
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Endocrinol. , 08 August 2022
Sec. Obesity
Volume 13 - 2022 | https://doi.org/10.3389/fendo.2022.954755
This article is part of the Research Topic Association of Novel Anthropometric Indexes with Metabolic Syndrome and Beyond, volume II View all 16 articles
A correction has been applied to this article in:
Corrigendum: Prevalence of overweight and obesity among saudi children: a comparison of two widely used international standards and the national growth references
 Hazzaa M. Al-Hazzaa1*
Hazzaa M. Al-Hazzaa1* Amani A. Alrasheedi2
Amani A. Alrasheedi2 Rayan A. Alsulaimani3
Rayan A. Alsulaimani3 Laura Jabri4
Laura Jabri4 Abdulrahman M. Alhowikan5
Abdulrahman M. Alhowikan5 Maha H. Alhussain6
Maha H. Alhussain6 Rowaedh A. Bawaked7
Rowaedh A. Bawaked7 Saleh A. Alqahtani8,9
Saleh A. Alqahtani8,9Objective: To compare three body mass index (BMI) classifications that are used to assess the prevalence of overweight and obesity among Saudi children aged 6–13 years: the International Obesity Task Force (IOTF) age and gender cutoffs, the World Health Organization (WHO) growth references for school-aged children, and the Saudi (KSA) national growth references.
Methods: The sample comprised 2,169 children (52.5% girls) derived from two cross-sectional studies conducted in Riyadh and Jeddah during the 2017 and 2019 school years, respectively. Body weight and height were measured, and BMI was calculated.
Results: The proportions (%) of the participants who were classified as underweight, overweight, and obese varied according to the reference used: IOTF reference (13.8, 18.4, and 12.7), WHO reference (17.2, 19.1, and 18.9), and KSA reference (7.0, 22.4, and 9.3), respectively, indicating higher values for overweight and obesity prevalence when the WHO references were used. Kappa agreement measures between the three references were found to be high, with the coefficients ranging from 0.936 (between the IOTF and KSA references) to 0.849 (between the IOTF and WHO references). In all three classifications, girls exhibited lower overweight or obesity prevalence than boys. Family income, but not paternal or maternal education, was significantly (p = 0.015) associated with overweight/obesity when using the IOTF standards. In addition, having a small family in the house was significantly (p < 0.05) associated with obesity, irrespective of the classification system.
Conclusion: Inconsistency was observed when estimating the prevalence of underweight, overweight, and obesity among Saudi children. However, when defining the overall prevalence of overweight plus obesity among Saudi children, the IOTF classification system performed in a similar way to the KSA references (31.1% versus 31.7%) compared to the WHO references (38.0%).
Childhood obesity is arguably the most serious recent public health challenge (1). Indeed, it is a worldwide public health concern with many major negative consequences (2, 3). Being overweight or obese in childhood and adolescence is associated with greater risk and earlier onset of chronic disorders, such as type 2 diabetes (2). Childhood and adolescent obesity have been shown to have adverse psychosocial consequences and lower educational attainment (3), and excess body weight in childhood and adolescence is more likely to lead to lifelong overweight and obesity (4, 5). Additionally, in a recent eight-country study, the economic impacts of obesity were found to be substantial in all eight countries, regardless of economic or geographical setting, ranging from 0.8% of gross domestic product (GDP) in India to 2.4% in Saudi Arabia (6).
The age-standardized prevalence of obesity increased globally from 0.7% (0.4–1.2%) in 1975 to 5.6% (4.8–6.5%) in 2016 in girls, and from 0.9% (0.5–1.3%) in 1975 to 7.8% (6.7–9.1%) in 2016 in boys (7). However, the prevalence of obesity was about 20% or more in several countries and regions, such as Polynesia and Micronesia, the Middle East and North Africa, the Caribbean, and the USA (7). In Saudi Arabia, the percentage of children classified as overweight or obese has significantly increased in the past two decades (8–11). A recent review of overweight and obesity among Saudi children found that the ranges of overweight and obesity were larger in boys (19.3–35.6%) than in girls (11.8–19.2%) (10).
The implementation of school-based BMI measurement has become popular as a potential approach to addressing overweight and obesity among youth (12). However, defining overweight and obesity in children and adolescents is not as straightforward as it is in adults. Usually, the International Obesity Task Force (IOTF) BMI cutoff values are used, which are set using data collected from six countries: Singapore, the Netherlands, Brazil, Hong Kong, the UK, and the USA (13). Another approach is to use the World Health Organization’s (WHO) reference standards for children and adolescents aged 5–19 years, which are based on weight-for-height Z-scores (14). Both of these methods for defining overweight and obesity in children are generally valid; however, they often produce different results. Within the same population, the IOTF reference tends to yield the lowest values, and the WHO reference tends to yield the highest values (15–20). For instance, a study involving Saudi national data reported major differences between the use of Saudi growth charts of weight for age (21) and the WHO reference (14). The study concluded that the utilization of the WHO standards in Saudi Arabia, and possibly similar countries, increases the reported prevalence of undernutrition, stunting, and wasting, which potentially leads to unnecessary referrals, investigations, and parental concern (21).
Thus, it is challenging to determine the actual prevalence of underweight, overweight, and obesity among children and adolescents when such inconsistency exists among the most common international classification systems (13, 14). Therefore, the present study aimed to compare the three classifications that are used to assess overweight and obesity among Saudi children aged 6–13 years, namely the IOTF age and gender cutoff values (13), WHO growth references for school-aged children (14), and the Saudi (KSA) national growth references (22).
The population in this study consisted of healthy students of both sexes aged 6–13 years who attended public and private primary schools in two major cities in Saudi Arabia. The sample was drawn from two cross-sectional studies conducted in Riyadh and Jeddah during the 2017 and 2019 school years, respectively (23, 24). Riyadh and Jeddah are the first- and second-most populated cities in Saudi Arabia, respectively. The two cities are also composed of a multiethnic population coming from all parts of the country. All healthy Saudi children enrolled in primary schools from grades 1–6 during the study periods were eligible for inclusion in the study. Detailed descriptions of the study design and sample selection were previously published (23, 24).
Briefly, the sample size was calculated assuming that the population proportion would yield the maximum possible sample size required (proportion = 0.50), with a 95% confidence level and a 4% margin of error. An additional 20% of participants were added to account for non-responders or missing data. A representative random sample was chosen from schools in each selected city using a multistage stratified cluster sampling technique. Stratification was based on sex (boys’ and girls’ schools are segregated in Saudi Arabia), major geographical location (east, west, north, and south), and type of school (public versus private). Participating children were selected from primary schools relative to the actual number of students in public and private schools in each city. Within each area, one private and two public schools were randomly selected. Then, classes were randomly selected from each of the six grades. All Saudi students in the designated classes were invited to participate in the study.
Measurements of body weight (to the nearest 100 g) and standing height (to the nearest 0.1 cm) were performed at the schools by trained researchers using calibrated portable scales (Seca 869, UK) and height measuring rods, respectively. Students wore minimal clothing and no shoes when the measurements were taken. Body mass index (BMI) was computed as the ratio of weight in kilograms divided by the squared height in meters.
The outcome measure in the present study was the classification of the BMI data into the categories of underweight, normal weight, overweight, and obesity. Two commonly used international reference standards (cutoff values) were used to classify the BMI data. The first was the extended IOTF age- and sex-specific BMI cutoff reference standards, which are based on data from children and adolescents in six countries: Brazil, Hong Kong, the Netherlands, Singapore, the UK, and the USA (13). The second was the WHO growth references for school-aged children and adolescents (5–19 years), published in 2007 and based on weight-for-height Z-scores (14). For comparison, we also included the KSA national growth references (from underweight to obesity), which were calculated from the z−scores of BMI for age for children and adolescents aged 5–18 years (22). The IOTF references provide percentile cut-offs corresponding to a BMI of 18.5, 25, and 30 kg/m2 at 18 years of age for underweight, over weight, and obesity, respectively (13). The prevalence of underweight, overweight, and obese are defined by the WHO (14) and the KSA (22) cut-off values as BMI-for-age less than 2 standard deviation (SD) scores below the mean, greater than 1 SD above the mean, and greater than 2 SDs above the mean, respectively. All three classification systems used are all based on the lambda (L), mu (M), and sigma (S) method (25, 26). The LMS parameters correspond to median BMI (M), coefficient of variation (S), and the power in the Box–Cox transformation (L), which transforms the data so that it closely resembles a normal distribution (25, 26).
Ethical approval was obtained from the Institutional Review Board (IRB) at King Saud University, Riyadh (IRB Log Number: 17/0064/IRB) and Princess Nourah bint Abdulrahman University, Riyadh (IRB Log Number: 19-0014). The research procedures were conducted in accordance with the principles stated in the Declaration of Helsinki. Written informed consent was obtained from all parents/guardians of the participating children. In addition, approval for conducting this research in schools was attained from the Riyadh and Jeddah directorates of schools, the Ministry of Education, and the principals of the selected schools.
Data were entered into an SPSS data file, checked for accuracy, cleaned, and analyzed using the IBM-SPSS software, version 22 (Chicago, IL, USA). Descriptive statistics were obtained for the selected variables and reported as means and standard deviations or percentages for continuous or categorical variables, respectively. Differences between boys and girls in selected measurements were tested using the t-test for independent samples. Chi-square tests of proportions were used to test the differences in BMI classifications (prevalence rates) based on the IOTF, WHO, or KSA national growth references relative to selected sociodemographic factors. Kappa agreement measures for the whole sample were assessed between the three reference standards. Logistic regression analysis, adjusted for age, was used to test the associations of selected sociodemographic variables with overweight/obesity versus non-overweight/non-obesity among Saudi children. Furthermore, Spearman’s rho correlation coefficients, while controlling for age, were calculated between obesity indices, based on the IOTF, WHO, and KSA reference standards, and selected variables. The alpha level was set at 0.05, and a p-value less than the alpha level was considered significant.
Table 1 presents the descriptive characteristics of the participants. The study included 2,169 participants (52.5% girls) who were between 6 and 13 years of age, and the mean age (SD) was 9.3 (1.7) years. There were significant differences in body weight (p = 0.001), BMI (p < 0.001), and maternal education (p = 0.005) relative to the sex of the participants. However, no significant differences were observed in age, height, paternal education, or family income relative to the sex of the participants.
The proportions (%) of the participants who were classified as underweight, normal weight, overweight, or obese using the IOTF, WHO, and KSA references relative to age are shown in Table 2. In general, it was found that the proportion of participants categorized as overweight or obese increased with age when all three classifications were used. Overall, the underweight and obesity prevalence rates were much lower when the KSA reference standards were used than when the other two references were used. Whereas the combined overweight and obesity prevalence was much higher when the WHO reference standards were used. This finding is depicted in Figure 1, which shows the prevalence of overweight or obesity by age groups for the three classifications. Also, Spearman’s rho correlation coefficients, while controlling for age, between the three reference standards were fairly high (IOTF reference with WHO reference: r = 0.915, p < 0.001; IOTF reference with KSA reference: r = 0.914, p < 0.001; and WHO reference with KSA reference: r = 0.866, p < 0.001).
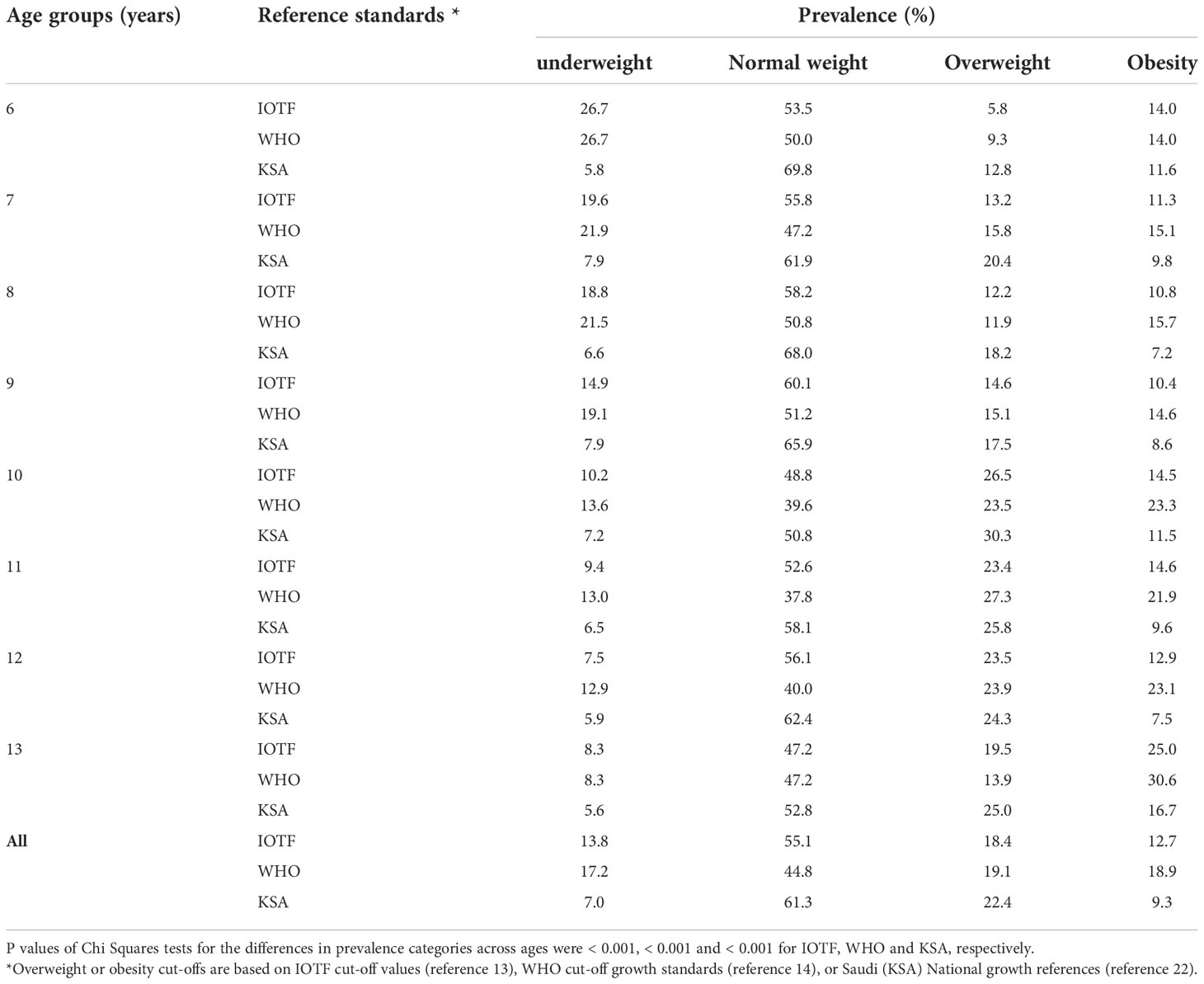
Table 2 The prevalence of underweight, normal weight, overweight, and obesity among Saudi children using IOTF or WHO reference standards relative to age.
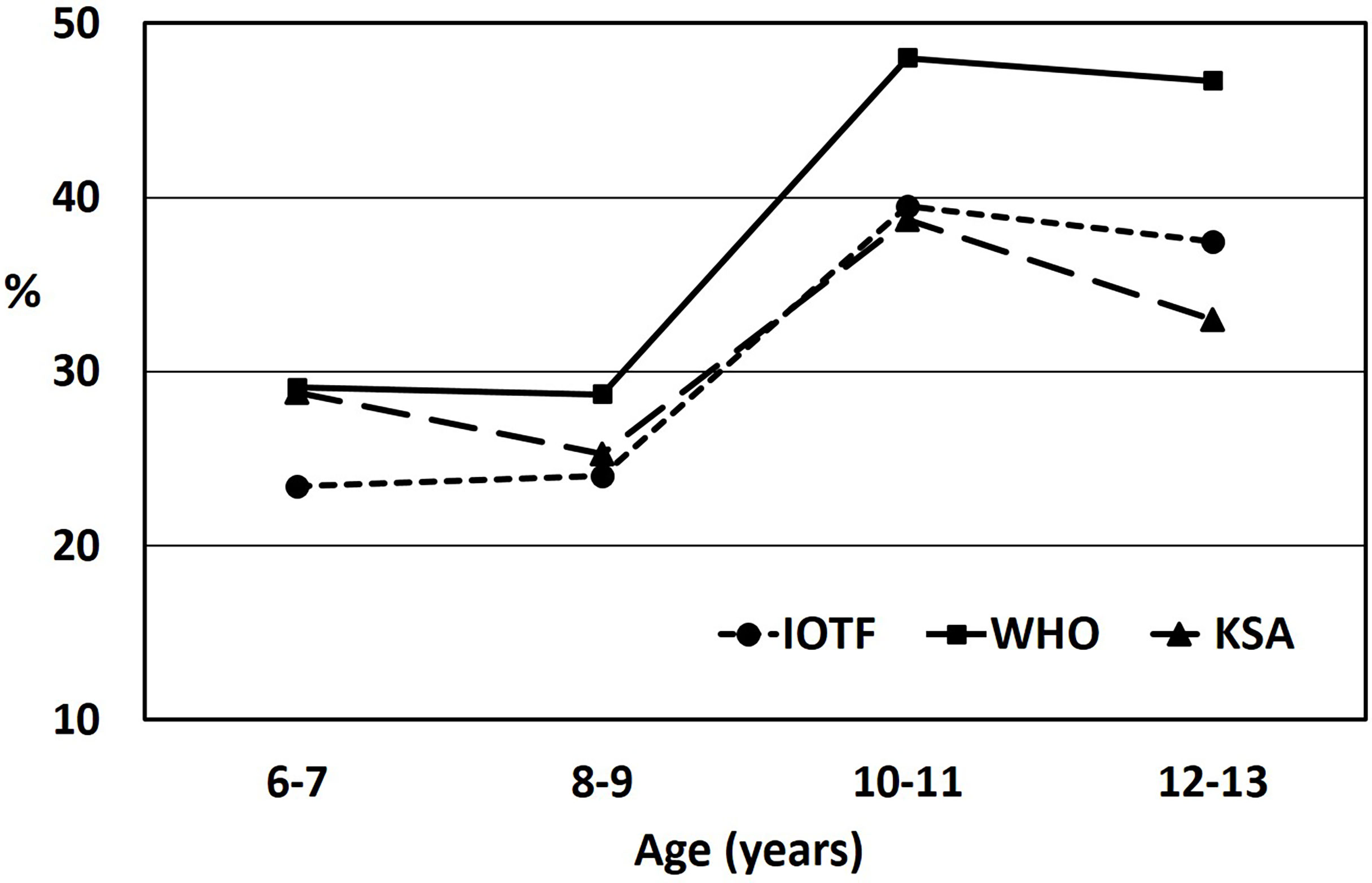
Figure 1 Overweight or obesity prevalence among Saudi children relative to age, based on International Obesity Task Force cut-off standards (IOTF), World Health Organization (WHO) reference standards, or Saudi (KSA) National growth references. Significant differences at p < 0.001 in all reference standards were found relative to age.
Figure 2 illustrates the prevalence of overweight or obesity based on the IOTF, WHO, or KSA references relative to sex. It is clear that, for either sex, the reported overweight or obesity prevalence was higher when the WHO reference standards were used compared to when the IOTF or KSA references were used. There were significant differences found between the boys’ and girls’ reference standards relative to sex (p values for the IOTF reference = 0.048, the WHO reference = 0.009, and the KSA reference = 0.005). In addition, Kappa agreement measures for the entire sample between the three reference standards were found to be fairly high; the coefficients were as follows: between the IOTF and KSA references = 0.936 (p < 0.001), between the WHO and KSA references = 0.862 (p < 0.001), and between the IOTF and WHO references = 0.849 (p < 0.001).
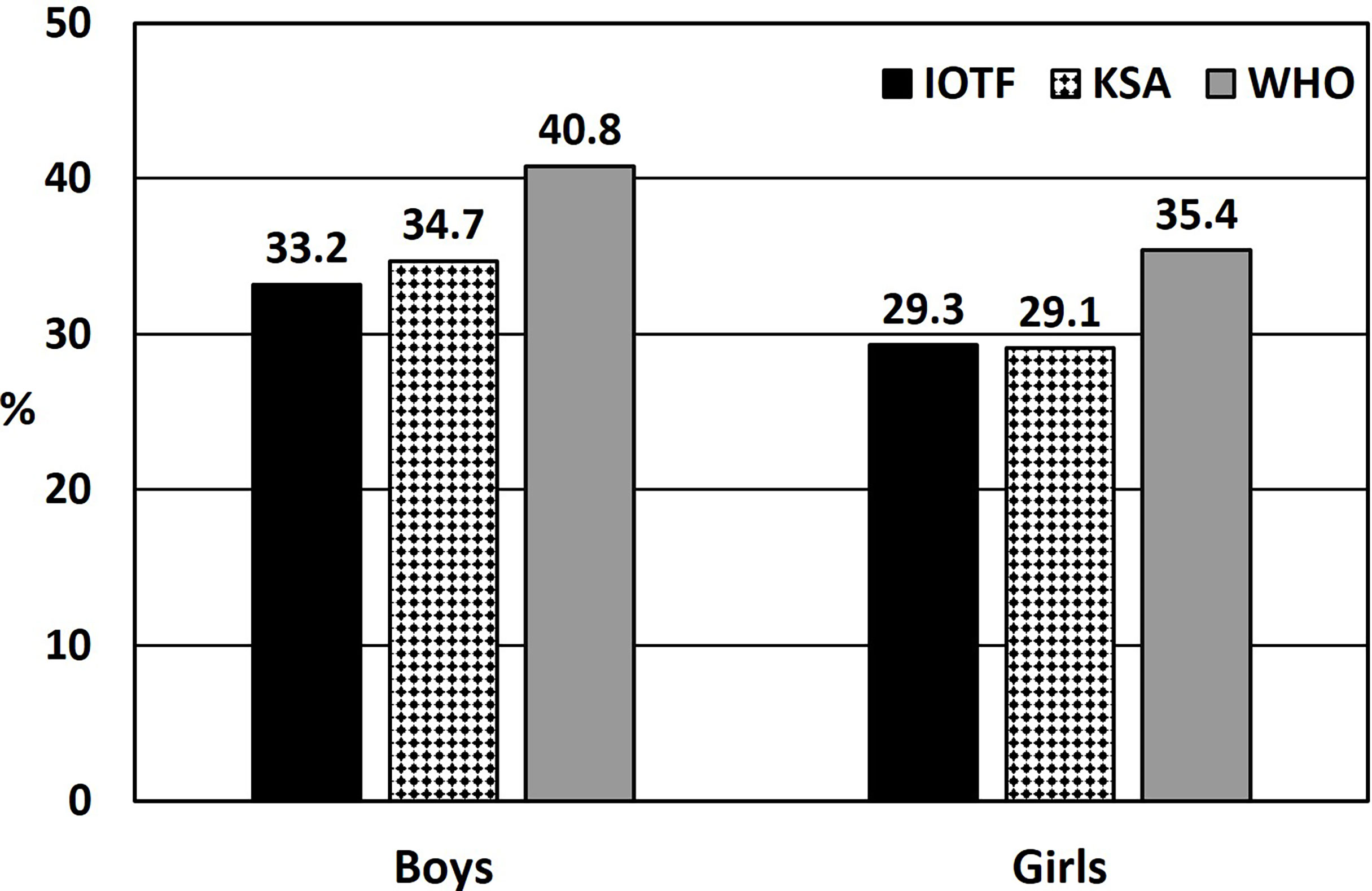
Figure 2 Overweight or obesity prevalence among Saudi children relative to sex, based on International Obesity Task Force cut-off standards (IOTF), World Health Organization (WHO) reference standards, or Saudi (KSA) National growth references. Significant differences between boys’ and girls’ reference standards (p values for IOTF = 0.048, WHO = 0.009, and KSA = 0.005).
Table 3 displays the prevalence of underweight, normal weight, overweight, and obesity among the participating children when the IOTF, WHO, or KSA reference standards were used relative to selected variables. In each case, the prevalence rates of the BMI categories relative to sex, city, family income, and number of family members living in the house were all significant (p-values ranged from < 0.001 to 0.034). However, there was no significant difference between the prevalence rates relative to school type, paternal, or maternal education when any reference standards were used.
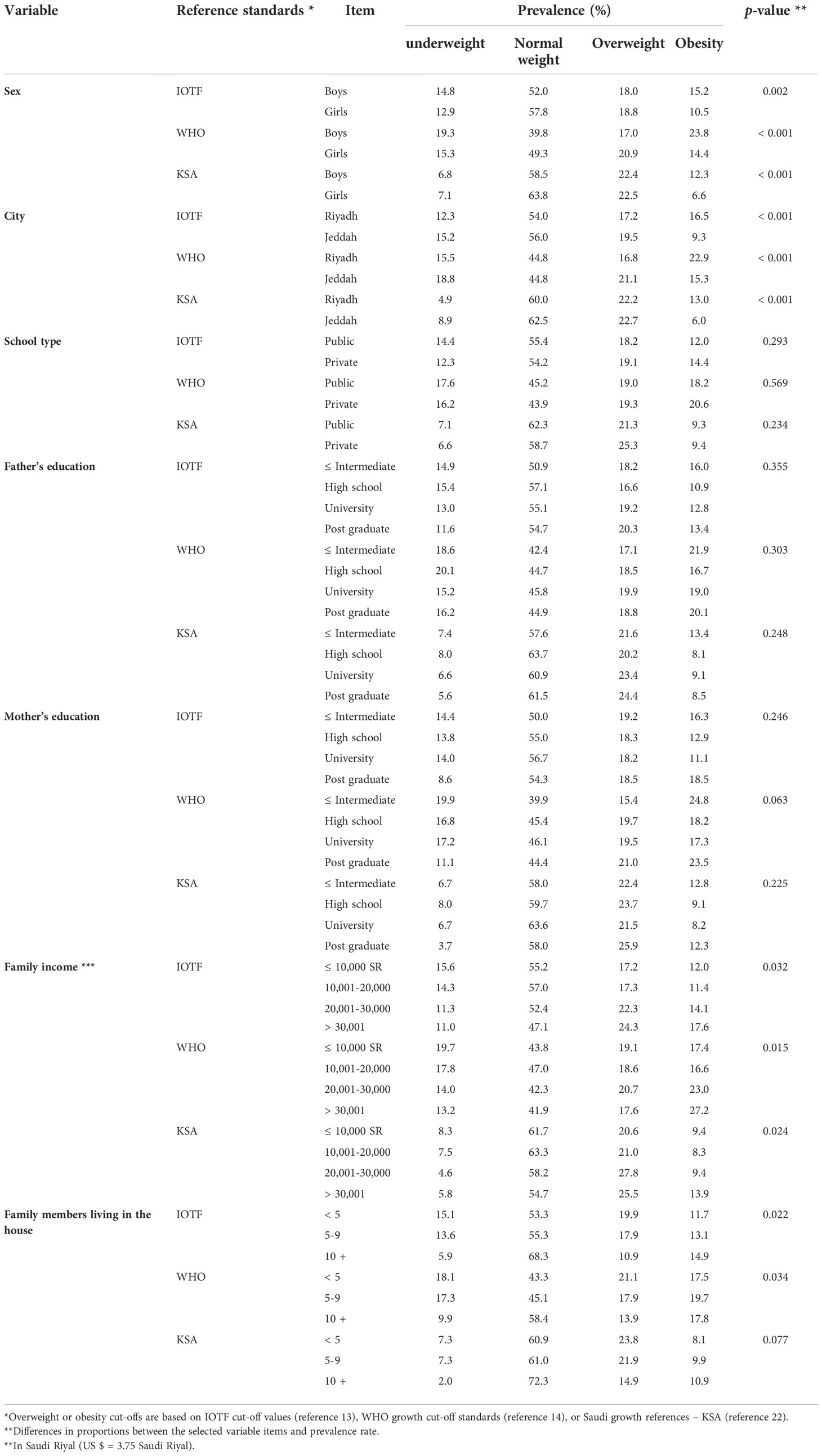
Table 3 The prevalence of underweight, normal weight, overweight, and obesity among Saudi children using IOTF or WHO reference standards relative to selected variables.
Table 4 shows the logistic regression analysis results, adjusted for age, for selected sociodemographic variables relative to overweight/obesity versus non-overweight/non-obesity among the participants. There were significant associations (p < 0.001) between overweight/obesity and increasing age when all three classification standards were used. However, only when the WHO (p = 0.043) and KSA (p = 0.036) standards were used was there a significant association between overweight/obesity and sex (boys). In terms of geographic region, the incidence of overweight/obesity compared to the incidence of non-overweight/non-obesity was higher in children living in Riyadh than in children living in Jeddah when the references from the IOTF (p = 0.031) and KSA (p = 0.005) were used, but not when the WHO reference was used (p = 0.122). Furthermore, having a small family (2–5 members) in the house was associated with increased prevalence of overweight/obesity irrespective of the classification system (p values ranged from 0.017 to 0.025). Parental education levels did not show any significant association with overweight/obesity in all classification systems. Finally, a low to intermediate family income of (10,001–20,000 Saudi Riyals) was found to be significantly (p = 0.015) associated with overweight/obesity when using the IOTF standards.
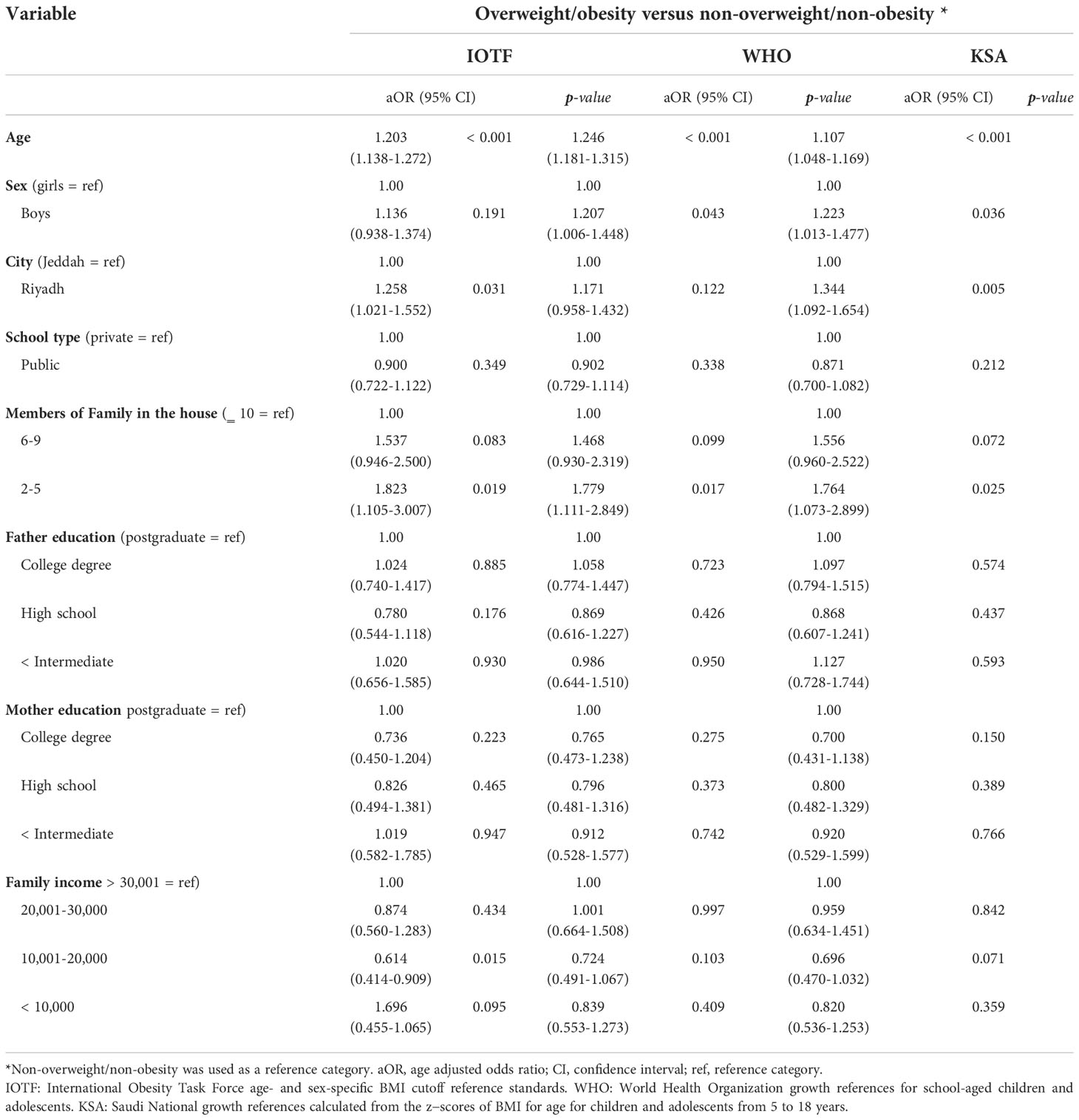
Table 4 Results of logistic regression analysis, adjusted for age, of selected sociodemographic variables relative to overweight/obesity versus non-overweight/non-obesity among Saudi children.
The present study aimed to compare the results of three different BMI classifications (the IOTF age and gender cutoffs, the WHO growth references for school-aged children, and the KSA national growth references) using data obtained from Saudi children aged 6–13 years. The findings showed that the proportions of the participants classified as overweight or obese were fairly high, regardless of the classification system used. The IOTF cutoffs appear to be somewhat closer to the KSA growth references than to the WHO references. In all three classifications, girls exhibited lower overweight or obesity prevalence than boys. Family income, but not paternal or maternal education, was significantly associated with overweight/obesity when the IOTF standards were used. In addition, having a small family in the house was significantly associated with obesity, irrespective of the reference used. Hence, it seems that estimating the prevalence of underweight, overweight, and obesity among Saudi children yields inconsistent results when the IOTF, WHO, and KSA growth references are used.
Regardless of the BMI reference standards used, we observed a high prevalence of overweight and obesity among the participants, with somewhat variable levels of underweight status. It appears that the prevalence of overweight and obesity among Saudi children and adolescents has been rising over the last decades (9, 10). Recently, it was observed that the most important risk factors for obesity among Saudi children 5–9 years-of-age are parental characteristics, awareness of the degree of obesity burden, and lifestyle behaviors, such as frequent snacking, physical inactivity, and screen time (27). Also, among Saudi children and adolescents, obesity and other risk factors were found to have a significant impact on abnormal glucose metabolism (28). Therefore, efforts to prevent overweight and obesity in children must focus primarily on early identification, followed by appropriate reduction of common risk factors.
The present study found a higher prevalence of underweight, overweight, and obesity when the WHO reference standards were used compared to the IOTF cutoffs and the KSA national growth references. Currently, the use of age- and gender-specific BMI cutoffs is recommended to estimate overweight and obesity status among children and adolescents (13, 14, 29). However, it is somewhat challenging to estimate overweight and obesity prevalence when the most common international classification systems reveal different results (15–20, 30, 31). It appears that the discrepancies resulting from the use of the IOTF and WHO reference standards are due to differences in the cutoff values, the criteria used to select the sample, and the approaches used to define the cutoffs (32). An understanding of how the IOTF and WHO BMI standards for children and adolescents are constructed and their comparability may provide an explanation of their inherent limitations. In contrast to adult anthropometric cutoffs, which are based on mortality outcomes (33, 34), BMI cutoffs for children under the age of 18 years are statistically determined (13, 14). Indeed, it was reported that using the IOTF cutoffs and population-specific standards for childhood BMI failed to adequately predict cardiovascular disease risk factors in mid-adulthood from childhood BMI values (35). Accordingly, the choice of the reference standards used to express BMI data may influence the status of overweight and obesity among children from different populations. In addition, such differences in overweight and obesity, based on various cut-off references, may impact policy decision-making. In light of such limitations, many studies have argued that common references cannot be applied to children from different populations since they differ in their growth patterns (36–38). However, from the findings of the present study, it appears that the agreement between the IOTF and KSA references is much closer than that between the WHO and KSA references, when defining overweight plus obesity prevalence among Saudi children.
In terms of agreement measures, the Kappa agreement measures among the three reference standards were found to be fairly high, with the coefficients ranging from 0.936 between the IOTF and KSA references to 0.849 between the IOTF and WHO references. A lower Kappa coefficient (0.72) was reported between the IOTF and WHO references in a study with Brazilian children (39). Moreover, agreement between the IOTF and WHO references and French references ranged from moderate (Kappa = 0.43) to perfect (Kappa = 1.00) among French children (40). However, in a group of South American children, moderate agreements were observed between body fat estimated by dual-energy x-ray absorptiometry (DXA) and by the IOTF (Kappa = 0.61) and WHO (Kappa = 0.63) references, with the IOTF cutoffs showing the highest specificity (0.98 [0.94, 0.99]) (41). Data from a study conducted with Italian children and adolescents aged 5–17 years indicated that the WHO references had the highest sensitivity, while the IOTF classification had the highest specificity, in identifying obese subjects with clustered cardiometabolic risk factors (42).
Previous local, regional, and international studies have reported varying prevalence rates of overweight and obesity among children and adolescents when using the IOTF or WHO reference standards. Among Saudi adolescents from Riyadh, the IOTF reference reportedly produced more conservative (by 4–6%) estimates of overweight and obesity than the WHO reference standards (43). The average difference in overweight/obesity prevalence when using IOTF and WHO references in our study was 6.9%. In another study conducted on 6–16-year-old school children from Riyadh, the overall prevalence rates of overweight and obesity, as defined by the WHO 2007 growth standards, were reported to be 13.4% (14.2% for girls and 12% for boys) and 18.2% (18% for girls and 18.4% for boys), respectively (11). In comparison, in the present study with children aged 6–13 years, the overweight prevalence was higher (19.1%), but the obesity rate was similar (18.9%).
At the regional level, among a group of 10–14-year-old Kuwaiti adolescents, the prevalence of overweight and obesity calculated using Kuwaiti local reference data (36.7%) was significantly lower than that obtained using the IOTF (44.7%) or WHO (50.5%) reference standards (44). In another study, the prevalence of overweight and obesity among school children aged 10–13 years in Bahrain was calculated to be higher when the WHO reference was used compared to when the IOTF reference was used (17). Also, a school-based cross-sectional study conducted in eight Arab countries, including Saudi Arabia, involving adolescents aged 15–18 years showed that the use of the WHO standard resulted in a lower prevalence of overweight but a higher prevalence of obesity than the use of the IOTF reference standards (45).
Internationally, studies have shown varying degrees of consistency. Among 5–17-year-old Canadian children and adolescents, 16.4% of the participants were classified as overweight and 8.4% as obese when the IOTF reference was used, while 19.8% were classified as overweight and 11.7% as obese when the WHO standards were used (18). Moreover, the IOTF classification appears to be more specific when applied to identify overweight and obesity among indigenous Canadian school children aged 8–14 years than other systems, such as those of the Centers for Disease Control and Prevention (CDC) and the WHO (15). A recent study involving Cree youth revealed that participants classified as overweight by the IOTF classification system, but not by the WHO reference standards, displayed less severe clinical obesity (20). That is, false-positive subjects with obesity identified by WHO cutoffs were effectively classified as overweight by IOTF (20). Inconsistency was also apparent when the prevalence of underweight, overweight, and obesity among Malaysian children aged 6–14 years was estimated; use of the WHO reference resulted in a higher prevalence of overweight and obesity than the use of the IOTF reference (31). Thus, from previous studies’ findings, it appears that the IOTF reference standards are more accurate than those of the WHO in identifying children and adolescents with obesity (15–20, 38).
Paternal or maternal education levels in the current study did not show any significant association with overweight/obesity in all classification systems. However, family income exhibited a significant association with overweight/obesity when the IOTF standards were used. However, when the WHO 2007 growth standards were used, overweight and obesity among school children from Riyadh aged 6–16 years appeared to significantly increase with higher socioeconomic status, including higher family income (11). In a study involving adolescents from eight Arab countries, including Saudi Arabia, major differences in obesity prevalence were found among the eight countries when both the IOTF and WHO reference standards were used, and the differences were attributed to a variety of factors, including socioeconomic status (45). Also, in a population-based cross-sectional study involving Pakistani children aged 5–12 years, a significant correlation was found between overweight and obesity status and high socioeconomic status, whereas body thinness was associated with low socioeconomic status and lower parental education (30). Interestingly, an analysis of data from a large number of children aged 6–9 years in 24 countries in the WHO European region showed that there was an inverse relationship between the prevalence of childhood overweight or obesity and parental education in high-income countries, and a positive correlation was observed in most of the middle-income countries (46).
Across all three classification systems used in this study, girls exhibited lower overweight or obesity incidence than boys. This finding aligns with results reported in some previous studies that used the IOTF or WHO cutoff references (10, 31, 47). However, others have reported mixed results (11, 15, 17, 20, 38). Finally, our findings revealed that having a small family in the house was significantly associated with increased prevalence of overweight/obesity irrespective of the reference used. This is an important finding of the present study. A recent study from the United States indicated that having more siblings is associated with lower BMI and decreased likelihood of obesity (48). It may be speculated that larger families may have a bigger reason to prepare and eat meals at home, which means better meal quality for children. Also, small families may be more inclined (and can afford) to eat outside home, which may include more fast foods. Another confounding factor for the relationship between obesity and family size may include family income, however, the correlation between family size and income was weak in the present study. It is possible that physical activity and dietary intake may influence body weight, but we did not assess these two factors in the present study.
The present study has some strengths and limitations. The strengths of this study include a relatively large sample size and representative BMI data from children in two major Saudi cities. Also, measurements of weight and height were performed directly and did not rely on self-reporting. In addition, the sample was drawn from both public and private schools. The present study, however, has some limitations. First, the findings are limited to children aged 6–13 years and cannot be generalized to adolescents aged 14–17 years or preschoolers from 2-5 years. Second, the sample was drawn from urban areas and cannot be generalized to children residing in rural areas.
The proportions of the Saudi children who were classified as overweight or obese appeared to be fairly high, regardless of the classification system used. The IOTF cutoffs appear to be somewhat closer to the KSA growth references than to the WHO references. The Kappa agreement measures between the three references were found to be high, with the coefficients ranging from as high as 0.936 (between the IOTF and KSA references) to as low as 0.849 (between the IOTF and WHO references). In all three classifications, girls exhibited a lower incidence of overweight or obesity compared with boys. Family income, but not parental or maternal education, exhibited a significant positive association with obesity when using the IOTF standards. In addition, having a large family in the house was significantly associated with decreased obesity, irrespective of the IOTF or WHO references. It seems that using the IOTF, WHO, or KSA growth references to estimate the prevalence of underweight, overweight, and obesity among Saudi children leads to inconsistent results. However, the agreement between the IOTF and KSA references is much closer than that between the WHO and KSA references, which means that the IOTF classification system performed in a similar way to the KSA references (31.1% versus 31.7%) compared to the WHO references (38.0%) when assessing the overall prevalence of overweight plus obesity among Saudi children. Therefore, the choice of the currently available BMI classification systems has important implications for child health and the assessment of clinical obesity.
The original contributions presented in the study are included in the article/supplementary material. Further inquiries can be directed to the corresponding author.
Ethical approval was obtained from the Institutional Review Board (IRB) at King Saud University, Riyadh (IRB Log Number: 17/0064/IRB) and Princess Nourah bint Abdulrahman University, Riyadh (IRB Log Number: 19-0014). Written informed consent to participate in this study was provided by the participants‘ legal guardian/next of kin.
Conceptualization: HA-H. Methodology: HA-H, AMA, MA, AAA, LJ, and RA. Investigation: HA-H, AMA, MA, AAA, LJ, RA, RB, and SA. Data collection and supervision: HA-H, AMA, MA, AAA, LJ, and RA. Statistical analysis: HA-H. Interpretation of the findings: HA-H, AMA, MA, AAA, LJ, RA, RB, and SA. Drafting the paper: HA-H. Reviewing and editing the draft: AMA, MA, AAA, LJ, RA, RB, and SA. All authors critically read, revised the draft for important intellectual content, approved the final version of the manuscript to be published, and agreed to be accountable for all aspects of the work.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
We would like to thank all the participants and their parents for taking part in this study. Also, appreciation is extended to all research assistants who helped during the data collection.
1. Lobstein T, Baur L, Uauy R. IASO international obesity task force. obesity in children and young people: a crisis in public health. Obes Rev (2004) Suppl 1:4–104. doi: 10.1111/j.1467-789X.2004.00133.x
2. Park M, Falconer C, Viner R, Kinra S. The impact of childhood obesity on morbidity and mortality in adulthood: a systematic review. Obes Rev (2012) 13:985–1000. doi: 10.1111/j.1467-789X.2012.01015.x
3. Quek YH, Tam WW, Zhang MW, Ho R. Exploring the association between childhood and adolescent obesity and depression: a meta-analysis. Obes Rev (2017) 18:742–54. doi: 10.1111/obr.12535
4. Singh AS, Mulder C, Twisk JW, van Mechelen W, Chinapaw MJ. Tracking of childhood overweight into adulthood: a systematic review of the literature. Obes Rev (2008) 9:474–88. doi: 10.1111/j.1467-789X.2008.00475.x
5. Whitaker RC, Wright JA, Pepe MS, Seidel KD, Dietz WH. Predicting obesity in young adulthood from childhood and parental obesity. N Engl J Med (1997) 337(13):869–73. doi: 10.1056/NEJM199709253371301
6. Okunogbe A, Nugent R, Spencer G, Ralston J, Wilding J. Economic impacts of overweight and obesity: current and future estimates for eight countries. BMJ Glob Health (2021) 6(10):e006351. doi: 10.1136/bmjgh-2021-006351
7. NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population based measurement studies in 128·9 million children, adolescents, and adults. Lancet (2017) 390:2627–42. doi: 10.1016/S0140-6736(17)32129-3
8. Al-Hazzaa HM. Prevalence and trends in obesity among school boys in central Saudi Arabia between 1988 and 2005. Saudi Med J (2007) 28:1569–74.
9. Al-Hazzaa HM, Abahussain N, Al-Sobayel H, Qahwaji D, Musaiger AO. Prevalence of overweight, obesity and abdominal obesity among urban Saudi adolescents: Gender and regional variations. J Health Popul Nutr (2014) 32:634–45.
10. Hammad SS, Berry DC. The child obesity epidemic in Saudi Arabia: A review of the literature. J Transcult Nurs (2017) 28:505–15. doi: 10.1177/1043659616668398
11. Al−Hussaini A, Bashir MS, Khormi M, AlTuraiki M, Alkhamis W, Alrajhi M, et al. Overweight and obesity among Saudi children and adolescents: Where do we stand today? Saudi J Gastroenterol (2019) 25:229–35. doi: 10.4103/sjg.SJG_617_18
12. Nihiser AJ, Lee SM, Wechsler H, McKenna M, Odom E, Reinold C, et al. BMI measurement in schools. Pediatrics (2009) 124 Suppl 1:S89–97. doi: 10.1542/peds.2008-3586L
13. Cole TJ, Lobstein T. Extended international (IOTF) body mass index cut-offs for thinness, overweight and obesity. Pediatr Obes (2012) 7:284–94. doi: 10.1111/j.2047-6310.2012.00064.x
14. de Onis M, Onyango A, Borghi E, Siyam A, Nishida C, Siekmann J. Development of a WHO growth reference for school-aged children and adolescents. Bull World Health Organization (2007) 85:661–8.
15. Medehouenou TC, Ayotte P, St-Jean A, Meziou S, Roy C, Muckle G, et al. Overweight and obesity prevalence among school-aged nunavik Inuit children according to three BMI classification systems. J Adolesc Health (2015) 57(1):31–6. doi: 10.1016/j.jadohealth.2015.03.022
16. Minghelli B, Nunes C, Oliveira R. Body mass index and waist circumference to define thinness, overweight and obesity in Portuguese adolescents: comparison between CDC, IOTF, WHO references. Pediatr Endocrinol Rev (2014) 12(1):35–41.
17. Musaiger AO, Al-Mannai, Al-Marzog Q. Overweight and obesity among children (10-13 years) in Bahrain: A comparison between two international standards. Pak J Med Sci (2014) 30(3):497–500. doi: 10.12669/pjms.303.4796
18. Roberts KC, Shields M, de Groh M, Aziz A, Jo-Anne Gilbert J-A. Overweight and obesity in children and adolescents: results from the 2009 to 2011 Canadian health measures survey. Health Rep (2012) 23:37–41.
19. Shields M, Tremblay MS. Canadian Childhood obesity estimates based on WHO, IOTF and CDC cut-points. Int J Pediatr Obes (2010) 5(3):265–73. doi: 10.3109/17477160903268282
20. St-Jean A, Meziou S, Ayotte P, Lucas M. Overweight and obesity prevalence among cree youth of eeyou istchee according to three body mass index classification systems. BMC Pediatr (2017) 17(1):196. doi: 10.1186/s12887-017-0951-4
21. El Mouzan MI, Foster PJ, Al Herbish AS, Al Salloum AA, Al Omar AA, Qurachi MM, et al. The implications of using the world health organization child growth standards in Saudi Arabia. Nutr Today (2009) 44(2):62–70. doi: 10.1097/NT.0b013e31819dc6c5
22. El Mouzan MI, Al Salloum AA, Alqurashi MM, Al Herbish AS, Al Omar A. The LMS and z scale growth reference for Saudi school-age children and adolescents. Saudi J Gastroenterol (2016) 22(4):331–6. doi: 10.4103/1319-3767.187608
23. Al-Hazzaa HM, Alhowikan AM, Alhussain MH, Obeid OA. Breakfast consumption among Saudi primary-school children relative to sex and socio-demographic factors. BMC Public Health (2020) 20:448. doi: 10.1186/s12889–020-8418-1
24. Al-Hazzaa HM, Al-Rasheedi AA, Alsulaimani RA, Jabri L. Anthropometric, familial- and lifestyle-related characteristics of school children skipping breakfast in jeddah, Saudi Arabia. Nutrients (2020) 12:E3668. doi: 10.3390/nu12123668
25. Cole TJ, Bellizzi MC, Flegal KM, Dietz WH. Establishing a standard definition for child overweight and obesity worldwide: international survey. BMJ (2000) 320:1240–3. doi: 10.1136/bmj.320.7244.1240
26. Cole TJ, Green PJ. Smoothing reference centile curves: the LMS method and penalized likelihood. Stat Med (1992) 11(10):1305–19. doi: 10.1002/sim.4780111005
27. Aljassim H, Jradi H. Childhood overweight and obesity among the Saudi population: a case-control study among school children. J Health Popul Nutr (2021) 40(1):15. doi: 10.1186/s41043-021-00242-1
28. Al-Rubeaan K. National surveillance for type 1, type 2 diabetes and prediabetes among children and adolescents: a population-based study (SAUDI-DM). J Epidemiol Community Health (2015) 69(11):1045–51. doi: 10.1136/jech-2015-205710
29. National Institute of Health and Care Excellence. Obesity: Identification, assessment and management of overweight and obesity in children, young people and adults: NICE clinical guideline (2015). Available at: http://www.nice.org.uk/Guidance/CG43 (Accessed 27-4-2022).
30. Mushtaq MU, Gull S, Khurshid U, Shahid U, Shad MA, Siddiqui AM. Prevalence and socio-demographic correlates of stunting and thinness among Pakistani primary school children. BMC Public Health (2011) 11(1):790. doi: 10.1186/1471-2458-11-790
31. Partap U, Young EH, Allotey P, Sandhu MS, Reidpath DD. The use of different international references to assess child anthropometric status in a Malaysian population. J Pediatr (2017) 190:63–68.e1. doi: 10.1016/j.jpeds.2017.07.049
32. Monasta L, Lobstein T, Cole TJ, Vignerová J, Cattaneo A. Defining overweight and obesity in pre-school children: IOTF reference or WHO standard? Obes Rev (2011) 12(4):295–300. doi: 10.1111/j.1467-789X.2010.00748.x
33. Bhaskaran K, Dos-Santos-Silva I, Leon DA, Douglas IJ, Smeeth L. Association of BMI with overall and cause-specific mortality: a population-based cohort study of 3·6 million adults in the UK. Lancet Diabetes Endocrinol (2018) 6(12):944–53. doi: 10.1016/S2213-8587(18)30288-2
34. Berrington de Gonzalez A, Hartge P, Cerhan JR, Flint AJ, Hannan L, MacInnis RJ, et al. Body-mass index and mortality among 1. 46 million white adults N Engl J Med (2010) 363(23):2211–9. doi: 10.1056/NEJMoa1000367
35. Li L, Pinot de Moira A, Power C. Predicting cardiovascular disease risk factors in midadulthood from childhood body mass index: utility of different cutoffs for childhood body mass index. Am J Clin Nutr (2011) 93:1204–11. doi: 10.3945/ajcn.110.001222
36. Khadilkar VV, Khadilkar AV. Revised Indian academy of pediatrics 2015 growth charts for height, weight and body mass index for 5-18-year-old Indian children. Indian J Endocrinol Metab (2015) 19:470–6. doi: 10.4103/2230-8210.159028
37. Ma J, Wang Z, Song Y, Hu P, Zhang B. BMI percentile curves for Chinese children aged 7-18 years, in comparison with the WHO and the US centers for disease control and prevention references. Public Health Nutr (2010) 13:1990–6. doi: 10.1017/S1368980010000492
38. Mushtaq MU, Gull S, Mushtaq K, Abdullah HM, Khurshid U, Shahid U, et al. Height, weight and BMI percentiles and nutritional status relative to the international growth references among Pakistani school-aged children. BMC Pediatr (2012) 12:31. doi: 10.1186/1471-2431-12-31
39. Pelegrini A, Silva DAS, Gaya ACA, Petroski EL. Comparison of three criteria for overweight and obesity classification in Brazilian adolescents. Nutr J (2013) 12:5. doi: 10.1186/1475-2891-12-5
40. Kêkê LM, Samouda H, Jacobs J, di Pompeo C, Lemdani M, Hubert H, et al. Body mass index and childhood obesity classification systems: A comparison of the French, international obesity task force (IOTF) and world health organization (WHO) references. Rev Epidemiol Sante Publique (2015) 63(3):173–82. doi: 10.1016/j.respe.2014.11.003
41. Anzolin CC, Silva DA, Zanuto EF, Cayres SU, Codogno JS, Costa Junior P, et al. Accuracy of different cutoff points of body mass index to identify overweight according to body fat values estimated by DEXA. J Pediatr (Rio J) (2017) 93(1):58–63. doi: 10.1016/j.jped.2016.04.010
42. Valerio G, Balsamo A, Baroni MG, Brufani C, Forziato C, Grugni G, et al. Childhood obesity classification systems and cardiometabolic risk factors: a comparison of the Italian, world health organization and international obesity task force references. Ital J Pediatr (2017) 43(1):19. doi: 10.1186/s13052-017-0338-z
43. Alqahtani N, Scott J. Childhood obesity estimates based on WHO and IOTF reference values. J Obes Weight Loss Ther (2015) 5:249. doi: 10.4172/2165-7904.1000249
44. El-Ghaziri M, Boodai S, Young D, Reilly JJ. Impact of using national v. international definitions of underweight, overweight and obesity: an example from Kuwait. Public Health Nutr (2011) 14:2074–8. doi: 10.1017/S1368980011001285
45. Musaiger AO, Al-Mannai M, Al-Haifi AR, Nabag F, Elati J, Abahussain N, et al. Prevalence of overweight and obesity among adolescents in eight Arab countries: comparison between two international standards (ARABEAT-2). Nutr Hosp (2016) 33(5):567. doi: 10.20960/nh.567
46. Buoncristiano M, Williams J, Simmonds P, Nurk E, Ahrens W, Nardone P, et al. Socioeconomic inequalities in overweight and obesity among 6- to 9-year-old children in 24 countries from the world health organization European region. Obes Rev (2021) 22 Suppl 6:e13213. doi: 10.1111/obr.13213
47. Kunešová M, Vignerová J, Pařízková J, Procházka B, Braunerová R, Riedlová J, et al. Long-term changes in prevalence of overweight and obesity in Czech 7-year-old children: evaluation of different cut-off criteria of childhood obesity. Obes Rev (2011) 12(7):483–91. doi: 10.1111/j.1467-789X.2011.00870.x
Keywords: body mass index (BMI), children, International Obesity Task Force (IOTF), overweight, obesity, sociodemographic, underweight, World Health Organization (WHO)
Citation: Al-Hazzaa HM, Alrasheedi AA, Alsulaimani RA, Jabri L, Alhowikan AM, Alhussain MH, Bawaked RA and Alqahtani SA (2022) Prevalence of overweight and obesity among saudi children: A comparison of two widely used international standards and the national growth references. Front. Endocrinol. 13:954755. doi: 10.3389/fendo.2022.954755
Received: 27 May 2022; Accepted: 18 July 2022;
Published: 08 August 2022.
Edited by:
Mostafa Qorbani, Alborz University of Medical Sciences, IranReviewed by:
Nami Mohammadian Khonsari, Alborz University of Medical Sciences, IranCopyright © 2022 Al-Hazzaa, Alrasheedi, Alsulaimani, Jabri, Alhowikan, Alhussain, Bawaked and Alqahtani. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hazzaa M. Al-Hazzaa, aGFsaGF6emFhQGhvdG1haWwuY29t
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.