- 1Department of Obstetrics and Gynecology, Fondazione Istituti di Ricovero e Cura a Carattere Scientifico (IRCCS) Policlinico San Matteo, Pavia, Italy
- 2Department of Obstetrics and Gynecology, University of Pavia, Pavia, Italy
- 3Department of Pathology, Fondazione Istituti di Ricovero e Cura a Carattere Scientifico (IRCCS) Policlinico San Matteo, Pavia, Italy
- 4Department of Brain and Behavioural Sciences, University of Pavia, Pavia, Italy
- 5Child Neurology and Psychiatry Unit, Istituti di Ricovero e Cura a Carattere Scientifico (IRCCS) Mondino Foundation, Pavia, Italy
The placenta plays a fundamental role during pregnancy for fetal growth and development. A suboptimal placental function may result in severe consequences during the infant’s first years of life. In recent years, a new field known as neuroplacentology has emerged and it focuses on the role of the placenta in fetal and neonatal brain development. Because of the limited data, our aim was to provide a narrative review of the most recent knowledge about the relation between placental lesions and fetal and newborn neurological development. Papers published online from 2000 until February 2022 were taken into consideration and particular attention was given to articles in which placental lesions were related to neonatal morbidity and short-term and long-term neurological outcome. Most research regarding the role of placental lesions in neurodevelopment has been conducted on fetal growth restriction and preterm infants. Principal neurological outcomes investigated were periventricular leukomalacia, intraventricular hemorrhages, neonatal encephalopathy and autism spectrum disorder. No consequences in motor development were found. All the considered studies agree about the crucial role played by placenta in fetal and neonatal neurological development and outcome. However, the causal mechanisms remain largely unknown. Knowledge on the pathophysiological mechanisms and on placenta-related risks for neurological problems may provide clues for early interventions aiming to improve neurological outcomes, especially among pediatricians and child psychiatrists.
Introduction and aim of the study
The placenta represents the interface between the mother and the fetus; for this reason, the study of placental histological lesions and neonatal outcomes has spread greatly in recent years. As we all know, the placenta plays a fundamental role in the growth and development of the fetus, not only by allowing the transport of nutrients and oxygen and removing waste products from the fetal circulation (1), but also by constituting a protective and selective barrier for the passage of hormones, neurotransmitters, toxic agents and infectious microorganism (2, 3).
A compromised placental function may result in a higher risk of morbidity of the fetus and it may have consequences during the infant’s first years of life, but also later during adulthood.
Barker et al. firstly discovered the link between the nutritional environment in utero and cardiovascular morbidities in adults (4). From that moment, other adult chronic diseases, such as type 2 diabetes, insulin resistance, obesity, hypertension and cardiovascular disorders, have all been linked to fetal programming (5) in which the placenta plays a key role.
In recent years, a new field known as “neuroplacentology” has emerged: it focuses on the placenta’s role in protecting and shaping fetal and neonatal brain development.
As seen for other pathologies, placental failure can directly damage the developing brain or increase its susceptibility to injury, leading to possible permanent neurological disabilities (6). By adverse neurological outcomes, we observe organic lesions (periventricular leukomalacia, intraventricular hemorrhages, and strokes), alterations in neurocognitive development and neuropsychiatric disorders (autism spectrum disorders) and motor deficits which can arise both immediately after birth and in subsequent years (neonatal encephalopathy) (6–9).
However, the increasing literature data about neuroplacentology need a review in order to understand the relationship between placental histological lesions and impaired neurodevelopmental outcomes. In our opinion, it is very important to highlight the fact that placental unit dysfunction impairs the neurological development in two categories of newborn: fetal growth restriction and preterm.
Materials and methods
We consulted the most significant medical databases, including PubMed, Cochrane Database of Systematic Reviews, EMBASE, and Web of Science, according to a combination of the following keywords: neuroplacentology, placental pathology and neurological outcome, neurological morbidity, placental epigenetics and neurodevelopment, and cerebral palsy, including pluralization and US English/UK English spelling variations and suffixes/prefixes.
For our analysis, all papers published online from 2000 until February 2022, including literature reviews, case series, and retrospective or prospective trials, were considered. We performed the research by employing a narrative review method (10, 11).
The first selection was based on the title, the second on the abstract, and the third on the full-text article.
We selected for analysis, study in which placental lesions were related to neonatal morbidity and short-term and long-term neurological outcomes. Therefore, we included only papers in which the following criteria were met: (I) description of histological placental lesions linked to adverse neurological outcomes (II) types of neurological injuries induced by placental impairment (III) most frequent placental functional modifications in newborns with a major risk of developing neurological disease, (IV) Redline classification of placental lesions (12).
The selected articles were assessed as full-text and resulting information was tabulated.
Exclusion criteria were as follows: (I) case reports considered to be of minor significance in this field were excluded by the present literature review; (II) abstracts of medical conferences, editorials, and preliminary studies; (III) multimedia materials regarding the aim of the study; (IV) papers written in languages other than English, (V) studies regarding the TORCH complex, (VI), studies regarding twin pregnancy, and chromosomal abnormalities.
Bias across studies as well as bias and risks related to the source of funding and conflict of interest of authors of the included studies, were assessed. Eventual disagreements were resolved through discussion.
Results
For our purpose, a total of 1500 articles were identified by a searching strategy and 10 were identified through the references. Duplicated papers, presented in more than one database, and irrelevant works were not considered for our analysis; furthermore, after removing articles not published in English and published before 2000, 500 articles were screened by title and/or abstract. Full-text articles were assessed on the remaining 80 studies.
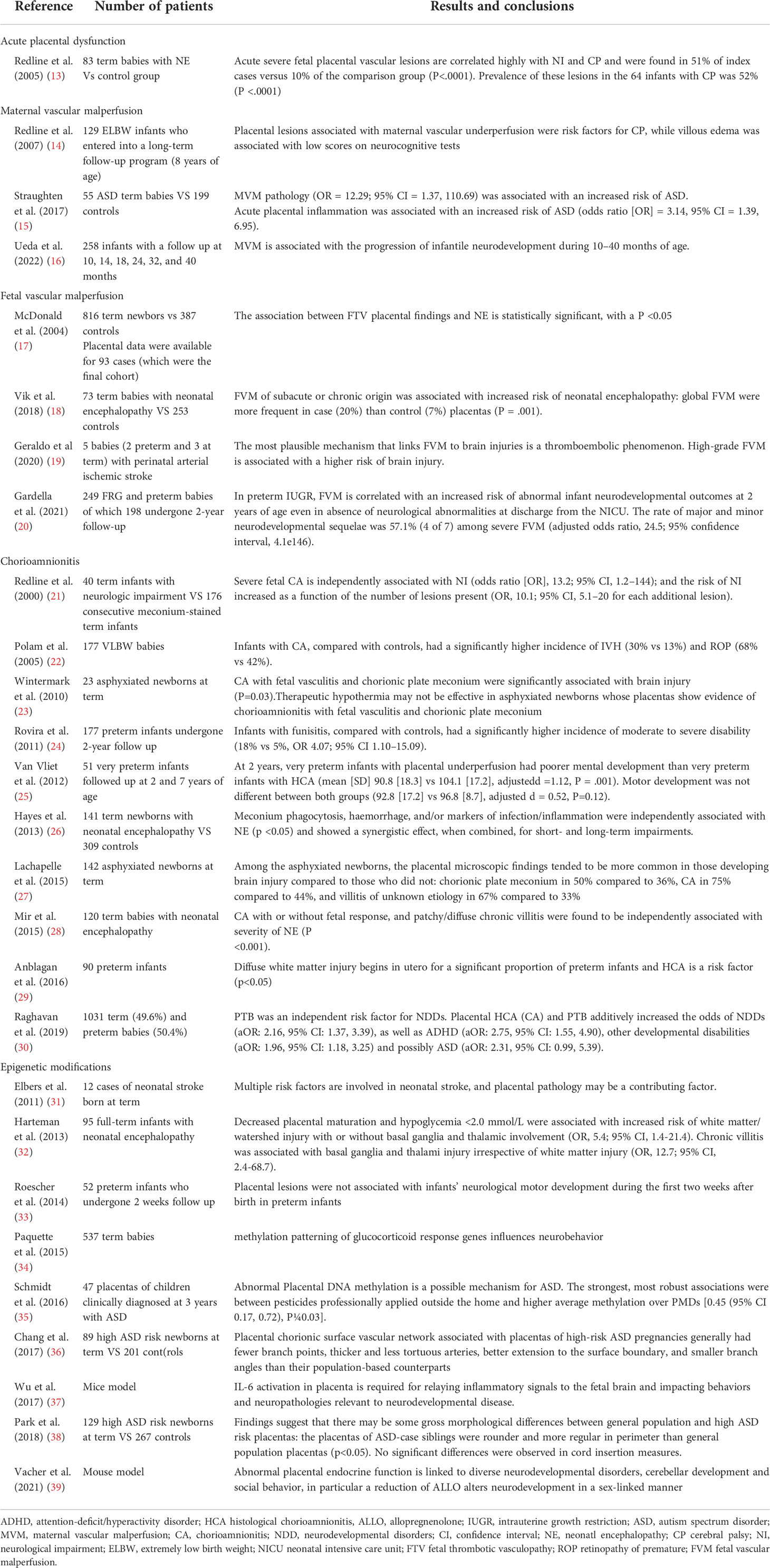
Finally, 27 studies were included and compared (Table 1). Among these, 6 studies focused on long term neurological outcomes (14, 20, 24, 25, 31, 40) with follow-up periods between 2 weeks (40) and 8 years (14).
Acute placental dysfunction
Acute placental dysfunction regards the main placental lesions found in term newborns affected by neurological impairments. The correlation between neurological injuries and placenta pathology was investigated in term newborns in 9 of the research analyses included in the review (13, 17, 21, 23, 26–28, 34).
The main placental lesions investigated were acute interruption of placental circulation, such as in abruptio placentae or umbilical cord true knots, thrombosis, wrapping and torsion. These conditions commonly correlate with neurological hypoxic-ischemic injuries both before and/or during delivery (13, 23, 27, 41, 42) which are neonatal encephalopathy (13, 18, 21), neonatal stroke (31, 43), periventricular leukomalacia and intraventricular hemorrhage (13, 18, 21).
Maternal vascular malperfusion and fetal vascular malperfusion
On the other hand, most of the literature research has focused on preterm and FGR newborns because of their close connection with neurological injuries. In these fetuses the most frequent vascular placental lesions are maternal vascular malperfusion and fetal vascular malperfusion (13, 44).
Maternal vascular malperfusion (MVM) is predominantly associated with an increased risk of autism spectrum disorders 15, but it is also correlated with cerebral palsy, periventricular hemorrhage (14, 25).
In several research analysis, fetal vascular malperfusion (FVM) has been linked to neonatal encephalopathy and cerebral palsy, particularly in term infants (13, 17, 18), while in preterm babies it may be responsible for lower 2-year neurodevelopmental general quotient (GQ) by Griffiths’ Scales, in particular referring to personal-social abilities, hearing, speech and performance subscales scores (20), while it seems to not be associated with short-term neonatal outcomes (20).
Chorioamnionitis
Histological chorioamnionitis has been linked to the etiology of neuropsychiatric disorders, including generalized cognitive impairment, autism spectrum disease and schizophrenia (45–50). However, white matter brain lesions (51–53) and abnormalities in social behavior, complex learning tasks and sensorimotor gating (46–48) represent the most significant adverse outcomes related to chorioamnionitis. Furthermore, if associated with funisitis and fetal thrombotic vasculopathy, chorioamnionitis is involved in the development of neonatal encephalopathy (21, 23, 26, 28), and of intraventricular hemorrhage (22, 51, 54–56).
On the other hand, chronic villitis is also correlated with neonatal encephalopathy, nevertheless it is a non-infectious inflammatory process (17, 26, 28, 32).
Abnormal placental morphology
A different placental morphology may be associated with some altered neurological outcomes. It was reported that the placentas of fetuses affected by autism spectrum disorder (ASD) appeared thicker and rounder (38). Instead, Chang et al. observed some anatomical variations in the placentas of a cohort with an elevated risk of ASD, in particular in the vascular architecture: the placental arteries were thicker and less tortuous, more extended to the surface but with fewer branches and smaller branch angles than population-based counterparts (36). The placentas analyzed in this study (36) were taken from two independently collected cohorts, Early Autism Risk Longitudinal Investigation (EARLI) and National Children’s Study (NCS): EARLI includes pregnancies for a high risk of autism because it focuses on the prenatal and early life periods of children who have biological siblings affected by ASD (57). NCS is a cohort of pregnancies with an unknown risk for ASD, where placentas were used by Chang as an ASD low-risk population.
Epigenetic modifications
Nowadays, proteomic and metabolomic studies regarding placental dysfunction have found abnormal synthesis of glucocorticoids, due to maternal stressors (such as malnutrition or hypoxia) or barrier dysfunction. The exposition of fetal tissues to high levels of glucocorticoids (in particular cortisol), may lead to epigenetic changes (which are altered DNA methylation and altered mRNA expression) (58, 59) and may disturb the trajectory of multiple neurodevelopmental processes (60).
In 2015, Paquette et al. have demonstrated that methylation patterning of glucocorticoid response genes influences neurobehavior through quantification of placental methylation using bisulfite pyrosequencing in 537 term infant placentas and analyzing profiles of neurobehavior via the Neonatal Intensive Care Unit Network Neurobehavioral Scales (46).
Furthermore, the placenta is responsible for the production of neurotransmitters, such as serotonin, dopamine, norepinephrine and epinephrine: anything that compromises their passage from the placenta to the the fetal brain can increase the risk for neurobehavioral disorders (61).
Discussion
The possible mechanisms through which placenta can impact brain development are different. It is thought that an antenatal and/or an intra-partum one (6, 14, 17, 21), as well as both acute and chronic placental dysfunctions (41) are responsible for possible neurological impairments. The impact of such events depends on when they occur during gestation (41) and the histopathological examination of the placenta at the time of delivery is useful to understand the timing of the exposure during pregnancy (62).
For this reason and to highlight the importance of placental abnormal mechanisms and how they could impact neurodevelopment, we regrouped the articles in different sections: acute placental dysfunction, chorioamnionitis, MVF, FVF, and epigenetic and metabolic placental alterations (Table 1). Furthermore, for each section, we distinguished between term and preterm and/or FRG newborns.
Because the heterogeneity of placental lesions associated with adverse neurological outcomes reflects different pathways, we have listed the works in chronological order with the aim of not being a fully exhaustive review but only of highlighting the main points for the reader’s knowledge.
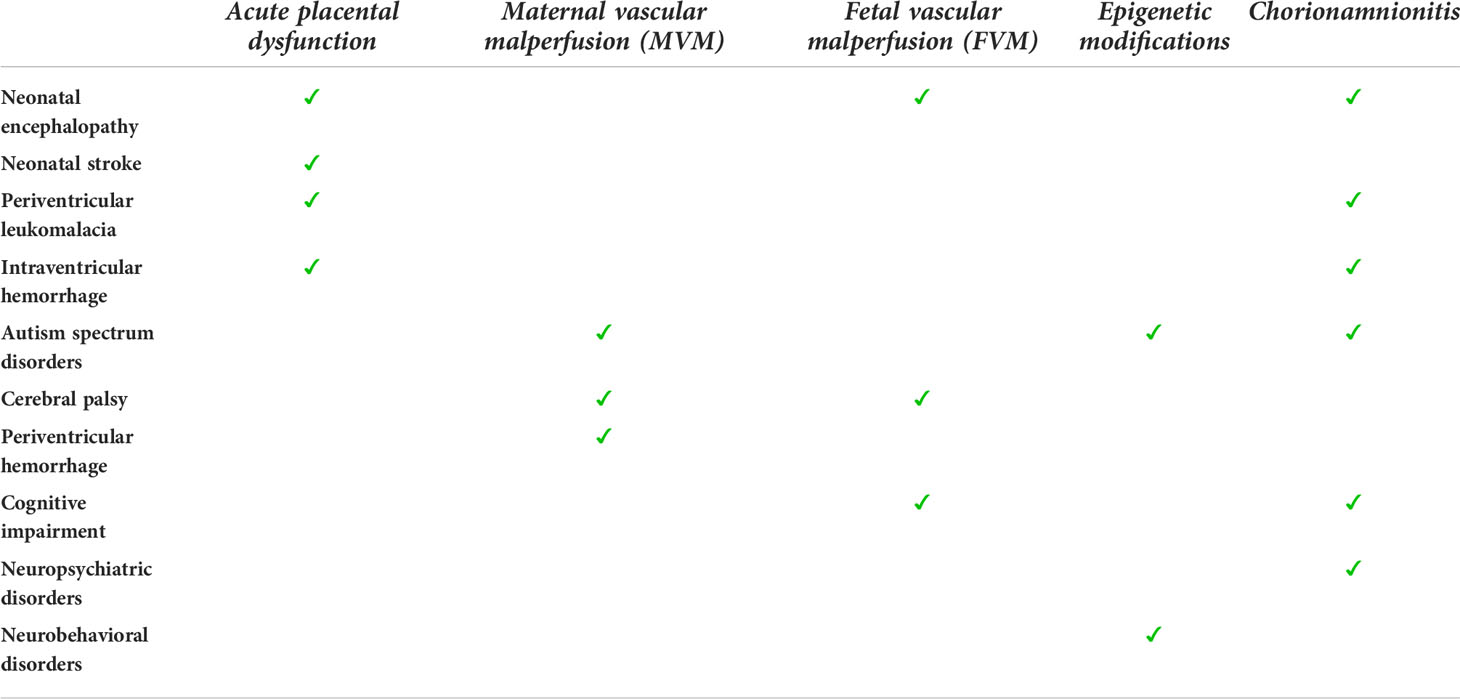
The commonalities and the correlations between placental lesions and fetal neurological outcomes are shown in Table 2.
Acute placental dysfunctions
Predominantly, they include the acute interruption of placental circulation, such as in abruptio placentae or umbilical cord true knots, thrombosis, wrapping and torsion, and commonly correlate with neurological hypoxic-ischemic injuries both before and/or during the delivery (13, 23, 27, 41, 42).
The complex causal pathway underlying how these placental injuries could bring to neurodevelopmental impairment is poorly understood, probably because only recently attention was paid to the lesions that affect the fetal placental side including fetal thrombosis, inflammation of the fetal vessel wall, and hemodynamically significant umbilical cord abnormalities. The fetal placental bed receives up to 55% of the total fetal cardiac output. Probably, these lesions influence fetal neurodevelopment through different pathways: an impaired fetoplacental vascular regulation, a decreased gas and metabolite exchange, the activation of platelets and leukocytes, the generation of cytokines and other thromboinflammatory mediators, the release of heat shock proteins from ischemic placental tissue, and embolism of placental thrombi to other fetal vascular beds (13).
Chronic placental dysfunction
However, most research regarding the role of placental lesions in neurological development has been conducted on IUGR and preterm infants, because these conditions are strongly associated with pathology of the placenta (63) and because prematurity is an independent risk factor for neurodevelopmental disabilities (30).
Histological chorioamnionitis, maternal vascular malperfusion, fetal vascular malperfusion and fetal thrombotic vasculopathy are the most common placental injuries associated with adverse neurological outcomes in preterm and FGR births (8, 20, 24, 25, 30, 64–66).
Fetal vascular malperfusion
Fetal vascular malperfusion, a term introduced by the Amsterdam International Consensus group of placental pathologists in 2015, indicates a reduced or absent perfusion of the villous parenchyma by the fetus (67). The most common etiology of FVM is umbilical cord obstruction, while other possible contributing factors are maternal diabetes, fetal cardiac insufficiency or hyperviscosity, inherited or acquired thrombophilias (67). Both fetal coagulopathy or a maternal hypercoagulable state, antiphospholipid antibody syndrome or antiplatelet antibodies which increase the likelihood of thrombosis (68).
Regarding brain injuries, fetal vascular malperfusion (FVM) has been associated with neonatal encephalopathy, cerebral palsy (13, 17, 18), and lower personal-social abilities, hearing, speech and performance subscales scores (20).
The most plausible mechanism that links FVM to brain injuries is a thromboembolic phenomenon. Indeed, it is believed that FVM-related thromboemboli spread into the venous fetal circulation, reaching the cerebral circulation through the right atrium, the foramen ovale and the fetal ductus arteriosus (69, 70). Vascular occlusion could interest both arterial and venous systems, even simultaneously (71).
Some common risk factors underlying FVM, activating coagulation and inflammatory pathways in both the arterial and venous system or a secondary reduction of venous flow in the dural sinuses, can be contributing factors (71, 72).
High-grade FVM is associated with a higher risk of brain injury (73), as demonstrated by Geraldo et al. in their case series: they described the clinical-neuroimaging features of 5 neonates with arterial ischemic stroke and highlighted that all the patients were classified as having high-grade FVM (19).
Maternal vascular malperfusion
Maternal vascular malperfusion (MVM) consists of a group of placental gross and histological findings regarding both maternal decidual vessels, reflecting abnormal spiral artery remodeling, and in the villous parenchyma, reflecting abnormalities in oxygenation and flow dynamics in the intervillous space (74). It is common in pregnancies complicated by preeclampsia and FGR, oligohydramnios, and stillbirth (75). The exact etiopathological mechanism that leads to MVM is not clear, but it seems that a defective deep spiral artery remodeling at the junctional zone is a fundamental process (74). It could be caused by a hypoxic-ischemic injury which leads to oxidative stress of the intervillous space (76).
Severe MVM is often associated with autism spectrum disorders (15), cerebral palsy, periventricular hemorrhage (14, 25). Probably, MVM may be responsible for hypoxic conditions in fetal blood, which may contribute to altered neurodevelopment during the early infantile period (16).
Chorioamnionitis
Chorioamnionitis is the inflammatory involvement of the chorion and the amnios, while we talk about funisitis, if the inflammation affects the umbilical cord, and of villitis when it affects the villous tree (77). From a histopathological point of view, they are all characterized by the infiltration of neutrophils (77). One of their most frequent causes is an intra-amniotic infection which could reach the amniotic cavity from the lower genital tract (78), from the maternal blood (79, 80), during invasive procedures (81) and maybe from the peritoneal cavity through the fallopian tubes.
Ascending microbial infection is the most frequent mechanism for intra-amniotic infection (81) and the most frequent microorganisms found are Ureaplasma, Gardnerella vaginalis, Fusobacterium species, Candida albicans (81). Rupture of membranes is not necessary for bacteria to reach the amniotic cavity (82).
But chorioamnionitis is also caused by a “sterile inflammation” (83) and possible mechanisms are: inflammatory processes as non-specific mechanisms of host defense against danger signals of non-microbial origin, extra-amniotic infection, non-viable microorganisms which may release chemotactic factors leading to inflammation (81).
Several studies have demonstrated the link between histological chorioamnionitis and various forms of neurodevelopmental impairment such as white matter brain lesions (51–53) and abnormalities in social behavior, complex learning tasks and sensorimotor gating (46–48), neuropsychiatric disorders (45–50), neonatal encephalopathy (21, 23, 26, 28), and intraventricular hemorrhages (22, 51, 55, 56).
It is believed that chorioamnionitis, leading to the activation of the maternal immune system, could trigger a fetal inflammatory response (FIRS) with a release of proinflammatory cytokines (84) and local thrombosis in severely inflamed vessels (85) that could directly impact the immature brain and increase its susceptibility to neurodevelopmental disorders (13, 51, 86–88).
Epigenetic modifications
Finally, placental epigenetic changes are linked to altered neurodevelopment. From this point of view, these modifications consist predominantly in altered DNA methylation and altered mRNA expression (58, 59) and are influenced by clinical pregnancy features and environmental exposure to toxins (60).
These modifications can be caused by maternal stressors, such as hypoxia or malnutrition, which, for example, could impact on the synthesis of glucocorticoids in the placenta (89, 90). Maternal obesity increases the risk of long-term neurological impairment and psychiatric disorders (91–93).
As described by Cirulli, exposure to a poor socioeconomic environment characterized by stress, maternal depression and/or maternal obesity can lead to increased risk for neuropsychiatric diseases, cognitive impairment and Alzheimer’s disease (94)
Confirming this, MARBLES study suggested that pesticide exposure could alter placental DNA methylation more than other factors (35). Also, vitamin D deficiency (DVD) can contribute to placental cytokine response and neurobehavioral outcomes: indeed, higher concentrations of 25(OH)D during pregnancy were associated with a decreased probability of autistic phenotypes (95).
Glucocorticoids (GCs) and neurotrophins have important effects on brain plasticity (94).
In perspective, another key placental hormone in shaping the fetal brain might be placenta allopregnanolone (ALLO), a major GABAergic neurosteroid, synthesized from progesterone. It was demonstrated that ALLO is a potent regulator in many neurodevelopmental processes, including neurogenesis, neuritogenesis, cell survival, synapse stabilization and myelination (96) and the decrease of its levels leads to increased apoptosis, excitotoxicity and impaired myelination, particularly in males (97). Vacher et al. demonstrated that placental ALLO insufficiency led to cerebellar white matter abnormalities that correlated with autistic-like behavior only in male offspring (39) using a new conditional mouse model, in which the gene encoding ALLO’s synthetic enzyme (akr1c14) is specifically deleted in trophoblasts. A single injection of ALLO during late gestation abolished these alterations (39).
Nevertheless, the relation between placental lesions and short-term neurological injuries (like white matter diseases and intraventricular hemorrhage) in preterm infants has been widely studied, as we see also in this case the causal mechanism remains largely unknown.
Furthermore, Roescher et al. (33) reported that placental lesions were not associated with adverse neurological motor development during the first two weeks after birth in preterm infants.
On the other hand, it seems that placental pathology strongly correlates with long-term neurological outcomes of cognitive performance, particularly in cases of fetal vascular malperfusion (20). Regarding this, van Vliet et al. in 2012 (25) demonstrated that at 2 years, very preterm infants with placental underperfusion had poorer mental development than very preterm infants with histological chorioamnionitis, while no differences between either group were seen regarding motor development. This hypothesis has been confirmed by Gardella et al. (20). The authors reported that fetal vascular malperfusion is correlated with an increased risk of abnormal infant neurodevelopmental outcomes at 2 years of age even in the absence of brain lesions or neurological abnormalities at discharge (20).
However, placental dysfunction alone almost never is sufficient. Indeed, recent studies support the multifactorial pathogenesis hypothesis and the co-occurence of several risk factors being associated with many neurodevelopmental disorders (98, 99). Among these, preterm birth (especially if spontaneous and not medically indicated) (15, 52, 100–103, 29) and fetal growth restriction (14) are the principal ones, with all their respective risk factors (20, 104, 30, 105, 106). There is, however, also a maternal infectious or maternal inflammatory status involved (15, 107–111): indeed, maternal inflammation and cytokine production, especially interleukin-6, -2, and -17a (IL-6, IL-2, and IL-17a), are strongly linked to neurodevelopmental impairment in offspring (37, 112–114).
Regarding the limitations of our review: first of all this paper is a narrative review and not a systematic analysis due to heterogeneity of the considered placental lesions. In addition, the previous literature data derived from retrospective analyses in which the observational time of neurological development in newborns is different: only in 5 of the selected studies patients underwent at least a 2-year follow-up.
Finally, most studies included in this review were conducted in high-risk populations, such as IUGR and preterm infants. Studies in a low- or moderate risk group, such as term infants, in which the incidence of cerebral palsy is low, may reveal different results.
Conclusion
The histological examination of placental tissue may be useful in particular in the follow-up of preterm and FGR newborns, because, even in the absence of neurological impairment at discharge, the likelihood of intact 2 year survival is lower, especially in those whose placenta presents FVM lesions.
Furthermore, in addition to histopathological analysis, proteomic and epigenetic evaluations of placenta may be fundamental for assessing the impact of injury in neurodevelopment.
We are conscious that more research is necessary regarding the pathophysiological mechanisms leading from placental injury to adverse neurological outcomes, with the aim of identifying other possible intrauterine risk factors and diagnostic biomarkers. This may help to identify a group of pregnancies and neonates at major risk of adverse neonatal outcomes with the aim of monitoring these infants more closely.
Especially interesting is the therapeutic aspect that such knowledge can influence for example the most appropriate use of therapeutic hypothermia in case of acute perinatal asphyxia and neonatal encephalopathy or developing hormone replacement strategies to maintain the normal neurodevelopment and protect the brain from further injury.
Author contributions
ALS and MD wrote the manuscript. BG and AS designed the structure of the manuscript. AS, BG, SC, SO and GF contributed to the literature search. MD, BG, and AS reviewed and revised the initial manuscript and approved the final manuscript as submitted. All authors contributed to the article and approved the submitted version.
Funding
The study is supported by grants of the Italian ministry of health, “ricercar corrente” to the IRCCS Fondazione Policlinico San Matteo, Pavia, Italy.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
2. Bonnin A, Levitt P. Fetal, maternal, and placental sources of serotonin and new implications for developmental programming of the brain. Neuroscience (2011) 197:1–7. doi: 10.1016/j.neuroscience.2011.10.005
3. Robbins JR, Bakardjiev AI. Pathogens and the placental fortress. Curr Opin Microbiol (2012) 15:36–43. doi: 10.1016/j.mib.2011.11.006
4. Barker DJ, Osmond C. Childhood respiratory infection and adult chronic bronchitis in England and Wales. BMJ (Clin. Res Ed.) (1986) 293:1271–5. doi: 10.1136/bmj.293.6557.1271
6. Roescher AM, Timmer A, Erwich JJH, Bos AF. Placental pathology, perinatal death, neonatal outcome, and neurological development: A systematic review. PloS One (2014) 9(2):e89419. doi: 10.1371/journal.pone.0089419
7. Mir IN, Leon R, Chalak LF. placental origins of neonatal diseases: Toward a precision medicine approach. Pediatr Res (2021) 89:377–83. doi: 10.1038/s41390-020-01293-6
8. Redline RW. Placental pathology: A systematic approach with clinical correlations. Placenta (2008) 29(Suppl A):S86–91. doi: 10.1016/j.placenta.2007.09.003
9. Kratimenos P, Penn AA. Placental programming of neuropsychiatric disease. Pediatr Res (2019) 86:157–64. doi: 10.1038/s41390-019-0405-9
10. Green BN, Johnson CD, Adams A. Writing narrative literature reviews for peer-reviewed journals: secrets of the trade. J Chiropr. Med (2006) 5:101–17.
11. Gregory AT, Denniss AR. An introduction to writing narrative and systematic reviews - tasks, tips and traps for aspiring authors. Heart. Lung Circ (2018) 27:893–8. doi: 10.1016/j.hlc.2018.03.027
12. Redline RW. Placental pathology: Pathways leading to or associated with perinatal brain injury in experimental neurology, special issue: Placental mediated mechanism of perinatal brain injury. Exp Neurol (2022) 347:113917. doi: 10.1016/j.expneurol.2021.113917
13. Redline RW. Severe fetal placental vascular lesions in term infants with neurologic impairment. Am J Obstet. Gynecol. (2005) 192:452–7.
14. Redline RW, Minich N, Taylor HG, Hack M. Placental lesions as predictors of cerebral palsy and abnormal neurocognitive function at school age in extremely low birth weight infants (<1 kg). Pediatr Dev Pathol (2007) 10:282–92. doi: 10.2350/06-12-0203.1
15. Straughen JK, Misra DP, Divine G, Shah R, Perez G, VanHorn S, et al. The association between placental histopathology and autism spectrum disorder. Placenta (2017) 57:183–8. doi: 10.1016/j.placenta.2017.07.006
16. Ueda M, Tsuchiya KJ, Yaguchi C, Futura-Isomura N, Horikoshi Y, Matsumoto M, et al. Placental pathology predicts infantile neurodevelopment. Sci Rep (2022) 12:2578. doi: 10.1038/s41598-022-06300-w
17. McDonald DG, Kelehan P, McMenamin JB, Gorman WA, Madden D, Tobbia IN, et al. Placental fetal thrombotic vasculopathy is associated with neonatal encephalopathy. Hum Pathol (2004) 35:875–80. doi: 10.1016/j.humpath.2004.02.014
18. Vik T, Redline R, Nelson KB, Bjellmo S, Vogt C, Ng P, et al. The placenta in neonatal encephalopathy: A case-control study. J Pediatr (2018) 202:77.e3–85.e3. doi: 10.1016/j.jpeds.2018.06.005
19. Geraldo AF, Parodi A, Bertamino M, Buffelli F, Uccella S, Tortora D, et al. Perinatal arterial ischemic stroke in fetal vascular malperfusion: A case series and literature review. Am J Neuroradiol (2020) 41:2377–83. doi: 10.3174/ajnr.A6857
20. Gardella B, Dominoni M, Caporali C, Cesari S, Fiandrino G, Longo S, et al. Placental features of fetal vascular malperfusion and infant neurodevelopmental outcomes at 2 years of age in severe fetal growth restriction. Am J Obstet. Gynecol. (2021) 225:413.e1–11. doi: 10.1016/j.ajog.2021.03.037
21. Redline RW, O’Riordan MA. Placental lesions associated with cerebral palsy and neurologic impairment following term birth. Arch Pathol Lab Med (2000) 124:1785–91. doi: 10.5858/2000-124-1785-PLAWCP
22. Polam S, Koons A, Anwar M, Shen-Schwarz S, Hegyi T. Effect of chorioamnionitis on neurodevelopmental outcome in preterm infants. Arch Pediatr Adolesc Med (2005) 159:1032–5. doi: 10.1001/archpedi.159.11.1032
23. Wintermark P, Boyd T, Gregas MC, Labrecque M, Hansen A. Placental pathology in asphyxiated newborns meeting the criteria for therapeutic hypothermia. Am J Obstet. Gynecol. (2010) 203:579 e571–e579. doi: 10.1016/j.ajog.2010.08.024
24. Rovira N, Alarcon A, Iriondo M, Ibanez M, Poo P, Cusi V, et al. Impact of histological chorioamnionitis, funisitis and clinical chorioamnionitis on neurodevelopmental outcome of preterm infants, Early Hum. Dev. (2011) 87(4):253–7.
25. Van Vliet EO, de Kieviet JF, van der Voorn JP, Been JV, Oosterlaan J, van Elburg RM. Placental pathology and long-term neurodevelopment of very preterm infants. Am J Obstet. Gynecol. (2012) 206(6):489 e1–7. doi: 10.1016/j.ajog.2012.03.024
26. Hayes BC, Cooley S, Donnelly J, Doherty E, Grehan A, Madigan C, et al. The placenta in infants >36 weeks gestation with neonatal encephalopathy: A case control study. Arch Dis Child Fetal Neonatal Ed (2013) 98:F233–239. doi: 10.1136/archdischild-2012-301992
27. Lachapelle J, Chen M, Oskoui M, Ali N, Brown R, Wintermark P. Placental pathology in asphyxiated newborns treated with therapeutic hypothermia. J Neonatal. Perinatal. Med (2015) 8:33–40.
28. Mir IN, Johnson-Welch SF, Nelson DB, Brown LS, Rosenfeld CR, Chalak LF. Placental pathology is associated with severity of neonatal encephalopathy and adverse developmental outcomes following hypothermia. Am J Obstet. Gynecol. (2015) 213:849.e1–7. doi: 10.1016/j.ajog.2015.09.072
29. Anblagan D, Pataky R, Evans MJ, Telford EJ, Serag A, Sparrow S, et al. Association between preterm brain injury and exposure to chorioamnionitis during fetal life. Sci Rep (2016) 6:37932. doi: 10.1038/srep37932
30. Raghavan R, Helfrich BB, Cerda SR, Ji Y, Burd I, Wang G, et al. Preterm birth subtypes, placental pathology findings, and risk of neurodevelopmental disabilities during childhood. Placenta (2019) 83:17–25. doi: 10.1016/j.placenta.2019.06.374
31. Elbers J, Viero S, MacGregor D, DeVeber G, Moore AM. Placental pathology in neonatal stroke. Pediatrics (2011) 127:e722–9. doi: 10.1542/peds.2010-1490
32. Harteman JC, Nikkels PGJ, Benders MJNL, Kwee A, Groenendaal F, de Vries LS. Placental pathology in full-term infants with hypoxicischemic neonatal encephalopathy and association with magnetic resonance imaging pattern of brain injury. J Pediatr (2013) 163:968.e2–95.e2. doi: 10.1016/j.jpeds.2013.06.010
33. Roescher AM, Timmer A, Hitzert MM, de Vries NKS, Verhagen EA, Erwich JJHM, et al. Placental pathology and neurological morbidity in preterm infants during the first two weeks after birth. Early Hum Dev (2014) 90(1):21–5. doi: 10.1016/j.earlhumdev.2013.11.004
34. Paquette AG, Lester BM, Lesseur C, Armstrong DA, Guerin DJ, Appleton AA, et al. Placental epigenetic patterning of glucocorticoid response genes is associated with infant neurodevelopment. Epigenomics (2015) 7(5):767–79. doi: 10.2217/epi.15.28
35. Schmidt RJ, Schroeder DI, Crary-Dooley FK, Barkoski JM, Tancredi DJ, Walker CK, et al. Self-reported pregnancy exposures and placental DNA methylation in the MARBLES prospective autism sibling study. Environ Epigenet. (2016) 2(4):dvw024. doi: 10.1093/eep/dvw024
36. Chang JM, Zeng H, Han R, Chang YM, Shah R, Salafia CM, et al. Autism risk classification using placental chorionic surface vascular network features. BMC Med Inform. Decis. Mak. (2017) 17:162.
37. Wu WL, Hsiao EY, Yan Z, MAzmanian SK, PAtterson PH. The placental interleukin-6 signaling controls fetal brain development and behavior. Brain Behav Immun (2017) 62:11–23. doi: 10.1016/j.bbi.2016.11.007
38. Park BY, Misra DP, Moye J, Miller RK, Croen L, Fallin MD, et al. National Children’s Study Consortium. Placental gross shape differences in a high autism risk cohort and the general population. PloS One (2018) 13:e0191276.
39. Vacher CM, Lacaille H, O’Reilly JJ, Salzbank J, Bakalar D, Sebaoui S, et al. Placental endocrine function shapes cerebellar development and social behavior. Nat Neurosci (2021) 24(10):1392–401. doi: 10.1038/s41593-021-00896-4
40. Conti N, Torricelli M, Voltolini C, Vannuccini S, Clifton VL, Bloise E, et al. Term histologic chorioamnionitis: A heterogeneous condition, Eur. J Obstet. Gynecol. Reprod Biol (2015) 188:34–8.
41. Nelson KB, Blair E. The placenta and neurologic and psychiatric outcomes in the child: study design matters. Placenta (2011) 32:623–5. doi: 10.1016/j.placenta.2011.06.021
42. VanWijk MJ, Kublickiene K, Boer K, VanBavel E. Vascular function in preeclampsia. Cardiovasc Res (2000) 47:38–48. doi: 10.1016/S0008-6363(00)00087-0
43. Roy B, Arbuckle S, Walker K, Morgan C, Galea C, Badawi N, et al. The role of the placenta in perinatal stroke: A systematic review. J Child Neurol (2020) 35:773–83. doi: 10.1177/0883073820929214
44. Spinillo A, Gardella B, Adamo L, Muscettola G, Fiandrino G, Cesari S. Pathologic placental lesions in early and late fetal growth restriction. Acta Obstet Gynecol Scand (2019) 98:1585–94. doi: 10.1111/aogs.13699
45. Faa G, Manchia M, Pintus R, Gerosa C, Marcialis MA, Fanos V. Fetal programming of neuropsychiatric disorders. Birth Defects Res C (2016) 108:207–23. doi: 10.1002/bdrc.21139
46. Patterson PH. Immune involvement in schizophrenia and autism: Etiology, pathology and animal models. Behav Brain Res (2009) 204:313–21. doi: 10.1016/j.bbr.2008.12.016
47. Wolff AR, Bilkey DK. The maternal immune activation (MIA) model of schizophrenia produces pre-pulse inhibition (PPI) deficits in both juvenile and adult rats but these effects are not associated with maternal weight loss Behav. Brain Res (2010) 213:323–7. doi: 10.1016/j.bbr.2010.05.008
48. Ozawa K, Hashimoto K, Kishimoto T, Shimizu E, Ishikura H, Iyo M. Immune activation during pregnancy in mice leads to dopaminergic hyperfunction and cognitive impairment in the offspring: A neurodevelopmental animal model of schizophrenia. Biol Psychiatry (2006) 59:546–54. doi: 10.1016/j.biopsych.2005.07.031
49. Brown AS. Epidemiologic studies of exposure to prenatal infection and risk of schizophrenia and autism. Dev Neurobiol (2012) 72:1272–6. doi: 10.1002/dneu.22024
50. Careaga M, Murai T, Bauman MD. Maternal immune activation and autism spectrum disorder: From rodents to nonhuman and human primates. Biol Psychiatry (2017) 81:391–401. doi: 10.1016/j.biopsych.2016.10.020
51. Wu YW, Colford JM Jr.. Chorioamnionitis as a risk factor for cerebral palsy: A meta-analysis. JAMA (2000) 284:1417–24. doi: 10.1001/jama.284.11.1417
52. Malaeb S, Dammann O. Fetal inflammatory response and brain injury in the preterm newborn. J Child Neurol (2009) 24:1119–26. doi: 10.1177/0883073809338066
53. Soucy-Giguere L, Gasse C, Giguere Y, Demers S, Bujold E, Boutin A. Intra-amniotic inflammation and child neurodevelopment: A systematic review protocol. Syst Rev (2018) 7(1):12. doi: 10.1186/s13643-018-0683-z
54. Ogunyemi D, Murillo M, Jackson U, Hunter N, Alperson B. The relationship between placental histopathology findings and perinatal outcome in preterm infants. J Matern Fetal Neonatal Med (2003) 13:102–9. doi: 10.1080/jmf.13.2.102.109
55. Mehta R, Nanjundaswamy S, Shen-Schwarz S, Petrova A. Neonatal morbidity and placental pathology. Indian J Pediatr (2006) 73:25–8. doi: 10.1007/BF02758255
56. Beaudet L, Karuri S, Lau J, Magee F, Lee SK, von Dadelszen P. Placental pathology and clinical outcomes in a cohort of infants admitted to a neonatal intensive care unit. J Obstet Gynaecol Can (2007) 29:315–23. doi: 10.1016/S1701-2163(16)32431-8
57. Newschaffer CJ, Croen LA, Fallin MD, Hertz-Picciotto I, Nguyen DV, Lee NL, et al. Infant siblings and the investigation of autism risk factors. J Neurodev Disord (2012) 4:1–16. doi: 10.1186/1866-1955-4-7
58. Gomez-Roig MD, Mazarico E, Cardenas D, Fernandez MT, Diaz M, Ruiz de Gauna B, et al. Placental 11B-hydroxysteroid dehydrogenase type 2 mRNA levels in intrauterine growth restriction versus small-for-gestational-age fetuses. Fetal Diagn. Ther (2016) 39:147–51.
59. Brosens I, Pijenenborg R, Vercruysse L, Romero R. The “Great Obstetrical Syndromes” are associated with disorders of deep placentation. Am J Obstet. Gynecol. (2011) 204:193–201.
60. Davis EP, Waffarn F, Sandman CA. Prenatal treatment with glucocorticoids sensitizes the HPA axis response to stress among full-term infants. Dev Psychobiol (2011) 53:175–83. doi: 10.1002/dev.20510
61. Rosenfeld CS. The Placenta-Brain-Axis. J Neurosci Res (2021) 99(1):271–83. doi: 10.1002/jnr.24603
62. Redline RW. Inflammatory responses in the placenta and umbilical cord. Semin Fetal Neonatal Med (2006) 11:296–301. doi: 10.1016/j.siny.2006.02.011
63. Redline RW, Ravishankar S. Fetal vascular malperfusion, an update. APMIS (2018) 126:561–9. doi: 10.1111/apm.12849
64. Peng CC, Chang JH, Lin HY, Cheng PJ, Su BH. Intrauterine inflammation, infection, or both (Triple I): A new concept for chorioamnionitis, Pediatr. Neonatol. (2018) 59(3):231–7. doi: 10.1016/j.pedneo.2017.09.001
65. Lee J, Kim JS, Park JW, Park CW, Park JS, Jun JK, et al. Chronic chorioamnionitis is the most common placental lesion in late preterm birth. Placenta (2013) 34(8):681–9. doi: 10.1016/j.placenta.2013.04.014
66. Scifres CM, Parks WT, Feghali M, Caritis SN, Catov JM. Placental maternal vascular malperfusion and adverse pregnancy outcomes in gestational diabetes mellitus. Placenta (2017) 49:10–5. doi: 10.1016/j.placenta.2016.11.004
67. Redline RW, Ravidhankar S. Fetal vascular malperfusion, an update. APMIS (2018) 126:561–9. doi: 10.1111/apm.12849
68. Heider A. Fetal vascular malperfusion. Arch Pathol Lab Med (2017) 141:1484–9. doi: 10.5858/arpa.2017-0212-RA
69. Cheong JLY, Cowan FM. Neonatal arterial ischaemic stroke: obstetric issues. Semin Fetal Neonatal Med (2009) 14:267–71. doi: 10.1016/j.siny.2009.07.009
70. Chabrier S, Saliba E, Nguyen The Tich S, Charollais A, Varlet MN, Tardy B, et al. Obstetrical and neonatal characteristics vary with birthweight in a cohort of 100 term newborns with symptomatic arterial ischemic stroke. Eur J Paediatr Neurol (2010) 14:206–13. doi: 10.1016/j.ejpn.2009.05.004
71. Bernson-Leung ME, Boyd TK, Meserve EE, Danehy AR, Kapur K, Trenor 3CC, et al. Placental pathology in neonatal stroke: A retrospective case-control study. J Pediatr (2018) 195:39–47.e5. doi: 10.1016/j.jpeds.2017.11.061
72. Prandoni P. Venous and arterial thrombosis: Is there a link? Adv Exp Med Biol (2017) 906:273–83. doi: 10.1007/5584_2016_121
73. Chisholm KM, Heerema-McKenney A. Fetal thrombotic vasculopathy. Am J Surg Pathol (2015) 39:274–80. doi: 10.1097/PAS.0000000000000334
74. Ernst LM. Maternal vascular malperfusion of the placental bed. APMIS (2018) 126:551–60. doi: 10.1111/apm.12833
75. Roberts DJ, Post MD. The placenta in pre-eclampsia and intrauterine growth restriction. J Clin Pathol (2008) 61:1254. doi: 10.1136/jcp.2008.055236
76. Burton GJ. Oxygen, the Janus gas; its effects on human placental development and function. J Anat (2009) 215:27. doi: 10.1111/j.1469-7580.2008.00978.x
77. Redline RW, Faye-Petersen O, Heller D, Qureshi F, Savell V, Vogler C. Amniotic infection syndrome: Nosology and reproducibility of placental reaction patterns. Pediatr Dev Pathol (2003) 6(5):435–48. doi: 10.1007/s10024-003-7070-y
78. Romero R, Salafia CM, Athanassiadis AP, Hanaoka S, Mazor M, Sepulveda W, et al. The relationship between acute inflammatory lesions of the preterm placenta and amniotic fluid microbiology. Am J Obstet Gynecol. (1992) 166(5):1382–8. doi: 10.1016/0002-9378(92)91609-E
79. Benedetti TJ, Valle R, Ledger WJ. Antepartum pneumonia in pregnancy. Am J Obstet Gynecol. (1982) 144(4):413–7. doi: 10.1016/0002-9378(82)90246-0
80. Kaul AK, Khan S, Martens MG, Crosson JT, Lupo VR, Kaul R. Experimental gestational pyelonephritis induces preterm births and low birth weights in C3H/HeJ mice. Infect Immun (1999) 67(11):5958–66. doi: 10.1128/IAI.67.11.5958-5966.1999
81. Kim CJ, Romero R, Chaemsaithong P, Chaiyasit N, Yoon BH, Kim YM. Acute chorioamnionitis and funisitis: Definition, pathologic features, and clinical significance. Am J Obstet Gynecol (2015) 213(4 Suppl):S29–52. doi: 10.1016/j.ajog.2015.08.040
82. Galask RP, Varner MW, Petzold CR, Wilbur SL. Bacterial attachment to the chorioamniotic membranes. Am J Obstet Gynecol. (1984) 148(7):915–28. doi: 10.1016/0002-9378(84)90534-9
83. Romero R, Miranda J, Chaiworapongsa T, Korzeniewski SJ, Chaemsaithong P, Gotsch F, et al. Prevalence and clinical significance of sterile intra-amniotic inflammation in patients with preterm labor and intact membranes. Am J Reprod Immunol (2014) 72(5):458–74. doi: 10.1111/aji.12296
84. Dammann O, Phillips TM, Allred EN, O’Shea TM, Paneth N, Van Marter LJ, et al. ELGAN STUDY INVESTIGATORS. Mediators of fetal inflammation in extremely low gestational age newborns. Cytokine (2001) 13:234–9. doi: 10.1006/cyto.2000.0820
85. Redline RW, Wilson-Costello D, Borawski E, Fanaroff AA, Hack M. Placental lesions associated with neurologic impairment and cerebral palsy in very low birth weight infants. Arch Pathol Lab Med (1998) 122:1091–8.
86. Chau V, McFadden DE, Poskitt KJ, Miller SP. Chorioamnionitis in the pathogenesis of brain injury in preterm infants. Clin perinatol. (2014) 41(1):83–103. doi: 10.1016/j.clp.2013.10.009
87. Burd I, Balakrishnan B, Kannan S. Models of fetal brain injury, intrauterine inflammation, and preterm birth. Am J Reprod Immunol (2012) 67(4):287–94. doi: 10.1111/j.1600-0897.2012.01110.x
88. Dammann O, Kuban KC, Leviton A. Perinatal infection, fetal inflammatory response, white matter damage, and cognitive limitations in children born preterm,Ment. Retard Dev Disabil. Res Rev (2002) 8(1):46–50. doi: 10.1002/mrdd.10005
89. Adelman DM, Gertsenstein M, Nagy A, Simon MC, Maltepe E. Placental cell fates are regulated in vivo by HIF-mediated hypoxia responses. Genes Dev (2000) 14:3191–203. doi: 10.1101/gad.853700a
90. Gheorghe CP, Goyal R, Mittal A, Longo LD. Gene expression in the placenta: maternal stress and epigenetic responses. Int J Dev Biol (2012) 54:507–23. doi: 10.1387/ijdb.082770cg
91. Buss C, Entringer S, Davis EP, Hobel CJ, Swanson JM, Wadhwa PD, et al. Impaired executive function mediates the association between maternal pre-pregnancy body mass index and child ADHD symptoms. PloS One (2012) 7:e37758. doi: 10.1371/journal.pone.0037758
92. Hinkle SN, Schieve LA, Stein AD, Swan DW, Ramakrishnan U, Sharma AJ. Associations between maternal prepregnancy body mass index and child neurodevelopment at 2 years of age. Int J Obes (2012) 36:1312–9. doi: 10.1038/ijo.2012.143
93. Cirulli F, Musillo C, Berry A. Maternal obesity as a risk factor for brain development and mental health in the offspring. Neuroscience (2020) 1:447:122–135. doi: 10.1016/j.neuroscience.2020.01.023
94. Cirulli F. Interactions between early life stress and metabolic stress in programming of mental and metabolic health. Behav Sci (2017) 14:65–71. doi: 10.1016/j.cobeha.2016.12.009
95. Garcia-Serna AM, Morales E. Neurodevelopmental effects of prenatal vitamin D in humans: Systematic review and meta-analysis. Mol Psychiatry (2020) 25(10):2468–81. doi: 10.1038/s41380-019-0357-9
96. Schumacher M, Mattern C, Ghoumari A, Oudinet JP, Liere P, Labombarda F, et al. Revisiting the roles of progesterone and allopregnanolone in the nervous system: Resurgence of the progesterone receptors. Prog Neurobiol (2014) 113:6–39. doi: 10.1016/j.pneurobio.2013.09.004
97. Brunton PJ, Russell JA, Hirst JJ. Allopregnanolone in the brain: Protecting pregnancy and birth outcomes. Prog Neurobiol (2014) 113:106–36. doi: 10.1016/j.pneurobio.2013.08.005
98. Craig F, Lamanna AL, Margari F, Matera E, Simone M, Margari L. Overlap between autism spectrum disorders and attention deficit hyperactivity disorder: Searching for distinctive/common clinical features. Autism Res (2015) 8(3):328–37. doi: 10.1002/aur.1449
99. Brucato M, Ladd-Acosta C, Li M, Caruso D, Hong X, Kaczaniuk J, et al. Prenatal exposure to fever is associated with autism spectrum disorder in the boston birth cohort. Autism Res (2017) 10(11):1878–90. doi: 10.1002/aur.1841
100. Goldenberg RL, Culhane JF, Iams JD, Romero R. Epidemiology and causes of preterm birth. Lancet (2008) 371:75–84. doi: 10.1016/S0140-6736(08)60074-4
101. Nadeau HC, Subramaniam A, Andrews WW. Infection and preterm birth. Semin Fetal Neonatal Med (2016) 21:100–5. doi: 10.1016/j.siny.2015.12.008
102. Wu HC, Shen CM, Wu YY, Yuh YS, Kua KE. Subclinical histologic chorioamnionitis and related clinical and laboratory parameters in preterm deliveries. Pediatr Neonatol. (2009) 50:217–21. doi: 10.1016/S1875-9572(09)60066-8
103. Leviton A, Joseph RM, Allred EN, Fichorova RN, O’Shea TM, Kuban KKC, et al. The risk of neurodevelopmental disorders at age 10years associated with blood concentrations of interleukins 4 and 10 during the first postnatal month of children born extremely preterm. Cytokine (2018) 110:181–8. doi: 10.1016/j.cyto.2018.05.004
104. Roescher AM, Hitzert MM, Timmer A, Verhagen EA, Erwich JJ, Bos AF. Placental pathology is associated with illness severity in preterm infants in the first twenty-four hours after birth. Early Hum Dev (2011) 87(4):315–9. doi: 10.1016/j.earlhumdev.2011.01.040
105. Galinsky R, Polglase GR, Hooper SB, Black MJ, Moss TJ. The consequences of chorioamnionitis: Preterm birth and effects on development. J Pregnancy (2013) 2013:412831. doi: 10.1155/2013/412831
106. Hodyl NA, Aboustate N, Bianco-Miotto T, Roberts CT, Clifton VL, Stark MJ. Child neurodevelopmental outcomes following preterm and term birth: What can the placenta tell us? Placenta (2017) 57:79–86. doi: 10.1016/j.placenta.2017.06.009
107. Hack M, Taylor HG, Schluchter M, Andreias L, Drotar D, Klein N. Behavioral outcomes of extremely low birth weight children at age 8 years. J Dev Behav Pediatr (2009) 30:122–30. doi: 10.1097/DBP.0b013e31819e6a16
108. Johnson S, Hollis C, Kochhar P, Hennessy E, Wolke D, Marlow N. Autism spectrum disorders in extremely preterm children. J Pediatr (2010) 156:525–31 e2. doi: 10.1016/j.jpeds.2009.10.041
109. Pinto-Martin JA, Levy SE, Feldman JF, Lorenz JM, Paneth N, Whitaker AH. Prevalence of autism spectrum disorder in adolescents born weighing <2000 grams. Pediatrics (2011) 128:883–91. doi: 10.1542/peds.2010-2846
110. Treyvaud K, Ure A, Doyle LW, Lee KJ, Rogers CE, Kidokoro H, et al. Psychiatric outcomes at age seven for very preterm children: Rates and predictors. J Child Psychol Psychiatry (2013) 54:772–9. doi: 10.1111/jcpp.12040
111. Joseph RM, O’Shea TM, Allred EN, Heeren T, Hirtz D, Paneth N, et al. Prevalence and associated features of autism spectrum disorder in extremely low gestational age newborns at age 10 years. Autism Res (2017) 10:224–32. doi: 10.1002/aur.1644
112. Bilbo SD, Block CL, Bolton JL, Hanamsagar R, Tran PK. Beyond infection—maternal immune activation by environmental factors, microglial development, and relevance for autism spectrum disorders. Exp Neurol (2018) 299:241–51. doi: 10.1016/j.expneurol.2017.07.002
113. Wong H, Hoeffer C. Maternal IL-17A in autism. Exp Neurol (2018) 299:228–40. doi: 10.1016/j.expneurol.2017.04.010
Keywords: neuroplacentology, placental pathology and neurological outcome, neurological morbidity, placental epigenetic and neurodevelopment, cerebral palsy
Citation: Gardella B, Dominoni M, Scatigno AL, Cesari S, Fiandrino G, Orcesi S and Spinillo A (2022) What is known about neuroplacentology in fetal growth restriction and in preterm infants: A narrative review of literature. Front. Endocrinol. 13:936171. doi: 10.3389/fendo.2022.936171
Received: 04 May 2022; Accepted: 11 July 2022;
Published: 19 August 2022.
Edited by:
Imran N. Mir, University of Texas Southwestern Medical Center, United StatesReviewed by:
Valerio Gaetano Vellone, University of Genoa, ItalyKaela Margaret Varberg, University of Kansas Medical Center, United States
Rachel Leon, University of Texas Southwestern Medical Center, United States
Copyright © 2022 Gardella, Dominoni, Scatigno, Cesari, Fiandrino, Orcesi and Spinillo. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Barbara Gardella, YmFyYmFyYS5nYXJkZWxsYUBnbWFpbC5jb20=
 Barbara Gardella
Barbara Gardella Mattia Dominoni
Mattia Dominoni Annachiara Licia Scatigno
Annachiara Licia Scatigno Stefania Cesari3
Stefania Cesari3