- 1Department of Internal Medicine, Allegheny General Hospital, Pittsburgh, PA, United States
- 2Department of Internal Medicine, Dr. Sampurnanand Medical College, Jodhpur, India
- 3Department of Neurology, Allegheny General Hospital, Pittsburgh, PA, United States
- 4Department of Internal Medicine, Government Medical College-Kolhapur, Kolhapur, India
- 5Department of Immunology, Mayo Clinic, Rochester, MN, United States
- 6Department of Internal Medicine, Dow Medical College, Dow University of Health Sciences, Karachi, Pakistan
- 7Department of Gastroenterology and Hepatology, Rutgers Robert Wood Johnson School of Medicine, New Brunswick, NJ, United States
- 8Department of Anesthesiology and Perioperative Medicine, Mayo Clinic Rochester, MN, United States
- 9Department of Emergency Medicine, Marshfield Clinic, Marshfield, WI, United States
- 10Department of Internal Medicine, North Alabama Medical Center, Florence, AL, United States
- 11Department of Internal Medicine, Patliputra Medical College and Hospital, Dhanbad, India
- 12Department of Internal Medicine, Gandhi Medical College, Secunderabad, India
- 13Department of Nephrology, Mayo Clinic, Rochester, MI, United States
- 14Department of Gastroenterology and Hepatology, Mayo Clinic, Rochester, MI, United States
- 15Department of Cardiology, University of Nebraska Medical Center, Omaha, NE, United States
- 16Department of Medicine, Division of Endocrinology and Metabolism, State University of New York (SUNY) Upstate Medical University, Syracuse, NY, United States
- 17Division of Pulmonary and Critical Care Medicine, Mayo Clinic, Rochester, MI, United States
Background: Obesity affects the course of critical illnesses. We aimed to estimate the association of obesity with the severity and mortality in coronavirus disease 2019 (COVID-19) patients.
Data Sources: A systematic search was conducted from the inception of the COVID-19 pandemic through to 13 October 2021, on databases including Medline (PubMed), Embase, Science Web, and Cochrane Central Controlled Trials Registry. Preprint servers such as BioRxiv, MedRxiv, ChemRxiv, and SSRN were also scanned.
Study Selection and Data Extraction: Full-length articles focusing on the association of obesity and outcome in COVID-19 patients were included. Preferred Reporting Items for Systematic Reviews and Meta-Analysis guidelines were used for study selection and data extraction. Our Population of interest were COVID-19 positive patients, obesity is our Intervention/Exposure point, Comparators are Non-obese vs obese patients The chief outcome of the study was the severity of the confirmed COVID-19 positive hospitalized patients in terms of admission to the intensive care unit (ICU) or the requirement of invasive mechanical ventilation/intubation with obesity. All-cause mortality in COVID-19 positive hospitalized patients with obesity was the secondary outcome of the study.
Results: In total, 3,140,413 patients from 167 studies were included in the study. Obesity was associated with an increased risk of severe disease (RR=1.52, 95% CI 1.41-1.63, p<0.001, I2 = 97%). Similarly, high mortality was observed in obese patients (RR=1.09, 95% CI 1.02-1.16, p=0.006, I2 = 97%). In multivariate meta-regression on severity, the covariate of the female gender, pulmonary disease, diabetes, older age, cardiovascular diseases, and hypertension was found to be significant and explained R2 = 40% of the between-study heterogeneity for severity. The aforementioned covariates were found to be significant for mortality as well, and these covariates collectively explained R2 = 50% of the between-study variability for mortality.
Conclusions: Our findings suggest that obesity is significantly associated with increased severity and higher mortality among COVID-19 patients. Therefore, the inclusion of obesity or its surrogate body mass index in prognostic scores and improvement of guidelines for patient care management is recommended.
Introduction
The entire world is enduring the effects of the global coronavirus disease 2019 (COVID-19) pandemic, which began in December 2019, when pneumonia of unknown origin was diagnosed in Hubei province, Wuhan, China (1, 2). It was later in January 2020 that the novel coronavirus strand was isolated and subsequently named severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in February 2020 (3, 4). As of 28 December 2021 the Covid-19 pandemic has affected >281 million individuals and has led to >5.4 million global deaths (5). Even though many treatments have been proposed to combat COVID-19, there is currently no uniformly successful therapy (6–11). Although it is a widespread disease affecting multiple systems, obesity has been identified as one of the major comorbid factors in patients suffering from COVID-19 (12–21).
Overweight (BMI 25 kg/m2-29.9 kg/m2) and obesity (BMI 30 kg/m2 or more) are major public health problems, especially during the COVID-19 pandemic, because of their association with increased morbidity and mortality (22, 23). Berrington de Gonzalez et al. (2010) studied the association between being overweight and obesity on overall mortality in 1.46 million white adults over a median follow-up period of 10 years. They found an approximately linear relationship in the hazard ratios for BMI. The hazard ratio for every 5-unit increment of BMI was 1.31 in the BMI range of 25 kg/m2 to 49.9 kg/m2 (24). According to the 2017-2018 National Health and Nutrition Examination Survey (NHANES), approximately 42.5% of U.S. adults aged 20 or over are obese and approximately 9% have class 3 obesity or severe obesity (BMI 40 kg/m2or more) (25).
According to WHO, the prevalence of obesity has nearly tripled in the last four decades amounting to 13% of the entire world’s adult population (26), which is a cause for concern during the pandemic. The interplay between obesity and other disease conditions has been established for a long time. The presence of these comorbid determinants is related to increased predisposition and severity of COVID-19 (27–30). Many studies have reported increased rates of hospitalization, mechanical ventilation, and mortality in patients with a higher BMI (31–35).
During the pandemic, due to worldwide lockdowns lasting several months, compromised work routine, increased calorie intake, lack of exercise options, and stress due to uncertainty, people are at an increased risk of becoming overweight and developing obesity (36). This could have an excessive toll on the management of COVID-19 disease. To mitigate the impact of heightened morbidity and mortality associated with COVID-19 infection in patients with obesity, it is vital to be cognizant of the implications of increased BMI and its dynamic interaction with other comorbid components. Hence, we evaluated obesity as a paramount risk factor for mortality and severity in COVID-19 infection, independent of potential confounders via systematic review and meta-regression.
Methods
Data Sources and Searches
For documentation, we adopted the Preferred Systematic Analyses and Meta-Analysis Reporting Items recommendations (37). A systematic search was conducted from COVID-19 databases from the pandemic inception through October 13th, 2021 for full-length articles focusing on the association of increased BMI/Obesity [overweight is defined as a BMI between 25.0 and 29.9, and a BMI of 30 or higher is considered obese (38)] in COVID-19 using a pre-specified data extraction protocol including bibliographic information (year of publication, first author), study information (country, sample size), patient characteristics (age, baseline comorbidities, gender), treatment information and outcome data. The search strategy consisted of keywords “SARS-CoV-2”, “COVID-19”, “Coronavirus”, “Obesity”, “BMI”, “Overweight” “Risk factors” across the three large COVID-19 databases (WHO COVID-19, CDC COVID-19, and LitCOVID PubMed) OVID-Medline Embase, Scopus, Web of Science, and Cochrane Central Controlled Trials Registry. Studies were included from all over the world. There were no language barriers during the literature search. Other literature sources such as the BioRxiv (preprints), MedRxiv (preprints), ChemRxiv (preprints), and SSRN (preprints) were searched as well. We screened the title and abstract of each study identified in the literature search to include eligible articles where obesity or BMI was mentioned as a risk factor and overall comparative results or association with COVID-19 were provided in the abstract. Following this step, we conducted a full text review for final evaluation for study inclusion and data extraction. To discover further eligible studies, we manually searched the reference lists of the included studies, and previously published meta-analysis, systematic review, and the relevant literature. We also scanned the clinicaltrials.gov registry for completed, as well as in-progress randomized controlled trials (RCTs).
Study Selection
The inclusion criteria for the systematic review are as follows:
1. Studies reporting outcomes such as severity or mortality events of confirmed COVID-19 positive patients, at least one functional endpoint of COVID-19 positive hospitalized patients where body mass index (BMI) values or comparison of obese vs non-obese were provided.
2. Full text and peer-reviewed articles (Case-studies and case series, randomized controlled trials) were included.
3. Studies published only in the English language were included.
Exclusion Criteria
1.Studies published in a language other than English were not considered.
2. Studies with insufficient information were excluded. Case reports, reviews, or nonhuman studies were excluded.
3. Studies focused on patients aged under 18 years old were also excluded.
Data Extraction and Quality Assessment
The authors (HK and SSR) downloaded all articles from electronic search to EndNote X9 (39) and duplicates were eliminated. Based on the preset eligibility criteria, each study was reviewed by at least two authors (AT, GSS, HK, NJ, YC, RS, SK, KI, and SSR) independently and verified with internal author-reviewer, and disagreements were discussed amongst all author-reviewers and resolved via a consensus. The cases included obese Covid-19 positive hospitalized patients and the controls included the non-obese Covid-19 positive hospitalized patients.
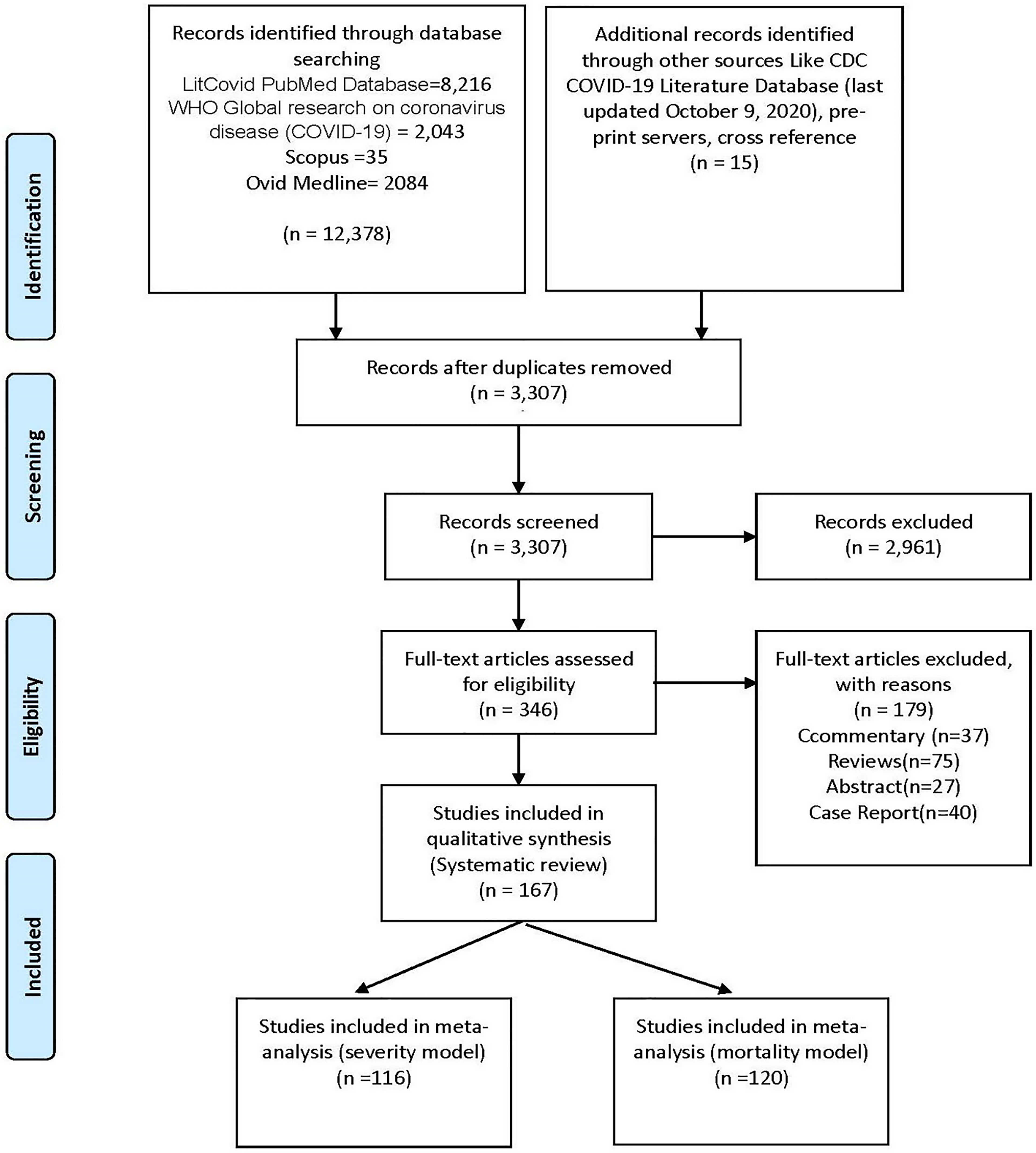
Unadjusted and adjusted impact measurements were also extracted where appropriate. From each study, various details including first author name, study type, hospitalized total covid-19 positive patients, the definition of COVID-19 severity, definition of obesity, total obese & non-obese COVID-19 positive patients, patients with high severity and mortality, median age, gender (female sex proportion), proportions of hypertension, pulmonary disease, cardiovascular disease, diabetes, dyslipidemia, liver disease were recorded (Supplementary Table 1). The included data was checked for accuracy by all authors. Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines were followed (Figure 1 and Supplemental Table 2).
Risk of Bias Assessment
The NIH study quality assessment Tool was used for measuring the risk of bias in case-control studies and cohort studies (40). The NIH quality assessment tools were based on quality assessment methods, concepts, and other tools developed by researchers in the Agency for Healthcare Research and Quality (AHRQ), Cochrane Collaboration, USPSTF, Scottish Intercollegiate Guidelines Network, and National Health Service Centre for Reviews and Dissemination, consulting epidemiologists and evidence-based medicine experts, with adaptations by methodologists and NHLBI staff (40). Three authors (AT, KI, SA, and SSR) evaluated the likelihood of bias independently, and any conflict was resolved by consensus (Supplementary Tables 3A–C).
Data Synthesis and Analysis
All-cause severity in hospitalized COVID-19 patients with high BMI/obesity was the primary outcome. The severity criteria were defined as the need for ICU admission or the need for mechanical ventilation for the admitted COVID-19 positive patients. If both severities were given in the article, then the category with a higher number of reported events was selected as the severity for COVID-19. The severity rate was evaluated in comparison to the control group (non-obese COVID-19 hospitalized patients). While all-cause mortality in COVID-19 hospitalized patients with high BMI/obesity was the secondary outcome.
The meta-analysis specifically included case-control and cohort studies comparing the effects of high BMI/obesity in COVID-19 hospitalized patients comparing them to the non-obese COVID-19 hospitalized patients. All outcomes were analyzed using the Mantel-Haenszel method for dichotomous data to estimate pooled risk ratio (RR) utilizing the Review Manager (RevMan)- Version 5.4, The Cochrane Collaboration, 2020. Meta-analysis was performed first for studies reporting severity of patients in both groups followed by that for studies reporting severity of disease assuming independence of results for studies that reported both. Due to anticipated heterogeneity, summary statistics were calculated using a random-effects model. This model accounts for variability between studies as well as within studies. Statistical heterogeneity was assessed using Q value and I2 statistics.
To explore the differences between studies that might be expected to influence the effect size, we performed random effects (maximum likelihood method) univariate and multivariate meta-regression analyses. The potential sources of variability hypothesized were the gender of the study sample, the proportion of subjects with diabetes, pulmonary disease, dyslipidemia, cardiovascular disease, and hypertension. Covariates were selected for further modeling if they significantly (P < 0.05) modified the association between mortality or severity in the COVID-19 hospitalized patients with high BMI/Obesity. Two models were created, one for severity and the other for mortality of disease as primary and secondary outcomes, respectively. Subsequently, preselected covariates were included in a manual backward and stepwise multiple meta-regression analysis with P = 0.05 as a cutoff point for removal. P < 0.05. (P < 0.10 for heterogeneity) was considered statistically significant. All meta-analysis and meta-regression tests were 2-tailed. The meta-regression was performed with the Comprehensive Meta-Analysis software package (Biostat, Englewood, NJ, USA)14 (41).
We conducted sensitivity analysis with BMI categories (BMI <18 kg/m2, BMI 18 kg/m2-25 kg/m2, BMI 25 kg/m2-29.9 kg/m2, BMI >30 kg/m2, and BMI>40 kg/m2) to decrease inherent selection bias in observational studies (42).
Results
Study Characteristics of Included Studies
A total of 167 studies, consisting of 3,140,413 COVID-19 patients were included in the meta-analysis. The median age for included patients was 62 (56.4-65.5) with an average of 44.3% female participants (Supplementary Table 1). Of the comorbidities considered, 28.1% were diabetics, 22.8% had cardiovascular diseases. For the primary endpoint, i.e. disease severity, a total of 116 studies with predefined severity events with obese vs non-obese were included in the meta-analysis (31, 33, 43–156). These had a combined sample size of 1,685,283 with 117,839 patients reaching the endpoint of high disease severity (Supplementary Table 1). Similarly, a total of 120 studies (33, 43–45, 47, 51, 52, 54–59, 61, 62, 64–67, 69, 71, 73–75, 78, 80, 82, 86, 89–91, 93, 96, 99, 100, 104, 106–108, 112–115, 117–120, 122, 124, 125, 127–134, 136, 138, 139, 141–143, 147, 149, 150, 152, 153, 157–207) were included for mortality meta-analysis as a secondary outcome. These had a combined sample size of 1,935,503 with 277,780 patients reaching the endpoint of mortality.
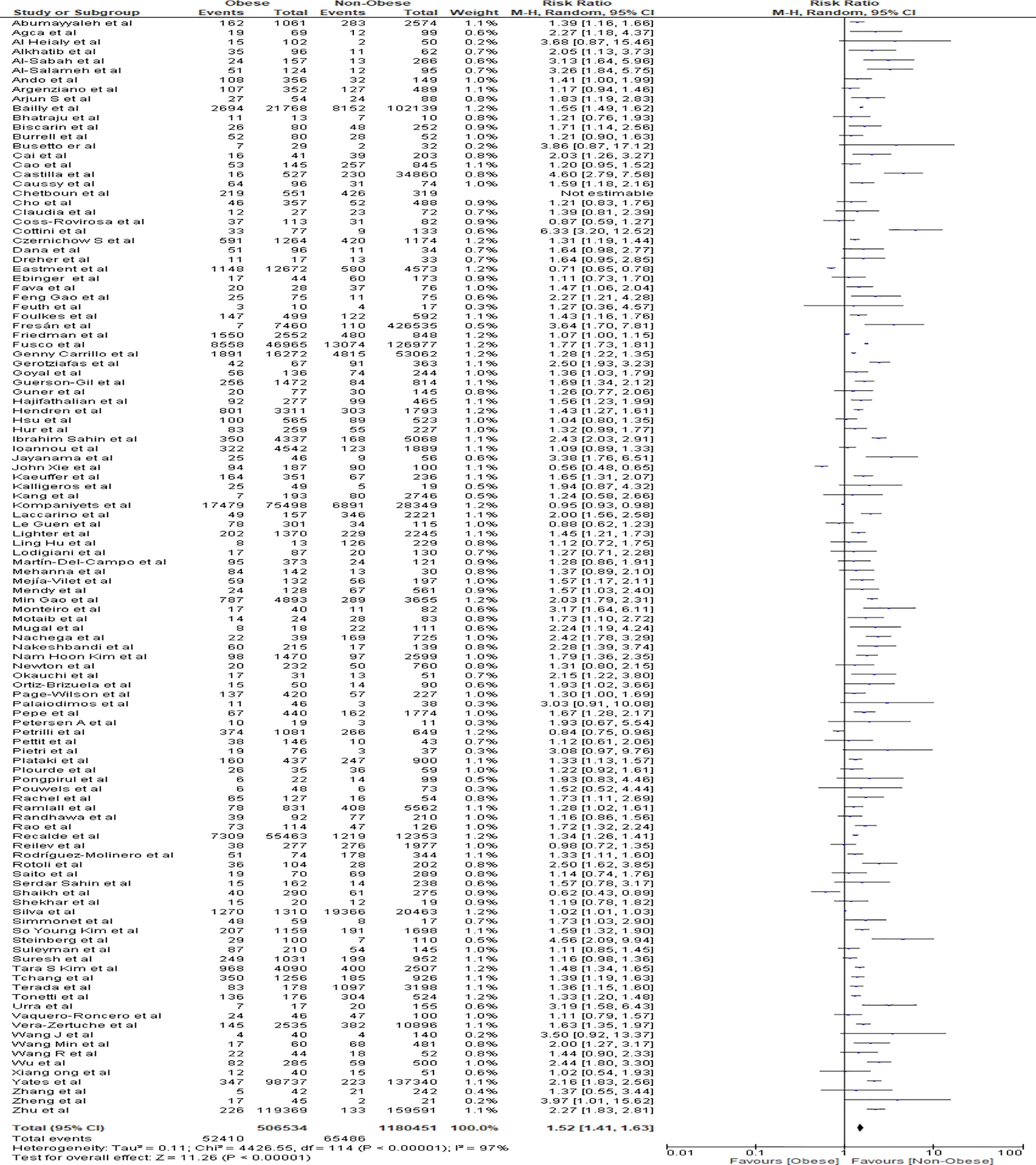
Meta-Analysis for Severity Outcome
Findings from the meta-analysis showed that being obese was correlated with increased severity of COVID-19 positive hospitalized patients in comparison to non-obese patients (RR=1.52, 95% CI 1.41-1.63, p<0.001). Heterogeneity was high with I2 = 97% (Figure 2).
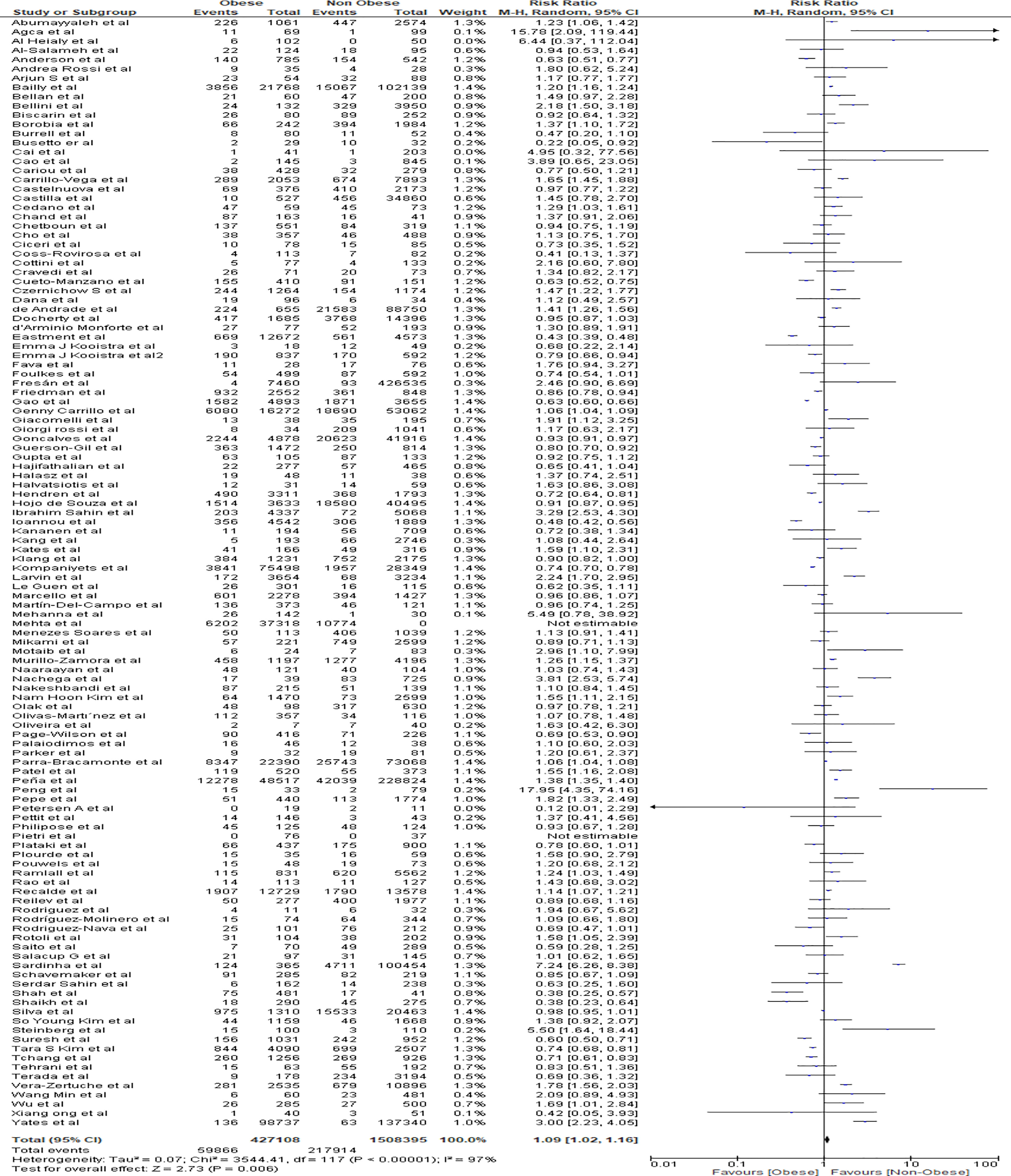
Meta-Analysis for Mortality Outcome
Meta-analysis findings showed that obesity was associated with an increased risk of mortality in obese patients from COVID 19 infections in comparison to the non-obese patient population (RR=1.09, 95% CI 1.02-1.16, p=0.006). Heterogeneity was high with I2 = 97% (Figure 3).
Multivariate Meta-Regression Model for Severity Outcome
Multivariate meta-regression was performed to explain variations in the association between COVID-19 severity and obesity. We found that age, female gender, the proportion of pulmonary disease, diabetes, cardiovascular diseases, and hypertension covariates to be significant, and this explained R2 = 40% of the between-study heterogeneity in severity. Figure 4A shows the resulting equation and individual covariate effect graphs.
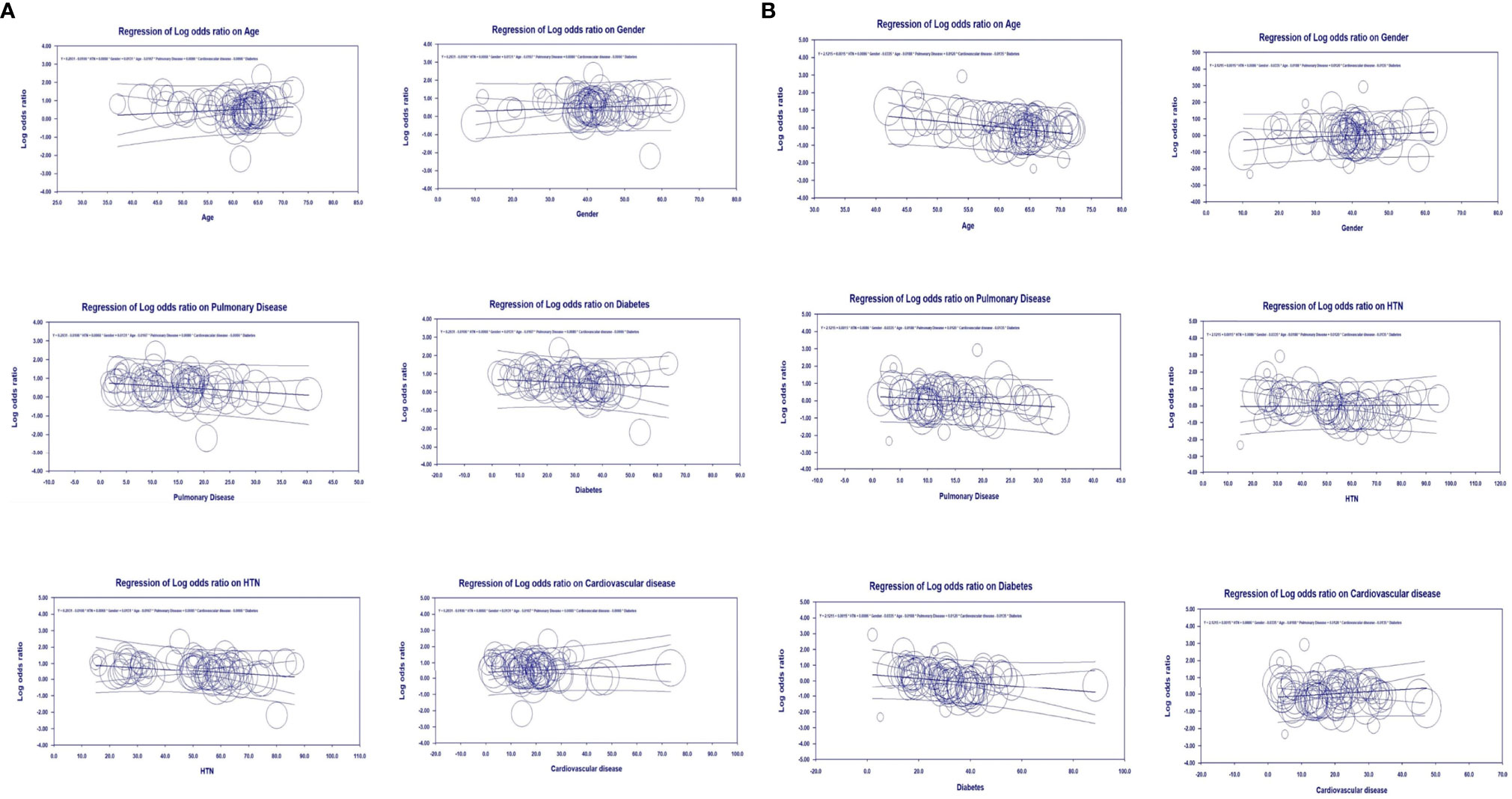
Figure 4 Meta-regression analyses, (A) Severity meta-regression analysis, (B) Mortality meta-regression analysis.
Multivariate Meta-Regression Model for Mortality Outcome
Multivariate meta-regression was performed to explain variations in the association between mortality and obesity, and revealed that age, female gender, the proportion of pulmonary disease, diabetes, hypertension, and cardiovascular diseases were significant together. Overall, these covariates together explained R2 = 50% of the between-study heterogeneity in mortality. Figure 4B shows the resulting equation and individual covariate effect graphs.
Sensitivity Analysis
We did not find any statistical significance for risk of mortality with COVID-19 when analyzed by BMI categories during sensitivity analysis (Supplementary Figures 1A–C). However, we observed that underweight status (BMI<18 kg/m2) is associated with increased risk of mortality in COVID-19 (RR 1.50, 95% CI 1.36-1.65, p=<0.001; I2 = 46%) (Supplementary Figure 1D) but not statistically significant to severity of COVID-19 (RR 1.04, 95% CI 0.85-1.28, p=0.69; I2 = 83%) (Supplementary Figure 1E) as compared to normal BMI category of 18-24.99 kg/m2. Normal weight is protective to COVID-19 disease severity compare to overweight (BMI 25-29.9 kg/m2) (RR 0.75, 95% CI 0.69-0.82, p=<0.001; I2 = 88%), Class 1 and Class 2 obesity (BMI of 30-39.99 kg/m2) (RR 0.67, 95% CI 0.60-0.74, p=<0.001; I2 = 94%) and Class 3 obesity (BMI >40 kg/m2) (RR 0.77, 95% CI 0.68-0.88, p=<0.001; I2 = 89%).
Publication Bias
Visual inspection of the standard error plots for the severity analysis also (Supplementary Figure 2A) suggests symmetry without an underrepresentation of studies of any precision. However, in Egger’s regression test the null hypothesis of no small study effects was rejected at p<0.05 (estimated bias coefficient = -0.27 ± 0.16SE).
Similarly, visual inspection of the standard error plots for the mortality analysis (Supplementary Figure 2B) suggests symmetry without an underrepresentation of studies of any precision. Corroborating inspection findings, Egger’s regression test, the null hypothesis of no small study effects, was rejected at p<0.05 (estimated bias coefficient = -0.20 ± 0.15SE).
Discussion
Summary of Result
In our study, we found that obesity has a strong association with increased severity and mortality of COVID-19 infection. Our results suggest that obese individuals are 1.5 times more likely to experience severe outcomes and 1.09 times more likely to die when compared to non-obese individuals with COVID-19 disease. Our meta-regression severity model suggested that 40% of the heterogeneity could be explained by age, gender, diabetes, hypertension, pulmonary and cardiovascular diseases. The mortality meta-regression model suggested that 50% of the heterogeneity could be explained by age, gender, diabetes, hypertension, pulmonary and cardiovascular diseases. Through these regression models, we were able to address the major amount of heterogeneity seen in our meta-analysis.
Comparison With Existing Literature
Various meta-analyses were conducted to evaluate the association of obesity with mortality and severity in critically ill patients (208–210). The results were not universal, despite a wide variety of observations. In a total of 62,045 critically ill patients, Akinnusi et al. compared the ICU mortality between obese and non-obese patients and found no dissimilarities (208). Hogue et al. (n=22) conducted a meta-analysis of 88,051 patients and found that obesity did not impact ICU mortality (209). However, Oliveros and Villamor et al. found that ICU mortality was increased only in underweight patients and reduced in overweight and obese patients (210). In another study, Zhao et al. observed that having a high BMI is related to a longer duration on mechanical ventilation but lower mortality (211). We also found four meta-analyses (studies n=6, 17, 40, 76) (212–215) that explored the association of obesity and worse outcomes in COVID-19 and found a similar association. On the contrary, one study (216) refuted the possibility of this association. Owing to their small sample population (Studies n=2), it is likely that they were underpowered to tease out the true difference or association (216). With a much larger sample size (n=167) our study provides more robust evidence to establish this association.
Over the last year, five meta-regression studies evaluating the direct relationship between obesity and COVID-19 have been published. Yang et al. (studies n=41) concluded that in COVID-19 patients obesity is associated with increased mortality, increased rates of hospitalization, ICU admissions, and the need for mechanical ventilation. However, they found no confounding factors causing heterogeneity regarding hospitalization, ICU admission, and in-hospital mortality of COVID-19 patients (217). In another such study, Mesas et al. (studies n=60) described that obesity was linked to increased mortality only in studies with fewer chronic or critical patients and reported the mean age of patients as the most important source of heterogeneity, followed by sex and health condition (218). Soereto et al. (studies n=16) reported that patients with higher BMI were at increased risk of developing ‘poor outcomes’ - defined as mortality, ICU admission, ARDS incidence, severe COVID-19, need for mechanical ventilation, and hospitalization. In their meta-regression, the heterogeneity in poor outcomes was explained by age, type 2 diabetes mellitus, hypertension, and gender (219). Cai Z. et al (220) also published meta-analysis results involving 46 studies and a population size of 625,153 patients. They also found similar results as our meta-analysis, wherein patients with obesity have a higher risk of hospitalization, ICU admission, and mechanical ventilation. We have improved upon that and analyzed 167 studies involving more than 3.14 million patients and achieved similar results. Another meta-analysis and regression study by Poly TN et al (213) included 17 studies and reiterated that patients with class III obesity are at more risk than patients with class II or class I obesity. Du et al (148) and Chu et al (149) (studies n=16 and 22, respectively) found that the association between obesity and COVID-19 severity and mortality was significantly influenced by age, but not by gender or other comorbidities. Our meta-regression identified the likely confounders to be age, gender, and co-morbidities. Through this model, we were able to explain high heterogeneity with the highest number of confounders, which other meta-regressions in recent literature were not able to reach and many did not define high heterogeneity in their analysis (217–219, 221, 222). Thus, we established the remarkable, strong association that obesity plays in worsening these outcomes in patients with COVID-19 infection.
In the sensitivity analyses, we were only able to find statistically significant results for increased mortality in BMI<18 kg/m2 as compared to BMI 18 kg/m2-25 kg/m2, however, such significance was not noted in any other BMI categories with severity and mortality in COVID-19. This could be due to BMI being a crude estimate of adiposity, and that it may not be sensitive enough to tease out the real differences. However, in their study, Anderson et al (157) found that patients with obesity have a greater chance of intubation or mortality, with people with class 3 obesity having the greatest risk compared to overweight patients.
Pathophysiological Connection of Obesity and COVID-19 Infection
Obesity is known to be associated with many comorbid conditions (223), including hypertension, atherogenic dyslipidemia, cardiovascular disease, insulin resistance or type 2 diabetes, and altered cortisol metabolism, etc (224). Various biological mechanisms contribute towards increased risk of severity or mortality upon COVID-19 infection in obese patients. First, ectopic fat exacerbates the inflammation caused by COVID-19 by the upregulation of proinflammatory cytokines like interleukin-6 (IL-6) and tumor necrosis factor-alpha (TNF-α), angiotensin II (ATII), and prothrombotics (225–227). Second, obese patients are found to have decreased levels of anti-inflammatory adipokine, adiponectin, which is linked to an increased level of ATII (228, 229). Obesity is associated with overexpression of ACE2 receptors which may aid infection and serve as viral reservoir (230). Further, coronavirus reduces the activity of ACE2 inhibitors, which again leads to an increase in the ATII level (231, 232). Higher levels of ATII lead to progression of lung injury among COVID-19 patients by triggering the NADH/NADPH oxidase system and promoting fibrosis, contraction, and vasoconstriction (233, 234). Moreover, it is associated with endothelial dysfunction (235), the key pathogenic event in COVID-19 leading to mortality and morbidity (236, 237). Furthermore, an increased expression of inflammatory adipokine molecules enhances the production of cytokines TNF-α and IL-6, which are associated with alveolar damage that leads to higher severity and mortality (238). Obesity or increased adiposity plays a key role in endothelial dysfunction by activating several cascades of pathological events, namely activation of renin-angiotensin system (239), activation of procoagulant/hypercoagulation pathway (240), activation of proinflammatory mediators (241), insulin resistance (242), oxidative stress (243), platelet dysfunction (244), and immune dysregulation (245). In the study by Danzinger et al (246) obesity was found to be associated with increased incidence of acute kidney injury and an increase in short- and long-term mortality. These events are summarized in Supplementary Figure 3.
Public Health Implication
The COVID-19 pandemic has created a multitude of concerns globally, and public health providers are working towards minimizing the damaging effects of COVID-19. There is no direct and effective treatment available to control the infection, thus, global morbidity and mortality increase day by day (5). COVID19 shows a wide spectrum of symptoms; many individuals recover without many health complications. However, some infected patients had severe symptoms which required hospitalization, care in intensive care units (ICU), prolonged symptom management, still many succumbed to death (247). Elderly patients were more vulnerable to severe outcomes because they have had multiple diseases and associated risks. A significant number of studies reported that elderly patients and patients with diabetes, stroke, CKD, and COPD are associated with poor outcomes (248, 249). Obesity, especially, class 3 obesity, was associated with an increased rate of mortality among patients infected with COVID-19. Similarly, during the previous H1N1 pandemic, patients with obesity observed prolonged hospitalization, mechanical ventilation, and increased mortality when it was calculated as an independent risk factor (250, 251).
Several population-based cohort studies reported that obesity is linked to increased comorbidities like diabetes, hypertension, and heart disease. Importantly, the mortality rate among patients with obesity proportionally increased with BMI (22, 252). Moreover, obesity makes patients’ conditions worse if patients develop infections by downregulating the inflammatory cascade. Hyperactivation of inflammatory pathways alter the level of cytokines, adiponectin, and leptin and distort both macro- and micro-vascular responses (22, 252, 253). Obesity is also associated with lung function impairment, which involves altering mechanics and airway resistance and decreasing the gas exchange (254, 255). The findings of our study suggest that health care providers and physicians should pay attention to the obesity status of COVID-19 patients because this group of patients is at high risk of worse consequences. The conclusions of our study as well as of others, highlight the need for vigilance, and an earlier start to treatment in obese patients with COVID-19 infection (256, 257) as obese patients had higher hospitalization, ICU care, a requirement of mechanical ventilation with poor prognosis, and worse outcomes.
Effect of COVID-19 on Obesity and Prevention/Treatment Strategies for Patients With Obesity
COVID-19 plays a role in the emergence of obesity in this regard. The public health response to the COVID-19 pandemic is mostly based on restricting human contact and isolation, which affects people’s behavior, and is linked to an increased risk of mental disease (258) and adds to increased incidence of obesity (259). Maintaining a healthy body weight requires regular physical activity, which was cut down during the isolation required during the COVID-19 pandemic (260). People tend to overeat as a result of increased anxiety and monotony, resulting in the consumption of additional energy/calories and an intense desire for food (261). Similarly, quarantine during the COVID-19 outbreak has led to an economic burden, and in some cases, this might mean people having to choose cheaper, less healthy meals. These foods are processed and associated with more fat, carbohydrates, and higher calorie intake (262), which is more likely to cause weight gain than a balanced healthy diet (263).
Obesity must be avoided at all costs. Increased physical activity and calorie restriction are typically used to lose weight. For weight maintenance, it is recommended that people exercise for more than 300 minutes each week (264). People use a range of weight-loss tactics to achieve this, such as consuming fewer calories, daily exercise, intermittent fasting, and using weight-loss medications or diuretics (265). Decreasing calorie consumption is by far the most popular method for weight reduction (266, 267). Metformin usage was reported to be strongly linked with a decrease in COVID-19 mortality in one study (268). This discovery might be explained by a number of factors. Metformin usage was reported to be strongly linked with a decrease in COVID-19 mortality in another recent study (269). This discovery might be explained by a number of factors (268). First, metformin inhibits SARS-CoV-2 from attaching to the receptor (270). Second, metformin suppresses SARS-CoV-2 infectivity and COVID-19 mortality by inhibiting the mTOR signaling pathway (268). Finally, metformin has been shown to reduce inflammatory responses (271). Metformin also lowers the risk of negative outcomes in COVID-19 individuals by lowering their BMI and body weight (272).
Strengths and Limitations
The prime strength of this study is the large sample size. With an exhaustive search strategy, we compiled 167 studies conducted globally. We also added the most recent studies to our meta-analysis and meta-regression model including those that reported contradictory information. This enabled us to arrive at a more definitive conclusion about the risk associations. To define the heterogeneity in the meta-analysis, we also conducted a meta-regression analysis. For moderators, we used the most probable confounders based on the available evidence. This enabled us to delineate the impact of obesity as an independent risk factor for mortality and severity in COVID-19.
We included five studies from preprint databases (78, 102, 109, 146, 200) that may not be comparable to peer-reviewed articles in terms of their quality of methodology. However, given the time-sensitive nature of this pandemic, the benefit of early dissemination of critical information and its inclusion in various analyses outweighs the risk from minor methodological flaws. The second factor was the heterogeneity in the studies in terms of the study design and methodology, patient sample, and treatment received. There was a lack of uniformity in the type of outcomes evaluated for severity and their definitions in different studies. For the same reason, it was not possible to deduce the effect of obesity on individual outcomes. The third limitation is that the analysis was undertaken for hospitalized patients only, meaning we cannot generalize our results for patients treated in outpatient clinics or at home. Analyzing outpatient data may help us gain a complete picture of the impact of obesity on overall COVID-19 outcomes. The fourth limitation is that our analysis did not compare the outcomes with respect to visceral obesity and only BMI was used. However, it was beyond the scope of this analysis because of the lack of those details in most included studies. We suggest that prospective studies should obtain and report this information about their sample population. Lastly, it is possible that some confounders, which could have otherwise accounted for the residual heterogeneity, were not evaluated in the meta-regression analysis due to limited information.
Conclusion
Our findings suggest that obesity significantly increases the risk of severity and mortality in hospitalized COVID-19 patients. Therefore, the inclusion of obesity or surrogate body mass index in prognostic scores and streamlining the management strategy and treatment guidelines to account for the impact of obesity would be vital to improving patient outcomes in hospitalized COVID-19 patients. Our findings also serve as a call for the scientific community to delve further into its pathophysiology and identify potential pharmacological targets, since COVID-19 is an ever-evolving disease. Finally, this information must be disseminated to the general public to intensify the primary prevention of obesity.
Data Availability Statement
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found in the article/Supplementary Material.
Author Contributions
Authors RS and SSR contributed equally to defining the study outline and manuscript writing and are co-primary authors. Data review and collection were performed by AT, GSS, HK, KI, NJ, RS, SK, AP, YC, and SSR; statistical analysis was undertaken by AB, SK, and VB; risk of bias was done by AT, SA, KI, NS, and SSR. Study design and the distribution of articles for critical review were performed by IM, VP, RK, and VB. All authors approved the final version of the published study. RS, SSR, VB, and VP are the guarantors of the published work, and take responsibility for the integrity of the work as a whole, from inception to the published article. All authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
The first version of this manuscript was submitted to medRxiv preprint server. Data from this study were submitted as an abstract format for the upcoming SCCM 51st Critical Care Congress in San Juan, Puerto Rico, and received Bronze Snapshot Awards.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fendo.2022.780872/full#supplementary-material
References
1. Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, et al. Clinical Course and Risk Factors for Mortality of Adult Inpatients With COVID-19 in Wuhan, China: A Retrospective Cohort Study. Lancet (2020) 395(10229):1054–62. doi: 10.1016/S0140-6736(20)30566-3
2. Shah A, Kashyap R, Tosh P, Sampathkumar P, O'Horo JC. Guide to Understanding the 2019 Novel Coronavirus. Mayo Clin Proc (2020) 95(4):646–52. doi: 10.1016/j.mayocp.2020.02.003
3. Wang C, Horby PW, Hayden FG, Gao GF. A Novel Coronavirus Outbreak of Global Health Concern. Lancet (2020) 395(10223):470–3. doi: 10.1016/S0140-6736(20)30185-9
4. Organization WH. Naming the Coronavirus Disease (COVID-19) and the Virus That Causes it (2020). World Health Organization. Available at: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance/naming-the-coronavirus-disease-(covid-2019)-and-the-virus-that-causes-it (Accessed March 17, 2021).
5. Dong E, Du H, Gardner L. An Interactive Web-Based Dashboard to Track COVID-19 in Real Time. Lancet Infect Dis (2020) 20(5):533–4. doi: 10.1016/S1473-3099(20)30120-1
6. Bansal V, Mahapure KS, Bhurwal A, Gupta I, Hassanain S, Makadia J, et al. Mortality Benefit of Remdesivir in COVID-19: A Systematic Review and Meta-Analysis. Front Med (Lausanne) (2020) 7:606429. doi: 10.3389/fmed.2020.606429
7. Jain R, Javeri Y, Nasa P, Kashyap R, Khanna A, Tayar A, et al. Consensus Statement for Pharmacological Management of Coronavirus Disease 2019 (COVID-19): A Pragmatic Approach. Asploro J Biomed Clin Case Rep (2020) 3(3):241. doi: 10.36502/2020/ASJBCCR.6219
8. Romil S, Shaik L, Mehra I, Kashyap R, Surani S. Novel and Controversial Therapies in COVID-19. Open Respir Med J (2020) 14:79–86. doi: 10.2174/1874306402014010079
9. Bansal V, Mahapure KS, Mehra I, Bhurwal A, Tekin A, Singh R, et al. Mortality Benefit of Convalescent Plasma in COVID-19: A Systematic Review and Meta-Analysis. Front Med (Lausanne) (2021) 8:624924. doi: 10.3389/fmed.2021.624924
10. Singh R, Rathore SS, Khan H, Bhurwal A, Sheraton M, Ghosh P, et al. Mortality and Severity in COVID-19 Patients on ACEIs & ARBs - A Meta-Regression Analysis. Front Med (Lausanne) (2021) 8:703661. doi: 10.3389/fmed.2021.703661
11. Karale S, Bansal V, Makadia J, Tayyeb M, Khan H, Ghanta SS, et al. A Meta-Analysis of Mortality, Need for ICU Admission, Use of Mechanical Ventilation and Adverse Effects With Ivermectin Use in COVID-19 Patients. medRxiv (2021) 2021.2004.2030.21256415. doi: 10.1101/2021.04.30.21256415
12. Prevention CfDCa. People With Certain Medical Conditions (2021). CDC. Available at: https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-with-medical-conditions.html (Accessed March 17, 2021).
13. Rathore SS, Rojas GA, Sondhi M, Pothuru S, Pydi R, Kancherla N, et al. Myocarditis Associated With Covid-19 Disease: A Systematic Review of Published Case Reports and Case Series. Int J Clin Pract (2021) 75(11):e14470. doi: 10.1111/ijcp.14470
14. Sheraton M, Deo N, Kashyap R, Surani S. A Review of Neurological Complications of COVID-19. Cureus (2020) 12(5):e8192. doi: 10.7759/cureus.8192
15. Singh R, Kashyap R, Hutton A, Sharma M, Surani S. A Review of Cardiac Complications in Coronavirus Disease 2019. Cureus (2020) 12(5):e8034. doi: 10.7759/cureus.8034
16. Shah K, Bedi S, Onyeaka H, Singh R, Chaudhari G. The Role of Psychological First Aid to Support Public Mental Health in the COVID-19 Pandemic. Cureus (2020) 12(6):e8821. doi: 10.7759/cureus.8821
17. Shah K, Mann S, Singh R, Bangar R, Kulkarni R. Impact of COVID-19 on the Mental Health of Children and Adolescents. Cureus (2020) 12(8):e10051. doi: 10.7759/cureus.10051
18. Menon T, Sharma R, Kataria S, Sardar S, Adhikari R, Tousif S, et al. The Association of Acute Kidney Injury With Disease Severity and Mortality in COVID-19: A Systematic Review and Meta-Analysis. Cureus (2021) 13(3):e13894. doi: 10.7759/cureus.13894
19. Singh R, Shiza ST, Saadat R, Dawe M, Rehman U. Association of Guillain-Barre Syndrome With COVID-19: A Case Report and Literature Review. Cureus (2021) 13(3):e13828. doi: 10.7759/cureus.13828
20. Menon T, Sharma R, Earthineni G, Iftikhar H, Sondhi M, Shams S, et al. Association of Gastrointestinal System With Severity and Mortality of COVID-19: A Systematic Review and Meta-Analysis. Cureus (2021) 13(2):e13317. doi: 10.7759/cureus.13317
21. Menon T, Gandhi SAQ, Tariq W, Sharma R, Sardar S, Arshad AM, et al. Impact of Chronic Kidney Disease on Severity and Mortality in COVID-19 Patients: A Systematic Review and Meta-Analysis. Cureus (2021) 13(4):e14279. doi: 10.7759/cureus.14279
22. Prospective Studies C, Whitlock G, Lewington S, Sherliker P, Clarke R, Emberson J, et al. Body-Mass Index and Cause-Specific Mortality in 900 000 Adults: Collaborative Analyses of 57 Prospective Studies. Lancet (2009) 373(9669):1083–96. doi: 10.1016/S0140-6736(09)60318-4
23. Goyal P, Ringel JB, Rajan M, Choi JJ, Pinheiro LC, Li HA, et al. Obesity and COVID-19 in New York City: A Retrospective Cohort Study. Ann Intern Med (2020) 173(10):855–8. doi: 10.7326/M20-2730
24. Berrington de Gonzalez A, Hartge P, Cerhan JR, Flint AJ, Hannan L, MacInnis RJ, et al. Body-Mass Index and Mortality Among 1.46 Million White Adults. N Engl J Med (2010) 363(23):2211–9. doi: 10.1056/NEJMoa1000367
25. Fryar CD, Carroll MD, Afful J. revalence of Overweight, Obesity, and Severe Obesity Among Adults Aged 20 and Over: United States, 1960–1962 Through 2017–2018. NCHS Health E-Stats, Centers for Disease Control and Prevention. https://www.cdc.gov/nchs/data/hestat/obesity-adult-17-18/overweight-obesity-adults-H.pdf. Published 2020. Updated 01.29.2021. Accessed 01.30.2021.
26. Organization WH. Obesity and Overweight (2020). WHO. Available at: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (Accessed March 17, 2021).
27. Barnes AS. The Epidemic of Obesity and Diabetes: Trends and Treatments. Tex Heart Inst J (2011) 38(2):142–4.
28. Klop B, Elte JW, Cabezas MC. Dyslipidemia in Obesity: Mechanisms and Potential Targets. Nutrients (2013) 5(4):1218–40. doi: 10.3390/nu5041218
29. Fifi JT, Mocco J. COVID-19 Related Stroke in Young Individuals. Lancet Neurol (2020) 19(9):713–5. doi: 10.1016/S1474-4422(20)30272-6
30. Jain S, Chaves SS. Obesity and Influenza. Clin Infect Dis (2011) 53(5):422–4. doi: 10.1093/cid/cir448
31. Kalligeros M, Shehadeh F, Mylona EK, Benitez G, Beckwith CG, Chan PA, et al. Association of Obesity With Disease Severity Among Patients With Coronavirus Disease 2019. Obes (Silver Spring) (2020) 28(7):1200–4. doi: 10.1002/oby.22859
32. Prevention CfDCa. Obesity, Race/Ethnicity, and COVID-19 (2020). CDC. Available at: https://www.cdc.gov/obesity/data/obesity-and-covid-19.html (Accessed March 17, 2021).
33. Hendren NS, de Lemos JA, Ayers C, Das SR, Rao A, Carter S, et al. Association of Body Mass Index and Age With Morbidity and Mortality in Patients Hospitalized With COVID-19: Results From the American Heart Association COVID-19 Cardiovascular Disease Registry. Circulation (2021) 143(2):135–44. doi: 10.1161/CIRCULATIONAHA.120.051936
34. Domecq JP, Lal A, Sheldrick CR, Kumar VK, Boman K, Bolesta S, et al. Outcomes of Patients With Coronavirus Disease 2019 Receiving Organ Support Therapies: The International Viral Infection and Respiratory Illness Universal Study Registry. Crit Care Med (2021) 49(3):437–48. doi: 10.1097/CCM.0000000000004879
35. Walkey AJ, Kumar VK, Harhay MO, Bolesta S, Bansal V, Gajic O, et al. The Viral Infection and Respiratory Illness Universal Study (VIRUS): An International Registry of Coronavirus 2019-Related Critical Illness. Crit Care Explor (2020) 2(4):e0113. doi: 10.1097/CCE.0000000000000113
36. Zupo R, Castellana F, Sardone R, Sila A, Giagulli VA, Triggiani V, et al. Preliminary Trajectories in Dietary Behaviors During the COVID-19 Pandemic: A Public Health Call to Action to Face Obesity. Int J Environ Res Public Health (2020) 17(19). doi: 10.3390/ijerph17197073
37. Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP, et al. The PRISMA Statement for Reporting Systematic Reviews and Meta-Analyses of Studies That Evaluate Healthcare Interventions: Explanation and Elaboration. BMJ (2009) 339:b2700. doi: 10.1136/bmj.b2700
38. Centers for Disease Control and Prevention. Defining Adult Overweight & Obesity. Available at: https://www.cdc.gov/obesity/adult/defining.html (Accessed 11/20/2021).
39. Hupe M. EndNote X9. J Electronic Resour Med Libraries (2019) 16(3-4):117–9. doi: 10.1080/15424065.2019.1691963
40. National Heart Lung and Blood Institute. Study Quality Assessment Tools (2021). Available at: https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools (Accessed August 20th 2021).
41. Borenstein M, Hedges L, Higgins J, Rothstein H. Comprehensive Meta-Analysis Version 3. Biostat, Englewood, NJ 2013 (2013). Available at: https://www.meta-analysis.com/index.php?cart=BBFA4702757 (Accessed 03/11/2021).
42. Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al. Cochrane Handbook for Systematic Reviews of Interventions. John Wiley & Sons; (2019).
43. Abumayyaleh M, Nunez Gil IJ, El-Battrawy I, Estrada V, Becerra-Munoz VM, Aparisi A, et al. Does There Exist an Obesity Paradox in COVID-19? Insights of the International HOPE-COVID-19-Registry. Obes Res Clin Pract (2021) 15(3):275–80. doi: 10.1111/cob.12414
44. Agca M, Tuncay E, Yildirim E, Yildiz R, Sevim T, Ernam D, et al. Is Obesity a Potential Risk Factor for Poor Prognosis of COVID-19? Infect Chemother (2021) 53(2):319–31. doi: 10.1038/s41366-020-00721-1
45. Al Heialy S, Hachim MY, Hachim IY, Bin Naeem K, Hannawi H, Lakshmanan J, et al. Combination of Obesity and Co-Morbidities Leads to Unfavorable Outcomes in COVID-19 Patients. Saudi J Biol Sci (2021) 28(2):1445–50. doi: 10.1002/oby.22937
46. Al-Sabah S, Al-Haddad M, Al-Youha S, Jamal M, Almazeedi S. COVID-19: Impact of Obesity and Diabetes on Disease Severity. Clin Obes (2020) 10(6):e12414. doi: 10.7326/M20-3214
47. Al-Salameh A, Lanoix JP, Bennis Y, Jamal M, Almazeedi S. The Association Between Body Mass Index Class and Coronavirus Disease 2019 Outcomes. Int J Obes (Lond) (2021) 45(3):700–5. doi: 10.1038/s41598-021-96720-x
48. Alkhatib AL, Kreniske J, Zifodya JS, Andrejak C, Brochot E, Deschasse G, et al. BMI is Associated With Coronavirus Disease 2019 Intensive Care Unit Admission in African Americans. Obes (Silver Spring) (2020) 28(10):1798–801. doi: 10.1016/j.numecd.2020.11.012
49. Ando W, Horii T, Uematsu T, Hanaki H, Atsuda K, Otori K. Impact of Overlapping Risks of Type 2 Diabetes and Obesity on Coronavirus Disease Severity in the United States. Sci Rep (2021) 11(1):17968. doi: 10.1136/bmj.m1996
50. Argenziano MG, Bruce SL, Slater CL, Fonseca V, Tahboub M, Khatib J, et al. Characterization and Clinical Course of 1000 Patients With Coronavirus Disease 2019 in New York: Retrospective Case Series. BMJ (2020) 369:m1996. doi: 10.1016/j.chest.2020.08.301
51. Arjun S, Farraj K, Yeroushalmi K, Desai J, Paz SG, Im J, et al. Evaluating Obesity Paradox IN COVID 19: Insights From a Safety-Net Hospital In New York. Chest (2020) 158(4):302a-302a. doi: 10.1016/j.cmi.2021.09.010
52. Bailly L, Fabre R, Courjon J, Carles M, Dellamonica J, Pradier C. Obesity, Diabetes, Hypertension and Severe Outcomes Among Inpatients With Coronavirus Disease 2019: A Nationwide Study. Clin Microbiol Infect (2021). doi: 10.1038/s41598-020-77698-4
53. Bhatraju PK, Ghassemieh BJ, Nichols M, Kim R, Jerome KR, Nalla AK, et al. Covid-19 in Critically Ill Patients in the Seattle Region - Case Series. N Engl J Med (2020) 382(21):2012–22. doi: 10.1016/j.numecd.2020.11.030
54. Biscarini S, Colaneri M, Ludovisi S, Seminari E, Pieri TC, Valsecchi P, et al. The Obesity Paradox: Analysis From the SMAtteo COvid-19 REgistry (SMACORE) Cohort. Nutr Metab Cardiovasc Dis (2020) 30(11):1920–5. doi: 10.1056/NEJMoa2004500
55. Burrell AJ, Pellegrini B, Salimi F, Begum H, Broadley T, Campbell LT, et al. Outcomes for Patients With COVID-19 Admitted to Australian Intensive Care Units During the First Four Months of the Pandemic. Med J Aust (2021) 214(1):23–30. doi: 10.1016/j.numecd.2020.07.047
56. Busetto L, Bettini S, Fabris R, Serra R, Dal Pra C, Maffei P, et al. Obesity and COVID-19: An Italian Snapshot. Obes (Silver Spring) (2020) 28(9):1600–5. doi: 10.3390/jcm9061733
57. Cai Q, Chen F, Wang T, Luo F, Liu X, Wu Q, et al. Obesity and COVID-19 Severity in a Designated Hospital in Shenzhen, China. Diabetes Care (2020) 43(7):1392–8. doi: 10.5694/mja2.50883
58. Cao P, Song Y, Zhuang Z, Ran J, Xu L, Geng Y, et al. Obesity and COVID-19 in Adult Patients With Diabetes. Diabetes (2021) 70(5):1061–9. doi: 10.1002/oby.22918
59. Castilla J, Guevara M, Miqueleiz A, Baigorria F, Ibero-Esparza C, Navascues A, et al. Risk Factors of Infection, Hospitalization and Death From SARS-CoV-2: A Population-Based Cohort Study. J Clin Med (2021) 10(12). doi: 10.2337/dc20-0576
60. Caussy C, Wallet F, Laville M, Disse E. Obesity is Associated With Severe Forms of COVID-19. Obes (Silver Spring) (2020) 28(7):1175. doi: 10.2337/db20-0671
61. Chetboun M, Raverdy V, Labreuche J, Simonnet A, Wallet F, Caussy C, et al. BMI and Pneumonia Outcomes in Critically Ill Covid-19 Patients: An International Multicenter Study. Obes (Silver Spring) (2021) 29(9):1477–86. doi: 10.1007/s00125-020-05180-x
62. Cho Y, Cho Y, Choi HJ, Lee H, Lim TH, Kang H, et al. The Effect of BMI on COVID-19 Outcomes Among Older Patients in South Korea: A Nationwide Retrospective Cohort Study. Ann Med (2021) 53(1):1292–301. doi: 10.1371/journal.pone.0238905
63. Gregoriano C, Koch D, Haubitz S, Conen A, Fux CA, Mueller B, et al. Characteristics, Predictors and Outcomes Among 99 Patients Hospitalised With COVID-19 in a Tertiary Care Centre in Switzerland: An Observational Analysis. Swiss Med Wkly (2020) 150:w20316. doi: 10.1016/j.numecd.2020.07.031
64. Coss-Rovirosa MF, Aguilar-Soto M, Cuenca D, Velez-Pintado M, Camiro-Zuniga A, Ferreira-Hermosillo A, et al. Are Overweight and Obesity Risk Factors for Invasive Mechanical Ventilation in Severe Coronavirus Disease 2019 Pneumonia? Arch Endocrinol Metab (2021) 65(4):462–7. doi: 10.3390/jcm10122608
65. Cottini M, Lombardi C, Berti A. Primary Care Physicians ATSPoBI. Obesity is a Major Risk Factor for Hospitalization in Community-Managed COVID-19 Pneumonia. Mayo Clin Proc (2021) 96(4):921–31. doi: 10.1002/oby.22842
66. Czernichow S, Beeker N, Rives-Lange C, Guerot E, Diehl JL, Katsahian S, et al. Obesity Doubles Mortality in Patients Hospitalized for Severe Acute Respiratory Syndrome Coronavirus 2 in Paris Hospitals, France: A Cohort Study on 5,795 Patients. Obes (Silver Spring) (2020) 28(12):2282–9. doi: 10.1080/20009666.2020.1830516
67. Dana R, Bannay A, Bourst P, Ziegler C, Losser MR, Gibot S, et al. Obesity and Mortality in Critically Ill COVID-19 Patients With Respiratory Failure. Int J Obes (Lond) (2021) 45(9):2028–37. doi: 10.1177/0885066620946692
68. Dreher M, Kersten A, Bickenbach J, Balfanz P, Hartmann B, Cornelissen C, et al. The Characteristics of 50 Hospitalized COVID-19 Patients With and Without ARDS. Dtsch Arztebl Int (2020) 117(16):271–8. doi: 10.1002/oby.23223
69. Eastment MC, Berry K, Locke E, Green P, O'Hare A, Crothers K, et al. BMI and Outcomes of SARS-CoV-2 Among US Veterans. Obes (Silver Spring) (2021) 29(5):900–8. doi: 10.1080/07853890.2021.1946587
70. Ebinger JE, Achamallah N, Ji H, Claggett BL, Sun N, Botting P, et al. Pre-Existing Traits Associated With Covid-19 Illness Severity. PLoS One (2020) 15(7):e0236240. doi: 10.1016/j.clim.2020.108509
71. Fava A, Cucchiari D, Montero N, Toapanta N, Centellas FJ, Vila-Santandreu A, et al. Clinical Characteristics and Risk Factors for Severe COVID-19 in Hospitalized Kidney Transplant Recipients: A Multicentric Cohort Study. Am J Transplant (2020) 20(11):3030–41. doi: 10.4414/smw.2020.20316
72. Feuth T, Saaresranta T, Karlsson A, Valtonen M, Peltola V, Rintala E, et al. Is Sleep Apnea a Risk Factor for Covid-19? Findings From a Retrospective Cohort Study. Sleep Med Disorders: Int J (2020) 4(3). doi: 10.20945/2359-3997000000350
73. Foulkes AS, Selvaggi C, Shinnick D, Lumish H, Kim E, Cao T, et al. Understanding the Link Between Obesity and Severe COVID-19 Outcomes: Causal Mediation by Systemic Inflammatory Response. J Clin Endocrinol Metab (2022) 107(2):e698–707. doi: 10.1210/clinem/dgab629
74. Fresan U, Guevara M, Elia F, Albeniz E, Burgui C, Castilla J, et al. Independent Role of Severe Obesity as a Risk Factor for COVID-19 Hospitalization: A Spanish Population-Based Cohort Study. Obes (Silver Spring) (2021) 29(1):29–37. doi: 10.1111/ajt.16185
75. Friedman AN, Guirguis J, Kapoor R. Obesity, Inflammatory and Thrombotic Markers, and Major Clinical Outcomes in Critically Ill Patients With COVID-19 in the U.S. Obes (Silver Spring) (2021) 29(10):1719–30. doi: 10.1136/bmjopen-2021-050321
76. Gao F, Zheng KI, Wang XB, Sun QF, Pan KH, Wang TY, et al. Obesity Is a Risk Factor for Greater COVID-19 Severity. Diabetes Care (2020) 43(7):e72–4. doi: 10.1002/oby.23014
77. Di Fusco M, Shea KM, Lin J, Nguyen JL, Angulo FJ, Benigno M, et al. Health Outcomes and Economic Burden of Hospitalized COVID-19 Patients in the United States. J Med Econ (2021) 24(1):308–17. doi: 10.1016/j.ijid.2020.09.037
78. Carrillo G, Méndez-Domínguez N, Santos-Zaldivar KD, Rochel-Pérez A, Azuela-Morales M, Cuevas-Koh O, et al. Clinical Course and Severity Outcome Indicators Among COVID-19 Hospitalized Patients in Relation to Comorbidities Distribution: Mexican Cohort. medRxiv (2020). 2020.2007.2031.20165480. doi: 10.1038/s41366-021-00872-9
79. Gerotziafas GT, Sergentanis TN, Voiriot G, Lassel L, Papageorgiou C, Elabbadi A, et al. Derivation and Validation of a Predictive Score for Disease Worsening in Patients With COVID-19. Thromb Haemost (2020) 120(12):1680–90. doi: 10.1371/journal.pone.0243126
80. Guerson-Gil A, Palaiodimos L, Assa A, Karamanis D, Kokkinidis D, Chamorro-Pareja N, et al. Sex-Specific Impact of Severe Obesity in the Outcomes of Hospitalized Patients With COVID-19: A Large Retrospective Study From the Bronx, New York. Eur J Clin Microbiol Infect Dis (2021) 40(9):1963–74. doi: 10.1136/bmj.m1985
81. Guner R, Hasanoglu I, Kayaaslan B, Aypak A, Kaya Kalem A, Eser F, et al. COVID-19 Experience of the Major Pandemic Response Center in the Capital: Results of the Pandemic's First Month in Turkey. Turk J Med Sci (2020) 50(8):1801–9. doi: 10.3238/arztebl.2020.0271
82. Hajifathalian K, Kumar S, Newberry C, Shah S, Fortune B, Krisko T, et al. Obesity Is Associated With Worse Outcomes in COVID-19: Analysis of Early Data From New York City. Obes (Silver Spring) (2020) 28(9):1606–12. doi: 10.1002/oby.23111
83. Hsu HE, Ashe EM, Silverstein M, Hofman M, Lange SJ, Razzaghi H, et al. Race/Ethnicity, Underlying Medical Conditions, Homelessness, and Hospitalization Status of Adult Patients With COVID-19 at an Urban Safety-Net Medical Center — Boston, Massachusetts, 2020. Centers for Disease Control and Prevention. Morbidity Mortality Weekly Rep (MMWR) (2020). doi: 10.1371/journal.pone.0236240
84. Hur K, Price CPE, Gray EL, Gulati RK, Maksimoski M, Racette SD, et al. Factors Associated With Intubation and Prolonged Intubation in Hospitalized Patients With COVID-19. Otolaryngol Head Neck Surg (2020) 163(1):170–8. doi: 10.1111/ajt.16246
85. Goyal P, Choi JJ, Pinheiro LC, Schenck EJ, Chen R, Jabri A, et al. Clinical Characteristics of Covid-19 in New York City. N Engl J Med (2020) 382(24):2372–4. doi: 10.15406/smdij.2020.04.00075
86. Ioannou GN, Locke E, Green P, Berry K, O'Hare AM, Shah JA, et al. Risk Factors for Hospitalization, Mechanical Ventilation, or Death Among 10131 US Veterans With SARS-CoV-2 Infection. JAMA Netw Open (2020) 3(9):e2022310. doi: 10.1210/clinem/dgab629
87. Jayanama K, Srichatrapimuk S, Thammavaranucupt K, Kirdlarp S, Suppadungsuk S, Wongsinin T, et al. The Association Between Body Mass Index and Severity of Coronavirus Disease 2019 (COVID-19): A Cohort Study. PLoS One (2021) 16(2):e0247023. doi: 10.1002/oby.23029
88. Kaeuffer C, Le Hyaric C, Fabacher T, Mootien J, Dervieux B, Ruch Y, et al. Clinical Characteristics and Risk Factors Associated With Severe COVID-19: Prospective Analysis of 1,045 Hospitalised Cases in North-Eastern France, March 2020. Euro Surveill (2020) 25(48). doi: 10.1002/oby.23245
89. Kang IS, Kong KA. Body Mass Index and Severity/Fatality From Coronavirus Disease 2019: A Nationwide Epidemiological Study in Korea. PLoS One (2021) 16(6):e0253640. doi: 10.1080/13696998.2021.1886109
90. Kompaniyets L, Goodman AB, Belay B, Freedman DS, Sucosky MS, Lange SJ, et al. Body Mass Index and Risk for COVID-19-Related Hospitalization, Intensive Care Unit Admission, Invasive Mechanical Ventilation, and Death - United States, March-December 2020. MMWR Morb Mortal Wkly Rep (2021) 70(10):355–61. doi: 10.2337/dc20-0682
91. Sahin I, Haymana C, Demir T, Demirci I, Tasci I, Atmaca A, et al. Clinical Characteristics and Outcomes of COVID-19 Patients With Overweight and Obesity: Turkish Nationwide Cohort Study (TurCObesity). Exp Clin Endocrinol Diabetes (2022) 130(2):115–24. doi: 10.1055/a-1552-4449.
92. Xie J, Zu Y, Alkhatib A, Pham TT, Gill F, Jang A, et al. Metabolic Syndrome and COVID-19 Mortality Among Adult Black Patients in New Orleans. Diabetes Care (2020) 44(1):188–93. doi: 10.2337/dc20-1714
93. Gao M, Piernas C, Astbury NM, Hippisley-Cox J, O'Rahilly S, Aveyard P, et al. Associations Between Body-Mass Index and COVID-19 Severity in 6.9 Million People in England: A Prospective, Community-Based, Cohort Study. Lancet Diabetes Endocrinol (2021) 9(6):350–9. doi: 10.1055/s-0040-1716544
94. Hu L, Chen S, Fu Y, Gao Z, Long H, Ren HW, et al. Risk Factors Associated With Clinical Outcomes in 323 Coronavirus Disease 2019 (COVID-19) Hospitalized Patients in Wuhan, China. Clin Infect Dis (2020) 71(16):2089–98. doi: 10.1016/j.phrs.2020.104931
95. Iaccarino G, Grassi G, Borghi C, Carugo S, Fallo F, Ferri C, et al. Gender Differences in Predictors of Intensive Care Units Admission Among COVID-19 Patients: The Results of the SARS-RAS Study of the Italian Society of Hypertension. PLoS One (2020) 15(10):e0237297. doi: 10.1371/journal.pone.0237297
96. Le Guen CL, King NA, Zhao H, Renza-Stingone EP, Gerhard GS, Soans RS. COVID-19 Patients With Obesity at Risk for Worse Outcomes Despite Younger Age and Fewer Inflammatory Derangements. Surg Obes Relat Dis (2021) 17(10):1722–30. doi: 10.1155/2021/6667135
97. Lighter J, Phillips M, Hochman S, Sterling S, Johnson D, Francois F, et al. Obesity in Patients Younger Than 60 Years Is a Risk Factor for COVID-19 Hospital Admission. Clin Infect Dis (2020) 71(15):896–7. doi: 10.1007/s10096-021-04260-z
98. Lodigiani C, Iapichino G, Carenzo L, Cecconi M, Ferrazzi P, Sebastian T, et al. Venous and Arterial Thromboembolic Complications in COVID-19 Patients Admitted to an Academic Hospital in Milan, Italy. Thromb Res (2020) 191:9–14. doi: 10.3906/sag-2006-164
99. Martin-Del-Campo F, Ruvalcaba-Contreras N, Velazquez-Vidaurri AL, Cueto-Manzano AM, Rojas-Campos E, Cortes-Sanabria L, et al. Morbid Obesity is Associated With Mortality and Acute Kidney Injury in Hospitalized Patients With COVID-19. Clin Nutr ESPEN (2021) 45:200–5. doi: 10.1186/s12879-021-05782-9
100. Mehanna O, El Askary A, Ali E, El Esawy B, FathAlla T, Gharib AF. Impact of Obesity and Its Associated Comorbid Conditions on COVID-19 Presentation. Diabetes Metab Syndr Obes (2021) 14:409–15. doi: 10.1002/oby.22923
101. Mejia-Vilet JM, Cordova-Sanchez BM, Fernandez-Camargo DA, Mendez-Perez RA, Morales-Buenrostro LE. Hernandez-Gilsoul T. A Risk Score to Predict Admission to the Intensive Care Unit in Patients With COVID-19: The ABC-GOALS Score. Salud Publica Mex. (2020) 63(1, ene-feb):1–11. doi: 10.1177/2047487320939675
102. Mendy A, Apewokin S, Wells AA, Morrow AL. Factors Associated With Hospitalization and Disease Severity in a Racially and Ethnically Diverse Population of COVID-19 Patients. medRxiv (2020). 2020.2006.2025.20137323. doi: 10.1016/j.diabres.2020.108331
103. Monteiro AC, Suri R, Emeruwa IO, Stretch RJ, Cortes-Lopez RY, Sherman A, et al. Obesity and Smoking as Risk Factors for Invasive Mechanical Ventilation in COVID-19: A Retrospective, Observational Cohort Study. PLoS One (2020) 15(12):e0238552. doi: 10.1371/journal.pone.0248580
104. Motaib I, Zbiri S, Elamari S, Dini N, Chadli A, El Kettani C. Obesity and Disease Severity Among Patients With COVID-19. Cureus (2021) 13(2):e13165. doi: 10.15585/mmwr.mm6927a3
105. Mughal MS, Kaur IP, Jaffery AR, Dalmacion DL, Wang C, Koyoda S, et al. COVID-19 Patients in a Tertiary US Hospital: Assessment of Clinical Course and Predictors of the Disease Severity. Respir Med (2020) 172:106130. doi: 10.1177/0194599820929640
106. Nachega JB, Ishoso DK, Otokoye JO, Hermans MP, Machekano RN, Sam-Agudu NA, et al. Clinical Characteristics and Outcomes of Patients Hospitalized for COVID-19 in Africa: Early Insights From the Democratic Republic of the Congo. Am J Trop Med Hyg (2020) 103(6):2419–28. doi: 10.4269/ajtmh.20-1240
107. Nakeshbandi M, Maini R, Daniel P, Rosengarten S, Parmar P, Wilson C, et al. The Impact of Obesity on COVID-19 Complications: A Retrospective Cohort Study. Int J Obes (Lond) (2020) 44(9):1832–7. doi: 10.1371/journal.pone.0247023
108. Kim NH, Kim KJ, Choi J, Kim SG. Metabolically Unhealthy Individuals, Either With Obesity or Not, Have a Higher Risk of Critical Coronavirus Disease 2019 Outcomes Than Metabolically Healthy Individuals Without Obesity. Metabolism 2021:154894. doi: 10.1016/j.metabol.2021.154894
109. Newton S, Zollinger B, Freeman J, Moran S, Helfand A, Authelet K, et al. Factors Associated With Clinical Severity in Emergency Department Patients Presenting With Symptomatic SARS-CoV-2 Infection. medRxiv (2020). 2020.2012.2008.20246017. doi: 10.2807/1560-7917.ES.2020.25.48.2000895
110. Okauchi Y, Matsuno K, Nishida T, Sawada K, Kawasaki A, Ito N, et al. Obesity, Glucose Intolerance, Advanced Age, and Lymphocytopenia are Independent Risk Factors for Oxygen Requirement in Japanese Patients With Coronavirus Disease 2019 (COVID-19). Endocr J (2021) 68(7):849–56. doi: 10.1016/j.clnu.2021.12.027
111. Ortiz-Brizuela E, Villanueva-Reza M, Gonzalez-Lara MF, Tamez-Torres KM, Roman-Montes CM, Diaz-Mejia BA, et al. Clinical and Epidemiological Characteristics of Patients Diagnosed With Covid-19 in a Tertiary Care Center in Mexico City: A Prospective Cohort Study. Rev Invest Clin (2020) 72(3):165–77. doi: 10.1371/journal.pone.0253640
112. Page-Wilson G, Arakawa R, Nemeth S, Bell F, Girvin Z, Tuohy MC, et al. Obesity is Independently Associated With Septic Shock, Renal Complications, and Mortality in a Multiracial Patient Cohort Hospitalized With COVID-19. PLoS One (2021) 16(8):e0255811. doi: 10.1093/cid/ciaa1097
113. Palaiodimos L, Kokkinidis DG, Li W, Karamanis D, Ognibene J, Arora S, et al. Severe Obesity, Increasing Age and Male Sex are Independently Associated With Worse in-Hospital Outcomes, and Higher in-Hospital Mortality, in a Cohort of Patients With COVID-19 in the Bronx, New York. Metabolism (2020) 108:154262. doi: 10.1016/j.metabol.2021.154894
114. Pepe M, Maroun-Eid C, Romero R, Arroyo-Espliguero R, Fernandez-Rozas I, Aparisi A, et al. Clinical Presentation, Therapeutic Approach, and Outcome of Young Patients Admitted for COVID-19, With Respect to the Elderly Counterpart. Clin Exp Med (2021) 21(2):249–68. doi: 10.1002/oby.23076
115. Petersen A, Bressem K, Albrecht J, Thiess HM, Vahldiek J, Hamm B, et al. The Role of Visceral Adiposity in the Severity of COVID-19: Highlights From a Unicenter Cross-Sectional Pilot Study in Germany. Metabolism (2020) 110:154317. doi: 10.3390/ijerph17249336
116. Petrilli CM, Jones SA, Yang J, Rajagopalan H, O'Donnell L, Chernyak Y, et al. Factors Associated With Hospital Admission and Critical Illness Among 5279 People With Coronavirus Disease 2019 in New York City: Prospective Cohort Study. BMJ (2020) 369:m1966. doi: 10.1002/oby.22913
117. Pettit NN, MacKenzie EL, Ridgway JP, Pursell K, Ash D, Patel B, et al. Obesity is Associated With Increased Risk for Mortality Among Hospitalized Patients With COVID-19. Obes (Silver Spring) (2020) 28(10):1806–10. doi: 10.15585/mmwr.mm7010e4
118. Pietri L, Giorgi R, Begu A, Lojou M, Koubi M, Cauchois R, et al. Excess Body Weight Is an Independent Risk Factor for Severe Forms of COVID-19. Metabolism (2021) 117:154703. doi: 10.1038/s41366-021-00747-z
119. Plataki M, Pan D, Goyal P, Hoffman K, Choi JMK, Huang H, et al. Association of Body Mass Index With Morbidity in Patients Hospitalised With COVID-19. BMJ Open Respir Res (2021) 8(1). doi: 10.1097/CCM.0000000000005216
120. Plourde G, Fournier-Ross E, Tessier-Grenier H, Mullie LA, Chasse M, Carrier FM. Association Between Obesity and Hospital Mortality in Critical COVID-19: A Retrospective Cohort Study. Int J Obes (Lond) (2021) 45(12):2617–22. doi: 10.1371/journal.pone.0237297
121. Pongpirul WA, Wiboonchutikul S, Charoenpong L, Panitantum N, Vachiraphan A, Uttayamakul S, et al. Clinical Course and Potential Predictive Factors for Pneumonia of Adult Patients With Coronavirus Disease 2019 (COVID-19): A Retrospective Observational Analysis of 193 Confirmed Cases in Thailand. PLoS Negl Trop Dis (2020) 14(10):e0008806. doi: 10.1177/00220345211029638
122. Pouwels S, Ramnarain D, Aupers E, Rutjes-Weurding L, van Oers J. Obesity May Not Be Associated With 28-Day Mortality, Duration of Invasive Mechanical Ventilation and Length of Intensive Care Unit and Hospital Stay in Critically Ill Patients With Severe Acute Respiratory Syndrome Coronavirus-2: A Retrospective Cohort Study. Medicina (Kaunas) (2021) 57(7). doi: 10.1016/j.soard.2021.06.006
123. Frank RC, Mendez SR, Stevenson EK, Guseh JS, Chung M, Silverman MG. Obesity and the Risk of Intubation or Death in Patients With Coronavirus Disease 2019. Crit Care Med (2020) 48(11):e1097–101. doi: 10.1093/cid/ciaa415
124. Kim SY, Yoo DM, Min C, Wee JH, Kim JH, Choi HG. Analysis of Mortality and Morbidity in COVID-19 Patients With Obesity Using Clinical Epidemiological Data From the Korean Center for Disease Control & Prevention. Int J Environ Res Public Health (2020) 17(24). doi: 10.1093/cid/ciaa539
125. Ramlall V, Thangaraj PM, Meydan C, Foox J, Butler D, Kim J, et al. Immune Complement and Coagulation Dysfunction in Adverse Outcomes of SARS-CoV-2 Infection. Nat Med (2020) 26(10):1609–15. doi: 10.1016/j.thromres.2020.04.024
126. Randhawa G, Syed KA, Singh K, Kundal SV, Oli S, Silver M, et al. The Relationship Between Obesity, Hemoglobin A1c and the Severity of COVID-19 at an Urban Tertiary Care Center in New York City: A Retrospective Cohort Study. BMJ Open (2021) 11(1):e044526. doi: 10.1101/2020.05.29.20086645
127. Rao X, Wu C, Wang S, Tong S, Wang G, Wu G, et al. The Importance of Overweight in COVID-19: A Retrospective Analysis in a Single Center of Wuhan, China. Med (Baltimore) (2020) 99(43):e22766. doi: 10.1016/j.clnesp.2021.08.027
128. Recalde M, Roel E, Pistillo A, Sena AG, Prats-Uribe A, Ahmed WU, et al. Characteristics and Outcomes of 627 044 COVID-19 Patients Living With and Without Obesity in the United States, Spain, and the United Kingdom. Int J Obes (Lond) (2021) 45(11):2347–57. doi: 10.2147/DMSO.S287779
129. Reilev M, Kristensen KB, Pottegard A, Lund LC, Hallas J, Ernst MT, et al. Characteristics and Predictors of Hospitalization and Death in the First 11 122 Cases With a Positive RT-PCR Test for SARS-CoV-2 in Denmark: A Nationwide Cohort. Int J Epidemiol (2020) 49(5):1468–81. doi: 10.1001/jamanetworkopen.2021.6315
130. Rodriguez-Molinero A, Galvez-Barron C, Minarro A, Macho O, Lopez GF, Robles MT, et al. Association Between COVID-19 Prognosis and Disease Presentation, Comorbidities and Chronic Treatment of Hospitalized Patients. PLoS One (2020) 15(10):e0239571. doi: 10.1371/journal.pone.0239571
131. Rottoli M, Bernante P, Belvedere A, Balsamo F, Garelli S, Giannella M, et al. How Important Is Obesity as a Risk Factor for Respiratory Failure, Intensive Care Admission and Death in Hospitalised COVID-19 Patients? Results From a Single Italian Centre. Eur J Endocrinol (2020) 183(4):389–97. doi: 10.1101/2020.06.25.20137323
132. Sahin S, Sezer H, Cicek E, Yagiz Ozogul Y, Yildirim M, Icli TB, et al. The Role of Obesity in Predicting the Clinical Outcomes of COVID-19. Obes Facts (2021) 14(5):481–9. doi: 10.4269/ajtmh.20-0483
133. Saito T, Yamaguchi T, Kuroda S, Kitai T, Yonetsu T, Kohsaka S, et al. Impact of Body Mass Index on the Outcome of Japanese Patients With Cardiovascular Diseases and/or Risk Factors Hospitalized With COVID-19 Infection. J Cardiol (2021). doi: 10.1007/s11606-020-05983-z
134. Shaikh FS, Aldhafferi N, Buker A, Alqahtani A, Dey S, Abdulhamid S, et al. Comorbidities and Risk Factors for Severe Outcomes in COVID-19 Patients in Saudi Arabia: A Retrospective Cohort Study. J Multidiscip Healthc (2021) 14:2169–83. doi: 10.1371/journal.pone.0238552
135. Shekhar R, Sheikh AB, Upadhyay S, Atencio J, Kapuria D. Early Experience With COVID-19 Patients at Academic Hospital in Southwestern United States. Infect Dis (Lond) (2020) 52(8):596–9. doi: 10.7759/cureus.13165
136. Silva NJ, Ribeiro-Silva RC, Ferreira AJF, Teixeira CSS, Rocha AS, Alves FJO, et al. Combined Association of Obesity and Other Cardiometabolic Diseases With Severe COVID-19 Outcomes: A Nationwide Cross-Sectional Study of 21 773 Brazilian Adult and Elderly Inpatients. BMJ Open (2021) 11(8):e050739. doi: 10.1016/j.rmed.2020.106130
137. Simonnet A, Chetboun M, Poissy J, Raverdy V, Noulette J, Duhamel A, et al. High Prevalence of Obesity in Severe Acute Respiratory Syndrome Coronavirus-2 (SARS-CoV-2) Requiring Invasive Mechanical Ventilation. Obes (Silver Spring) (2020) 28(7):1195–9. doi: 10.1016/j.puhe.2020.10.029
138. Kim TS, Roslin M, Wang JJ, Kane J, Hirsch JS, Kim EJ, et al. BMI as a Risk Factor for Clinical Outcomes in Patients Hospitalized With COVID-19 in New York. Obes (Silver Spring) (2021) 29(2):279–84. doi: 10.7759/cureus.15235
139. Steinberg E, Wright E, Kushner B. In Young Adults With COVID-19, Obesity Is Associated With Adverse Outcomes. West J Emerg Med (2020) 21(4):752–5. doi: 10.4269/ajtmh.20-1240
140. Suleyman G, Fadel RA, Malette KM, Hammond C, Abdulla H, Entz A, et al. Clinical Characteristics and Morbidity Associated With Coronavirus Disease 2019 in a Series of Patients in Metropolitan Detroit. JAMA Netw Open (2020) 3(6):e2012270. doi: 10.1038/s41366-020-0648-x
141. Suresh S, Siddiqui M, Abu Ghanimeh M, Jou J, Simmer S, Mendiratta V, et al. Association of Obesity With Illness Severity in Hospitalized Patients With COVID-19: A Retrospective Cohort Study. Obes Res Clin Pract (2021) 15(2):172–6. doi: 10.1101/2020.12.08.20246017
142. Tchang BG, Askin G, Sahagun A, Hwang J, Huang H, Mendelsohn Curanaj FA, et al. The Independent Risk of Obesity and Diabetes and Their Interaction in COVID-19: A Retrospective Cohort Study. Obes (Silver Spring) (2021) 29(6):971–5. doi: 10.1507/endocrj.EJ20-0784
143. Terada M, Ohtsu H, Saito S, Hayakawa K, Tsuzuki S, Asai Y, et al. Risk Factors for Severity on Admission and the Disease Progression During Hospitalisation in a Large Cohort of Patients With COVID-19 in Japan. BMJ Open (2021) 11(6):e047007. doi: 10.1016/j.toxrep.2021.07.020
144. Tonetti T, Grasselli G, Zanella A, Pizzilli G, Fumagalli R, Piva S, et al. Use of Critical Care Resources During the First 2 Weeks (February 24-March 8, 2020) of the Covid-19 Outbreak in Italy. Ann Intensive Care (2020) 10(1):133. doi: 10.1371/journal.pone.0245772
145. Urra JM, Cabrera CM, Porras L, Rodenas I. Selective CD8 Cell Reduction by SARS-CoV-2 Is Associated With a Worse Prognosis and Systemic Inflammation in COVID-19 Patients. Clin Immunol (2020) 217:108486. doi: 10.1371/journal.pone.0249038
146. Vaquero-Roncero LM, Sánchez-Barrado E, Escobar-Macias D, Arribas-Pérez P, Gonzalez-Porras JR, Bermejo-Martín JF, et al. C-Reactive Protein and SOFA Score as Early Predictors of Critical Care Requirement in Patients With COVID-19 Pneumonia in Spain. medRxiv (2020) 2005:2022. doi: 10.1101/2020.05.22.20110429
147. Vera-Zertuche JM, Mancilla-Galindo J, Tlalpa-Prisco M, Aguilar-Alonso P, Aguirre-Garcia MM, Segura-Badilla O, et al. Obesity Is a Strong Risk Factor for Short-Term Mortality and Adverse Outcomes in Mexican Patients With COVID-19: A National Observational Study. Epidemiol Infect (2021) 149:e109. doi: 10.1371/journal.pone.0255811
148. Wang J, Zhu L, Liu L, Zhao XA, Zhang Z, Xue L, et al. Overweight and Obesity are Risk Factors of Severe Illness in Patients With COVID-19. Obes (Silver Spring) (2020) 28(11):2049–55. doi: 10.1016/j.metabol.2020.154262
149. Wu X, Li C, Chen S, Zhang X, Wang F, Shi T, et al. Association of Body Mass Index With Severity and Mortality of COVID-19 Pneumonia: A Two-Center, Retrospective Cohort Study From Wuhan, China. Aging (Albany NY) (2021) 13(6):7767–80. doi: 10.7196/SAMJ.2020.v110i10.15067
150. Min W, Fang Y, Xinxin Z, Chuanfang C, Qi L, Tao Z, et al. Clinical Characteristics and Outcomes of Patients With New Coronavirus Pneumonia With Different Body Mass Indexes. Chin J Endocrinol Metab (2020) 36. doi: 10.1016/j.annepidem.2020.08.005
151. Wang R, Xie L, Du P, Fan H, Song M. Clinical Characteristics of 96 Hospitalized Patients With Coronavirus Disease 2019. Chin J Respir Crit Care Med (2020) 19(2):144–7. doi: 10.1186/s12902-021-00805-7
152. Ong SWX, Young BE, Leo YS, Lye DC. Association of Higher Body Mass Index With Severe Coronavirus Disease 2019 (COVID-19) in Younger Patients. Clin Infect Dis (2020) 71(16):2300–2. doi: 10.1016/j.arcmed.2020.12.002
153. Yates T, Razieh C, Zaccardi F, Rowlands AV, Seidu S, Davies MJ, et al. Obesity, Walking Pace and Risk of Severe COVID-19 and Mortality: Analysis of UK Biobank. Int J Obes (Lond) (2021) 45(5):1155–9. doi: 10.1038/s41366-021-00771-z
154. Zhu Z, Hasegawa K, Ma B, Fujiogi M, Camargo CA Jr., Liang L. Association of Obesity and Its Genetic Predisposition With the Risk of Severe COVID-19: Analysis of Population-Based Cohort Data. Metabolism (2020) 112:154345. doi: 10.1007/s10238-021-00684-1
155. Zhang J, Xu Y, Shen B, He H, Liu M, Zhao M, et al. The Association Between Obesity and Severity in Patients With Coronavirus Disease 2019: A Retrospective, Single-Center Study, Wuhan. Int J Med Sci (2021) 18(8):1768–77. doi: 10.1016/j.metabol.2020.154317
156. Zheng KI, Gao F, Wang XB, Sun QF, Pan KH, Wang TY, et al. Letter to the Editor: Obesity as a Risk Factor for Greater Severity of COVID-19 in Patients With Metabolic Associated Fatty Liver Disease. Metabolism (2020) 108:154244. doi: 10.1136/bmj.m1966
157. Anderson MR, Geleris J, Anderson DR, Zucker J, Nobel YR, Freedberg D, et al. Body Mass Index and Risk for Intubation or Death in SARS-CoV-2 Infection : A Retrospective Cohort Study. Ann Intern Med (2020) 173(10):782–90. doi: 10.1002/oby.22941
158. Rossi AP, Gottin L, Donadello K, Schweiger V, Nocini R, Taiana M, et al. Obesity as a Risk Factor for Unfavourable Outcomes in Critically Ill Patients Affected by Covid 19. Nutr Metab Cardiovasc Dis (2021) 31(3):762–8. doi: 10.1101/2020.08.12.20156257
159. Bellan M, Patti G, Hayden E, Azzolina D, Pirisi M, Acquaviva A, et al. Fatality Rate and Predictors of Mortality in an Italian Cohort of Hospitalized COVID-19 Patients. Sci Rep (2020) 10(1):20731. doi: 10.1016/j.metabol.2021.154703
160. Bellini B, Cresci B, Cosentino C, Profili F, Bartolacci S, Scoccimarro D, et al. Obesity as a Risk Factor for Hospitalization in COronaVirus Disease-19 (COVID-19) Patients: Analysis of the Tuscany Regional Database. Nutr Metab Cardiovasc Dis (2021) 31(3):769–73. doi: 10.1136/bmjresp-2021-000970
161. Borobia AM, Carcas AJ, Arnalich F, Alvarez-Sala R, Monserrat-Villatoro J, Quintana M, et al. A Cohort of Patients With COVID-19 in a Major Teaching Hospital in Europe. J Clin Med (2020) 9(6). doi: 10.1038/s41366-021-00938-8
162. Cariou B, Hadjadj S, Wargny M, Pichelin M, Al-Salameh A, Allix I, et al. Phenotypic Characteristics and Prognosis of Inpatients With COVID-19 and Diabetes: The CORONADO Study. Diabetologia (2020) 63(8):1500–15. doi: 10.1371/journal.pntd.0008806
163. Carrillo-Vega MF, Salinas-Escudero G, Garcia-Pena C, Gutierrez-Robledo LM, Parra-Rodriguez L. Early Estimation of the Risk Factors for Hospitalization and Mortality by COVID-19 in Mexico. PLoS One (2020) 15(9):e0238905. doi: 10.3390/medicina57070674
164. Di Castelnuovo A, Bonaccio M, Costanzo S, Gialluisi A, Antinori A, Berselli N, et al. Common Cardiovascular Risk Factors and in-Hospital Mortality in 3,894 Patients With COVID-19: Survival Analysis and Machine Learning-Based Findings From the Multicentre Italian CORIST Study. Nutr Metab Cardiovasc Dis (2020) 30(11):1899–913. doi: 10.1097/CCM.0000000000004553
165. Cedano J, Fabian Corona E, Gonzalez-Lara M, Santana M, Younes I, Ayad S, et al. Characteristics and Outcomes of Patients With COVID-19 in an Intensive Care Unit of a Community Hospital; Retrospective Cohort Study. J Community Hosp Intern Med Perspect (2021) 11(1):27–32. doi: 10.1038/s41591-020-1021-2
166. Chand S, Kapoor S, Orsi D, Fazzari MJ, Tanner TG, Umeh GC, et al. COVID-19-Associated Critical Illness-Report of the First 300 Patients Admitted to Intensive Care Units at a New York City Medical Center. J Intensive Care Med (2020) 35(10):963–70. doi: 10.1177/0885066620946692
167. Ciceri F, Castagna A, Rovere-Querini P, De Cobelli F, Ruggeri A, Galli L, et al. Early Predictors of Clinical Outcomes of COVID-19 Outbreak in Milan, Italy. Clin Immunol (2020) 217:108509. doi: 10.1097/MD.0000000000022766
168. Cravedi P, Mothi SS, Azzi Y, Haverly M, Farouk SS, Perez-Saez MJ, et al. COVID-19 and Kidney Transplantation: Results From the TANGO International Transplant Consortium. Am J Transplant (2020) 20(11):3140–8. doi: 10.1038/s41366-021-00893-4
169. Cueto-Manzano AM, Espinel-Bermudez MC, Hernandez-Gonzalez SO, Rojas-Campos E, Nava-Zavala AH, Fuentes-Orozco C, et al. Risk Factors for Mortality of Adult Patients With COVID-19 Hospitalised in an Emerging Country: A Cohort Study. BMJ Open (2021) 11(7):e050321. doi: 10.1093/ije/dyaa140
170. d'Arminio Monforte A, Tavelli A, Bai F, Tomasoni D, Falcinella C, Castoldi R, et al. The Importance of Patients' Case-Mix for the Correct Interpretation of the Hospital Fatality Rate in COVID-19 Disease. Int J Infect Dis (2020) 100:67–74. doi: 10.1016/j.medin.2020.05.018
171. de Andrade CLT, de Aguiar Pereira CC, Martins M, Lima SML, Portela MC. COVID-19 Hospitalizations in Brazil's Unified Health System (SUS). PLoS One (2020) 15(12):e0243126. doi: 10.1371/journal.pone.0239571
172. Docherty AB, Harrison EM, Green CA, Hardwick HE, Pius R, Norman L, et al. Features of 20 133 UK Patients in Hospital With Covid-19 Using the ISARIC WHO Clinical Characterisation Protocol: Prospective Observational Cohort Study. BMJ (2020) 369:m1985. doi: 10.1016/j.mayocpiqo.2020.10.007
173. Giacomelli A, Ridolfo AL, Milazzo L, Oreni L, Bernacchia D, Siano M, et al. 30-Day Mortality in Patients Hospitalized With COVID-19 During the First Wave of the Italian Epidemic: A Prospective Cohort Study. Pharmacol Res (2020) 158:104931. doi: 10.1530/EJE-20-0541
174. Giorgi Rossi P, Marino M, Formisano D, Venturelli F, Vicentini M, Grilli R, et al. Characteristics and Outcomes of a Cohort of COVID-19 Patients in the Province of Reggio Emilia, Italy. PLoS One (2020) 15(8):e0238281. doi: 10.1371/journal.pone.0238281
175. Goncalves DA, Ribeiro V, Gualberto A, Peres F, Luconi M, Gameiro J. COVID-19 and Obesity: An Epidemiologic Analysis of the Brazilian Data. Int J Endocrinol (2021) 2021:6667135. doi: 10.1055/a-1552-4449
176. Gupta R, Agrawal R, Bukhari Z, Jabbar A, Wang D, Diks J, et al. Higher Comorbidities and Early Death in Hospitalized African-American Patients With Covid-19. BMC Infect Dis (2021) 21(1):78. doi: 10.1016/j.jjcc.2021.09.013
177. Halasz G, Leoni MLG, Villani GQ, Nolli M, Villani M. Obesity, Overweight and Survival in Critically Ill Patients With SARS-CoV-2 Pneumonia: Is There an Obesity Paradox? Preliminary Results From Italy. Eur J Prev Cardiol (2021) 28(9):e15–7. doi: 10.1002/jmv.26252
178. Halvatsiotis P, Kotanidou A, Tzannis K, Jahaj E, Magira E, Theodorakopoulou M, et al. Demographic and Clinical Features of Critically Ill Patients With COVID-19 in Greece: The Burden of Diabetes and Obesity. Diabetes Res Clin Pract (2020) 166:108331. doi: 10.1016/j.diabres.2020.108331
179. de Souza FSH, Hojo-Souza NS, Batista BDO, da Silva CM, Guidoni DL. On the Analysis of Mortality Risk Factors for Hospitalized COVID-19 Patients: A Data-Driven Study Using the Major Brazilian Database. PLoS One (2021) 16(3):e0248580. doi: 10.3390/jcm10061176
180. Kananen L, Eriksdotter M, Bostrom AM, Kivipelto M, Annetorp M, Metzner C, et al. Body Mass Index and Mini Nutritional Assessment-Short Form as Predictors of in-Geriatric Hospital Mortality in Older Adults With COVID-19. Clin Nutr (2021). doi: 10.1080/07853890.2020.1791356
181. Kates OS, Haydel BM, Florman SS, Rana MM, Chaudhry ZS, Ramesh MS, et al. Coronavirus Disease 2019 in Solid Organ Transplant: A Multicenter Cohort Study. Clin Infect Dis (2021) 73(11):e4090–9. doi: 10.2147/JMDH.S317884
182. Klang E, Kassim G, Soffer S, Freeman R, Levin MA, Reich DL. Severe Obesity as an Independent Risk Factor for COVID-19 Mortality in Hospitalized Patients Younger Than 50. Obes (Silver Spring) (2020) 28(9):1595–9. doi: 10.1080/23744235.2020.1774645
183. Kooistra EJ, Brinkman S, van der Voort PHJ, de Keizer NF, Dongelmans DA, Kox M, et al. Body Mass Index and Mortality in Coronavirus Disease 2019 and Other Diseases: A Cohort Study in 35,506 ICU Patients. Crit Care Med (2022) 50(1):e1–e10. doi: 10.1136/bmjopen-2021-050739
184. Kooistra EJ, de Nooijer AH, Claassen WJ, Grondman I, Janssen NAF, Netea MG, et al. A Higher BMI Is Not Associated With a Different Immune Response and Disease Course in Critically Ill COVID-19 Patients. Int J Obes (Lond) (2021) 45(3):687–94. doi: 10.1002/oby.22831
185. Larvin H, Wilmott S, Kang J, Aggarwal VR, Pavitt S, Wu J. Additive Effect of Periodontal Disease and Obesity on COVID-19 Outcomes. J Dent Res (2021) 100(11):1228–35. doi: 10.5811/westjem.2020.5.47972
186. Kalyanaraman Marcello R, Dolle J, Grami S, Adule R, Li Z, Tatem K, et al. Characteristics and Outcomes of COVID-19 Patients in New York City's Public Hospital System. PLoS One (2020) 15(12):e0243027. doi: 10.1001/jamanetworkopen.2020.12270
187. Mehta HB, Li S, Goodwin JS. Risk Factors Associated With SARS-CoV-2 Infections, Hospitalization, and Mortality Among US Nursing Home Residents. JAMA Netw Open (2021) 4(3):e216315. doi: 10.1016/j.orcp.2021.02.006
188. Soares RCM, Mattos LR, Raposo LM. Risk Factors for Hospitalization and Mortality Due to COVID-19 in Espirito Santo State, Brazil. Am J Trop Med Hyg (2020) 103(3):1184–90. doi: 10.1002/oby.23172
189. Mikami T, Miyashita H, Yamada T, Harrington M, Steinberg D, Dunn A, et al. Risk Factors for Mortality in Patients With COVID-19 in New York City. J Gen Intern Med (2021) 36(1):17–26. doi: 10.1016/j.ijid.2020.10.071
190. Murillo-Zamora E, Hernandez-Suarez CM. Survival in Adult Inpatients With COVID-19. Public Health (2021) 190:1–3. doi: 10.1136/bmjopen-2020-047007
191. Naaraayan A, Nimkar A, Pant S, Hasan A, Durdevic M, Elenius H, et al. Sex Disparity in the Effect of Obesity in Hospitalized COVID-19 Patients: A Retrospective Cohort Study From the New York City Metropolitan Area. Cureus (2021) 13(5):e15235. doi: 10.1186/s13613-020-00750-z
192. Olak AS, Susuki AM, Kanashiro M, Paoliello MMB, Aschner M, Urbano MR. Risk Factors Associated With COVID-19-Induced Death in Patients Hospitalized in Intensive Care Units (ICUs) in a City in Southern Brazil. Toxicol Rep (2021) 8:1565–8. doi: 10.1016/j.clim.2020.108486
193. Olivas-Martinez A, Cardenas-Fragoso JL, Jimenez JV, Paoliello MMB, Aschner M, Urbano MR, et al. In-Hospital Mortality From Severe COVID-19 in a Tertiary Care Center in Mexico City; Causes of Death, Risk Factors and the Impact of Hospital Saturation. PLoS One (2021) 16(2):e0245772. doi: 10.1101/2020.05.22.20110429
194. Oliveira E, Parikh A, Lopez-Ruiz A, Lozano-Cruz OA, Ortiz-Brizuela E, Tovar-Mendez VH, et al. ICU Outcomes and Survival in Patients With Severe COVID-19 in the Largest Health Care System in Central Florida. PLoS One (2021) 16(3):e0249038. doi: 10.1017/S0950268821001023
195. Parker A, Koegelenberg CFN, Moolla MS, et al. High HIV Prevalence in an Early Cohort of Hospital Admissions With COVID-19 in Cape Town, South Africa. S Afr Med J (2020) 110(10):982–7. doi: 10.1002/oby.22979
196. Parra-Bracamonte GM, Lopez-Villalobos N, Parra-Bracamonte FE. Clinical Characteristics and Risk Factors for Mortality of Patients With COVID-19 in a Large Data Set From Mexico. Ann Epidemiol (2020) 52:93–8.e92. doi: 10.1016/j.annepidem.2020.08.005
197. Patel KHK, Li X, Quint JK, Ware JS, Peters NS, Ng FS. Increasing Adiposity and the Presence of Cardiometabolic Morbidity is Associated With Increased Covid-19-Related Mortality: Results From the UK Biobank. BMC Endocr Disord (2021) 21(1):144. doi: 10.1186/s12902-021-00805-7
198. Pena JE, Rascon-Pacheco RA, Ascencio-Montiel IJ, Gonzalez-Figueroa E, Fernandez-Garate JE, Medina-Gomez OS, et al. Hypertension, Diabetes and Obesity, Major Risk Factors for Death in Patients With COVID-19 in Mexico. Arch Med Res (2021) 52(4):443–9. doi: 10.18632/aging.202813
199. Peng YD, Meng K, Guan HQ, Leng L, Zhu RR, Wang BY, et al. Clinical Characteristics and Outcomes of 112 Cardiovascular Disease Patients Infected by 2019-Ncov. Zhonghua Xin Xue Guan Bing Za Zhi (2020) 48(6):450–5. doi: 10.1093/cid/ciaa548
200. Philipose Z, Smati N, Wong CSJ, Aspey K, Mendall M. Obesity, Old Age, and Frailty are the True Risk Factors for COVID-19 Mortality and Not Chronic Disease or Ethnicity. MedRxiv (2020). doi: 10.1038/s41366-021-00771-z
201. Rodriguez A, Moreno G, Gomez J, Carbonell R, Pico-Plana E, Benavent Bofill C, et al. Severe Infection Due to the SARS-CoV-2 Coronavirus: Experience of a Tertiary Hospital With COVID-19 Patients During the 2020 Pandemic. Med Intensiva (Engl Ed). (2020) 44(9):525–33. doi: 10.7150/ijms.54655
202. Rodriguez-Nava G, Yanez-Bello MA, Trelles-Garcia DP, Chung CW, Chaudry S, Khan AS, et al. Clinical Characteristics and Risk Factors for Death of Hospitalized Patients With COVID-19 in a Community Hospital: A Retrospective Cohort Study. Mayo Clin Proc Innov Qual Outcomes (2021) 5(1):1–10. doi: 10.1016/j.metabol.2020.154244
203. Salacup G, Lo KB, Gul F, Peterson E, De Joy R, Bhargav R, et al. Characteristics and Clinical Outcomes of COVID-19 Patients in an Underserved-Inner City Population: A Single Tertiary Center Cohort. J Med Virol (2021) 93(1):416–23. doi: 10.1016/j.metabol.2020.154345
204. Sardinha DM, Do Socorro Pompeu De Loiola R, Ferreira A, de Sa CAF, Rodrigues YC, Lima KVB, et al. Risk Factors Associated With the Severity of COVID-19 in a Region of the Brazilian Amazon. Sci Rep (2021) 11(1):20569. doi: 10.1038/s41598-021-00009-y
205. Shah P, Owens J, Franklin J, Mehta A, Heymann W, Sewell W, et al. Demographics, Comorbidities and Outcomes in Hospitalized Covid-19 Patients in Rural Southwest Georgia. Ann Med (2020) 52(7):354–60. doi: 10.1080/07853890.2020.1791356
206. Schavemaker R, Schultz MJ, Lagrand WK, van Slobbe-Bijlsma ER, Serpa Neto A, Paulus F, et al. Associations of Body Mass Index With Ventilation Management and Clinical Outcomes in Invasively Ventilated Patients With ARDS Related to COVID-19-Insights From the PRoVENT-COVID Study. J Clin Med (2021) 10(6). doi: 10.3390/jcm10061176
207. Tehrani S, Killander A, Astrand P, Jakobsson J, Gille-Johnson P. Risk Factors for Death in Adult COVID-19 Patients: Frailty Predicts Fatal Outcome in Older Patients. Int J Infect Dis (2021) 102:415–21. doi: 10.1056/NEJMc2010419
208. Akinnusi ME, Pineda LA, El Solh AA. Effect of Obesity on Intensive Care Morbidity and Mortality: A Meta-Analysis. Crit Care Med (2008) 36(1):151–8. doi: 10.1097/01.CCM.0000297885.60037.6E
209. Hogue CW Jr., Stearns JD, Colantuoni E, Robinson KA, Stierer T, Mitter N, et al. The Impact of Obesity on Outcomes After Critical Illness: A Meta-Analysis. Intensive Care Med (2009) 35(7):1152–70. doi: 10.1007/s00134-009-1424-5
210. Oliveros H, Villamor E. Obesity and Mortality in Critically Ill Adults: A Systematic Review and Meta-Analysis. Obes (Silver Spring) (2008) 16(3):515–21. doi: 10.1038/oby.2007.102
211. Zhao Y, Li Z, Yang T, Wang M, Xi X. Is Body Mass Index Associated With Outcomes of Mechanically Ventilated Adult Patients in Intensive Critical Units? A Systematic Review and Meta-Analysis. PLoS One (2018) 13(6):e0198669. doi: 10.1371/journal.pone.0198669
212. Foldi M, Farkas N, Kiss S, Dembrovszky F, Szakacs Z, Balasko M, et al. Visceral Adiposity Elevates the Risk of Critical Condition in COVID-19: A Systematic Review and Meta-Analysis. Obes (Silver Spring) (2021) 29(3):521–8. doi: 10.1002/oby.23096
213. Poly TN, Islam MM, Yang HC, Lin MC, Jian WS, Hsu MH, et al. Obesity and Mortality Among Patients Diagnosed With COVID-19: A Systematic Review and Meta-Analysis. Front Med (Lausanne) (2021) 8(28):620044. doi: 10.3389/fmed.2021.620044
214. Aghili SMM, Ebrahimpur M, Arjmand B, Shadman Z, Pejman Sani M, Qorbani M, et al. Obesity in COVID-19 Era, Implications for Mechanisms, Comorbidities, and Prognosis: A Review and Meta-Analysis. Int J Obes (Lond) (2021) 45(5):998–1016. doi: 10.1038/s41366-021-00776-8
215. Booth A, Reed AB, Ponzo S, Yassaee A, Aral M, Plans D, et al. Population Risk Factors for Severe Disease and Mortality in COVID-19: A Global Systematic Review and Meta-Analysis. PLoS One (2021) 16(3):e0247461. doi: 10.1371/journal.pone.0247461
216. Ng WH, Tipih T, Makoah NA, Vermeulen JG, Goedhals D, Sempa JB, et al. Comorbidities in SARS-CoV-2 Patients: A Systematic Review and Meta-Analysis. mBio (2021) 12(1). doi: 10.1128/mBio.03647-20
217. Yang J, Tian C, Chen Y, Zhu C, Chi H, Li J. Obesity Aggravates COVID-19: An Updated Systematic Review and Meta-Analysis. J Med Virol (2021) 93(5):2662–74. doi: 10.1002/jmv.26677
218. Mesas AE, Cavero-Redondo I, Alvarez-Bueno C, Sarria Cabrera MA, Maffei de Andrade S, Sequi-Dominguez I, et al. Predictors of in-Hospital COVID-19 Mortality: A Comprehensive Systematic Review and Meta-Analysis Exploring Differences by Age, Sex and Health Conditions. PLoS One (2020) 15(11):e0241742. doi: 10.1371/journal.pone.0241742
219. Soeroto AY, Soetedjo NN, Purwiga A, Santoso P, Kulsum ID, Suryadinata H, et al. Effect of Increased BMI and Obesity on the Outcome of COVID-19 Adult Patients: A Systematic Review and Meta-Analysis. Diabetes Metab Syndr (2020) 14(6):1897–904. doi: 10.1016/j.dsx.2020.09.029
220. Cai Z, Yang Y, Zhang J. Obesity is Associated With Severe Disease and Mortality in Patients With Coronavirus Disease 2019 (COVID-19): A Meta-Analysis. BMC Public Health (2021) 21(1):1505. doi: 10.1186/s12889-021-11546-6
221. Du Y, Lv Y, Zha W, Zhou N, Hong X. Association of Body Mass Index (BMI) With Critical COVID-19 and in-Hospital Mortality: A Dose-Response Meta-Analysis. Metabolism (2021) 117:154373. doi: 10.1016/j.metabol.2020.154373
222. Chu Y, Yang J, Shi J, Zhang P, Wang X. Obesity is Associated With Increased Severity of Disease in COVID-19 Pneumonia: A Systematic Review and Meta-Analysis. Eur J Med Res (2020) 25(1):64. doi: 10.1186/s40001-020-00464-9
223. Khaodhiar L, McCowen KC, Blackburn GL. Obesity and its Comorbid Conditions. Clin Cornerstone (1999) 2(3):17–31. doi: 10.1016/S1098-3597(99)90002-9
224. Dube S, Norby BJ, Pattan V, Carter RE, Basu A, Basu R. 11beta-Hydroxysteroid Dehydrogenase Types 1 and 2 Activity in Subcutaneous Adipose Tissue in Humans: Implications in Obesity and Diabetes. J Clin Endocrinol Metab (2015) 100(1):E70–76. doi: 10.1210/jc.2014-3017
225. Aksoy H, Karadag AS, Wollina U. Angiotensin II Receptors: Impact for COVID-19 Severity. Dermatol Ther (2020) 33(6):e13989. doi: 10.1111/dth.13989
226. Saiki A, Ohira M, Endo K, Koide N, Oyama T, Murano T, et al. Circulating Angiotensin II Is Associated With Body Fat Accumulation and Insulin Resistance in Obese Subjects With Type 2 Diabetes Mellitus. Metabolism (2009) 58(5):708–13. doi: 10.1016/j.metabol.2009.01.013
227. Ellulu MS, Patimah I, Khaza'ai H, Rahmat A, Abed Y. Obesity and Inflammation: The Linking Mechanism and the Complications. Arch Med Sci (2017) 13(4):851–63. doi: 10.5114/aoms.2016.58928
228. Ran J, Hirano T, Fukui T, Saito K, Kageyama H, Okada K, et al. Angiotensin II Infusion Decreases Plasma Adiponectin Level via its Type 1 Receptor in Rats: An Implication for Hypertension-Related Insulin Resistance. Metabolism (2006) 55(4):478–88. doi: 10.1016/j.metabol.2005.10.009
229. Fujita K, Maeda N, Sonoda M, Ohashi K, Hibuse T, Nishizawa H, et al. Adiponectin Protects Against Angiotensin II-Induced Cardiac Fibrosis Through Activation of PPAR-Alpha. Arterioscler Thromb Vasc Biol (2008) 28(5):863–70. doi: 10.1161/ATVBAHA.107.156687
230. Kruglikov IL, Scherer PE. The Role of Adipocytes and Adipocyte-Like Cells in the Severity of COVID-19 Infections. Obes (Silver Spring) (2020) 28(7):1187–90. doi: 10.1002/oby.22856
231. Gheblawi M, Wang K, Viveiros A, Nguyen Q, Zhong JC, Turner AJ, et al. Angiotensin-Converting Enzyme 2: SARS-CoV-2 Receptor and Regulator of the Renin-Angiotensin System: Celebrating the 20th Anniversary of the Discovery of ACE2. Circ Res (2020) 126(10):1456–74. doi: 10.1161/CIRCRESAHA.120.317015
232. Cheng H, Wang Y, Wang GQ. Organ-Protective Effect of Angiotensin-Converting Enzyme 2 and its Effect on the Prognosis of COVID-19. J Med Virol (2020) 92(7):726–30. doi: 10.1002/jmv.25785
233. Um JY, Chung HS, Song MY, Shin HD, Kim HM. Association of Interleukin-1beta Gene Polymorphism With Body Mass Index in Women. Clin Chem (2004) 50(3):647–50. doi: 10.1373/clinchem.2003.025858
234. Zhang Y, Murugesan P, Huang K, Cai H. NADPH Oxidases and Oxidase Crosstalk in Cardiovascular Diseases: Novel Therapeutic Targets. Nat Rev Cardiol (2020) 17(3):170–94. doi: 10.1038/s41569-019-0260-8
235. Tounian P, Aggoun Y, Dubern B, Varille V, Guy-Grand B, Sidi D, et al. Presence of Increased Stiffness of the Common Carotid Artery and Endothelial Dysfunction in Severely Obese Children: A Prospective Study. Lancet (2001) 358(9291):1400–4. doi: 10.1016/S0140-6736(01)06525-4.
236. Jin Y, Ji W, Yang H, Chen S, Zhang W, Duan G. Endothelial Activation and Dysfunction in COVID-19: From Basic Mechanisms to Potential Therapeutic Approaches. Signal Transduct Target Ther (2020) 5(1):293. doi: 10.1038/s41392-020-00454-7
237. Gavriilaki E, Anyfanti P, Gavriilaki M, Lazaridis A, Douma S, Gkaliagkousi E. Endothelial Dysfunction in COVID-19: Lessons Learned From Coronaviruses. Curr Hypertens Rep (2020) 22(9):63. doi: 10.1007/s11906-020-01078-6
238. Zhang C, Wu Z, Li JW, Zhao H, Wang GQ. Cytokine Release Syndrome in Severe COVID-19: Interleukin-6 Receptor Antagonist Tocilizumab may be the Key to Reduce Mortality. Int J Antimicrob Agents (2020) 55(5):105954. doi: 10.1016/j.ijantimicag.2020.105954
239. Cabandugama PK, Gardner MJ, Sowers JR. The Renin Angiotensin Aldosterone System in Obesity and Hypertension: Roles in the Cardiorenal Metabolic Syndrome. Med Clin North Am (2017) 101(1):129–37. doi: 10.1016/j.mcna.2016.08.009
240. Blokhin IO, Lentz SR. Mechanisms of Thrombosis in Obesity. Curr Opin Hematol (2013) 20(5):437–44. doi: 10.1097/MOH.0b013e3283634443
241. Kwaifa IK, Bahari H, Yong YK, Noor SM. Endothelial Dysfunction in Obesity-Induced Inflammation: Molecular Mechanisms and Clinical Implications. Biomolecules (2020) 10(2). doi: 10.3390/biom10020291
242. Prieto D, Contreras C, Sanchez A. Endothelial Dysfunction, Obesity and Insulin Resistance. Curr Vasc Pharmacol (2014) 12(3):412–26. doi: 10.2174/1570161112666140423221008
243. Virdis A. Endothelial Dysfunction in Obesity: Role of Inflammation. High Blood Press Cardiovasc Prev (2016) 23(2):83–5. doi: 10.1007/s40292-016-0133-8
244. Anfossi G, Russo I, Trovati M. Platelet Dysfunction in Central Obesity. Nutr Metab Cardiovasc Dis (2009) 19(6):440–9. doi: 10.1016/j.numecd.2009.01.006
245. Daryabor G, Kabelitz D, Kalantar K. An Update on Immune Dysregulation in Obesity-Related Insulin Resistance. Scand J Immunol (2019) 89(4):e12747. doi: 10.1111/sji.12747
246. Danziger J, Chen KP, Lee J, Feng M, Mark RG, Celi LA, et al. Obesity, Acute Kidney Injury, and Mortality in Critical Illness. Crit Care Med (2016) 44(2):328–34. doi: 10.1097/CCM.0000000000001398
247. Richardson S, Hirsch JS, Narasimhan M, Crawford JM, McGinn T, Davidson KW, et al. Presenting Characteristics, Comorbidities, and Outcomes Among 5700 Patients Hospitalized With COVID-19 in the New York City Area. JAMA (2020) 323(20):2052–9. doi: 10.1001/jama.2020.6775
248. Chen J, Qi T, Liu L, Ling Y, Qian Z, Li T, et al. Clinical Progression of Patients With COVID-19 in Shanghai, China. J Infect (2020) 80(5):e1–6. doi: 10.1016/j.jinf.2020.03.004
249. Godeau D, Petit A, Richard I, Roquelaure Y, Descatha A. Return-To-Work, Disabilities and Occupational Health in the Age of COVID-19. Scand J Work Environ Health (2021) 47(5):408–9. doi: 10.5271/sjweh.3960
250. Morgan OW, Bramley A, Fowlkes A, Freedman DS, Taylor TH, Gargiullo P, et al. Morbid Obesity as a Risk Factor for Hospitalization and Death Due to 2009 Pandemic Influenza A(H1N1) Disease. PLoS One (2010) 5(3):e9694. doi: 10.1371/journal.pone.0009694
251. Venkata C, Sampathkumar P, Afessa B. Hospitalized Patients With 2009 H1N1 Influenza Infection: The Mayo Clinic Experience. Mayo Clin Proc (2010) 85(9):798–805. doi: 10.4065/mcp.2010.0166
252. Zheng W, McLerran DF, Rolland B, Zhang X, Inoue M, Matsuo K, et al. Association Between Body-Mass Index and Risk of Death in More Than 1 Million Asians. N Engl J Med (2011) 364(8):719–29. doi: 10.1056/NEJMoa1010679
253. Murugan AT, Sharma G. Obesity and Respiratory Diseases. Chron Respir Dis (2008) 5(4):233–42. doi: 10.1177/1479972308096978
254. Falagas ME, Athanasoulia AP, Peppas G, Karageorgopoulos DE. Effect of Body Mass Index on the Outcome of Infections: A Systematic Review. Obes Rev (2009) 10(3):280–9. doi: 10.1111/j.1467-789X.2008.00546.x
255. Steele RM, Finucane FM, Griffin SJ, Wareham NJ, Ekelund U. Obesity is Associated With Altered Lung Function Independently of Physical Activity and Fitness. Obes (Silver Spring) (2009) 17(3):578–84. doi: 10.1038/oby.2008.584
256. Hamer M, Gale CR, Kivimaki M, Batty GD. Overweight, Obesity, and Risk of Hospitalization for COVID-19: A Community-Based Cohort Study of Adults in the United Kingdom. Proc Natl Acad Sci USA (2020) 117(35):21011–3. doi: 10.1073/pnas.2011086117
257. Chang TH, Chou CC, Chang LY. Effect of Obesity and Body Mass Index on Coronavirus Disease 2019 Severity: A Systematic Review and Meta-Analysis. Obes Rev (2020) 21(11):e13089. doi: 10.1111/obr.13089
258. Bhasker AG, Greve JW. Are Patients Suffering From Severe Obesity Getting a Raw Deal During COVID-19 Pandemic? Obes Surg (2020) 30(10):4107–8. doi: 10.1007/s11695-020-04677-z
259. Cauberghe V, Van Wesenbeeck I, De Jans S, Hudders L, Ponnet K. How Adolescents Use Social Media to Cope With Feelings of Loneliness and Anxiety During COVID-19 Lockdown. Cyberpsychol Behav Soc Netw (2021) 24(4):250–7. doi: 10.1089/cyber.2020.0478
260. Hawkley LC, Thisted RA, Cacioppo JT. Loneliness Predicts Reduced Physical Activity: Cross-Sectional & Longitudinal Analyses. Health Psychol (2009) 28(3):354–63. doi: 10.1037/a0014400
261. Moynihan AB, van Tilburg WA, Igou ER, Wisman A, Donnelly AE, Mulcaire JB. Eaten Up by Boredom: Consuming Food to Escape Awareness of the Bored Self. Front Psychol (2015) 6:369. doi: 10.3389/fpsyg.2015.00369
262. Drewnowski A. The Cost of US Foods as Related to Their Nutritive Value. Am J Clin Nutr (2010) 92(5):1181–8. doi: 10.3945/ajcn.2010.29300
263. Hall KD, Ayuketah A, Brychta R, Cai H, Cassimatis T, Chen KY, et al. Ultra-Processed Diets Cause Excess Calorie Intake and Weight Gain: An Inpatient Randomized Controlled Trial of Ad Libitum Food Intake. Cell Metab (2019) 30(1):67–77.e63. doi: 10.1016/j.cmet.2019.05.008
264. Jensen MD, Ryan DH, Apovian CM, Ard JD, Comuzzie AG, Donato KA, et al. 2013 AHA/ACC/TOS Guideline for the Management of Overweight and Obesity in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society. Circulation (2014) 129(25 Suppl 2):S102–138. doi: 10.1161/01.cir.0000437739.71477.ee
266. Kruger J, Galuska DA, Serdula MK, Jones DA. Attempting to Lose Weight: Specific Practices Among U.S. Adults. Am J Prev Med (2004) 26(5):402–6. doi: 10.1016/j.amepre.2004.02.001
267. Bish CL, Blanck HM, Maynard LM, Serdula MK, Thompson NJ, Khan LK. Health-Related Quality of Life and Weight Loss Practices Among Overweight and Obese US Adults, 2003 Behavioral Risk Factor Surveillance System. MedGenMed (2007) 9(2):35.
268. Sharma S, Ray A, Sadasivam B. Metformin in COVID-19: A Possible Role Beyond Diabetes. Diabetes Res Clin Pract (2020) 164:108183. doi: 10.1016/j.diabres.2020.108183
269. Crouse AB, Grimes T, Li P, Might M, Ovalle F, Shalev A. Metformin Use Is Associated With Reduced Mortality in a Diverse Population With COVID-19 and Diabetes. Front Endocrinol (Lausanne) (2020) 11:600439. doi: 10.3389/fendo.2020.600439
270. Ursini F, Ciaffi J, Landini MP, Meliconi R. COVID-19 and Diabetes: Is Metformin a Friend or Foe? Diabetes Res Clin Pract (2020) 164:108167. doi: 10.1016/j.diabres.2020.108167
271. Singh AK, Gupta R, Ghosh A, Misra A. Diabetes in COVID-19: Prevalence, Pathophysiology, Prognosis and Practical Considerations. Diabetes Metab Syndr (2020) 14(4):303–10. doi: 10.1016/j.dsx.2020.04.004
Keywords: obesity, COVID – 19, systematic review & meta-analysis, meta-regression analysis, severity, mortality
Citation: Singh R, Rathore SS, Khan H, Karale S, Chawla Y, Iqbal K, Bhurwal A, Tekin A, Jain N, Mehra I, Anand S, Reddy S, Sharma N, Sidhu GS, Panagopoulos A, Pattan V, Kashyap R and Bansal V (2022) Association of Obesity With COVID-19 Severity and Mortality: An Updated Systemic Review, Meta-Analysis, and Meta-Regression. Front. Endocrinol. 13:780872. doi: 10.3389/fendo.2022.780872
Received: 21 September 2021; Accepted: 10 January 2022;
Published: 03 June 2022.
Edited by:
Jeff M. P. Holly, University of Bristol, United KingdomReviewed by:
Mahmoud Elkazzaz, Damietta University, EgyptAndree Kurniawan, University of Pelita Harapan, Indonesia
Copyright © 2022 Singh, Rathore, Khan, Karale, Chawla, Iqbal, Bhurwal, Tekin, Jain, Mehra, Anand, Reddy, Sharma, Sidhu, Panagopoulos, Pattan, Kashyap and Bansal. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Vikas Bansal, YmFuc2FsLnZpa2FzQG1heW8uZWR1
†These authors have contributed equally to this work and share first authorship
 Romil Singh
Romil Singh Sawai Singh Rathore
Sawai Singh Rathore Hira Khan
Hira Khan Smruti Karale
Smruti Karale Yogesh Chawla5
Yogesh Chawla5 Abhishek Bhurwal
Abhishek Bhurwal Aysun Tekin
Aysun Tekin Ishita Mehra
Ishita Mehra Sohini Anand
Sohini Anand Sanjana Reddy
Sanjana Reddy Guneet Singh Sidhu
Guneet Singh Sidhu Anastasios Panagopoulos
Anastasios Panagopoulos Vishwanath Pattan
Vishwanath Pattan Rahul Kashyap
Rahul Kashyap Vikas Bansal
Vikas Bansal