
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Endocrinol., 18 August 2022
Sec. Adrenal Endocrinology
Volume 13 - 2022 | https://doi.org/10.3389/fendo.2022.925591
Background: Unilateral adrenalectomy is the mainstay treatment for unilateral primary aldosteronism (PA). This meta-analysis aimed to systematically analyse predictors of clinical success after unilateral adrenalectomy in PA.
Methods: A search was performed using PubMed/Medline, Scopus, Embase and Web of Science from their inception to February 2022. Observational studies in adult PA patients which reported predictors of clinical success after unilateral adrenalectomy were included. A random-effects model was employed to pool the fully adjusted odds ratio (OR) or standardized mean difference (SMD) with 95% confidence interval (95% CI).
Results: Thirty-two studies involving 5,601 patients were included. Females had a higher clinical success rate (OR 2.81; 95% CI 2.06–3.83). Older patients, patients with a longer duration of hypertension and those taking a higher number of antihypertensive medications had lower clinical success rates (OR 0.97; 95% CI 0.94–0.99, OR 0.92; 95% CI 0.88–0.96 and OR 0.44; 95% CI 0.29–0.67, respectively). Compared to non-clinical success cases, patients with clinical success had a lower body mass index (SMD -0.49 kg/m2; 95% CI -0.58,-0.39), lower systolic (SMD -0.37 mmHg; 95% CI -0.56,-0.18) and diastolic blood pressure (SMD -0.19 mmHg; 95% CI -0.33,-0.06), lower serum potassium (SMD -0.16 mEq/L; 95% CI -0.28,-0.04), higher eGFR (SMD 0.51 mL/min/1.73m2; 95% CI 0.16,0.87), a lower incidence of dyslipidemia (OR 0.29; 95% CI 0.15–0.58) and a lower incidence of diabetes mellitus (OR 0.36; 95% CI 0.22–0.59).
Conclusions: Multiple predictors of clinical success after unilateral adrenalectomy in PA were identified which can help improve the quality of care for PA patients.
Systematic Review Registration: INPLASY, identifier 202240129.
Primary aldosteronism (PA) is the most common cause of endocrine hypertension with a prevalence of 60% in resistant hypertension patients (1). An increased risk of cardiovascular and cerebrovascular diseases was observed in PA patients compared to essential hypertension patients (2). The goal of PA treatment includes blood pressure control, normalized serum potassium level without potassium supplements and prevention of further cardiovascular and renal complications. Currently, there are two therapeutic approaches for PA: unilateral adrenalectomy for unilateral disease and targeted medical therapy for bilateral disease (3). Surgical management by unilateral adrenalectomy in PA can reduce cardiovascular risk, improve quality of life and has the long-term advantage of greater cost-saving over life-long medical therapy (4–6). The clinical cure rate in PA after adrenal venous sampling (AVS)-guided adrenalectomy was significantly higher than in non-AVS-guided adrenalectomy (40% versus 30.5%, p=0.027) (7). Whether the operation was AVS-guided or not, the clinical cure rate was approximately 27.1% (8).
There are multiple predictive factors related to clinical success after adrenalectomy in PA. In AVS-guided adrenalectomy, duration of hypertension, gender, antihypertensive medication dosage, body mass index, target organ damage, and size of the largest nodule at imaging can help predict the clinical success after surgery in PA (9). Another study showed that gender, body mass index, duration of hypertension, creatinine levels, and number of antihypertensive medications could facilitate the prediction of clinical success after adrenalectomy (10). Different definitions of clinical cure in PA were used in each of the studies, e.g., the primary aldosteronism surgical outcome criteria (PASO) and other criteria such as normotension without the help of antihypertensive medications (11, 12). Moreover, studies comparing AVS-guided and non-AVS-guided surgery used diverse measures to diagnose unilateral PA. As AVS may play a major role in the clinical success rate after adrenalectomy, this diversity could affect clinical outcomes.
Reports of multiple predictors of clinical success after adrenalectomy in PA have been published. However, those results remain unclear and inconsistent, with varying quality across the studies. The present systematic review and meta-analysis aimed to clarify predictors of clinical success after unilateral adrenalectomy. In addition, subgroup analysis of patients with AVS-guided surgery and those without AVS-guided surgery was also conducted.
The reporting in this study followed the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) guidelines (13). The pre-defined protocol was registered in INPLASY 202240129. A comprehensive search of four databases, PubMed/Medline, Scopus, Embase and Web of Science, was performed from their inception to February 2022. The keywords included were “hyperaldosteronism OR primary aldosteronism OR primary hyperaldosteronism OR aldosteronism” AND ”adrenalectomy OR surgical OR surgery OR unilateral adrenalectomy” AND ”patient outcome assessment OR clinical outcome OR outcome OR predictor OR predictive factor”. Medical subject heading (MeSH) terms were employed in the PubMed/Medline search. Details of the search strategy are presented in the Supplementary Appendix. Manual searches were conducted to identify references from the included studies, other relevant publications, and non-included reviews, and these were included as additional studies for the initial screening. Rayyan, a web-based program (Rayyan Systems Inc., Cambridge, MA, USA) (14), was employed for duplicate removal and initial screening of abstracts and titles.
Two authors (WM, PA) independently conducted the searches, screened for titles and abstracts. Pertinent studies were retrieved and underwent full-text screening for inclusion criteria. Then the two authors independently evaluated the methodological quality of the included studies and conducted the data extraction. The third author (PI) together with the first two authors (WM, PA) discussed and reached a consensus in cases of disagreement during the article search and selection processes.
Inclusion criteria for articles were as follows: 1) observational (non-randomized) studies that included adult PA patients; 2) studies that reported either predictive factors of complete clinical success versus partial success plus no clinical success as well as those that reported predictive factors for complete plus partial clinical success versus no clinical success after unilateral adrenalectomy. The predictive factors could be reported as either adjusted or unadjusted odds ratio (OR) or as crude data; 3) studies that reported the number of patients with both complete clinical success and those with partial or no clinical success after unilateral adrenalectomy; 4) standard diagnostic and/or confirmation criteria was employed to diagnose and confirm PA (15), 5) the definitions of clinical success or non-success should be clearly specified in the articles, and 6) the studies should provide adequate information in accordance with the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement (16). As various definitions of clinical success were used among the studies, three categories of clinical success (complete, partial and no clinical success) were grouped. Complete clinical success was defined as normal blood pressure without the use of anti-hypertensive medications. Partial clinical success was defined as less anti-hypertensive medications or a reduction in blood pressure with either the same amount or less of anti-hypertensive medications used. No clinical success was defined as unchanged blood pressure with the same amount of anti-hypertensive medications used.
In cases of duplicate studies of the same patient population, the study reporting higher number of participants was selected as the main data source. Exclusion criteria were articles published in a language other than English, review articles, case reports, grey literature, editorial comments, conference abstracts and animal studies. Studies involving special populations such as pregnant women or children were also excluded.
Data extraction was independently conducted by two authors (WM, PA). The variables extracted from each study included: 1) study characteristics, i.e., the name of the first author, year of publication, ethnicity of the included population and study design; 2) patient characteristics, i.e., means and standard deviations (SD) of age, percentage of males, mean and SD of body mass index (BMI), percentage of AVS, mean and SD of duration of hypertension, mean and SD of number of anti-hypertensive medications used, mean and SD of defined daily dose (DDD) and mean and SD of duration of follow-up; and 3) criteria of clinical success employed in each study; 4) number of patients with complete clinical success versus partial or no clinical success after unilateral adrenalectomy was extracted where available. If that data was not available, the number of patients with complete plus partial clinical success versus no clinical success was extracted and 5) predictive factors of clinical success after unilateral adrenalectomy, including both clinical and laboratory predictors. Adjusted odds ratio, unadjusted odds ratio or crude data for the predictive factors were also collected.
Meta-analysis was performed using the STATA program version 16.0. (StataCorp LLC, College Station, TX, USA). For primary analysis, the adjusted odds ratio of predictive factors of clinical success reported in each study were used to calculate the pooled adjusted OR using a random effects model. For secondary analysis, pooled standardized mean differences (SMD) were calculated for crude continuous data and pooled OR for crude binary data. The predictive factors included in the meta-analysis should have been reported in at least two of the studies. Pooled OR were calculated using the logarithm of effect size and standard error from each study. Random effect modelling by the DerSimonian-Liard method was performed as the observed estimates of effect size can vary across studies due to sampling variability. The statistical significance level for this meta-analysis was set at p<0.05. To evaluate the statistical heterogeneity among the studies, the I2 statistic was assessed. I2 values >75% with a significant Cochran Q test (p<0.05) were considered to indicate high heterogeneity. I2 values of <75% were considered as moderate to high heterogeneity. Publication bias was assessed using funnel plots and Egger’s linear regression tests. Funnel plots should be a symmetrical inverted funnel when there is an absence of publication bias and asymmetrical when there is publication bias. A p-value of <0.05 was considered to indicate statistically significant publication bias for Egger’s regressions. For the predictors which contained publication bias, the effect size and 95% CI by the trim-and-fill method were also used to eliminate publication bias
As there was a difference in clinical success rate among studies which were AVS-guided and those that were non-AVS-guided (7), further subgroup analysis by AVS-guided adrenalectomy was also conducted to determine the effect of potential confounders. The subgroups were studies where all patients had performed AVS before adrenalectomy and studies with only some or none of the patients had undergone AVS before adrenalectomy. The included predictors for subgroup analysis should be reported in at least one study per each subgroup.
The Newcastle-Ottawa scale (NOS) for cohort studies was used to assess risk of bias. The assessment was conducted by two authors independently (WM and PA) and discrepancies were resolved through discussion with the third author (PI). The NOS scale evaluated 3 domains: selection of study groups (4 points), comparability of groups (2 points), and outcomes (3 points) (17). Risk of bias is rated as low if NOS ≥7, moderate if NOS 4-6 and high if NOS ≤3.
A total of 2,503 articles were retrieved from database searches, including 486 from PubMed, 808 from Embase, 957 from Scopus, and 252 from Web of Science. From the retrieved articles, 1,310 duplicates were removed. A screening of titles and abstracts of the remaining 1,193 articles was performed which resulted in the exclusion of 1,118 additional articles which were not relevant to the objectives of this study. The full texts of the remaining 75 articles were retrieved and reviewed, resulting in the exclusion of an additional 43 articles due to a variety of reasons including consisting of editorial comments, conference abstracts, reviews or short communications; not providing outcomes of interest; and using the same cohort as other included studies. Finally, a total of 32 studies were included (9–12, 18–45). The PRISMA selection process used is shown in Figure 1.
Table 1 shows the characteristics of the included studies. All 32 studies included were non-randomized cohort studies. Most of the studies (20 of 32) had been conducted in non-Asian populations. All studies provided data on age, sex and duration of follow-up. However, not all of the included studies provided data on BMI, percentage of AVS performed, number of anti-hypertensive medications, DDD and duration of hypertension. The majority (53%) of the clinical remission criteria used in the studies was Primary Aldosteronism Surgical Outcome (PASO) criteria. Other criteria used for determining clinical remission are as shown in Table 1. Thirteen of the 32 studies were multi-center, of which 3 were multi-continent international studies (9, 11, 12, 26, 31–34, 38, 39, 41, 43, 44). The clinical remission rates ranged from 15 to 82%. Eleven of the studies had performed AVS in all of the patients (9–12, 20, 29, 32, 38, 39, 42, 45). Four studies had compared complete and partial clinical success versus no clinical success (25, 33, 41, 45).
Risk of bias was assessed using NOS for cohort studies (Table 1). Most of the studies (31 of 32) evidenced high quality with a low risk of bias (9–12, 19–45). One study had moderate quality with a moderate risk of bias (18) as the comparable cohort was not adjusted or matched for confounders and had an inadequately short cohort follow-up time. Details of the NOS of the included studies are shown in the Supplementary Table.
A total of 32 studies comprising 5,601 patients were included in this meta-analysis. In the primary analysis, the pooled adjusted odds ratios of 13 predictive factors were determined. The median number of studies reporting these predictive factors with adjusted odds ratios was 6 (range 2–14). In terms of demographics, older patients had a lower clinical success rate after adrenalectomy than younger patients (OR 0.97; 95% CI 0.94–0.99; p=0.01; I2 19.29, Q-test p-value 0.27). Females had a higher rate of clinical success than males (OR 2.81; 95% CI 2.06–3.83; p<0.001; I2 39.65, Q-test p-value 0.007). Patients with higher BMI had a lower clinical success rate than those with a lower BMI (OR 0.86; 95% CI 0.76–0.98; p=0.02; I2 78.78, Q-test p-value <0.001). Corrected OR by trim-and-fill method for BMI showed an OR of 0.94; 95% CI 0.81-1.09. In terms of hypertensive status, a longer duration of hypertension or a higher number of antihypertensive medications used was associated with a lower clinical success rate than a shorter duration of hypertension and lower number of medications used (OR 0.92; 95% CI 0.88–0.96; p<0.001; I2 90.56, Q-test p-value <0.001 and OR 0.44; 95% CI 0.29–0.67; p<0.001; I2 75.20, Q-test p-value <0.001, respectively). The corrected OR by the trim-and-fill method for duration of hypertension was 0.95; 95% CI 0.91-0.99 and for the number of antihypertensive medications was 0.51 (0.33,0.79). Other predictive factors, including DDD, diabetes mellitus, systolic blood pressure, preoperative aldosterone level, serum potassium, presence or absence of target organ damage, eGFR and tumor size, revealed no significant association with clinical success after unilateral adrenalectomy. The primary analysis of adjusted odds ratios are shown in Table 2. The forest plot of the predictors using fully adjusted odds ratios which were significantly associated with clinical success are as shown in Supplementary Figure.
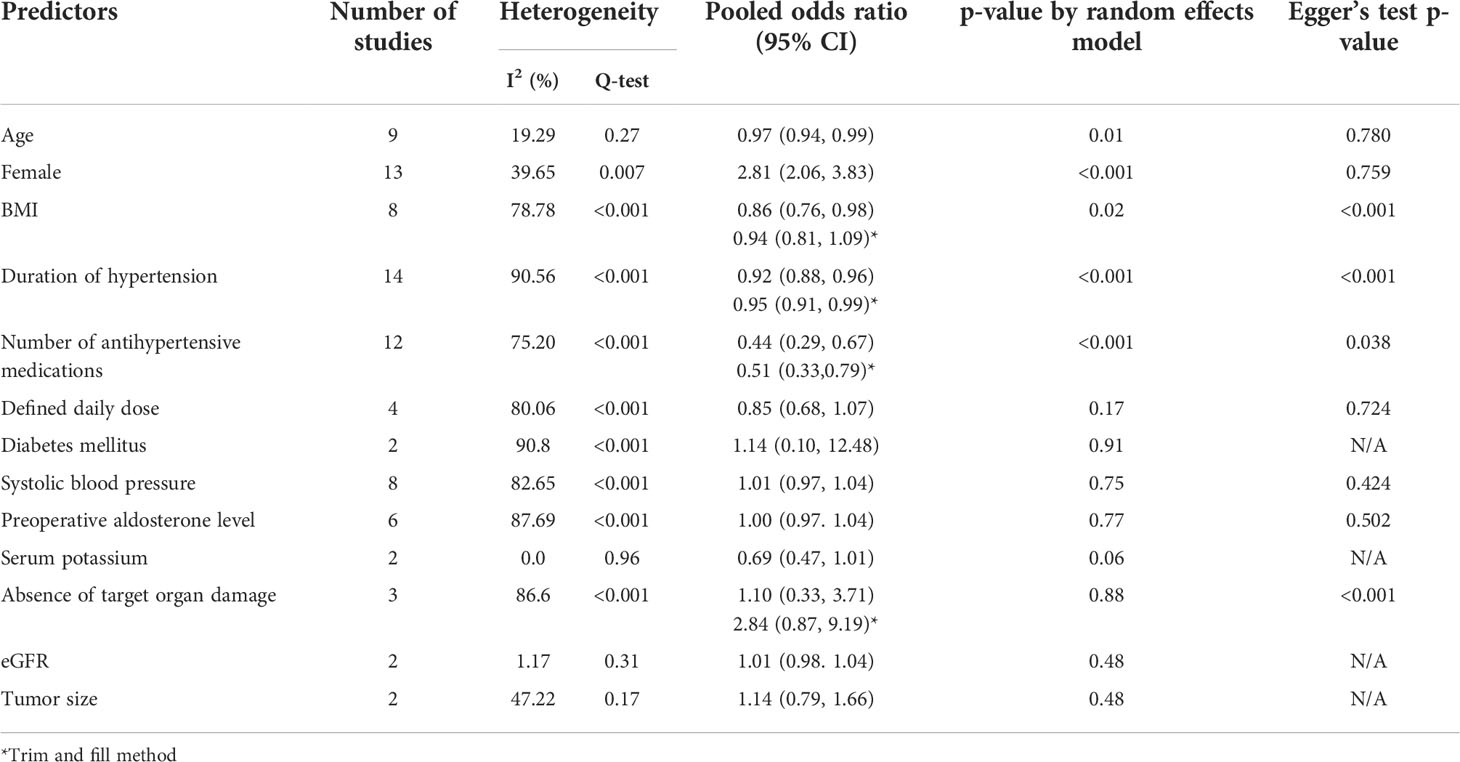
Table 2 Meta-analysis of predictive factors of clinical success after adrenalectomy in primary aldosteronism using fully adjusted odds ratio.
For secondary analysis, crude data of the 19 predictive factors were employed. The median number of studies reporting these predictive factors with crude data was 17 (range 3–23). Among the demographic data, age, sex and BMI were significantly related to clinical success rate. Younger patients had a higher rate of clinical success after adrenalectomy than older patients with an SMD of 0.54 years (95% CI -0.66,-0.42; p<0.001; I2 52.49, Q-test p-value <0.001). Females had a higher clinical success rate than males (OR 2.96; 95% CI 2.21–4.14; p<0.001; I2 73.70, Q-test p-value <0.001). The corrected OR by the trim-and-fill method for females was 2.34; 95% CI 1.68- 3.27. Patients with lower BMI had a higher rate of clinical success with an SMD of 0.49 kg/m2 (95% CI -0.58,-0.39; p<0.001; I2 16.78, Q-test p-value 0.26). Lower blood pressure was observed in patients with clinical success than those without clinical success including systolic blood pressure (SMD -0.37 mmHg (95% CI -0.56,-0.18; p<0.001; I2 81.37, Q-test p-value <0.001) and diastolic blood pressure (SMD -0.19 mmHg (95% CI -0.33,-0.06; p<0.001; I2 59.32, Q-test p-value <0.001). In terms of hypertensive status, shorter duration of hypertension and a lower number of antihypertensive medications used was found in the clinical success patients than the patients without clinical success with SMD of 0.72 years; 95% CI -0.97,-0.46; p<0.001; I2 88.60, Q-test p-value <0.001 and SMD of -0.81 drugs; 95% CI -1.09,-0.54; p<0.001; I2 85.67, Q-test p-value <0.001. Laboratory investigations found serum potassium and eGFR were associated with clinical success rate. In patients with clinical success, lower serum potassium and higher eGFR were observed than in patients without clinical success with SMD of -0.16 mEq/L; 95% CI -0.28,-0.04; p=0.01; I2 42.27, Q-test p-value =0.03 and SMD of 0.51 mL/min/1.73m2; 95% CI 0.16,0.87; p<0.001; I2 71.87, Q-test p-value =0.01, respectively. Other laboratory investigations, including preoperative aldosterone, renin and aldosterone/renin ratio, did not show an association with clinical success. For underlying diseases, the incidence of dyslipidemia and diabetes mellitus were significantly lower in those with clinical success than those without clinical success (OR 0.29; 95% CI 0.15–0.58; p<0.001; I2 56.94, Q-test p-value=0.10 and OR 0.36; 95% CI 0.22–0.59; p<0.001; I2 47.90, Q-test p-value=0.05, respectively). Corrected OR by the trim-and-fill method for diabetes mellitus was 0.56; 95%CI 0.34-0.91. Left ventricular hypertrophy did not demonstrate a link with clinical success. The forest plot of the predictors using crude data which were significantly associated with clinical success are shown in Supplementary Figure.
Subgroup analysis categorized by studies in which all patients had AVS and the studies in which some or an unknown percentage of patients had AVS was conducted. As shown in Table 3, the results of the pooled adjusted odds ratio for predictive factors of clinical success did not change significantly (p-value of group differences >0.05) except for DDD of antihypertensive medications (p-value of group differences=0.03). Significant association of DDD with clinical success was demonstrated only in the studies which performed AVS in some patients or where the AVS status was unknown, while in the studies which performed AVS in all patients DDD was not associated with clinical success. However, the results of heterogeneity for age, female and systolic blood pressure showed significant improvement after subgroup analysis by AVS.
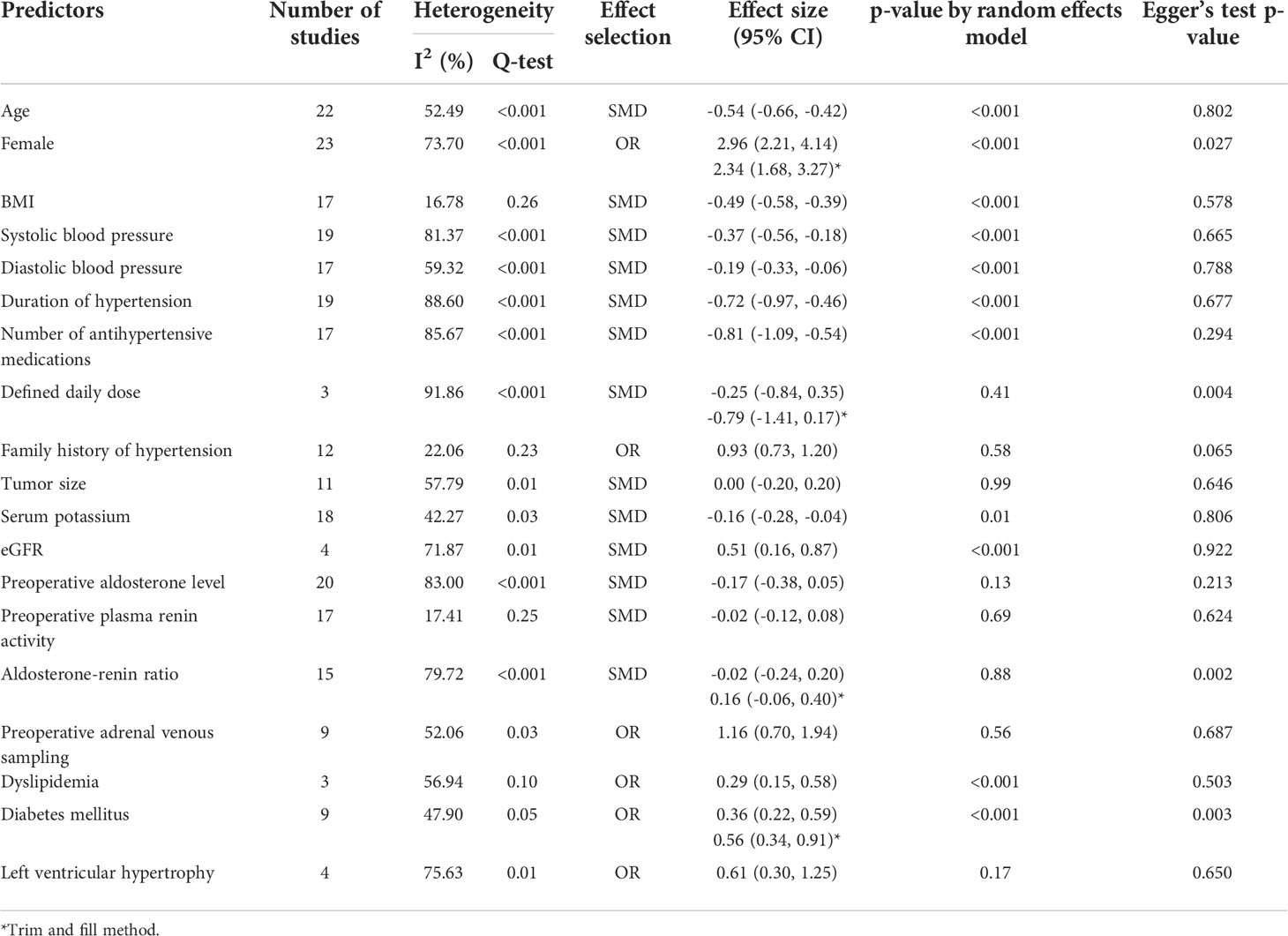
Table 3 Meta-analysis of predictive factors of clinical success after adrenalectomy in primary aldosteronism using crude data.
The results of subgroup analysis by AVS of crude data for predictors of clinical success also did not show significant changes except for serum potassium (p-value of group differences=0.03). Significant association of serum potassium with clinical success was demonstrated only in the studies which performed AVS in some patients or in patients with unknown status, while in studies which performed AVS in all patients, serum potassium was not associated with clinical success. The results of heterogeneity for age, systolic blood pressure, diastolic blood pressure, tumor size, serum potassium, preoperative aldosterone level and left ventricular hypertrophy revealed significant improvement after subgroup analysis by AVS. Data are as shown in Table 4.

Table 4 Subgroup analysis of the predictive factors of clinical success after adrenalectomy in primary aldosteronism by adrenal venous sampling status using fully adjusted odds ratio .
In the primary analysis of the adjusted odds ratio, Egger’s regression test revealed publication bias for BMI, duration of hypertension and number of antihypertensive medications used as well as absence of target organ damage. Among the crude data, predictive factors including being female, DDD, aldosterone-renin ratio and diabetes mellitus showed publication bias. Data are shown in Tables 2 and 5. Funnel plots and funnel plots with the trim-and-fill method for each of the predictive factors are provided in Supplementary Figure.
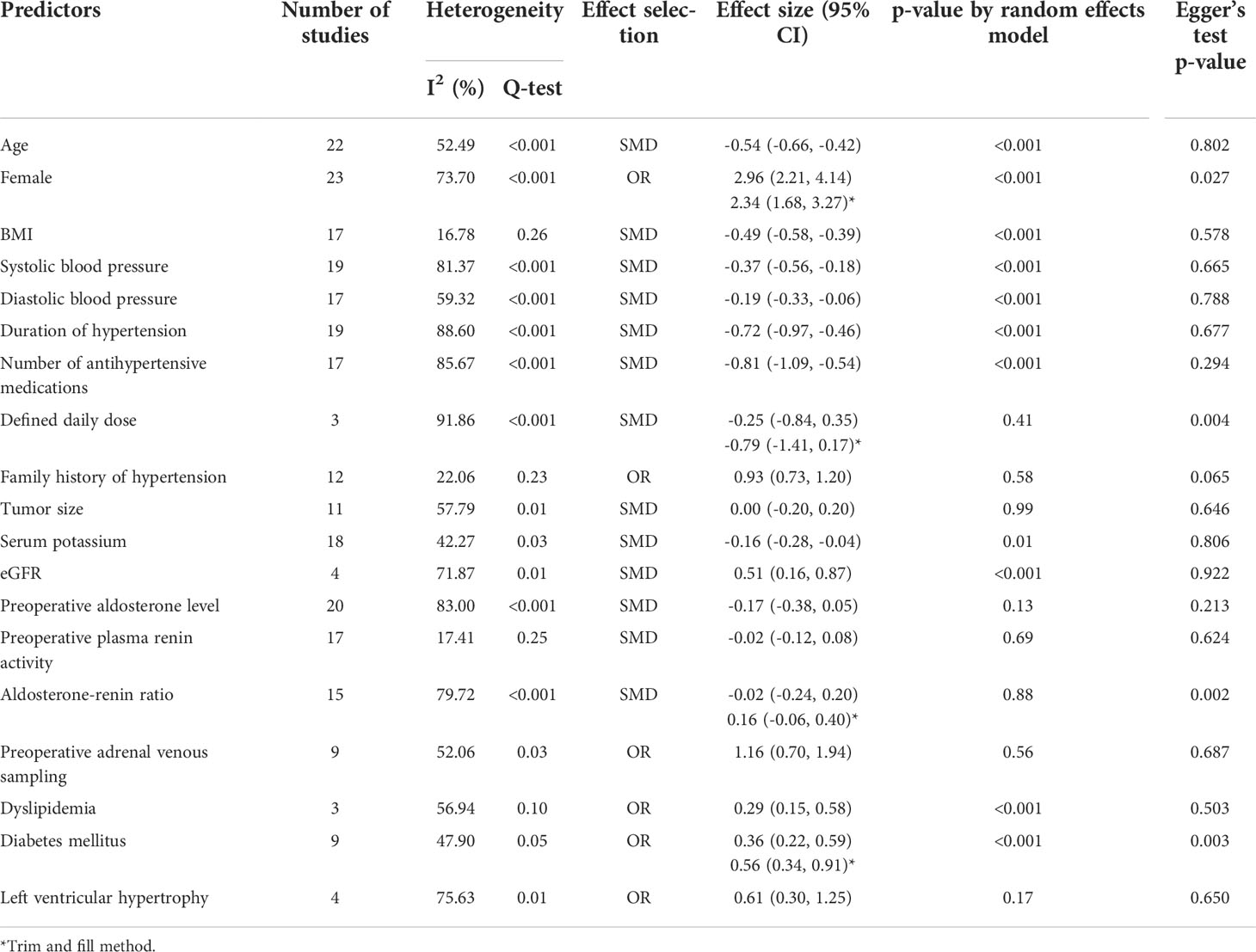
Table 5 Meta-analysis of predictive factors of clinical success after adrenalectomy in primary aldosteronism using crude data.
This systematic review and meta-analysis is the first to describe and quantify the degree of predictive factors associated with clinical success after unilateral adrenalectomy in patients with PA. The present study found that multiple predictive factors are associated with higher rates of clinical success after unilateral adrenalectomy. Based on fully adjusted odds ratios, younger age, being female, a lower BMI, shorter duration of hypertension and lower number of medications used were significantly related to the clinical success rate. Further analysis of the predictors using crude data demonstrated that lower systolic and diastolic blood pressure, lower serum potassium, higher eGFR and the absence of diabetes and dyslipidemia were also associated with a higher incidence of clinical success after adrenalectomy.
Interestingly, younger patients and female patients had better chance of clinical success than older patients and male patients. A previous study showed that mildly decreased renin and aldosterone levels were observed in elderly patients (46), so the levels of aldosterone and renin may not explain this association. A high postoperative incidence of persistent hypertension and hyperkalemia were observed in elderly patients, especially in individuals with long-standing hypertension (47). A probable explanation is that in the elderly essential hypertension is more prevalent than in younger patients, thus leading to persistent hypertension even after unilateral adrenalectomy (48). However, the reason for the association between age and decreased success rate is still unclear and needs further study. The underlying mechanism behind the association between female sex and higher success rates remains unclear. Previous human and animal studies have shown that estrogen may have a protective effect on salt-sensitive hypertension and may possibly also have a vasoprotective effect by suppressing renin-angiotensin-aldosterone system activity (49, 50). Lower BMI tended to be associated with clinical success after adrenalectomy. The physiological factors behind this finding are uncertain. This relationship cannot be explained by a high level of aldosterone as a study showed that BMI has a positive correlation with plasma aldosterone levels in essential hypertension patients but not in PA patients (51). As with older patients, obese patients may have a higher prevalence of essential hypertension, a component of metabolic syndrome which can cause persistent hypertension after definite treatment of PA. A shorter duration of hypertension and a lower number of antihypertensive medications used also predicts a higher success rate. Patients with long-standing hypertension from chronic exposure to aldosterone and who required multiple medications showed an increased chance of vascular remodelling involving increased intima-media thickness and arterial stiffness which can lead to a higher risk of cardiovascular disease, chronic kidney disease and metabolic syndrome (52). These changes in vascular morphology may indicate a lower chance of success even after specific treatment of PA.
From the analysis based on crude data, lower blood pressure, which indicates a lower severity of disease, was significantly associated with a higher chance of success. Vascular remodelling may play a role in this association. A study revealed that in severe hypertension, there is less of a compensatory mechanism to counteract elevated blood pressure, leading subsequently to vascular damage (53). Moreover, higher eGFR, absence of diabetes and dyslipidemia are associated with a higher rate of clinical success. Again, the underpinning explanation of that association could be that increased and irreversible vascular damage can be observed in patients with chronic kidney disease, dyslipidemia and diabetes over and above that caused by hypertension (54, 55). Thus, the chance of curing the hypertension is low even after the primary cause of hypertension has been eliminated by adrenalectomy in PA. An interesting and unexpected result which needs further clarification was that the lower the potassium level, the higher the rate of clinical success as a higher degree of hypokalemia means a greater severity of hyperaldosteronism (56), the predictors which were acquired from crude data should be interpreted with caution. The association between these predictive factors and clinical success does not represent a causal relationship since it is based on unadjusted data which could be confounded by multiple interfering factors.
AVS can interfere with the success of adrenalectomy. Higher rates of success were observed in AVS patients (7). Further subgroup meta-analysis categorized by AVS-guided and non-AVS-guided adrenalectomy has also been conducted. The majority of those results remained the same after subgroup analysis was performed. DDD of medications and serum potassium showed different results after subgroup analysis. However, the DDD results should be interpreted with caution as there was only one study in a subgroup of patients who had AVS. After subgroup analysis, the majority of the predictors showed improvement in terms of heterogeneity. It could be implied that performing AVS modified the effect of clinical success for most of the predictors.
One of the strengths of this first meta-analysis is that only studies which had pre-defined and clear criteria for clinical success were included. Also, funnel plots and Egger’s test indicated that there was publication bias in some of the predictive factors which indicates that many negative unpublished results were not published. Funnel plots with the trim-and-fill method were also applied in this meta-analysis to rectify the corrected effect size. Most of the results remained constant after the trim-and-fill method with the exception of BMI with fully adjusted OR which showed a non-significant association following trim-and-fill. Nevertheless, the results of the association with BMI from crude data remained the same after the trim-and-fill method was applied. Another strength of this study is that the subgroup analysis of whether the included studies had conducted AVS before adrenalectomy was performed or not to reduce the effect modification from AVS. The information acquired from this meta-analysis can be utilized in multiple ways. These predictors can help clinicians identify patients who may have a lower chance of clinical success and so begin early monitoring, early re-initiation of antihypertensive medications and close follow-up after adrenalectomy. Conversely, in patients with multiple predictors of success, clinicians may have higher confidence to proceed to adrenalectomy. In addition, these predictors can help clinicians provide advice to patients regarding the chance of cure and assist them in making a decision regarding adrenalectomy.
There are some limitations in this meta-analysis. First, multiple criteria of clinical success were employed by the different studies. The variety of criteria of clinical success may have affected the outcomes of this meta-analysis. PASO criteria of clinical cure of PA were first developed in 2017 and have been used mostly in the studies published after 2017. Second, the duration of follow-up among the studies ranged widely, from 1 month to 5 years. As some patients’ hypertensive status may have improved slowly after 5 years of adrenalectomy, this could have affected the outcomes especially clinical success rate of the meta-analysis. Third, there was a high level of heterogeneity among the studies. However, the subgroup analysis by AVS status showed significant improvement in terms of heterogeneity for the majority of the predictors. Lastly, the pooled adjusted odds ratio of the predictive factors in most of the included studies were presented as categorical data with different cut-off levels among the studies which may have affected the meta-analysis outcomes.
In summary, demographic data and laboratory investigations can help predict the likelihood of clinical success after unilateral adrenalectomy in PA patients. The success rate is higher in PA patients who are younger, female, have a lower BMI, a shorter duration of hypertension, use a lower number of medications, have lower systolic and diastolic blood pressure, lower serum potassium, higher eGFR and no history of diabetes or dyslipidemia. These predictors can be used in future research to develop numerical scores which could facilitate the prediction of clinical success after surgery and further improve the quality of care of PA patients.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
WM designed the study, collected, analyzed, and interpreted the data, and was the major contributor in writing the manuscript. PA collected and performed data analysis. PP performed the data analyses and edited the manuscript. PI performed data analysis, reviewed and edited the manuscript. All authors contributed to the article and approved the submitted version.
The authors are grateful to Dr.Lamar G.Robert and Dr.Chongchit A.Robert for reviewing the manuscript.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fendo.2022.925591/full#supplementary-material
1. Brown JM, Siddiqui M, Calhoun DA, Carey RM, Hopkins PN, Williams GH, et al. The unrecognized prevalence of primary aldosteronism: A cross-sectional study. Ann Intern Med (2020) 173(1):10–20. doi: 10.7326/M20-0065
2. Wu X, Yu J, Tian H. Cardiovascular risk in primary aldosteronism: A systematic review and meta-analysis. Med (Baltimore) (2019) 98(26):e15985. doi: 10.1097/MD.0000000000015985
3. Wannachalee T, Lieberman L, Turcu AF. High prevalence of autonomous aldosterone production in hypertension: How to identify and treat it. Curr Hypertens Rep (2022) 24:123–32. doi: 10.1007/s11906-022-01176-7
4. Hundemer GL, Curhan GC, Yozamp N, Wang M, Vaidya A. Cardiometabolic outcomes and mortality in medically treated primary aldosteronism: a retrospective cohort study. Lancet Diabetes Endocrinol (2018) 6(1):51–9. doi: 10.1016/S2213-8587(17)30367-4
5. Velema M, Dekkers T, Hermus A, Timmers H, Lenders J, Groenewoud H, et al. Quality of life in primary aldosteronism: A comparative effectiveness study of adrenalectomy and medical treatment. J Clin Endocrinol Metab (2018) 103(1):16–24. doi: 10.1210/jc.2017-01442
6. Sywak M, Pasieka JL. Long-term follow-up and cost benefit of adrenalectomy in patients with primary hyperaldosteronism. Br J Surg (2002) 89(12):1587–93. doi: 10.1046/j.1365-2168.2002.02261.x
7. Rossi GP, Rossitto G, Amar L, Azizi M, Riester A, Reincke M, et al. Clinical outcomes of 1625 patients with primary aldosteronism subtyped with adrenal vein sampling. Hypertension (2019) 74(4):800–8. doi: 10.1161/HYPERTENSIONAHA.119.13463
8. Vorselaars WMCM, Nell S, Postma EL, Zarnegar R, Drake FT, Duh Q-Y, et al. Clinical outcomes after unilateral adrenalectomy for primary aldosteronism. JAMA Surg (2019) 154(4):e185842–e. doi: 10.1001/jamasurg.2018.5842
9. Burrello J, Burrello A, Stowasser M, Nishikawa T, Quinkler M, Prejbisz A, et al. The primary aldosteronism surgical outcome score for the prediction of clinical outcomes after adrenalectomy for unilateral primary aldosteronism. Ann Surg (2020) 272(6):1125–32. doi: 10.1097/SLA.0000000000003200
10. Wachtel H, Cerullo I, Bartlett EK, Kelz RR, Cohen DL, Karakousis GC, et al. Long-term blood pressure control in patients undergoing adrenalectomy for primary hyperaldosteronism. Surgery (2014) 156(6):1394–402. doi: 10.1016/j.surg.2014.08.021
11. Umakoshi H, Tsuiki M, Yokomoto-Umakoshi M, Takeda Y, Takashi Y, Kurihara I, et al. Correlation between lateralization index of adrenal venous sampling and standardized outcome in primary aldosteronism. J Endocr Soc (2018) 2(8):893–902. doi: 10.1210/js.2018-00055
12. Williams TA, Lenders JWM, Mulatero P, Burrello J, Rottenkolber M, Adolf C, et al. Outcomes after adrenalectomy for unilateral primary aldosteronism: an international consensus on outcome measures and analysis of remission rates in an international cohort. Lancet Diabetes Endocrinol (2017) 5(9):689–99. doi: 10.1016/S2213-8587(17)30135-3
13. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Bmj (2021) 372:n71. doi: 10.1136/bmj.n71
14. Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan-a web and mobile app for systematic reviews. Syst Rev (2016) 5(1):210. doi: 10.1186/s13643-016-0384-4
15. Funder JW, Carey RM, Mantero F, Murad MH, Reincke M, Shibata H, et al. The management of primary aldosteronism: Case detection, diagnosis, and treatment: An endocrine society clinical practice guideline. J Clin Endocrinol Metab (2016) 101(5):1889–916. doi: 10.1210/jc.2015-4061
16. von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: Guidelines for reporting observational studies. J Clin Epidemiol (2008) 61(4):344–9. doi: 10.1016/j.jclinepi.2007.11.008
17. Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol (2010) 25(9):603–5. doi: 10.1007/s10654-010-9491-z
18. Pang TC, Bambach C, Monaghan JC, Sidhu SB, Bune A, Delbridge LW, et al. Outcomes of laparoscopic adrenalectomy for hyperaldosteronism. ANZ J Surg (2007) 77(9):768–73. doi: 10.1111/j.1445-2197.2007.04225.x
19. Zarnegar R, Young WF Jr, Lee J, Sweet MP, Kebebew E, Farley DR, et al. The aldosteronoma resolution score: predicting complete resolution of hypertension after adrenalectomy for aldosteronoma. Ann Surg (2008) 247(3):511–8. doi: 10.1097/SLA.0b013e318165c075
20. Murashima M, Trerotola SO, Fraker DL, Han D, Townsend RR, Cohen DL. Adrenal venous sampling for primary aldosteronism and clinical outcomes after unilateral adrenalectomy: A single-center experience. J Clin Hypertens (Greenwich) (2009) 11(6):316–23. doi: 10.1111/j.1751-7176.2009.00120.x
21. Kim RM, Lee J, Soh EY. Predictors of resolution of hypertension after adrenalectomy in patients with aldosterone-producing adenoma. J Korean Med Sci (2010) 25(7):1041–4. doi: 10.3346/jkms.2010.25.7.1041
22. van der Linden P, Steichen O, Zinzindohoué F, Plouin PF. Blood pressure and medication changes following adrenalectomy for unilateral primary aldosteronism: a follow-up study. J Hypertens (2012) 30(4):761–9. doi: 10.1097/HJH.0b013e328350225d
23. Wang W, Hu W, Zhang X, Wang B, Bin C, Huang H. Predictors of successful outcome after adrenalectomy for primary aldosteronism. Int Surg (2012) 97(2):104–11. doi: 10.9738/CC140.1
24. Zhang X, Zhu Z, Xu T, Shen Z. Factors affecting complete hypertension cure after adrenalectomy for aldosterone-producing adenoma: outcomes in a large series. Urol Int (2013) 90(4):430–4. doi: 10.1159/000347028
25. Hartmann I, Grepl M, Vidlar A, Smakal O, Vaclavik J, Frysak Z, et al. Outcomes of adrenalectomy in patients with primary hyperaldosteronism–a single centre experience. BioMed Pap Med Fac Univ Palacky Olomouc Czech Repub (2014) 158(4):583–90. doi: 10.5507/bp.2014.059
26. Utsumi T, Kamiya N, Endo T, Yano M, Kamijima S, Kawamura K, et al. Development of a novel nomogram to predict hypertension cure after laparoscopic adrenalectomy in patients with primary aldosteronism. World J Surg (2014) 38(10):2640–4. doi: 10.1007/s00268-014-2612-1
27. Worth PJ, Kunio NR, Siegfried I, Sheppard BC, Gilbert EW. Characteristics predicting clinical improvement and cure following laparoscopic adrenalectomy for primary aldosteronism in a large cohort. Am J Surg (2015) 210(4):702–9. doi: 10.1016/j.amjsurg.2015.05.033
28. Citton M, Viel G, Rossi GP, Mantero F, Nitti D, Iacobone M. Outcome of surgical treatment of primary aldosteronism. Langenbecks Arch Surg (2015) 400(3):325–31. doi: 10.1007/s00423-014-1269-4
29. Hannon MJ, Sze WC, Carpenter R, Parvanta L, Matson M, Sahdev A, et al. Clinical outcomes following unilateral adrenalectomy in patients with primary aldosteronism. Qjm (2017) 110(5):277–81. doi: 10.1093/qjmed/hcw194
30. Grytaas MA, Strømsøy SS, Rørvik JT, Arnes JB, Heie A, Arnesen T, et al. Clinical characteristics and long-term outcome of primary aldosteronism in a Norwegian population. Horm Metab Res (2017) 49(11):838–46. doi: 10.1055/s-0043-118909
31. Sellgren F, Koman A, Nordenström E, Hellman P, Hennings J, Muth A. Outcomes after surgery for unilateral dominant primary aldosteronism in Sweden. World J Surg (2020) 44(2):561–9. doi: 10.1007/s00268-019-05265-8
32. Morisaki M, Kurihara I, Itoh H, Naruse M, Takeda Y, Katabami T, et al. Predictors of clinical success after surgery for primary aldosteronism in the Japanese nationwide cohort. J Endocr Soc (2019) 3(11):2012–22. doi: 10.1210/js.2019-00295
33. Chan CK, Kim JH, Chueh E, Chang CC, Lin YF, Lai TS, et al. Aldosterone level after saline infusion test could predict clinical outcome in primary aldosteronism after adrenalectomy. Surgery (2019) 166(3):362–8. doi: 10.1016/j.surg.2019.05.001
34. Vorselaars W, van Beek DJ, Postma EL, Spiering W, Borel Rinkes IHM, Valk GD, et al. Clinical outcomes after surgery for primary aldosteronism: Evaluation of the PASO-investigators' consensus criteria within a worldwide cohort of patients. Surgery (2019) 166(1):61–8. doi: 10.1016/j.surg.2019.01.031
35. BiLiGe W, Wang C, Bao J, Yu D, Min A, Hong Z, et al. Predicting factors related with uncured hypertension after retroperitoneal laparoscopic adrenalectomy for unilateral primary aldosteronism. Med (Baltimore) (2019) 98(30):e16611. doi: 10.1097/MD.0000000000016611
36. Thiesmeyer JW, Ullmann TM, Stamatiou AT, Limberg J, Stefanova D, Beninato T, et al. Association of adrenal venous sampling with outcomes in primary aldosteronism for unilateral adenomas. JAMA Surg (2021) 156(2):165–71. doi: 10.1001/jamasurg.2020.5011
37. Picado O, Whitfield BW, Khan ZF, Jeraq M, Farrá JC, Lew JI. Long-term outcome success after operative treatment for primary aldosteronism. Surgery (2021) 169(3):528–32. doi: 10.1016/j.surg.2020.07.046
38. Yang Y, Williams TA, Song Y, Yang S, He W, Wang K, et al. Nomogram-based preoperative score for predicting clinical outcome in unilateral primary aldosteronism. J Clin Endocrinol Metab (2020) 105(12):4382–92. doi: 10.1210/clinem/dgaa634
39. Saiki A, Otsuki M, Mukai K, Hayashi R, Shimomura I, Kurihara I, et al. Basal plasma aldosterone concentration predicts therapeutic outcomes in primary aldosteronism. J Endocr Soc (2020) 4(4):bvaa011. doi: 10.1210/jendso/bvaa011
40. Wang H, Wang F, Zhang Y, Wen J, Dong D, Chang X, et al. Surgical outcomes of aldosterone-producing adenoma on the basis of the histopathological findings. Front Endocrinol (Lausanne) (2021) 12:663096. doi: 10.3389/fendo.2021.663096
41. Chan YHB, Loh LM, Foo RS, Loh WJ, Lim DST, Zhang M, et al. Re-evaluating absent clinical success after adrenalectomy in unilateral primary aldosteronism. Surgery (2021) 170(5):1389–96. doi: 10.1016/j.surg.2021.05.038
42. Dominguez DA, Chatani P, Murphy R, Copeland AR, Chang R, Sadowski SM, et al. Contralateral suppression index does not predict clinical cure in patients undergoing surgery for primary aldosteronism. Ann Surg Oncol (2021) 28(12):7487–95. doi: 10.1245/s10434-021-09692-7
43. Romero-Velez G, Laird AM, Barajas ME, Sierra-Salazar M, Herrera MF, Libutti SK, et al. Outcomes of adrenalectomy and the aldosteronoma resolution score in the black and Hispanic population. World J Surg (2021) 45(5):1475–82. doi: 10.1007/s00268-021-05967-y
44. Leung H-T, Yuen W-C, Lang BH-H, Tan KC-B, Fung BT-C, Lau EY-F, et al. Unilateral adrenalectomy for aldosterone-producing adenoma in Hong Kong: Outcomes and factors predicting resolution of hypertension. Surg Pract (2021) 25(3):138–45. doi: 10.1111/1744-1633.12507
45. Mørup S, Voss N, Clausen C, Feltoft CL, Andreassen M, Krogh J. Prognostic value of contralateral suppression for remission after surgery in patients with primary aldosteronism. Clin Endocrinol (Oxf) (2022) 96(6):793–802. doi: 10.1111/cen.14678
46. Bauer JH. Age-related changes in the renin-aldosterone system. physiological effects and clinical implications. Drugs Aging (1993) 3(3):238–45. doi: 10.2165/00002512-199303030-00005
47. Takeda M, Yamamoto K, Akasaka H, Rakugi H, Naruse M, Takeda Y, et al. Clinical characteristics and postoperative outcomes of primary aldosteronism in the elderly. J Clin Endocrinol Metab (2018) 103(10):3620–9. doi: 10.1210/jc.2018-00059
48. Lacruz ME, Kluttig A, Hartwig S, Löer M, Tiller D, Greiser KH, et al. Prevalence and incidence of hypertension in the general adult population: Results of the CARLA-cohort study. Med (Baltimore) (2015) 94(22):e952. doi: 10.1097/MD.0000000000000952
49. Barrett Mueller K, Lu Q, Mohammad NN, Luu V, McCurley A, Williams GH, et al. Estrogen receptor inhibits mineralocorticoid receptor transcriptional regulatory function. Endocrinology (2014) 155(11):4461–72. doi: 10.1210/en.2014-1270
50. Manosroi W, Tan JW, Rariy CM, Sun B, Goodarzi MO, Saxena AR, et al. The association of estrogen receptor-β gene variation with salt-sensitive blood pressure. J Clin Endocrinol Metab (2017) 102(11):4124–35. doi: 10.1210/jc.2017-00957
51. Rossi GP, Belfiore A, Bernini G, Fabris B, Caridi G, Ferri C, et al. Body mass index predicts plasma aldosterone concentrations in overweight-obese primary hypertensive patients. J Clin Endocrinol Metab (2008) 93(7):2566–71. doi: 10.1210/jc.2008-0251
52. Widimsky J, Strauch B, Petrák O, Rosa J, Somloova Z, Zelinka T, et al. Vascular disturbances in primary aldosteronism: Clinical evidence. Kidney Blood Pressure Res (2012) 35(6):529–33. doi: 10.1159/000340031
53. Schmidt BM, Horisberger K, Feuring M, Schultz A, Wehling M. Aldosterone blunts human baroreflex sensitivity by a nongenomic mechanism. Exp Clin Endocrinol Diabetes (2005) 113(5):252–6. doi: 10.1055/s-2005-837650
54. Stinghen AE, Pecoits-Filho R. Vascular damage in kidney disease: Beyond hypertension. Int J Hypertens (2011) 2011:232683. doi: 10.4061/2011/232683
55. Rask-Madsen C, King GL. Vascular complications of diabetes: mechanisms of injury and protective factors. Cell Metab (2013) 17(1):20–33. doi: 10.1016/j.cmet.2012.11.012
Keywords: primary aldosteronism, adrenalectomy, clinical success, predictive factors, meta-analysis
Citation: Manosroi W, Atthakomol P, Phinyo P and Inthaphan P (2022) Predictive factors of clinical success after adrenalectomy in primary aldosteronism: A systematic review and meta-analysis. Front. Endocrinol. 13:925591. doi: 10.3389/fendo.2022.925591
Received: 21 April 2022; Accepted: 03 August 2022;
Published: 18 August 2022.
Edited by:
Giuseppe Reimondo, University of Turin, ItalyReviewed by:
Andreas Muth, University of Gothenburg, SwedenCopyright © 2022 Manosroi, Atthakomol, Phinyo and Inthaphan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Worapaka Manosroi, V29yYXBha2EubUBjbXUuYWMudGg=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.