- Department of Otorhinolaryngology-Head and Neck Surgery, The First Affiliated Hospital of Anhui Medical University, Hefei, China
Sistrunk procedure is the standard method for thyroglossal duct cyst resection. While this procedure is successful and safe, it results in postoperative scars on the front of neck. We propose a total transoral technique without external incision that starts with careful separation of the floor of the mouth and genioglossus muscle followed by the exact localization of the cyst using methylene blue. Simultaneously, the hyoid bone connected to the cyst and tract was removed. Finally, routine hemostasis is conducted, and the operative cavity is closed. All patients who received this operation in our department recovered successfully without experiencing severe intraoperative or postoperative complications.
Introduction
Thyroglossal duct cyst (TGDC) is one of the most commonly observed neck masses in clinical medicine. It is characterized by an active, painless mass in the midline or slightly to one side of the neck, usually located below the hyoid bone (about 75% of patients), and can move along with the tongue. This cyst develops embryologically when the thyroid primordium descends from the base of the tongue to its typical location in front of the trachea. If the tract does not degenerate, clinical cysts may develop (1).
Sistrunk procedure is the widely accepted surgical treatment for TGDC and is similar to open thyroid surgery. This procedure entails the removal of the central part of hyoid bone and thyroid remnants. However, the procedure leaves a roughly 5 cm scar in front of the neck.
Kim et al. (2) were the first to report a successful transoral TGDC resection. No other teams have reported the clinical application of this method. Considering different details, our goal is to share our experience with this approach. Informed consent and ethical review were obtained (IRB number: PJ2021-03-22).
Methods
We describe this procedure using the example of a 24-year-old woman who required it for cosmetic purposes. Therefore, we decided to perform a scarless procedure. Figure 1 illustrates relevant anatomical diagrams. The proposed technique was conducted under general anesthesia and oral endotracheal intubation. To maintain oral operating space, a unilateral oral distractor was employed. Subsequently, methylene blue was injected into the cyst from the outside (Figure 2A). At the oral lingual frenulum, a transverse incision of about 2 cm in length was made (Figure 2B). The soft tissue of the mouth floor was meticulously dissected, and genioglossus muscles with marked morphological characteristics were identified, separated, and retracted bilaterally (Figure 2C). Using a 4 mm rigid nasal endoscope, we longitudinally separated and transected suprahyoid muscles (Figure 2D). Then the hyoid bone was located and identified (Figure 3A). The hyoid bone’s body was then cut using a Kerrison rongeur (Figure 3B). Following this step, it was often found that the partially blue-stained cyst remained in the operation cavity. We employed a cryogenic plasma knife to transect the infrahyoid muscles at a distance of 0.5 cm from the hyoid bone. By pulling the hyoid bone upward using forceps, the cyst was completely exposed. Using a plasma knife, the tissue surrounding the cyst was meticulously dissected, and the hyoid bone was pulled out (Figure 3C). The hyoid bone and cyst were removed together (Figure 3D). After sufficient hemostasis, the operative cavity was flushed with distilled water. A drainage tube was inserted from the mouth floor and fixed under the chin. Finally, the oral mucosa was sutured with a 4-0 suture and bandaged with external neck pressure (Video 1, Supporting Information).
Figure 2 (A) Methylene blue injection. (B) Transverse frenotomy incision. (C) The genioglossus muscles were retracted bilaterally. (D) Transection of suprahyoid muscles.
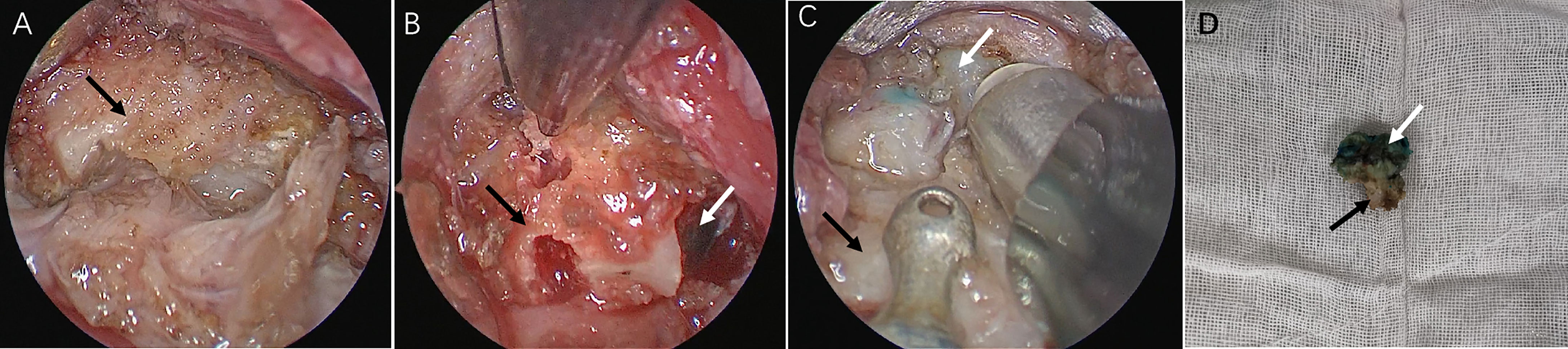
Figure 3 (A) Identification of hyoid bone (black arrow). (B) Identification of TGDC (white arrow). (C) Dissection of the cyst. (D) Specimen.
The drain was removed when drainage volume was less than 5 mL per 24 h. After operation, no special dietary restrictions were found, and patients were given saline to gargle and maintain their mouth clean. Patients were discharged two days following extubation unless there were special circumstances and were required to comply with regular outpatient follow-up.
Results
Our technique was successful in five patients. The characteristics of patients and operations are listed in Table 1. During at least a half-year follow-up, no recurrences or peri/postoperative complications were observed, and all patients achieved excellent cosmetic outcomes with their necks (Figures 4 and 5).
Discussion
After diagnosis with a thyroglossal duct cyst, patients tended to seek surgical treatment with an otolaryngologist. A standard Sistrunk procedure is often adopted to resect the lesion. However, growing esthetic concerns motivate patients to seek cosmetic treatment for their unsightly scar in the neck. While the auxiliary use of local drugs and the improvement of surgical hardware can indeed reduce the obvious degree of postoperative scarring, they can also introduce complications such as pruritus and local pain.
Currently, researchers have focused on hidden scars or scarless cosmetic surgery. Cai et al. (3) used endoscope-assisted surgery to successfully resect TGDC via a small submental incision, but scarring remains inevitable. One study published by Qu et al. (4) presented a study in which they successfully executed the breast approach on 13 patients, but one had an infection, one developed skin bruising, and another had subcutaneous fluid. Anuwong et al. (5) also completed this operation with the bilateral areola approach. Considering the author’s experience with endoscopic surgery, none of the 11 patients included in their study experienced postoperative complications, and the operation time was shorter. Paek et al. (6) successfully completed TGDC resection for two patients using the bilateral axillo-breast approach. However, this procedure requires more incisions. Kim et al. (7) and Lee et al. (8) selected the retroauricular approach, successfully removed TGDC with robot assistance, and the incision can be hidden, but the costs and hardware constraints obstruct wider accessibility. Han et al. (9) and Banuchi et al. (10) completed the operation by employing the transoral vestibular approach. The former adopts a single incision without insufflation, while the latter adopts the same three incisions with CO2 insufflation as the vestibular approach for thyroid. Both operations were completed successfully without complications. However, the single incision method of Han et al. (9) does not avoid the problem of narrow operation space. Asians have a relatively flat jaw, which may impede the use of this technology among other races. Compared with the above approaches, the distance of frenotomy incision is the shortest, and this approach conforms to the law of anatomy. The surgical path is positioned in the midline without important vessels and nerves and does not require extensive tissue dissection and CO2 insufflation, which avoids possible complications of hypercapnia and numbness in the operation area. However, it should be noted that limitations are still present. The frenotomy incision may bring the risk of incision infection; sublingual edema may cause airway obstruction; narrow operation space significantly increases the difficulty of this procedure, requiring more patience and time. Our operation time was between two and four hours, while the time reported by Woo et al. (11) was about one hour. Similarly, the operation time of Anuwong et al. (5) is also shorter compared with Qu et al. (4) We believe that this technique can be executed more efficiently as experience grows.
The tongue must be retracted upward to expose the mouth floor and the frenum. After recognizing Wharton’s duct orifice, we made a frenotomy incision closer to the mandible. Then, blunt separation was used for tissue dissection. In so doing, risk of Wharton’s duct injury can be avoided (12). The next issue is the limited operating space, implying why we used 4 mm nasal endoscope. Based on our experience, it is critical to precisely locate the cyst when using the transoral approach. As a result, we used methylene blue for intraoperative localization. The next step requires the surgeon to have extensive experience with endoscopic procedures to avoid cyst rupture because the rupture would lead to blue staining in the operation field, making boundary identification is difficult.
At present, there remain a few reports on endoscopic TGDC surgery, and there are insufficient materials to define indications and contraindications of this operation. In our study, the patients had strong cosmetic intentions and had no history of neck surgery, neck radiotherapy, thyroglossal cyst infection, or thyroglossal fistula. In the above literature, most specimens are 2-3 cm, with the largest specimen of 6 cm in the study of Woo et al. (11) There is no consensus on lesion size limitation. In our method, syringe can be utilized to extract part of the capsule, which may overcome the sample size limitation, but this must be confirmed by follow-up research.
Conclusion
TGDC removal using a frenotomy incision is an alternative to conventional procedure with a safe, effective, cosmetic, and well-tolerated outcome. However, because the sample size was relatively small, additional research on indications, complications, and recurrences is still required.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by Ethics Committee of the First Affiliated Hospital of Anhui Medical University. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
Concept and design: All authors. Acquisition, analysis, or interpretation of data: All authors. Drafting of the manuscript: SC. Critical revision of the manuscript for important intellectual content: All authors. Statistical analysis: SC. Administrative, technical, or material support: All authors. Supervision: YZ. All authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fendo.2021.774174/full#supplementary-material
References
1. Thompson LD. Thyroglossal Duct Cyst. Ear Nose Throat J (2017) 96:54–5. doi: 10.1177/014556131709600204
2. Kim JP, Park JJ, Lee EJ, Woo SH. Intraoral Removal of a Thyroglossal Duct Cyst Using a Frenotomy Incision. Thyroid (2011) 21:1381–4. doi: 10.1089/thy.2011.0180
3. Cai Q, Huang X, Liang F, Chen J, Liang M, Pan Y, et al. Endoscope-Assisted Concurrent Resection of Thyroglossal Duct Cysts and Benign Thyroid Nodules via a Small Submental Incisions. Eur Arch Otorhinolaryngol (2014) 271:1771–5. doi: 10.1007/s00405-013-2688-5
4. Qu R, Wang C, Dong Z, Li J, Liu D. Another Strategy for the Treatment of Thyroglossal Duct Cyst: Totally Endoscopic Surgery by Breast Approach. Surg Laparosc Endosc Percutan Tech (2018) 28:118–22. doi: 10.1097/SLE.0000000000000514
5. Anuwong A, Jitpratoom P, Sasanakietkul T. Bilateral Areolar Endoscopic Sistrunk Operation: A Novel Technique for Thyroglossal Duct Cyst Surgery. Surg Endosc (2017) 31:1993–8. doi: 10.1007/s00464-016-5137-x
6. Paek SH, Choi JY, Lee K-E, Youn Y-K. Bilateral Axillo-Breast Approach (BABA) Endoscopic Sistrunk Operation in Patients With Thyroglossal Duct Cyst: Technical Report of the Novel Endoscopic Sistrunk Operation. Surg Laparosc Endosc Percutan Tech (2014) 24:e95–8. doi: 10.1097/SLE.0b013e31828fa7bf
7. Kim C-H, Byeon HK, Shin YS, Koh YW, Choi EC. Robot-Assisted Sistrunk Operation via a Retroauricular Approach for Thyroglossal Duct Cyst. Head Neck (2014) 36:456–8. doi: 10.1002/hed.23422
8. Lee DW, Tae K. Robot-Assisted Excision of Thyroglossal Duct Cyst by a Postauricular Facelift Approach. Wideochir Inne Tech Maloinwazyjne (2020) 15:245–8. doi: 10.5114/wiitm.2019.88751
9. Han P, Liang F, Cai Q, Chen R, Yu S, Huang X. Endoscope-Assisted Resection of Thyroglossal Duct Cysts via a Submaxillary Vestibular Approach. Head Neck (2018) 40:377–83. doi: 10.1002/hed.24972
10. Banuchi VE, Long SM, Sachs BY, Kostas JC, Ali KM, Russell JO. Transoral Endoscopic Vestibular Approach Sistrunk Procedure: First Reported Case Series. Head Neck (2021) 44:1–5. doi: 10.1002/hed.26889
11. Woo SH, Park JJ, Hong JC, Wang S-G, Park GC, Eun YG, et al. Endoscope-Assisted Transoral Removal of a Thyroglossal Duct Cyst Using a Frenotomy Incision: A Prospective Clinical Trial. Laryngoscope (2015) 125:2730–5. doi: 10.1002/lary.25508
12. Wilhelm T, Harlaar JJ, Kerver A, Kleinrensink G-J, Benhidjeb T. Surgical Anatomy of the Floor of the Oral Cavity and the Cervical Spaces as a Rationale for Trans-Oral, Minimal-Invasive Endoscopic Surgical Procedures: Results of Anatomical Studies. Eur Arch Otorhinolaryngol (2010) 267:1285–90. doi: 10.1007/s00405-010-1219-x
Keywords: endoscopic surgery, thyroglossal cyst, transoral procedures, outcome, cosmetic (plastic) surgery
Citation: Chen S, Wang D, Qiu J, Liu Y and Zhao Y (2022) Endoscopic-Assisted Transoral Thyroglossal Cyst Resection. Front. Endocrinol. 12:774174. doi: 10.3389/fendo.2021.774174
Received: 11 September 2021; Accepted: 30 December 2021;
Published: 18 February 2022.
Edited by:
Paolo Miccoli, University of Pisa, ItalyReviewed by:
Kyung Tae, Hanyang University, South KoreaChe-Wei Wu, Kaohsiung Medical University, Taiwan
Copyright © 2022 Chen, Wang, Qiu, Liu and Zhao. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yi Zhao, emhhb3lpMTEyNjU5QDE2My5jb20=
 Shanwen Chen
Shanwen Chen Dong Wang
Dong Wang Jianxin Qiu
Jianxin Qiu Yehai Liu
Yehai Liu