
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Endocrinol. , 22 August 2022
Sec. Thyroid Endocrinology
Volume 13 - 2022 | https://doi.org/10.3389/fendo.2022.967044
This article is part of the Research Topic Ambulatory and Outpatient Thyroid Surgery View all 6 articles
 Wanqing Tang1
Wanqing Tang1 Xiuyun Tang2†
Xiuyun Tang2† Danni Jiang1
Danni Jiang1 Xiaojuan Zhang1
Xiaojuan Zhang1 Rongling Wang1
Rongling Wang1 Xiaoyan Niu1
Xiaoyan Niu1 Yichen Zang1
Yichen Zang1 Mingzhu Zhang1
Mingzhu Zhang1 Xinya Wang1
Xinya Wang1 Cheng Zhao1*
Cheng Zhao1*Background: To evaluate the safety and efficacy of radiofrequency ablation (RFA), microwave ablation (MWA), and laser ablation (LA) for the treatment of cervical metastatic lymph nodes (CMLNs) of papillary thyroid carcinoma (PTC).
Methods: The Pubmed, EMBASE, Web of Science, and Cochrane Library databases were searched for studies on the safety and efficacy of thermal ablations (RFA, MWA, and LA) for the treatment of CMLNs of PTC until March 30, 2022. A review of 334 potential papers identified 17 eligible papers including 312 patients. Fixed-effects model or random-effects model was used to evaluate the pooled proportions of volume reduction rate (VRR), complete disappearance, and recurrence, and pooled estimates of changes in the largest diameter, volume, and serum Tg after ablation. The pooled proportions of overall and major complications were calculated. Subgroup analysis based on treatment modalities. The heterogeneity among studies was analyzed by using Q statistics and inconsistency index I2. MINORS scale was used to evaluate the quality of the studies.
Results: 17 eligible studies were finally identified, including 312 patients and 559 CMLNs. The pooled proportions of VRR, complete disappearance and recurrence of CMLNs were 91.28% [95% confidence interval (CI): 86.60-95.97%], 67.9% [95% CI: 53.1-81.1%] and 7.8% [95%CI: 3.0-14.1%], respectively. The pooled estimates of changes in the largest diameter, volume and serum Tg were 8.12 mm [95%CI: 6.78-9.46 mm], 338.75 mm3 [95%CI: 206.85 -470.65 mm3] and 5.96 ng/ml [95%CI: 3.68-8.24 ng/ml], respectively. The pooled proportions of overall and major complications were 2.9% [95%CI: 0.3-7.1%] and 0.3% [95%CI: 0-1.9%], respectively. Significant between-study heterogeneity was observed for complete disappearance (P<0.01, I2 =88.6%), VRR (P<0.001, I2 =99.9%), recurrence (P=0.02, I2 =47.76%), overall complications (P<0.02, I2 =44.8%), and changes in the largest diameter (P < 0.001, I2 =82.6%), volume (P<0.001, I2 =97.0%), and serum Tg (P < 0.001, I2 =93.7%). Subgroup analysis showed heterogeneity of the VRR among the treatment modality (I2 range: 84.4-100%). The VRR of MWA was the highest (97.97%), followed by RFA (95.57%) and LA (84.46%) (P < 0.001).
Conclusion: All thermal ablations were safe and effective for the treatment of CMLNs of PTC. However, each treatment had significant heterogeneity in VRR. Compared with RFA and MWA, LA was less effective in reducing the volume of CMLNs of PTC.
Papillary thyroid carcinoma (PTC) is the most common pathological type of thyroid carcinoma, accounting for about 80-90% of thyroid malignant tumors (1). Thyroidectomy and radioactive iodine therapy are the main methods for the treatment of PTC, but 20-30% of patients have recurrence and lymph node metastasis after operation (2). Although reoperation is still the main treatment for cervical metastatic lymph nodes (CMLNs) of PTC (3, 4), the difficulty of reoperation and the risk of postoperative complications are increased due to the neck distortion, scar formation, and fibrous tissue adhesion (5, 6). Reoperation is not suitable for patients with high surgical risk or patients who refuse surgery. The guidelines of the American Thyroid Association recommend active surveillance for small CMLNs (7). However, some patients will have a sudden increase in the volume or number of CMLNs during the follow-up, and some patients will seek intervention due to psychological pressure.
In recent years, thermal ablation has developed rapidly and has been widely used for the treatment of benign (8–10) and malignant (11–13) thyroid nodules. Its application in CMLNs of PTC is also increasing and the therapeutic effect is remarkable (14). More and more evidence indicates that thermal ablations, including radiofrequency ablation (RFA), microwave ablation (MWA), and laser ablation (LA), are safe and effective for the treatment of CMLNs. However, most of the studies are retrospective, the sample size is small, and there is a lack of comparative study of various thermal ablation methods. Therefore, it is still necessary to comprehensively evaluate the efficacy and safety of thermal ablations for CMLNs of PTC. Therefore, this study aims to evaluate the safety and efficacy of thermal ablation for the treatment of CMLNs of PTC.
This meta-analysis was performed according to the Preferred Reporting Items for a Systematic Review and Meta-analysis (PRISMA) guidelines (15). The Pubmed, EMBASE, Web of Science, and Cochrane Library databases were searched to identify publications on thermal ablation in treating CMLNs of PTC. The beginning date of literature was not limited, and the search was finalized on March 30, 2022. The search terms used were as follows: [(thyroid) AND (carcinoma OR cancer) AND (radiofrequency ablation OR RFA OR laser ablation OR LA OR microwave ablation OR MWA OR thermal ablation) AND (lymph node OR metastasis OR metastatic lymph node)]. References for selected articles were also further reviewed to find relevant articles. Two reviewers independently conducted the literature search, and any disagreement in the inclusion of articles was resolved by discussion until consensus was reached. We were not blinded to authors, institutions, journals, or interventions while selecting studies or extracting data.
Studies investigating thermal ablations (i.e., RFA, LA, and MWA) for the treatment of CMLNs of PTC were eligible for inclusion. The included studies met the following criteria: 1) Population and intervention: patients were diagnosed with CMLNs of PTC; the main treatment was either RFA, LA, or MWA; and sample size ≥ 5 patients; 2) Study design: both retrospective and prospective studies were included; 3) Outcomes: the therapeutic effect (i.e., volume reduction, complete disappearance, recurrence, and complications) was reported in detail.
The exclusion criteria included the following: 1) case reports or series with< 5 patients; 2) abstracts, reviews, comments, and editorials; 3) articles not written in English. Two reviewers independently reviewed the literature in consensus.
We extracted the following data from the included studies into standardized formats: (a) study characteristics: first author, year of publication, affiliation, duration of study, study design, and sample size; (b) patients’ demographic and clinical characteristics: age, sex, ablation techniques (RFA, LA or MWA), nodule characteristics (largest diameter and volume), and follow-up time; (c) outcomes: changes in the largest diameter (mm), serum Tg (ng/ml), and volume (mm3); volume reduction rate(VRR) (%) calculated as [(initial volume - final volume)/initial volume x 100%], complete disappearance rate [determined by ultrasound at final follow-up], and recurrence; (d) safety: frequency of overall and major complications. One reviewer extracted the data, and the other confirmed the validity of the data.
The quality of the included studies was independently assessed then in consensus by two reviewers using the structured criteria of MINORS scale.
The Society of Interventional Radiology defined the complications caused by thermal ablation, including major and minor complications (16, 17). A major complication was defined as one that might be life-threatening, lead to substantial morbidity or disability, or prolong hospitalization time if left untreated. In this study, major complications included hypothyroidism, transient (lasting> 1 month) or permanent hoarseness. Minor complications included hoarseness (lasting < 1 month), hematoma, and pain requiring medication. Side effects were symptoms that did not require treatment or medication, including mild, transient postoperative pain, heat sensation, fever, local infection, and neck discomfort.
The primary outcomes of this meta-analysis were the pooled proportions of VRR, complete disappearance, recurrence, overall complications, and major complications, and pooled estimates of changes in the largest diameter, volume, and serum Tg. In the meta-analysis, the weighted mean difference (WMD) and 95% confidence interval (CI) of continuous variables were evaluated, and the pooled proportions and 95%CI of categorical variables were evaluated. We used the inconsistency index I2 with the Q statistic and P-value to evaluate the heterogeneity (18, 19). When I2>50% or P<0.05, we chose the random-effects model; in contrast, we used the fixed-effects model when I2<50% or P>0.05 (19, 20). At the same time, subgroup meta-analysis was performed by treatment modality (RFA, LA, and MWA). Funnel plots and Egger’s test were used to evaluate publication bias, P<0.05 indicated significant publication bias (21). Sensitivity analysis was performed to identify the influence of an individual study on pooled estimates by removing one study at a time (18). All data were analyzed using STATA software version 15.0 (StataCorp, College Station, TX).
The study selection procedure was displayed in Figure 1. The initial literature search identified 334 articles. After removal of duplicates, 243 were screened for eligibility. Among them, 226 were excluded after reviewing the abstracts (3 review articles, 8 case reports, 7 letters/editorial/abstract, 194 articles of irrelevant contents, 1 article with other ablation methods, 2 registration tests, and 11 non-English articles). Then the full texts of the remaining 17 articles were thoroughly reviewed. Finally, 17 articles with a total of 312 patients with 559 CMLNs of PTC were included (22–38). After searching the bibliography of these articles, no additional eligible study was identified.
The detailed characteristics of the 17 eligible studies are shown in Table 1. Among the 17 studies included, there were 13 retrospective studies (22–24, 26–32, 34, 36, 37) and 4 prospective studies (25, 33, 35, 38). All included studies were conducted in single centers. The cohort sizes varied from 5 to 45 patients with numbers of CMLNs ranging from 8 to 98. The mean ages of included study’s patients ranged from 15.6 to 62.3 years. The mean follow-up period ranged from 6.0 to 52.0 months, with 13 studies reporting an average of more than one year (23–25, 27, 29–36, 38). The types of thermal ablation techniques included 5 MWA (11, 23–26), 6 RFA (27–32), and 6 LA (33–38). The institutions of 10 studies were in China (11, 23–26, 28, 30, 32, 36, 38), two studies were in South Korea (27, 31), and five studies were in Italy (29, 33–35, 37). The quality assessment by MINORS showed moderate overall quality of the included studies (Table S1). All studies clearly described the thermal ablation techniques and equipment (Table 2).
The overall pooled estimates for the WMD in largest diameter from baseline to the last follow-up after ablation are summarized in Figure 2 with corresponding forest plots. The heterogeneity among studies was significant (I2 = 82.6%, P < 0.001), so the random-effects model was used for the analysis. The pooled WMD was 8.12mm (95%CI: 6.77-9.46mm). RFA, LA, and MWA all induced a statistically significant reduction in largest diameter after ablation (all P<0.001). In addition, MWA achieved a higher pooled WMD (8.69mm, 95%CI: 5.99-11.38mm) than RFA (7.82mm, 95%CI: 5.17-10.48mm) and LA (7.55mm, 95%CI: 6.61-8.48mm). The differences in the pooled WMD among the three therapies in the largest diameter were statistically significant (P <0.001). No publication bias was found in funnel plot and Egger’s test (P=0.132).
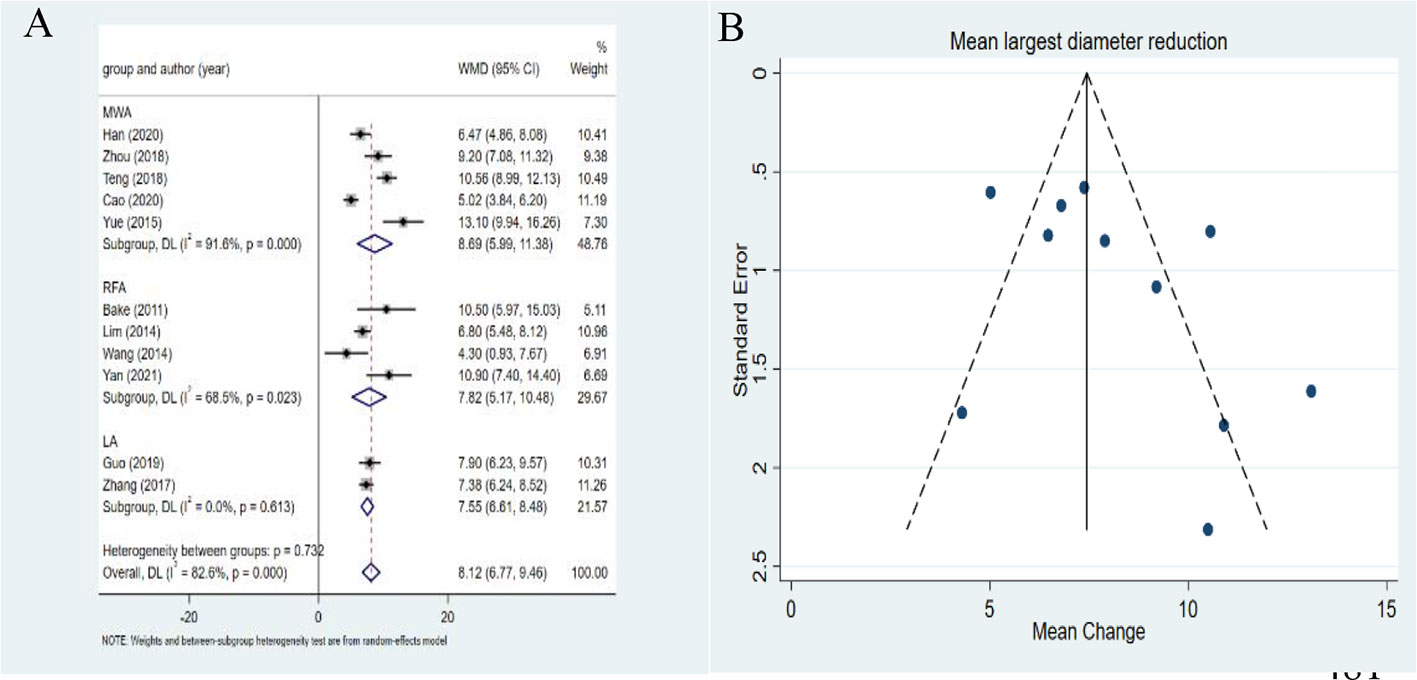
Figure 2 Forest plots (A) and funnel plots (B) of reduction of largest diameter of metastatic lymph nodes.
The overall pooled estimates for the WMD in tumor volume from baseline to the last follow-up after ablation are summarized in Figure 3 with corresponding forest plots. The pooled WMD was 338.75mm3 (95%CI: 206.85-470.65mm3). A significant heterogeneity was observed (I2 =97.0%, P<0.001). RFA, LA, and MWA all induced a statistically significant reduction in tumor volume after ablation (P=0.001, P=0.002, P=0.028 in the RFA, LA and MWA groups, respectively). In addition, MWA achieved a higher pooled WMD (527.78mm3,95%CI: 57.64-997.93mm3) than RFA (237.25mm3,95%CI: 96.20-378.30mm3) and LA (228.50mm3,95%CI: 81.29-375.72mm3). The differences in the pooled WMD among the three therapies were statistically significant (P<0.001). The funnel plot and Egger’s test showed a significant publication bias (P=0.025). After the trim-and-fill method adjusting publication bias, the adjusted pooled estimates for mean volume reduction were still 338.75mm3 (95%CI: 206.85-470.65mm3).
The pooled estimate of VRR was 91.28% (95%CI: 86.60-95.97%) (Figure 4A). There was significant heterogeneity for VRR (I2 =99.9%, P<0.001). MWA achieved a higher pooled proportion (97.97%, 95%CI: 95.24-100.70%) than RFA (95.57%,95%CI: 93.33-97.80%) and LA (84.46%, 95%CI: 75.62-93.31%). The differences in the pooled proportion among the three modalities were statistically significant (P<0.001). No publication bias was found in funnel plot and Egger’s test (P=0.364) (Figure 4B).
The pooled WMD was 5.96ng/ml (95%CI: 3.68-8.24ng/ml) (Figure 5A). A significant heterogeneity was noted in the serum Tg (I2 =93.7%, P<0.001). RFA, LA, and MWA all induced a statistically significant reduction in serum Tg after ablation (P= 0.013, P=0.027, and P<0.001 in the RFA, LA, and MWA groups, respectively). In addition, RFA yielded higher pooled WMD (6.47 ng/ml, 95%CI: 1.34-11.60 ng/ml) than LA (5.45 ng/ml, 95%CI: 0.62-10.28 ng/ml) and MWA (5.83 ng/ml, 95%CI: 2.65-9.00 ng/ml). The differences in the pooled WMD among the three therapies in serum Tg were statistically significant (P<0.001). The funnel plot and Egger’s test showed a significant publication bias (P=0.011) (Figure 5B). After the trim-and-fill method adjusting publication bias, the adjusted pooled estimates for serum Tg were 5.436 ng/ml (95%CI: 3.264-7.609 ng/ml).
The complete disappearance demonstrated a pooled proportion of 63.3% (95%CI: 46.7-78.5%), 74.6% (95%CI: 37.7-98.8%) and 67.8% (95%CI: 29.7-96.1%) after RFA, LA and MWA treatment, respectively (Figure 6A). The heterogeneity among studies was significant (I2 =88.56%, P<0.01). These results showed that the proportion of complete disappearance after LA was higher than the other two therapies. The differences in the pooled proportion among the three therapies in complete disappearance were statically significant (P<0.001). No publication bias was found in funnel plot and Egger’s test (P=0.523) (Figure 6B).
The recurrence demonstrated a pooled proportion of 9.8% (95%CI: 2.0-21.0%), 9.8% (95%CI: 0-28.0%), and 5.0% (95%CI: 0.8-11.3%) after RFA, LA and MWA treatment, respectively (Figure 7A). The results showed that the proportion of recurrence after MWA was lower than the other two therapies. The differences in the pooled proportion among the three therapies in recurrence were statically significant (P<0.01). No publication bias was found in funnel plot and Egger’s test (P=0.533) (Figure 7B).
16 complications among 559 CMLNs in 312 patients were reported. The pooled proportion of major complications was 0.3% (95% CI: 0-1.9%). The major complications demonstrated pooled proportions of 0.7% (95%CI: 0-4.7%), 0.5% (95%CI: 0-4.8%), and 0% (95%CI: 0-3.3%) in MWA, RFA and LA, respectively (Figure 8A). However, no statistical significance was observed among the three therapies (P=0.332). No publication bias was seen for major complications (P=0.622) (Figure 8B). The pooled proportion of overall complications was 2.9% (95%CI: 0.3-7.1%). The pooled proportions of overall complications were 3.2% (95%CI: 0.1 -8.8%), 0.5% (95%CI: 0- 4.8%), and 8.8% (95%CI: 0 -26.0%) in MWA, RFA and LA, respectively (Figure 9A). These results demonstrated that the overall complications of RFA was the lowest. The differences in the pooled proportion among the three therapies in overall complications were statistically significant (P=0.008). No publication bias was found in funnel plot and Egger’s test (P=0.136) (Figure 9B).
All seven major complications were voice changes lasting at least one month. Nine minor complications were reported including 2 cases of skin scald, 1 case of hematoma, 3 cases of pain, and 3 cases of hoarseness lasting less than 1 month. All hoarseness resolved within 1 month after ablation. In addition to pain relieved by medication, all minor complications resolved spontaneously within 3 months. The incidences of major and minor complications were 2.2% (7/312) and 2.9% (9/312), respectively.
A sensitivity analysis was used to evaluate the reliability of the results. When one study was deleted at a time, no such deletion had any significant impact on the results.
This meta-analysis showed that ultrasound-guided thermal ablation was an effective treatment for CMLNs of PTC. The pooled estimate for mean VRR of CMLNs after thermal ablation was 91.28% (95% CI: 86.60-95.97%), and the pooled estimate for serum Tg was 5.96 ng/ml (95%CI: 3.68-8.24 ng/ml). The pooled proportion of complete disappearance of CMLNs was 63.3% (95%CI: 46.7-78.5%), and the pooled proportion of recurrence after ablation was 7.8% (95%CI: 3.0 -14.1%). In addition, the pooled proportion of major complications was very low (0.3%, 95%CI: 0-1.9%), and all of them were non-life-threatening voice changes. Based on the above results, all three thermal ablation techniques have shown efficacy and safety for the treatment of CMLNs of PTC.
So far, many studies have described the safety and efficacy of thermal ablation for the treatment of CMLNs of PTC. However, there are no definitive guidelines on how RFA, LA, and MWA should be used to treat CMLNs of PTC, and few studies are comparing these three treatments (39, 40). In addition, due to the lack of well-designed prospective randomized trials, a direct comparison among them is difficult for the treatment of CMLNs of PTC. Therefore, our systematic review and meta-analysis collected the available evidence, which was crucial and will promote clinical practice.
Through subgroup analysis of treatment methods, the mean VRR of CMLNs was comparable between MWA (97.97%) and RFA (95.57%), while that of LA was lower (84.46%). This finding was consistent with a meta-analysis by Choi et al (41), who found comparable VRR between RFA and MWA in the treatment of papillary thyroid microcarcinoma. In addition, Javadov et al. (42) found that the VRR of RFA and MWA for the treatment of benign thyroid nodules was comparable, which was similar to our result. However, our findings were for CMLNs of PTC, rather than benign thyroid nodules and papillary thyroid microcarcinoma reported in these studies.
In our current study, we found that thermal ablation was effective in the treatment of CMLNs of PTC, although existing heterogeneity. It could be attributed to the following reasons. First, there were differences among the three thermal ablations. Second, the follow-up time of some studies was not long enough to observe the results, which may affect the accuracy of these results. Third, some studies reported that the proportion of complete disappearance was very low, which may be due to the residual calcification or scar-like lesions remained. These residues had not changed significantly after one year, but no obvious enhancement was observed on contrast-enhanced ultrasound, and no tumor cells were found in FNA. Lastly, the difference in recurrence may be related to different definitions of recurrence.
Overall, thermal ablation was safe for the treatment of CMLNs of PTC. The pooled proportions of overall (2.9%, 95%CI: 0.3-7.1%) and major (0.3%, 95% CI: 0 -1.9%) complications were similar to those previously reported in a meta-analysis evaluating the safety of thermal ablation for the treatment of papillary thyroid microcarcinoma (pooled proportions of overall and major complications:3.2% and 0.7%, respectively) (5). However, in a meta-analysis of the safety and efficacy of MWA for the treatment of benign thyroid nodules and papillary thyroid microcarcinoma, the pooled proportions of major and minor complications were 11.5% and 5.1% (43), respectively. All were higher than the results of this study. In fact, in the subgroup analysis by treatment modality, we found that the pooled proportion of major complications of MWA was higher than that of the other two methods, although the difference was not statistically significant. The reasons for this difference may be attributed to the following aspects. First of all, compared with other thermal ablations, MWA could achieve a larger ablation area in a shorter time (44, 45). The risk of thermal damage was greater, which was more likely to affect the surrounding recurrent laryngeal nerve, a relatively high incidence of major complications. Secondly, this difference may be related to variation in operators’ experience or procedural techniques, so it did not necessarily mean that the safety of MWA was lower than that of the other two methods. The pooled proportion of overall complications of RFA was lower than that of the other two treatments, and the difference was statistically significant. The low incidence of RFA complications may be due to the slow rise of RFA temperature and the easy removal of heat (46). Except for the slight difference in the incidence of complications among different treatments, no life-threatening complications were reported in all studies, which confirmed that all thermal ablations were safe.
In terms of heterogeneity, very little heterogeneity was present for the major complications of CMLNs of PTC (P=0.64, I2 =0%). However, significant between-study heterogeneity was noted for the largest diameter, volume, VRR, serum Tg, and complete disappearance of CMLNs of PTC (P<0.001). After subgroup analysis by treatment modality, we noticed that each treatment had great heterogeneity, with I2 exceeding 80%. We believed that a small number of studies included in each subgroup might be attributable to this finding. In addition, the heterogeneity among studies was moderate in terms of recurrence and overall complications of CMLNs of PTC (P=0.02, I2 =47.76%; P=0.02, I2 =44.82%). LA accounted for most of the heterogeneity (I2 =70.80%; I2 =68.97%), while MWA showed no heterogeneity (I2 =0%), which may indicate that MWA may have more consistent treatment effects than LA.
Three treatment modalities are achieved by the thermal ablation mechanism (45). Compared with surgery, thermal ablation has the advantages of small trauma, low incidence of complications, and rapid recovery. It is a good treatment for patients with surgical contraindications or rejection of surgery. However, it should be noted that some small CMLNs may not be detected by ultrasound (47), which will reduce the therapeutic effect to some extent. In the included studies, the follow-up time varied from 6 to 52 months. For some studies, the follow-up time may not be long enough to accurately determine the efficacy of thermal ablations. Although some studies have not been included in our study due to the small sample size, it is undeniable that they have achieved good therapeutic effects. In the future, we need to further verify the efficacy and safety of thermal ablations in a longer follow-up period.
There are some limitations to our study. First, there are few studies included. Although thermal ablation develops rapidly, its application in CMLNs of PTC is less. Second, most studies are retrospective studies, which may affect the accuracy of the results. Moreover, the included studies were mainly concentrated in China, South Korea, and Italy. Our meta-analysis results may not be similar in other regions because of the different clinical practice environments in these regions.
In conclusion, the current systematic review and meta-analysis comprehensively reviewed the safety and efficacy of RFA, LA, and MWA for the treatment of CMLNs of PTC. Our results show that thermal ablation is safe and effective. However, future research needs longer follow-ups and more population studies.
The original contributions presented in the study are included in the article/Supplementary Material. Further inquiries can be directed to the corresponding author.
WT, XT and DJ were major contributors in writing the manuscript. XZ, XN, and RW contributed to literature search, screening, and data extraction. YZ, MZ, and XW contributed to statistical analyses. WT and XT contributed to data validation. .WT and CZ are responsible for review and modification of the manuscript. All authors read and approved the final manuscript.
All the authors of included original studies should be appreciated sincerely.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fendo.2022.967044/full#supplementary-material
1. vanSonnenberg E, Simeone JF. Microwave ablation versus surgery for papillary thyroid carcinoma: More therapeutic options, more controversies. Radiology (2022) 220896. doi: 10.1148/radiol.220896
2. Spartalis E, Karagiannis SP, Plakopitis N, Theodori MA, Athanasiadis DI, Schizas D, et al. Percutaneous laser ablation of cervical metastatic lymph nodes in papillary thyroid carcinoma: Clinical efficacy and anatomical considerations. Expert Rev Med Devices (2021) 18(1):75–82. doi: 10.1080/17434440.2021.1864323
3. Fontenot TE, Deniwar A, Bhatia P, Al-Qurayshi Z, Randolph GW, Kandil E. Percutaneous ethanol injection vs reoperation for locally recurrent papillary thyroid cancer: A systematic review and pooled analysis. JAMA otolaryngol– Head Neck Surgery (2015) 141(6):512–8. doi: 10.1001/jamaoto.2015.0596
4. Weslley Rosario P, Franco Mourão G, Regina Calsolari M. Role of adjuvant therapy with radioactive iodine in patients with elevated serum thyroglobulin after neck reoperation due to recurrent papillary thyroid cancer: A monoinstitutional comparative study. Endocrine (2020) 68(1):144–50. doi: 10.1007/s12020-019-02165-8
5. Choi Y, Jung SL, Bae JS, Lee SH, Jung CK, Jang J, et al. Comparison of efficacy and complications between radiofrequency ablation and repeat surgery in the treatment of locally recurrent thyroid cancers: A single-center propensity score matching study. Int J hyperthermia Off J Eur Soc Hyperthermic Oncol North Am Hyperthermia Group (2019) 36(1):359–67. doi: 10.1080/02656736.2019.1571248
6. Kim JH, Yoo WS, Park YJ, Park DJ, Yun TJ, Choi SH, et al. Efficacy and safety of radiofrequency ablation for treatment of locally recurrent thyroid cancers smaller than 2 cm. Radiology (2015) 276(3):909–18. doi: 10.1148/radiol.15140079
7. Haugen BR, Alexander EK, Bible KC, Doherty GM, Mandel SJ, Nikiforov YE, et al. 2015 American Thyroid association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: The American thyroid association guidelines task force on thyroid nodules and differentiated thyroid cancer. Thyroid Off J Am Thyroid Assoc (2016) 26(1):1–133. doi: 10.1089/thy.2015.0020
8. Fu QQ, Kang S, Wu CP, Wang SY, Liu YY, Tian JW, et al. A study on the efficacy of microwave ablation for benign thyroid nodules and related influencing factors. Int J hyperthermia Off J Eur Soc Hyperthermic Oncol North Am Hyperthermia Group (2021) 38(1):1469–75. doi: 10.1080/02656736.2021.1988151
9. Nguyen VB, Nguyen TX, Nguyen VVH, Nguyen HT, Nguyen DT, Le CV. Efficacy and safety of single-session radiofrequency ablation in treating benign thyroid nodules: A short-term prospective cohort study. Int J Endocrinol (2021) 2021:7556393. doi: 10.1155/2021/7556393
10. Bernardi S, Giudici F, Cesareo R, Antonelli G, Cavallaro M, Deandrea M, et al. Five-year results of radiofrequency and laser ablation of benign thyroid nodules: A multicenter study from the Italian minimally invasive treatments of the thyroid group. Thyroid Off J Am Thyroid Assoc (2020) 30(12):1759–70. doi: 10.1089/thy.2020.0202
11. Zhou W, Jiang S, Zhan W, Zhou J, Xu S, Zhang L. Ultrasound-guided percutaneous laser ablation of unifocal T1N0M0 papillary thyroid microcarcinoma: Preliminary results. Eur Radiol (2017) 27(7):2934–40. doi: 10.1007/s00330-016-4610-1
12. Teng DK, Li HQ, Sui GQ, Lin YQ, Luo Q, Fu P, et al. Preliminary report of microwave ablation for the primary papillary thyroid microcarcinoma: A large-cohort of 185 patients feasibility study. Endocrine (2019) 64(1):109–17. doi: 10.1007/s12020-019-01868-2
13. Xiao J, Zhang Y, Yan L, Zhang M, Li X, Tang J, et al. Ultrasonography-guided radiofrequency ablation for solitary T1aN0M0 and T1bN0M0 papillary thyroid carcinoma: a retrospective comparative study. Eur J Endocrinol (2021) 186(1):105–13. doi: 10.1530/eje-21-0580
14. Kuo JH, Sinclair CF, Lang B, Spiezia S, Yu M, Ha EJ, et al. A comprehensive review of interventional ablation techniques for the management of thyroid nodules and metastatic lymph nodes. Surgery (2022) 171(4):920–31. doi: 10.1016/j.surg.2021.07.043
15. Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: Explanation and elaboration. BMJ (Clinical Res ed). (2009) 339:b2700. doi: 10.1136/bmj.b2700
16. Burke DR, Lewis CA, Cardella JF, Citron SJ, Drooz AT, Haskal ZJ, et al. Quality improvement guidelines for percutaneous transhepatic cholangiography and biliary drainage. J Vasc Interv Radiol (2003) 14(9 Pt 2):S243–6.
17. Lewis CA, Allen TE, Burke DR, Cardella JF, Citron SJ, Cole PE, et al. Quality improvement guidelines for central venous access. the standards of practice committee of the society of cardiovascular & interventional radiology. J Vasc Interv Radiol (1997) 8(3):475–9. doi: 10.1016/S1051-0443(97)70592-X
18. Copas J, Shi JQ. Meta-analysis, funnel plots and sensitivity analysis. Biostatistics (Oxford England) (2000) 1(3):247–62. doi: 10.1093/biostatistics/1.3.247
19. Petitti DB. Approaches to heterogeneity in meta-analysis. Stat Med (2001) 20(23):3625–33. doi: 10.1002/sim.1091
20. Lee J, Kim KW, Choi SH, Huh J, Park SH. Systematic review and meta-analysis of studies evaluating diagnostic test accuracy: A practical review for clinical researchers-part II. statistical methods of meta-analysis. Korean J Radiol (2015) 16(6):1188–96. doi: 10.3348/kjr.2015.16.6.1188
21. Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ (Clinical Res ed) (1997) 315(7109):629–34. doi: 10.1136/bmj.315.7109.629
22. Zhou W, Chen Y, Zhang L, Ni X, Xu S, Zhan W. Percutaneous microwave ablation of metastatic lymph nodes from papillary thyroid carcinoma: Preliminary results. World J Surgery (2019) 43(4):1029–37. doi: 10.1007/s00268-018-04879-8
23. Teng D, Ding L, Wang Y, Liu C, Xia Y, Wang H. Safety and efficiency of ultrasound-guided low power microwave ablation in the treatment of cervical metastatic lymph node from papillary thyroid carcinoma: A mean of 32 months follow-up study. Endocrine (2018) 62(3):648–54. doi: 10.1007/s12020-018-1711-4
24. Cao XJ, Wei Y, Zhao ZL, Peng LL, Li Y, Yu MA. Efficacy and safety of microwave ablation for cervical metastatic lymph nodes arising post resection of papillary thyroid carcinoma: A retrospective study. Int J hyperthermia Off J Eur Soc Hyperthermic Oncol North Am Hyperthermia Group (2020) 37(1):450–5. doi: 10.1080/02656736.2020.1759829
25. Yue W, Chen L, Wang S, Yu S. Locoregional control of recurrent papillary thyroid carcinoma by ultrasound-guided percutaneous microwave ablation: A prospective study. Int J hyperthermia Off J Eur Soc Hyperthermic Oncol North Am Hyperthermia Group (2015) 31(4):403–8. doi: 10.3109/02656736.2015.1014433
26. Han ZY, Dou JP, Cheng ZG, Liu FY, Yu J, Yu XL, et al. Efficacy and safety of percutaneous ultrasound-guided microwave ablation for cervical metastatic lymph nodes from papillary thyroid carcinoma. Int J hyperthermia Off J Eur Soc Hyperthermic Oncol North Am Hyperthermia Group (2020) 37(1):971–5. doi: 10.1080/02656736.2020.1805128
27. Lim HK, Baek JH, Lee JH, Kim WB, Kim TY, Shong YK, et al. Efficacy and safety of radiofrequency ablation for treating locoregional recurrence from papillary thyroid cancer. Eur Radiol (2015) 25(1):163–70. doi: 10.1007/s00330-014-3405-5
28. Wang L, Ge M, Xu D, Chen L, Qian C, Shi K, et al. Ultrasonography-guided percutaneous radiofrequency ablation for cervical lymph node metastasis from thyroid carcinoma. J Cancer Res Ther (2014) 10(Suppl):C144–9. doi: 10.4103/0973-1482.145844
29. Yan L, Zhang Y, Jiang B, Luo Y. Radiofrequency ablation for cervical metastatic lymph nodes in children and adolescents with papillary thyroid carcinoma: A preliminary study. Front Endocrinol (Lausanne) (2021) 12:624054. doi: 10.3389/fendo.2021.624054
30. Guang Y, Luo Y, Zhang Y, Zhang M, Li N, Zhang Y, et al. Efficacy and safety of percutaneous ultrasound guided radiofrequency ablation for treating cervical metastatic lymph nodes from papillary thyroid carcinoma. J Cancer Res Clin Oncol (2017) 143(8):1555–62. doi: 10.1007/s00432-017-2386-6
31. Baek JH, Kim YS, Sung JY, Choi H, Lee JH. Locoregional control of metastatic well-differentiated thyroid cancer by ultrasound-guided radiofrequency ablation. AJR Am J Roentgenol (2011) 197(2):W331–6. doi: 10.2214/AJR.10.5345
32. Guang Y, Luo YK, Zhang Y, Zhang MB, Li N, Zhang Y, et al. Ultrasound-guided radiofrequency ablation for cervical lymph nodes metastasis from papillary thyroid carcinoma. Zhongguo yi xue ke xue yuan xue bao Acta Academiae Medicinae Sinicae (2018) 40(1):67–71. doi: 10.3881/j.issn.1000-503X.2018.01.010
33. Papini E, Bizzarri G, Bianchini A, Valle D, Misischi I, Guglielmi R, et al. Percutaneous ultrasound-guided laser ablation is effective for treating selected nodal metastases in papillary thyroid cancer. J Clin Endocrinol Metab (2013) 98(1):E92–7. doi: 10.1210/jc.2012-2991
34. Mauri G, Cova L, Ierace T, Baroli A, Di Mauro E, Pacella CM, et al. Treatment of metastatic lymph nodes in the neck from papillary thyroid carcinoma with percutaneous laser ablation. Cardiovasc Intervent Radiol (2016) 39(7):1023–30. doi: 10.1007/s00270-016-1313-6
35. Mauri G, Cova L, Tondolo T, Ierace T, Baroli A, Di Mauro E, et al. Percutaneous laser ablation of metastatic lymph nodes in the neck from papillary thyroid carcinoma: Preliminary results. J Clin Endocrinol Metab (2013) 98(7):E1203–7. doi: 10.1210/jc.2013-1140
36. Guo Y, Li Z, Wang S, Liao X, Li C. Single-fiber laser ablation in treating selected metastatic lymph nodes of papillary thyroid carcinoma and benign cold thyroid nodules-preliminary results. Lasers Surg Med (2020) 52(5):408–18. doi: 10.1002/lsm.23150
37. Offi C, Misso C, Antonelli G, Esposito MG, Brancaccio U, Spiezia S. Laser ablation treatment of recurrent lymph node metastases from papillary thyroid carcinoma. J Clin Med (2021) 10(22). doi: 10.3390/jcm10225295
38. Zhang L, Zhou W, Zhan W. Role of ultrasound in the assessment of percutaneous laser ablation of cervical metastatic lymph nodes from thyroid carcinoma. Acta radiologica (Stockholm Sweden 1987). (2018) 59(4):434–40. doi: 10.1177/0284185117721261
39. Ding Z, Chen J, Chen Z, Zeng X, Zheng P, Wang X, et al. Efficacy and safety of thermal ablation for treating lymph node metastasis from papillary thyroid carcinoma: A systematic review and meta-analysis. Front Oncol (2022) 12:738299. doi: 10.3389/fonc.2022.738299
40. Qiu Y, Xing Z, He Y, Liu J, Yang Q, Luo Y. Ultrasound-guided thermal ablation for cervical lymph node metastasis from thyroid carcinoma: A meta-analysis of clinical efficacy and safety. Lasers Med science (2022) 37(3):1747–54. doi: 10.1007/s10103-021-03428-5
41. Choi Y, Jung SL. Efficacy and safety of thermal ablation techniques for the treatment of primary papillary thyroid microcarcinoma: A systematic review and meta-analysis. Thyroid Off J Am Thyroid Assoc (2020) 30(5):720–31. doi: 10.1089/thy.2019.0707
42. Javadov M, Karatay E, Ugurlu MU. Clinical and functional results of radiofrequency ablation and microwave ablation in patients with benign thyroid nodules. Saudi Med J (2021) 42(8):838–46. doi: 10.15537/smj.2021.42.8.20210307
43. Cui T, Jin C, Jiao D, Teng D, Sui G. Safety and efficacy of microwave ablation for benign thyroid nodules and papillary thyroid microcarcinomas: A systematic review and meta-analysis. Eur J Radiol (2019) 118:58–64. doi: 10.1016/j.ejrad.2019.06.027
44. Pfannenstiel A, Iannuccilli J, Cornelis FH, Dupuy DE, Beard WL, Prakash P. Shaping the future of microwave tumor ablation: a new direction in precision and control of device performance. Int J Hyperthermia Off J Eur Soc Hyperthermic Oncol North Am Hyperthermia Group (2022) 39(1):664–74. doi: 10.1080/02656736.2021.1991012
45. Geoghegan R, Ter Haar G, Nightingale K, Marks L, Natarajan S. Methods of monitoring thermal ablation of soft tissue tumors - a comprehensive review. Med Phys (2022) 49(2):769–91. doi: 10.1002/mp.15439
46. Tong M, Li S, Li Y, Li Y, Feng Y, Che Y. Efficacy and safety of radiofrequency, microwave and laser ablation for treating papillary thyroid microcarcinoma: A systematic review and meta-analysis. Int J hyperthermia Off J Eur Soc Hyperthermic Oncol North Am Hyperthermia Group (2019) 36(1):1278–86. doi: 10.1080/02656736.2019.1700559
Keywords: metastatic lymph nodes, thermal ablation, meta-analysis, systematic review, papillary thyroid carcinoma
Citation: Tang W, Tang X, Jiang D, Zhang X, Wang R, Niu X, Zang Y, Zhang M, Wang X and Zhao C (2022) Safety and efficacy of thermal ablation for cervical metastatic lymph nodes in papillary thyroid carcinoma: A systematic review and meta-analysis. Front. Endocrinol. 13:967044. doi: 10.3389/fendo.2022.967044
Received: 12 June 2022; Accepted: 01 August 2022;
Published: 22 August 2022.
Edited by:
Stefano Spiezia, Local Health Authority Naples 1 Center, ItalyReviewed by:
Chiara Offi, Local Health Authority Naples 1 Center, ItalyCopyright © 2022 Tang, Tang, Jiang, Zhang, Wang, Niu, Zang, Zhang, Wang and Zhao. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Cheng Zhao, emhhb2NoZW5nZHJAMTYzLmNvbQ==
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.