
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Endocrinol., 10 September 2021
Sec. Reproduction
Volume 12 - 2021 | https://doi.org/10.3389/fendo.2021.736384
This article is part of the Research TopicDisruptors on Male Reproduction - Emerging Risk FactorsView all 19 articles
This study aimed to investigate the situations of pornography use among male college students of China, to explore the addiction possibility for pornography use, and to study the associations between pornography use and reproductive hormone levels and semen quality. Five hundred sixty-eight participants met the inclusion criteria and finished all of the questionnaires and hormone level and semen parameter examinations. A majority of participants (except one) had pornography use experience, 94.2% participants started pornography use before college, and 95.9% participants reported they had masturbation experience when using pornography. Early contact to pornography, frequent pornography use, high amount of time spending on pornography use, and frequent masturbation during pornography use were correlated with addiction trends. Earlier pornography use was found to be associated with lower serum prolactin (PRL), follicle-stimulating hormone (FSH), and progesterone (Prog), as well as lower sperm concentration and total sperm count. Higher frequency of pornography use was associated with lower serum estrogen (E2). In conclusion, pornography use was common among male college students in China. Early contact, high frequent use, and high frequency of masturbation during pornography use could lead to addiction trends and aberrant reproductive hormone levels and semen quality.
Sex demand is considered an embarrassing issue in many eastern countries, particularly in China in the past years. It is hard for adolescents to get sex information from parents or schools. At the same time, adolescents during the puberty process have high demands for sexual sensation and sex information physically and psychologically. With the quick development of the Internet, pornography has become easily accessible to all ages because of its affordability, accessibility, and anonymity (1). It was estimated that 42.7% of Internet visitors have visited pornography websites, and 25% of Internet visitors visit pornography websites everyday (2). Adolescents are important audience for pornography works (3). An investigation among 563 US college students reported that by age 17, an overwhelming majority of boys (93%) and girls (62%) have been exposed to pornography, and boys were more likely to be exposed at an earlier age and with higher frequency (4). Similarly, situations happened in other regions (5–7). A 6-year longitudinal study showed that among middle school students of Hong Kong, from grade 7 (average age = 12.7) to grade 12, pornography consumption increased significantly, and boys were more likely to contact pornography works (8, 9). However, the pornography exposure to adolescents, especially to college students in mainland of China were not clear.
Some of the investigations showed that pornography had some positive or neutral effects on adolescents’ sexual practice. For example, pornography was found to be a resource to provide information about the human body, to increase the sense of sexual competence, and to decrease the sexual shame (10). On the other hand, there are also studies suggesting its negative effects. Several publications showed that increased pornography exposure was associated with earlier and quicker onset of sexual activity (11), more permissive attitude to casual sex (12), worse mental health (5), higher likelihood to risky sexual behaviors, and more acceptance of sexual violence (13). Moreover, a recent study revealed that problematic pornography user displayed a similar neural response as the drug addicts displayed (14). A study among Canadian university students (mean age 21) showed that daily and greater pornography use was associated with a sharp rise in addictive score (15).
Pornography is a specific sexual stimulus that can cause sexually related physical and psychological reactions, including sexual imagination, sexual erection, and masturbation (16). All of these behaviors were modulated by sexual hormones and feedback to hormone secretions, which was a typical feedback loop of hypothathalamus-putuitary-gonadal axis (HPG) activity (17, 18). Adolescents, including college students, are in the late stage of puberty, which is the important process of sexual hormones and organ maturation (19). However, none of the existing studies about pornography exhibited the effects of pornography on reproductive hormones and reproductive potentials.
The purposes of this study were as follows: (1) to explicate the current situation of pornography use among Chinese college students; (2) to investigate college students’ addiction trends for pornography use; and (3) to research the associations between pornography use and reproductive hormones and semen parameters.
All of the participants in this study originated from a cohort termed the male reproductive health in Chongqing College students (MARHCS), which began in 2013 (20). This was the second follow-up study of the cohort. Since April 2015, all volunteers who participated in the baseline survey in 2013 received our cell phone and email illustrating this study, and they scheduled an investigation time from May 23, 2015 to June 7, 2015. All volunteers were asked to complete a questionnaire and underwent a physical examination. Individuals were included if they met the following criteria: over 18 years of age; 2–7 days of abstinence; no history of inflammation of the urogenital system, epididymitis, or testicular injury; no history of incomplete orchiocatabasis; and no history of varicocele treatment. Subjects were excluded if any of the following symptoms were detected by aurologist at the physical examination stage of the investigation: an absence of prominentialaryngea, pubis, or testis; abnormal penis or breasts; varicocele; or an epididymal knob. Five hundred sixty-eight males completed the survey, and all of them had a mean coming-out age of 22.4 years (SD = 1.2). Semen samples were collected and analyzed according to WHO guideline (WHO, 2010). Abstinence duration and ejaculation time were recorded. Peripheral blood was collected under aseptic conditions. The serum was isolated by centrifugation for serum reproductive hormone measurements. The Ethics Council of the Army Medical University approved the study, and informed consent was obtained from all subjects.
The questionnaires contained three parts: demographic information, lifestyle factors, and pornography use situations. The demographic information consisted of age, body mass index (BMI), and abstinence duration (days). Lifestyle factors included smoking, drinking, coffee consumption, cola consumption, and fried food consumption, which have all been reported to have an influence on semen quality (20).
The questions about pornography use situations and addictive behaviors were set according to previous studies about pornography exposure (21–25). Before the participants filled out the questionnaires, they were asked to read the definition of pornography, which included the following terms: sexually explicit material, sexually explicit media, pornography, porn, cyber-porn, Internet or online pornography, online erotica or erotica, and cyberpornography (24, 25).
All collected serum samples were taken from a low-temperature refrigerator at −80°C and then sent to the Army Medical University Affiliated Southwest Hospital Laboratory. The serum samples were then liquefied and tested of six reproductive hormone levels, including estradiol (E2), follicle-stimulating hormone (FSH), luteinizing hormone (LH), progesterone (Prog), prolactin (PRL), and testosterone (T). The chemiluminescence method was used to determine the serum hormone levels, and the instrument was selected by Beckman’s fully automated immunoassay analyzer DXI 800 (Beckman Coulter Inc., Brea, CA, USA).
Semen samples were collected by masturbation into a sterile, wide-mouth plastic container in an independent clean room. Then, the samples were incubated at 37°C for liquidation and were analyzed within 60 min. Semen volumes were measured by weighing, assuming that 1 ml of volume equals 1 g of weight. The semen parameters (motility, progressive motility, concentration, and total sperm count) were assessed with a computer-aided sperm analysis system (SCA CASA System; Microptic S.L., Barcelona, Spain) by a well-trained laboratory technician. Sperm morphology was identified by sperm smears using a Diff-Quick staining kit (Boruide, BRED-015). All semen analyses were performed according to the WHO criteria recommendations (26).
Semen parameters and sex hormones were presented as medians and percentiles. The Jonckheere-Terpstratest and Mann-Whitney U test were used to compare differences between the semen parameters of the groups. A multivariable-linear regression model was applied to exclude potential confounders (e.g., age, BMI, abstinence duration, tobacco smoking, alcohol drinking, coffee consumption, cola consumption, and fried food consumption), which have been reported to have effects on semen parameters (20). All semen parameters were log-transformed when they were nonnormally distributed. Additionally, all of the statistical data were analysis with the Statistical Package for the Social Sciences (SPSS, Chicago, IL, USA), and differences were considered statistically significant if p < 0.05, and all the tests were performed by two tailed.
Descriptive results are demonstrated in Table 1. Five hundred sixty-eight participants met the inclusion criteria and finished the examination. The average age of the respondents was 22.4 years, and the average BMI value and abstinence duration were 22.2 (kg/m2) and 4.1 days, respectively.

Table 1 Demographic characteristics, lifestyle factors, reproductive hormone levels, and semen parameters of the participants.
The average E2, FSH, LH, PRL, Prog, and T concentrations were 30.6 pg/ml, 3.5 mIU/ml, 4.3 mIU/ml, 10.4 ng/ml, 0.6 ng/ml, and 3.8 ng/ml respectively. The average semen volume, sperm concentration, total sperm count, total motility, progressive motility, and morphologically normal spermatozoa count were 3.8 ml, 56 million/ml, 203 million, 79%, 55%, and 11.73%, respectively.
As Table 2 shows, almost all of the male students (except one) had experienced pornography use, albeit to varying extents. A total of 84.2% of the students first searched for pornography during middle or high school, and approximately 45.3% of the students used pornography more than once per week. Additionally, approximately 51.6% of the students spent approximately 15 to 30 min using pornography at each use. Only 4.1% students reported they had never masturbated during pornography use, when asked about their masturbation frequency when using pornography. In contrast, 14.9% of the students masturbated almost every time they used pornography.
Approximately half of the students reported they had used less pornography in the most recent 3 months. Additionally, 6.4% of the students reported they had used pornography more than before. One hundred and eighty (31.7%) students reported that they needed more time to feel sexual excitement than ever when using pornography. Excluding students who had no sexual partners (N = 238, 42%), 6.5% (N = 37) of the students reported that it was easier for them to achieve sexual satisfaction by using pornography than with a real sexual partner. Moreover, pornography use was significantly associated with addiction possibility. Earlier contact, more frequent use, longer time, and more masturbation during pornography use were all found to be correlated with addictive possibility (Table 3).
Univariate analyses were applied to estimate the associations between pornography use and sex hormones. According to the increase of ages of “first time to contact pornography” from primary school to college, the Prog, FSH, and PRL concentrations were increased from 0.4 to 0.8 ng/ml, 2.7 to 3.2 mIU/ml, and 8.5 to 10.7 ng/ml, respectively (p < 0.05, p < 0.05, p < 0.05). The E2 concentration decreased from 32 to 26 pg/ml according to the increase of frequency of pornography use (p < 0.05) (Figure 1).
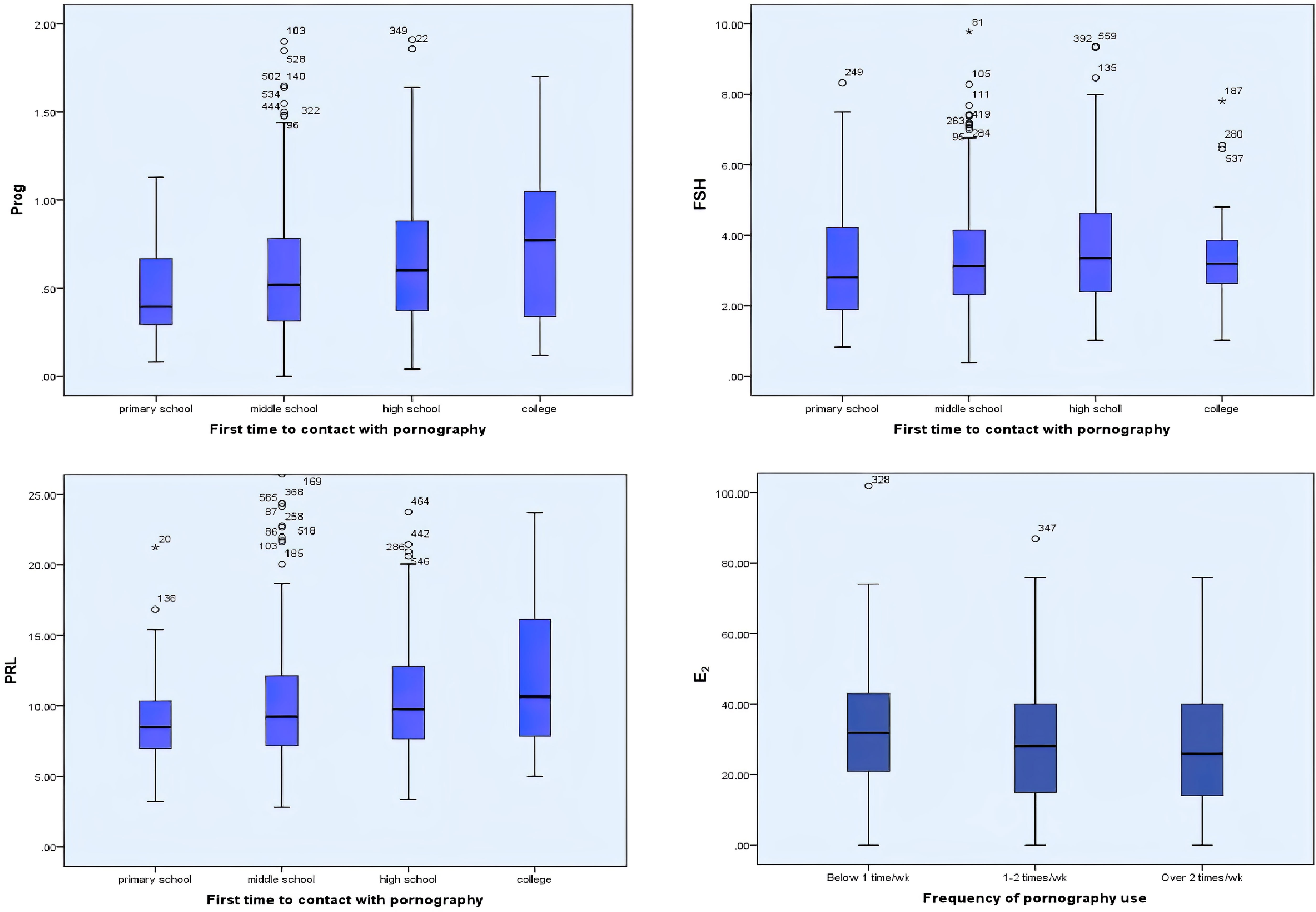
Figure 1 Univariate analyses were applied to estimate the associations between pornography use and sex hormones. The ages of first-time contact pornography were positively correlated with Prog, FS, and PRL concentrations in serum (p < 0.05, p < 0.05, p < 0.05). The frequency of pornography use were negatively correlated with E2 concentrations in serum (p < 0.05). *:extreme values.
After adjusting the potential confounders (age, BMI, abstinence duration, tobacco smoking, alcohol consumption, coffee consumption, cola consumption, and fried foods consumption), students with higher pornography use frequency had lower E2 concentration in serum (β coefficient = −3.29; 95% confidence interval (CI), −5.14, −1.13, p = 0.003). Students with earlier exposure to pornography had lower PRL and Prog concentration in serum (β coefficient = 0.92; 95% CI, 0.37, 1.47, p = 0.001; β coefficient = 0.10; 95% CI, 0.05, 0.14, p < 0.001) (Table 4).
Univariate analyses were applied to estimate the associations between pornography use and semen parameters. As shown in Figure 2, earlier pornography use, higher-frequency exposure to pornography, higher-frequency of masturbation when using pornography were associated with lower sperm concentration and total sperm count (p < 0.05).
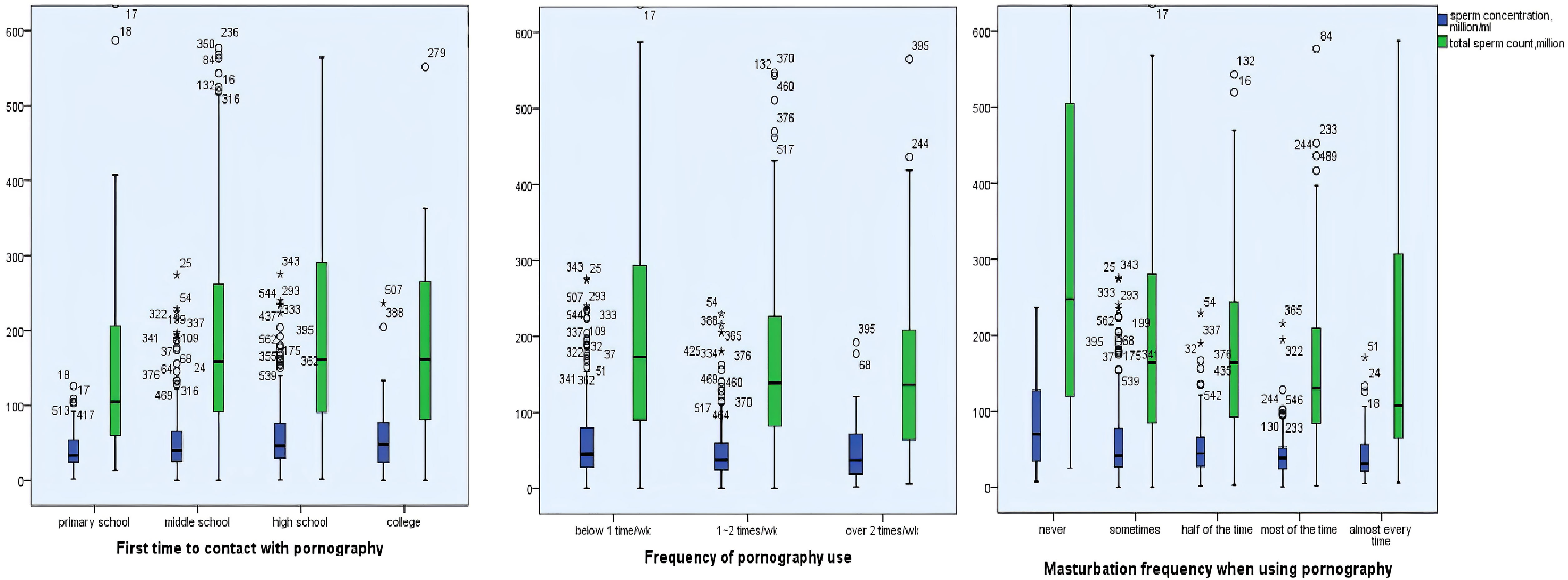
Figure 2 Univariate analyses were applied to estimate the associations between pornography use and semen parameters. The ages of first-time contact pornography were positively correlated with sperm concentration and total sperm count (p < 0.05). The frequency of pornography use and masturbation frequency when using pornography were negatively correlated with sperm concentration and total sperm count (p < 0.05, p < 0.05). *:extreme values.
Multivariable linear regression models were used to adjust the potential confounders (age, BMI, abstinence duration, tobacco smoking, alcohol consumption, coffee consumption, cola consumption, and fried foods consumption). After adjusting for potential confounders, the associations between pornography use and sperm concentration were still solid. The sperm concentration was positively associated with the ages of first time to contact with pornography (β coefficient = 11.17; 95% CI, 1.86, 21.34; p = 0.017) but negatively associated with masturbation frequency when using pornography (β = −7.40; 95% CI, −14.82, −0.46; p = 0.038). However, higher morphologically normal spermatozoa ratio (%) was found to be positively associated with masturbation frequency when using pornography (β = 7.40; 95% CI, 2.33, 12.72; p = 0.003) (Table 5).
Adolescent pornography use is a hot public health issue (27, 28). The present study is an exploratory study designed to describe pornography use among college students in China and to explore the effects of pornography use on students’ reproduction health. We found that pornography use was quite common among college students in China. Pornography use was correlated with masturbation behavior and exposure to prolonged pornography may lead to addictive potential. Pornography use was also found to be significantly associated with sex hormone levels in serum and semen parameters.
Like in other countries or areas, pornography use among college students was quite common in China. In the present study, 94.2% of college students had contacted to pornography before college, which is consistent with other recent studies in other countries (29, 30).
The American Society of Addiction Medicine (ASAM) defined “addiction” in 2011 as: Addiction is a primary, chronic disease of brain reward, motivation, memory and related circuitry. Dysfunction in these circuits leads to characteristic biological, psychological, social, and spiritual manifestation. This is reflected in an individual pathologically pursuing reward and/or relief by substance and other behavior (31). Regarding pornography addiction, the clinical diagnostic criteria is still devoid. A number of studies supported the “self-reported pornography addiction” questionnaire to access the cognitive, behavioral, and emotional aspects of problematic pornography use (21–25). The questions about pornography use situations and addictive behaviors were set according to these previous studies. Quite a lot of studies led to the conclusion that frequent pornography use fitted into the addiction framework and shared a similar basic mechanism with substance addiction. The present study confirmed that pornography use might lead to addictive possibility; 31.7% of students reported they need more time to feel sexual excitement when using pornography, and nearly 6.5% of students thought it would be easier to achieve sexual satisfaction when using pornography than with a real sexual partner. Pornography has been reported to be a dopamine-producing base behavior (32). Dopamine is a neurotransmitter that is associated with activation of the brain’s reward system, and its presence helps initiate feelings of enjoyment and pleasure. Moreover, a study from the Max Planck Institute for Human Development showed that frequent pornography consumption was associated with the frontostriatal network, and pornography consumption hours were negatively associated with striatum volume. Individuals with a lower striatum volume may need more external stimulation to experience pleasure and might therefore experience pornography consumption as more rewarding (33). Therefore, frequent pornography use might break the balance of the dopamine pathway. Like heroin or other drugs, frequent pornography use may cause addiction, which might be a reason for why the pornography users showed difficulty in obtaining sexual excitement.
In the present study, we found that early pornography exposure was associated with lower adult FSH, Prog, and PRL levels in serum. After adjusting with potential confounders, we still found a significant association between “the first time contact with pornography” and Prog levels in serum. During puberty, the HPG axis is initiated, and the gonadal steroid hormones are dramatically increased (18), as well as the quick development of reproductive organs. FSH is responsible for starting the process of the sperm production (spermatogenesis) by initiating spermatogenic epithelium cell division and maturation. FSH have been also reported to be related with gonadotropin levels which lead to the induction of spermatogenesis effectively (34, 35). Recent studies showed that Prog produced by cumulus cells has been associated with various physiological processes in sperm production, including stimulation of acrosome reaction. Male normal prolactin levels help maintain a high level of testosterone in the testis and affect the growth and secretion of the gonadal glands (36). Hyperprolactinemia is a high level of serum prolactin, which can interfere with the periodic release of GnRH, the elimination of gonadotropin pulsed secretion, so that the release of LH and FSH decreased, eventually leading to hypogonadism (testosterone synthesis and secretion, spermatogenic dysfunction) (37). Thus, pornography use at an early stage may affect the function of the HPG axis and subsequently affect the secretion of steroid hormones, such as estrogen, androgen, prolactin, and progesterone, eventually affecting semen quality.
We also found that earlier pornography use was associated with lower sperm concentrations with or without adjusting to potential confounders. A majority of students are exposed to pornography before college. As we discussed in the previous section, adolescence is a key time for reproductive maturation, from sexual hormone secretion to sexual organ development. The time of puberty initiation and the time for first sexual encounter were found to be two developmental milestones associated with reproductive maturation (38). Earlier contact to pornography might lead to disturbance of sexual hormone secretion, and therefor lead to lower sperm concentration in adult semen. Besides, earlier contact to pornography might lead to higher frequency of masturbation, which is also a risk factor for lower sperm concentration. There are no other studies focused on male puberty pornography use and adult semen qualities, but some studies revealed that adolescents who were exposed to pornography were more likely to reach early sexual maturation and be higher sensation seekers (39).
The present study showed that pornography use was significantly correlated with masturbation behavior. Higher masturbation frequency during pornography use showed adverse effects on the sperm concentration and total sperm count. Masturbation was the most common behavior performed during pornography use in the present study and in other studies (40). However, a few studies have investigated the relationship between masturbation frequency during pornography use and semen parameters. A large online study on male sexual health in three European countries showed that frequent pornography use significantly increased the masturbation frequency among coupled men with decreased sexual desire (41). Additionally, higher masturbation frequency might increase the threshold of sexual arousal. Thus, we hypothesize that frequent masturbation might lead to frequent arousal and ejaculation, leading to continual hyperemia in the genitals and gonads, which could eventually affect spermatogenesis. Besides, frequent masturbation is usually accompanied with shorter abstinence time, which is also a risk factor for lower sperm concentration (20).
The present study showed that the frequency of masturbation when using pornography was negatively associated with sperm concentration while positively associated with morphological normal spermatozoa. It seems that this behavior has brought controversial effect to semen quality. Actually, it just reflects the physiology of sperm production. As the abstinence period grows, the accumulation of sperms leads to an increase in sperm concentration, while the accumulated sperms become senescent and lead to a decrease in the proportion of morphological normal spermatozoa. Vice versa, the masturbation behavior during using pornography decreased the abstinence period of the subjects, and consequently decreased the sperm concentration and increased the proportion of morphological normal spermatozoa.
The main strengths of this study were as follows. First, this was a follow-up study of MARHCS cohort. All of the participants were familiar with the study design, and they were well educated and could fully understand all of the questions, which make our results more credible. Second, our sample constituted a large healthy population with a narrow age range, and the selection of the same sampling season significantly reduced potential confounders. Third, the semen quality evaluation methods were used as per the WHO recommendations, which make our results more comparable with those of other studies.
There are some limitations to our study. First, the pornography use data were obtained via self-review, which raises the possibility of information bias. Secondly, the subjects of the present study were all recruited from the universities which were located in the university town of Chongqing, although the students came from different provinces all over China. The sampling season was restricted in summer and was several years ago. The population was highly homogenous, with similar ages, lifestyles, and education levels, which make it challenging to compare with other populations. Thirdly, each subject only offered one semen sample in each follow-up investigation, which might have introduced intra-individual bias to this study. Fourthly, sex is a sensitive topic for Chinese students to talk about. Thus, the pornography use data the students reported may be conservative, and the potential effects may have been underestimated. Although we adjusted for potential confounders on semen parameters and sex hormones, some other potential confounders might still exist, such as environmental exposure, psychological distress, and socioeconomic status. Whether the findings of the present study could be replicated in independent populations with different characteristics and circumstances await further studies. The results of the current study should be interpreted with caution, and further studies evaluating the relationship between pornography use and reproductive phenotypes should be conducted.
In conclusion, the present study showed that pornography use was quite common among college students in China. Our results showed pornography use was correlated with masturbation behavior and may lead to addictive behavior. This is also the first study to investigate the associations between pornography use and semen parameters. The results showed that pornography use was significantly associated with sex hormones in serum and semen parameters, which indicated that early and frequent pornography exposure may lead to adverse male reproductive outcome. Our results may have important implications for public health.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by The Ethics Council of the Army Medical University. The patients/participants provided their written informed consent to participate in this study.
ZC and MM contributed to interpretation of the data and drafted the paper. The study was conceived and designed by ZC and JC. MM and QC contributed to statistical analyses. Data acquisition was conducted by ZC, MM, QC, XW, HY, NZ, LS, JL, and LA. All authors contributed to the article and approved the submitted version.
This work was supported by the Fundamental Research Funds for the Central Universities, SWU [grant number 7110100301], National Natural Science Foundation of China [grant numbers 81502788], and National Key Research and Development program of China [grant number 2017YFC1002001].
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
We thank the participants in the study for their cooperation.
1. Cooper A. Sexuality and the Internet: Surfing Into the New Millennium. Cyber Psychol Behav (1998) 1:187–93. doi: 10.1089/cpb.1999.2.475
2. Braithwaite SR, Coulson G, Keddington K, Fincham FD. The Influence of Pornography on Sexual Scripts and Hooking Up Among Emerging Adults in College. Arch Sex Behav (2015) 44:111–23. doi: 10.1007/s10508-014-0351-x
3. Peter J, Valkenburg PM. Adolescents and Pornography: A Review of 20 Years of Research. J Sex Res (2016) 53:509–31. doi: 10.1080/00224499.2016.1143441
4. Sabina C, Wolak J, Finkelhor D. The Nature and Dynamics of Internet Pornography Exposure for Youth. CyberPsychol Behav (2008) 11:691–3. doi: 10.1089/cpb.2007.0179
5. Camilleri C, Perry JT, Sammut S. Compulsive Internet Pornography Use and Mental Health: A Cross-Sectional Study in a Sample of University Students in the United States. Front Psychol (2021) 11:613244. doi: 10.3389/fpsyg.2020.613244
6. Madigan S, Villani V, Azzopardi C, Laut D, Smith T, Temple JR, et al. The Prevalence of Unwanted Online Sexual Exposure and Solicitation Among Youth: A Meta-Analysis. J Adolesc Health (2018) 63:133–41. doi: 10.1016/j.jadohealth.2018.03.012
7. Zohor Ali AA, Muhammad NA, Jamil TR, Ahmad S, Abd Aziz NA. Internet Pornography Exposures Amongst Young People in Malaysia: A Cross-Sectional Study Looking Into the Role of Gender and Perceived Realism Versus the Actual Sexual Activities. Addict Behav Rep (2021) 14:100350. doi: 10.1016/j.abrep.2021.100350
8. Shek DT, Ma CM. A Six-Year Longitudinal Study of Consumption of Pornographic Materials in Chinese Adolescents in Hong Kong. J Pediatr Adolesc Gynecol (2016) 29:S12–21. doi: 10.1016/j.jpag.2015.10.004
9. Ma CM, Shek DT. Consumption of Pornographic Materials in Early Adolescents in Hong Kong. J Pediatr Adolesc Gynecol (2013) 26:S18–25. doi: 10.1016/j.jpag.2013.03.011
10. Poulsen FO, Busby DM, Galovan AM. Pornography Use: Who Uses It and How It Is Associated With Couple Outcomes. J Sex Res (2013) 50:72–83. doi: 10.1080/00224499.2011.648027
11. Stulhofer A, Busko V, Landripet I. Pornography, Sexual Socialization, and Satisfaction Among Young Men. Arch Sex Behav (2010) 39:168–78. doi: 10.1007/s10508-008-9387-0
12. Day A. Getting the 'Blues': The Existence, Diffusion and Influence of Pornography on Young Peoples' Sexual Health in Sierra Leone. Cult Health Sex (2014) 16:178–89. doi: 10.1080/13691058.2013.855819.\
13. Babchishin KM, Hanson RK, VanZuylen H. Online Child Pornography Offenders are Different: A Meta-Analysis of the Characteristics of Online and Offline Sex Offenders Against Children. Arch Sex Behav (2015) 44:45–66. doi: 10.1007/s10508-014-0270-x
14. Voon V, Mole TB, Banca P, Porter L, Morris L, Mitchell S, et al. Neural Correlates of Sexual Cue Reactivity in Individuals With and Without Compulsive Sexual Behaviours. PloS One (2014) 9:e102419. doi: 10.1371/journal.pone.0102419
15. Happer C, Hodgins DC. Examining Correlates of Problematic Internet Pornography Use Among University Students. J Behav Addict (2016) 5:179–91. doi: 10.1556/2006.5.2016.022
16. Sun C, Bridges A, Johnson JA, Ezzell MB. Pornography and the Male Sexual Script: An Analysis of Consumption and Sexual Relations. Arch Sex Behav (2016) 45:983–94. doi: 10.1007/s10508-014-0391-2
17. Parhar IS, Ogawa S, Ubuka T. Reproductive Neuroendocrine Pathways of Social Behavior. Front Endocrinol (2016) 7:28. doi: 10.3389/fendo.2016.00028
18. Sisk CL, Zehr JL. Pubertal Hormones Organize the Adolescent Brain and Behavior. Front Neuroendocrin (2005) 26:163–74. doi: 10.1016/j.yfrne.2005.10.003
19. Schulz KM, Richardson HN, Zehr JL, Osetek AJ, Menard TA, Sisk CL. Gonadal Hormones Masculinize and Defeminize Reproductive Behaviors During Puberty in the Male Syrian Hamster. Horm Behav (2004) 45:242–9. doi: 10.1016/j.yhbeh.2003.12.007
20. Yang H, Chen Q, Zhou N, Sun L, Bao H, Tan L, et al. Lifestyles Associated With Human Semen Quality: Results From MARHCS Cohort Study in Chongqing, China. Med (Baltimore) (2015) 94:e1166. doi: 10.1097/MD.0000000000001166
21. Baltieri DA, Aguiar AS, de Oliveira VH, de Souza Gatti AL, de Souza Aranha ESRA. Validation of the Pornography Consumption Inventory in a Sample of Male Brazilian University Students. J Sex Marital Ther (2015) 41:649–60. doi: 10.1080/0092623X.2014.958793
22. Kor A, Zilcha-Mano S, Fogel YA, Mikulincer M, Reid RC, Potenza MN. Psychometric Development of the Problematic Pornography Use Scale. Addict Behav (2014) 39:861–8. doi: 10.1016/j.addbeh.2014.01.027
23. Grubbs JB, Exline JJ, Pargament KI, Hook JN, Carlisle RD. Transgression as Addiction: Religiosity and Moral Disapproval as Predictors of Perceived Addiction to Pornography. Arch Sex Behav (2015) 44:125–36. doi: 10.1007/s10508-013-0257-z
24. Harkness EL, Mullan BM, Blaszczynski A. Association Between Pornography Use and Sexual Risk Behaviors in Adult Consumers: A Systematic Review. Cyberpsychol Behav Soc Netw (2015) 18:59–71. doi: 10.1089/cyber.2014.0343
25. Kraus S, Rosenberg H. The Pornography Craving Questionnaire: Psychometric Properties. Arch Sex Behav (2014) 43:451–62. doi: 10.1007/s10508-013-0229-3
26. WHO. WHO Laboratory Manual for the Examination and Processing of Human Semen. 5th ed. Geneva, Switzerland: WHO Press (2010).
27. Limb M. Internet Pornography is an Urgent Public Health Issue, Conference Hears. BMJ (2014) 348:g4475. doi: 10.1136/bmj.g4475
28. Laws I. Better Sex Education for Children is Needed to Combat Dangers of Pornography. BMJ (2013) 347:f5764. doi: 10.1136/bmj.f5764
29. Mattebo M, Tyden T, Haggstrom-Nordin E, Nilsson KW, Larsson M. Pornography and Sexual Experiences Among High School Students in Sweden. JDBP (2014) 35:179–88. doi: 10.1097/DBP.0000000000000034
30. Mohsen J, Tai HL. The Youth Sexuality Study Task Force. Sexual Media Use by Young Adults in Hong Kong: Prevalence and Associated Factors. Arch Sex Behav (2003) 32:545–53. doi: 10.1023/a:1026089511526
31. American Society of Addiction Medicine (ASAM). Public Policy Statement: Definition of Addiction. Available at: http://www.asam.org/for-the-public/definition-of-addiction.
32. Christensen JF. Pleasure Junkies All Around! Why It Matters and Why 'The Arts' Might Be the Answer: A Biopsychological Perspective. Proc Biol Sci (2017) 284:20162837. doi: 10.1098/rspb.2016.2837
33. Kuhn S, Gallinat J. Brain Structure and Functional Connectivity Associated With Pornography Consumption: The Brain on Porn. JAMA Psychiatry (2014) 71:827–34. doi: 10.1001/jamapsychiatry.2014.93
34. Rohayem J, Hauffa BP, Zacharin M, Kliesch S, Zitzmann M, German Adolescent Hypogonadotropic Hypogonadism Study Group. Testicular Growth and Spermatogenesis: New Goals for Pubertal Hormone Replacement in Boys With Hypogonadotropic Hypogonadism? -A Multicentre Prospective Study of hCG/rFSH Treatment Outcomes During Adolescence. Clin Endocrinol (Oxf) (2017) 86:75–87. doi: 10.1111/cen.13164
35. Matsumoto AM, Snyder PJ, Bhasin S, Martin K, Weber T, Winters S, et al. Stimulation of Spermatogenesis With Recombinant Human Follicle-Stimulating Hormone (Follitropin Alfa; GONAL-F): Long-Term Treatment in Azoospermic Men With Hypogonadotropic Hypogonadism. Fertil Steril (2009) 92:979–90. doi: 10.1016/j.fertnstert.2008.07.1742
36. Awoniyi CA, Reece MS, Hurst BS, Faber KA, Chandrashekar V, Schlaff WD. Maintenance of Sexual Function With Testosterone in the Gonadotropin-Releasing Hormone-Immunized Hypogonadotropic Infertile Male Rat. Biol Reprod (1993) 49:1170–6. doi: 10.1095/biolreprod49.6.1170
37. De Rosa M, Zarrilli S, Di Sarno A, Milano N, Gaccione M, Boggia B, et al. Hyperprolactinemia in Men: Clinical and Biochemical Features and Response to Treatment. Endocrine (2003) 20:75–82. doi: 10.1385/ENDO:20:1-2:75
38. Cornwell RE, Law Smith MJ, Boothroyd LG, Moore FR, Davis HP, Stirrat M, et al. Reproductive Strategy, Sexual Development and Attraction to Facial Characteristics. Philos Trans R Soc Lond B Biol Sci (2006) 361:2143–54. doi: 10.1098/rstb.2006.1936
39. Luder MT, Pittet I, Berchtold A, Akre C, Michaud PA, Suris JC. Associations Between Online Pornography and Sexual Behavior Among Adolescents: Myth or Reality? Arch Sex Behav (2011) 40:1027–35. doi: 10.1007/s10508-010-9714-0
40. Perry SL. Is the Link Between Pornography Use and Relational Happiness Really More About Masturbation? Results From Two National Surveys. J Sex Res (2020) 57:64–76. doi: 10.1080/00224499.2018.1556772
Keywords: pornography, addiction, reproductive hormone, semen quality, college students
Citation: Cui Z, Mo M, Chen Q, Wang X, Yang H, Zhou N, Sun L, Liu J, Ao L and Cao J (2021) Pornography Use Could Lead to Addiction and Was Associated With Reproductive Hormone Levels and Semen Quality: A Report From the MARHCS Study in China. Front. Endocrinol. 12:736384. doi: 10.3389/fendo.2021.736384
Received: 05 July 2021; Accepted: 17 August 2021;
Published: 10 September 2021.
Edited by:
Richard Ivell, University of Nottingham, United KingdomReviewed by:
Zengjun Wang, Nanjing Medical University, ChinaCopyright © 2021 Cui, Mo, Chen, Wang, Yang, Zhou, Sun, Liu, Ao and Cao. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jia Cao, Y2FvamlhMTk2MkAxMjYuY29t
†These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.