
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Endocrinol. , 31 October 2022
Sec. Obesity
Volume 13 - 2022 | https://doi.org/10.3389/fendo.2022.972954
This article is part of the Research Topic Pediatric Obesity: How to Diverge from Developmental Pathways? View all 6 articles
Background: Pediatric obesity has become a global public health problem. China has the largest population of obese children in the world. It is important to develop effective interventions to control child obesity. This systematic review summarizes proof from randomized controlled trials to assess the efficacy of lifestyle intervention to reduce BMI and metabolic risk factors for overweight/obese Chinese children.
Methods: We searched studies from five databases (PubMed, MEDLINE, EMBASE, Cochrane Database of Systematic Reviews, and CNKI). Research that meets the following requirements was included: randomized controlled trials, participants are overweight/obese Chinese children aged <18 years old, and the effectiveness of lifestyle interventions is evaluated.
Results: Eight randomized controlled trials were included. A significant difference was found between the intervention group and the control group for the BMI changes (mean difference = −1.49; 95% CI: −2.20 to -0.77; p < 0.001). Subgroup analyses consistently demonstrated that effects of lifestyle interventions on BMI change including multiple-component interventions (mean difference = −2.03 kg/m2; 95% CI: −3.62 to -0.43; p < 0.001) were stronger than those only with physical activities or health education; effects of lifestyle interventions on BMI change were also strengthened if duration of intervention last for more than 1 year (mean difference = −3.03 kg/m2; 95% CI: −4.00 to -2.06; p = 0.01) or with age during 12-18 years old (mean difference = −1.90 kg/m2; 95% CI: −3.37 to -0.43; p < 0.001).
Conclusions: Lifestyle interventions are effective in reducing BMI in Chinese children with overweight/obesity, and the effectiveness is more profound when the lifestyle intervention includes multiple components, lasts longer than one year, and/or is conducted among teens. These findings provide an important evidence base for developing and implementing potentially effective lifestyle interventions for the treatment of overweight/obesity among Chinese children.
Pediatric obesity has become a global public health problem (1, 2). China’s latest census results show that the national prevalence in 2015-2019 is estimated to be 6.8% for overweight and 3.6% for obesity in children younger than 6 years, 11.1% for overweight and 7.9% for obesity in 6–17 years’ children and adolescents (3). Childhood obesity is correlated with metabolic disorders like elevated blood pressure, type 2 diabetes, and metabolic syndrome (3–5), which often persist into adulthood (5). Therefore, it is critical to manage and treat overweight and obesity in children.
Lifestyle interventions are the first-line treatment for childhood obesity (6). Several types of interventions, including physical activity (PA), dietary improvement (DI), and health education (HE) have been applied to address overweight and obesity in children (7–9). However, evidence of potential efficacy applies mostly to children in western countries (6, 10, 11), the efficacy and feasibility of lifestyle interventions in children and adolescents in China lack evidence, particularly from systematic reviews, which hinders the development of childhood obesity management in China. It is vital to assess the changes in cardiovascular metabolic outcomes which are closely related to changes in body weight or BMI (12, 13).
Systematic review and meta-analysis of randomized controlled trials were carried out to evaluate the effectiveness of lifestyle intervention for the treatment of overweight/obesity in children in China and to examine the characteristics of intervention components associated with the improvement of metabolic outcomes. Expected results may help children maintain a healthy weight. We speculated that lifestyle intervention improves metabolic outcomes for Chinese overweight/obese children.
We searched the five databases (PubMed, MEDLINE, EMBASE, Cochrane Database of Systematic Reviews, and CNKI) to identify RCTs of lifestyle interventions for overweight/obesity among children in China. Both English and non-English language publications between January 1980 and April 2022 were included. We conducted the literature search process using the following keywords (Pediatric Obesity OR Obesity in Childhood OR Childhood Onset Obesity OR Child Obesity OR Childhood Obesity OR Adolescent Obesity OR Childhood Overweight OR Adolescent Overweight) AND (Behavior OR Lifestyle OR Suppress Appetite OR Diet OR Exercise OR Running OR Jogging OR Swimming OR Walk OR Education OR Courses) AND (Therapy OR Management OR Treatment OR Intervention OR Adjustment).
Included researches meet the following criteria (1): individual RCT (2), investigating lifestyle interventions in Chinese children with overweight/obesity (3), collecting anthropometric data through physical examination and calculating body mass index (BMI) (4), providing a brief description of the intervention group and comparison group (5), the full-text publications available. We excluded studies that did not report BMI changes or any metabolic outcome changes.
The main results were changes in BMI. Secondary outcomes were metabolic outcomes including changes in fasting blood glucose (FBG), blood pressure, total cholesterol, low-density lipoprotein [LDL], high-density lipoprotein [HDL], and triglyceride [TG].
We carefully read the reports of each study, including the intervention and the control group measures, the participants’ numbers, the participant age, the trial period, and the metabolic outcomes. Cochrane risk of bias tools was applied to evaluate the methodological quality of RCT (14, 15). Review manager 5.4 was used to create a visual representation of the results of the risk of bias evaluation.
We calculated pooled mean difference (MD) with a 95% confidence interval (CI) for outcomes. We assessed heterogeneity with the I2 test and Chi-square statistics. When heterogeneity across studies was considerable (I2 ≥ 50%), the weighted results are summarized using a random effects model (16). We conducted subgroup analyses to explore the source of heterogeneity. Then, we classified interventions according to specified intervention components (HE, PA, and DI), duration of intervention, and age. Results with P < 0.05 are reported as significant. We performed statistical analysis with the RevMan Version 5.4.
Figure 1 shows our screening process and rational for excluding studies. Eight RCTs were included in the meta-analysis (17–24). Among them, two studies (17, 20) grouped the intervention participants by 3 intervention groups and reported the results separately. Each intervention group has been seen as a single study and analyzed independently. The 12 studies included boys and girls from 6 to 18 years old. All data were extracted from the published papers. Table 1 reported the characteristics of the included studies. Four studies describing favorable consequences evaluating combined diet and PA interventions (20–22, 24). The other studies showed meaningful intervention effects on BMI, and they have the following characteristics: at least 30-minute moderate exercise each day (n=3), only education sessions (n=2), combined HE and PA interventions (n=2), and record diary behavior (n=1).
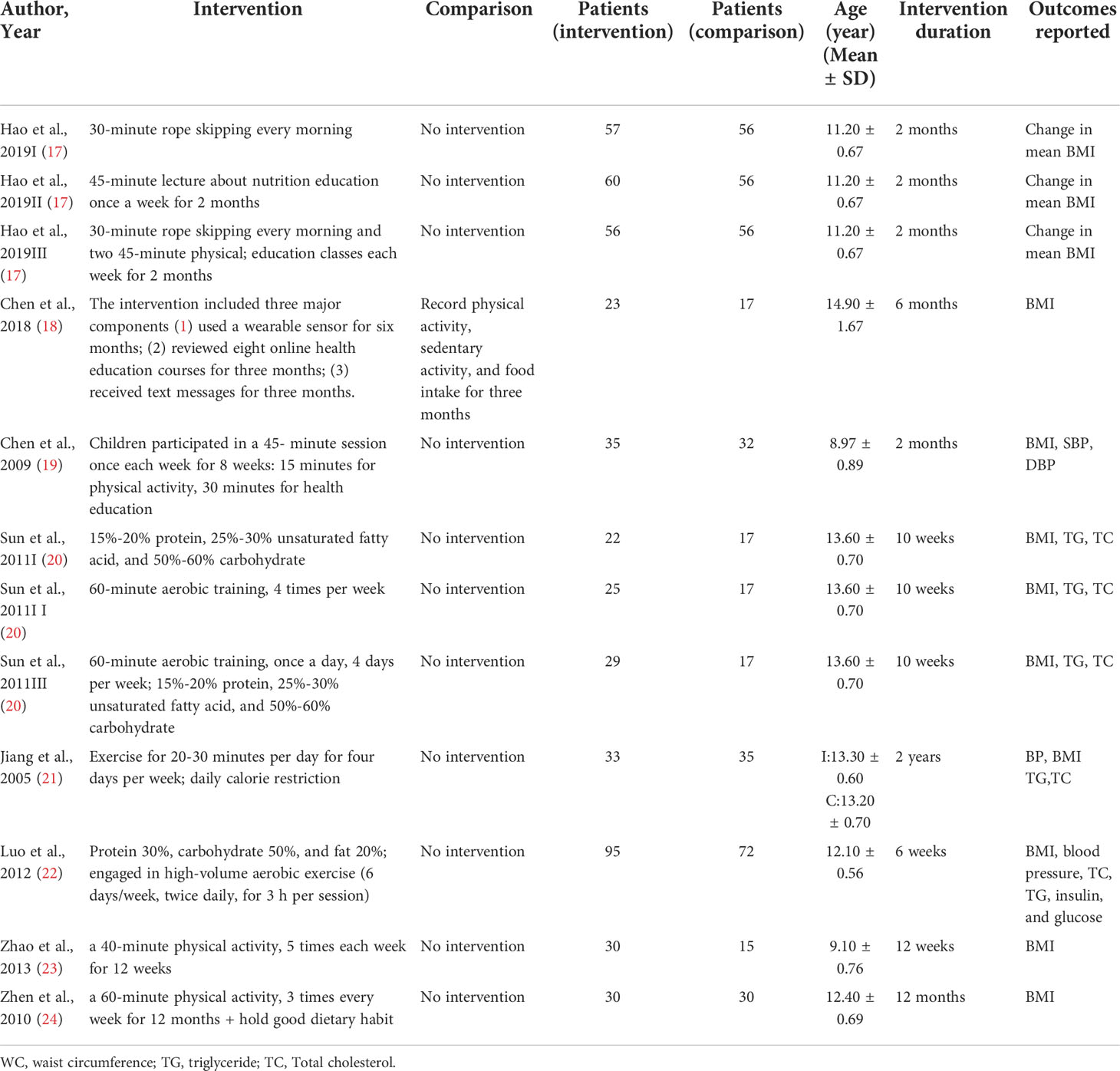
Table 1 Characteristics of studies on the effects of lifestyle interventions for children with overweight/obesity.
Figure 2 shows the results of methodological quality evaluation. Due to the inadequate details of the methodological report, 45.2% of the judges among all departments were “the obvious dangers of bias”. Two of the 12 studies had a high risk for at least one department. Low bias risks accounted for 52.4% of all departments.
The overall effect size of 12 studies that reported BMI as an outcome was summarized in Figure 3. All of the 12 studies with BMI as an outcome showed a significant effect in favor of the intervention group. A quantitative synthesis of studies by a total of 915 participants showed significantly reduced BMI compared to the control group(mean difference = -1.49; 95%CI:-2.20~-0.77; P<0.00001). However, substantial heterogeneity was detected among the studies (I2 = 99%; p < 0.0001).
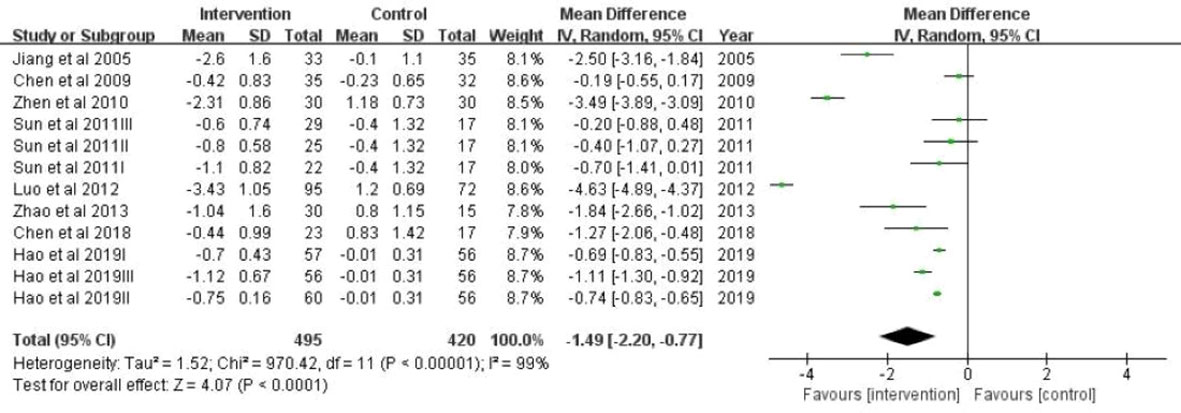
Figure 3 A forest plot providing data on the impact of lifestyle interventions on BMI with 95% confidence intervals of individual studies. Using a random effects model and an inverse variance method, a summary estimate of the 95% confidence interval was calculated. SD, standard deviation; IV, inverse variance; CI, confidence interval.
Figure 4 showed the results of subgroup analyses that BMI was significantly different by whether or not the studies including multi-component interventions. The effects of lifestyle interventions on BMI change including multiple-component interventions (n = 5) were -2.03 (95% CI: -3.62, -0.43) kg/m2, which were stronger than those only with physical activities (n = 3) (pooled BMI = -0.90; (95% CI: -1.53, -0.27) kg/m2) or only with health education (n = 2) (pooled BMI =-0.85 (95% CI: -1.28, -0.43) kg/m2).
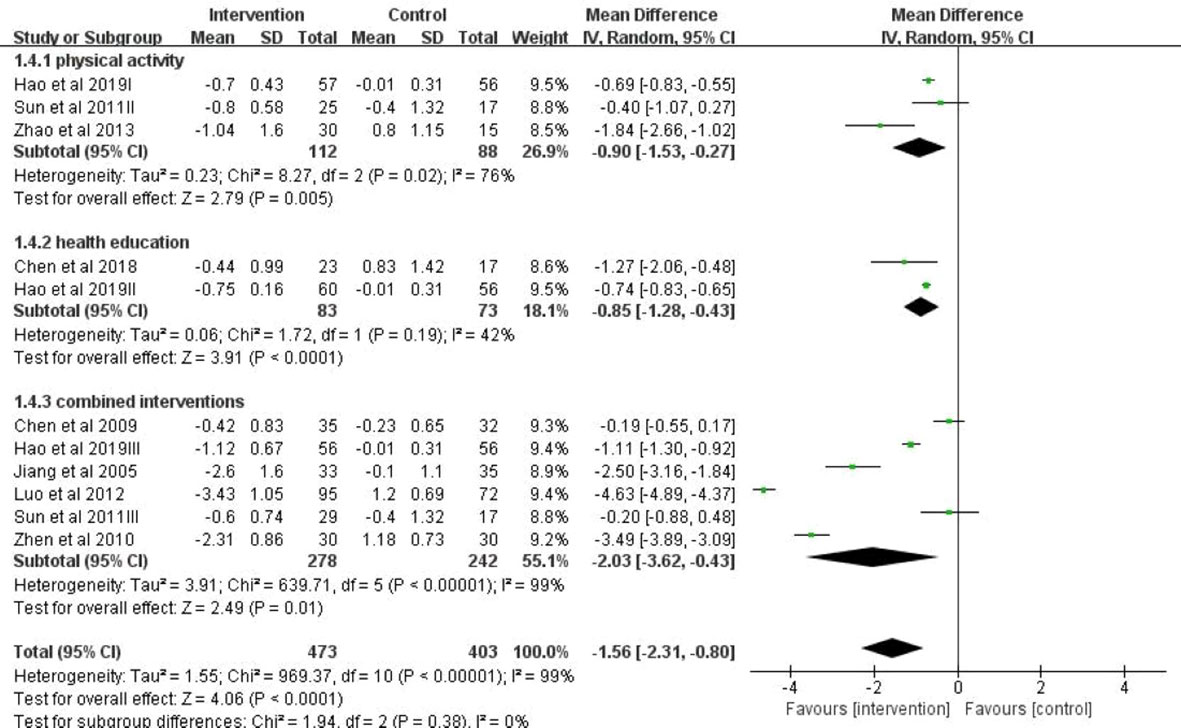
Figure 4 A forest plot providing data on the impact of lifestyle interventions on BMI with 95% confidence intervals of individual studies, grouped by intervention type. Using a random effects model and an inverse variance method, a summary estimate of the 95% confidence interval was calculated. SD, standard deviation; IV, inverse variance; CI, confidence interval.
The subgroup analysis also showed significant differences in the BMI change by different duration of intervention (Figure 5). When the intervention period was over 1 year (mean difference = -3.03; 95% CI: -4.00, -2.06), this preventive effect was even more remarkable compared with the subgroup with intervention duration <1 year (mean difference = -1.19; 95% CI: -1.93, -0.44).
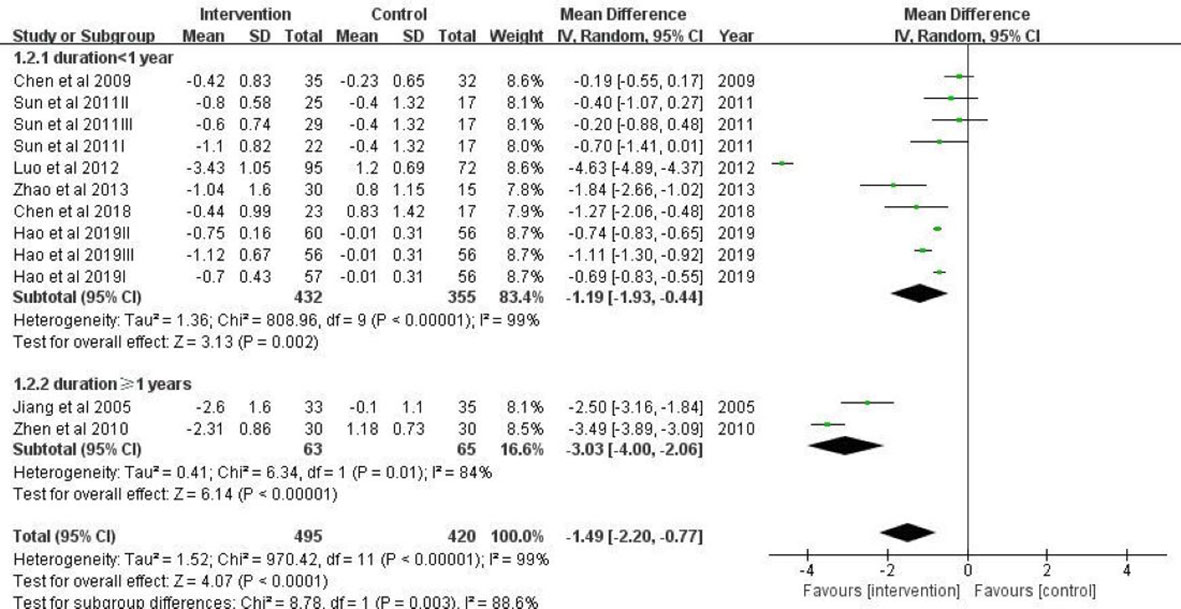
Figure 5 A forest plot providing data on the impact of lifestyle interventions on BMI with 95% confidence intervals of individual studies, grouped by duration of intervention. Using a random effects model and an inverse variance method, a summary estimate of the 95% confidence interval was calculated. SD, standard deviation; IV, inverse variance; CI, confidence interval.
Grouping estimates revealed that a significant effect of lifestyle intervention on BMI was found in studies that focused on adolescents ≥12 years old (mean difference = -1.90; 95% CI:-3.37, -0.43) (Figure 6). In studies conducted in children aged 6-12 years (mean difference = -0.79; 95% CI: -1.04, -0.55), the protective effect was weakened.
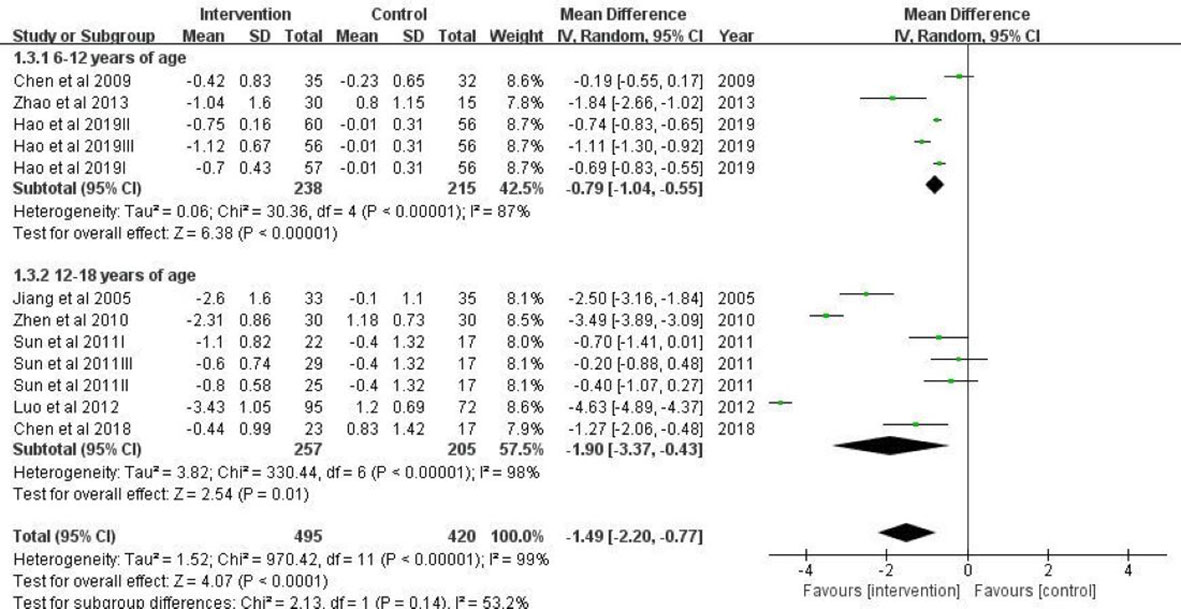
Figure 6 A forest plot providing data on the impact of lifestyle interventions on BMI with 95% confidence intervals of individual studies, grouped by age. Using a random effects model and an inverse variance method, a summary estimate of the 95% confidence interval was calculated. SD, standard deviation; IV, inverse variance; CI, confidence interval.
There is a lack of studies assessing the effects of lifestyle interventions on metabolic outcomes in overweight/obese children in China. Only one study reported changes in fasting blood glucose (FBG) (22). This study included a 6-week dietary and physical intervention in 167 Chinese children with obesity aged 11-13 years. This study observed a significant reduction in FBG only in the girls in intervention group, whereas FBG was unchanged in the boys.
Three studies reported lipids profile changes (20–22). Sun et al. reported 240-minute aerobic training per week significantly reduced serum low-density lipoprotein cholesterol whereas no significant effects of interventions on TG and total cholesterol were observed (20). Jiang et al. reported decreases in total cholesterol and triglycerides after a two-year family-based behavior treatment combining a low-calorie diet and PA intervention (21). Luo et al. reported a 6-week energy-limited diet combined with high-intensity aerobic exercise greatly reduced serum cholesterol and TG (22).
Only Chen et al. and Luo et al. reported blood pressure changes (19, 22). Chen et al. observed that both SBP and DBP decreased in the 8-month study, while no significant change in blood pressure levels was found in the control group. This intervention study combined exercise and health education (19). Luo et al. found decreases in both SBP and DBP after the 6-week energy-limited diet combined with high-intensity aerobic exercise intervention (22).
This systematic review identified eight RCTs of lifestyle interventions against overweight/obese Chinese children and adolescents from January 1, 1980, to April 2022. These studies reported BMI as statistically significant and beneficial interventional effects. These findings support proposals that lifestyle interventions be the focus of obesity management.
All of the randomized controlled trials in our study reported the benefits of lifestyle interventions against children overweight/obesity. Regarding the effectiveness of specific intervention components, we found that integrated interventions that combined diet, exercise, and health education were associated with a decrease in BMI. Our findings are unanimous with the proofs from precedent meta-analyses which suggest that multiple lifestyle changes can be beneficial in controlling children’s weight in the short and long term (25–27). However, because the components of lifestyle interventions vary widely in their implementation effectiveness, further exploration of specific interventions is important for improving the effects of metabolism. Evidence also suggests that the longer duration and older child age are associated with favorable weight-loss consequences, which is consistent with our results (28).
Only exercise intervention can lower the BMI but cannot improve metabolic outcomes. Metabolic outcomes are significantly improved only when exercise combines diet or health education. Prevailing recommendations suggest that schoolchildren should receive at least 60 minutes of moderate exercise each weekday (29). In our study, as short as 20 minutes 4 times of exercise each week appears to have admiring outcomes, especially in declining TG and total cholesterol (21). High volume moderate exercise intervention (3 h per session twice each day*6 day weekly) seems to have significantly admiring results in BMI, FBG, TG, and total cholesterol (22). However, the intervention of this intensity is difficult to achieve in family or school, it can only be achieved in weight-loss camp (30).
The types of dietary interventions do not appear to differ significantly in weight loss, consistent with the findings of a recent meta-analysis that regardless of the nutritional composition of an energy-restricted diet, good metabolic benefits can be achieved, which was also found in adult studies.
As far as we know, this is the first systematic review and meta-analysis using subgroup analyses to systematically review recent research, and analyze the effectiveness of lifestyle interventions for overweight/obese children in China. In addition to BMI, we also assessed metabolic outcomes from lifestyle interventions such as FBG, lipids, and blood pressure, which are common methodological limitations of previous reviews (6, 31–33).
Our results have the following limitations. First, there was considerable heterogeneity in the included studies, and this phenomenon is kindly common in complicated obesity interventions. Because of the restricted number of included studies, it is hard to further explore the origins of heterogeneity using meta-regression. Second, given the limited number of included studies as well as the limited sub-group data available for meta-analyses, it is hard to explore whether metabolic outcomes of intervention components were changed by gender, BMI status, or socio-economic factors of the participant’s population.
From a systematic review and meta-analyses, we found that lifestyle interventions are effective in reducing BMI in Chinese children with overweight/obesity, and the effectiveness is more profound when the lifestyle intervention includes multiple components, lasts longer than one year, and/or is conducted among teens. These findings provide an important evidence base for developing and implementing potentially effective lifestyle interventions for the treatment of overweight/obesity among children in China.
The original contributions presented in the study are included in the article/supplementary material. Further inquiries can be directed to the corresponding authors.
BL and WB conducted the literature search, performed the data extraction, quality assessment and statistical analysis. BL, wrote the original manuscript. ML and SG revised the manuscript. All authors contributed to the article and approved the submitted version.
This work was supported by grants from National Natural Science Foundation of China (81970732), Capital’s Funds for Health Improvement and Research (2020-2Z-40117), and the CAMS Innovation Fund for Medical Sciences (CIFMS) (2021-I2M-1-016) and National High Level Hospital Clinical Research Funding (2022-PUMCH-C-014).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Afshin A, Forouzanfar MH, Reitsma MB, Sur P, Estep K, Lee A, et al. Health effects of overweight and obesity in 195 countries over 25 years. N Engl J Med (2017) 377(1):13–27. doi: 10.1056/NEJMoa1614362
2. World Health Organization Global Health Observatory (GHO). Data: overweight and obesity. updated 2019. Available at: https://www.who.int/gho/ncd/risk_factors/overweight/en/.
3. Pan XF, Wang L, Pan A. Epidemiology and determinants of obesity in China. Lancet Diabetes Endocrinol (2021) 9(6):373–92. doi: 10.1016/s2213-8587(21)00045-0
4. Brown T, Avenell A, Edmunds LD, Moore H, Whittaker V, Avery L, et al. Systematic review of long-term lifestyle interventions to prevent weight gain and morbidity in adults. Obes Rev (2009) 10(6):627–38. doi: 10.1111/j.1467-789X.2009.00641.x
5. Twig G, Yaniv G, Levine H, Leiba A, Goldberger N, Derazne E, et al. Body-mass index in 2.3 million adolescents and cardiovascular death in adulthood. New Engl J Med (2016) 374(25):2430–40. doi: 10.1056/NEJMoa1503840
6. Bleich SN, Vercammen KA, Zatz LY, Frelier JM, Ebbeling CB, Peeters A. Interventions to prevent global childhood overweight and obesity: A systematic review. Lancet Diabetes Endocrinol (2018) 6(4):332–46. doi: 10.1016/s2213-8587(17)30358-3
7. Watson R. EU Parliament backs 30 minutes' exercise a day for all children to tackle obesity. BMJ (2008) 337:a1892. doi: 10.1136/bmj.a1892
8. Woo KS, Chook P, Yu CW, Sung RY, Qiao M, Leung SS, et al. Effects of diet and exercise on obesity-related vascular dysfunction in children. Circulation (2004) 109(16):1981–6. doi: 10.1161/01.Cir.0000126599.47470.Be
9. Lamerz A, Kuepper-Nybelen J, Wehle C, Bruning N, Trost-Brinkhues G, Brenner H, et al. Social class, parental education, and obesity prevalence in a study of six-year-old children in Germany. Int J Obes (2005) 29(4):373–80. doi: 10.1038/sj.ijo.0802914
10. Amini M, Djazayery A, Majdzadeh R, Taghdisi MH, Jazayeri S. Effect of school-based interventions to control childhood obesity: A review of reviews. Int J Prev Med (2015) 6:68. doi: 10.4103/2008-7802.162059
11. Wang Y, Cai L, Wu Y, Wilson RF, Weston C, Fawole O, et al. What childhood obesity prevention programmes work? a systematic review and meta-analysis. Obes Rev (2015) 16(7):547–65. doi: 10.1111/obr.12277
12. Sumithran P, Prendergast LA, Haywood CJ, Houlihan CA, Proietto J. Review of 3-year outcomes of a very-low-energy diet-based outpatient obesity treatment programme. Clin Obes (2016) 6(2):101–7. doi: 10.1111/cob.12135
13. Xu S, Xue Y. Pediatric obesity: Causes, symptoms, prevention and treatment. Exp Ther Med (2016) 11(1):15–20. doi: 10.3892/etm.2015.2853
14. Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. The cochrane collaboration's tool for assessing risk of bias in randomised trials. BMJ (2011) 343:d5928. doi: 10.1136/bmj.d5928
15. Pincus T, Miles C, Froud R, Underwood M, Carnes D, Taylor SJ. Methodological criteria for the assessment of moderators in systematic reviews of randomised controlled trials: A consensus study. BMC Med Res Method (2011) 11:14. doi: 10.1186/1471-2288-11-14
16. Riley RD, Higgins JP, Deeks JJ. Interpretation of random effects meta-analyses. BMJ (2011) 342:d549. doi: 10.1136/bmj.d549
17. Hao M, Han W, Yamauchi T. Short-term and long-term effects of a combined intervention of rope skipping and nutrition education for overweight children in northeast China. Asia Pac J Public Health (2019) 31(4):348–58. doi: 10.1177/1010539519848275
18. Chen JL, Guedes CM, Lung AE. Smartphone-based healthy weight management intervention for Chinese American adolescents: Short-term efficacy and factors associated with decreased weight. J Adolesc Health (2019) 64(4):443–9. doi: 10.1016/j.jadohealth.2018.08.022
19. Chen JL, Weiss S, Heyman MB, Lustig RH. Efficacy of a child-centred and family-based program in promoting healthy weight and healthy behaviors in Chinese American children: A randomized controlled study. J Public Health (Oxf) (2010) 32(2):219–29. doi: 10.1093/pubmed/fdp105
20. Sun MX, Huang XQ, Yan Y, Li BW, Zhong WJ, Chen JF, et al. One-hour after-school exercise ameliorates central adiposity and lipids in overweight Chinese adolescents: A randomized controlled trial. Chin Med J (2011) 124(3):323–9. doi: 10.3760/cma.j.issn.0366-6999.2011.03.001
21. Jiang JX, Xia XL, Greiner T, Lian GL, Rosenqvist U. A two year family based behaviour treatment for obese children. Arch Dis Child (2005) 90(12):1235–8. doi: 10.1136/adc.2005.071753
22. Luo B, Yang Y, Nieman DC, Zhang Y, Wang J, Wang R, et al. A 6-week diet and exercise intervention alters metabolic syndrome risk factors in obese Chinese children aged 11–13 years. J Sport Health Sci (2013) 2(4):236–41. doi: 10.1016/j.jshs.2013.05.001
23. Zhao P. Experimental study on obese pupils by exercise intervention. [dissertation/master’s thesis]. Beijing: Capital University of Physical Education And Sports (2013).
24. Zhen L. The effects of exercise-based comprehensive long-term intervention on overweight and obese children.[dissertation/master’s thesis]. Beijing: Capital University of Physical Education And Sports (2010).
25. Hooper L, Abdelhamid A, Bunn D, Brown T, Summerbell CD, Skeaff CM. Effects of total fat intake on body weight. Cochrane Database Syst Rev (2015) 8):Cd011834. doi: 10.1002/14651858.Cd011834
26. Oude Luttikhuis H, Baur L, Jansen H, Shrewsbury VA, O'Malley C, Stolk RP, et al. Interventions for treating obesity in children. Cochrane Database Syst Rev (2009) 1):Cd001872. doi: 10.1002/14651858.CD001872.pub2
27. Waters E, de Silva-Sanigorski A, Hall BJ, Brown T, Campbell KJ, Gao Y, et al. Interventions for preventing obesity in children. Cochrane Database syst Rev (2011) 12):Cd001871. doi: 10.1002/14651858.CD001871.pub3
28. Wilfley DE, Tibbs TL, Van Buren DJ, Reach KP, Walker MS, Epstein LH. Lifestyle interventions in the treatment of childhood overweight: A meta-analytic review of randomized controlled trials. Health Psychol (2007) 26(5):521–32. doi: 10.1037/0278-6133.26.5.521
29. Promotion OoDPaH. Physical activity guidelines for americans summary (2008). Available at: https://health.gov/paguidelines/guidelines/summary.aspx.
30. Lancaster GI, Febbraio MA. Exercise and the immune system: implications for elite athletes and the general population. Immunol Cell Biol (2016) 94(2):115–6. doi: 10.1038/icb.2015.103
31. Ijaz S, Nobles J, Johnson L, Moore T, Savović J, Jago R. Preventing childhood obesity in primary schools: A realist review from UK perspective. Int J Environ Res Public Health (2021) 18(24):13395. doi: 10.3390/ijerph182413395
32. Brown T, Moore TH, Hooper L, Gao Y, Zayegh A, Ijaz S, et al. Interventions for preventing obesity in children. Cochrane Database Syst Rev (2019) 7(7):Cd001871. doi: 10.1002/14651858.CD001871.pub4
Keywords: lifestyle interventions, pediatric obesity, childhood overweight, treatment, randomized controlled trials
Citation: Li B, Gao S, Bao W and Li M (2022) Effectiveness of lifestyle interventions for treatment of overweight/obesity among children in China: A systematic review and meta-analysis. Front. Endocrinol. 13:972954. doi: 10.3389/fendo.2022.972954
Received: 19 June 2022; Accepted: 17 October 2022;
Published: 31 October 2022.
Edited by:
Violeta Iotova, University Hospital St. Marina, BulgariaReviewed by:
Ying Zhao, Zhejiang University, ChinaCopyright © 2022 Li, Gao, Bao and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ming Li, bGltaW5nQHB1bWNoLmNu; Shan Gao, Z2Fvc2hhbm13QDE2My5jb20=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.