
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Endocrinol. , 01 February 2023
Sec. Adrenal Endocrinology
Volume 14 - 2023 | https://doi.org/10.3389/fendo.2023.1119251
This article is part of the Research Topic Cross-Talk and Interaction between Endocrinology and Urology: Challenges and Opportunities View all 24 articles
Objective: To compare the efficacy and safety between conservative treatment and surgery for the patients with small (1-3cm) nonfunctional adrenal incidentaloma (NFAI).
Methods: The patients with small (1-3cm) NFAI who received conservative treatment or surgery in our hospital from November 2018 to December 2019 were retrospectively collected. A total of 83 patients were included in this study. They were divided into two groups according to the treatment methods: the surgery group (n=51) and the conservative treatment group (n=32).Then patients’ demographics, tumor characteristics, functional indicators and complications were compared. Statistical analysis was performed using t-test for continuous variables and Pearson chi-square test or Fisher’s exact test for categorical variables.
Results: At the time of diagnosis, after 3 months, after 6 months, after 12 months, and after 24 months, we found that there was no significant difference between the two groups in systolic blood pressure, diastolic blood pressure, serum potassium levels, and hormone levels. 51 patients chose to have surgery, of which 41 patients chose RLA and 10 patients chose RARLA. RARLA group patients had the highest total cost and conservative treatment group patients had the lowest cost, and the difference was significant (P < 0.001). There was no significant difference in tumor size in the conservative treatment group between at the time of diagnosis and after 24 months (P = 0.305).
Conclusion: Surgical treatment is more effective for 1-3cm NFAI, but conservative treatment is safer and more economical. Follow-up after conservative or surgical treatment is necessary.
Adrenal incidentaloma (AI) refers to the adrenal tumor whose diameter ≥ 1cm is accidentally found by imaging examination during physical examination or diagnosis and treatment of other non-adrenal diseases (1, 2). AI is a common disease, accounting for 8.7% of the autopsy population (3). And as people aged, the incidence in the elderly population increased to 10% (4). Approximately 80% of AI are benign and have no endocrine function, while 20% are malignant and have endocrine function (5). Nonfunctional adrenal incidentaloma (NFAI) is adrenal tumor that has no endocrine function at the time of diagnosis, accounting for roughly 75% of all AI (5). Almost all patients with NFAI have no symptoms, but one study found a 41% long-term incidence of hypertension in patients with NFAI (6). Due to the fact that NFAI is mostly benign, and considering the trauma and risk of surgery, a basic consensus in the past has been to recommend conservative treatment for tumors between 1 and 3cm with no endocrine function (1, 7). However, with the development of minimally invasive concept and the progress of surgical technology and equipment, the trauma and risk of surgery gradually decreased (8, 9). Doctors and patients are becoming increasingly concerned about the tumor’s malignant potential, the potential for hormone secretion, and the potential close relationship with hypertension. Patients with small adrenal tumors discovered in an outpatient clinic are increasingly requesting or being recommended surgical treatment. However, for these small NFAI, conservative treatment or surgical treatment is still being discussed by endocrinologists and urologists.
In order to compare the efficacy and safety of conservative treatment and surgical treatment for these patients with small NFAI, we carried out this study. We hope to provide new data for the treatment of these patients through this study.
Our prospectively maintained database was retrospectively scrutinized to acquire details regarding the baseline demographic and clinical information after obtaining the approval of the institutional review board and ethics committee of the First Affiliated Hospital of Nanchang University.
The patients with small (1-3cm) NFAI who received conservative treatment or surgery in our hospital from November 2018 to December 2019 were retrospectively collected. The patients were included in this analysis according to the following inclusion criteria: [1] Patients diagnosed as adrenal tumor; [2] The tumor size was 1-3 cm; [3] Unilateral tumor; [4] At the initial diagnosis, the serum potassium was between 3.5-5.5 mmol/L; [5] the levels of aldosterone, cortisol and VMA were within the normal range. The exclusion criteria were as follows: [1] During hospitalization, other operations other than adrenalectomy were performed; [2] systolic blood pressure exceeded 140 mmHg at initial diagnosis; [3] diastolic blood pressure exceeded 90 mmHg at initial diagnosis; [4] accompanied by other serious complications.
Patients in the conservative treatment group did not receive any medical or lifestyle interventions. All the patients in the surgery group were operated by the same medical team, and the surgical methods were divided into retroperitoneal laparoscopic adrenalectomy (RLA) and robot assisted laparoscopic adrenalectomy (RARLA) according to the characteristics of the tumor. All patients underwent follow-up examinations at 3, 6, 12 and 24 months after diagnosis or surgery. All patients were asked to sign an informed consent form.
Variables in the study include demographic characteristics (age, sex, body mass index (BMI)), serum potassium level, blood pressure level, hormone level (aldosterone, cortisol, Urine Vanilla Amygdalic Acid (VMA)), tumor characteristics (tumor size, tumor site), treatment methods (surgical treatment, waiting for observation), and other variables (total cost).
The primary end points of this study were to compare the average differences in tumor size, blood pressure and hormone levels between the surgery group and the conservative treatment group at the time of diagnosis, after 3 months, after 6 months, after 12 months, and after 24 months. The secondary endpoint was the total cost of the two groups, which was defined as the cost of hospitalization and outpatient services.
Means and standard deviations were determined for the normally distributed continuous variables, while those with nonnormal distribution were presented as median and interquartile range. Categorical variables were presented as frequencies and their proportions. The Student’s t-test was performed for the normally distributed continuous variables. The Mann-Whitney test was employed to analyze VMA between the surgery group and the conservative treatment group. Analysis of variance was used to compare the total cost among conservative treatment, Retroperitoneal laparoscopic adrenalectomy (RLA) and Robot assisted laparoscopic adrenalectomy (RARLA) groups. All categorical variables were compared with the Chi square test. SPSS 26.0 (IBM Corp, Armonk, NY) was utilized for all statistical analysis with a two-sided p value < 0.05 denoting statistical significance.
According to the inclusion and exclusion criteria, 81 patients were included in this study from November 2018 to December 2019. Thirty-two patients with unilateral nonfunctioning adrenal incidentaloma chose conservative treatment, while 51 patients chose to undergo surgery, of which 41 patients chose RLA, and 10 patients chose RARLA. There was no significant difference in baseline characteristics between the two groups (Table 1).
By comparing the average difference between the two groups of patients at the time of diagnosis, after 3 months, after 6 months, after 12 months, and after 24 months, we found that there was no significant difference between the two groups in systolic blood pressure, diastolic blood pressure, serum potassium levels, and hormone levels (Table 2). After 24 months, only 2 (3.9%) patients in the surgery group had an increase in aldosterone, while the conservative treatment group was 3 (9.4%). However, 2 (3.9%) patients in the surgery group had increased cortisol, compared with 4 (12.5%) in the conservative treatment group.
51 patients chose to have surgery, of which 41 patients chose RLA and 10 patients chose RARLA. We compared the total cost of conservative treatment, RLA and RARLA groups and found that RARLA groups patients had the highest total cost and conservative treatment groups patients had the lowest cost, and the difference was significant (P < 0.001) (Figure 1). There was no significant difference in tumor size in the conservative treatment group between at the time of diagnosis and after 24 months (P = 0.305) (Figure 2).
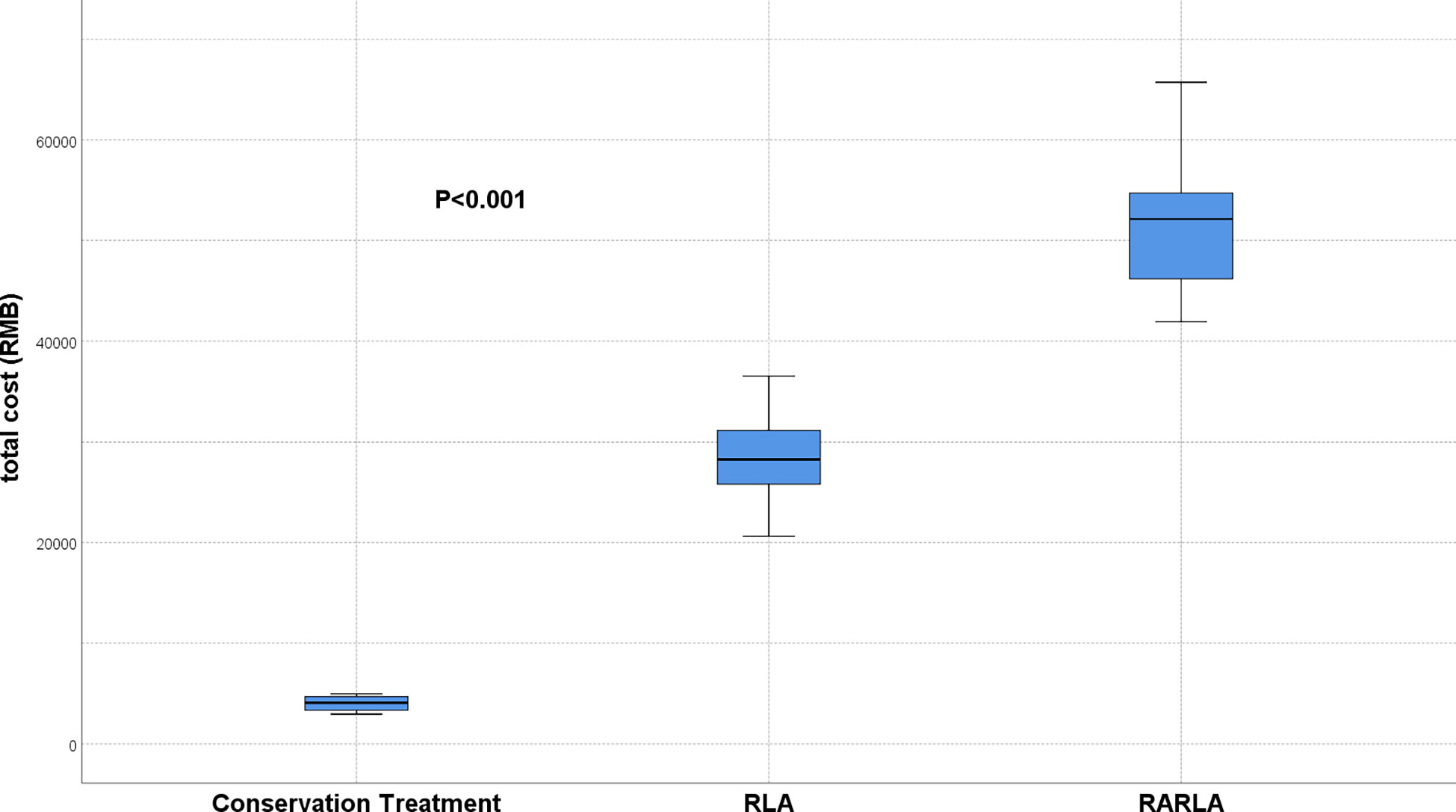
Figure 1 Comparison of total costs in the conservative treatment, LPA and RALPA groups. The total costs of conservative treatment was the least, while RALPA was the most.
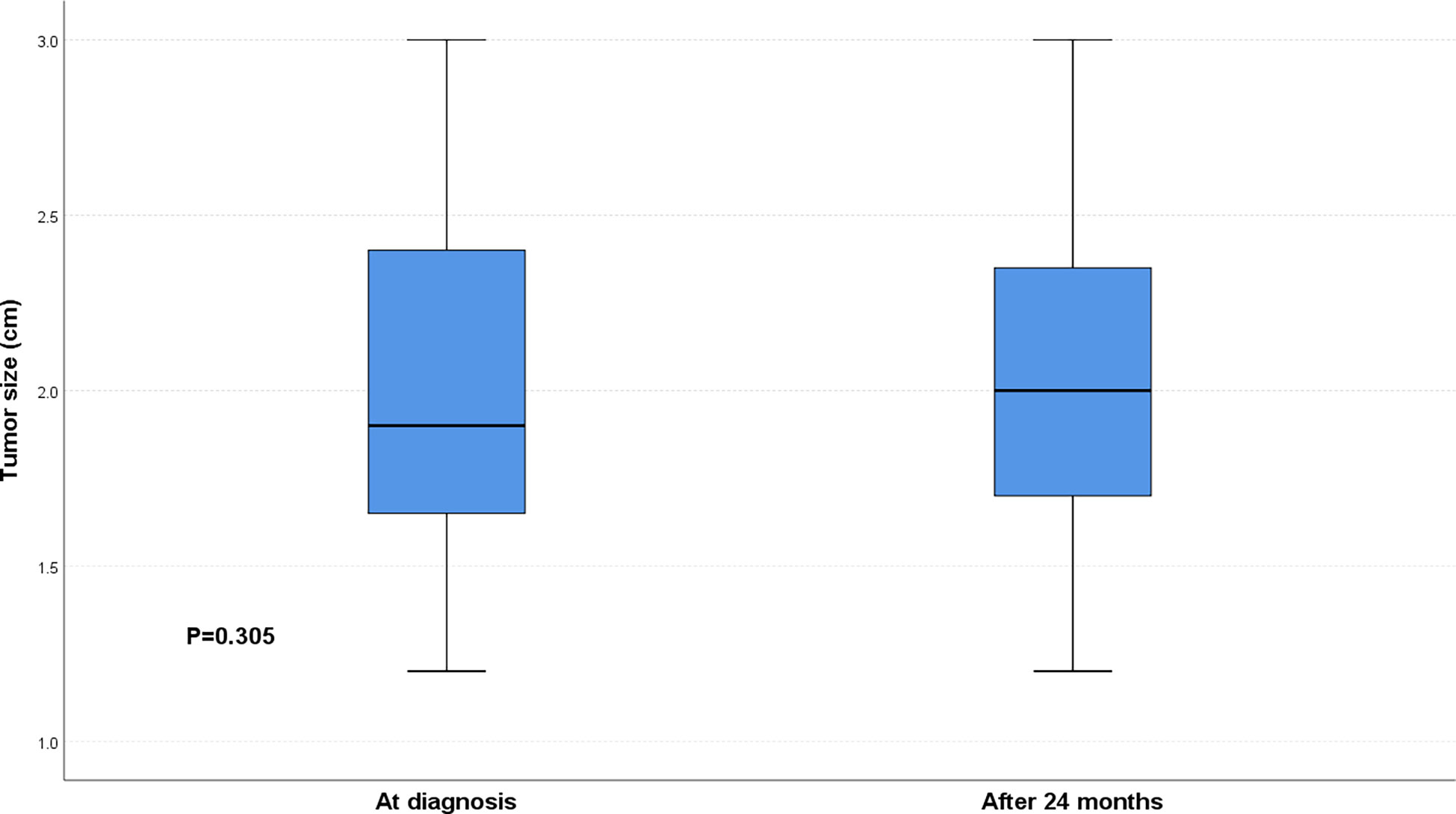
Figure 2 Comparison of tumor size at diagnosis and 24 months later in the conservative treatment group. Within 24 months, patients in the conservative treatment group showed no significant tumor growth.
Physical examination has become a service item accepted by an increasing number of people as people pay more attention to their health. The growing popularity of physical examinations, as well as the accompanying increase in imaging, is a major reason for the rising incidence of adrenal incidentaloma (AI) year after year (10). Nonfunctional adrenal incidentaloma (NFAI) are adrenal tumors that have no endocrine function at the time of diagnosis, accounting for roughly 75% of all adrenal incidentaloma (5). Although most NFAI are benign and non-functional, with no obvious clinical symptoms, it has become an important disease affecting human health, attracting the long-term attention of endocrinologists and urologists due to its relatively high incidence in the population and the potential for malignant lesions (3, 4, 11). Endocrinologists and urologists share the goal of finding an effective, safe, and cost-effective treatment.
Previously, the general consensus was to surgically resect NFAI larger than 3cm and to treat tumors smaller than 3cm conservatively (7). Of course, as with other types of tumors, size is not the sole determinant of treatment. Another general agreement is that when a NFAI becomes functional or significantly grows in size during conservative treatment, surgical treatment is a better option than conservative treatment (10, 12).
However, as research on NFAI progresses, its potential impact on people’s health becomes clearer. NFAI, on the one hand, are thought to be risk factors for cardiovascular disease. Tuna (13) compared the prevalence of hypertension in the general population to patients with NFAI in one study. The study’s findings revealed that the incidence of hypertension in patients with NFAI was significantly higher than in the general population. Furthermore, Cansu and his colleagues revealed in a paper that NFAI can increase patients’ cardiovascular risk, and that this effect may be related to carotid intima media thickness (CIMT), pulse wave velocity (PWV), augmentation index (AIx) (14). This viewpoint was supported by Emral’s research (15). NFAI, on the other hand, are thought to be closely related to metabolic disorders. Ribeiro Cavalari (16) compared the prevalence of metabolic syndrome in NFAI to that of the general population in one study. The incidence of NFAI was 69.2% versus 31.0% in the general population, indicating a significant difference between the two. In another study, patients with NFAI were found to have a higher risk of insulin resistance and diabetes (17). Furthermore, NFAI can cause a decrease in serum adiponectin levels as well as an (17) increase in blood lipid levels, affecting bone metabolism (18) and the appearance of periodontal disease (19).
According to the above studies, even if the NFAI does not have significant cortisol and aldosterone overproduction, it can still have a negative impact on our health in a variety of ways. This appears to imply that early surgical treatment for patients with NFAI can prevent further damage. Our findings appear to support this viewpoint, with increased aldosterone and cortisol occurring in 3.9% of the surgery group after 2 years, compared to 9.4% and 12.5% in the conservative group, respectively. Although our findings did not indicate hypertension in the conservative treatment group, this could be due to the shorter follow-up period.
Safety and cost are also important considerations in treatment selection. Conservative treatment for small NFAI was previously recommended because it was safer and less expensive than surgery. However, with the introduction of laparoscopic (8) and Da Vinci surgical robots (9), the risk of surgery has decreased significantly. That is one of the reasons why an increasing number of patients are undergoing surgery. Of course, the risk of surgery remains higher than the risk of conservative treatment; after all, surgery is a traumatic procedure. Our findings show that conservative treatment is more cost-effective, whereas patients undergoing robot-assisted abdominal surgery as part of the surgical approach face greater financial strain.
In conclusion, for patients with 1-3cm NFAI, surgical treatment is more appropriate in terms of therapeutic effect. Conservative treatment may be an option if safety or economic factors are taken into account; after all, as our study demonstrated, conservative treatment did not significantly increase the size of the tumor within two years.
Surgical treatment is more effective for 1-3cm NFAI, but conservative treatment is safer and more economical. Follow-up after conservative or surgical treatment is necessary.
The original contributions presented in the study are included in the article/Supplementary Material. Further inquiries can be directed to the corresponding authors.
The studies involving human participants were reviewed and approved by the Ethical Committee of The First Affiliated Hospital of Nanchang University. The patients/participants provided their written informed consent to participate in this study.
Conception and design: GW and XCZ. Surgeons: GW and XCZ. Acquisition of data: SX and XPZ. Preparation of tools: YY and CZ. Analysis and interpretation of data: XL and XPZ. Drafting of the manuscript and statistical analysis: XL and SX. Critical revision: GW and HX. Obtaining funding: XCZ and HX. All authors contributed to the article and approved the submitted version.
Key Research and Development Program of Jiangxi Province (20171ACB20029 to XZ). Applied Research and Cultivation Program of Jiangxi Province (20212BAG70001 to HX).
Thanks to HX and GW for providing suggestions for the writing of the article.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Fassnacht M, Arlt W, Bancos I, Dralle H, Newell-Price J, Sahdev A, et al. Management of adrenal incidentalomas: European society of endocrinology clinical practice guideline in collaboration with the European network for the study of adrenal tumors. Eur J Endocrinol (2016) 175(2):G1–g34. doi: 10.1530/EJE-16-0467
2. Suradi HH, Amarin JZ, Zayed AA. Adrenal incidentaloma. N Engl J Med (2021) 385(8):768. doi: 10.1056/NEJMc2108550
3. Brunt LM. Sages guidelines for minimally invasive treatment of adrenal pathology. Surg Endosc (2013) 27(11):3957–9. doi: 10.1007/s00464-013-3168-0
4. Podbregar A, Janez A, Goricar K, Jensterle M. The prevalence and characteristics of non-functioning and autonomous cortisol secreting adrenal incidentaloma after patients' stratification by body mass index and age. BMC Endocr Disord (2020) 20(1):118. doi: 10.1186/s12902-020-00599-0
5. Bernardi S, Calabrò V, Cavallaro M, Lovriha S, Eramo R, Fabris B, et al. Is the adrenal incidentaloma functionally active? an approach-To-The-Patient-Based review. J Clin Med (2022) 11(14):4064. doi: 10.3390/jcm11144064
6. Graham DJ, Mchenry CR. The adrenal incidentaloma: guidelines for evaluation and recommendations for management. Surg Oncol Clin N Am (1998) 7(4):749–64. doi: 10.1016/S1055-3207(18)30243-6
7. Cambos S, Tabarin A. Management of adrenal incidentalomas: Working through uncertainty. Best Pract Res Clin Endocrinol Metab (2020) 34(3):101427. doi: 10.1016/j.beem.2020.101427
8. Baba S, Iwamura M. Retroperitoneal laparoscopic adrenalectomy. BioMed Pharmacother (2002) 56(Suppl 1):113s–9s. doi: 10.1016/s0753-3322(02)00225-1
9. Ye C, Yang Y, Guo F, Wang F, Zhang C, Yang B, et al. Robotic enucleation of adrenal masses: technique and outcomes. World J Urol (2020) 38(4):853–8. doi: 10.1007/s00345-019-02868-7
10. Jason DS, Oltmann SC. Evaluation of an adrenal incidentaloma. Surg Clin North Am (2019) 99(4):721–9. doi: 10.1016/j.suc.2019.04.009
11. Müller A, Ingargiola E, Solitro F, Bollito E, Puglisi S, Terzolo M, et al. May an adrenal incidentaloma change its nature? J Endocrinol Invest (2020) 43(9):1301–7. doi: 10.1007/s40618-020-01219-3
12. Kebebew E. Adrenal incidentaloma. N Engl J Med (2021) 384(16):1542–51. doi: 10.1056/NEJMcp2031112
13. Tuna MM, Imga NN, Doğan BA, Yılmaz FM, Topçuoğlu C, Akbaba G, et al. Non-functioning adrenal incidentalomas are associated with higher hypertension prevalence and higher risk of atherosclerosis. J Endocrinol Invest (2014) 37(8):765–8. doi: 10.1007/s40618-014-0106-5
14. Cansu GB, SARI R, Yilmaz N, Özdem S, Çubuk M. Markers of subclinical cardiovascular disease in nonfunctional adrenal incidentaloma patients without traditional cardiovascular risk factors. Exp Clin Endocrinol Diabetes (2017) 125(1):57–63. doi: 10.1055/s-0042-109866
15. Emral R, Aydoğan B, Köse AD, Demir Ö, Çorapçıoğlu D. Could a nonfunctional adrenal incidentaloma be a risk factor for increased carotid intima-media thickness and metabolic syndrome. Endocrinol Diabetes Nutr (Engl Ed) (2019) 66(7):402–9. doi: 10.1016/j.endinu.2019.01.007
16. Ribeiro Cavalari EM, De Paula MP, Arruda M, Carraro N, Martins A, de Souza K, et al. Nonfunctioning adrenal incidentaloma: A novel predictive factor for metabolic syndrome. Clin Endocrinol (Oxf) (2018) 89(5):586–95. doi: 10.1111/cen.13822
17. Akkus G, Evran M, Sert M, Tetiker T. Adipocytokines in non-functional adrenal incidentalomas and relation with insulin resistance parameters. Endocr Metab Immune Disord Drug Targets (2019) 19(3):326–32. doi: 10.2174/1871530318666181009112042
18. Francucci CM, Caudarella R, Rilli S, Fiscaletti P, Ceccoli L, Boscaro M. Adrenal incidentaloma: effects on bone metabolism. J Endocrinol Invest (2008) 31(7 Suppl):48–52.
Keywords: nonfunctional adrenal incidentaloma, conservative treatment, surgery, efficacy, safety
Citation: Li X, Xiao S, Zhan X, Yu Y, Zhang C, Xi H, Wang G and Zhou X (2023) For small (1-3cm) nonfunctional adrenal incidentaloma (NFAI), which option is more appropriate for conservative treatment or surgery? Front. Endocrinol. 14:1119251. doi: 10.3389/fendo.2023.1119251
Received: 08 December 2022; Accepted: 19 January 2023;
Published: 01 February 2023.
Edited by:
Yuxuan Song, Peking University People’s Hospital, ChinaReviewed by:
Jiaxiang Liu, Chinese Academy of Medical Sciences and Peking Union Medical College, ChinaCopyright © 2023 Li, Xiao, Zhan, Yu, Zhang, Xi, Wang and Zhou. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xiaochen Zhou, bW9fZGlzY0AxMjYuY29t; Gongxian Wang, dXJvd2d4QDE2My5jb20=; Haibo Xi, MTM4NzA4MzQ1NzhAMTYzLmNvbQ==
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.