- 1Department of Endocrinology, Shandong Provincial Hospital, Cheeloo College of Medicine, Shandong University, Jinan, China
- 2Shandong Clinical Medical Center of Endocrinology and Metabolism, Shandong Academy of Clinical Medicine, Jinan, China
- 3Institute of Endocrinology and Metabolism, Shandong Academy of Clinical Medicine, Jinan, China
- 4Department of Endocrinology, Shandong Provincial Hospital Affiliated to Shandong First Medical University, Jinan, China
- 5Health Management Center, Shandong Provincial Hospital Affiliated to Shandong First Medical University, Jinan, China
- 6Department of Scientific Center, Shandong Provincial Hospital Affiliated to Shandong First Medical University, Jinan, China
A Corrigendum on
High Circulating Follicle-Stimulating Hormone Level Is a Potential Risk Factor for Renal Dysfunction in Post-Menopausal Women
By Li Q, Zheng D, Lin H, Zhong F, Liu J, Wu Y, Wang Z, Guan Q, Zhao M, Gao L and Zhao J (2021). Front. Endocrinol. 12:627903. doi: 10.3389/fendo.2021.627903
In the original article, there was a mistake in Supplementary Table 2D as published. The Supplementary Table 2D was used to show the association between FSH quartiles and the presence of renal dysfunction in postmenopausal women with diabetes by multivariate logistic regression. Due to our fault, the content of the table was mistakenly inserted as the total data in postmenopausal women (the correct data should be in postmenopausal women with diabetes). The corrected Supplementary Table 2D appears below. The authors apologize for this error and state that this does not change the scientific conclusions of the article in any way. The original article has been updated.
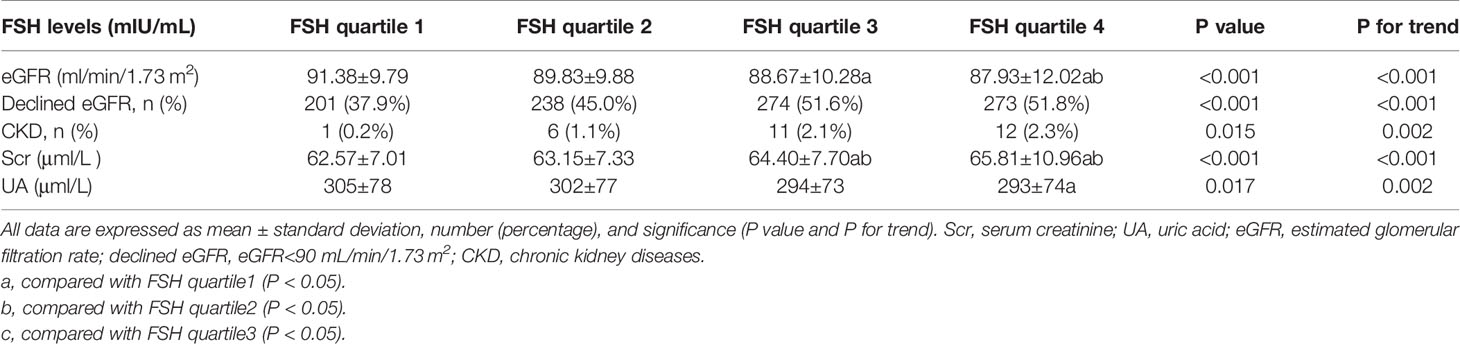
Supplementary Table 2a Comparisons among groups according to FSH quartiles in postmenopausal women without diabetes.

Supplemetary Table 2b Multivariate stepwise logistic regression of FSH quartiles for the presence of renal dysfunction in postmenopausal women without diabetes.
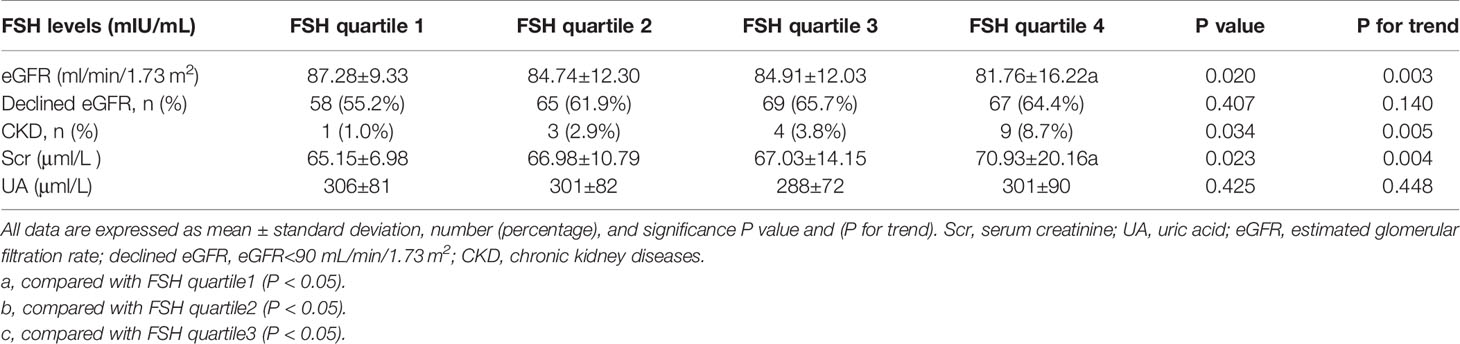
Supplementary Table 2c Comparisons among groups according to FSH quartiles in postmenopausal women with diabetes.
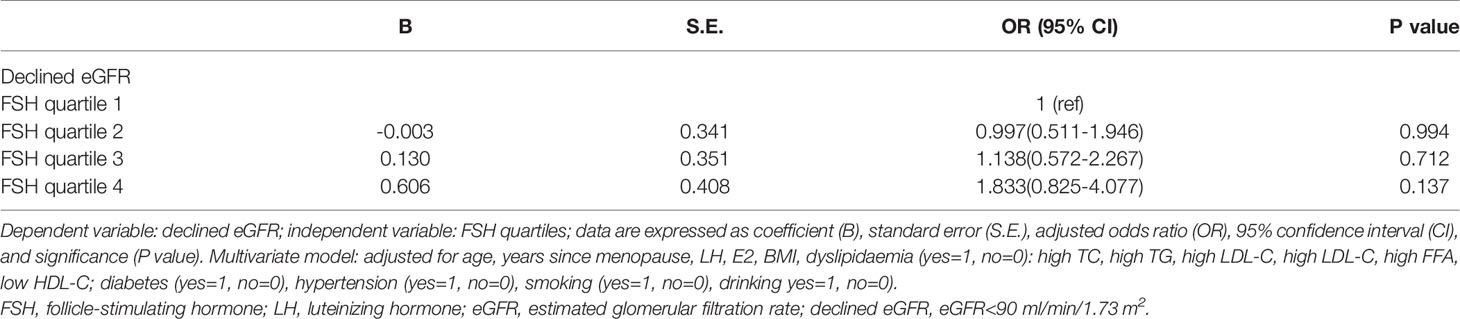
Supplementary Table 2d Multivariate logistic regression of FSH quartiles for the presence of renal dysfunction in postmenopausal women with diabetes.
In the original article, there was an error. The definition of pre-menopause and peri-menopause in section of Materials and Methods was not accurate enough.
A correction has been made to Materials and Methods, Definitions of Study Outcomes, 1:
Menopausal status was determined based on responses to a self-report questionnaire regarding menstrual history or amenorrhea. Pre-menopause was defined as the presence of menses within the past 3 months. Peri-menopause was defined as the presence of menses within the past 3 months with menstrual irregularity in the year preceding the questionnaire, or 3–11 months of amenorrhea. We selected subjects with 3–11 months of amenorrhea as peri-menopause because their E2 levels were similar to those in post-menopause. Post-menopause was defined as the cessation of menstruation for a minimum of 12 months (17, 19). Renal dysfunction was defined as declined estimated glomerular filtration rate (eGFR<90 ml/min/1.73 m2) or CKD (eGFR<60 ml/min/1.73 m2). Dyslipidaemia was defined as follows: 1) high total cholesterol (≥ 6.22 mmol/l); 2) high triglyceride (≥1.70 mmol/l); 3) high low-density lipoprotein cholesterol (≥ 4.14 mmol/l); 4) high free fatty acids (≥ 0.9 mmol/l); and 5) low high-density lipoprotein cholesterol <1.30 mmol/l) (20). Hypertension and diabetes were diagnosed based on self-reported previous diagnosis, or were defined as systolic blood pressure ≥130 mmHg or diastolic blood pressure ≥ 85 mmHg for hypertension (21) and fasting plasma glucose ≥7.0 mmol/l or post-prandial 2-h plasma glucose ≥11.1 mmol/l for diabetes (we chooe the former). Never smoking or drinking was assigned a value of 0; otherwise, it was assigned a value of 1.
The authors apologize for these errors and state that this does not change the scientific conclusions of the article in any way. The original article has been updated.
Publisher’s Note
All claims expressed in this article are solely those to the authors and do not necessarily represent those of their affiliated organization, or those of the publisher, the editors and reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fendo.2021.710836/full#supplementary-material
Keywords: FSH, menopause, eGFR, CKD, renal dysfunction, aging
Citation: Li Q, Zheng D, Lin H, Zhong F, Liu J, Wu Y, Wang Z, Guan Q, Zhao M, Gao L and Zhao J (2021) Corrigendum: High Circulating Follicle-Stimulating Hormone Level Is a Potential Risk Factor for Renal Dysfunction in Post-Menopausal Women. Front. Endocrinol. 12:710836. doi: 10.3389/fendo.2021.710836
Received: 17 May 2021; Accepted: 28 July 2021;
Published: 31 August 2021.
Edited and reviewed by:
Marc R. Blackman, Washington DC VA Medical Center, United StatesCopyright © 2021 Li, Zheng, Lin, Zhong, Liu, Wu, Wang, Guan, Zhao, Gao and Zhao. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jiajun Zhao, amp6aGFvQHNkdS5lZHUuY24=
 Qihang Li
Qihang Li Dongmei Zheng2,3,4
Dongmei Zheng2,3,4 Yafei Wu
Yafei Wu Qingbo Guan
Qingbo Guan Ling Gao
Ling Gao Jiajun Zhao
Jiajun Zhao