- Department of Endocrinology, First Affiliated Hospital of Anhui Medical University, Hefei, China
Background: The purpose of the study was to evaluate characteristics and risk of cardiovascular disease (CVD) according to age at diagnosis and disease duration among adults with diabetes mellitus (DM).
Methods: The association between age at diagnosis, diabetes duration and CVD were examined in 1,765 patients with DM. High risk of estimated ten-year atherosclerotic cardiovascular disease (ASCVD) was performed by the Prediction for ASCVD Risk in China (China-PAR) project. Data were compared with analysis of variance and χ2 test, respectively. Multiple logistic regression was used to determine the risk factors of CVD.
Results: The mean age at diagnosis (± standard deviation) was 52.91 ± 10.25 years and diabetes duration was 8.06 ± 5.66 years. Subjects were divided into early-onset DM group (≤43 years), late-onset DM group (44 to 59 years), elderly-onset DM group (≥60 years) according to age at diagnosis. Diabetes duration was classified by 5 years. Both early-onset and longest diabetes duration (>15 years) had prominent hyperglycaemia. Diabetes duration was associated with the risk of ischemic stroke (odds ratio (OR), 1.091) and coronary artery disease (OR, 1.080). Early-onset group (OR, 2.323), and late-onset group (OR, 5.199), and hypertension (OR, 2.729) were associated with the risk of ischemic stroke. Late-onset group (OR, 5.001), disease duration (OR, 1.080), and hypertension (OR, 2.015) and hyperlipidemia (OR, 1.527) might increase the risk of coronary artery disease. Aged over 65 (OR, 10.192), central obesity (OR, 1.992), hypertension (OR, 18.816), cardiovascular drugs (OR, 5.184), antihypertensive drugs (OR, 2.780), and participants with disease duration >15 years (OR, 1.976) were associated with the high risk of estimated ten-year ASCVD in participants with DM.
Conclusion: Age at diagnosis, diabetes duration, hypertension and hyperlipidemia were independent risks of CVD. Longest (>15 years) diabetes duration increased the high risk of ten-year ASCVD prediction among Chinese patients with DM. It’s urgent to emphasize the importance of age at diagnosis and diabetes duration to improve primary complication of diabetes.
1 Introduction
Diabetes mellitus (DM), commonly referred to as diabetes, is a chronic metabolic disorder caused by insufficient insulin production and/or insulin resistance resulting from both environmental and genetic components (1). Its prevalence increased dramatically over the last three decades. An estimated 536.6 million people in 20–79 year olds have DM in 2021, and this number is expected to reach 12.2% (783.2 million) by the year 2045 (1). Considering the health and economic consequences associated with DM (complications, obesity, mortality), there is huge interest in strategies to reduce DM prevalence (2, 3). Cardiovascular disease (CVD), including coronary artery disease, cerebrovascular disease, or peripheral arterial disease, is a macrovascular complication that mostly develops in patients with diabetes (4). The prevalence rate of CVD is higher in adults with diabetes than in those without diabetes (4). CVD mostly developed in the following cases: genetic predisposition, hypoglycaemia, during treatment, increased insulin resistance (4). Furthermore, CVD greatly contributes to morbidity and mortality among patients with DM. In addition, compared with patients without CVD, those diagnosed with the disease are particularly prominent among younger patients with hyperglycaemia and serious renal complications (5). Similar to the increase in DM prevalence, cerebrovascular disease prevalence has also increased globally and increasingly been recognised as cerebral macrovascular complications of type 2 diabetes mellitus (T2DM) (6). T2DM is associated with a 2.5-times increased risk of ischaemic stroke (7). Ischaemic stroke is also common among adults with prediabetes than among people with normoglycaemia, suggesting that cerebral infarcts processes start before the onset of diabetes (8, 9). In view of ageing populations and the growing prevalence of DM, DM prevention strategies are of paramount importance and identifying the mechanisms linking DM with CVD is key to reduce the macrovascular complications.
Previous data suggested that age, age at diagnosis and disease duration had varying effects on the risk of vascular complications in patients with DM (10–12). For example, Zoungas et al. reported that age or age-onset, and duration of diabetes were independently associated with macrovascular events and death, whereas only duration is independently associated with microvascular events (12). Subsequent studies confirmed age and duration of diabetes were strong risk factors for myocardial infarction, stroke, and heart failure (10). Furthermore, studies of people with T2DM using a propensity score-matched cohort analysis provide excellent insight into the early clinical course of diabetes, indicating the earlier onset of T2DM induce the higher risk of microvascular (11). Few studies evaluated clinical characteristics and macrovascular complications according to age at diagnosis and prolonged duration of diabetes among Chinese patients with DM (13). Therefore, the aim of our study is to investigate the relationship between onset age of diabetes and complications, and provide a better understanding of age at diagnosis on the risk of complications, and improved explanation of the modifiable risk factors to reduce the burden of macrovascular complications and T2DM.
2 Methods
2.1 Setting and study subjects
The current data analysis was based on the China National Diabetic Chronic Complications Study (China DiaChronic Study), which has been reported in detail previously (14). Briefly, a total of 53,401 Chinese adults with diagnosed diabetes ages 18–74 were recruited and completed baseline questionnaires and medical examinations between March 2018 and January 2020. The multistage sampling scheme (stratification, clustering, and random) was used to sample study participants based on the disease surveillance points (DSPs) started in 2013 from the China Chronic Disease and Risk Factors Surveillance (CCDRFS). The sampling details have been described elsewhere (15, 16). Stage 1, four DSPs were selected from 25 provinces, autonomous regions and municipalities, five DSPs were selected from Sichuan, Henan, Shandong, 2 to 3 DSPs were selected from Qinghai, Tibet, Xinjiang. In total, there are 122 study sites (65 urban and 57 rural DSPs) from the 2013 CCDRFS were invited to participate. Stage 2, four neighborhoods/villages were selected from each DSP, and a total of 260 neighborhoods and 228 villages were acquired. Stage 3, 58,560 Chinese adults with diagnosed diabetes ages 18-74 were recruited in the study after selecting 120 participants at each neighborhood/village by gender and age ratio.
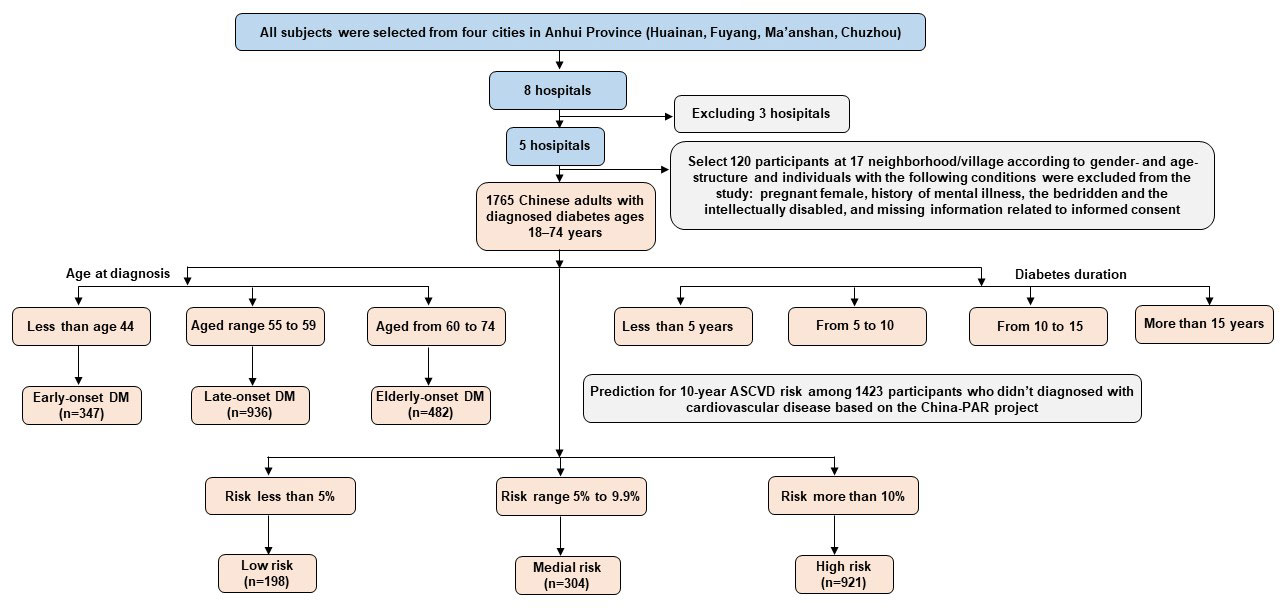
In this study, a total of 1,765 participants were recruited from four cities (Huainan, Fuyang, Ma’anshan, Chuzhou) in Anhui province. Each participant received a series of medical examinations including a general physical examination and biochemical tests of blood and urine sample, as well as a standard self-administered questionnaire survey. Moreover, to avoid the influence of confounding factors, we restricted our analysis to those participants aged 18−74 years, and who had resided in the study sites for at least 6 months during the 12 months prior to the survey. We also excluded those who reported the following conditions: pregnant female, history of mental illness, the bedridden and the intellectually disabled, and missing information related to informed consent. Information on personal age at diabetes mellitus diagnosis and diabetes duration was obtained by a self-administrated questionnaire. Diabetes duration was calculated by subtracting age at diagnosis from age at study baseline. Duration of diabetes was classified into four ordinal groups (≤5, >5−10, >10−15 and >15 years). For age at diagnosis, they were asked “When did you first diagnose diabetes?” Age at diagnosis was classified into three groups: less than age 44 (early-onset DM), aged range of 44 to 59 (late-onset DM), aged from 60 and 74 (elderly-onset DM). Furthermore, the China-PAR project was used to predict 10-year atherosclerotic cardiovascular disease (ASCVD) risk among Chinese population, the details have been described elsewhere (17–19). The Chinese prediction models directly included age, SBP, total cholesterol, HDL-C, current smoking, and diabetes. Four additional covariates (waist circumference (WC), geographic region, urbanization, and family history of ASCVD) met the pre-defined inclusion criteria based on relative integrated discrimination improvement (IDI) of 6% or greater. This tool is applicable to people aged 20 and above without history of cardiovascular and cerebrovascular diseases. Therefore, 1423 participants were selected in our study. According to predicted ASCVD risk, participants were divided into three categories: low risk (<5%), median risk (5%−9.9%), high risk (≥10%). Details of the workflow chart are presented in Figure 1. Personal identification was removed and remained anonymous when the data were released for this research. All participants provided written informed consent, and Ethical Review Committee (Approval No: 2018-010) approved the study, which was registered in the Chinese Clinical Trial registry (ChiCTR1800014432).
2.2 Estimation of sample size
The sample size calculation was estimated by using following formula.
Z1-α/2 = 1.96, the prevalence of diabetes mellitus was 11.2% (p), the desired level of relative precision was 0.15 (ε) (20). Then, considering multicenter design and drop-out rate of 10% total sample size, hence the minimum sample required for conducting this study was found to be 1540.
2.3 Assessment of covariates
Information on sociodemographic characteristics collected in the baseline was used in the current data analysis, including age, sex, medical insurrance, marital status (single, married, lived together, divorced, separated and widowed), total annual family income and education level (primary school or below, middle school, and college, and university or above). Lifestyle factors including alcohol drinking (never, former, and current), cigarette smoking (never, former, and current), and family medical histories (yes, no) was collected at baseline by trained interviewers using semi-structured questionnaires. The general health examinations were performed by qualified personnel. Hyperglycaemia was defined as a glycosylated hemoglobin (HbA1c) >7.0% and fasting plasma glucose (FPG) >7.0 mmol/L (1). Body mass index (BMI) was calculated as weight in kilograms divided by height in meters squared. Obesity was defined as a BMI of ≥28 kg/m2 (21). WC was calculated by horizontal girth of waist through belly button. Central obesity was defined as WC ≥90 cm in men and WC ≥85 cm in women for Chinese (22). Resting blood pressure including systolic blood pressure (SBP) and diastolic blood pressure (DBP) was measured and fasting blood was drawn for laboratory assays of blood lipids, fasting glucose, glycosylated hemoglobin, hepatic function, renal function. Hypertension was defined as self-reported physiciandiagnosed hypertension or current use of antihypertensive medications or SBP ≥140mmHg/DBP ≥90 mmHg by the 2017 American College of Cardiology/American Heart Association guidelines (23). Myocardial infarction was defined as a history of physician-diagnosed myocardial infarction. Hyperlipidemia was defined as a history of physician-diagnosed hyperlipidemia or current usage of lipid-lowering medications or total cholesterol (TC) ≥5.20 mmol/L or triglycerides (TG) ≥1.70 mmol/L or high-density lipoprotein cholesterol (HDL-C)<1.0 mmol/L or low-density lipoprotein cholesterol (LDL-C) ≥3.4 mmol/L by the 2019 China Cholesterol Education Program (CCEP) expert advice for the management of dyslipidaemias to reduce cardiovascular risk (24). Information on medications collected in the baseline was used in our study, including antihypertensive drugs, cardiovascular drugs, lipid lowering medication, glucose lowering medication.
2.4 Ascertainment of the outcome
The presence of diabetic macrovascular complications (coronary artery disease and cerebrovascular disease) was assessed from the questionnaire of each participants. To collect the information, the participants were asked: “Have you ever been diagnosed as cardiovascular disease or ischemic stroke by physicians in medical institutions at county/district level or above?” Those participants who answered “yes” were then defined as having a event of cardiovascular disease or ischemic stroke. Furthermore, these patients were asked two questions: “When did you first diagnose these diseases?” “Did you hospitalized after you suffer from above mentioned disease?” A total of 234 ischemic stroke cases and 145 coronary artery disease cases were observed in this study.
2.5 Statistical analysis
Data were presented as mean (standard deviation) for continuous variables and percentages for categorical variables, respectively. χ2 test was employed to compare categorical variables between groups. Statistical differences between groups for continuous variables were compared with Mann-Whitney U tests or analysis of variance. Binary logistic regression analysis with forward selection was performed to identify independent factors associated with the risk of ischemic stroke and coronary artery disease. The results were presented as odds ratio (OR) and 95 percent confidence interval (95% CI), taking age at diagnosis of 60 to 74 years as the reference groups, based on the previous studies suggesting that the onset age after 60 years was less likely to have macrovascular and microvascular complications (11). Potential covariates included in the adjusted model were age, BMI, WC, hypertension, hyperlipidemia, diabetes duration, family history of ischemic stroke and coronary artery disease, age at diagnosis, lipid lowering medication, cardiovascular drugs, antihypertensive drugs. Analysis of variance (ANOVA) with Tukey’s test for multiple comparison was conducted to compare following values (BMI, HbA1c, FPG, LDL-C, TC, TG) and trends according to disease duration among the three age groups. Furthermore, Hosmer-Lemeshow test was performed to evaluate the goodness of fit of the logistic regression model. All analyses were conducted using SPSS version 25.0 (IBM Co., Armonk, NY, USA) All statistical tests were two-tailed and the significance level was set at P<0.05.
3 Results
3.1 Characteristics of study population
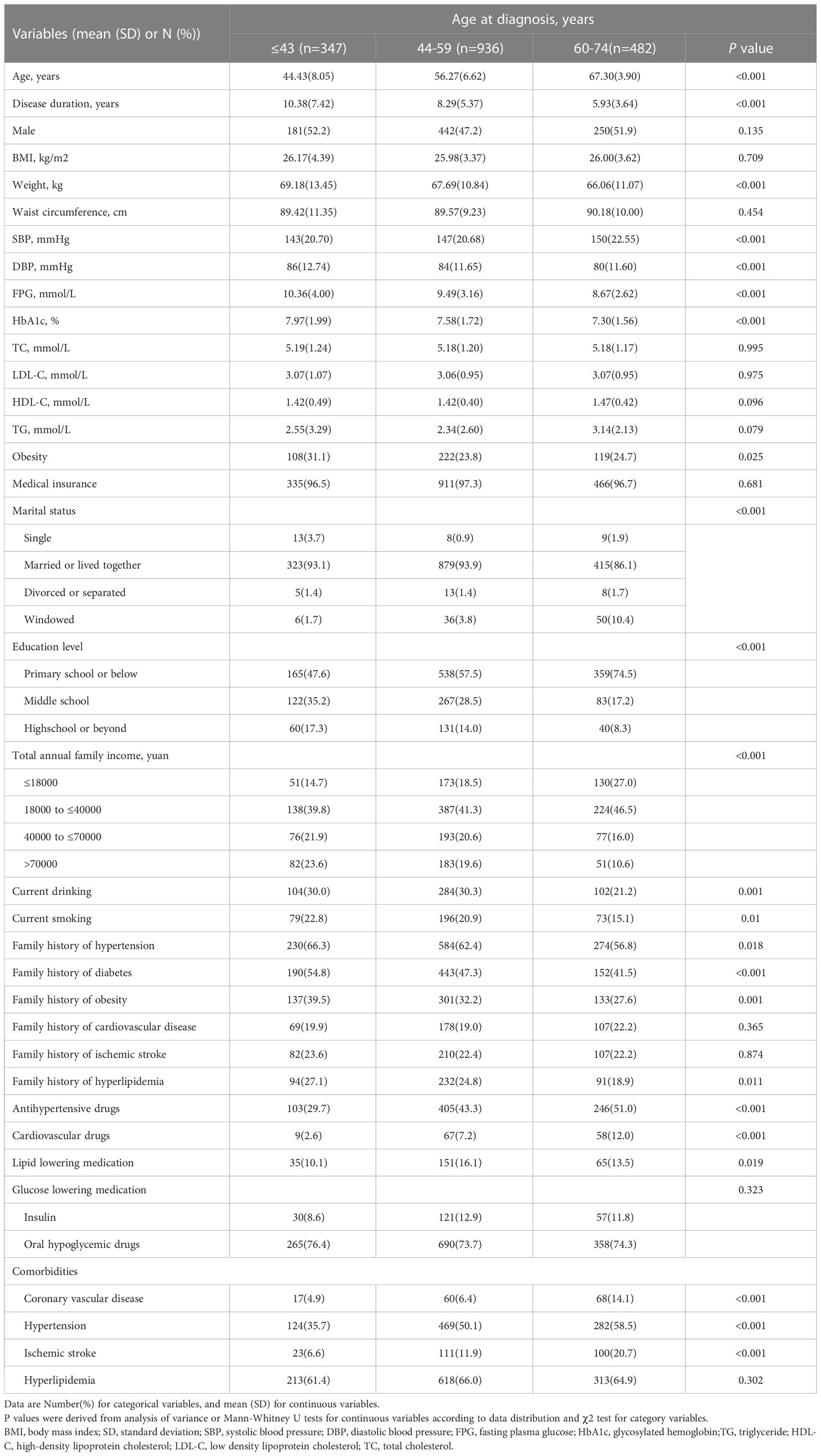
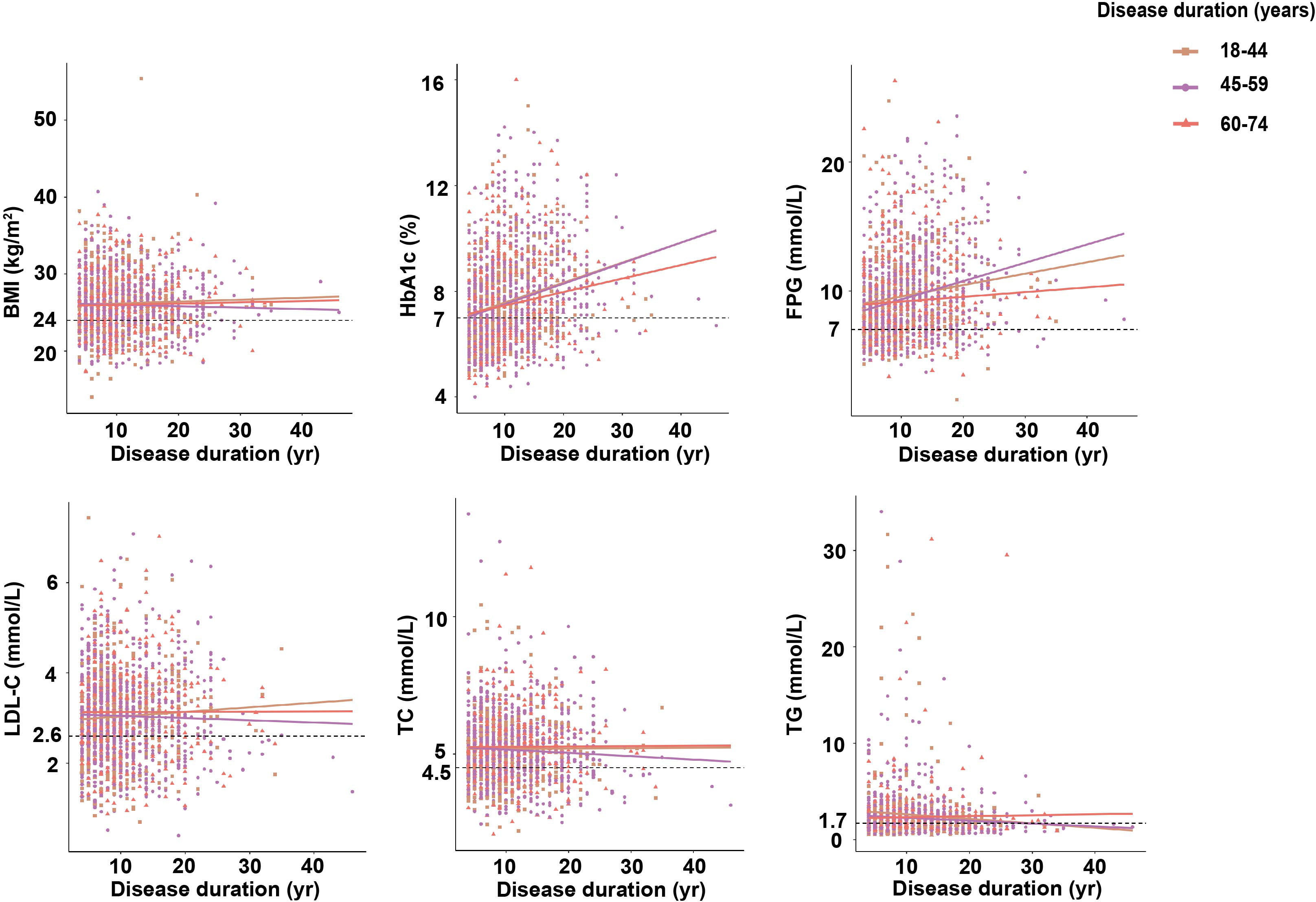
The baseline characteristics of the study population by strata of age at diagnosis and diabetes duration are shown in Tables 1, 2, respectively. Of a total of 1765 patients, the mean (± SD) age of the cohort was 56.96 ± 10.02 years and the age at diagnosis was 52.91 ± 10.25 years, with 19.7%, 53.0% and 27.3% of patients reporting their age at diagnosis as 18−43, >44−59 and >60−74 years, respectively (Table 1). The mean (± SD) diabetes duration was 8.06 ± 5.66 years, with 40.0%, 29.9%, 18.5% and 11.7% of patients reporting a diabetes duration of ≤5, >5−10, >10−15 and >15 years, respectively (Table 2). The mean age at diagnosis of the group with the longest diabetes duration (>15 years) was significnatly lower than of the groups with shorter diabetes duration (P<0.001, Table 2). Early-onset group (aged ≤43 years) and longest diabetes duration group (>15 years) were more likely to have higher level of FPG and HbA1c, and higher family history of diabetes, compared to those diagnosed at older age group (44 to 59 and 60 to 74 years) and shorter diabetes duration (≤ 15 years) (P<0.001, Tables 1, 2). Furthermore, compared with the younger onset age group, participants reporting diagnosed at elderly onset group were more likely to have hypertension and take antihypertensive drugs, to have coronary vascular disease and use cardiovascular drugs, to have ischemic stroke and take lipid lowering medication (P<0.001, Table 1). Besides, the longest diabetes duration (>15 years) were also more likely to have hypertension, ischemic stroke and coronary vascular disease compared with the shorter diabetes duration. However, participants reporting with the longer diabetes duration (10−15 years) were more likely to take antihypertensive drugs, and cardiovascular drugs (P<0.001, Table 2). Meanwhile, compared with participants reporting older age group and shorter diabetes duration, those reporting diagnosed at early-onset group and longest diabetes duration were more likely to have higher DBP level (P<0.001, Tables 1, 2). No interaction was observed between the age at diagnosis and diabetes duration on gender, WC, lipid abnormalities, medical insurance, family history of diseases (cardiovascular disease, ischemic stroke and hyperlipidemia), glucose lowering medication and comorbidities of hyperlipidemia (all P >0.05) (Tables 1, 2).
3.2 Different patterns of parameters and disease duration according to age at diagnosis
As shown in Figure 2, HbA1c and FPG increased with the duration of disease, which exceeding the maximum normal reference value (HbA1c<7.0%, FPG<7.0 mmol/L) (1). The HbA1c showed positively associated with the duration of diabetes and the degree of increase was more prominent in participants with late-onset group (R2 = 0.066, 44 to 59 years) than those with early-onset group (R2 = 0.058, P<0.001, ≤43 years) and elderly-onset group (R2 = 0.026, P<0.001, 60 to 74 years). The significant association was also observed in FPG, and the degree of increase was more prominent in participants reporting late-onset group (R2 = 0.065, P<0.001) than those with early-onset group (R2 = 0.02, P<0.001), while no significant association with elderly-onset group (P =0.17). However, the trend of increasing BMI, TC, TG, LDL-C according to disease duration was incomparable among age groups (all P >0.05).
3.3 Risk factors of diabetic macrovascular complications (coronary artery disease and ischemic stroke) in participants with DM
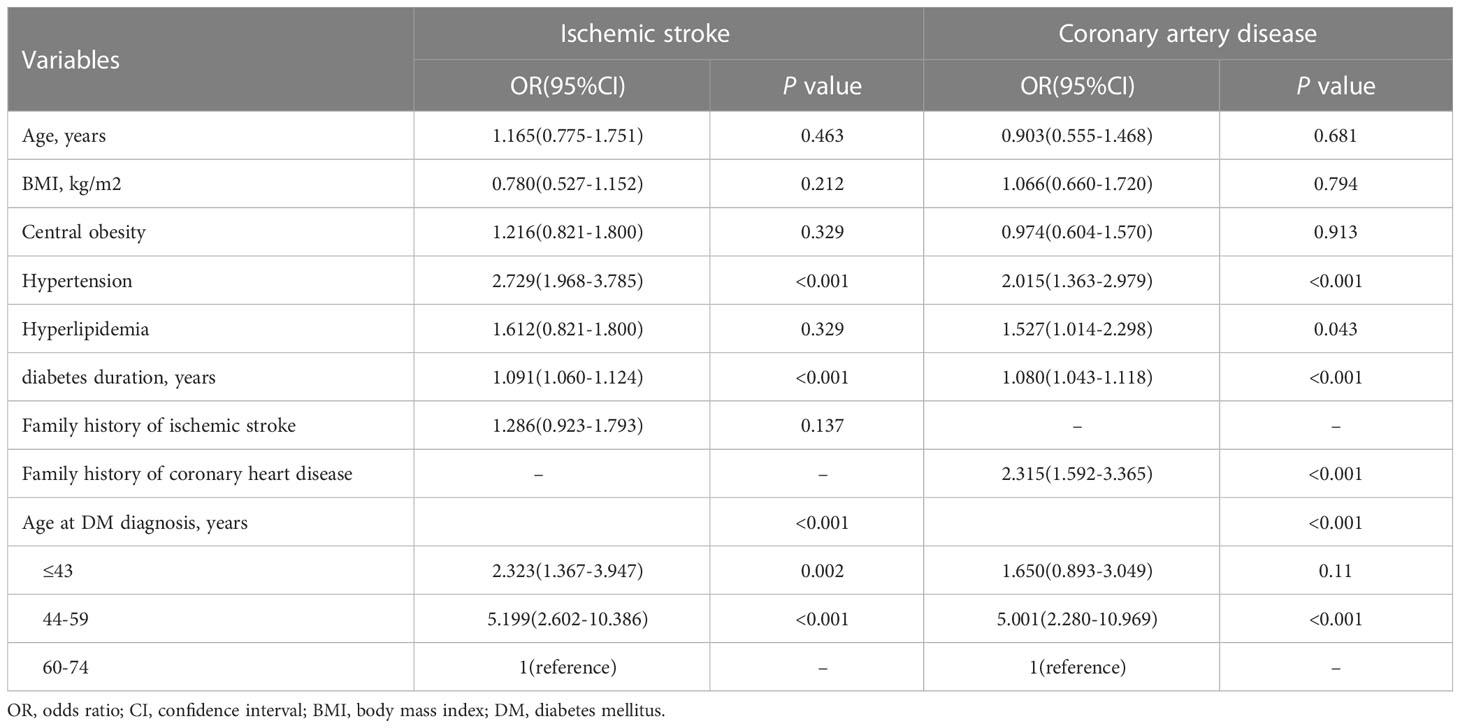
The prevalence of ischemic stroke was different among the three age-onset groups and four diabetes duration groups (P<0.001) (Tables 1, 2). Coronary artery disease and ischemic stroke were significantly more common in elderly-onset group and longest diabetes duration (P<0.001) (Tables 1, 2). With regard to risk factors associated with ischemic stroke complications in patients with DM, disease duration (OR, 1.091; 95% CI, 1.060 to 1.124; P<0.001), hypertension (OR, 2.729; 95% CI, 1.968 to 3.785; P<0.001), early-onset group (≤43 years, OR, 2.323; 95% CI, 1.367 to 3.947; P = 0.002), and late-onset group (44 to 59 years, OR, 5.199; 95% CI, 2.602 to 10.386, P< 0.001) were independently associated with the risk of ischemic stroke. Meanwhile, diabetes duration (OR, 1.080; 95% CI, 1.043 to 1.118; P<0.001), hypertension (OR, 2.015; 95% CI, 1.363-2.979, P<0.001), hyperlipidemia (OR, 1.527; 95% CI, 1.014-2.298, P = 0.043), family history of coronary heart disease (OR, 2.315; 95% CI, 1.592-3.365, P<0.001), and late-onset group (44 to 59 years old; OR, 5.001, 95% CI, 2.280-10.969, P<0.001) were associated with coronary artery disease. No interactions was observed between age, BMI, central obesity, and the risk of macrovascular events (all P >0.05) (Table 3).
3.4 Characteristics of the participants stratified by estimated ten-year ASCVD risk (%)
The baseline characteristics of the 1,423 participants stratified by estimated ten-year ASCVD were shown in Table 4, respectively. Overall, the mean (± SD) age of the cohort was 55.68 ± 10.01 years, the age at diagnosis was 52.03 ± 10.15 years, and the mean (± SD) diabetes duration was 7.66 ± 5.36 years, respectively (Table 4). According to predicted ASCVD risk, participants who were identified with high risk (≥10%) were more likely to be male (51.8% vs. 50.3% vs. 38.9%; P = 0.004), older (59.40 years vs. 52.91 years vs. 42.58 years; P<0.001), current smoking (22.4% vs. 12.1% vs. 21.1%; P = 0.005) and higher central obesity (82.7% vs. 67.1% vs. 59.1%; P<0.001), higher BMI (26.38 kg/m2 vs. 25.17 kg/m2 vs. 24.87 kg/m2; P<0.001) and WC (91.05 cm vs. 87.11cm vs. 85.25 cm; P<0.001), higher value of SBP (154.45 mmHg vs. 136.54 mmHg, vs. 126.90 mmHg; P<0.001) and DBP (85.42 mmHg vs. 81.30 mmHg vs. 78.68 mmHg; P<0.001), higher TC (5.28 mmol/L vs. 5.21 mmol/L vs. 4.95 mmol/L; P = 0.002) and TG level (2.63 mmol/L vs. 2.01 mmol/L vs. 1.92 mmol/L; P<0.001) compared with the lower risk groups (low risk and median risk). In addition, compared with the lower risk groups, participants who were identified with high risk were more likely to diagnose at elderly-onset group (60-74 years, 23.7% vs. 1.0% vs. 9.9%; P<0.001) and less likely to diagnose at early-onset group (11.5% vs. 66.7% vs. 23.4%; P<0.001), and more likely to have lower family history of diabetes (42.1% vs. 48.0% vs. 42.1%; P = 0.002) and have hypertension (59.8% vs. 5.6% vs. 22.0%; P<0.001) and hyperlipidemia (66.3% vs. 47.5% vs. 60.0%; P<0.001). Furthermore, compared with the lower risk groups, participants who were identified with high risk were more likely to take blood pressure medicine (50.6% vs. 20.4% vs. 5.1%; P<0.001), lipid lowering medication (12.9% vs. 8.9% vs. 3.5%; P<0.001) Besides, participants who were identified with medial risk were more likely to take cardiovascular drugs (4.6% vs. 2.0% vs. 0.5%; P = 0.005). Compared to those with a diabetes duration of<5 years, a diabetes duration of ≥10 years,was associated with increased estimated risk of 10-year ASCVD risk (P = 0.001). However, there was no evidence for FPG, HbA1c, LDL-C, current drinking, medical insurance, family history of a series of diseases (hypertension, obesity, cardiovascular disease, ischemic stroke and hyperlipidemia) and glucose lowering medication between three groups (all P >0.05) (Table 4).
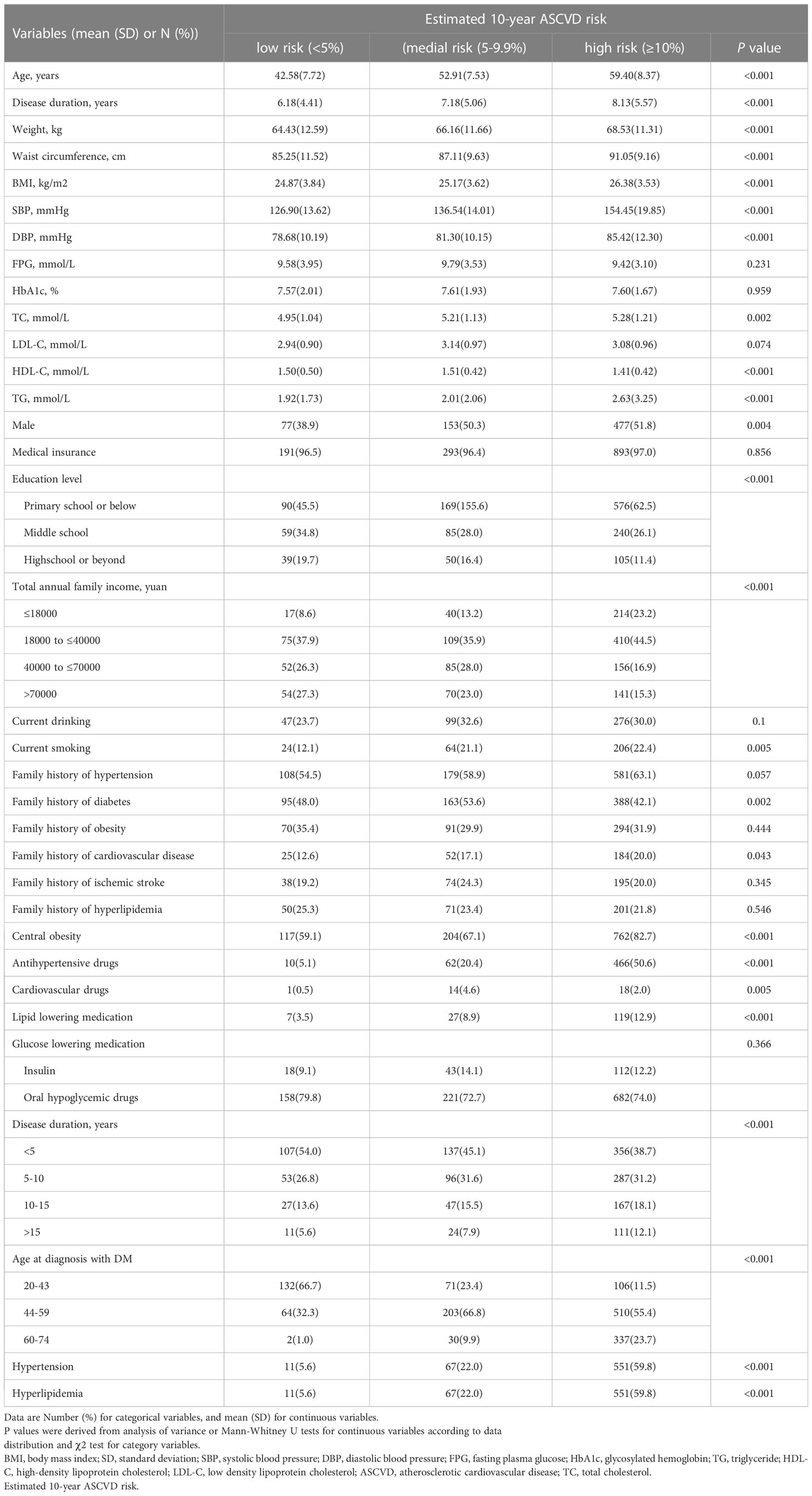
Table 4 Characteristics of the participants with diabetes mellitus stratified by estimated 10-year ASCVD risk (%).
3.5 Risk factors of the high risk of estimated ten-year ASCVD in participants with DM
The risk of estimated 10-year ASCVD was different among the three groups (<5%, 5%-9.9%, ≥10%: 13.9% vs. 21.4% vs. 64.7%, P<0.001). With regard to risk factors associated with high risk of 10-year ASCVD in participants with DM, aged over 65 (OR, 10.192; 95% CI, 6.188 to 16.788; P<0.001), central obesity (OR,1.992; 95% CI, 1.361 to 2.914; P<0.001), hypertension (OR, 18.816; 95% CI, 7.286 to 48.592; P<0.001), hyperlipidemia (OR, 1.366; 95% CI, 1.007 to 1.852; P = 0.045) were independently associated with the high risk of estimated ten-year ASCVD in participants with DM. Compared to those with a diabetes duration of ≤15 years, a diabetes duration of >15 years was associated with increased high risk of estimated ten-year ASCVD in in participants with DM (OR, 1.976; 95% CI, 1.156 to 3.377; P = 0.013). Compared to those without using cardiovascular and antihypertensive drugs, treatment with using above drugs were associated with increased high risk of estimated ten-year ASCVD (OR, 5.184, 95% CI, 1.976 to 13.601; P = 0.001; OR 2.780; 95%CI, 1.047 to 7.384; P = 0.040). No interactions was observed between BMI, family history of ASCVD, age at diagnosis, and patients with diabetes duration 5–10 years, 10–15 years and the age at diagnosis (all P >0.05) (Table 5).
4 Discussions
In this population-based study, we have described the risks for diabetes related complications, and how this varies by attained age, BMI, WC, hypertension, hyperlipidemia, duration of diabetes, age at diagnosis, and family history of ischemic stroke and coronary heart disease. Several factors increase the risk of heart attack, such as hyperglycaemia, obesity, abnormal cholesterol levels, hypertension, and smoking (20).
Participants who were diagnosed with early-onset (age ≤43 years) had higher FPG and HbA1c level than those diagnosed at older ages (aged 44 to 74 years). Most complications in patients with DM are associated with hyperglycaemia, which are important components of metabolic syndrome and may be the early manifestations of insulin resistance (25). Hyperglycaemia can induce oxidative stress in the vasculature, leading to disruption of the normal endothelial function and impaired relaxation of the arterial vascular smooth muscle cells (26). Hyperglycaemia also leads to excessive production of advanced glycation end products and cytokines, which cause activation of adhesion molecules and thickening of intima media (27). Vascular endothelial dysfunction and adhesion activation are also related to hypertension (28), dyslipidemia and diabetic cardiomyopathy (29). Individuals with early-onset diabetes have accompanying metabolic risk factors similar to, or even worse than, those of individuals with late-onset diabetes. For early-onset patients with diabetes, effective glycemic control may contribute to hyperglycaemic episodes, treatment of dyslipidemia, hypertension, obesity, therefore, counteract both microvascular and macrovascular complications of diabetes. Although glucose levels can be controlled through diet, exercise and medications including insulin and oral hypoglycemic agents, many patients continue to undergo numerous life-threatening complications following glucose normalization, suggesting the persistent detrimental effects of high glucose exposure through metabolic memory even after glycaemic control has been established (30, 31). Moreover, the landmark Diabetes Control and Complications Trial (DCCT) confirmed that the damage of hyperglycaemia to microvessels can be delayed for a long time after intensive glycaemic control (32).
Several studies have shown that diabetes duration leads to atherosclerotic lesions, including intimal thickness and thin cap fibroatheromas, which contribute to the deleterious effects on small and large vessels and lead to the development of cardiovascular disease and mortality (12, 33, 34). Further study suggested that diabetes duration during adulthood was associated with coronary artery calcified plaque and left ventricular systolic and diastolic dysfunction in later life, suggesting that the cumulative exposure to chronic hyperglycemia may lead to increased risk of atherosclerosis and impaired cardiac function (35). Our study identified that increasing duration increased the high risk of estimated ten-year ASCVD. These studies are backed up by data from a large population based study from the UK Biobank, which identified that duration of diabetes was independently associated with a greater risk of CVD, myocardial infarction and stroke (36). Further study takes the findings to a broader population based scale where they showed that increasing duration and late-stage complications of DM increase the associated risk of infective endocarditis (37).
We also observed hypertension and hyperdemia were independent risk factors for high risk of estimated 10-year ASCVD in patients with diabetes. As highlighted in the study, ASCVD was prone to occur in the patients with the agedness, central obesity, longer diabetes duration, hypertension and hyperlipidemia. Previous study found that diabetic dyslipidemia precedes T2DM by several years, and lipid abnormalities were associated with an increased risk of CVD (38). Some scholars emphasized that diabetes patients are commonly accompanied by lipid metabolism disorder and hyperlipidemia due to the dysfunction of insulin biological regulation (39). On the one hand, insulin resistance can lead to blood glucose fluctuation and chronic hyperglycemia, which in turn triggers oxidative stress and increases the expression of pro-inflammatory factors and pro-coagulant factors that leads to cell damage (40). On the other hand, insulin resistance can induce an imbalance in lipoproteins profle alterations that contributes to the development of dyslipidemia and the lipid triad (41). The abnormal association between insulin resistance and endothelial signal conduction disorder leads to inflammation, which further disrupts the balance between endothelial vasodilator and vasoconstrictor mechanisms, and leads to the formation of atherosclerotic plaque (40, 42). New therapies focused on decreasing insulin resistance may be investigated as a potential future therapeutic target for mitigating both CVD and atherosclerotic plaque generation.
Compared to those patients with DM who have’t been diagnosed as ASCVD, the high risk of estimated 10-year ASCVD in DM patients treatment with antihypertensive drugs is estimated to increase up to 3-times, and the high risk level is 5-times higher than without using cardiovascular drugs. It’s well known that both antihypertensive drugs and cardiovascular drugs are perfect preventive medications for ASCVD in high-risk patients with DM. Obviously, we may arrive at a conclusion that high-risk population are more willing to take antihypertensive drugs and cardiovascular drugs under medical advice. These findings advance the arguments for wider and earlier use of China-PAR model in this population and provide important practical value for the prevention of cardiovascular diseases in diabetic patients. However, the data of patients using cardiovascular drugs in the analysis model is so small that can’t reflect the real world impact of all diabetes patients after receiving cardiovascular drug treatment.
The patients with early-onset DM were characterized by a higher level of BMI and weight, and were more likely to have obesity than older-onset DM. As an important indicator to reflect the obesity, BMI can evaluate the severity of insulin resistance in obese DM patients. Obesity increased the risk for development of DM and may lead to an earlier age of diagnosis (43, 44). Our analysis is consistent with these findings. The significant proportion of metabolic disorders and insulin resistance among patients with early-onset DM, and the risk for development of macrovascular complications from diabetes is increased among obese individuals with DM (43). Therefore, it is suggested that early-onset DM patients should repair metabolic disorders and ameliorate insulin resistance by reducing weight and BMI as soon as possible.
The results of the present study show that early-onset age of DM increases the risk of macrovascular complications later in life. Compared with late-onset DM, people with early-onset DM have a significantly higher risk of developing macrovascular complications, especially ischemic stroke. Our findings are consistent with those of two previous studies (4, 45). It was found in previous studies that patients diagnosed with early-onset (20-39 years) T2DM had a higher risk of developing cardiovascular disease and a higher cardiac 10-year expected risk than patients with late-onset T2DM (46). These studies all suggested that the impending increase in average duration of diabetes in people with T2DM is likely to increase the burden of coronary artery disease and ischemic stroke. The groups with younger age at diagnosis (age ≤59 years) was independently associated with the risk of macrovascular complications compared to the elderly-onset group (60 to 74 years). These results were similar to other studies. Observational studies showed that patients with younger age at diabetes diagnosis was associated with higher risk of vascular disease (47). And cardiovascular complications were more common in patients with early-onset T2DM at any given age (48). Therefore, early and sustained interventions are essential to delay T2DM onset, and improve blood glucose levels, and cardiovascular risk profiles of those already diagnosed. However, other studies argued that patients with early-onset diabetes are more likely to have microvascular complications than macrovascular complications (11). In the study, the increase in comorbidities of coronary vascular disease and ischemic stroke with age at diagnosis was more pronounced in the elderly-onset (60 to 74 years) than those with younger onset (age ≤59 years). Both age at diagnosis and duration of diabetes affected the risk for coronary artery disease and ischemic stroke, but the relative impact was different for each. For ischemic stroke, the incidence risk was primarily driven by disease duration and age at diagnosis, which led to the relative risk of people with different diabetes duration at a given age. However, these relative risks were smaller for coronary artery disease, indicating less of an effect of duration of diabetes and more so of age at diagnosis than for ischemic stroke.
Our findings should be interpreted in light of the strengths and limitations of our study. The strengths of this work include that data were derived from a large, multi-center and multi-level design cohort of patients with diabetes, and had comprehensive clinical implications for diabetes complications. our study found that people with early-onset diabetes had a high risk of complications, indicating diabetes-related complications will increasingly occur in people of working age, which may result in substantial healthcare burden. It is essential to intensified efforts to prevent these complications. We first used the China-PAR project to predict the ten-year ASCVD in the study, which will help to improve primary prevention of macrovascular complications. The China-PAR project developed based on the recent epidemics of CVD and risk factors will be better to identify high risk individuals with appropriately predicted risk probability, and to evaluate ASCVD outcome with standardized review process, using the same diagnosis criteria across cohorts.
The present study had some limitations. First, information on coronary heart disease and cerebrovascular disease was collected from the questionnaire, which is similar to most other epidemiological studies (49). However, it is not practical to measure coronary heart disease and cerebrovascular disease by equipment in a large-scale study. Second, previous studies show that younger age at diabetes diagnosis was associated with high risk of macrovascular and microvascular disease (47). The diabetes duration has been thought to be an noteworthy factor, absent of the ability to quantify the effects of duration of diabetes after the diagnosis of diabetes. Longer periods of follow-up may be need to be carried out among participants. It is a great pity that numbers of clinical events and kinds of complications were present in small amounts. Patients were grouped according to their age at onset, but for asymptomatic patients, the age onset and disease duration might be underestimated. However, in view of the similarity between our cohort and the cohort of patients with diabetes observed by other teams, we still believe that our findings are somewhat universal and comparable among onset-age groups (10, 12, 47). Furthermore, this was a cross-sectional study in four cities that does not represent broad sections of the people with diabetes at different region cross the country. In addition, several limitations should be addressed in our study when using the China-PAR modeling. Firstly, the project is aimed to develop and validate 10-year risk prediction equations for ASCVD from all Chinese participants, not diabetes patients. Thus, cautions should be used and training among physicians is required to communicate predicted 10-year risk of ASCVD to patients when the modeling are applied in prevention practice. Secondly, further investigation is warranted to examine whether the 10-year risk prediction modeling could have good performance in large-scale cohorts with short durations of follow-up.
5 Conclusions
The present study demonstrated that higher FPG and HbA1c according to disease duration were observed in patients diagnosed at early-onset age than those diagnosed at older age. Age at diagnosis and diabetes duration, hypertension and hyperlipidemia were associated with an increased risk of macrovascular events and high risk of ten-year ASCVD prediction. Further prospective cohort studies are necessary to examine our findings in large-scale populations.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
Ethics statement
The studies involving human participants were reviewed and approved by the Ethical Review Committee (Approval No: 2018-010). The patients/participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
QZ, HH, and FD designed and proposed the study. XY, JZ, XZ, TJ, and YZ collected the patients’ data. XY prepared and drafted the manuscript. JZ and XZ analyzed and illustrated the data. YZ and TJ revised the paper. All authors have read and approved the manuscript. In addition, we confirm that all listed authors meet the authorship criteria and that all authors are in agreement with the content of the manuscript. All authors contributed to the article and approved the submitted version.
Funding
This study was supported by a research grant from the National Natural Science Foundation of China (grant number: 81970703).
Acknowledgments
We thank all the investigators and participants for their contributions to this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviation
DM, Diabetes mellitus; CVD, Cardiovascular disease; ASCVD, Atherosclerotic cardiovascular disease; China-PAR, The Prediction for ASCVD Risk in China project; FPG, Fasting plasma glucose; HbA1c, Glycosylated hemoglobin; OR, odds ratio; 95% CI, 95 percent confidence interval; T2DM, Type 2 diabetes mellitus; China DiaChronic Study, The China National Diabetic Chronic Complications Study; DSPs, Disease surveillance points; CCDRFS, The China Chronic Disease and Risk Factors Surveillance; WC, Waist circumference; BMI, Body mass index; SBP, Systolic blood pressure; DBP, Diastolic blood pressure; TC, Total cholesterol; TG, Triglycerides; HDL-C, High-density lipoprotein cholesterol; LDL-C, Low-density lipoprotein cholesterol.
References
1. Sun H, Saeedi P, Karuranga S, Pinkepank M, Ogurtsova K, Duncan BB, et al. IDF diabetes atlas: global, regional and country-level diabetes prevalence estimates for 2021 and projections for 2045. Diabetes Res Clin Pract (2022) 183:109119. doi: 10.1016/j.diabres.2021.109119
2. Ali MK, Pearson-Stuttard J, Selvin E, Gregg EW. Interpreting global trends in type 2 diabetes complications and mortality. Diabetologia (2022) 65(1):3–13. doi: 10.1007/s00125-021-05585-2
3. Yousri NA, Suhre K, Yassin E, Al-Shakaki A, Robay A, Elshafei M, et al. Metabolic and metabo-clinical signatures of type 2 diabetes, obesity, retinopathy, and dyslipidemia. Diabetes (2022) 71(2):184–205. doi: 10.2337/db21-0490
4. Yusuf S, Joseph P, Rangarajan S, Islam S, Mente A, Hystad P, et al. Modifiable risk factors, cardiovascular disease, and mortality in 155 722 individuals from 21 high-income, middle-income, and low-income countries (PURE): a prospective cohort study. Lancet (2020) 395(10226):795–808. doi: 10.1016/S0140-6736(19)32008-2
5. Tancredi M, Rosengren A, Svensson AM, Kosiborod M, Pivodic A, Gudbjörnsdottir S, et al. Excess mortality among persons with type 2 diabetes. N Engl J Med (2015) 373(18):1720–32. doi: 10.1056/NEJMoa1504347
6. van Sloten TT, Sedaghat S, Carnethon MR, Launer LJ, Stehouwer CDA. Cerebral microvascular complications of type 2 diabetes: stroke, cognitive dysfunction, and depression. Lancet Diabetes Endocrinol (2020) 8(4):325–36. doi: 10.1016/S2213-8587(19)30405-X
7. Sarwar N, Gao P, Seshasai SR, Gobin R, Kaptoge S, Di Angelantonio E, et al. Diabetes mellitus, fasting blood glucose concentration, and risk of vascular disease: a collaborative meta-analysis of 102 prospective studies. Lancet (2010) 375(9733):2215–22.
8. Lee M, Saver JL, Hong KS, Song S, Chang KH, Ovbiagele B. Effect of pre-diabetes on future risk of stroke: meta-analysis. Bmj (2012) 344:e3564. doi: 10.1136/bmj.e3564
9. Cummings DM, Kirian K, Howard G, Howard V, Yuan Y, Muntner P, et al. Consequences of comorbidity of elevated stress and/or depressive symptoms and incident cardiovascular outcomes in diabetes: results from the REasons for geographic and racial differences in stroke (REGARDS) study. Diabetes Care (2016) 39(1):101–9. doi: 10.2337/dc15-1174
10. Morton JI, Lazzarini PA, Polkinghorne KR, Carstensen B, Magliano DJ, Shaw JE.. The association of attained age, age at diagnosis, and duration of type 2 diabetes with the long-term risk for major diabetes-related complications. Diabetes Res Clin Pract (2022) 190:110022. doi: 10.1016/j.diabres.2022.110022
11. Huang L, Wu P, Zhang Y, Lin Y, Shen X, Zhao F, et al. Relationship between onset age of type 2 diabetes mellitus and vascular complications based on propensity score matching analysis. J Diabetes Investig (2022) 13(6):1062–72. doi: 10.1111/jdi.13763
12. Zoungas S, Woodward M, Li Q, Cooper ME, Hamet P, Harrap S, et al. Impact of age, age at diagnosis and duration of diabetes on the risk of macrovascular and microvascular complications and death in type 2 diabetes. Diabetologia (2014) 57(12):2465–74. doi: 10.1007/s00125-014-3369-7
13. Huang JX, Liao YF, Li YM. Clinical features and microvascular complications risk factors of early-onset type 2 diabetes mellitus. Curr Med Sci (2019) 39(5):754–8. doi: 10.1007/s11596-019-2102-7
14. Hou XH, Wang LM, Chen SY, Liang YB, Zhang M, Huang ZJ, et al. Data resource profile: a protocol of China national diabetic chronic complications study. BioMed Environ Sci (2022) 35(7):633–40.
15. Liu S, Wu X, Lopez AD, Wang L, Cai Y, Page A, et al. An integrated national mortality surveillance system for death registration and mortality surveillance, China. Bull World Health Organ (2016) 94(1):46–57. doi: 10.2471/BLT.15.153148
16. Zhao ZP, Wang LM, Li YC, Jiang Y, Zhang M, Huang ZJ, et al. [Provincial representativeness assessment of China non-communicable and chronic disease risk factor surveillance system in 2013]. Zhonghua Yu Fang Yi Xue Za Zhi (2018) 52(2):165–9.
17. Yang X, Li J, Hu D, Chen J, Li Y, Huang J, et al. Predicting the 10-year risks of atherosclerotic cardiovascular disease in Chinese population: the China-PAR project (Prediction for ASCVD risk in China). Circulation (2016) 134(19):1430–40. doi: 10.1161/CIRCULATIONAHA.116.022367
18. Yang XL, Chen JC, Li JX, Cao J, Lu XF, Liu FC, et al. Risk stratification of atherosclerotic cardiovascular disease in Chinese adults. Chronic Dis Transl Med (2016) 2(2):102–9. doi: 10.1016/j.cdtm.2016.10.001
19. Huang K, Liang F, Yang X, Liu F, Li J, Xiao Q, et al. Long term exposure to ambient fine particulate matter and incidence of stroke: prospective cohort study from the China-PAR project. Bmj (2019) 367:l6720. doi: 10.1136/bmj.l6720
20. Li Y, Teng D, Shi X, Qin G, Qin Y, Quan H, et al. Prevalence of diabetes recorded in mainland China using 2018 diagnostic criteria from the American diabetes association: national cross sectional study. Bmj (2020) 369:m997. doi: 10.1136/bmj.m997
21. Flegal KM. BMI and obesity trends in Chinese national survey data. Lancet (2021) 398(10294):5–7. doi: 10.1016/S0140-6736(21)00892-8
22. Zhang L, Wang Z, Wang X, Chen Z, Shao L, Tian Y, et al. Prevalence of abdominal obesity in China: results from a cross-sectional study of nearly half a million participants. Obes (Silver Spring) (2019) 27(11):1898–905. doi: 10.1002/oby.22620
23. Whelton PK, Carey RM, Aronow WS, Casey DE Jr, Collins KJ, Dennison Himmelfarb C, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American college of Cardiology/American heart association task force on clinical practice guidelines. Hypertension (2018) 71(6):e13–e115.
24. China Cholesterol education program (CCEP) expert advice for the management of dyslipidaemias to reduce cardiovascular risk (2019). Zhonghua Nei Ke Za Zhi (2020) 59(1):18–22.
25. Irving R, Tusié-Luna MT, Mills J, Wright-Pascoe R, McLaughlin W, Aguilar-Salinas CA, et al. Early onset type 2 diabetes in Jamaica and in mexico. opportunities derived from an interethnic study. Rev Invest Clin (2011) 63(2):198–209.
26. Fiorentino TV, Prioletta A, Zuo P, Folli F. Hyperglycemia-induced oxidative stress and its role in diabetes mellitus related cardiovascular diseases. Curr Pharm Des (2013) 19(32):5695–703. doi: 10.2174/1381612811319320005
27. Vlassara H, Uribarri J. Advanced glycation end products (AGE) and diabetes: cause, effect, or both? Curr Diabetes Rep (2014) 14(1):453. doi: 10.1007/s11892-013-0453-1
28. Dikalova AE, Pandey A, Xiao L, Arslanbaeva L, Sidorova T, Lopez MG, et al. Mitochondrial deacetylase Sirt3 reduces vascular dysfunction and hypertension while Sirt3 depletion in essential hypertension is linked to vascular inflammation and oxidative stress. Circ Res (2020) 126(4):439–52. doi: 10.1161/CIRCRESAHA.119.315767
29. Knapp M, Tu X, Wu R. Vascular endothelial dysfunction, a major mediator in diabetic cardiomyopathy. Acta Pharmacol Sin (2019) 40(1):1–8. doi: 10.1038/s41401-018-0042-6
30. de Boer IH. Kidney disease and related findings in the diabetes control and complications trial/epidemiology of diabetes interventions and complications study. Diabetes Care (2014) 37(1):24–30. doi: 10.2337/dc13-2113
31. Kato M, Natarajan R. Epigenetics and epigenomics in diabetic kidney disease and metabolic memory. Nat Rev Nephrol (2019) 15(6):327–45. doi: 10.1038/s41581-019-0135-6
32. Home P. Contributions of basal and post-prandial hyperglycaemia to micro- and macrovascular complications in people with type 2 diabetes. Curr Med Res Opin (2005) 21(7):989–98. doi: 10.1185/030079905X49662
33. Li FR, Yang HL, Zhou R, Zheng JZ, Chen GC, Zou MC, et al. Diabetes duration and glycaemic control as predictors of cardiovascular disease and mortality. Diabetes Obes Metab (2021) 23(6):1361–70. doi: 10.1111/dom.14348
34. Casanova F, Adingupu DD, Adams F, Gooding KM, Looker HC, Aizawa K, et al. The impact of cardiovascular co-morbidities and duration of diabetes on the association between microvascular function and glycaemic control. Cardiovasc Diabetol (2017) 16(1):114. doi: 10.1186/s12933-017-0594-7
35. Reis JP, Allen NB, Bancks MP, Carr JJ, Lewis CE, Lima JA, et al. Duration of diabetes and prediabetes during adulthood and subclinical atherosclerosis and cardiac dysfunction in middle age: the CARDIA study. Diabetes Care (2018) 41(4):731–8. doi: 10.2337/dc17-2233
36. de Jong M, Woodward M, Peters SAE. Duration of diabetes and the risk of major cardiovascular events in women and men: a prospective cohort study of UK biobank participants. Diabetes Res Clin Pract (2022) 188:109899. doi: 10.1016/j.diabres.2022.109899
37. Østergaard L, Mogensen UM, Bundgaard JS, Dahl A, Wang A, Torp-Pedersen C, et al. Duration and complications of diabetes mellitus and the associated risk of infective endocarditis. Int J Cardiol (2019) 278:280–4. doi: 10.1016/j.ijcard.2018.09.106
38. Fan D, Li L, Li Z, Zhang Y, Ma X, Wu L, et al. Effect of hyperlipidemia on the incidence of cardio-cerebrovascular events in patients with type 2 diabetes. Lipids Health Dis (2018) 17(1):102. doi: 10.1186/s12944-018-0676-x
39. Beverly JK, Budoff MJ. Atherosclerosis: pathophysiology of insulin resistance, hyperglycemia, hyperlipidemia, and inflammation. J Diabetes (2020) 12(2):102–4. doi: 10.1111/1753-0407.12970
40. Ormazabal V, Nair S, Elfeky O, Aguayo C, Salomon C, Zuñiga FA. Association between insulin resistance and the development of cardiovascular disease. Cardiovasc Diabetol (2018) 17(1):122. doi: 10.1186/s12933-018-0762-4
41. Jin JL, Zhang HW, Cao YX, Liu HH, Hua Q, Li YF, et al. Association of small dense low-density lipoprotein with cardiovascular outcome in patients with coronary artery disease and diabetes: a prospective, observational cohort study. Cardiovasc Diabetol (2020) 19(1):45. doi: 10.1186/s12933-020-01015-6
42. Balakrishnan B, Gupta A, Basri R, Sharma VM, Slayton M, Gentner K, et al. Endothelial-specific expression of CIDEC improves high-fat diet-induced vascular and metabolic dysfunction. Diabetes (2023) 72(1):19–32. doi: 10.2337/db22-0294
43. Polemiti E, Baudry J, Kuxhaus O, Jäger S, Bergmann MM, Weikert C, et al. BMI and BMI change following incident type 2 diabetes and risk of microvascular and macrovascular complications: the EPIC-potsdam study. Diabetologia (2021) 64(4):814–25. doi: 10.1007/s00125-020-05362-7
44. Islam ST, Srinivasan S, Craig ME. Environmental determinants of type 1 diabetes: a role for overweight and insulin resistance. J Paediatr Child Health (2014) 50(11):874–9. doi: 10.1111/jpc.12616
45. Huo X, Gao L, Guo L, Xu W, Wang W, Zhi X, et al. Risk of non-fatal cardiovascular diseases in early-onset versus late-onset type 2 diabetes in China: a cross-sectional study. Lancet Diabetes Endocrinol (2016) 4(2):115–24. doi: 10.1016/S2213-8587(15)00508-2
46. Kim SM, Lee G, Choi S, Kim K, Jeong SM, Son JS, et al. Association of early-onset diabetes, prediabetes and early glycaemic recovery with the risk of all-cause and cardiovascular mortality. Diabetologia (2020) 63(11):2305–14. doi: 10.1007/s00125-020-05252-y
47. Nanayakkara N, Curtis AJ, Heritier S, Gadowski AM, Pavkov ME, Kenealy T, et al. Impact of age at type 2 diabetes mellitus diagnosis on mortality and vascular complications: systematic review and meta-analyses. Diabetologia (2021) 64(2):275–87. doi: 10.1007/s00125-020-05319-w
48. Yeung RO, Zhang Y, Luk A, Yang W, Sobrepena L, Yoon KH, et al. Metabolic profiles and treatment gaps in young-onset type 2 diabetes in Asia (the JADE programme): a cross-sectional study of a prospective cohort. Lancet Diabetes Endocrinol (2014) 2(12):935–43. doi: 10.1016/S2213-8587(14)70137-8
Keywords: diabetes mellitus, cardiovascular disease, diabetes duration, age at diagnosis, macrovascular complications
Citation: Yao X, Zhang J, Zhang X, Jiang T, Zhang Y, Dai F, Hu H and Zhang Q (2023) Age at diagnosis, diabetes duration and the risk of cardiovascular disease in patients with diabetes mellitus: a cross-sectional study. Front. Endocrinol. 14:1131395. doi: 10.3389/fendo.2023.1131395
Received: 25 December 2022; Accepted: 17 April 2023;
Published: 08 May 2023.
Edited by:
Gaetano Santulli, Albert Einstein College of Medicine, United StatesReviewed by:
Yijun Lin, Xiamen University Affiliated Cardiovascular Hospital, ChinaMin Xu, Chang Zhou No.1 Hospital, China
Copyright © 2023 Yao, Zhang, Zhang, Jiang, Zhang, Dai, Hu and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Honglin Hu, aHVob25nbGluQGFobXUuZWR1LmNu; Qiu Zhang, emhhbmdxaXVAYWhtdS5lZHUuY24=
 Xuelin Yao
Xuelin Yao Jie Zhang
Jie Zhang Qiu Zhang
Qiu Zhang