- 1Key Laboratory of Public Health Safety, NHC Key Laboratory of Health Technology Assessment, School of Public Health, Fudan University, Shanghai, China
- 2Guizhou Province Center for Disease Prevention and Control, Chronic Disease Prevention and Cure Research Institute, Guiyang, China
Background and aims: Controversy remains regarding the prediction effects of different adiposity measure indicators for the risk of cardiovascular disease (CVD). Our study aimed to assess the associations of three traditional anthropometric indicators, namely, waist circumference (WC), waist-to-height ratio (WHtR), and body mass index (BMI) as well as three non-traditional anthropometric indicators, namely, the Chinese visceral adiposity index (CVAI), lipid accumulation product (LAP), and body shape index (ABSI), with the risk of CVD among Southwest Chinese population.
Methods: Our study was based on the Guizhou Population Health Cohort Study (GPHCS) conducted from 2010 to 2020. A total of 9,280 participants were recruited from 12 areas in Guizhou Province, China, from November 2010 to December 2012, and followed up for major chronic diseases until December 2020. A total of 7,837 individuals with valid data were included in this analysis. The gender-specific associations of WC, WHtR, BMI, CVAI, LAP, and ABSI with CVD were evaluated using Cox proportional hazards models. Receiver operating characteristic (ROC) curve analysis was used to estimate the prediction powers of different indicators for CVD.
Results: No association of six indicators with CVD was observed among male participants. Female participants with either WC-based central obesity (HR: 1.82, 95% CI: 1.12–2.97) or WHtR-based central obesity (HR: 1.68, 95% CI: 1.07–2.64) had a higher risk of CVD, after adjusted for age, area, ethnic group, smoking, alcohol drinking, MET, previous history of diabetes, hypertension and dyslipidemia, medication use, and nutraceutical intake. Compared with female participants in the lowest quartile (Q1), those in the highest quartile (Q4) of WHtR (HR: 2.24, 95% CI: 1.17–4.27), CVAI (HR: 3.98, 95% CI: 1.87–8.49), and ABSI (HR: 1.94, 95% CI: 1.06–3.52) had an increased risk for incident CVD. CAVI showed the maximum predictive power of CVD with the biggest AUC of 0.687 (95% CI: 0.654–0.720) compared to other indicators in female participants.
Conclusions: Visceral adiposity measures, especially CVAI, are stronger predictive indicators of CVD among female and not male participants in Southwest China. Different anthropometric indexes need to be combined to comprehensively assess health risks.
Introduction
Cardiovascular disease (CVD) remains the leading cause of mortality and morbidity worldwide, with ischemic heart disease (IHD) and stroke as the main contributors (1). It was estimated that CVD caused 17.8 million deaths in 2017 worldwide (2), and 4 million deaths in 2016 in China (3). The burden of IHD and stroke in China has rapidly and substantially increased during the past two decades (4). IHD caused more than 1 million deaths per year, and the number of individuals with acute myocardial infarction (AMI) will increase to 23 million by 2030 (5). Unlike in Western countries, the epidemic profile of stroke in China surpasses that of IHD, with annual estimates of 11 million prevalent cases, 2.4 million new cases, and 1.1 million deaths (6). Adiposity is an imbalance between energy intake and metabolism expenditure resulting in abnormal fat accumulation. The prevalence of adiposity has reached nearly 33.3% worldwide, doubling since 1980, and is generally highest in developed countries and increasing in Asian countries (7). Two types of obesity, central (visceral) and general (peripheral) obesity, are often assessed by waist circumference (WC) and body mass index (BMI), respectively. Based on BMI criteria, the prevalence was 34.3% for overweight and 16.4% for obesity in Chinese adults (≥18 years) (8).
In fact, the distribution rather than the mount of adipose tissue may have a more critical effect on the development of CVD. Imaging-based assessments of subcutaneous adiposity tissue (SAT) and visceral adiposity tissue (VAT) by routine clinical practices, including computed tomography (CT), magnetic resonance imaging (MRI), dual-energy x-ray absorptiometry (DEXA), and dual bioelectrical impedance analysis (BIA), were largely limited due to their higher costs, related technical challenges, and potential radiation exposure risk. Previous research debated the prediction values of several common anthropometric indicators of adiposity for CVD (9–11); some suggested that waist-to-height ratio (WHtR) was superior to WC and BMI (12, 13). These results had significant heterogeneities as they covered different ethnic populations (14). Recently, visceral adiposity index (VAI), lipid accumulation product (LAP), and body shape index (ABSI), which are the products of WC, BMI, and blood lipids, have been proposed as reliable indexes of body fat accumulation, and they have been applied to the prediction of diabetes (15–17). With reference to VAI and considering the characteristic of body fat in the Asian population, the Chinese visceral adiposity index (CVAI) has been designed for the Chinese population; this surrogate indicator may be more sensitive than VAI, WC, and BMI to discriminate diabetes (18). However, studies investigating the associations between these novel indicators and CVD are limited.
Growing researches suggested that adiposity was significantly associated with CVD and CVD-related risk factors in East China (19–21). The disease burden and risk profiles for CVD vary geographically in China, with higher incidences but less healthcare services in southwestern provinces compared with eastern regions (22–24). However, limited knowledge is available on the effects of adiposity on CVD risk in Southwest China. Guizhou Province lies to the east of the Yunnan-Guizhou Plateau in Southwest China, with complex topography, poor transportation system, and undeveloped economic and educational level, leading to deficiency in medical resources. There are 56 ethnic groups in Guizhou Province, the majority of which are Han. The diet and living habits of different ethnic groups are different, and some prefer pickled food, which increases the risk of hypertension and stroke (25). In this study, we aimed to provide an insight to explore the associations of several anthropometric indicators with cardiovascular onsets, by using data from a large cohort study in Guizhou Province, Southwest China.
Methods
Study population and data collection
The Guizhou Population Health Cohort Study (GPHCS) is a good representation of the geographic, socio-demographic, ethnic composition of the adult population in Guizhou Province in Southwest China, enrolling a total of 9,280 adults at baseline between November 2010 and December 2012, from 12 areas (5 urban districts and 7 rural counties) in Guizhou Province using the multistage proportional stratified cluster sampling method, considering population size, population stability, and local capacity. The inclusive criteria were as follows: (1) age of 18 years or above; (2) living locally for more than 6 months and having no plan to move out; (3) completing survey questionnaire, blood sampling, and physical examination; and (4) signing the written informed consent. All participants were followed up for major chronic diseases and vital status through a repeated investigation by trained investigators between 2016 and 2020, and record linkage to the Death Registration Information System and Basic Public Health Service System. Ethics approval was obtained from the ethics review board of Guizhou Province (No.S2017-02).
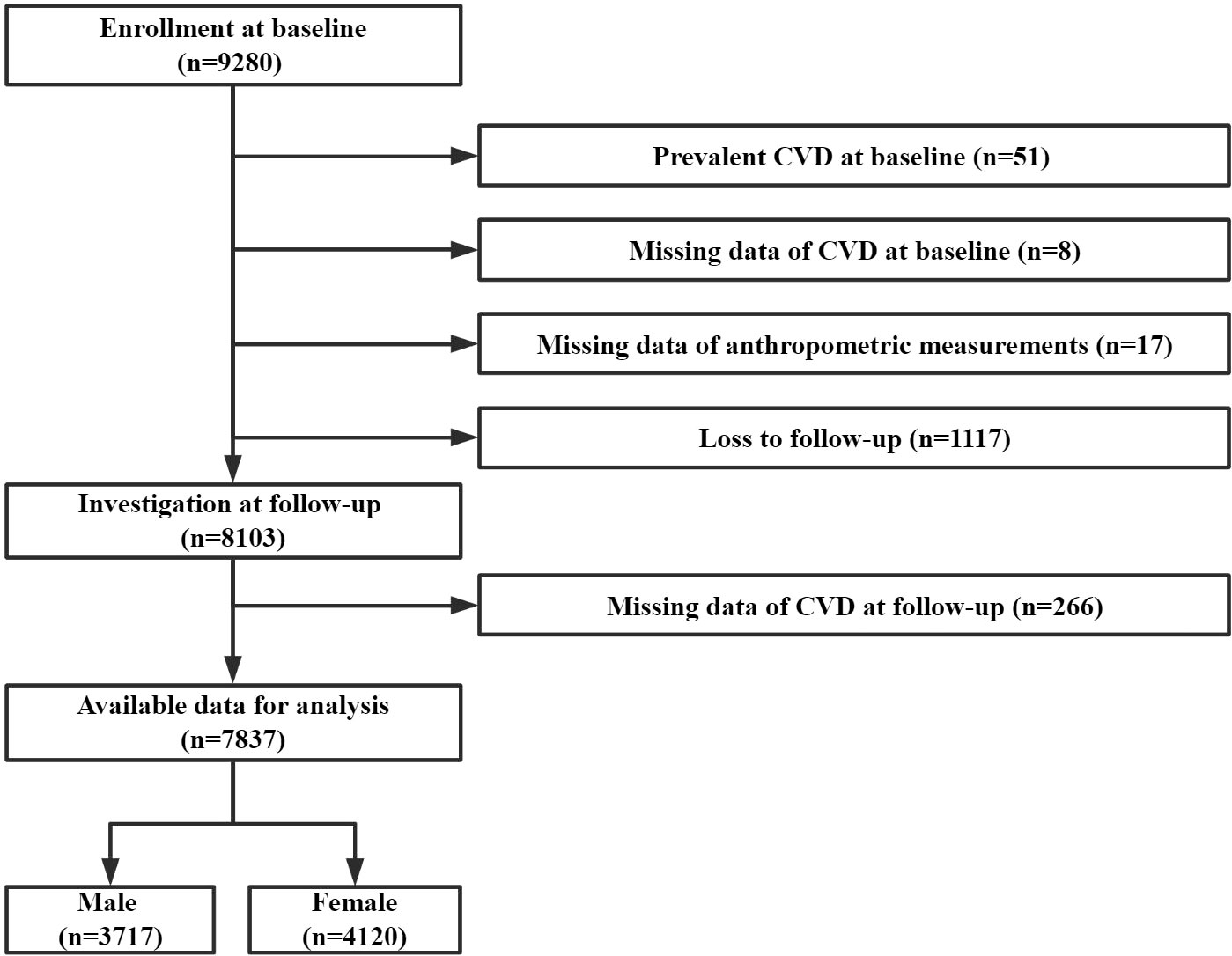
In this study, we excluded participants with a previous diagnosis of CVD, those with missing data of anthropometric measurements and CVD, or those lost to follow-up. Finally, 7,837 participants were included in the primary analyses (Figure 1).
Outcomes of interest
The primary outcomes were the first occurrence of cardiovascular events, including stroke and IHD. The main types were ischemic stroke (I63), hemorrhagic stroke (I60–61), and myocardial infarction (I21), coded by International Classification of Diseases 10th revision (ICD-10). All reported CVD events were identified using imagological diagnosis by trained clinical staff. The person-year (PY) of follow-up was calculated from the date of baseline investigation to the date of the occurrence of CVD, death, or follow-up, whichever came first. Incidence rate was calculated as the number of incident cases divided by follow-up PYs.
Anthropometric measurements and laboratory biochemical information
Anthropometric measurements, including standing height (cm), weight (kg), and WC (cm), were taken by trained health professionals according to standard protocols. Standing height and weight were measured with participants standing without shoes and in lightweight clothes. WC was measured on the midaxillary line between the lowest border of the rib cage and the top of the iliac crest. All parameters were recorded as the mean value of the twice measurements, and usually to the nearest 0.1 cm or 0.1 kg. Blood pressure was measured three times in a 3-min interval from the left arm after the participant rests in a seated position; the recorded values of systolic blood pressure (SBP) and diastolic blood pressure (DBP) were calculated as the mean of the last two of three consecutive measurements.
All participants provided a 10-ml blood sample after an overnight fast of at least 10 h, they also undergo an oral glucose tolerance test (OGTT), and the plasma was obtained at 2 h during the test. Concentrations of fasting plasma glucose (FPG), 2-h postload glucose (2h-PG), and Hemoglobin A1c (HbA1c) were analyzed locally within 2 h after the blood sample collected using the glucose oxidase methods (Roche Diagnostics, Mannheim, Germany). Serum triglycerides (TG), total cholesterol (CHOL), low-density lipoprotein cholesterol (LDL-C), and high-density lipoprotein cholesterol (HDL-C) were measured using enzymatic methods (Roche Diagnostics, Mannheim, Germany).
Traditional and non-traditional anthropometric indicators were calculated by the following formula:
Other data collections
Standardized in-person interviews using structured questionnaires were conducted for each participant to obtain the socio-demographic (age, gender, area, ethnic group, education level, marriage status, and occupation type), lifestyle (physical activity, tobacco smoking, and alcohol use), comorbidity status (diabetes, hypertension, and dyslipidemia), medication use, and nutraceutical consumption information.
Smoking was defined as smoking at least one cigarette a day for 12 months or more. Alcohol drinking was defined as drinking at least three times a week for 12 months or more. The physical activity level was calculated as the product of the duration and frequency of each activity, weighted by an estimate of the metabolic equivalent (MET) of that activity and summed for all activities performed, with the result expressed as the average MET hours per day. Diabetes was defined as those above the threshold of glycemia (FPG ≥ 6.1 mmol/L or 2h-PG ≥ 7.8 mmol/L), having a reported diabetes history, or experiencing anti-diabetes medications (26). Hypertension was defined as abnormal level of current blood pressure (SBP > 140 mmHg or DBP > 90 mmHg), having a reported hypertension history, or experiencing anti-hypertension medications (26). Dyslipidemia was defined as abnormal level of current blood lipids (TG ≥ 1.7 mmol/L, CHOL ≥ 5.2 mmol/L, LDL ≥ 3.4 mmol/L, HDL < 1.0 mmol/L), having a reported dyslipidemia history, or experiencing anti-dyslipidemia medications (26). Medication use was defined as regularly taking any medications for diabetes (including metformin, insulin, etc.), hypertension (including amlodipine, nifedipine, etc.), dyslipidemia (including atorvastatin, simvastatin, etc.), or obesity. Nutraceutical intake was defined as intaking common nutraceuticals (including vitamin, minerals, etc.) or foods with healthcare functions (including wine, tea, etc.) at least once a week for 12 months or more.
Statistical analyses
Baseline characteristics for participants were presented according to the presence of incident CVD and compared using Student’s t-test for continuous variables, or Chi-square test for categorical variables. Considering the body fat distribution and blood biochemical profiles are distinctly different in male and female participants, all analyses were conducted separately by sex.
The proportional hazard assumption was satisfied and then age-adjusted or multivariate-adjusted Cox proportional hazard models were used to assess the associations of incident CVD with adiposity categories and anthropometric indicators. The corresponding hazard ratios (HRs) and 95% confidence intervals (95% CIs) were calculated. Participants were categorized into different adiposity category groups according to gender-specific cutoffs for WC (normal weight, <85 cm for female participants and <90 cm for male participants; and central obesity, ≥85 cm for female participants and ≥90 cm for male participants) (27), WHtR (normal weight, <0.5; and central obesity, >0.5) (28), and BMI (lower weight, <18.5 kg/m2; normal weight, 18.5–23.9 kg/m2; overweight, 24.0–27.9 kg/m2; and obesity, ≥28.0 kg/m2) (27), based on Chinese guidelines. Participants were also categorized into four groups according to the quartiles of traditional (WC, WHtR, and BMI) and non-traditional (CVAI, LAP, and ABSI) anthropometric indicators, respectively. The restricted cubic splines (RCS) in Cox regression analyses were applied to evaluate the potential dose–response relationships of these six anthropometric indicators with CVD events. Receiver operator characteristic (ROC) curve analyses were generated for multivariate-adjusted Cox proportional hazard models, and the predictive powers of six indicators for CVD were compared according to the area under the ROC curve (AUC). Similar analyses were conducted in subgroups stratified by baseline demographic (age, area, and ethnic group).
All analyses and figures were performed by using R program (version 4.1.0, R Foundation for Statistical Computing, Vienna, Austria).
Results
Baseline characteristic descriptions
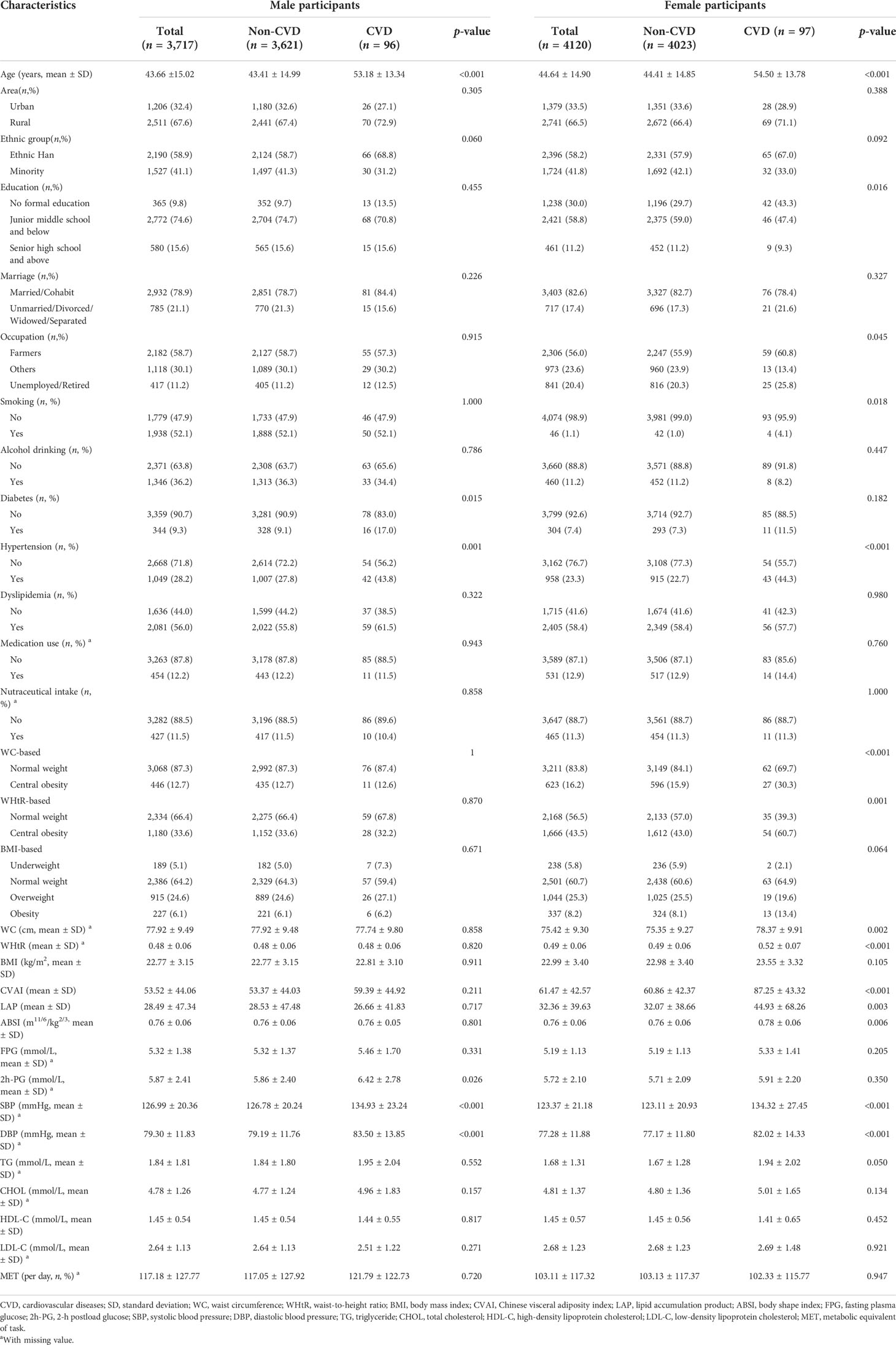
Of the 7,837 participants included, the mean (SD) age was 44.18 ± 14.97 years, and more than half were female (52.57%), ethnically Han (58.52%), and rural residents (67.02%). During the median 6.59 years of follow-up, 193 cases of first-onset CVD were identified (incident rate: 3.47 per 1,000 person-years), including 141 ischemic strokes (incident rate: 2.53 per 1,000 person-years), 46 hemorrhagic strokes (incident rate: 0.82 per 1,000 person-years), and 27 myocardial infarctions (incident rate: 0.48 per 1,000 person-years). Compared with female participants without CVD, those with CVD seemed to experience a higher level of WC, WHtR, CVAI, LAP, and ABSI at baseline (p < 0.05). However, there was no significant difference in these indicators between male participants with CVD and those without (Table 1).
Major analyses
Cox proportional hazard models indicated no association between any obesity type and incident CVD among male participants (Tables 2, 3). Female participants with either WC-based central obesity (HR:1.83, 95% CI: 1.12–2.98) or WHtR-based central obesity (HR:1.69, 95% CI: 1.07–2.65) had a higher risk of CVD after adjusting for age, area, ethnic group, smoking, alcohol drinking, MET, previous history of diabetes, hypertension, and dyslipidemia (Table 2, Model 2). The effect sizes of these positive associations were slightly decreased when further adjusted for medication use and nutraceutical intake (WC-based, HR: 1.82, 95% CI: 1.12–2.97; WHtR-based, HR:1.68, 95% CI: 1.07–2.64; Table 2, Model 3).
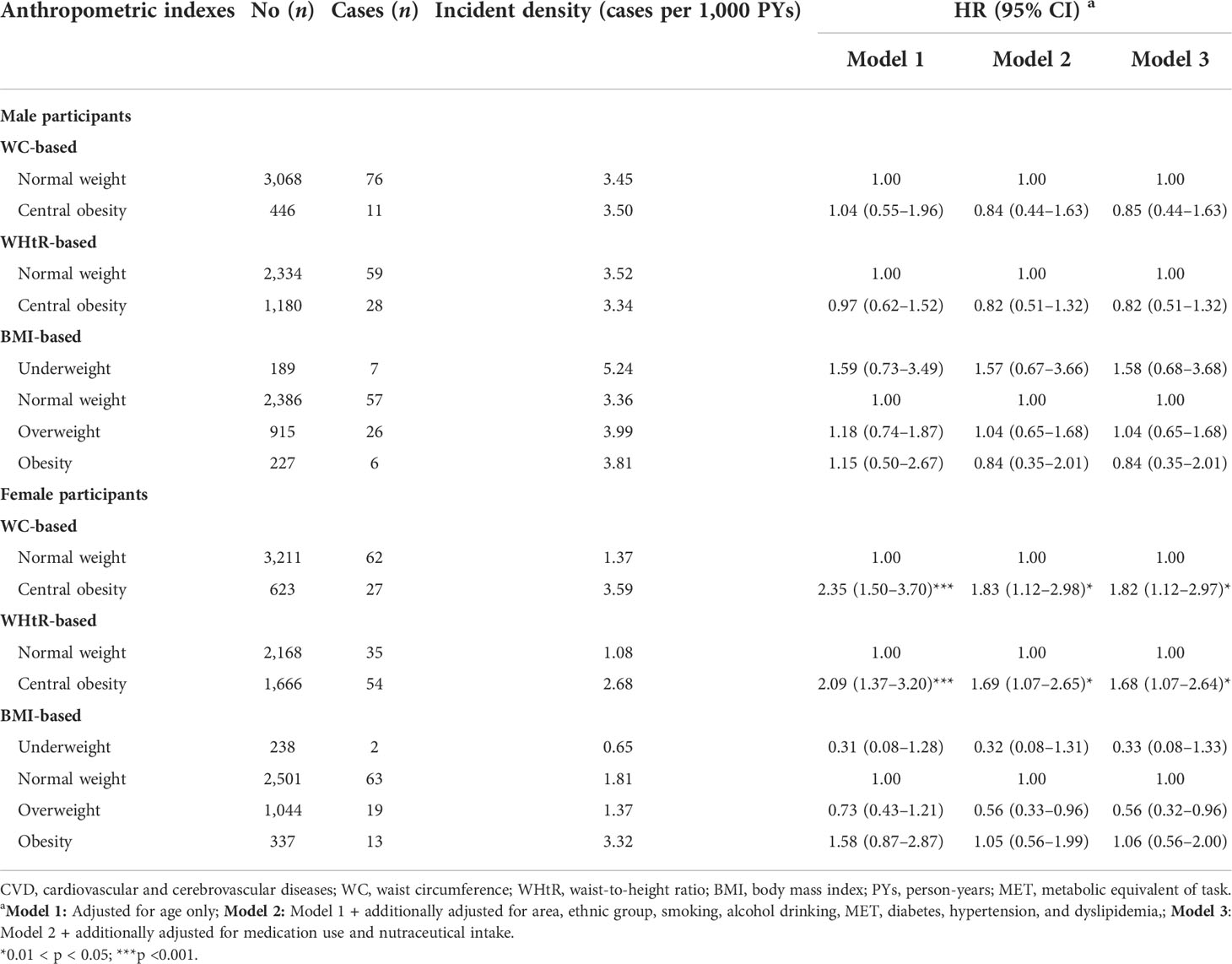
Table 2 Hazard ratios (HRs) and 95% confidence intervals (95% CIs) for overall CVD associated with adiposity category among male (n = 3,717) and female (n = 4,120) participants according to Cox regression models.
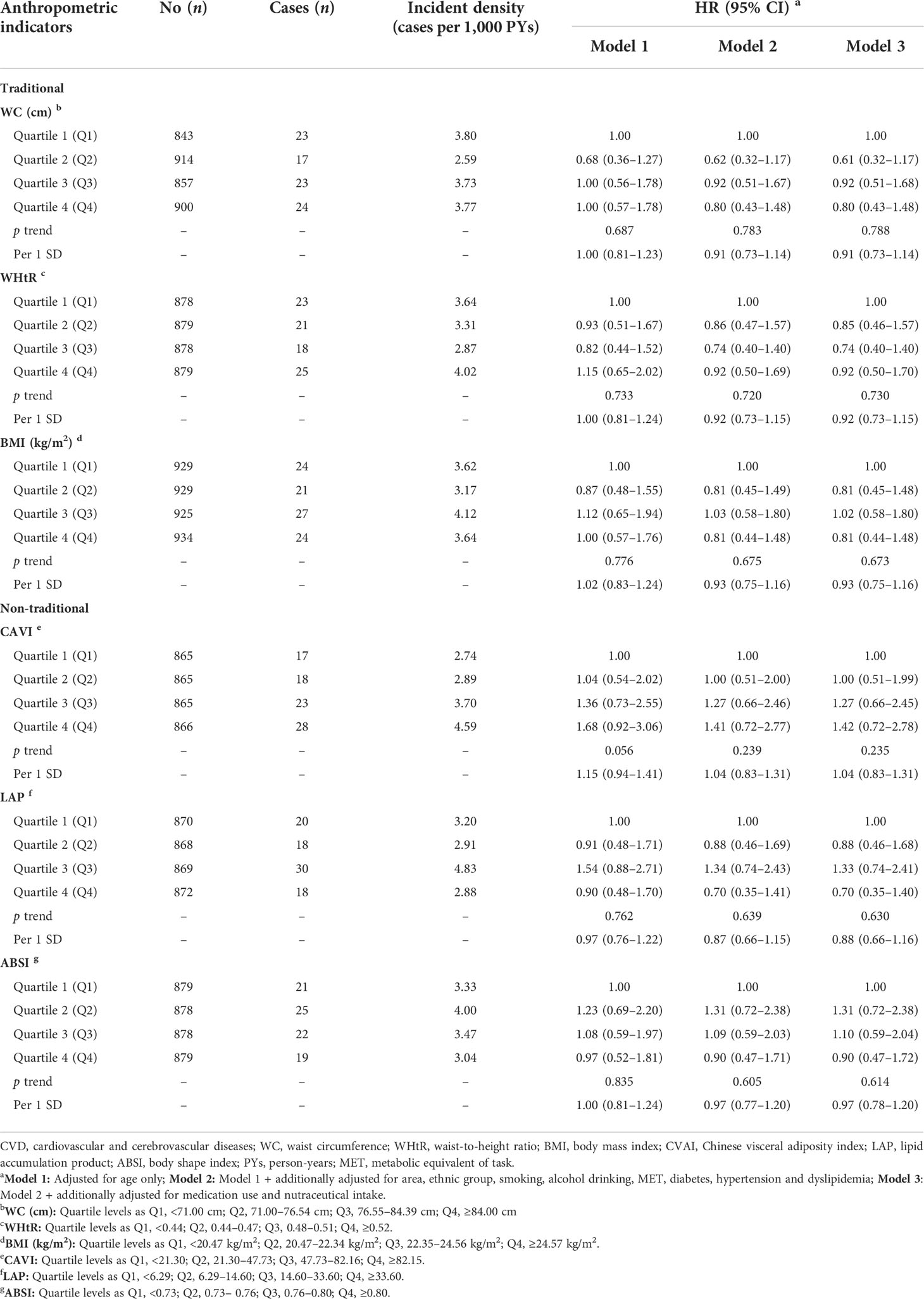
Table 3 Hazard ratios (HRs) and 95% confidence intervals (95% CIs) for overall CVDs associated with traditional and non-traditional anthropometric indicators among male participants (n = 3,717) according to Cox regression models.
The dose–response relationships of CVD with WC, WHtR, BMI, CVAI, LAP, and ABSI appeared to follow non-linear patterns among two gender groups (Figures S1, S2). Details regarding the associations of CVD risks and six anthropometric indicators are provided in Tables 3, 4. Similarly, these associations were seen only among female and not male participants. Compared with female participants in the lowest quartile (Q1), those in the highest quartile (Q4) of WHtR (HR: 2.24, 95% CI: 1.17–4.27), CVAI (HR: 3.98, 95% CI: 1.87–8.49), and ABSI (HR: 1.94, 95% CI: 1.06–3.52) had an increased risk of incident CVD (Table 4, Model 3). Additionally, per 1 SD increase in WHtR, CVAI, LAP, and ABSI increased 32%, 74%, 19%, and 26% risk of CVD, respectively (Table 4, Model 3). However, regardless of being evaluated in any form, BMI was unrelated to incident CVD.
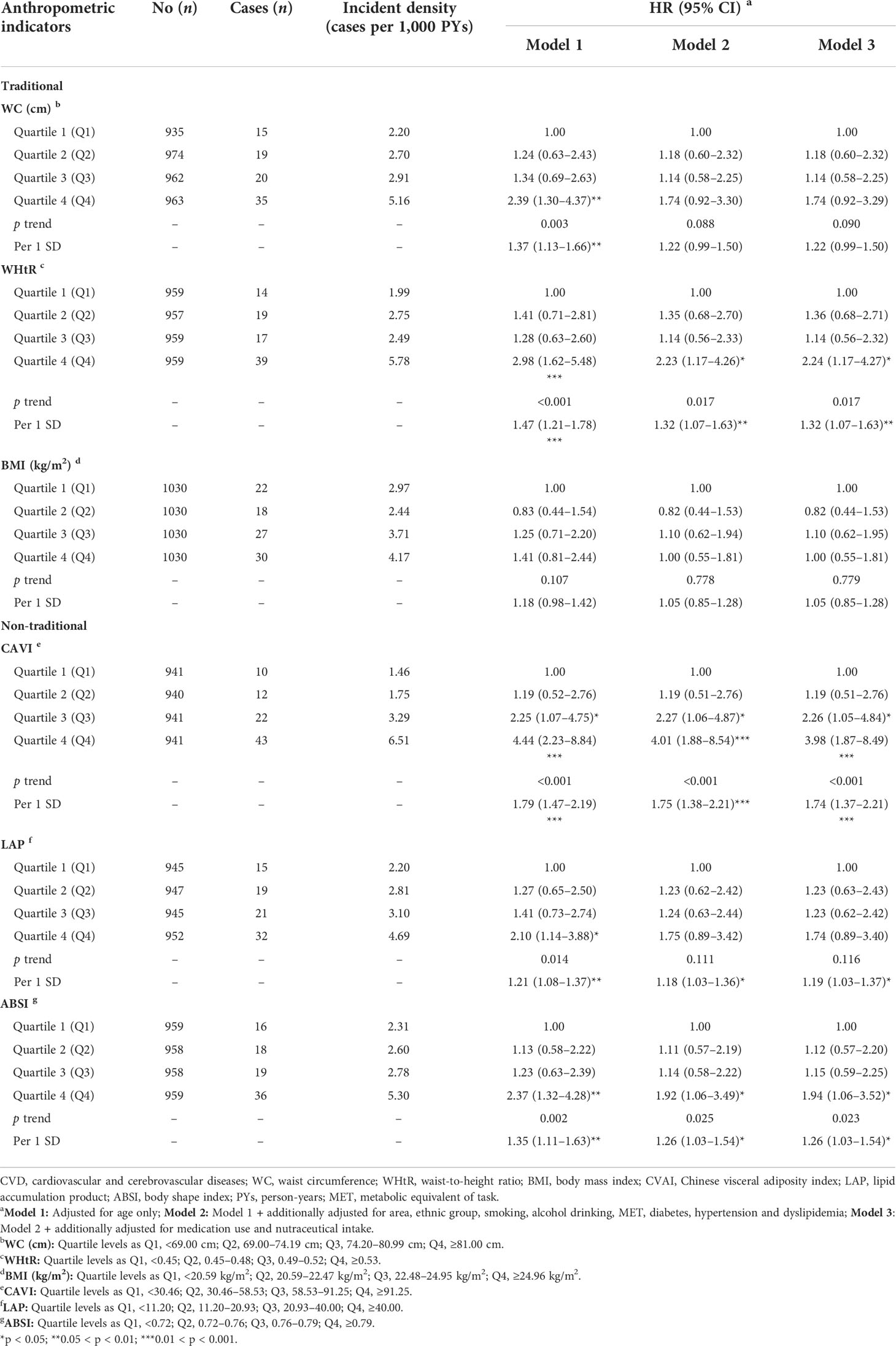
Table 4 Hazard ratios (HRs) and 95% confidence intervals (95% CIs) for overall CVDs associated with traditional and non-traditional anthropometric indicators among female participants (n = 4,120) according to Cox regression models.
Moreover, the HRs for ischemic stroke, hemorrhagic stroke, and myocardial infarction are presented in Tables S1–S6. Compared with female participants in the lowest quartile (Q1), those in the highest quartile (Q4) of CAVI (HR: 3.40, 95% CI: 1.56–7.44) had an elevated risk of ischemic stroke (Table S2, Model 3). In addition, CVAI and ABSI were positively associated with the risk of hemorrhagic stroke (Table S4, Model 3).
Figure 2 shows the ROC curves of six indicators in the prediction of CVD among male and female participants, respectively. Neither traditional nor non-traditional indicators predicted CVD in male participants (p > 0.05, Figures 2A, C). On the contrary, the area under the ROC curve (AUC) and 95% CI for each indicator were higher than 0.5 in female participants (p < 0.05, Figures 2B, D). CAVI showed the maximum predictive power of CVD with the biggest AUC of 0.687 (95% CI: 0.654–0.720) compared to other indicators in female participants.
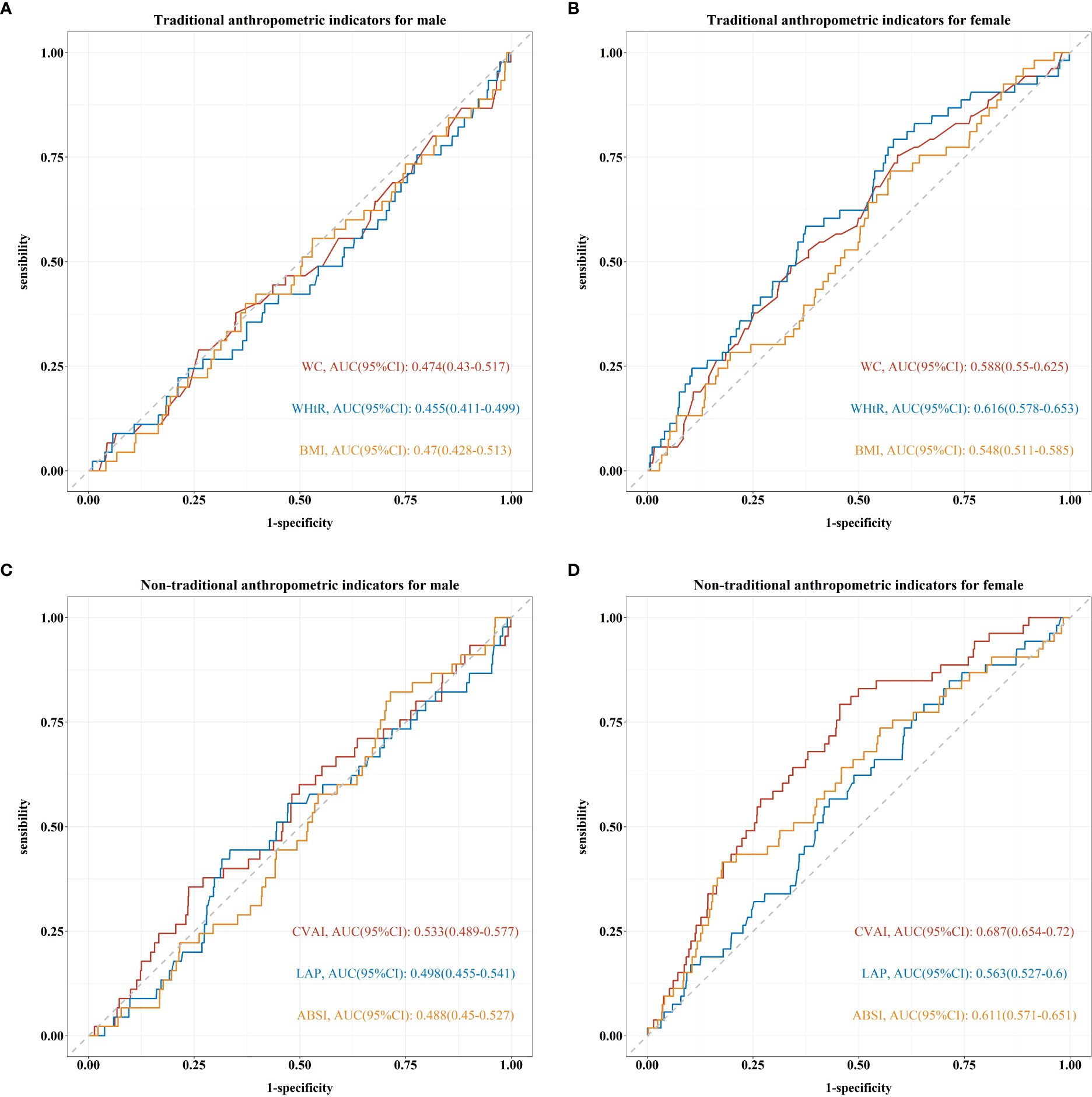
Figure 2 Receiver operating characteristic (ROC) curve and area under ROC curve (AUC) of traditional and non-traditional anthropometric indicators for predicting CVD among male and female participants based on the adjusted Cox regression model (Model 3). (A, B) For waist circumference (WC), waist-to-height ratio (WHtR), and body mass index (BMI), respectively. (C, D) For Chinese visceral adiposity index (CVAI), lipid accumulation product (LAP), and body shape index (ABSI).
Sensitive analyses and stratified analyses
Sensitive analyses were conducted after excluding female participants with less than 1 year of follow-up, and the results were similar to those in major analyses (Figure S3).
The multiple-adjusted HRs for incident CVD among female participants predicted by six anthropometric indicators varied according to age, area, and ethnic group (Figures 3A–F). The associations of WC and CVD were only observed in female participants aged more than 45 years (HR: 2.51, 95% CI: 1.06–5.98, Q4 vs. Q1) and living in rural region (HR: 3.02, 95% CI: 1.27–7.14, Q4 vs. Q1) (Figure 3A). Similar patterns were also seen for WHtR (Figure 3B) and ABSI (Figure 3E). The most frequent and strongest associations with CVD were found for CVAI, with the HR exceeding 6 (HR: 6.80, 95% CI: 2.67–17.30) in rural residents (Figure 3D).
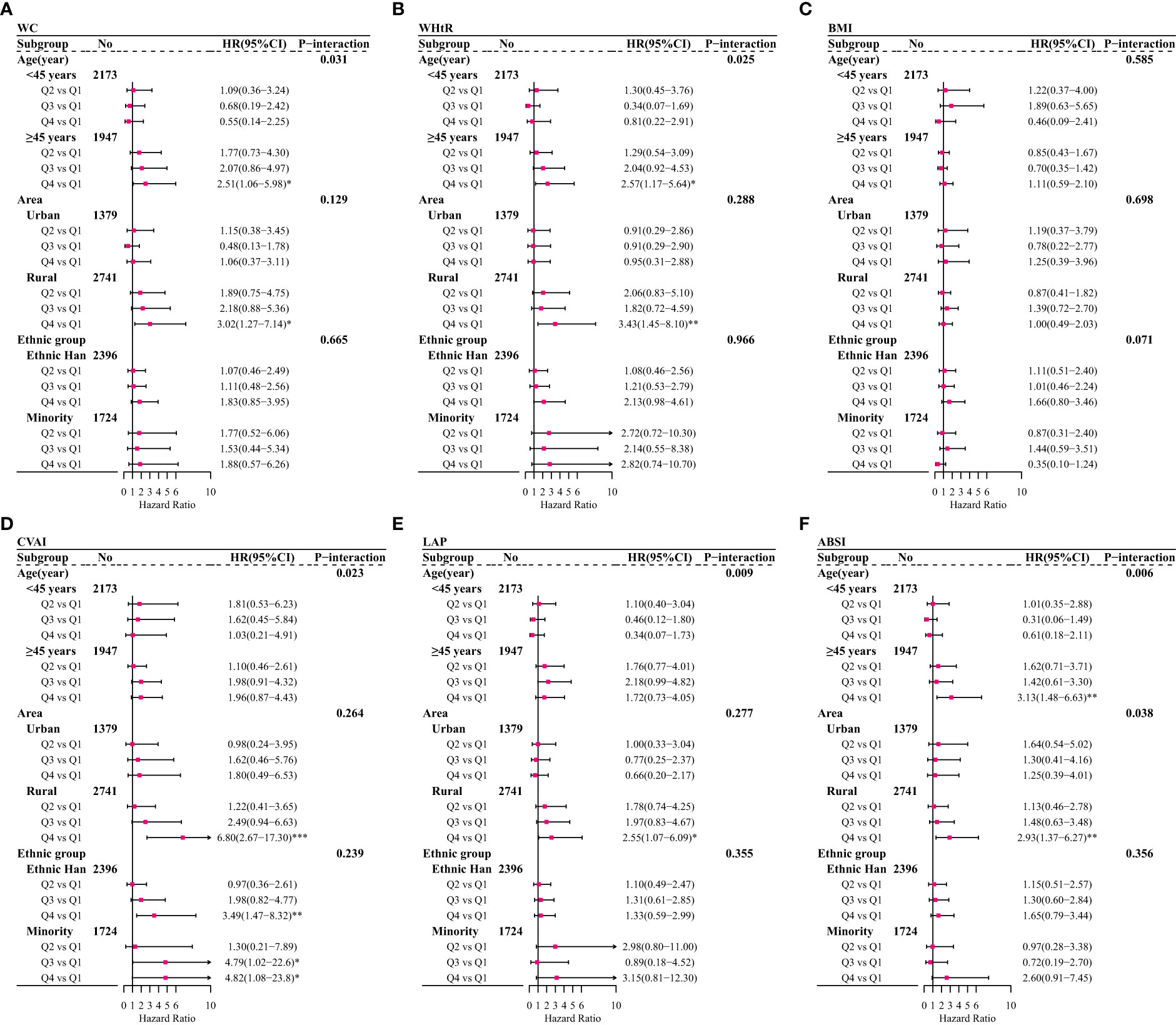
Figure 3 Adjusted hazard ratios (HRs) and 95% confidence intervals (95% CIs) for overall CVD or overall CVD associated with traditional and non-traditional anthropometric indicators among female participants after stratified by age, area, and ethnic group based on adjusted Cox regression model (Model 3). (A) For waist circumference (WC); (B) for waist-to-height ratio (WHtR); (C) for body mass index (BMI); (D) for Chinese visceral adiposity index (CVAI); (E) for lipid accumulation product (LAP); (F) for body shape index (ABSI); *p < 0.05; **0.05 < p <0.01;***0.01 < p < 0.001.
Discussion
In this large population-based cohort study of 7,837 people with a median of 6.59 years of follow-up in Southwest China, we observed that visceral adiposity measures, especially CVAI, were positively associated with overall CVD and ischemic stroke among female and not male participants. On the contrary, BMI, as a general obesity indicator, performed less predictive power for CVD.
The results of adiposity increasing the risks of CVD in this study are in accordance with those on previous studies (29–31). Adipose tissues release cytokines and chemokines into the vasculature, promoting systemic and vascular inflammation (32). Consistent with our results, obvious sex-related disparities in the associations of adiposity with CVD risk have also been proposed before (29), which may arise not only from differences in body fat distribution and metabolic profiles, but also from the differences in vascular anatomy and physiology, with female participants having smaller arterial diameter than male participants seen after normalizing for body size (33).
WC and WHtR are the most common indicators to measure visceral obesity. WHtR was designed to incorporate the effects of WC and height, namely, WC adjusted for height. There were more frequent associations of CVD with WHtR than WC in this study, suggesting that the distribution of body fat is important in discriminating CVD risk (34). We observed that BMI showed less prediction information for CVD as compared to WC or WHtR. The detrimental vascular effects of adiposity may be masked when using BMI as a measure of adiposity, which has been termed the “obesity paradox”, due to methodological deficiencies such as BMI failing to distinguish between fat tissue and skeletal muscle. In fact, an increase in total fat tissue percent or a decrease in skeletal muscle accelerates the occurrence of CVD (15, 35).
Moreover, the effects of visceral adipose tissue (VAT) on cardio-metabolic outcomes have been proved to be more deleterious than subcutaneous adipose tissue (SAT) (36). CVAI, which is estimated by synergistically integrating information of age, BMI, WC, and lipid profiles (HDL-C and TG), has outperformed traditional anthropometric measures as a useful surrogate for visceral adiposity in a Chinese population (18). As expected, CVAI showed the maximum predictive power of CVD, with a maximum HR of 3.98 (95% CI: 1.87–8.49) and the biggest AUC of 0.687 (95% CI: 0.654–0.720), compared to other indicators in female participants. Previous studies reported that CVAI was superior to BMI, WC, WHtR, LAP, or VAI for the diagnosis of diabetes and related complications (18, 20, 37). Additionally, after combining multiple measurements, ABSI (given the metrics of WC, height, and weight) and LAP (given the metrics of WC and TG) have also been considered as applicable indicators of some chronic diseases in adults (38, 39). In general, several measure indicators need to be combined to comprehensively assess health risks.
In the stratified analyses, the positive associations between visceral adiposity indicators of CVD were stronger in female participants aged more than 45 years or living in rural regions. The mechanism through which adiposity leads to cardiovascular risk is also discrepant in female participants between their pre-menopausal, pregnancy, and post-menopausal phases of life (40). Middle-aged female participants were more likely to accumulate fat due to declines in basal metabolic rate, and the estrogen deprivation secondary to menopause may lead to adverse cardiovascular consequences (41). Area and ethnic variations could be partly explained by regional environmental, socioeconomic characteristics, diet cultures, and local customs (22).
To our knowledge, this is one of few population-based cohort studies to assess CVD risk by a series of adiposity measure indicators. The strengths of our study include covering standardized methods for anthropometric measurements and local residents from various ethnic groups. There were several limitations to this study. First, assessments of some factors in this study, including physical activities, tobacco smoking, alcohol drinking, medications, and nutraceutical consumption, rely on self-reports from questionnaires, which might be influenced by recall bias. Second, we failed to collect any information of medication use for CVD, which have possible beneficial impact on CVD. Third, although the rate of loss to follow-up is above 10%, this rate is relatively low in all studies in Southwest China, given their poor traffic accessibility. Another thing to note is that our study population was from Southeast China, and CVAI was applicable to Chinese people; thus, the findings from this study should be generalized to other populations with caution.
In summary, our study contributes to a new knowledge about the associations of adiposity with incident CVD among Southwest Chinese across a variety of anthropometric indicators. Although visceral adiposity measure indicators are not diagnostic tools for cardiovascular events, the simplicity of anthropometric measurements (WC and BMI) and blood biochemical tests (TG and HDL) might therefore make them well applicable indicators for assessing CVD risk in clinical practice.
Conclusions
Visceral adiposity measures, especially CVAI, are stronger indicators of CVD among female not male participants in Southwest China. Different anthropometric indicators need to be combined to comprehensively assess health risks.
Data availability statement
The datasets for this manuscript will be made available upon request, further inquiries can be directed to the corresponding author TL,bGl1dGFvbWJzQDE2My5jb20=and NW,bmEud2FuZ0BmdWRhbi5lZHUuY24=.
Ethics statement
The studies involving human participants were reviewed and approved by the ethics review board of Guizhou Province (No. S2017-02). The patients/participants provided their written informed consent to participate in this study.
Author contributions
Conceptualization: NW, TL, and CF. Data curation: XZ and YC. Investigation: XZ, YY, and YZ. Methodology and formal analysis: YW and NW. Writing—original draft: YW and XZ. Writing—review and editing: NW, TL, and CF. All authors contributed to the preparation of the final document, read, and approved the final manuscript.
Funding
This work was supported by Guizhou Province Science and Technology Support Program (Qiankehe [2018]2819).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fendo.2022.969753/full#supplementary-material
Abbreviations
CVD, cardiovascular disease; SD, standard deviation; WC, waist circumference; WHtR, waist-to-height ratio; BMI, body mass index; CVAI, Chinese visceral adiposity index; LAP, lipid accumulation product; ABSI, body shape index; FPG, fasting plasma glucose; 2h-PG, 2-h postload glucose; TG, triglyceride; CHOL, total cholesterol; HDL-C, high-density lipoprotein cholesterol; LDL-C, low-density lipoprotein cholesterol; SBP, systolic blood pressure; DBP, diastolic blood pressure; MET, metabolic equivalent of task; ROC, receiver operator characteristic; AUC, area under the ROC curve.
References
1. Virani SS, Alonso A, Aparicio HJ, Benjamin EJ, Bittencourt MS, Callaway CW, et al. Heart disease and stroke statistics-2021 update: A report from the American heart association. Circulation (2021) 143(8):e254–743. doi: 10.1161/CIR.0000000000000950
2. James SLG, Abate D, Abate KH, Abay SM, Abbafati C, Abbasi N, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990-2017: a systematic analysis for the global burden of disease study 2017. Lancet (London England) (2018) 392(10159):1789–858. doi: 10.1016/S0140-6736(18)32279-7
3. Liu S, Li Y, Zeng X, Wang H, Yin P, Wang L, et al. Burden of cardiovascular diseases in China, 1990-2016: Findings from the 2016 global burden of disease study. JAMA Cardiol (2019) 4(4):342–52. doi: 10.1001/jamacardio.2019.0295
4. Zhao D, Liu J, Wang M, Zhang X, Zhou M. Epidemiology of cardiovascular disease in China: current features and implications. Nat Rev Cardiol (2019) 16(4):203–12. doi: 10.1038/s41569-018-0119-4
5. Li J, Li X, Wang Q, Hu S, Wang Y, Masoudi FA, et al. ST-segment elevation myocardial infarction in China from 2001 to 2011 (the China PEACE-retrospective acute myocardial infarction study): a retrospective analysis of hospital data. Lancet (London England) (2015) 385(9966):441–51. doi: 10.1016/S0140-6736(14)60921-1
6. Wu S, Wu B, Liu M, Chen Z, Wang W, Anderson CS, et al. Stroke in China: advances and challenges in epidemiology, prevention, and management. Lancet Neurol (2019) 18(4):394–405. doi: 10.1016/S1474-4422(18)30500-3
7. Chooi YC, Ding C, Magkos F. The epidemiology of obesity. Metab Clin Exp (2019) 92:6–10. doi: 10.1016/j.metabol.2018.09.005
8. Pan XF, Wang L, Pan A. Epidemiology and determinants of obesity in China. Lancet Diabetes Endocrinol (2021) 9(6):373–92. doi: 10.1016/S2213-8587(21)00045-0
9. Xia JY, Lloyd-Jones DM, Khan SS. Association of body mass index with mortality in cardiovascular disease: New insights into the obesity paradox from multiple perspectives. Trends Cardiovasc Med (2019) 29(4):220–5. doi: 10.1016/j.tcm.2018.08.006
10. Czernichow S, Kengne AP, Stamatakis E, Hamer M, Batty GD. Body mass index, waist circumference and waist-hip ratio: which is the better discriminator of cardiovascular disease mortality risk?: evidence from an individual-participant meta-analysis of 82 864 participants from nine cohort studies. Obes Rev (2011) 12(9):680–7. doi: 10.1111/j.1467-789X.2011.00879.x
11. Yin D, Yan Y, Xu N, Hui Y, Han G, Ma N, et al. Predictive values of obesity categories for cardiovascular disease risk factors in Chinese adult population. J Cell Biochem (2018) 120:7276–85. doi: 10.1002/jcb.28002
12. Ashwell M, Gunn P, Gibson S. Waist-to-height ratio is a better screening tool than waist circumference and BMI for adult cardiometabolic risk factors: systematic review and meta-analysis. Obes Rev (2012) 13(3):275–86. doi: 10.1111/j.1467-789X.2011.00952.x
13. Lo K, Wong M, Khalechelvam P, Tam W. Waist-to-height ratio, body mass index and waist circumference for screening paediatric cardio-metabolic risk factors: a meta-analysis. Obes Rev (2016) 17(12):1258–75. doi: 10.1111/obr.12456
14. Heymsfield SB, Peterson CM, Thomas DM, Heo M, Schuna JM Jr. Why are there race/ethnic differences in adult body mass index-adiposity relationships? a quantitative critical review. Obes Rev (2016) 17(3):262–75. doi: 10.1111/obr.12358
15. Ahn N, Baumeister SE, Amann U, Rathmann W, Peters A, Huth C, et al. Visceral adiposity index (VAI), lipid accumulation product (LAP), and product of triglycerides and glucose (TyG) to discriminate prediabetes and diabetes. Sci Rep (2019) 9(1):9693. doi: 10.1038/s41598-019-46187-8
16. Bawadi H, Abouwatfa M, Alsaeed S, Kerkadi A, Shi Z. Body shape index is a stronger predictor of diabetes. Nutrients (2019) 11(5):1018. doi: 10.3390/nu11051018
17. Tsou MT, Chang YC, Hsu CP, Kuo YC, Yun CH. Visceral adiposity index outperforms conventional anthropometric assessments as predictor of diabetes mellitus in elderly Chinese: a population-based study. Nutr Metab (2021) 18(1):87. doi: 10.1186/s12986-021-00608-6
18. Wu J, Gong L, Li Q, Hu J, Zhang S, Wang Y, et al. A novel visceral adiposity index for prediction of type 2 diabetes and pre-diabetes in Chinese adults: A 5-year prospective study. Sci Rep (2017) 7(1):13784. doi: 10.1038/s41598-017-14251-w
19. Wang Y, Jiang Y, Wang N, Zhu M, Liu X, Wang R, et al. Central but not general obesity is positively associated with the risk of hyperhomocysteinemia in middle-aged women. Nutrients (2019) 11(7):1614. doi: 10.3390/nu11071614
20. Wan H, Wang Y, Xiang Q, Fang S, Chen Y, Chen C, et al. Associations between abdominal obesity indices and diabetic complications: Chinese visceral adiposity index and neck circumference. Cardiovasc Diabetol (2020) 19(1):118. doi: 10.1186/s12933-020-01095-4
21. Gao M, Lv J, Yu C, Guo Y, Bian Z, Yang R, et al. Metabolically healthy obesity, transition to unhealthy metabolic status, and vascular disease in Chinese adults: A cohort study. PLoS Med (2020) 17(10):e1003351. doi: 10.1371/journal.pmed.1003351
22. Li X, Wu C, Lu J, Chen B, Li Y, Yang Y, et al. Cardiovascular risk factors in China: a nationwide population-based cohort study. Lancet Public Health (2020) 5(12):e672–81. doi: 10.1016/S2468-2667(20)30191-2
23. Ma RCW. Epidemiology of diabetes and diabetic complications in China. Diabetologia (2018) 61(6):1249–60. doi: 10.1007/s00125-018-4557-7
24. Li X, Krumholz HM, Yip W, Cheng KK, De Maeseneer J, Meng Q, et al. Quality of primary health care in China: challenges and recommendations. Lancet (London England) (2020) 395(10239):1802–12. doi: 10.1016/S0140-6736(20)30122-7
25. Wang Y, Su X, Chen Y, Wang Y, Zhou J, Liu T, et al. Unfavorable dietary quality contributes to elevated risk of ischemic stroke among residents in southwest China: Based on the Chinese diet balance index 2016 (DBI-16). Nutrients (2022) 14(3):694. doi: 10.3390/nu14030694
26. Writing group of Chinese guideline for cardiometabolic diseases prevention, editorial board of Chinese journal of cardiometabolic diseases. Chinese guideline for cardiometabolic diseases prevention. Chin J Cardiometabolic Dis2018 (2017) 46(1):10–25. doi: 10.3760/cma.j.issn.0253-3758.2018.01.004
27. National health and family planning commission of the people’s republic of china. health standard of the people’s republic of china. no. WS/T 428-2013: Criteria of weight for adults (2013). Available at: http://g.wanfangdata.com.cn/details/detail.do?_type=standards&id=WS/T428-2013 (Accessed 21 June 2021).
28. Browning LM, Hsieh SD, Ashwell M. A systematic review of waist-to-height ratio as a screening tool for the prediction of cardiovascular disease and diabetes: 0·5 could be a suitable global boundary value. Nutr Res Rev (2010) 23(2):247–69. doi: 10.1017/S0954422410000144
29. Mu L, Liu J, Zhou G, Wu C, Chen B, Lu Y, et al. Obesity prevalence and risks among Chinese adults: Findings from the China PEACE million persons project, 2014-2018. Circ Cardiovasc Qual Outcomes (2021) 14(6):e007292. doi: 10.1161/CIRCOUTCOMES.120.007292
30. Chen Z, Iona A, Parish S, Chen Y, Guo Y, Bragg F, et al. Adiposity and risk of ischaemic and haemorrhagic stroke in 0·5 million Chinese men and women: a prospective cohort study. Lancet Global Health (2018) 6(6):e630–40. doi: 10.1016/S2214-109X(18)30216-X
31. Wormser D, Kaptoge S, Di Angelantonio E, Wood AM, Pennells L, Thompson A, et al. Separate and combined associations of body-mass index and abdominal adiposity with cardiovascular disease: collaborative analysis of 58 prospective studies. Lancet (London England) (2011) 377(9771):1085–95. doi: 10.1016/S0140-6736(11)60105-0
32. Powell-Wiley TM, Poirier P, Burke LE, Després J P, Gordon-Larsen P, Lavie CJ, et al. Obesity and cardiovascular disease: A scientific statement from the American heart association. Circulation (2021) 143(21):e984–e1010. doi: 10.1161/CIR.0000000000000973
33. Ji H, Niiranen TJ, Rader F, Henglin M, Kim A, Ebinger JE, et al. Sex differences in blood pressure associations with cardiovascular outcomes. Circulation (2021) 143(7):761–3. doi: 10.1161/CIRCULATIONAHA.120.049360
34. Min YI, Gao Y, Anugu P, Anugu A, Correa A. Obesity and overall mortality: findings from the Jackson heart study. BMC Public Health (2021) 21(1):50. doi: 10.1186/s12889-020-10040-9
35. Antonopoulos AS, Oikonomou EK, Antoniades C, Tousoulis D. From the BMI paradox to the obesity paradox: the obesity-mortality association in coronary heart disease. Obes Rev (2016) 17(10):989–1000. doi: 10.1111/obr.12440
36. Hocking S, Samocha-Bonet D, Milner KL, Greenfield JR, Chisholm DJ. Adiposity and insulin resistance in humans: the role of the different tissue and cellular lipid depots. Endocr Rev (2013) 34(4):463–500. doi: 10.1210/er.2012-1041
37. Wu Z, Yu S, Kang X, Liu Y, Xu Z, Li Z, et al. Association of visceral adiposity index with incident nephropathy and retinopathy: a cohort study in the diabetic population. Cardiovasc Diabetol (2022) 21(1):32. doi: 10.1186/s12933-022-01464-1
38. Ji M, Zhang S, An R. Effectiveness of a body shape index (ABSI) in predicting chronic diseases and mortality: a systematic review and meta-analysis. Obes Rev (2018) 19(5):737–59. doi: 10.1111/obr.12666
39. Zhang B, Wang X, Zhong L, Wang YS. Lipid accumulation product as useful predictors of stroke: A correlation analysis between lipid accumulation index/cerebral vascular hemodynamics indexes and risk factors of stroke in 3264 people undergoing physical examination in xinjiang. Med (Baltimore) (2022) 101(2):e28444. doi: 10.1097/MD.0000000000028444
40. Faulkner JL. Obesity-associated cardiovascular risk in women: hypertension and heart failure. Clin Sci (London Engl 1979) (2021) 135(12):1523–44. doi: 10.1042/CS20210384
Keywords: visceral adiposity, anthropometric, cardiovascular disease, southwest China, cohort study
Citation: Wang Y, Zhao X, Chen Y, Yao Y, Zhang Y, Wang N, Liu T and Fu C (2022) Visceral adiposity measures are strongly associated with cardiovascular disease among female participants in Southwest China: A population-based prospective study. Front. Endocrinol. 13:969753. doi: 10.3389/fendo.2022.969753
Received: 15 June 2022; Accepted: 11 August 2022;
Published: 08 September 2022.
Edited by:
Yun Kyung Cho, Asan Medical Center, South KoreaReviewed by:
Yoshihiro Miyamoto, National Cerebral and Cardiovascular Center, JapanRuiping Wang, Shanghai Dermatology Hospital, China
Copyright © 2022 Wang, Zhao, Chen, Yao, Zhang, Wang, Liu and Fu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Na Wang, bmEud2FuZ0BmdWRhbi5lZHUuY24=; Tao Liu, bGl1dGFvbWJzQDE2My5jb20=
†These authors have contributed equally to this work
 Yingying Wang
Yingying Wang Xiaodeng Zhao
Xiaodeng Zhao Yun Chen
Yun Chen Yuntong Yao2
Yuntong Yao2 Na Wang
Na Wang Tao Liu
Tao Liu Chaowei Fu
Chaowei Fu