
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Endocrinol., 13 June 2023
Sec. Reproduction
Volume 14 - 2023 | https://doi.org/10.3389/fendo.2023.1131555
This article is part of the Research TopicMetabolic Factors in Erectile DysfunctionView all 14 articles
Background: The global prevalence of erectile dysfunction among patients with diabetes is high. It is the most underestimated problem but has a great physical, psychological, and social impact on the individual with the disease, family, and society in general. Thus, this study aimed to assess the magnitude of erectile dysfunction and associated factors among patients with diabetes attending follow-up at a public hospital, Harar, Eastern Ethiopia.
Methods: Facility-based cross-sectional study was conducted on selected 210 adult male patients with diabetes attending follow-up at a public hospital, Harar, Eastern Ethiopia, from 1 February to 30 March 2020. Simple random sampling was used to select study participants. A pre-tested interviewer-administered structured questionnaire was used to collect the data. The data were entered to EpiData version 3.1 and exported to SPSS version 20 for analysis. Bivariate and multivariable binary logistic regression were carried out, and a P-value of <0.05 was taken as statistically significant.
Result: A total of 210 adult male patients with diabetes participated in the study. The overall magnitude of erectile dysfunction was 83.8%, with 26.7% suffering from mild, 37.5% mild to moderate, 29% moderate, and 6.8% severe erectile dysfunctions. Age 46–59 years [adjusted odds ratio (AOR): 2.560; 95% confidence interval (CI) (1.73, 6.53)], age ≥ 60 years [AOR: 2.9; 95% CI (1.48, 5.67)], and poor glycemic control [AOR: 2.140; 95% CI (1.9, 7.44)] were significantly associated with erectile dysfunction among patients with diabetes.
Conclusion: The present study revealed a high magnitude of erectile dysfunction among population with diabetes. The age categories of 46–59 and ≥60 and having poor glycemic control were the only variables significantly associated with erectile dysfunction. Thus, routine screening and management for erectile dysfunction in patients with diabetes should be part of routine medical care particularly for adult male patients and those with poor glycemic control.
Diabetes mellitus (DM) is one of the most common and serious non-communicable disease affecting the lives and wellbeing of individuals with the disease, families, and societies at large. In 2019, approximately 463 million (9.3%) people were living with diabetes, and it was estimated that, by 2045, the prevalence will rise to 10.9% (700 million) (1). Its complications have major and long-lasting impacts at different levels (2). One of the most common and underestimated complications among DM is erectile dysfunction (ED) (3). According to the National Institutes of Health Consensus Development Conference, ED is defined as the persistent inability to achieve or maintain an erection sufficient for satisfactory sexual performance (4). ED is two to three times more common among individuals with DM than those without DM (5, 6).
The global prevalence of ED was 3%–76.5% (7). There is a great variation in the prevalence of ED among male patients with DM. On the basis of different epidemiological data, its prevalence was 52% (3). Different studies were carried out in different parts of the world, where the prevalence of ED among patients with DM ranges from 6.8% in Ethiopia to 95% in South Africa (8–21). In Africa, its general prevalence among patients with DM was 71.45% (22). Different studies on the prevalence of ED among patients with DM in some parts Ethiopia were carried out, and the prevalence was from 6.8% to 85.5% (8, 11, 19, 21, 23–25).
Although the number of people living with diabetes is rising in Ethiopia, there are only few studies on the complications of DM particularly ED. ED has a significant impact on the individual both physically and psychologically. It can also impair the quality of life of the patients, as well as their partners and families in general (5, 26). Factors including depression, older age, low educational status, poor quality of life, lack of regular physical activity, longer duration of DM, history of cardiovascular disease, cigarette smoking, hypercholesterolemia, poor glycemic control, obesity, taking beta blockers, and comorbidity were stated as the determinant factors for ED in patients with DM in different studies (8, 9, 11, 13, 16–19, 21, 23–25, 27).
ED is a treatable condition. If effective care and management including lifestyle modification, psychosexual therapy, and pharmacotherapy is applied, then it can be cured for up to 95% of cases (28). However, talking about sexual practice and experience is a very sensitive issue in Ethiopia where it is considered as a shameful act. This makes the diagnosis and treatment of ED difficult. The poor culture of openly discussing the sexual health problem among the community may mask the real magnitude of the problem in the population with diabetes. No study on ED in the eastern part of the country was carried out, and knowing its current magnitude and determinant factors may be important for early detection, managing the problem, and improving the quality of life of the patients. Thus this study aimed to assess the magnitude of ED and associated factors among patients with diabetes attending follow-up at a public hospital, Harar, Eastern Ethiopia.
A facility-based cross-sectional study was conducted at HiwotFana Comprehensive Specialized Hospital (HFCSH) from 1 February to 30 March 2020. The hospital is found in Harar city, Harari region, which is found at a distance of 526 km southeast of the capital city, Addis Ababa. HFCSH is a teaching hospital with a catchment of 5.2 million populations. It has a total of 185 inpatient beds distributed among four major departments.
All adult male patients with diabetes on follow-up at HFCSH during the study period were the source population, and male patients with diabetes who were on follow-up clinic during the study period, who are ≥ 18 years of age, and who are willing to participate in the study were included in the study. However, patients who were critically ill, have serious mental illness, had paraplegia from any cause, had past lower urinary tract and prostate surgery, and were not sexually active not because of ED for the previous 6 months prior to the study were excluded from the study.
The sample size was determined using the single population estimation formula by considering margin of error of 5%, confidence level of 95%, and the proportion of ED among patients with DM of 85.5% (24). The calculated sample size was 191, and, by adding 10% non-response rate, the final sample size became 210. To select the study participants, the number of male patients with diabetes expected to have follow-up during the study period in the follow-up clinic was taken from follow-up registration book; then, a systematic random sampling method was used to select study participants.
The data were collected by using an interviewer-administered structured questionnaire. The questionnaire was first prepared in English and then translated to Afan Oromo and Amharic languages and then translated back to English by language experts to check for consistency. The questionnaire was taken from previous similar studies in Ethiopia and from the abridged five-item version of the International Index of Erectile Function (IIEF-5) (29). The instrument produced high sensitivity and specificity, 92.2 and 92.1%, respectively. It has a total of five questions scored out of 25. Accordingly, individuals who scored 1–21 were reported as having ED. While those who scored 22–25 were reported as not having ED. Those who scored 1–7, 8–11, 12–16, and 17–21 out of 25 points were classified as having severe ED, moderate ED, mild to moderate ED, and mild ED, respectively (29). Four medical intern students collected the data.
The quality of data was assured by proper designing of the questionnaire and pre-testing on 10% of the total sample size before 1 week of the actual data collection, and amendments were made based on the information obtained. One-day training was given to the data collectors and supervisors by the principal investigator. During data collection, each questionnaire was reviewed for completeness and consistency by supervisor, and all the necessary feedback was given to the data collectors immediately.
The collected data were first checked for its completeness, cleaned and entered into EpiData version 3.1, and then exported to SPSS version 20 for analysis. Descriptive statistics such as frequency, percentage, mean, and standard deviation (SD) were computed. Bivariate binary logistic regression analysis was carried out to determine the association between each independent variable and dependent variable. Variables with p < 0.2 in bivariate analysis were entered for multiple logistic regressions. Finally, binary logistic regression was carried out, and a P-value of <0.05 was used to declare the statistical significance. To measure the strength of association, adjusted odds ratio (AOR) with their corresponding 95% confidence interval (CI) was used. The fitness of the model was checked using Hosmer and Lemeshow test, and multicollinearity was checked by using variance inflation factor of <10 and tolerance of >0.2.
A total of 210 adult male patients with diabetes participated in the study with a 100% response rate. The mean age of the study participants was 54.53 (± 13.73 SD) with a majority (79; 37.6%) of the study participants in the age group between 46 and 59 years. From the total participants, a majority (197; 93.8%) of them were married. Regarding their educational status, 86 (41%) had elementary education and 80 (40.5%) were government employees. Almost two-thirds (142; 67.6%) of the respondents, had an average monthly income of 1,501–3,000 Ethiopian birr (Table 1).
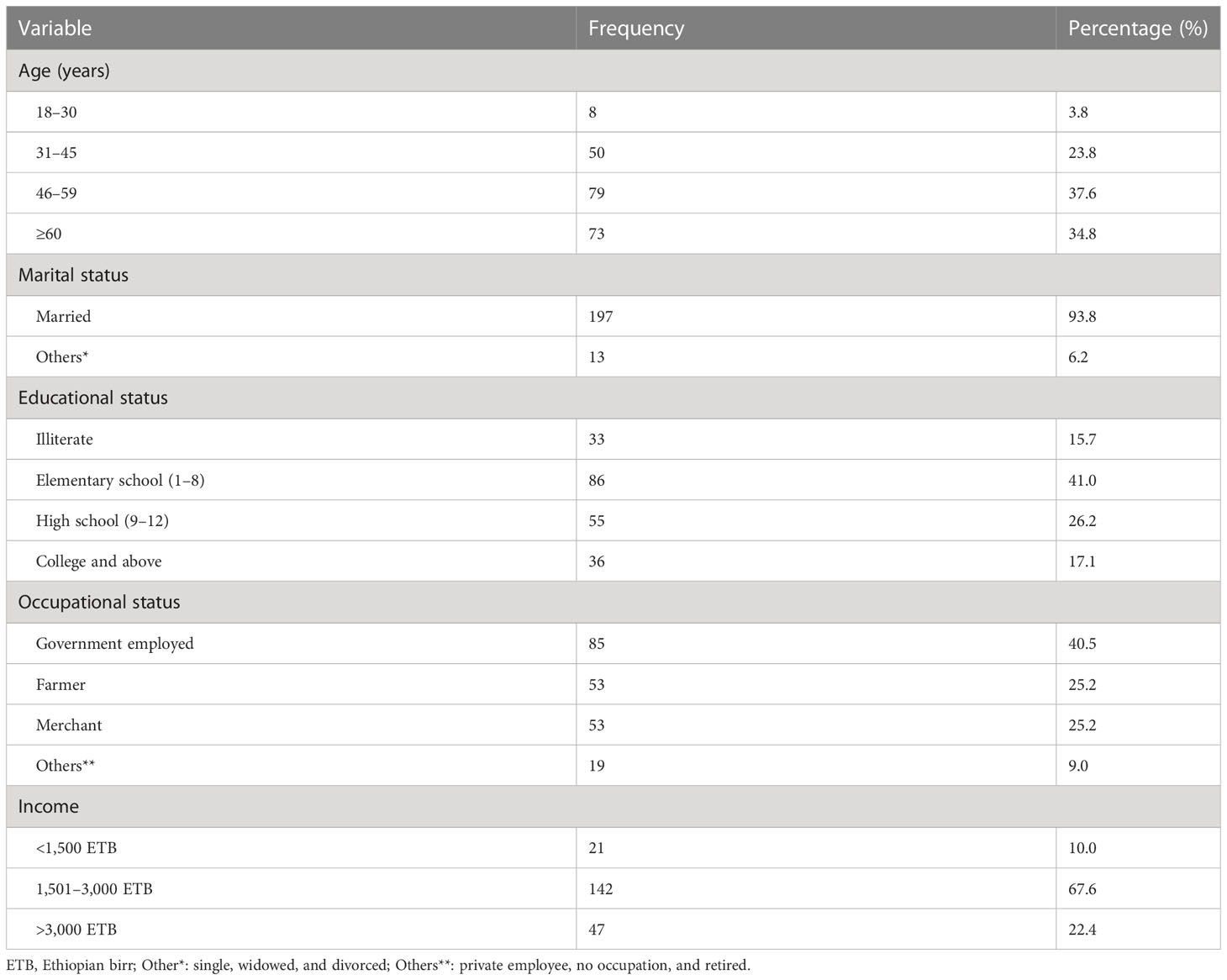
Table 1 Sociodemographic characteristics of adult male patients with diabetes attending follow-up at Hiwot Fana Comprehensive Specialized University Hospital, Harar, Eastern Ethiopia, 2020 (n = 210).
From the total participants, almost all of them did not have unsafe alcohol consumption. Majority of them (121; 57.6%) chew khat, and 32 (15.2%) were smokers. Regarding physical exercise, only about one-fifth (44; 21%) of the participants had regular physical exercise (Figure 1).
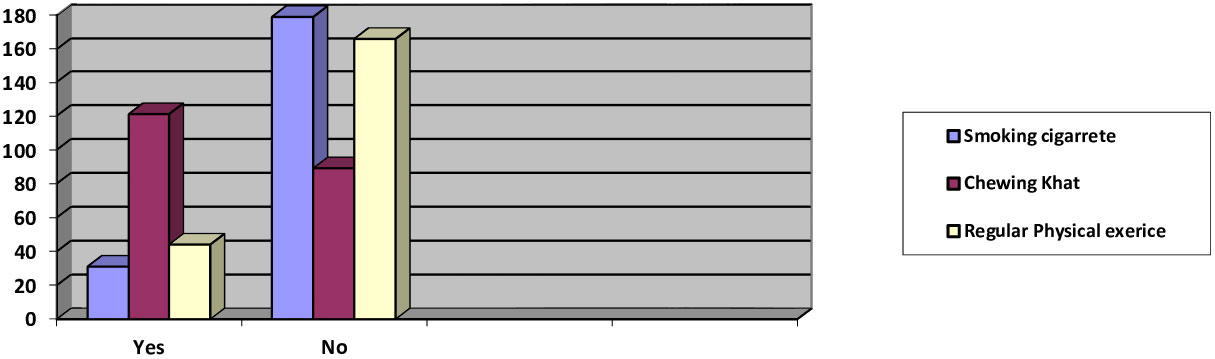
Figure 1 Behavioral characteristics of male patients with diabetes attending diabetic clinic at Hiwot Fana Comprehensive Specialized University Hospital (N = 210), Harar, Eastern Ethiopia, 2020 (n = 210).
Inadequate glycemic control was present at the time of the investigation, as evidenced by the mean fasting blood sugar (FBS) of 162 mg/dl (+19.9 SD). The mean body mass index (BMI) of the participants was 24.6 kg/m2 ( ± 3.3 SD), and almost half of them (103; 49%) had a BMI of 18.5 to 24.96 kg/m2. Majority (54.3%) of the respondents lived with diabetes for < 5 years with mean duration of 5.8 (± 4.21 SD) years. Majority of the participants (117; 55.7%) were within normal range of blood pressure (<140/90). Almost half (104; 49.5%) of the respondents had chronic diseases other than diabetes and were taking medications other than for diabetes (Table 2).
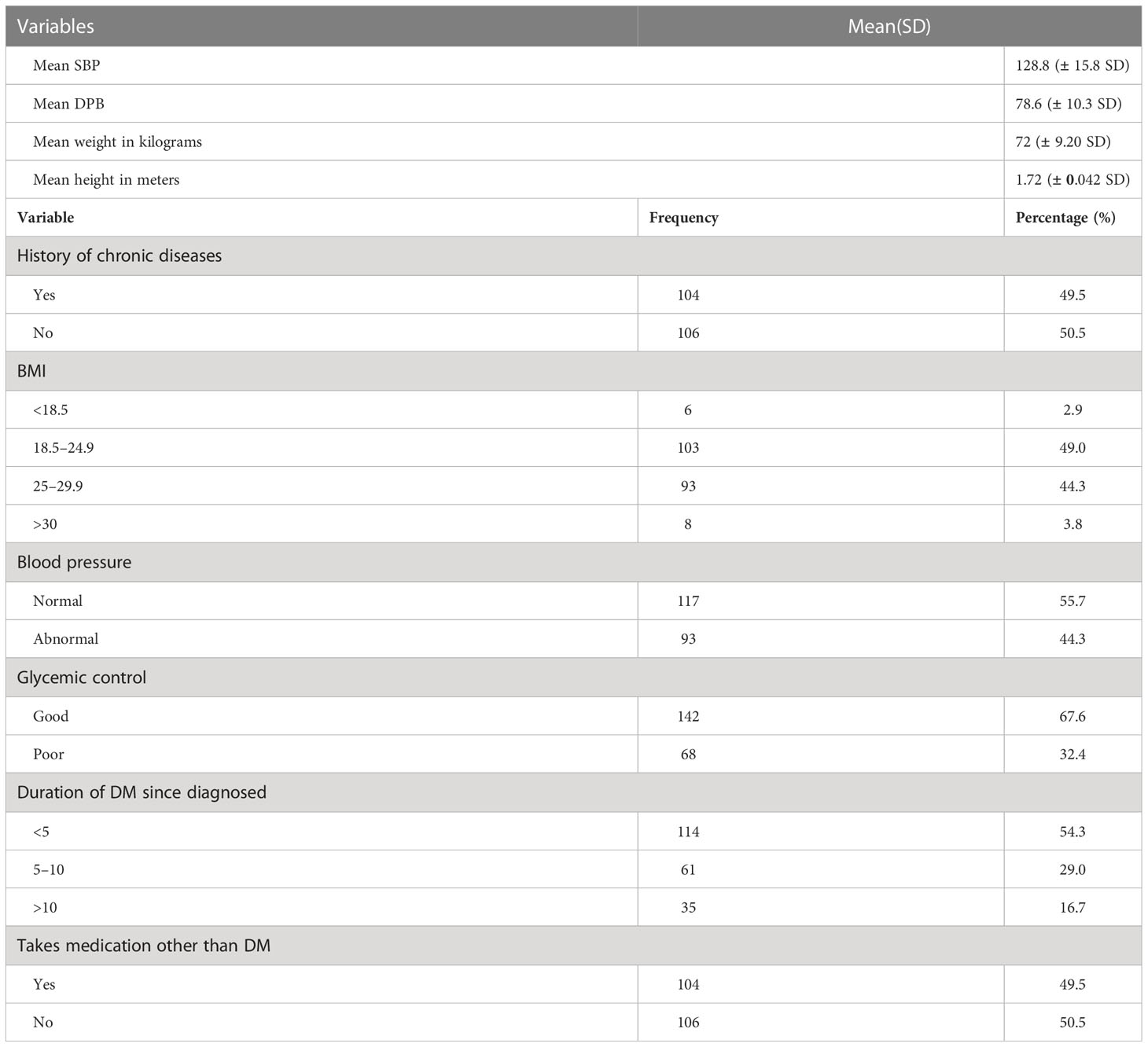
Table 2 Medical conditions of adult male patients with diabetes attending follow-up at Hiwot Fana Comprehensive Specialized University Hospital, Harar, Eastern Ethiopia, 2020 (n = 210).
The magnitude of ED in this study was found to be 83.8% (95% CI: 78.1, 88) of which 37.5% had mild to moderate ED and only 14 (7.95%) had ever sought treatment for the problem (Table 3).
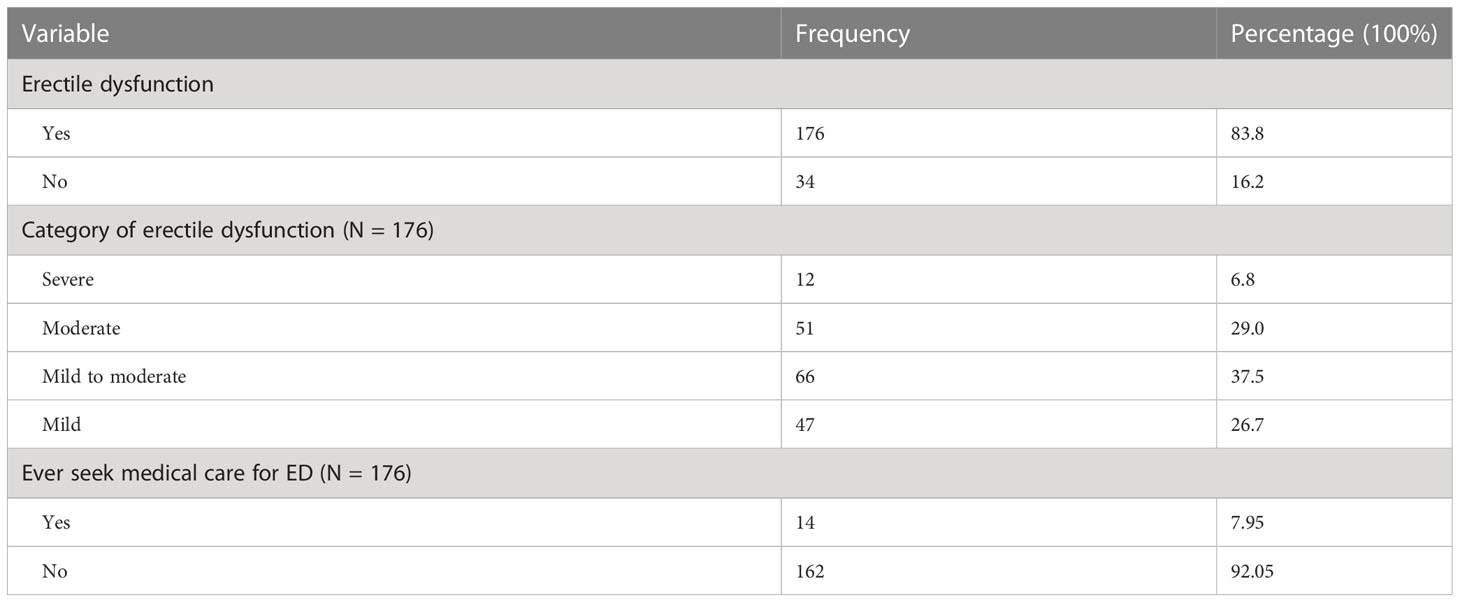
Table 3 Magnitude of erectile dysfunction among adult male patients with diabetes attending follow-up at Hiwot Fana Comprehensive Specialized University Hospital, Harar, Eastern Ethiopia, 2020 (n = 210).
Factors associated with ED among patients with diabetes attending follow-up were assessed in the current study. Independent variables in the bivariable logistic regression analysis that had a p value of less than 0.2 were passed for inclusion in the multivariable logistic regression analysis. Age and glycemic control were identified as the independent predictors significantly associated with ED. Adult male patients with diabetes who were more than 60 years old were 2.9 times more likely to experience ED compared with those in the age category of 18–30 years [AOR: 2.9; 95% CI (1.48, 5.67)]. Participants who were in the age category of 46–59 years were 2.56 times more likely to have ED than those who were in the age category of 18–30 years [AOR: 2.56; 95%CI: (1.73, 6.53)]. Likewise, adult male patients with diabetes who had poor glycemic control were 2.14 times more likely to have ED than those who had good glycemic control [AOR: 2.140; 95% CI (1.9, 7.44)] (Table 4).
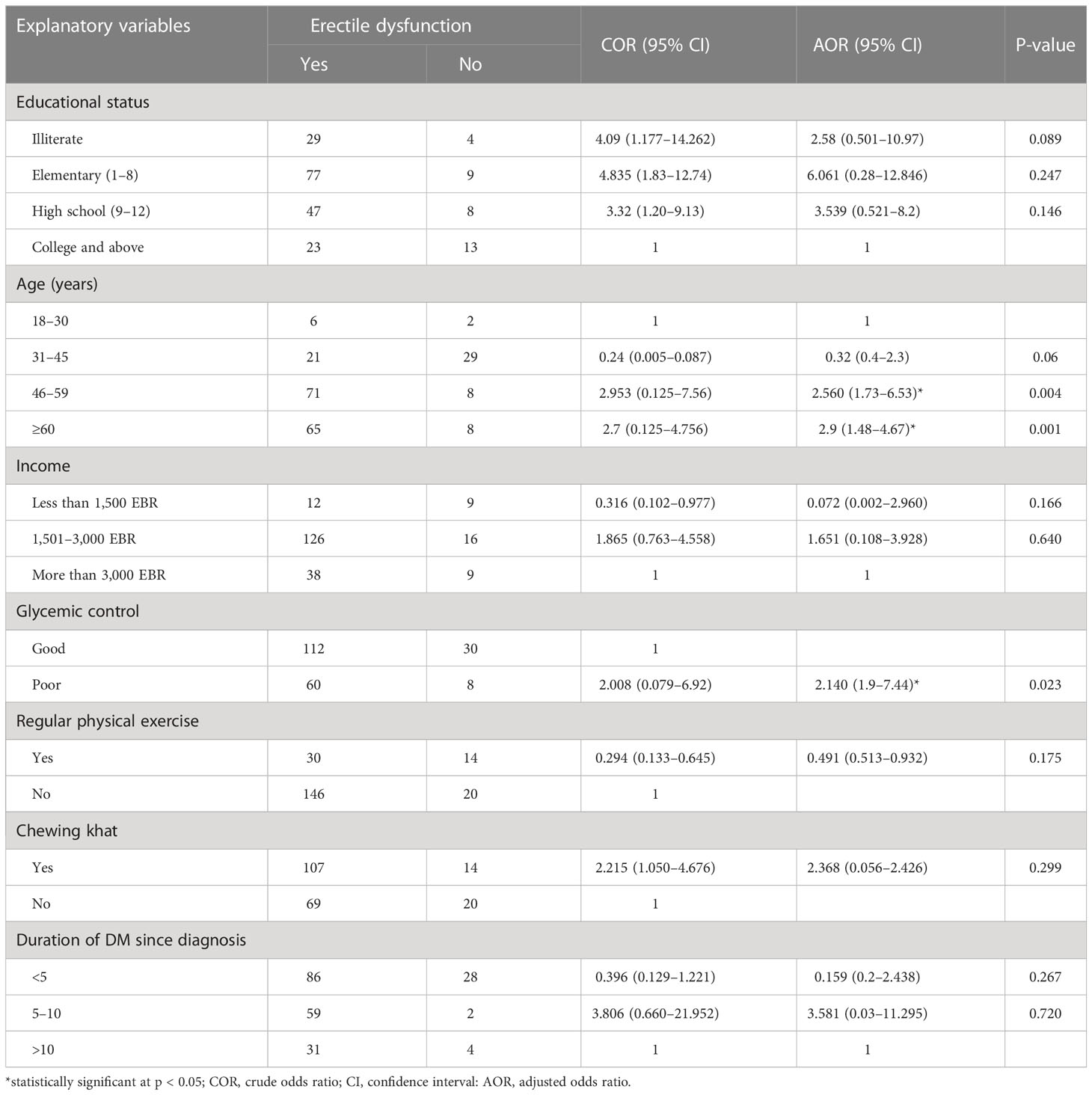
Table 4 Multivariable logistic regression analysis for factors associated with erectile dysfunction among adult male patients with diabetes attending follow-up at Hiwot Fana Comprehensive Specialized University Hospital, Harar, Eastern Ethiopia, 2020 (n = 210).
The current study assessed the magnitude and factors associated with ED among male patients with diabetes attending follow-up at HFCSH. The study found that an overall magnitude of ED was 83.8%. The finding is comparable with studies conducted in China (14), King Saudi University-Medical City in Saudi Arabia (14), and Bahirdar in Ethiopia (24), which showed ED prevalence of 79.1%, 80.5%, and 85.5%, respectively. However, The finding is comparable with studies conducted in Iran, 59.5% (20); Srilanka, 68% (16); Jamaica, 64% (17); Tanzania, 55.1% (15); Jimma, Ethiopia, 6.8% (21); and Central and Northwestern of Tigray, Ethiopia, 69.9% (19). This inconsistency might be due to sociocultural difference among the study population that talking about sexual issue is not such embarrassing in Iran, Srilanka, and Tanzania as it is in our country, so the population in those studies might get diagnosed and treated accordingly before the study was conducted; different data collection methods and tools to determine the magnitude of ED might be the other reason for the discrepancy that the study that was conducted in the Jimma, Ethiopia, used card review, but this study used interview.
The result of the present study presented that age was significantly associated with ED. Adult male patients with diabetes who were more than 60 years old were 2.9 times more likely to experience ED than those in the age category of 18–30 years, and those participants who were in the age of 46–59 years were 2.56 times more likely to have ED that those who those in the age category of 18–30 years. This current finding is consistent with studies conducted in Turkey (9) and Dessie in Ethiopia (8), where male patients with diabetes whose age were greater than 60 years were more likely to experience ED than those who were less than 60 years old. Old age was also associated with ED among male patients with diabetes in Mizan-Tepi University Teaching Hospital and Tepi General Hospital, Ethiopia (23), and Jimma Medical Center, Southwest Ethiopia (11), where the prevalence was higher among patients greater than 40 years of age than those who were less than 40 years old. Older age was also associated with ED in a study conducted in Bahir-dar Ethiopia where both age group 45–59 and >60 years were associated with ED (24).
Glycemic control is another independent predictor in the present study that exhibited significant association with ED. Adult male patients with diabetes who had poor glycemic control were 2.14 times more likely to experience ED compared to those who had good glycemic control. This is consistent with studies carried out in Italy (10) and Saudi Arabia (9), which revealed a significant association of ED with poor glycemic control. However, in the studies conducted in Turkey (13), Northern Srilanka (16), southwest Ethiopia (23), and Jimma Medical Center Ethiopia (11), there was no association found between ED and glycemic control among adult male patients with diabetes. This variation might be due to differences among the study population, the methodology used, time of study, and diverse population culture.
This study has established some important points that will help us generate a hypothesis. It showed the magnitude of ED among patients with diabetes, which increases from time to time and needs attention. It was also used to see the relationship between the factors and ED among patients with diabetes. Because this study used a cross-sectional study design, cause-and-effect relationship cannot be reported.
The overall finding of the current study revealed a high magnitude of ED among male patients with diabetes. Majority of the participants experienced mild to moderate ED. Health institutions and healthcare providers should include assessment and management of ED as part of routine medical care in diabetic follow-up clinics. Patients who are of old age and who had poor glycemic control require special attention in screening for ED.
The original contributions presented in the study are included in the article/supplementary material. Further inquiries can be directed to the corresponding author.
Ethical clearance was obtained from Institutional Health Research Ethical Review Committee (IHRERC) of the College of Health and Medical Science of Haramaya University. The ethical and supportive letters were submitted to Hiwot Fana Comprehensive Specialized Hospital, and consent was obtained from hospital administrator before data collection. A brief introductory orientation was given to the study participants prior to data collection, and written informed voluntary consent was obtained. Moreover, to maintain privacy, the names of the patients were not written on the questionnaire, and patients were interviewed alone in a separate room.
All the authors had made significant contribution in idea generation, study design, analysis, and interpretation. They participated in drafting and reviewing the manuscript. All authors contributed to the article and approved the submitted version.
The authors would like to thank all data collectors and study participants their willingness to participate in the study.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
AOR, adjusted odds ratio; BMI, body mass index; CI, confidence interval; COR, crude odds ratio; DM, diabetic mellitus; ED, erectile dysfunction; ETB, Ethiopian birr; FBS, fasting blood sugar; IIEF-5, International Index of Erectile Function-5; IDF, International Diabetic Federation; HFCSH, Hiwot Fana Comprehensive Specialized Hospital; HTN, hypertension; SD, standard deviation; WHO, World Health Organization.
1. Saeedi P, Petersohn I, Salpea P, Malanda B, Karuranga S, Unwin N, et al. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: results from the international diabetes federation diabetes atlas. Diabetes Res Clin Practice (2019) 157:107843. doi: 10.1016/j.diabres.2019.107843
2. Organization WH. Global report on diabetes 2016. Available at: https://www.who.int/publications/i/item/9789241565257.
4. Research NIoHOoMAo. Consensus NIH, US Development Panel on Impotence. NIH Consensus Conference. Impotence. JAMA. (1992) 270:83–90.
5. Feldman HA, Goldstein I, Hatzichristou DG, Krane RJ, McKinlay JB. Impotence and its medical and psychosocial correlates: results of the Massachusetts Male aging study. J Urol (1994) 151(1):54–61. doi: 10.1016/S0022-5347(17)34871-1
6. Maiorino MI, Bellastella G, Esposito K. Diabetes and sexual dysfunction: current perspectives. Diabetes Metab Syndrome Obesity: Targets Ther (2014) 7:95. doi: 10.2147/DMSO.S36455
7. Van Hemelrijck M, Kessler A, Sollie S, Challacombe B, Briggs K. The global prevalence of erectile dysfunction: a review. BJU Int (2019) 124(4):587–99. doi: 10.1111/bju.14813
8. Abeway S, Dagne K, Zegeye T. Erectile dysfunction and correlates among diabetic men at dessie referral hospital: north central Ethiopia, 2020. Diabetes Metab Syndrome Obesity: Targets Ther (2020) 13:4201. doi: 10.2147/DMSO.S278384
9. Almigbal TH. Erectile dysfunction in men with type 2 diabetes: is it associated with poor glycemic control? J Men's Health (2019) 15(1):e12–22. doi: 10.22374/jomh.v15i1.104
10. Giugliano F, Maiorino M, Bellastella G, Gicchino M, Giugliano D, Esposito K. Determinants of erectile dysfunction in type 2 diabetes. Int J Impotence Res (2010) 22(3):204–9. doi: 10.1038/ijir.2010.1
11. Hurisa AD, Negera GZ. Erectile dysfunction among diabetic patients in a tertiary hospital of southwest Ethiopia. Open Public Health J (2020) 13(1):240–45. doi: 10.2174/1874944502013010240
12. Kemp T, Rheeder P. The prevalence and associations of erectile dysfunction in a south African male diabetic urban population. J Endocrinol Metab Diabetes South Africa (2015) 20(3):134–40. doi: 10.1080/16089677.2015.1090185
13. Kiskac M, Zorlu M, Cakirca M, Buyukaydin B, Karatoprak C, Yavuz E. Frequency and determinants of erectile dysfunction in Turkish diabetic men. Nigerian J Clin Practice (2015) 18(2):209–12. doi: 10.4103/1119-3077.151043
14. Lo WH, Fu SN, Wong CKH, San Chen E. Prevalence, correlates, attitude and treatment seeking of erectile dysfunction among type 2 diabetic Chinese men attending primary care outpatient clinics. Asian J Androl (2014) 16(5):755. doi: 10.4103/1008-682X.127823
15. Mutagaywa RK, Lutale J, Aboud M, Kamala BA. Prevalence of erectile dysfunction and associated factors among diabetic men attending diabetic clinic at muhimbili national hospital in dar-es-Salaam, Tanzania. Pan Afr Med J (2014) 17:227–35. doi: 10.11604/pamj.2014.17.227.2695
16. Nisahan B, Kumanan T, Rajeshkannan N, Peranantharajah T, Aravinthan M. Erectile dysfunction and associated factors among men with diabetes mellitus from a tertiary diabetic center in northern Sri Lanka. BMC Res Notes (2019) 12(1):1–6. doi: 10.1186/s13104-019-4244-x
17. Peter J, Riley C, Layne B, Miller K, Walker L. Prevalence and risk factors associated with erectile dysfunction in diabetic men attending clinics in Kingston, Jamaica. J Diabetol (2012) 2(2).
18. Rosen RC, Wing RR, Schneider S, Wadden TA, Foster GD, West DS, et al. Erectile dysfunction in type 2 diabetic men: relationship to exercise fitness and cardiovascular risk factors in the look AHEAD trial. J Sexual Med (2009) 6(5):1414–22. doi: 10.1111/j.1743-6109.2008.01209.x
19. Seid A, Gerensea H, Tarko S, Zenebe Y, Mezemir R. Prevalence and determinants of erectile dysfunction among diabetic patients attending in hospitals of central and northwestern zone of tigray, northern Ethiopia: a cross-sectional study. BMC Endocrine Disord (2017) 17(1):1–7. doi: 10.1186/s12902-017-0167-5
20. Sharifi F, Asghari M, Jaberi Y, Salehi O, Mirzamohammadi F. Independent predictors of erectile dysfunction in type 2 diabetes mellitus: is it true what they say about risk factors? Int Scholarly Res Notices (2012) 2012. doi: 10.5402/2012/502353
21. Worku D, Hamza L, Woldemichael K. Patterns of diabetic complications at jimma university specialized hospital, southwest ethiopia. Ethiopian J Health Sci (2010) 20(1):33–9. doi: 10.4314/ejhs.v20i1.69424
22. Shiferaw WS, Akalu TY, Aynalem YA. Prevalence of erectile dysfunction in patients with diabetes mellitus and its association with body mass index and glycated hemoglobin in Africa: a systematic review and meta-analysis. Int J Endocrinol (2020) 2020:1–0. doi: 10.1155/2020/5148370
23. Asefa A, Nigussie T, Henok A, Mamo Y. Prevalence of sexual dysfunction and related factors among diabetes mellitus patients in southwest Ethiopia. BMC Endocrine Disord (2019) 19(1):1–8. doi: 10.1186/s12902-019-0473-1
24. Walle B, Lebeta KR, Fita YD, Abdissa HG. Prevalence of erectile dysfunction and associated factors among diabetic men attending the diabetic clinic at felege hiwot referral hospital, bahir dar, north West Ethiopia, 2016. BMC Res Notes (2018) 11(1):1–5. doi: 10.1186/s13104-018-3211-2
25. Weldesenbet AB, Kebede SA, Tusa BS. Prevalence of erectile dysfunction and its associated factors among patients with diabetes in Ethiopia: a systematic review and meta-analysis. J Int Med Res (2021) 49(2):0300060521993318. doi: 10.1177/0300060521993318
26. Hatzimouratidis K, Amar E, Eardley I, Giuliano F, Hatzichristou D, Montorsi F, et al. Guidelines on male sexual dysfunction: erectile dysfunction and premature ejaculation. Eur Urol (2010) 57(5):804–14. doi: 10.1016/j.eururo.2010.02.020
27. Moreira Júnior ED, Bestane WJ, Bartolo EB, Fittipaldi JAS. Prevalence and determinants of erectile dysfunction in santos, southeastern Brazil. Sao Paulo Med J (2002) 120(2):49–54. doi: 10.1590/S1516-31802002000200005
28. McMahon CG. Current diagnosis and management of erectile dysfunction. Med J Australia (2019) 210(10):469–76. doi: 10.5694/mja2.50167
Keywords: magnitude, erectile dysfunction diabetes mellitus, Eastern Ethiopia, complication of diabetes, patient
Citation: Gobena MB, Abdosh T, Dheresa M and Dechasa DB (2023) Erectile dysfunction and associated factors among patients with diabetes attending follow-up at a public hospital, Harar, Eastern Ethiopia. A cross-sectional study design. Front. Endocrinol. 14:1131555. doi: 10.3389/fendo.2023.1131555
Received: 05 January 2023; Accepted: 10 May 2023;
Published: 13 June 2023.
Edited by:
Ke Rao, Huazhong University of Science and Technology, ChinaReviewed by:
Hongjun Li, Peking Union Medical College Hospital (CAMS), ChinaCopyright © 2023 Gobena, Abdosh, Dheresa and Dechasa. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Deribe Bekele Dechasa, ZGVyaWJlZWJAZ21haWwuY29t
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.