
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Endocrinol. , 03 February 2023
Sec. Clinical Diabetes
Volume 14 - 2023 | https://doi.org/10.3389/fendo.2023.1068018
This article is part of the Research Topic Application of Telehealth to Diabetes Care Delivery and Medical Training: Challenges and Opportunities View all 8 articles
 Abrar M. Al-Mutairi1,2,3*
Abrar M. Al-Mutairi1,2,3* Mohammad A. Alshabeeb2,3,4
Mohammad A. Alshabeeb2,3,4 Salah Abohelaika5
Salah Abohelaika5 Fadhel A. Alomar6
Fadhel A. Alomar6 Keshore R. Bidasee7,8,9*
Keshore R. Bidasee7,8,9*Background: The lockdown at the start of coronavirus disease 2019 (COVID-19) pandemic in Saudi Arabia (March 2020 to June 2020) shifted routine in-person care for patients with type 2 diabetes mellitus (T2DM) to telemedicine. The aim of this study was to investigate the impact telemedicine had during this period on glycemic control (HbA1c) in patients with T2DM
Methods: 4,266 patients with T2DM were screened from five Ministry of National Guard Health Affairs hospitals in the Kingdom of Saudi Arabia. Age, gender, body mass index (BMI), HbA1c (before and after the COVID-19 lockdown), duration of T2DM, comorbidities and antidiabetic medications data were obtained. Mean and standard deviation of differences in HbA1c were calculated to assess the impact of telemedicine intervention. Correlations between clinically significant variances (when change in the level is ≥0.5%) in HbA1c with demographics and clinical characteristic data were determined using chi square test.
Results: Most of the participants were Saudis (97.7%) with 59.7% female and 56.4% ≥60 years of age. Obesity was 63.8%, dyslipidemia 91%, and hypertension 70%. Mean HbA1c of all patients slightly rose from 8.52% ± 1.5% before lockdown to 8.68% ± 1.6% after lockdown. There were n=1,064 patients (24.9%) whose HbA1c decreased by ≥0.5%, n =1,574 patients whose HbA1c increased by ≥0.5% (36.9%), and n =1,628 patients whose HbA1c changed by <0.5% in either direction (38.2%). More males had significant improvements in glycemia compared to females (28.1% vs 22.8%, p<0.0001), as were individuals below the age of 60 years (28.1% vs 22.5%, p<0.0001). Hypertensive individuals were less likely than non-hypertensive to have glycemic improvement (23.7% vs 27.9%, p=0.015). More patients on sulfonylureas had improvements in HbA1c (42.3% vs 37.9%, p=0.032), whereas patients on insulin had higher HbA1c (62.7% vs 56.2%, p=0.001). HbA1c changes were independent of BMI, duration of disease, hyperlipidemia, heart and kidney diseases.
Conclusion: Telemedicine was helpful in delivering care to T2DM patients during COVID-19 lockdown, with 63.1% of patients maintaining HbA1c and improving glycemia. More males than females showed improvements. However, the HbA1c levels in this cohort of patients pre- and post-lockdown were unsatisfactorily high, and may be due to in part lifestyle, age, education, and hypertension.
As a result of the global pandemic that emerged at the end of 2019 due to the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) (1), many countries began closing their boarders and implemented stay-at home (lockdown) measures to limit the spread of the virus and protect their citizens (2). This lockdown inadvertently restricted patients with per-existing comorbidities to visit outpatient clinics, limited their physical activities, influenced their eating habits, and impacted their psychological status (3). These unprecedented conditions were expected to worsen glycemia in DM patients which highlights the importance of optimizing drug therapy in chronic and long-term DM patients. In addition, patients with DM require regular face-to-face communication with diabetic practitioners, and diabetic educators to achieve optimal glycemic control (4). This approach is needed to blunt multi-organ comorbidities that arise from the persistent hyperglycemia in DM patients (3–5).
Healthcare sectors in many countries adopted strategies to provide timely and effective care to DM patients during this period (6). In Brazil, providing educational materials on healthy habits, mental health, and diabetes management via telephone calls during the lockdown was an effective healthcare measure (7). Globally, use of telehealth increases from 1% to >50% of diabetes clinics during the pandemic (8). It also became possible to achieve tight glycemic control and prevent fluctuation in blood glucose levels with the recent advances in technology that allow virtual care (9). During the period 25th March 2020 to 20th June 2020 of the COVID-19 pandemic, the hospitals and health centers in the Saudi Arabia used telehealth to ensure patients receive the necessary health care and medications at timely manner. A recent study, that involved 270 Saudi patients on anticoagulants, confirmed that tele-pharmacy clinic was as effective as face-to-face consultations (10). Other studies also suggest that telehealth is useful in managing DM patients and improving glycated hemoglobin A1C levels (HbA1c) in DM patients (11, 12). A prospective cohort study conducted by Tourkmani et al. (2021) screened diabetic COVID-19 patients from Saudi Arabia and reported that telehealth had a significant positive impact on glycemic control, in high-risk diabetic patients with HbA1c levels decreasing from 9.98% to 8.32%. However, the number of diabetic patients in this study was relatively small (n=130) potentially limiting the conclusion (13). Here, we investigated the effect of telehealth on glycemic control in a larger number of T2DM (n=4,266) in various regions of Saudi Arabia during the COVID-19 pandemic lockdown.
The study was approved by the Institutional Review Board (IRB) at King Abdullah International Medical Research Centre (KAIMRC, NRC21R/463/11). This is a multicenter retrospective cohort study; the data was collected from the patient’s medical records at the Ministry of National Guard Health Affairs (MNGHA), Saudi Arabia. All information was obtained from the BestCare electronic health records (EHRs) system. The health system covers all MNGHA individuals, with free full-healthcare services in five hospitals in the three main regions (Central, Western, and Eastern) of Saudi Arabia.
The recruited patients in this study included (i) all adult patients with T2DM, (ii) had an HbA1c value of ≥6.5%, and (iii) answered the scheduled phone calls during the follow up period (25th March 2020 to 20th June 2020). Pre-diabetic patients (HbA1c level of 5.7%- 6.4%) and those who did not answer phone calls throughout the scheduled virtual clinics were excluded. As a result of these criteria, 4,266 patients were included in this study. Figure 1 illustrates an inclusion and exclusion flowchart which also shows the main elements of focus during telemedicine communication and diabetic education. This involved a follow up of patient’s current status, documenting new episodes of complications or symptoms, reviewing recent laboratory results, ordering medications refill, and suggesting treatment plan modification when needed. The duration of T2DM, comorbidities, body mass index (BMI) classification, and prescribed medications were all recorded. The extracted data in particular HbA1c readings were grouped based on two primary time points: “pre-COVID-19 lockdown”, which included data from 15th September 2019 until 24th March 2020; and “post-COVID-19 lockdown”, which included data from 21st June 2020 until 15th September 2020.
Descriptive analyses are reported using mean (M) and standard deviation (SD) for continuous variables and frequencies and percentages for categorical variables. The HbA1c score changes between pre- and post-lockdown were calculated and the difference significance was assessed using the paired t-test. P-value ≤0.05 was used as a criterion to determine whether the observed differences are statistically significant. The American Diabetes Association suggests that changes in HbA1c mean levels below 0.5% are not clinically significant (14). The patients with clinically significant decreased HbA1c mean levels were compared to patients with clinically significant increased values using chi-square test to determine the impacting factors among demographic and clinical characteristics. Categorical covariates in the number and chemical classes of given drugs between the two compared groups were also assessed. The chosen statistical tests were run through using the Statistical Package for the Social Sciences (SPSS) software version 27.
A total of 4,618 T2DM patients were scheduled for the virtual integrated clinic at MNGHA facilities in Central, Western, and Eastern regions. Of these patients, 4,266 patients satisfied the inclusion criteria (Figure 1, with 2,547 females and 1,719 males (59.7% vs 40.3%, respectively). Baseline characteristics of the followed up patients are shown in Table 1. The majority of patients were Saudis (97.7%), with high percentage of them (82.5%) in the Central region. Patients aged ≥60 years represented the highest percentage of the participants (56.4%), and then those aged between 45–59 years old (36.8%). The younger patients ≤44 years old represented only 6.8%. Two thirds of the patients (66.3%) had diagnosed with T2DM for less than five years, and 63.8% were obese (BMI≥30). Most of the patients (95.2%) had at least one or more concomitant chronic illnesses; 3,029 (71.0%) patients had hypertension, 3,860 (90.5%) had hyperlipidemia, 348 (8.2%) had heart diseases, and 342 (8.0%) had kidney disease.
Table 2 shows the mean difference before and after lockdown among the tested cohort; the overall mean HbA1c increased slightly from 8.52% ( ± 1.5%) before lockdown to 8.68% ( ± 1.6%) after lockdown. This change is not clinically significant (HbA1c level difference <0.5%). However, subgrouping of the study cohort indicated that one quarter of the patients (n=1,064, 24.9%) showed significant glycemic improvement (mean HbA1c decreased by 1.38%), versus 1,574 patients (36.9%) demonstrated poorer control (mean HbA1c increased by 1.36%), while 1,628 patients (38.2%) reported minimal non-significant HbA1c changes (<0.5%). Comparisons between these three groups were made to identify the demographic factors that are associated with these changes as shown in Table 3. Higher percentage of males was detected in the group of improved outcome than in females (28.1% vs 22.8%, respectively, p<0.0001). Moreover, higher improvement rates were identified among patients in Western region than in the Central and Eastern regions (29.6% vs 24.3 and 24.7%, respectively, p= 0.005). Also, percentage of patients aged <60 years was higher in the HbA1c improved group than in those aged ≥60 (28.1% vs 22.5%, respectively, p<0.0001). In addition, lower rates of improvement were noted in those with hypertension compared to non-hypertensive diabetic patients (23.7% vs 27.9%, p=0.015). There was no association between the changes in HbA1c and other variables including patients’ nationality, BMI, disease duration, and other comorbid diseases. Further analysis was carried out using logistic regression to confirm the above mentioned associations; the results assured that male gender and age under 60 years were the only factors significantly impacting improved glycemia (p<0.0001, OR=1.40, and p=0.03, OR=1.28, respectively).
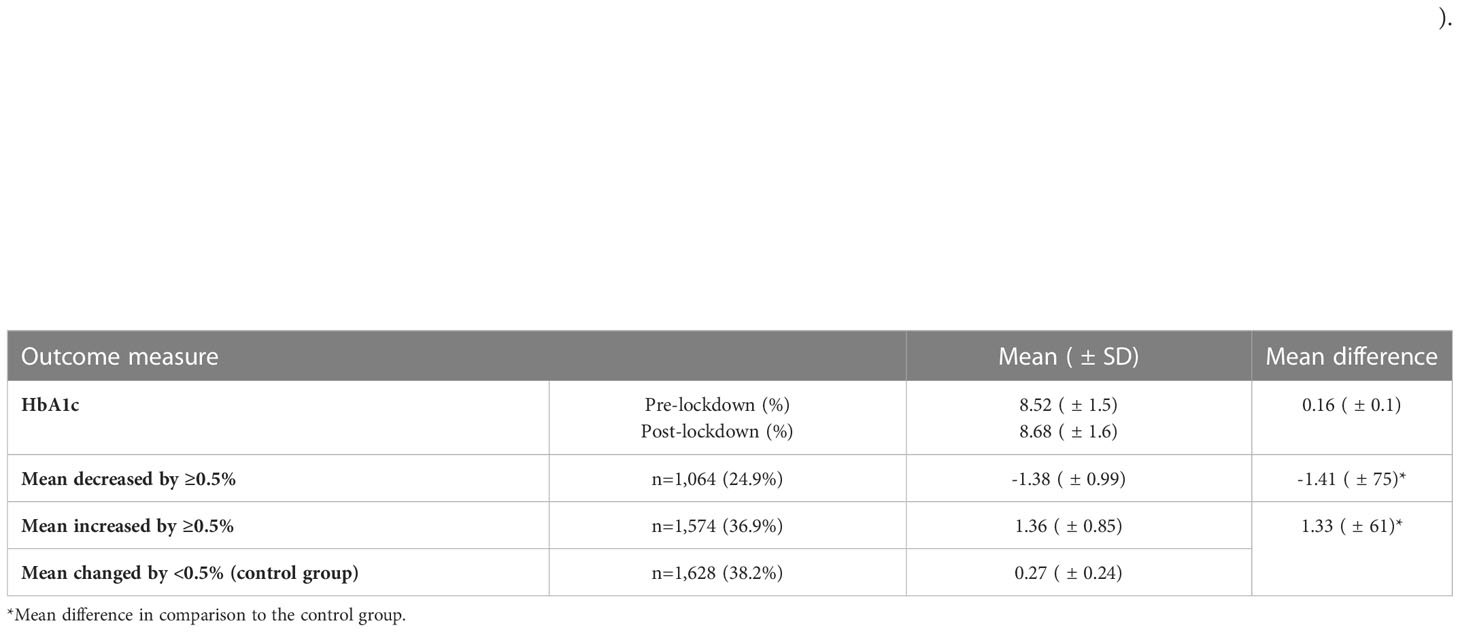
Table 2 HbA1c scores throughout pre to post COVID-19 lockdown and subgrouping of the cohort based on the score changes beyond the clinically significant cut-off point (0.5%).
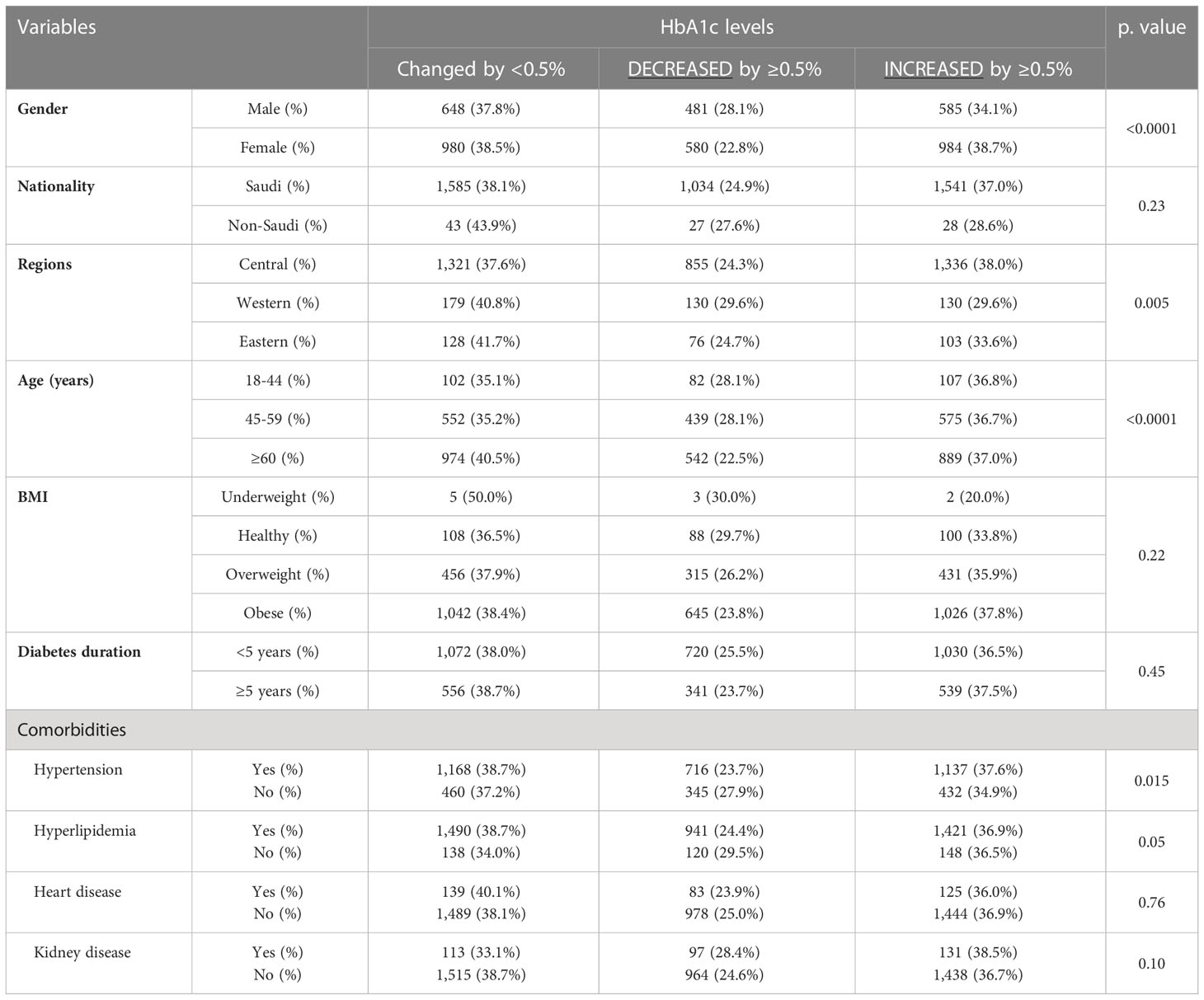
Table 3 Association of different demographic variables with HbA1c changes by more or less than 0.5% throughout the lockdown period in T2DM patients.
We failed to access medication history of 348 (8.1%) patients, thus the analysis of the medication usage was restricted to 3,918 T2DM patients only. The results, shown in Figure 2, demonstrated that the majority of patients were using two (34%) or three (33%) medications. One fifth (20%) of the patients was using a single drug therapy, whereas 14% of the tested cohort were found to be on four drug-regimen. As shown in Figure 3, metformin represented the highest usage rate by the T2DM patients (86%), then sulfonylureas (glibenclamide, gliclazide, glimepiride, and glipizide) and insulin (both sulfonylureas and insulin groups were used by 55% of the patients). List of different types of used insulin are described in Figure 3. The dipeptidyl peptidase-4 (DPP-4) inhibitors (linagliptin or sitagliptin) were used by 44% of the patients. Other classes such as alpha-glucosidase inhibitor (acarbose), incretin mimetics (glucagon-like peptide-1 (GLP-1) agonists (liraglutide and semaglutide), sodium-glucose cotransporter-2 (SGLT2) inhibitors (dapagliflozin and empagliflozin), and thiazolidinedione (pioglitazone) were used by 1-2% of the patients. The comparison between the groups of patients who had a reduction and an increase in HbA1c by ≥0.5% revealed significant associations with use of insulin and sulfonylureas. Table 4 shows that insulin users were lower in the group of decreased HbA1c levels than other patients on different oral antidiabetic agents (37.3% vs 43.8%, p=0.001, OR=0.76). Conversely, the individuals on oral sulfonylureas showed higher percentage in the reduced HbA1c group than patients on different treatment modalities (42.3% vs 37.9%, p=0.032, OR=1.20). Use of other major classes such as metformin and DDP-4 inhibitors, has no significant distribution differences among the compared cohorts. Likewise, no significant differences were noticed between patients on one or two medications in comparison to patients on three or four medications among the decreased group (40.3% vs 40.2%, p=1.0, OR=1.0).
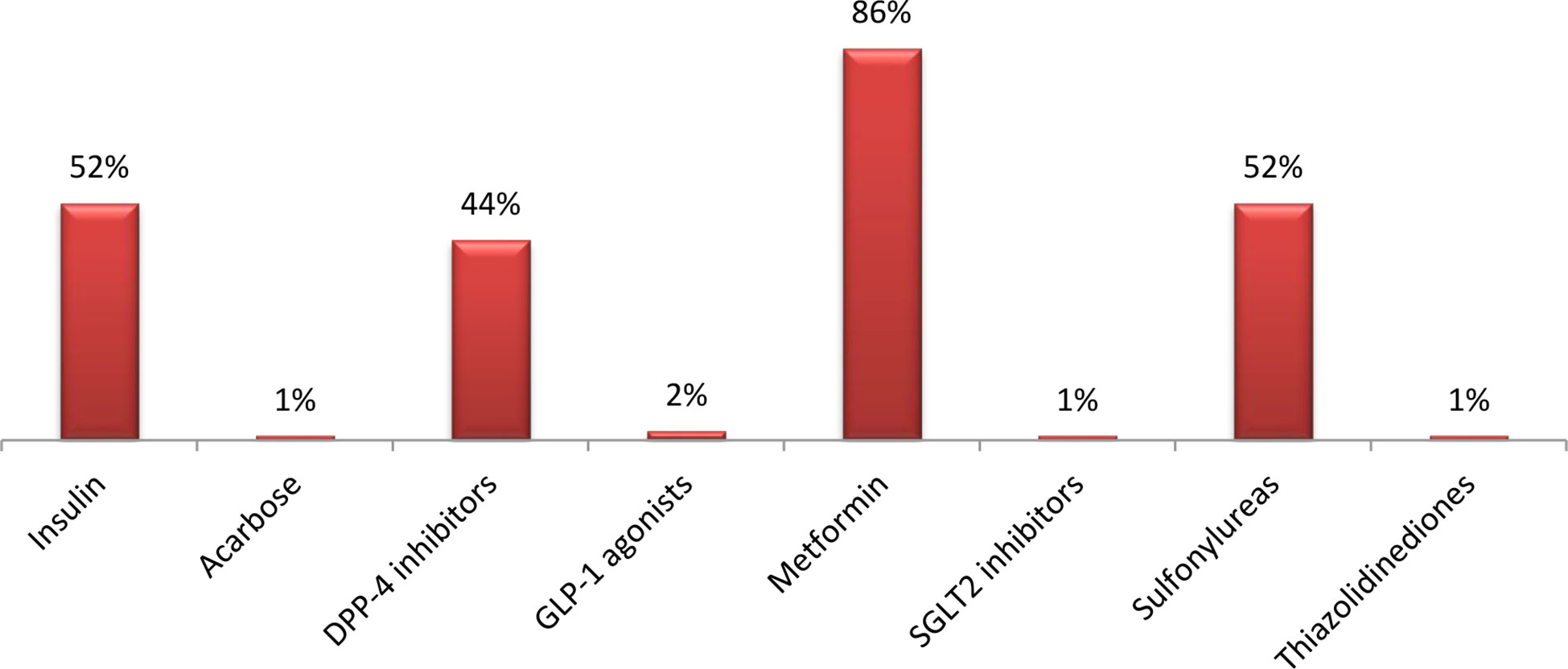
Figure 3 Percentage (%) of patients on different classes of anti-diabetic medications. Insulin: Regular, Aspart, NPH, Human insulin 70/30, Degludec, Detemir, Glargine. Alpha-glucosidase inhibitor: Acarbose. Dipeptidyl peptidase 4 (DDP-4) inhibitors: Linagliptin, Sitagliptin. Glucagon-like peptide-1 receptor (GLP-1) agonists: Liraglutide, Semaglutide. Biguanide: Metformin. Sodium-glucose cotransporter-2 (SGLT2) inhibitors: Dapagliflozin, Empagliflozin. Sulfonylureas: Glibenclamide, Gliclazide, Glimepiride, Glipizide. Thiazolidinedione: Pioglitazone.
This study assessed the effectiveness of virtual clinics as an intervention for glycemic control in T2DM. In addition, impact of several demographic factors on individuals’ glycemic control was investigated. Our findings showed no significant change in mean HbA1c level (0.16% ± 0.1%) between pre and post lockdown period (March 2020 to June 2020). Whereas, significant improvements in glycemia were noticed more in males than females, in patients aged below 60 years, in non-hypertensive individuals, and in patients on sulfonylureas.
According to the American Diabetes Association and the American National Institute for Health and Clinical Excellence, the clinical significant cut-off point in HbA1c level is 0.5% (15, 16). The slight mean change observed in HbA1c level in our study before and after commencing the virtual clinics matches the finding reported in a meta-analysis of five randomized control trials that included 953 diabetic patients. The meta-analysis study concluded that telephone contact intervention was associated with a small and clinically insignificant change in HbA1c (mean HbA1c difference=-0.38%) (17). A recent Japanese study which involved 2,727 participants demonstrated that both telemedicine and clinic visit are effective in reducing mean HbA1c level in patients with pre- emergency levels of ≥7% only. Nevertheless, no differences were observed between both approaches (11). The slight increase detected in HbA1c value after lockdown in our study may partially related to the function and procedure of the newly introduced telemedicine approach and can be also explained by the decrease in patients’ physical activity and changes in dietary intake due to the increased time spent at home during lockdown. Thus, there is a drastic need to develop effective strategies to encourage diabetic patients to plan long-term lifestyle changes including healthy diet and regular exercise to improve their blood glucose levels in both normal conditions and in crises.
To ensure successfulness of telemedicine program, health care providers engaged in virtual clinics must be well-trained in professional communication with patients remotely (17–20). Recent research shows that the most common method of telemedicine intervention is via phone call not the video calling (17). Telephone is an effective communication model and is commonly used and accessed by almost everyone. Findings in Brazil suggest that phone calls are the simplest form of digital health for people with low literacy, such as the elderly (21). The current evidence supports the use of phone calls to provide simple information about the COVID-19 precautions (22–24). Telemedicine can be delivered through several other communication forms including online-based programs, videoconferencing, and sending text messages (18). Use of the new social media tools such as WhatsApp, SnapChat, and Telegram might be also beneficial. In comparison to our study which kept track of patients through phone calls only, the study conducted by Tourkmani et al. (2021) at Prince Sultan Military Medical City in Saudi Arabia used additional methods such as WhatsApp messenger to deliver written instructions, educational materials, and audio-visual aids. The patients were also asked to submit their self-monitoring blood glucose results over WhatsApp if they had any difficulty in submitting them during the virtual appointment. Providing this extra telehealth service may contributed in the noticed reduction of HbA1c level from 9.98% ± 1.33% pre-intervention to 8.32% ± 1.31% post-intervention (13). In another study which introduced a WeChat app as a remote tool for management of T2DM, the results showed higher treatment satisfaction and improved glycemic control (25).
Several demographic factors are thought to impact individuals’ glycemic control (26, 27). Obesity is highly prevalent in diabetic patients (28, 29), however, our study found no association between variability in HbA1c scores and different body mass index status in contrast to Kakade et al. (30). The data on the impact of gender on glycemic control is mixed. Our study found that males had higher frequent glycemic improvement than females, consistent with some but not all previous studies (31–34). Glycemic control may be worse in women due to differences in glucose hemostasis (35), psychological factors (36), and antidiabetic medication response (37). Unlike the findings of Benoit et al. (38) and Al-Lawati et al. (34), individuals below the age of 60 in our cohort showed a significant clinical decrease in HbA1c compared to older subjects, which is consistent with a previously published study (39). Furthermore, our results showed no impact of DM duration on patients response which is inconsistent with previous findings (34–43) which reported that the longer the duration course, the poorer glycemic outcome is predicted. In addition, our data does not support a previous study that involved 300 Saudi diabetic patients who showed positive correlation between reduced HbA1c and disease duration (44). Also, our results failed to confirm previous findings (30–45) in which patients with high lipid profile had poorer glycemic control.
The prevalence of hypertension among the selected cohort in our study was similar to a previous small study on diabetic patients (n=154), with 72% of whom were hypertensive (46). The study found no association between glycemic control levels and the concomitant blood pressure control status. In contrast, our data showed lower percentages of hypertensive patients who had clinical glycemic improvement in comparison to normotensive individuals. This was expected as previous reports emphasized that people with hypertension tend to have higher levels of insulin resistance than others (47). Similar to our findings, a study on Omani population found higher HbA1c levels among patients with elevated diastolic blood pressure (45). The prescription pattern of antidiabetic agents seen in our study is very similar to a previous Saudi study (48), where metformin, sulfonylureas, and insulin were the most common prescribed diabetic medications, the majority of patients were on a combination therapy, and no association detected between glycemic outcome and the number of used DM medications. However, our data showed that 44% of the patients were using DPP-4 inhibitors versus only 3.74% in the study conducted by Misbahuddin et al. (48). In our study, patients on insulin showed poorer glycemic control as reported previously (38), though other studies showed a positive impact of insulin use on HbA1c outcome (49, 50). A recent study revealed that use of insulin by T2DM patients may deteriorate their general health condition, induces psychological distress, and associated with activity difficulties in comparison to those using oral agents (51). On the other hand, our results indicated that the sulfonylureas were the only antidiabetic class which tends to significantly improve glycemic control.
Taken together, the implementation of telemedicine in managing many chronic diseases such as DM may take place in all healthcare system soon. This approach is useful to deliver health education and suggesting the necessary interventions to patients remotely. Nonetheless, telemedicine has some limitations such as inability to examine patients physically which is very likely needed when diagnosing new patients. Also, the patients may need to buy costly smart phones to be able to communicate with healthcare providers via social media tools. In addition, using unclear phone line or internet with low quality can halt the provided services (52, 53). Thus, developing a more comprehensive telemedicine approach and a more professional and well-trained team is predicted to effectively manage diabetic patients. Further prospective research is suggested to examine the cost effectiveness and impact of telemedicine on patients’ outcome in Saudi Arabia. Expansion of telemedicine presents an opportunity to generate easier solutions. Thus, the effects of telemedicine on hospital efficiency indicators and staff performance should be further studied.
Our study illustrates that the virtual clinics scheduled during COVID-19 lockdown were effectively adopted at MNGHA to assist >63% of patients with T2DM maintain or lower HbA1c. More efforts are needed by health care providers and patients to achieve tighter glycemic controls. Telemedicine is a promising approach in managing patients with chronic diseases in particular diabetes. Thus, healthcare policymakers potentially need to consider use of telemedicine in normal times as well as in crises. Multidisciplinary health teams need to be carefully selected to promote practice of excellence and ensure the quality of care. More controlled prospective research is also needed to further evaluate the impact of telemedicine on T2DM. Variability in patients’ demographic and clinical characteristics such as gender, age, blood pressure status, use of insulin and sulfonylureas may play a role as determinants of glycemic outcome. More work is needed to determine the extent to which pre-diabetic patients (HbA1c 5.7 to 6.4%) developed diabetes during the COVID-19 lockdown.
The original contributions presented in the study are included in the article. Further inquiries can be directed to the corresponding authors.
The study, which involved human participants, was reviewed and approved by the Institutional Review Board (IRB) at King Abdullah International Medical Research Centre (reference number: NRC21R/463/11). Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
AA and MA have conceived and conceptualized the work. SA analyzed the prescribed medications. AA, SA, and FA took part in the statistical analyses of data. KRB took the lead in reorganizing the manuscript and approving the final version. All authors shared in manuscript preparation. All authors have agreed to all of the submitted materials. All authors contributed to the article and approved the submitted version.
We are grateful to Bien Paras from Research Data Management at KAIMRC for the help in extracting the data from BestCare database.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med (2020) 382:727–33. doi: 10.1056/NEJMoa2001017
2. Shatla M, Alharthi BT, Alharbi AG, Khan ZA, Althaqfi AA, Babkoor AA, et al. The impact of the COVID-19 pandemic on family medicine practices in Saudi Arabia. Cureus (2021) 13:1–17. doi: 10.7759/cureus.20437
3. Nachimuthu S, Vijayalakshmi R, Sudha M, Viswanathan V. Coping with diabetes during the COVID–19 lockdown in India: Results of an online pilot survey. Diabetes Metab Syndr (2020) 14:579–82. doi: 10.1016/j.dsx.2020.04.053
4. Zhou P, Xu L, Liu X, Huang J, Xu W, Chen W. Web-based telemedicine for management of type 2 diabetes through glucose uploads: A randomized controlled trial. Int J Clin Exp Pathol (2014) 7:8848.
5. Quinn LM, Davies MJ, Hadjiconstantinou M. Virtual consultations and the role of technology during the COVID-19 pandemic for people with type 2 diabetes: The UK perspective. J Med Internet Res (2020) 22:e21609. doi: 10.2196/21609
6. He F, Deng Y, Li W. Coronavirus disease 2019: What we know? J Med Virol (2020) 92:719–25. doi: 10.1002/jmv.25766
7. Alessi J, de Oliveira GB, Franco DW, Becker AS, Knijnik CP, Kobe GL, et al. Telehealth strategy to mitigate the negative psychological impact of the COVID-19 pandemic on type 2 diabetes: A randomized controlled trial. Acta Diabetologica (2021) 58:899–909. doi: 10.1007/s00592-021-01690-1
8. Haynes SC, Kompala T, Neinstein A, Rosenthal J, Crossen S. Disparities in telemedicine use for subspecialty diabetes care during COVID-19 shelter-in-place orders. J Diabetes Sci Technol (2021) 15:986–92. doi: 10.1177/1932296821997851
9. Jnr BA. Use of telemedicine and virtual care for remote treatment in response to COVID-19 pandemic. J Med Syst (2020) 44:1–9. doi: 10.1007/s10916-020-01596-5
10. Al Ammari M, AlThiab K, AlJohani M, Sultana K, Maklhafi N, AlOnazi H, et al. Tele-pharmacy anticoagulation clinic during COVID-19 pandemic: Patient outcomes. Front Pharmacol (2021) 12:652482. doi: 10.3389/fphar.2021.652482
11. Onishi Y, Yoshida Y, Takao T, Tahara T, Kikuchi T, Kobori T, et al. Diabetes management by either telemedicine or clinic visit improved glycemic control during the coronavirus disease 2019 pandemic state of emergency in Japan. J Diabetes Investig (2022) 13:386–90. doi: 10.1111/jdi.13546
12. Predieri B, Leo F, Candia F, Lucaccioni L, Madeo SF, Pugliese M, et al. Glycemic control improvement in Italian children and adolescents with type 1 diabetes followed through telemedicine during lockdown due to the COVID-19 pandemic. Front Endocrinol (2020) 965:595735. doi: 10.3389/fendo.2020.595735
13. Tourkmani AM, ALHarbi TJ, Rsheed AMB, Alrasheedy AA, ALMadani W, ALJuraisi F, et al. The impact of telemedicine on patients with uncontrolled type 2 diabetes mellitus during the COVID-19 pandemic in Saudi Arabia: Findings and implications. J Telemed Telecare (2021) 0(0):1–9. doi: 10.1177/1357633X20985763
14. Marathe PH, Gao HX, Close KL. American Diabetes association standards of medical care in diabetes 2017. Wiley Online Library (2017) 9:320–4. doi: 10.1111/1753-0407.12524
15. Lenters-Westra E, Schindhelm R, Bilo H, Groenier K, Slingerland R. Differences in interpretation of haemoglobin A1c values among diabetes care professionals. Neth J Med (2014) 72:462–6.
17. Iftinan GN, Wathoni N, Lestari K. Telepharmacy: A potential alternative approach for diabetic patients during the COVID-19 pandemic. J Multidiscip Healthc (2021) 14:2261. doi: 10.2147/JMDH.S325645
18. Zhai Y. A call for addressing barriers to telemedicine: Health disparities during the COVID-19 pandemic. Psychother Psychosom (2021) 90:64–6. doi: 10.1159/000509000
19. Sanchez Gonzalez ML, McCord CE, Dopp AR, Tarlow KR, Dickey NJ, McMaughan DK, et al. Telemental health training and delivery in primary care: A case report of interdisciplinary treatment. J Clin Psychol (2019) 75:260–70. doi: 10.1002/jclp.22719
20. Dale J, Caramlau I, Sturt J, Friede T, Walker R. Telephone peer-delivered intervention for diabetes motivation and support: The telecare exploratory RCT. Patient Educ Couns (2009) 75:91–8. doi: 10.1016/j.pec.2008.09.014
21. Purnamayanti NK, Wicaksana AL. Digital health services among patients with diabetes during the COVID-19 pandemic: A scoping review. Indian J Endocrinol Metab (2021) 25:86. doi: 10.4103/ijem.ijem_153_2
22. Evidence standards framework for digital health technologies. London, UK: National Institute for Health and Care Excellence (2019) (Accessed 10/06/2022).
23. Yang Y, Li W, Zhang Q, Zhang L, Cheung T, Xiang Y-T. Mental health services for older adults in China during the COVID-19 outbreak. Lancet Psychiatry (2020) 7:e19. doi: 10.1016/S2215-0366(20)30079-1
24. Bogdan-Martin D. Measuring digital development: Facts and figures 2019, technical report, International telecommunications union (2019) (Accessed 18/07/2022).
25. Kang J, Chen Y, Zhao Y, Zhang C. Effect of remote management on comprehensive management of diabetes mellitus during the COVID-19 epidemic. Prim Care Diabetes (2021) 15:417–23. doi: 10.1016/j.pcd.2020.12.004
26. Ahmad NS, Islahudin F, Paraidathathu T. Factors associated with good glycemic control among patients with type 2 diabetes mellitus. J Diabetes Investig (2014) 5:563–9. doi: 10.1111/jdi.12175
27. Alramadan MJ, Afroz A, Hussain SM, Batais MA, Almigbal TH, Al-Humrani HA, et al. Patient-related determinants of glycaemic control in people with type 2 diabetes in the gulf cooperation council countries: A systematic review. J Diabetes Res (2018) 2018:1–14. doi: 10.1155/2018/9389265
28. Yuan C, Lai CW, Chan LW, Chow M, Law HK, Ying M. The effect of diabetes self-management education on body weight, glycemic control, and other metabolic markers in patients with type 2 diabetes mellitus. J Diabetes Res (2014) 2014:1–7. doi: 10.1155/2014/789761
29. Khare J, Jindal S. Observational study on effect of lock down due to COVID 19 on glycemic control in patients with diabetes: Experience from central India. Diabetes Metab Syndr (2020) 14:1571–4. doi: 10.1016/j.dsx.2020.08.012
30. Kakade AA, Mohanty IR, Rai S. Assessment of factors associated with poor glycemic control among patients with type II diabetes mellitus. Integr Obes Diabetes (2018) 4:1–6. doi: 10.1016/j.jdiacomp.2008.12.008
31. Mondesir FL, Carson AP, Durant RW, Lewis MW, Safford MM, Levitan EB. Association of functional and structural social support with medication adherence among individuals treated for coronary heart disease risk factors: Findings from the REasons for geographic and racial differences in stroke (REGARDS) study. PloS One (2018) 13:e0198578. doi: 10.1371/journal.pone.0198578
32. Abdelmoneim I, Al Homrany M. Health education in the management of diabetes at the primary health care level: Is there a gender difference? East Mediterr Health J (2002) 8:18–23. doi: 10.26719/2002.8.1.18
33. Roy S, Sherman A, Monari-Sparks MJ, Schweiker O, Jain N, Sims E, et al. Association of comorbid and metabolic factors with optimal control of type 2 diabetes mellitus. N Am J Med Sci (2016) 8:31. doi: 10.4103/1947-2714.175197
34. Al-Lawati JA, Barakat MN, Al-Maskari M, Elsayed MK, Al-Lawati AM, Mohammed AJ. HbA1c levels among primary healthcare patients with type 2 diabetes mellitus in Oman. Oman Med J (2012) 27:465. doi: 10.5001/omj.2012.111
35. Mauvais-Jarvis F. Gender differences in glucose homeostasis and diabetes. Physiol Behav (2018) 187:20–3. doi: 10.1016/j.physbeh.2017.08.016
36. Arnetz L, Ekberg NR, Alvarsson M. Sex differences in type 2 diabetes: Focus on disease course and outcomes. Diabetes Metab syndrome obesity: Targets Ther (2014) 7:409. doi: 10.2147/DMSO.S51301
37. Lyons MR, Peterson LR, McGill JB, Herrero P, Coggan AR, Saeed IM, et al. Impact of sex on the heart's metabolic and functional responses to diabetic therapies. Am J Physiol Heart Circ Physiol (2013) 305:H1584–91. doi: 10.1152/ajpheart.00420.2013
38. Benoit SR, Fleming R, Philis-Tsimikas A, Ji M. Predictors of glycemic control among patients with type 2 diabetes: A longitudinal study. BMC Public Health (2005) 5:1–9. doi: 10.1186/1471-2458-5-36
39. D’Souza MS, Karkada SN, Hanrahan NP, Venkatesaperumal R, Amirtharaj A. Do perceptions of empowerment affect glycemic control and self-care among adults with type 2 diabetes? Glob J Health Sci (2015) 7:80. doi: 10.5539/gjhs.v7n5p80
40. Khattab M, Khader YS, Al-Khawaldeh A, Ajlouni K. Factors associated with poor glycemic control among patients with type 2 diabetes. J Diabetes Complicat (2010) 24:84–9. doi: 10.1016/j.jdiacomp.2008.12.008
41. Herrington WG, Alegre-Díaz J, Wade R, Gnatiuc L, Ramirez-Reyes R, Hill M, et al. Effect of diabetes duration and glycaemic control on 14-year cause-specific mortality in Mexican adults: A blood-based prospective cohort study. Lancet Diabetes Endocrinol (2018) 6:455–63. doi: 10.1016/S2213-8587(18)30050-0
42. Mamo Y, Bekele F, Nigussie T, Zewudie A. Determinants of poor glycemic control among adult patients with type 2 diabetes mellitus in jimma university medical center, jimma zone, south west Ethiopia: A case control study. BMC Endocr Disord (2019) 19:1–11. doi: 10.1186/s12902-019-0421-0
43. Malik M, Bakir A, Ai-Hamadi HA, Pugh R, Hossain M, Absood G, et al. Factors associated with diabetes and its control in a newly developed country. Pract Diabetes Inter (1999) 16:250–2. doi: 10.1002/pdi.1960160810
44. Binhemd TA. Diabetes mellitus: knowledge, attitude, practice and their relation to diabetes control in female diabetics. Ann Saudi Med (1992) 12:247–51. doi: 10.5144/0256-4947.1992.247
45. Al Balushi KA, Al-Haddabi M, Al-Zakwani I, Al Za’abi M. Glycemic control among patients with type 2 diabetes at a primary health care center in Oman. Prim Care Diabetes (2014) 8:239–43. doi: 10.1016/j.pcd.2014.01.003
46. Fi A, Han TM, Nor MBM, Aznan M, Ismail IZ. Prevalence of hypertension and glycaemic control in adult type-2 diabetes patients: a preliminary retrospective cohort study in kuantan, pahang, Malaysia. IIUM Med J Malaysia (2017) 16(1):115–21. doi: 10.31436/imjm.v16i1.366
47. Petrie JR, Guzik TJ, Touyz RM. Diabetes, hypertension, and cardiovascular disease: clinical insights and vascular mechanisms. Can J Cardiol (2018) 34:575–84. doi: 10.1016/j.cjca.2017.12.005
48. Misbahuddin M, Hussam A, Zohair J, Ziaullah M. Anti-diabetic drug utilization patterns in a government hospital in Saudi Arabia. Trop J Pharm Res (2018) 17:1193–200. doi: 10.4314/tjpr.v17i6.28
49. Guan X, Mu Y, Zhou X, Chen S, Dong J, Liao L, et al. Efficacy and safety of insulin therapy in patients with type 2 diabetes treated at different grades of hospitals in China: Subgroup analysis of the real-world SEAS study. Diabetes Technol Ther (2017) 19:34–40. doi: 10.1089/dia.2016.0305
50. Wallia A, Molitch ME. Insulin therapy for type 2 diabetes mellitus. JAMA (2014) 311:2315–25. doi: 10.1001/jama.2014.5951
51. Boels AM, Rutten G, Cleveringa F, van Avendonk M, Vos R. Insulin therapy in type 2 diabetes is associated with barriers to activity and worse health status: A cross-sectional study in primary care. Front Endocrinol (2021) 69:573235. doi: 10.3389/fendo.2021.573235
52. Hart J. Virtual integrative medicine: Pros and cons and optimizing patients' experience. Altern Complement Ther (2021) 27:31–3. doi: 10.1089/act.2020.29305.jha
Keywords: telemedicine, diabetes mellitus, glycated hemoglobin A1c, COVID-19, lockdown
Citation: Al-Mutairi AM, Alshabeeb MA, Abohelaika S, Alomar FA and Bidasee KR (2023) Impact of telemedicine on glycemic control in type 2 diabetes mellitus during the COVID-19 lockdown period. Front. Endocrinol. 14:1068018. doi: 10.3389/fendo.2023.1068018
Received: 12 October 2022; Accepted: 18 January 2023;
Published: 03 February 2023.
Edited by:
Matt Bouchonville, University of New Mexico School of Medicine, United StatesReviewed by:
Nicolas Renna, Universidad Nacional de Cuyo, ArgentinaCopyright © 2023 Al-Mutairi, Alshabeeb, Abohelaika, Alomar and Bidasee. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Abrar M. Al-Mutairi, YWxtdXRhaXJpYWJyQGtzYXUtaHMuZWR1LnNh; Keshore R. Bidasee, a2JpZGFzZWVAdW5tYy5lZHU=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.