- 1Division of Endocrinology and Metabolism, Department of Internal Medicine, Taichung Veterans General Hospital, Taichung, Taiwan
- 2Department of Medicine, School of Medicine, National Yang Ming Chiao Tung University, Taipei, Taiwan
- 3College of Medicine, National Chung Hsing University, Taichung, Taiwan
- 4Institute of Biomedical Sciences, National Chung Hsing University, Taichung, Taiwan
- 5Institute of Population Health Sciences, National Health Research Institute, Miaoli, Taiwan
- 6Division of Endocrinology and Metabolism, Department of Internal Medicine, National Cheng Kung University Hospital, Tainan, Taiwan
- 7College of Medicine, National Cheng Kung University, Tainan, Taiwan
- 8Division of Endocrinology and Metabolism, Department of Internal Medicine, Chung Shan Medical University Hospital, Taichung, Taiwan
- 9Institute of Medicine, School of Medicine, Chung Shan Medical University, Taichung, Taiwan
- 10National Center for Geriatrics and Welfare Research, National Health Research Institutes, Miaoli, Taiwan
- 11Department of Health Services Administration, China Medical University, Taichung, Taiwan
- 12Department of Family Medicine, Min-Sheng General Hospital, Taoyuan, Taiwan
- 13Section of Endocrinology and Metabolism, Department of Medicine, Taipei Veterans General Hospital, Taipei, Taiwan
Optimal control of diabetes and relevant risk factors substantially reduce the risks of chronic complications and mortality. We investigated all-cause mortality rate and major causes of death between 2007 and 2018 in patients with diabetes in Taiwan. This study was conducted using data from Taiwan National Health Insurance Research Database. We selected patients with diabetes diagnosed between 2007 and 2017 (grouped according to the year of diabetes diagnosis 2007-2010 vs. 2011-2017). Information on mortality and causes of death by the end of 2018 was confirmed through linking to the National Death Registry. Standardized mortality rate (SMR) were calculated by weighting the World Health Organization (WHO) standard population (WHO 2000-2025). More than 2.7 million of patients with diabetes were analyzed and a total of 566121 deaths were identified. Overall, the SMR was 11.72 per 1000 person-years. Patients with diabetes diagnosed in 2011-2017 had a lower SMR (8.42 vs. 12.92 per 1000 person-years) than those diagnosed in 2007-2010. Similar finding were noted regarding the major causes of death (cancer, diabetes, heart disease, hypertensive disease, and cerebrovascular disease). Compared with patients who were diagnosed in 2008-2010, those who were diagnosed in 2011-2014 and 2015-2018 had a higher 3-year survival rate (0.9356 vs. 0.9438 vs. 0.946, log-rank test p<0.001) after the diagnosis of diabetes. Patients who were diagnosed with diabetes after 2011 had a lower rate of all-cause mortality and major causes of death, compared with those who were diagnosed before 2010 in Taiwan.
Introduction
The continuous increase in the number of patients with diabetes (1–3) makes the disease become a major healthcare burden. According to a recent estimate (1), the global prevalence of adult people with diabetes was 536.6 million in 2021. The number was estimated to be 783.2 million in 2045 (1). Patients with diabetes are associated with a higher risk of micro- and macro-vascular complications (3–6), both of which lead to morbidities and mortality (5–7). There were 6.7 million of deaths due to diabetes globally in 2021, and total health expenditure due to diabetes was 966 billion USD (1).
Optimal control of diabetes and relevant risk factors could substantially reduce the risks of chronic complications and mortality (8–10). Since the launch of National Health Insurance (NHI) program in 1995 and the initiation of diabetes pay-for-performance (P4P) program in 2001 (11, 12), the outcomes of patients with diabetes in Taiwan have been improved overtime (13–15). The all-cause mortality rate in patients with diabetes declined between 2000 and 2014 (13, 14). Nevertheless, the healthcare quality for diabetes in Taiwan was rated as suboptimal in a recent report (16).
In this study, we aimed to update the rates of all-cause mortality and major causes of death in patients with diabetes in Taiwan. We investigated the mortality rates among patients diagnosed in different time periods to examine the differences in outcomes.
Materials and methods
Database and ethical approval
This study was conducted using data from Taiwan National Health Insurance Research Database (NHIRD). Since the launch of the NHI program in 1995, more than 99% of the inhabitants in Taiwan are covered by the program which represents an important source for healthcare quality assessments and researches. De-identified data were released by the Health and Welfare Data Science Center for analyses and research use. This study was conducted in accordance with the Declaration of Helsinki. The study protocol was approved by the Research Ethics Committee of the National Health Research Institute (approval number: EC1020408-E) prior to study procedures.
Study population and outcomes
We selected patients with diabetes diagnosed between 2007 and 2017 for analyses. Patents were considered as having diabetes if they had 3 or more outpatient clinic visits or one hospital admission with the diagnosis of diabetes in 1 year (17). The diagnosis of diabetes was based on the International Classification of Diseases (ICD), 9th and 10th Revision, Clinical Modification. For ICD-9-CM, the codes for diabetes diagnosis were 250.x. For ICD-10-CM, the codes were E0-E14. Patients were excluded from the analyses if they had missing information on sex or date of birth. Patients were grouped according to the year of diabetes diagnosis (2007-2010 vs. 2011-2017). Information on mortality and causes of death by the end of 2018 was confirmed through linking to the National Death Registry. To avoid confounding effect of diabetes duration on risk of mortality, we also examined the survival rate annually after diabetes diagnosed in different periods (2008-2010 vs. 2011-2014 vs. 2015-2018).
Statistical analyses
All the statistical analyses were performed using SAS version 9.4 (SAS Institute, Cary, NC, USA). We examined the crude mortality rate (expressed as per 1000 person-years) for all-cause mortality and top 5 causes of death in the study population, and in subgroups by sex, age, and year of diabetes diagnosis. We calculated standardized mortality rate (SMR) (expressed as per 1000 person-years) by weighting the World Health Organization (WHO) standard population (WHO 2000-2025). The annual survival rates after diabetes diagnosis were compared among patients diagnosed in different periods (2008-2010 vs. 2011-2014 vs. 2015-2018).
Results
Table 1 shows all-cause mortality rate in patients with diabetes between 2007 and 2017. Overall, more than 2.7 million of patients with diabetes were analyzed and a total of 566121 deaths were identified. The crude mortality rate was 29.64 per 1000 person-years, while the SMR was 11.72 per 1000 person-years. The mortality rate in men was higher than in women (14.57 vs. 8.82 per 1000 person-years), and the findings were similar across all age subgroups. Table 2 shows all-cause mortality rate by year of diabetes diagnosis (2007-2010 vs. 2011-2017). Overall, patients with diabetes diagnosed in 2011-2017 had a lower crude mortality rate (19.72 vs. 32.89 per 1000 person-years) and SMR (8.42 vs. 12.92 per 1000 person-years) than those diagnosed in 2007-2010. The findings were consistent in men and in women.
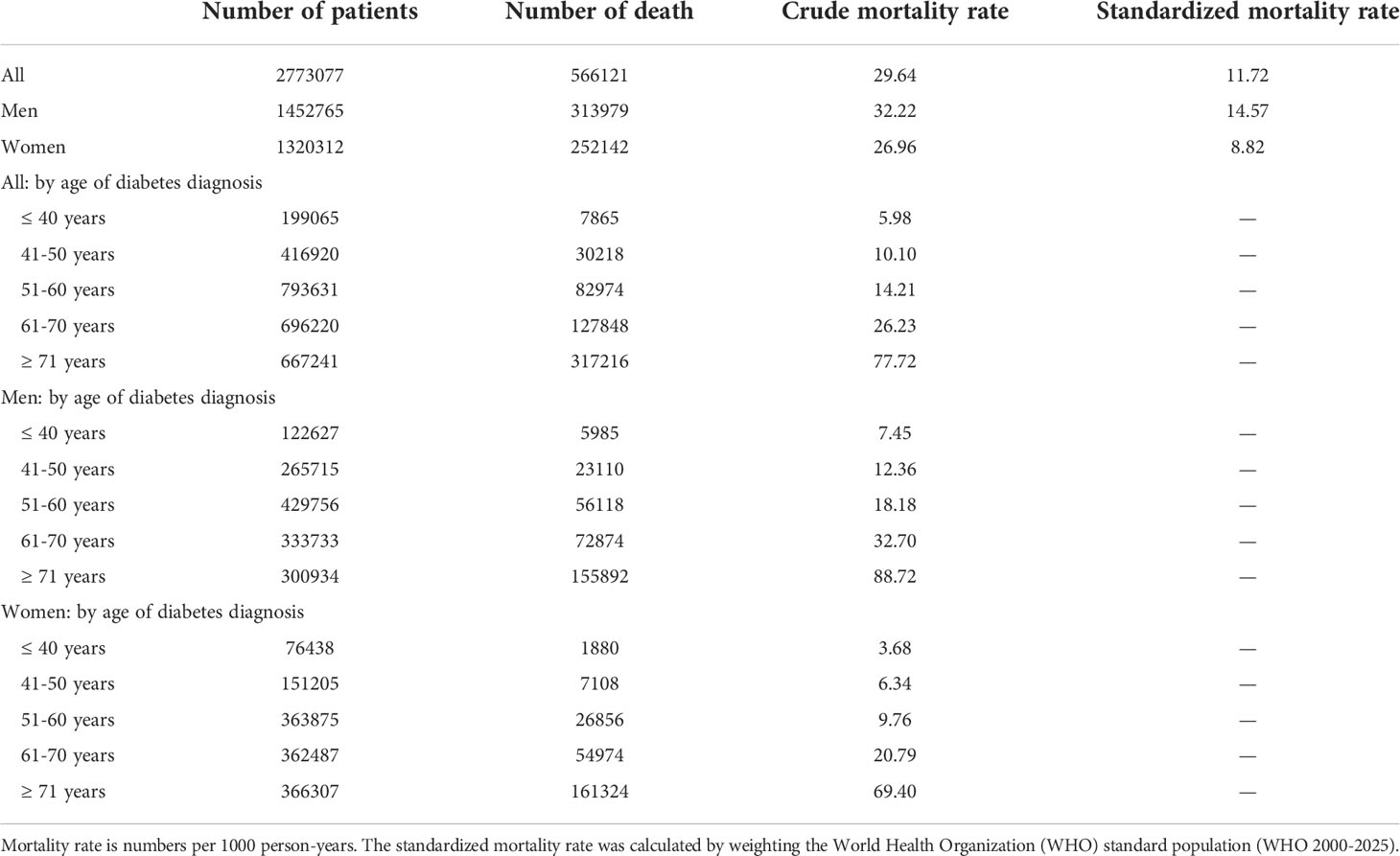
Table 1 All-cause mortality rates in patients with diabetes between 2007 and 2017 (follow up to the end of 2018).
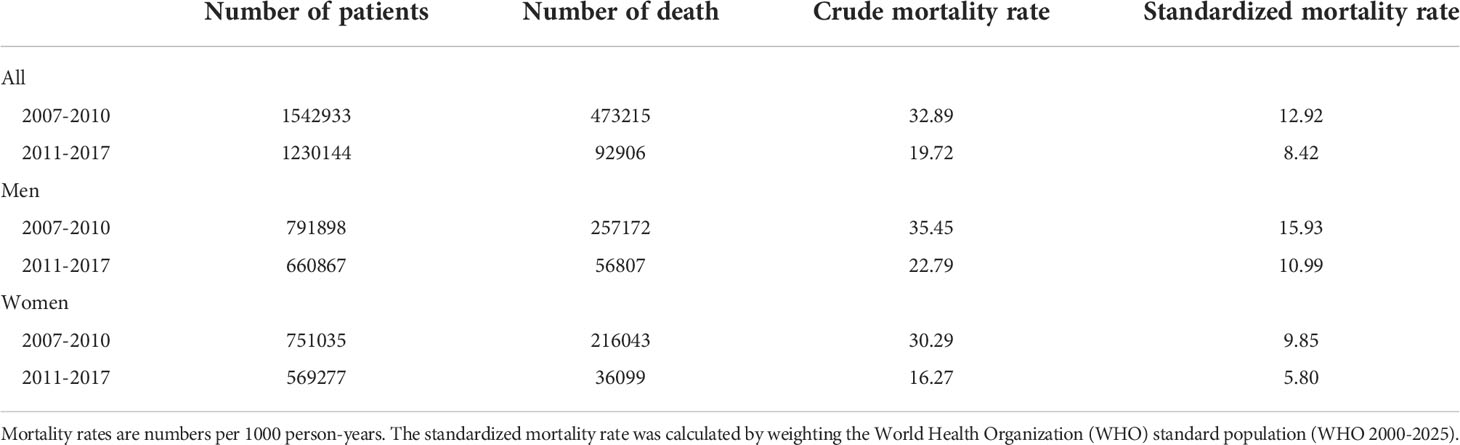
Table 2 All-cause mortality rates in diabetes patients by year of diabetes diagnosis (2007-2010 versus 2011-2017, follow up to 2018).
The major causes of death in patients with diabetes between 2007 and 2017 are shown in Table 3. The top 5 causes of death accounted for nearly 70% (394664/566121, 69.7%) of the total number of deaths. Malignancy (23.2%) was the leading cause of death, followed by diabetes (16.7%), heart disease (11.6%), hypertensive disease (11.3%), and cerebrovascular disease (7.0%). Men had a higher mortality rate than women in all the 5 causes of death, and the findings were consistent across all age subgroups.
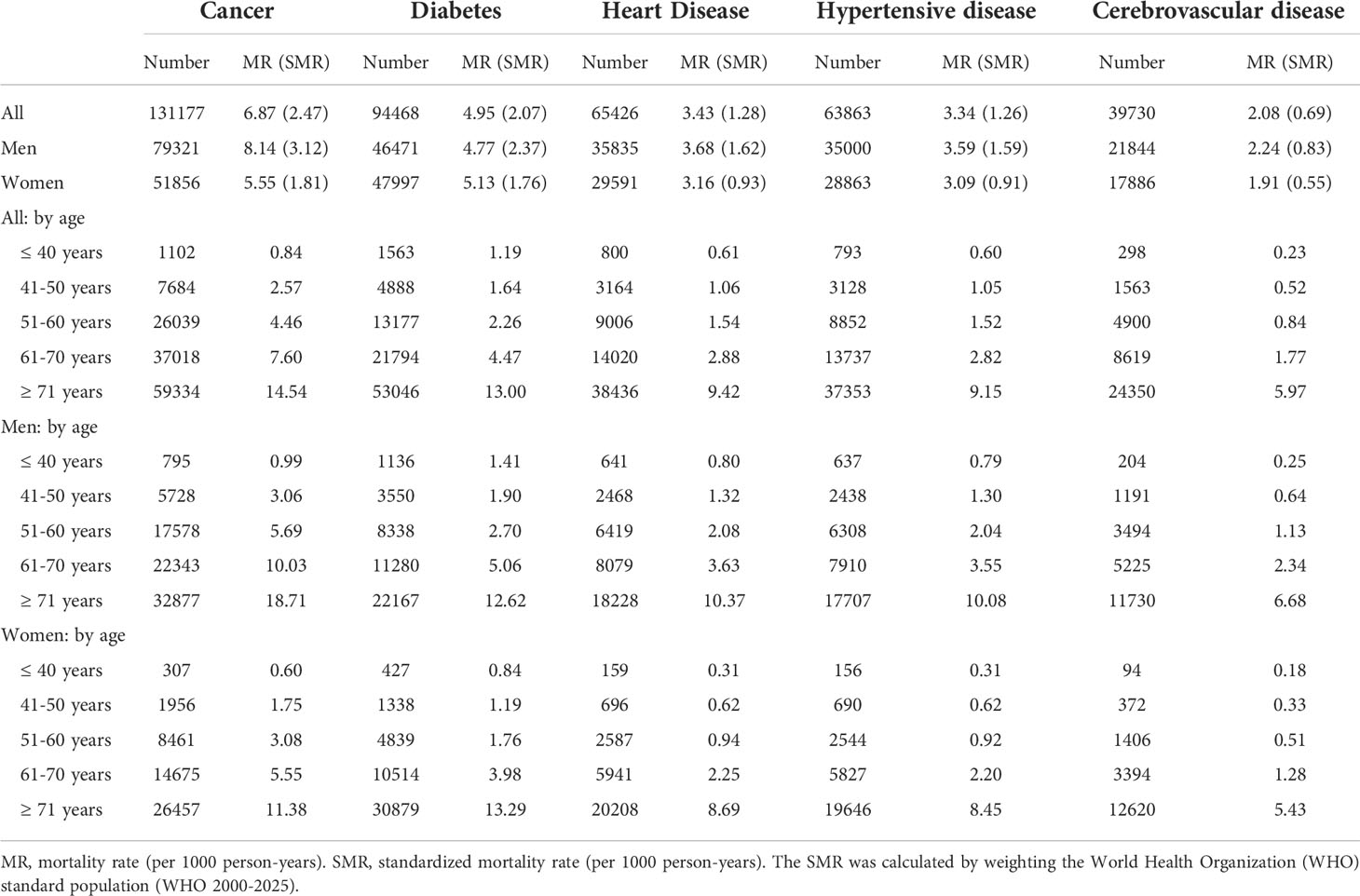
Table 3 Major causes of death in patients with diabetes between 2007 and 2017 (follow up to the end of 2018).
Table 4 shows the major causes of death by year of diabetes diagnosis (2007-2010 vs. 2011-2017). With respect to the top 5 causes of death, patients with diabetes diagnosed in 2011-2017 had a lower crude mortality rate and SMR than those diagnosed in 2007-2010. For example, the crude mortality rate and SMR for cancer (follow up to the end of 2018) in patients with diabetes diagnosed between 2007 and 2010 were 7.26 and 2.60 (per 1000 person-years), respectively. The respective rates in those diagnosed between 2011 and 2017 were 5.66 and 2.12 (per 1000-person years). The findings were consistent in men and in women.
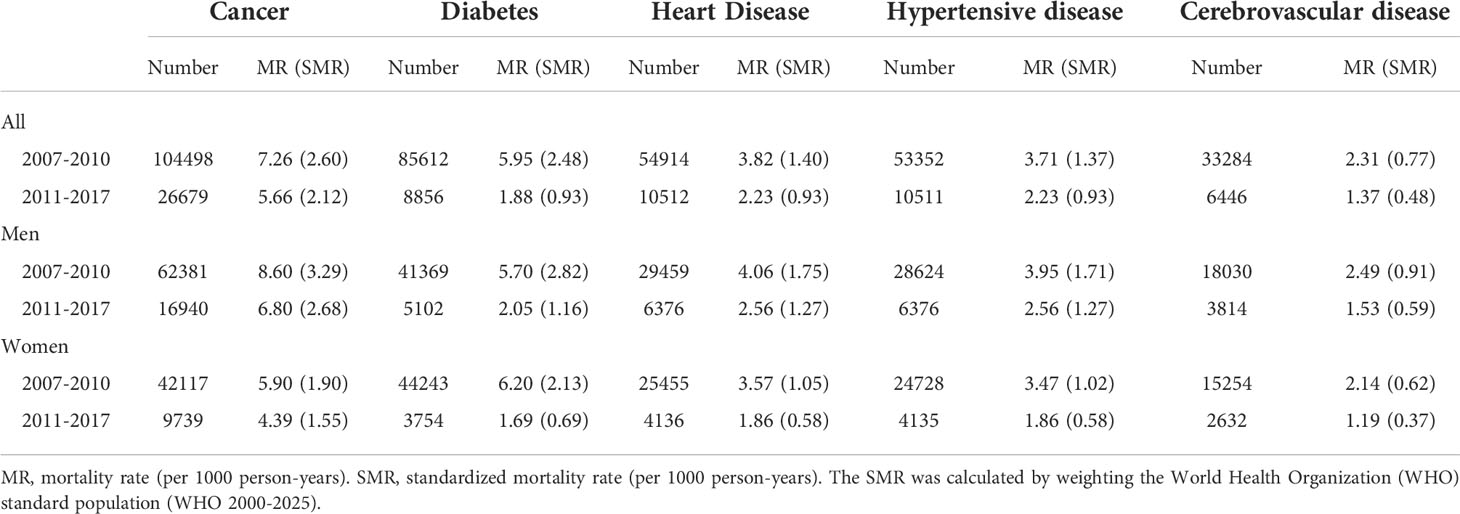
Table 4 Major causes of death in patients with diabetes by year of diabetes diagnosis (2007-2010 versus 2011-2017, follow up to the end of 2018).
The survival rates after the diagnosis of diabetes according to year of diagnosis are shown in Figure 1. Compared with patients who were diagnosed in 2008-2010, those who were diagnosed in 2011-2014 and 2015-2018 had a higher 3-year survival rate (0.9356 vs. 0.9438 vs. 0.946, log-rank test p<0.001) after the diagnosis of diabetes.
Discussion
In this study, we investigated all-cause mortality rate and major causes of death between 2007 and 2018 in patients with diabetes in Taiwan. We demonstrated that patients with diabetes diagnosed in 2011-2017 had a lower all-cause mortality rate (SMR 8.42 vs. 12.92 per 1000 person-years) than those diagnosed in 2007-2010. The findings were consistent in men and in women. Similar results were noted regarding the major causes of death (cancer, diabetes, heart disease, hypertensive disease, and cerebrovascular disease). Our results suggested an outcome improvement in diabetes patients during 2007-2018 in Taiwan.
All-cause mortality rate in patients with diabetes has declined in the past decades (6, 18–20). In a recent report (21), all-cause mortality rates among people with diabetes in high-income countries continue to decline between 1995 and 2016. The improvement in patients’ survival may be explained by optimal control of risk factors (8–10, 22) and the use of guidelines-recommended treatment (23, 24). In patients with diabetes in Taiwan, the control rates of glycemia, blood pressure, and low-density lipoprotein cholesterol (25–27), as well as the use of statins (28), continuously increased during our study period. Furthermore, the promotion of pay-for-performance program for diabetes care (29, 30) may also contribute to the reduction of all-cause mortality rate in our patients. The standardized mortality rate in our study (8-13 per 1000 person-years) was similar to the finding in a previous study (~15 per 1000 person-years) (31), which also revealed a decline in all-cause mortality rate in patients with diabetes between 1996 and 2009. Advances in the availability and performance of technology, developments of new drugs, pleiotropic effects of guidelines-recommended treatment (32), and technology-assisted facilitation of disease screening and patients’ follow-up (33, 34) may all contribute to the improvements in outcomes.
The decline in all-cause mortality rate was consistently observed in the major causes of deaths in our study population. The SMR (per 1000 person-years) of cancer mortality in 2007-2010 and 2011-2017 was 7.26 and 5.66, respectively (Table 4). Similar declines in the other causes of deaths (diabetes, heart disease, hypertensive disease, and cerebrovascular disease) were observed. Since cancer and cardiovascular disease share similar risk factors (35), it may not be surprised that improvement in diabetes care, the use of guidelines-recommended treatment (such as metformin) (32, 36), and optimal control of risk factors lead to a decline in rates of cancer and cardiovascular mortality. However, patients with diabetes remain at a higher risk of mortality compared with patients without diabetes (6, 37, 38). In 2018, the crude mortality rate and SMR of the Taiwan population were 7.33 and 4.15 per 1000 person-years, respectively (https://dep.mohw.gov.tw/DOS/lp-5069-113.html ). The respective rates of our study population were 29.64 and 11.72 per 1000 person-years (Table 1). According to our findings, cancer and cardiovascular diseases remain the major causes of death in patients with diabetes in Taiwan. Inflammatory pathways associated with adipose tissue (39, 40) have been associated with an increase in oxidative and cellular stress (39, 40). These may contribute to the chronic inflammation and unfavorable outcomes in patients with diabetes and cardiovascular diseases (41) or heart failure (42, 43). Hence, continuous efforts are required to promote health care for patients with diabetes to improve their outcomes despite our encouraging findings.
There are several limitations in this study. First, we did not have data on glycemia, blood pressure, and lipid profiles. These are important factors related to diabetes care and risk of mortality. Second, we did not have data on relevant medications, such as glucose- and blood pressure-lowering drugs, as well as statins. The use of some guidelines-recommended drugs (e.g. statins) may help reduce mortality risk in patients with diabetes (23, 24). Unfortunately, this cannot be examined in this study. Final, relevant information on lifestyles, such as smoking, alcohol consumption, and physical activity, are lacking. All these issues may influence patients’ survival and should be addressed in future studies. Despite the aforementioned limitations, our findings from a large database may provide insight on diabetes care program and health promotion policy.
In conclusion, we demonstrated an outcome improvement in patients with diabetes in Taiwan. Patients who were diagnosed with diabetes after 2011 had a lower rate of all-cause mortality and major causes of death, compared with those who were diagnosed before 2010. These promising findings may have implications for healthcare systems.
Data availability statement
The datasets presented in this article are not readily available due to privacy/ethical restrictions. Requests to access the datasets should be directed to C-CH, https://cch@nhri.edu.tw.
Ethics statement
The studies involving human participants were reviewed and approved by The Research Ethics Committee of the National Health Research Institute. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author contributions
J-SW, H-YO, Y-SY, and C-MH contributed to conception and design of the study. Y-LW, C-CH, and C-MH organized the database. Y-LW and C-CH performed the statistical analysis. J-SW and Y-LW wrote the first draft of the manuscript. H-YO, Y-SY, C-CH, and C-MH reviewed and edited the manuscript. All authors contributed to manuscript revision, read, and approved the submitted version.
Funding
This research was funded by the Diabetes Association of the Republic of China [grant number DAROC2021ATLAS-0001, 2021] and the Taiwanese Association of Diabetes Educators [grant number TADE-2021-RES-01, 2021]. The sponsors had no role in the design, execution, interpretation, or writing of the study.
Acknowledgments
We thank the Health and Welfare Data Science Center for providing data and Institute of Population Health Sciences, National Health Research Institutes for performing analysis.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Internal Diabetes Federation. IDF diabetes atlas 10th edition 2021. Available at: https://diabetesatlas.org/atlas/tenth-edition/ (Accessed Feb 15, 2022).
2. Sheen YJ, Hsu CC, Jiang YD, Huang CN, Liu JS, Sheu WH. Trends in prevalence and incidence of diabetes mellitus from 2005 to 2014 in Taiwan. J Formos Med Assoc (2019) 118 Suppl 2:S66–73. doi: 10.1016/j.jfma.2019.06.016
3. Zheng Y, Ley SH, Hu FB. Global aetiology and epidemiology of type 2 diabetes mellitus and its complications. Nat Rev Endocrinol (2018) 14:88–98. doi: 10.1038/nrendo.2017.151
4. Gregg EW, Sattar N, Ali MK. The changing face of diabetes complications. Lancet Diabetes Endocrinol (2016) 4:537–47. doi: 10.1016/S2213-8587(16)30010-9
5. Shah AD, Langenberg C, Rapsomaniki E, Denaxas S, Pujades-Rodriguez M, Gale CP, et al. Type 2 diabetes and incidence of cardiovascular diseases: a cohort study in 1•9 million people. Lancet Diabetes Endocrinol (2015) 3:105–13. doi: 10.1016/S2213-8587(14)70219-0
6. Rawshani A, Rawshani A, Franzén S, Eliasson B, Svensson AM, Miftaraj M, et al. Mortality and cardiovascular disease in type 1 and type 2 diabetes. N Engl J Med (2017) 376:1407–18. doi: 10.1056/NEJMoa1608664
7. GBD 2013 Mortality and Causes of Death Collaborators. Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990-2013: a systematic analysis for the global burden of disease study 2013. Lancet (2015) 385:117–71. doi: 10.1016/S0140-6736(14)61682-2
8. UK Prospective Diabetes Study (UKPDS) Group. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet (1998) 352:837–53. doi: 10.1016/S0140-6736(98)07019-6
9. Holman RR, Paul SK, Bethel MA, Matthews DR, Neil HA. 10-year follow-up of intensive glucose control in type 2 diabetes. N Engl J Med (2008) 359:1577–89. doi: 10.1056/NEJMoa0806470
10. Gaede P, Vedel P, Larsen N, Jensen GV, Parving HH, Pedersen O. Multifactorial intervention and cardiovascular disease in patients with type 2 diabetes. N Engl J Med (2003) 348:383–93. doi: 10.1056/NEJMoa021778
11. Hsieh HM, Lin TH, Lee IC, Huang CJ, Shin SJ, Chiu HC. The association between participation in a pay-for-performance program and macrovascular complications in patients with type 2 diabetes in Taiwan: A nationwide population-based cohort study. Prev Med (2016) 85:53–9. doi: 10.1016/j.ypmed.2015.12.013
12. Chen YC, Lee CT, Lin BJ, Chang YY, Shi HY. Impact of pay-for-performance on mortality in diabetes patients in Taiwan: A population-based study. Med (Baltimore) (2016) 95:e4197. doi: 10.1097/MD.0000000000004197
13. Li HY, Jiang YD, Chang CH, Chung CH, Lin BJ, Chuang LM. Mortality trends in patients with diabetes in Taiwan: a nationwide survey in 2000-2009. J Formos Med Assoc (2012) 111:645–50. doi: 10.1016/j.jfma.2012.09.013
14. Li HY, Wu YL, Tu ST, Hwu CM, Liu JS, Chuang LM. Trends of mortality in diabetic patients in Taiwan: A nationwide survey in 2005-2014. J Formos Med Assoc (2019) 118 Suppl 2:S83–9. doi: 10.1016/j.jfma.2019.07.008
15. Wang JS, Wu YL, Shin SJ, Tien KJ, Chin MC, Hwu CM. Hospitalization in patients with type 2 diabetes mellitus in Taiwan: A nationwide population-based observational study. J Formos Med Assoc (2019) 118 Suppl 2:S90–5. doi: 10.1016/j.jfma.2019.06.017
16. GBD 2016 Healthcare Access and Quality Collaborators. Measuring performance on the healthcare access and quality index for 195 countries and territories and selected subnational locations: a systematic analysis from the global burden of disease study 2016. Lancet (2018) 391:2236–71. doi: 10.1016/S0140-6736(18)30994-2
17. Lin CC, Lai MS, Syu CY, Chang SC, Tseng FY. Accuracy of diabetes diagnosis in health insurance claims data in Taiwan. J Formos Med Assoc (2005) 104:157–63.
18. Gregg EW, Cheng YJ, Srinivasan M, Lin J, Geiss LS, Albright AL, et al. Trends in cause-specific mortality among adults with and without diagnosed diabetes in the USA: an epidemiological analysis of linked national survey and vital statistics data. Lancet (2018) 391:2430–40. doi: 10.1016/S0140-6736(18)30314-3
19. Harding JL, Shaw JE, Peeters A, Guiver T, Davidson S, Magliano DJ. Mortality trends among people with type 1 and type 2 diabetes in Australia: 1997-2010. Diabetes Care (2014) 37:2579–86. doi: 10.2337/dc14-0096
20. Chen L, Islam RM, Wang J, Hird TR, Pavkov ME, Gregg EW, et al. A systematic review of trends in all-cause mortality among people with diabetes. Diabetologia (2020) 63:1718–35. doi: 10.1007/s00125-020-05199-0
21. Magliano DJ, Chen L, Carstensen B, Gregg EW, Pavkov ME, Salim A, et al. Trends in all-cause mortality among people with diagnosed diabetes in high-income settings: a multicountry analysis of aggregate data. Lancet Diabetes Endocrinol (2022) 10:112–9. doi: 10.1016/S2213-8587(21)00327-2
22. Joseph JJ, Deedwania P, Acharya T, Aguilar D, Bhatt DL, Chyun DA, et al. Comprehensive management of cardiovascular risk factors for adults with type 2 diabetes: A scientific statement from the American heart association. Circulation (2022) 145:e722–59. doi: 10.1161/CIR.0000000000001040
23. Cosentino F, Grant PJ, Aboyans V, Bailey CJ, Ceriello A, Delgado V, et al. 2019 ESC guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD. Eur Heart J (2020) 41:255–323. doi: 10.1093/eurheartj/ehz486
24. Colling C, Atlas SJ, Wexler DJ. Application of 2021 American diabetes association glycemic treatment clinical practice recommendations in primary care. Diabetes Care (2021) 44:1443–6. doi: 10.2337/dc21-0013
25. Yu NC, Su HY, Tsai ST, Lin BJ, Shiu RS, Hsieh YC, et al. ABC Control of diabetes: survey data from national diabetes health promotion centers in Taiwan. Diabetes Res Clin Pract (2009) 84:194–200. doi: 10.1016/j.diabres.2009.02.020
26. Yu NC, Su HY, Chiou ST, Yeh MC, Yeh SW, Tzeng MS, et al. Trends of ABC control 2006-2011: a national survey of diabetes health promotion institutes in Taiwan. Diabetes Res Clin Pract (2013) 99:112–9. doi: 10.1016/j.diabres.2012.11.018
27. Wang CY, Tu ST, Sheu WH, Chen IC, Chuang LM, Wu MS, et al. National survey of ABC (A1C, blood pressure, cholesterol) of diabetes health promotion institutes in Taiwan: 2002-2018. J Formos Med Assoc (2018) 117:952–4. doi: 10.1016/j.jfma.2018.08.013
28. Hsieh HC, Hsu JC, Lu CY. 10-year trends in statin utilization in Taiwan: a retrospective study using taiwan’s national health insurance research database. BMJ Open (2017) 7:e014150. doi: 10.1136/bmjopen-2016-014150
29. Chou CW, Kung PT, Chou WY, Tsai WC. Pay-for-performance programmes reduce stroke risks in patients with type 2 diabetes: a national cohort study. BMJ Open (2019) 9:e026626. doi: 10.1136/bmjopen-2018-026626
30. Kung FP, Tsai CF, Lu CL, Huang LC, Lu CH. Diabetes pay-for-performance program can reduce all-cause mortality in patients with newly diagnosed type 2 diabetes mellitus. Med (Baltimore) (2020) 99:e19139. doi: 10.1097/MD.0000000000019139
31. Lind M, Garcia-Rodriguez LA, Booth GL, Cea-Soriano L, Shah BR, Ekeroth G, et al. Mortality trends in patients with and without diabetes in Ontario, Canada and the UK from 1996 to 2009: a population-based study. Diabetologia (2013) 56:2601–8. doi: 10.1007/s00125-013-3063-1
32. Caturano A, Galiero R, Pafundi PC. Metformin for type 2 diabetes. JAMA (2019) 322:1312. doi: 10.1001/jama.2019.11489
33. Galiero R, Pafundi PC, Nevola R, Rinaldi L, Acierno C, Caturano A, et al. The importance of telemedicine during COVID-19 pandemic: A focus on diabetic retinopathy. J Diabetes Res (2020) 2020:9036847. doi: 10.1155/2020/9036847
34. Sasso FC, Pafundi PC, Gelso A, Bono V, Costagliola C, Marfella R, et al. Telemedicine for screening diabetic retinopathy: The NO BLIND Italian multicenter study. Diabetes Metab Res Rev (2019) 35:e3113. doi: 10.1002/dmrr.3113
35. Koene RJ, Prizment AE, Blaes A, Konety SH. Shared risk factors in cardiovascular disease and cancer. Circulation (2016) 133:1104–14. doi: 10.1161/CIRCULATIONAHA.115.020406
36. Morgillo F, Fasano M, Della Corte CM, Sasso FC, Papaccio F, Viscardi G, et al. Results of the safety run-in part of the METAL (METformin in advanced lung cancer) study: a multicentre, open-label phase I-II study of metformin with erlotinib in second-line therapy of patients with stage IV non-small-cell lung cancer. ESMO Open (2017) 2:e000132. doi: 10.1136/esmoopen-2016-000132
37. Kang YM, Kim YJ, Park JY, Lee WJ, Jung CH. Mortality and causes of death in a national sample of type 2 diabetic patients in Korea from 2002 to 2013. Cardiovasc Diabetol (2016) 15:131. doi: 10.1186/s12933-016-0451-0
38. Yang JJ, Yu D, Wen W, Saito E, Rahman S, Shu XO, et al. Association of diabetes with all-cause and cause-specific mortality in Asia: A pooled analysis of more than 1 million participants. JAMA Netw Open (2019) 2:e192696. doi: 10.1001/jamanetworkopen.2019.2696
39. D’Onofrio N, Pieretti G, Ciccarelli F, Gambardella A, Passariello N, Rizzo MR, et al. Abdominal fat SIRT6 expression and its relationship with inflammatory and metabolic pathways in pre-diabetic overweight patients. Int J Mol Sci (2019) 20:1153. doi: 10.3390/ijms20051153
40. Sardu C, Pieretti G, D’Onofrio N, Ciccarelli F, Paolisso P, Passavanti MB, et al. Inflammatory cytokines and SIRT1 levels in subcutaneous abdominal fat: Relationship with cardiac performance in overweight pre-diabetics patients. Front Physiol (2018) 9:1030. doi: 10.3389/fphys.2018.01030
41. Sardu C, Paolisso G, Marfella R. Inflammatory related cardiovascular diseases: From molecular mechanisms to therapeutic targets. Curr Pharm Des (2020) 26:2565–73. doi: 10.2174/1381612826666200213123029
42. Sardu C, Barbieri M, Santamaria M, Giordano V, Sacra C, Paolisso P, et al. Multipolar pacing by cardiac resynchronization therapy with a defibrillators treatment in type 2 diabetes mellitus failing heart patients: impact on responders rate, and clinical outcomes. Cardiovasc Diabetol (2017) 16:75. doi: 10.1186/s12933-017-0554-2
43. Sardu C, Santamaria M, Funaro S, Sacra C, Barbieri M, Paolisso P, et al. Cardiac electrophysiological alterations and clinical response in cardiac resynchronization therapy with a defibrillator treated patients affected by metabolic syndrome. Med (Baltimore) (2017) 96:e6558. doi: 10.1097/MD.0000000000006558
Keywords: diabetes, mortality, survival, cancer, heart disease
Citation: Wang J-S, Wu Y-L, Ou H-Y, Yang Y-S, Hsu C-C and Hwu C-M (2022) Trends in all-cause mortality and major causes of death between 2007 and 2018 among patients with diabetes in Taiwan. Front. Endocrinol. 13:984137. doi: 10.3389/fendo.2022.984137
Received: 01 July 2022; Accepted: 15 July 2022;
Published: 09 August 2022.
Edited by:
Ferdinando Carlo Sasso, University of Campania Luigi Vanvitelli, ItalyReviewed by:
Alfredo Caturano, University of Campania Luigi Vanvitelli, ItalyCelestino Sardu, University of Campania Luigi Vanvitelli, Italy
Copyright © 2022 Wang, Wu, Ou, Yang, Hsu and Hwu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Chih-Cheng Hsu, Y2NoQG5ocmkuZWR1LnR3; Chii-Min Hwu, Y2hod3VAdmdodHBlLmdvdi50dw==
†These authors have contributed equally to this work and share senior authorship
 Jun-Sing Wang
Jun-Sing Wang Yi-Ling Wu5
Yi-Ling Wu5 Horng-Yih Ou
Horng-Yih Ou Yi-Sun Yang
Yi-Sun Yang Chih-Cheng Hsu
Chih-Cheng Hsu Chii-Min Hwu
Chii-Min Hwu