analyzed, and the results are shown in Figure 2.
3.3 Traditional and network meta-analyses of outcome measures
3.3.1 FBG
3.3.1.1 Traditional meta-analysis and network meta-analysis and league table
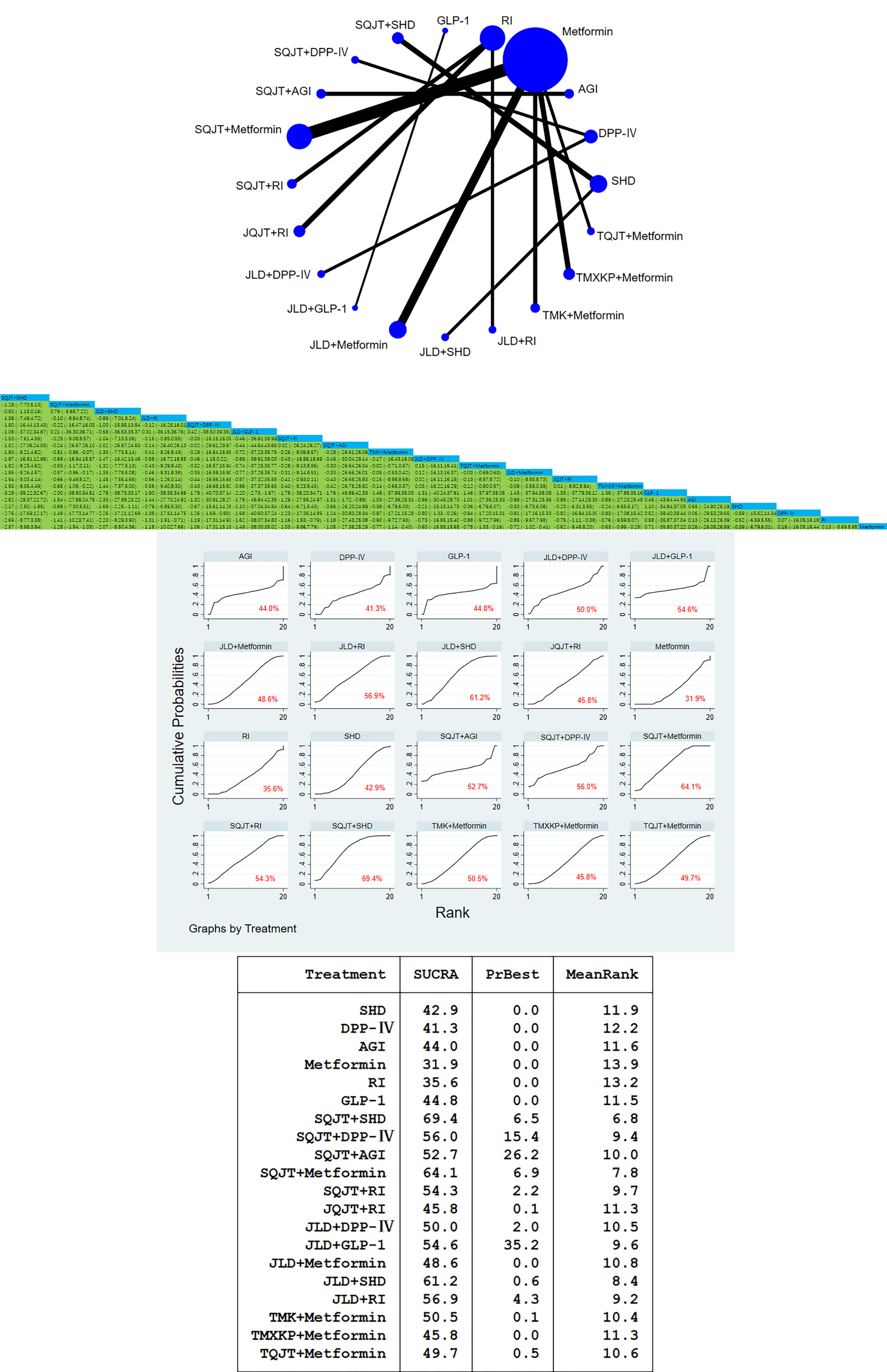
64 studies, a total of 6204 patients, all included the outcome index FBG. After traditional meta-analysis and network meta-analysis of FBG, it was concluded that the number of studies on SQJT combined with Metformin and JLD combined with Metformin was the largest. According to the result of direct and indirect comparison of TCM combined with CWM treatment: TCM combined with different CWM has significant hypoglycemic effect compared with simple CWM, among which, SQJT combined with SHD and JLD combined with SHD compared with simple SHD have hypoglycemic effect value [MD=-2.17, 95%CI=(-2.50, -1.85)], [MD=-1.68,95%CI=(-2.25,-1.11)]; SQJT combined with Metformin are better than Metformin alone, TMXKP combined with Metformin and TMK combined with Metformin, hypoglycemic effect value of respectively [MD=- 1.28, 95%CI=(-1.54, -1.03)], [MD=-0.65, 95%CI=(-1.09, -0.22)], [MD=-0.51, 95%CI=(-0.96, -0.07)]. The hypoglycemic effect of JLD combined with RI, SQJT combined with RI and JQJT combined with RI was significantly better than that of RI alone, effect value of respectively [MD=- 1.31, 95%CI=(-1.91, -0.71)], [MD=-1.16, 95%CI=(-1.53, -0.79)], [MD=-0.75, 95%CI=(-1.11, -0.38)] (Figure 3).
3.3.1.2 Cumulative curves under the area chart sort
According to the area ranking diagram under the FBG accumulation curve of the outcome index, SQJT combined with SHD had the best effect in reducing the FBG content among the intervention measures, while the hypoglycemic effect of CWM alone was significantly lower than that of other TCM combined with CWM. The sequence of hypoglycemic effect of comprehensive intervention measures is as follows: SQJT+SHD > SQJT+Metformin > JLD+SHD > JLD+RI > SQJT+DPP-IV > JLD+GLP-1 > SQJT+RI > SQJT+AGI > TMK+Metformin > JLD+DPP-IV > TQJT+Metformin > JLD+Metformin > JQJT+RI > TMXKP+Metformin > GLP-1 > AGI > SHD > DPP-IV > RI > Metformin, which proves that TCM combined with CWM has a significant effect on reducing FBG content, and SQJT combined with SHD has the most significant effect (Figure 3).
3.3.2 2hPG
3.3.2.1 Traditional meta-analysis and network meta-analysis and league table
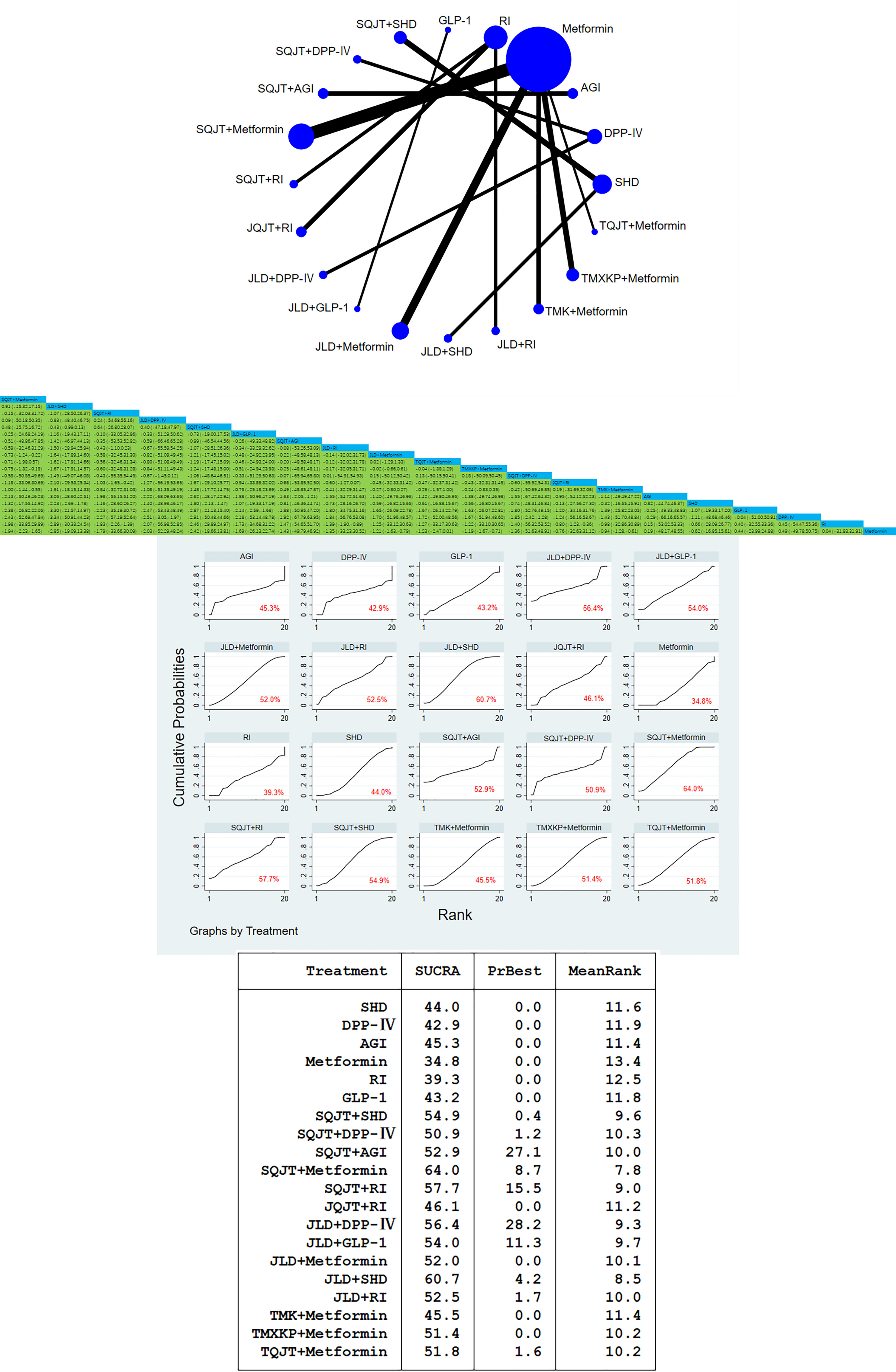
A total of 59 studies, involving a total of 5772 patients, included 2-hour postprandial glucose outcomes. In this study, traditional meta-analysis and network meta-analysis of blood glucose 2 hours after meals showed that there were most studies on the comparison between SQJT combined with Metformin, JLD combined with Metformin and Metformin alone, and most of the studies were direct comparison between TCM combined with CWM and CWM, while there was no direct comparison between different TCM. According to the result of 2hPG, SQJT combined with Metformin, JLD combined with Metformin, TMXKP combined with Metformin and TMK combined with Metformin have significant hypoglycemic effects compared with Metformin alone, effect value of respectively [MD=-1.94, 95%CI=(-2.23, -1.65)], [MD=-1.21, 95%CI=(-1.63, -0.79)], [MD=-1.19, 95%CI=(-1.67, -0.71)], [MD=-0.94, 95%CI=(-1.28,-0.61)]; The therapeutic effect of JLD combined with SHD and SQJT combined with SHD was significantly better than that of SHD alone, and the effect values were [MD=-2.23,95%CI=(-2.69,-1.78)] and [MD=-1.80,95%CI=(-2.13,-1.47)]; The hypoglycemic effect of SQJT combined with RI and JLD combined with RI was better than that of RI alone, and the effect values were [MD=-1.83,95%CI=(-2.26,-1.39)] and [MD=-1.39,95%CI=(-1.90,-0.89), respectively]; The above are the direct comparison between different TCM combined with CWM and simple CWM treatment, while the indirect comparison results between different TCM combined with CWM show that, the hypoglycemic effect of SQJT combined with Metformin is better than that of JLD combined with Metformin, TMXKP combined with Metformin and TMK combined with Metformin, effect value of respectively [MD=-0.73, 95%CI=(-1.24, -0.22)], [MD=-0.75, 95%CI=(-1.32, -0.19)], [MD=-1.00, 95%CI=(-1.44, -0.55)]; The therapeutic effect of SQJT combined with RI was better than that of JQJT combined with RI, and the effect value was [MD=-1.03,95%CI=(-1.65,-0.42)] (Figure 4).
3.3.2.2 Cumulative curves under the area chart sort
According to the outcome index, the area sorting diagram under the 2hPG accumulation curve showed that SQJT combined with Metformin had the most significant effect on reducing the 2hPG. The therapeutic effect ranking of various interventions is as follows: SQJT+Metformin > JLD+SHD > SQJT+RI > JLD+DPP-IV > SQJT+SHD > JLD+GLP-1 > SQJT+AGI > JLD+RI > JLD+Metformin > TQJT+Metformin > TMXKP+Metformin > SQJT+DPP-IV > JQJT+RI > TMK+Metformin > AGI > SHD > GLP-1 > DPP-IV > RI > Metformin, which proves that TCM combined with CWM has a significant effect on reducing 2hPG compared with CWM alone. The league table clearly shows the 95%CI for each intervention (Figure 4).
3.3.3 HbA1c
3.3.3.1 Traditional meta-analysis and network meta-analysis and league table
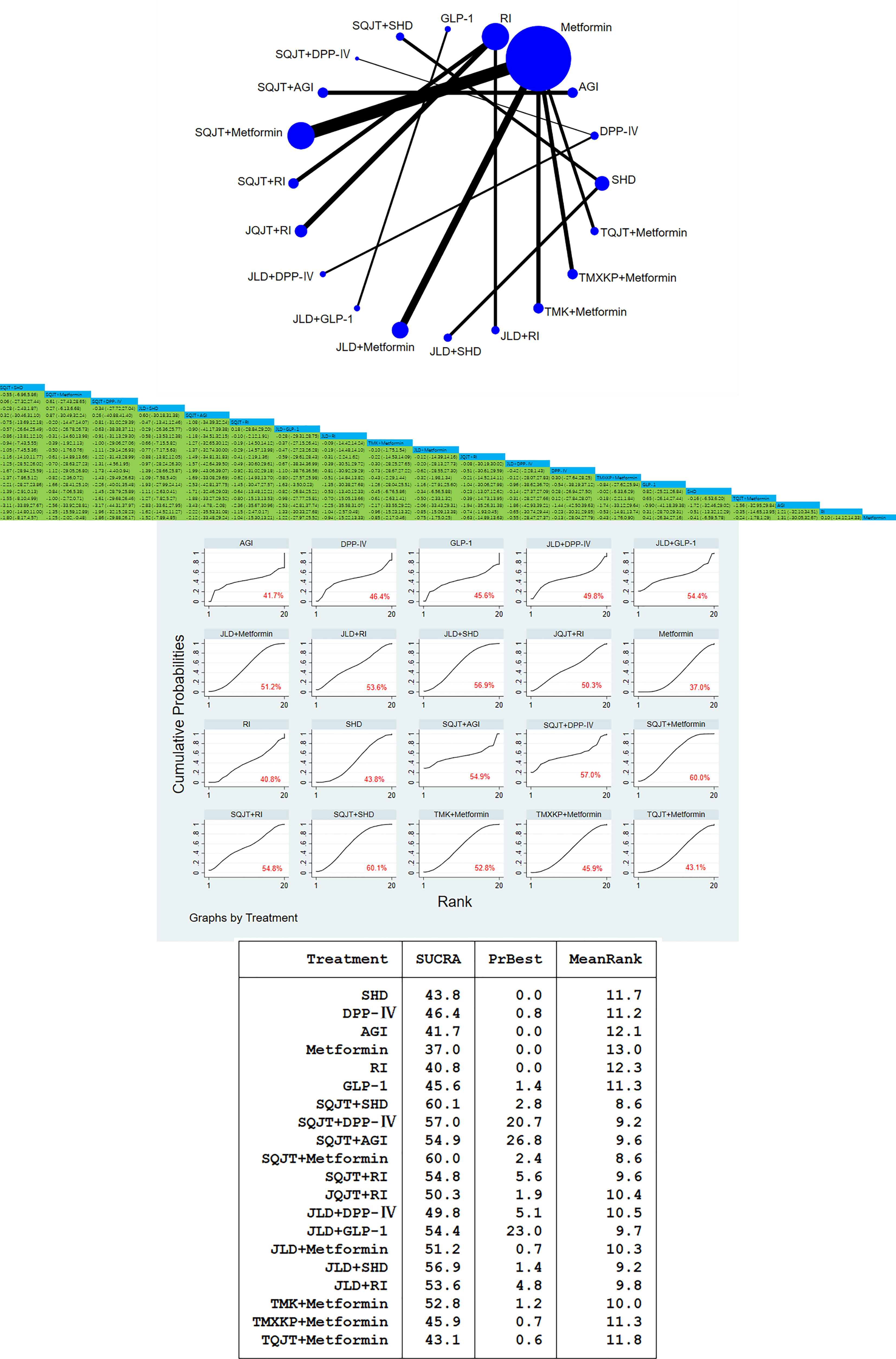
Fifty-seven studies with a total of 5,432 patients included HbA1c outcome measures. In this study, traditional meta-analysis and network meta-analysis of HbA1c showed that: Among the direct comparative studies of TCM combined with CWM and CWM alone, SQJT combined with Metformin and JLD combined with Metformin were the most relevant studies. According to the result of meta-analysis, SQJT combined with Metformin had a significant effect on reducing the HbA1c content compared with Metformin alone, and the effect value was [MD=-1.25, 95%CI=(-2.02, -0.48)]; SQJT combined with AGI had significant effect compared with AGI alone, and the effect value was [MD=-3.43, 95%CI=(-4.78, -2.08)]. There was no significant difference in the comparison of other interventions (Figure 5).
3.3.3.2 Cumulative curves under the area chart sort
According to the area ranking diagram under the cumulative curve of the glycosylated hemoglobin content of the outcome index, SQJT combined with SHD have the most significant effect on reducing the HbA1c, and the therapeutic effects of various intervention measures are ranked as follows: SQJT+SHD > SQJT+Metformin > SQJT+DPP-IV > JLD+SHD > SQJT+AGI > SQJT+RI > JLD+GLP-1 > JLD+RI > TMK+Metformin > JLD+Metformin > JQJT+RI > JLD+DPP-IV > DPP-IV > TMXKP+Metformin > GLP-1 > SHD > TQJT+Metformin > AGI > RI > Metformin, it was proved that TCM combined with CWM had a significant effect on reducing the level of HbA1c compared with CWM alone (Figure 5).
3.3.4 Incidence of adverse reactions
3.3.4.1 Traditional meta-analysis and network meta-analysis and league table
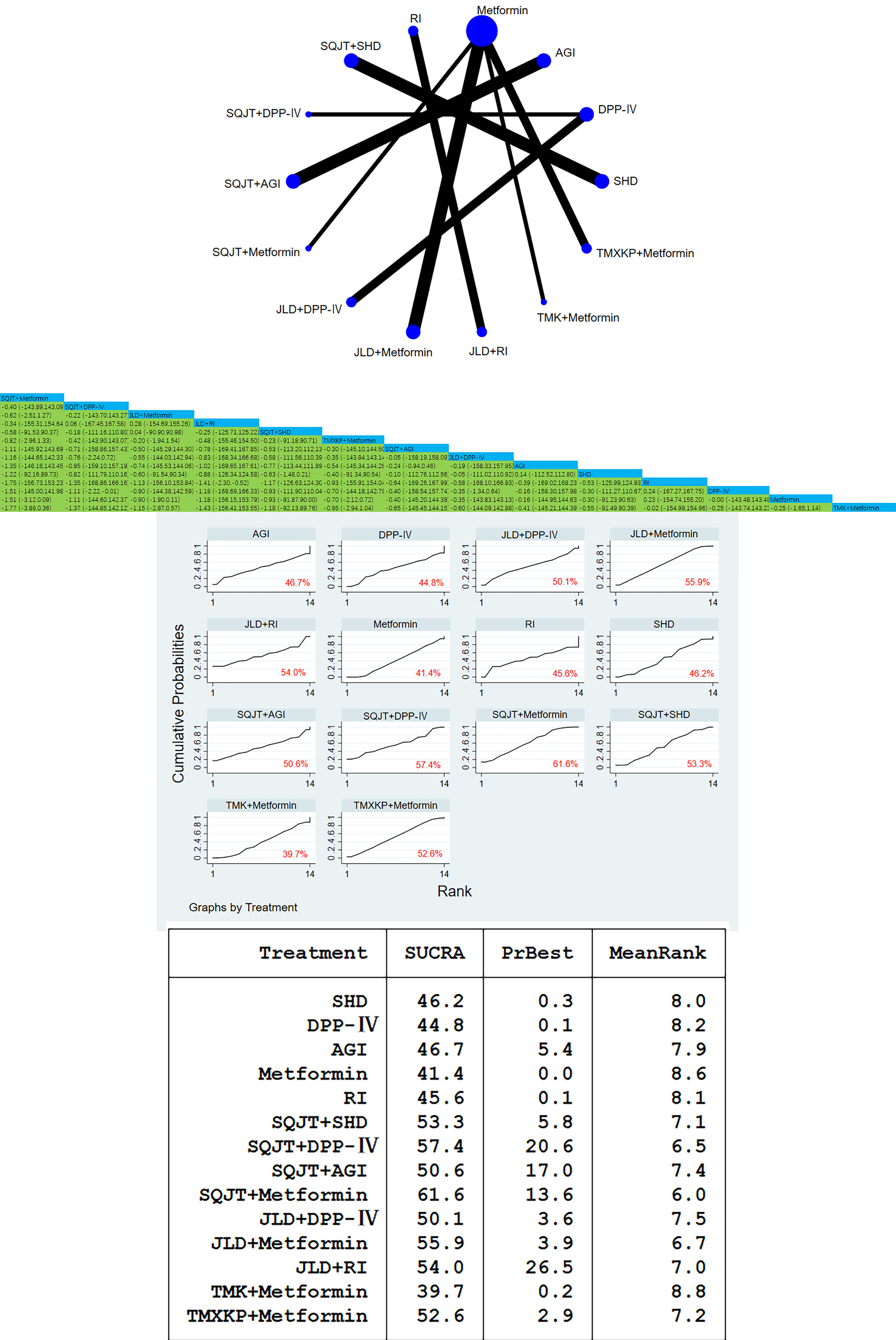
Eighteen RCTs, involving a total of 1867 patients, included the incidence of adverse reactions as an outcome indicator. In this study, traditional meta-analysis and network meta-analysis were performed on the incidence of adverse reactions. According to the result, SQJT combined with DPP-IV had more safety and lower incidence of adverse reactions compared with CWM alone, and the effect value was [OR=-1.11, 95%CI=(-2.22, -0.01)]; Compared with RI alone, JLD combined with RI had better safety, and the effect value was [OR=-1.41, 95%CI=(-2.30, -0.52)], there was no significant difference between other interventions (Figure 6).
3.3.4.2 Cumulative curves under the area chart sort
According to the area ranking graph under the cumulative curve of adverse reaction incidence of outcome indicators, JLD combined with Metformin was the best intervention measure, and the best ranking of various intervention measures was as follows: SQJT+Metformin > SQJT+DPP-IV > JLD+Metformin > JLD+RI > SQJT+SHD > TMXKP+Metformin > SQJT+AGI > JLD+DPP-IV > AGI > SHD > RI > DPP-IV > Metformin > TMK+Metformin (Figure 6).
3.3.5 Clinical efficacy
3.3.5.1 Traditional meta-analysis and network meta-analysis and league table
Thirty-two RCTs, with a total of 3,045 patients, included outcome measures of clinical efficacy. In this study, traditional meta-analysis and network meta-analysis of clinical efficacy were conducted. According to the result, compared with RI alone, JLD combined with RI and SQJT combined with RI showed better clinical efficacy, and the effect values were [OR=1.73, 95%CI= (0.59, 2.87)] and [OR=1.55, 95%CI=(0.72, 2.37)]; SQJT combined with SHD and JLD combined with SHD were more effective than SHD alone, and the effect values were [OR=1.72, 95%CI=(0.86, 2.58)] and [OR=1.25, 95%CI=(0.42, 2.07)], respectively; SQJT combined with AGI were superior to AGI alone, and the effect value was [OR=1.96, 95%CI=(1.22, 2.71)]. The comparison results of other intervention measures were shown in the figure (Figure 7).
3.3.5.2 Cumulative curves under the area chart sort
According to the area ranking diagram under the cumulative curve of clinical efficacy of outcome indicators, JLD combined with RI was the best intervention measure, and the best ranking of various intervention measures was as follows: JLD+RI > SQJT+SHD > SQJT+RI > JLD+Metformin > SQJT+AGI > JLD+GLP-1 > JLD+DPP-IV > SQJT+Metformin > JLD+SHD > JLD+RI > AGI > DPP-IV > GLP-1 > SHD > Metformin > RI (Figure 7).
4 Discussion
According to the results of this traditional meta-analysis and online meta-analysis, SQJT combined with CWM and JLD combined with CWM have more significant effects on reducing FBG, 2hPG, HbA1c, and the incidence of adverse reactions, as well as by enhancing clinical efficacy, compared with CWM alone. JQJT combined with CWM, TMK combined with CWM, and TMXKP combined with CWM were superior to CWM alone in reducing FBG and 2hPG. After a comprehensive analysis, it was found that SQJT combined with CWM had the most comprehensive effect on the clinical treatment of T2DM.
Clinically, CWM has a very significant hypoglycemic effect in the treatment of T2DM; however, the action pathway is relatively simple. Some CWM inevitably causes certain damage to the heart, liver, kidney, stomach, and other organs, as well as common adverse reactions, such as hypoglycemia, gastrointestinal reactions, allergic reactions, liver and kidney damage, cardiovascular damage, headache, and constipation (71). Studies have shown that some CWM treatments have certain adverse reactions to diabetes and diabetes complications, which may lead to the risk of hypoglycemia in elderly patients with diabetes. Repeated hypoglycemia may lead to cognitive decline and even dementia in elderly patients with diabetes (72). Certain medications, such as sulfonylureas and insulin, can increase the risk of severe hypoglycemia. With the gradual introduction of TCM, the application of TCM in the treatment of diabetes is increasingly extensive. TCM and other natural drugs have strong pharmacological activity, with anti-inflammatory, antioxidant, antidiabetic, and other effects (73). Many types of TCM were included in this study, such as salvia, red peony root, and other blood-activating drugs, which have been proven to maintain blood glucose levels and reduce the content of HbA1c (74). Kudzu root, coptis and rhizome can improve glucose uptake and utilization. Moreover, astragalus combined with Pueraria may regulate the AMPK signaling pathway through IL-6, TNF-α, and other targets to affect insulin resistance, glycogen synthesis, gluconeogenesis, and other processes (75). JQJT is a classic prescription for the treatment of thirst disease in “Bei-ji-qian-jin-yao-fang”. Its components include quercetin, kaempferol, luteolin, β-carotene, and β-sitosterol, which can improve the activity of INS-1 cells stimulated by high glucose, as well as downregulate the relative expression of BAX and PDX-1 mRNA and inhibit the oxidative stress of INS-1 cells. Moreover, apoptosis can be reduced, and the insulin secretion of beta cells can be promoted (76). Previous studies have shown that SQJT can increase the activity of superoxide dismutase (SOD) in the pancreatic tissue of rats, and its hypoglycemic effect may be related to the protection of pancreatic β cells and the restoration of insulin sensitivity in rats. This mechanism may be related to the enhancement of protein kinase B phosphorylation and the upregulation of glucose transporter 2 expression. It plays a hypoglycemic role by promoting glucose uptake and glycogen synthesis (77). Previous studies have found that SQJT can affect vascular factors and play a role in the treatment of T2DM. Through the coordination and mutual influence of the MAPK pathway and VEGF signaling pathway, vascular endothelial growth factor (VEGFA) affects the MAPK signaling pathway by binding with the receptor KDR, thus playing a role in the treatment of T2DM (78). JLD can improve glucose tolerance and reduce blood sugar by regulating the expression of genes and proteins related to the FGF21/AMPK pathway. Studies have shown that the regulation of glucose and lipid metabolism by JLD has a certain correlation with FGF21, which can activate FGF21 and improve the accumulation of lipids in the liver. Furthermore, JLD can further enhance the positive role of FGF21 in regulating glucose and lipid metabolism and in preserving energy homeostasis by activating the FGFR1/β-Klotho receptor complex (79). Schisandra, Mai Dong, and other drugs in TMXKP can enhance insulin sensitivity to a certain extent, but their regulatory effect on blood sugar is limited. The trivalent chromium in TMXKP has a significant effect on reducing blood glucose, inhibiting tyrosine phosphatase, and activating insulin receptor kinase, thus phosphorylating the insulin receptor, reducing insulin resistance and increasing insulin sensitivity. Therefore, it lowers blood sugar levels (80). Moreover, TMK can reduce insulin resistance and improve insulin sensitivity by inhibiting platelet aggregation and thrombin synthesis, thus playing a synergistic role in lowering blood sugar, regulating blood lipids, and improving microcirculation disorders (81). TQJT has a certain effect on lowering blood glucose levels. Gene chip technology has been applied in clinical studies to explore the mechanism of action of TQJT, and the results showed that TQJT can effectively reduce the FBG and triglyceride levels of KKAy mice and improve insulin sensitivity, which may be related to the improvement of glucose utilization via the MAPK pathway and GluT-4 upregulation (82). The combination of TCM and CWM is an increasingly widely used diagnosis and treatment method. TCM treatment can improve symptoms and improve clinical efficacy. The combination of TCM with CWM can reduce the dosage of CWM and reduce the clinical side effects caused by CWM. Furthermore, it can delay or reverse the early chronic complications of diabetes and improve quality of life. The combination of TCM and CWM uses modern science and technology, and TCM and CWM complement each other to develop a brand new medical system. Moreover, the combination of disease differentiation and dialysis can better guide the clinical treatment of T2DM.
5 Advantages and limitations
There have been few indirect clinical studies on the treatment of T2DM by different TCMs combined with CWM; therefore, the differences in the therapeutic effects of different TCMs combined with CWM are not clear. In this study, network meta-analysis was used to clearly compare the efficacy of different TCMs combined with CWM to guide clinical treatment and provide certain suggestions and aid. However, there were still several shortcomings in this study. (1) The literature included in this study belongs to TCM; inevitably, most of the studies were domestic studies, with few relevant foreign studies. (2) As limited by statistical methods, some of the relevant methods that were included in the study were not optimal, and the quality was not good. (3) The intervention time was not long enough for the included studies, the efficacy in the future for a long period of time was not clear. (4) The sample size that was included in the study was not large enough. When considering the above mentioned aspects, we will focus on large-sample, multicenter, double-blind, and other high-quality clinical studies in the future to improve our research conclusions, with a view to providing more authoritative and instructive suggestions for the clinical treatment of T2DM.
6 Conclusion
Through the combination of this traditional meta-analysis and network meta-analysis, it was concluded that different TCMs combined with CWM had more significant clinical efficacy and safety in the treatment of T2DM compared with CWM alone, among which SQJT combined with CWM may be the best intervention measure, SQJT combined with SHD and Metformin is the best clinical method to reduce blood glucose content, and JLD combined with RI has the best clinical effect. The order of the best possible intervention measures for different outcome indicators was also obtained. The aim of the study outcomes is to provide some suggestions and help for clinical applications.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material. Further inquiries can be directed to the corresponding author.
Author contributions
KM and LZ were involved in study design, data collection, analysis, and manuscript revision. KM and ML contribute to data collection, data interpretation and manuscript revision. CT and CY participated in data analysis, data interpretation, manuscript drafting and revision, YZ and JZ were responsible for the concise and unobstructed language expression of the article and graphic production. KM is the guarantor of this work, and ML is the corresponding author of this paper, providing valuable suggestions for the overall framework and content construction of this paper. All authors contributed to the article and approved the submitted version.
Funding
Funded by the Scientific and technological innovation project of China Academy of Chinese Medical Sciences, CI2021A01606, Beijing Natural Science Foundation and Beijing-Tianjin-Hebei Project (J200019), the National Natural Science Foundation of China (81973837).
Acknowledgments
Thanks to all the authors involved in this study for their contributions and to the advisors for their expert advice.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Zhu M, Wu J, Gao J. Exosomes for diabetes syndrome: ongoing applications and perspective. Biomater Sci (2022) 10(9):2154–71. doi: 10.1039/D2BM00161F
2. Bielka W, Przezak A, Pawlik A. The role of the gut microbiota in the pathogenesis of diabetes. Int J Mol Sci (2022) 23(1):480. doi: 10.3390/ijms23010480
3. Xu L, Li Y, Dai Y, Peng J. Natural products for the treatment of type 2 diabetes mellitus: pharmacology and mechanisms. Pharmacol Res (2018) 130:451–65. doi: 10.1016/j.phrs.2018.01.015
4. Tsapas A, Avgerinos I, Karagiannis T, Malandris K, Manolopoulos A, Andreadis P, et al. Comparative effectiveness of glucose-lowering drugs for type 2 diabetes: a systematic review and network meta-analysis. Ann Intern Med (2020) 173(4):278–86. doi: 10.7326/M20-0864
5. Zheng Y, Ding Q, Wei Y, Gou X, Tian J, Min L, et al. Effect of traditional Chinese medicine on gut microbiota in adults with type 2 diabetes: a systematic review and meta-analysis. Phytomed (2021) 88:153455. doi: 10.1016/j.phymed.2020.153455
6. Wang J, Ma Q, Li Y, Li P, Wang M, Wang T, et al. Research progress on traditional Chinese medicine syndromes of diabetes mellitus. BioMed Pharmacother (2020) 121:109565. doi: 10.1016/j.biopha.2019.109565
7. Shao W, Shi YQ, Liang J, Song C. Clinical study of shenqi jiangtang granules combined with miglitol in treatment of type 2 diabetes mellitus. Drugs Clinic (2022) 37(06):1324–8.
8. Wang ZZ, Yang B, Li GQ, Wang J. Efficacy and safety analysis of voglibose dispersing tablets combined with shenqi jiangtang granules in the treatment of type 2 diabetes mellitus. China Med Herald (2013) 10(27):14–6.
9. Liu YF. Clinical observation of shenqi jiangtang granules combined with conventional therapy on senile type 2 diabetes mellitus. New Chin Med (2016) 48(05):121–3. doi: 10.13457/j.cnki.jncm.2016.05.046
10. Xia QB. Curative effect evaluation of shenqi jiangtang granules combined with acarbose in the treatment of senile type 2 diabetes mellitus with deficiency of qi and yin. China Pharm (2016) 25(22):48–50.
11. Guan LH. Observation on the effect of shenqi jiangtang granules + glimepiide in the treatment of diabetic outpatients and its influence on blood glucose level and clinical symptoms. Chin J Clin Rational Drug Use (2018) 11(29):9–10 + 17. doi: 10.15887/j.cnki.13-1389/r.2018.29.005
12. Yuan Y. Curative effect and side effects of shenqi jiangtang granules combined with galiquantel tablets in the treatment of type 2 diabetes mellitus. Capital Food Med (2017) 24(16):77–8.
13. Zhang SY. Effects of shenqi jiangtang granules combined with glimepiide on FPG and 2hPG levels and quality of life in outpatients with type 2 diabetes. Capital Food Med (2018) 25(19):37.
14. Guo SH, Lu JL. Efficacy and safety analysis of shenqi jiangtang granules combined with glimepireide in the treatment of diabetic outpatients. Liaoning J Traditional Chin Med (2016) 43(11):2323–5. doi: 10.13192/j.issn.1000-1719.2016.11.032
15. Zhang W. Clinical observation of shenqi jiangtang granules combined with glimepiride in treating diabetes mellitus. Doctor (2017) 2(Z2):148 + 151. doi: 10.19604/j.cnki.dys.2017.z2.084
16. Gao FL. Clinical observation on the effect of dipeptidyl peptidase inhibitor combined with shenqi jiangtang granules in the treatment of type 2 diabetes patients. Capital Food Med (2020) 27(08):75. doi: 10.3969/j.issn.1005-8257.2020.08.062
17. Liu YJ. Effects of dipeptidyl peptidase-4 inhibitors combined with shenqi jiangtang granules on the changes of FPG and 2hPG levels in type 2 diabetes patients. J North Pharm (2018) 15(10):119–20.
18. Ren QW. Clinical observation of saxagliptin combined with shenqi jiangtang granules in treatment of 46 cases of type 2 diabetes mellitus. Chin J Ethnomed Ethnopharm (2019) 28(02):105–106 + 120.
19. Liu HP, Cheng LX, Guo CJ. Efficacy evaluation of metformin combined with shenqi jiangtang granules in the treatment of newly diagnosed type 2 diabetes mellitus. China Modern Doctor (2017) 55(32):33–35 + 39.
20. Cai CJ. Shenqi jiangtang granules combined with metformin in treatment of 38 cases of type 2 diabetes mellitus. Chin Med Modern Distance Educ China (2014) 12(23):58–9. doi: 10.3969/j.issn.1672-2779.2014.23.037
21. Wang YJ, Lei Y. Curative effect of shenqi jiangtang granules combined with metformin tablets in treatment of type II obese diabetes mellitus. Clin Res Pract (2016) 1(27):124–5. doi: 10.19347/j.cnki.2096-1413.2016.27.062
22. Liu SY, Peng QJ. Clinical observation of shenqi jiangtang granules combined with conventional therapy on senile type 2 diabetes mellitus. China Pract Med (2020) 15(33):116–8. doi: 10.14163/j.cnki.11-5547/r.2020.33.052
23. Yang HJ, Zhang TT, Shi DM, Xu HF. Effects of shenqi jiangtang granules combined with glimepiide and metformin on blood glucose level, islet cell function and endothelial factors in diabetic patients. Chin J Health Lab Technol (2019) 29(22):2744–6.
24. Liu MY, Pang QB, Song SH, Zhuang Q, Ma GQ. Clinical efficacy of shenqi jiangtang granules combined with metformin hydrochloride in the treatment of type 2 diabetes mellitus. Electronic J Pract Gynecol Endocrinol (2017) 4(35):162 + 164. doi: 10.16484/j.cnki.issn2095-8803.2017.35.114
25. Sun JR. Observation of curative effect of shenqi jiangtang granule combined with conventional Western medicine therapy on patients with type 2 diabetes. J Pract Diabetol (2020) 16(05):100–1.
26. Sui FL. Observation on effect of shenqi jiangtang granule combined with Western medicine in treatment of type 2 diabetes patients. Pract Clin J Integrated Traditional Chin Western Med (2019) 19(07):69–70. doi: 10.13638/j.issn.1671-4040.2019.07.034
27. Chen SY. Clinical study of shenqi jiangtang granule combined with Western medicine in treating 52 cases of type 2 diabetes mellitus. China Health Standard Manage (2018) 9(16):105–7.
28. Fan YL, Huang XJ, Gao JN, Chen HW. Clinical observation of shenqi jiangtang granules in adjuvant treatment of type 2 diabetes mellitus. China Med Equip (2014) 11(S1):220–1.
29. Liu GH, Kang Y. Curative effect and prognosis analysis of shenqi jiangtang granule adjuvant therapy in elderly patients with type 2 diabetes mellitus. J Hunan Normal Univ (Med Sci) (2018) 15(02):52–4. doi: 10.3969/j.issn.1673-016X.2018.02.015
30. Zhang L, Wang LL, Li MD, Wang YY. Clinical study on shenqi jiangtang granules adjuvant treatment of type 2 diabetes mellitus with deficiency of qi and yin. New Chin Med (2019) 51(04):166–8. doi: 10.13457/j.cnki.jncm.2019.04.052
31. Li SJ. Curative effect of degu asparton insulin combined with shenqi jiangtang granules in the treatment of type 2 diabetes mellitus. China Pract Med (2022) 17(08):164–6. doi: 10.14163/j.cnki.11-5547/r.2022.08.060
32. Du Y. Effects of diteinsulin combined with shenqi jiangtang granules on blood glucose and blood lipid in patients with type 2 diabetes mellitus. Chin J Modern Drug Appl (2022) 16(01):218–20. doi: 10.14164/j.cnki.cn11-5581/r.2022.01.081
33. Li XL, Ma J, Wang YP. Effects of shenqi jiangtang granules on serum glucagon-like peptide-1 and c-reactive protein in patients with type 2 diabetes mellitus. Northwest Pharm J (2021) 36(01):101–4.
34. Lv G. Clinical observation of shenqi jiangtang granules combined with insulin in the treatment of type 2 diabetes mellitus. Diabetes New World (2017) 20(21):61–2. doi: 10.16658/j.cnki.1672-4062.2017.21.061
35. Gao MK, Zhu ZZ. Effect analysis of jinqi jiangtang tablets combined with metformin in the treatment of type 2 diabetes mellitus. J Shanxi Health Vocational Coll (2021) 31(06):26–7.
36. Li T, Tan LX. Clinical effect of jinqi jiangtang tablets combined with metformin in the treatment of type 2 diabetes mellitus. Diabetes New World (2018) 21(14):69–70. doi: 10.16658/j.cnki.1672-4062.2018.14.069
37. Li T. Effect of jinqi jiangtang tablet combined with Western medicine on type 2 diabetes mellitus with deficiency of qi and yin. Shaanxi J Traditional Chin Med (2012) 33(04):416–7.
38. Yao QC. Clinical study of jinqi jiangtang tablets combined with metformin in the treatment of type 2 diabetes mellitus. Drugs Clinic (2014) 29(07):786–90.
39. Li XM. Clinical observation of jinqi jiangtang tablets combined with metformin in control of type 2 diabetes mellitus. Inner Mongolia J Traditional Chin Med (2017) 36(Z1):109–10. doi: 10.16040/j.cnki.cn15-1101.2017.z1.086
40. Hu XB. Efficacy and safety of sitagliptin combined with zinlida granules in the treatment of senile type 2 diabetes mellitus. Chin J Geriatric Care (2022) 20(01):55–7.
41. Wu J. Effect of jinlida granule combined with sitagliptin on blood glucose control in patients with type 2 diabetes mellitus. Clin Res (2021) 29(02):124–5.
42. Tang YG, Wang J, Yang JY. Effects of sitagliptin phosphate combined with zinlida granule on blood glucose and serum inflammatory factors in type II diabetes mellitus. Inner Mongolia J Traditional Chin Med (2017) 36(Z1):108–9.
43. Zhou XH, Liu SY, Lin YJ. Clinical study on the treatment of type 2 diabetes mellitus by jinlida granule combined with dulatospeptide. Drugs Clinic (2020) 35(08):1584–7.
44. Zhang SZ, Kong R, Miao HY, Wang ZX. Clinical study of jinlida granule combined with liraglutide in treatment of type 2 diabetes mellitus. Drugs Clinic (2018) 33(03):668–71.
45. Zhou L. Clinical observation of jinlida granule combined with metformin in treatment of type 2 diabetes mellitus. J Pract Diabetol (2020) 16(03):84–5.
46. Li HQ, Song RH, Liu XM. Clinical observation of jinlida granule combined with metformin on insulin resistance of type 2 diabetes mellitus with both qi and yin deficiency. Shenzhen J Integrated Traditional Chin Western Med (2017) 27(01):21–3. doi: 10.16458/j.cnki.1007-0893.2017.01.011
47. Tang YG, Wang J, Yang JX. Effect of jinlida granules on improving islet function and glucose lipid metabolism in type 2 diabetes mellitus. Inner Mongolia J Traditional Chin Med (2017) 36(15):56–7. doi: 10.16040/j.cnki.cn15-1101.2017.15.048
48. Wu AH, Liu LQ, Li CY. Effect of jinlida granules on function of pancreatic β cells in type 2 diabetes mellitus. Clin J Chin Med (2019) 11(26):118–20.
49. Xing XY, Zhang W. Effect of jinlida granules on improving islet function and glucose lipid metabolism in patients with type 2 diabetes mellitus. Chin J Clin Rational Drug Use (2021) 14(14):76–7. doi: 10.15887/j.cnki.13-1389/r.2021.14.032
50. Wang GZ. Clinical study of jinlida granule combined with metformin in the treatment of diabetes mellitus. Biped Health (2018) 27(15):109–10. doi: 10.19589/j.cnki.issn1004-6569.2018.15.109
51. Fu YF, Zhang SL, Tan LM. Clinical observation of jinlida granule combined with liraglutide and metformin in treatment of type 2 diabetes mellitus. China Pharm (2019) 28(08):53–5.
52. Ma QM, Wang SL, Feng Y. Zinlida combined with gewazhi improved the islet function in 40 patients with type 2 diabetes. Chin Med Modern Distance Educ China (2014) 12(11):48–9.
53. Xiao W. Effect of gliclazide combined with zinlida granules on blood glucose control and quality of life in elderly patients with type 2 diabetes mellitus. J Pract Diabetol (2019) 15(02):29–30.
54. Liu H. Clinical study of zinlida granule combined with glipizide in treatment of type 2 diabetes mellitus. Drugs Clinic (2018) 33(06):1490–3.
55. Luo LQ. Comparative analysis of the efficacy of jinlida granule combined with glimepiride and glimepiride alone in the treatment of diabetes mellitus. Psychol Month (2018) 2018(06):63–4. doi: 10.19738/j.cnki.psy.2018.06.038
56. Zhu W, Xing XY. Therapeutic effect of jinlida granule on patients with type 2 diabetes. Chin J Clin Rational Drug Use (2021) 14(11):101–3. doi: 10.15887/j.cnki.13-1389/r.2021.11.043
57. Huang JC, Ding SQ, Wang MY. To investigate the clinical efficacy and safety of jinlida granule combined with insulin in the treatment of type 2 diabetes based on adaptive immunity. World J Integrated Traditional Western Med (2020) 15(11):2062–6. doi: 10.13935/j.cnki.sjzx.201120
58. Luo XY. Clinical study of jinlida granule combined with hypoglycemic drugs in treatment of type 2 diabetes patients. Diabetes New World (2018) 21(16):59–60. doi: 10.16658/j.cnki.1672-4062.2018.16.059
59. Lin Y, Gao HY, Zhou F, Guo YJ, Song SX. Effects of metformin tablets combined with tangmaikang granules on serum levels of IL-6, TNF-α, CRP and APN in patients with type 2 diabetes mellitus. Prog Modern Biomed (2017) 17(30):5883–6. doi: 10.13241/j.cnki.pmb.2017.30.019
60. Hu ML, Deng HY, Fu J, Liao LY. Effect of tangmaikang granules on blood glucose level in patients with type 2 diabetes. Chin J Exp Traditional Med Formulae (2015) 21(14):173–6. doi: 10.13422/j.cnki.syfjx.2015140173
61. Li H, Liu H. Therapeutic effect of tangmaikang granules combined with metformin in the treatment of type 2 diabetes mellitus. Inf Traditional Chin Med (2019) 36(01):80–3. doi: 10.19656/j.cnki.1002-2406.190020
62. Du W, Guo JZ, Jin J. Curative effect of tangmaikang granules combined with metformin in treatment of newly diagnosed type 2 diabetes mellitus. J Ningxia Med Univ (2010) 32(01):93–4. doi: 10.16050/j.cnki.issn1674-6309.2010.01.038
63. Lou DJ, Zhu QQ, Ye F, Dong HY, Huang DH, Si XW. Effect of tianmai xiaoke tablet on insulin resistance and β cell function improvement in newly diagnosed type 2 diabetes patients. Chin J Traditional Med Sci Technol (2016) 23(04):397–9.
64. Shao Y, Han XL Ding HY. Tianmai xiaoke tablet combined with metformin in treatment of 40 cases of incipient type 2 diabetes mellitus. J Med Theory Pract (2017) 30(03):355–7. doi: 10.19381/j.issn.1001-7585.2017.03.022
65. Huang FL. Clinical observation of tianmai xiaoke tablet combined with metformin in the treatment of newly diagnosed type 2 diabetes patients. Ningxia Med J (2016) 38(09):818–20. doi: 10.13621/j.1001-5949.2016.09.0818
66. Yu WR. Clinical observation of tianmai xiaoke tablet combined with metformin in the treatment of newly diagnosed type 2 diabetes patients and analysis of TCM symptoms. World Latest Med Inf (2019) 19(13):124 + 127. doi: 10.19613/j.cnki.1671-3141.2019.13.086
67. Qin RJ. Therapeutic effect of tianmai xiaoke tablet on patients with type 2 diabetes mellitus and its influence on blood glucose and insulin sensitivity. Diabetes New World (2016) 19(18):26–8. doi: 10.16658/j.cnki.1672-4062.2016.18.026
68. Yao L. Clinical study of tianqi jiangtang capsule combined with metformin in the treatment of type 2 diabetes mellitus with deficiency of qi and yin.
69. Cao Y, Wang HY, Xu C. Effects of tianqi jiangtang capsule combined with metformin on interleukin-6, tumor necrosis factor α and c-reactive protein in patients with type 2 diabetes. Chin J Diabetes (2015) 23(08):739–41.
70. Lian FM, Li Y, Sun XF, Xiang HD, Xiao XH, Tong XL. A randomized, double-blind, parallel-controlled, multicenter clinical study of tianqi jiangtang capsule combined with metformin in the treatment of type 2 diabetes mellitus. Chin J Diabetes (2011) 19(08):600–2.
71. Yang LY, Hu QY. Research progress of traditional Chinese medicine in treatment of type 2 diabetes mellitus. Chin J Integrated Traditional Western Med (2020) 40(08):1007–11.
72. Peng YJ, Liu XM, Meng ZZ, Zhan HX, Piao SH, Rong XL, et al. Real world study on effectiveness of zhenzhu tiaozhi capsule combined with conventional Western medicine in treating 35 elderly patients with type 2 diabetes. J Traditional Chin Med (2022) 63(01):43–9. doi: 10.13288/j.11-2166/r.2022.01.009
73. Bai L, Li X, He L, Zheng Y, Lu H, Li J, et al. Antidiabetic potential of flavonoids from traditional Chinese medicine: a review. Am J Chin Med (2019) 47(5):933–57. doi: 10.1142/S0192415X19500496
74. Jiang L, Zhang Y, Zhang H, Chen Y, Huang W, Xiao Y, et al. Comparative efficacy of 6 traditional Chinese patent medicines combined with lifestyle modification in patients with prediabetes: a network meta-analysis. Diabetes Res Clin Pract (2022) 188:109878. doi: 10.1016/j.diabres.2022.109878
75. Xie WY, Zhang C, Xin JY, Li WH, Zhang TJ. A systematic review and meta-analysis of the efficacy and safety of tangmaikang granules in the treatment of diabetic peripheral neuropathy. China J Chin Mater Med (2023) 48(02):542–54. doi: 10.19540/j.cnki.cjcmm.20220926.502
76. Huang MY, Wang ZZ, Long JL, Yang X, Zhang Y, Yan D. To investigate the protective mechanism of jinqi jiangtang tablets against pancreatic β cells based on network pharmacology and molecular docking techniques. China J Chin Mater Med (2021) 46(20):5341–50. doi: 10.19540/j.cnki.cjcmm.20210713.402
77. Hong JN, Cheng GL, Huang ZW, Huang WJ, Wang LQ, Li B, et al. Research progress of shenqi jiangtang granules on the prevention and treatment of disorders of glycolipid metabolism. Chin Traditional Herbal Drugs (2022) 53(17):5544–52.
78. Zhang J, Li BB, Huang MY, Tan LP, Xiao X, Zhang GM, et al. Study on the mechanism of shenqi jiangtang granules in the treatment of type 2 diabetes mellitus based on network pharmacology. Chin Traditional Herbal Drugs (2020) 51(19):4873–83.
79. Liu Y, Li CR, Chang CP, Gao HL. Effects of jinlida granule on metabolic disorder and FGF21/AMPK signaling pathway in obese mice induced by high fat diet. Chin Traditional Herbal Drugs (2021) 52(05):1351–9.
80. Xie WQ, Wang YL, Diao JH. Therapeutic effect of tianmai xiaoke tablet on insulin resistant type 2 diabetes mellitus. J Henan Med Coll (2019) 31(06):761–4. doi: 10.3969/j.issn.1008-9276.2019.06.018
81. Yu L, Yuan Q, Shao ZG. Therapeutic effect of tangmaikang granules on type 2 diabetes mellitus and its effect on endotheliin-1. Chin Traditional Patent Med (2014), (11):2440–2.
Keywords: type 2 diabetes, traditional Chinese medicine, conventional western medicine, network meta-analysis, meta-analysis
Citation: Ma K, Zhou L, Zhang Y, Zhao J, Yao C, Tian C and Li M (2023) Efficacy and safety of traditional Chinese medicines combined with conventional Western medicines in the treatment of type 2 diabetes mellitus: a network meta-analysis of randomized controlled trials. Front. Endocrinol. 14:1134297. doi: 10.3389/fendo.2023.1134297
Received: 30 December 2022; Accepted: 17 April 2023;
Published: 08 May 2023.
Edited by:
Åke Sjöholm, Gävle Hospital, SwedenReviewed by:
Anu Grover, Ipca Laboratories, IndiaDe Jin, Hangzhou Hospital of Traditional Chinese Medicine, China
Copyright © 2023 Ma, Zhou, Zhang, Zhao, Yao, Tian and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Min Li, bGltaW4tNzIxMTRAMTYzLmNvbQ==
 Kaile Ma
Kaile Ma Lijuan Zhou1
Lijuan Zhou1 Chensi Yao
Chensi Yao Min Li
Min Li