
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Disaster Emerg. Med. , 28 October 2024
Sec. Emergency Health Services
Volume 2 - 2024 | https://doi.org/10.3389/femer.2024.1440545
 Romain Betz1,2*
Romain Betz1,2* Allison Gilbert2
Allison Gilbert2 Didier Moens1,2
Didier Moens1,2 Laurent Marissiaux1,2
Laurent Marissiaux1,2 Meryl Paquay2,3
Meryl Paquay2,3 Raphaëlle Lopez Iglesias2
Raphaëlle Lopez Iglesias2 Olivier Pirotte2
Olivier Pirotte2 Alexandre Ghuysen2,3
Alexandre Ghuysen2,3 Samuel Stipulante1,3
Samuel Stipulante1,3Introduction: The utilization of Clinical Ultrasound (CUS) in Helicopter Emergency Medical Services (HEMS) has become increasingly prevalent, reflecting its significant role in emergency care.
Methods: This descriptive, monocentric study, conducted at the Helicopter Medical Center (CMH) of Bra-sur-Lienne, Belgium, aimed to describe the use of CUS within HEMS and evaluate its potential impact on diagnostic accuracy, therapeutic interventions, and hospital destination decisions.
Results: Over a 5-year period, from January 2018 to December 2022, our retrospective analysis included 6,126 HEMS interventions, with CUS performed in 29.55% of cases. The study demonstrated that CUS led to therapeutic changes in 30.88% of instances and affected the hospital destination in 9% of cases, despite a potential bias toward directing patients to the University Hospital Center of Liège (CHU of Liège) due to operational constraints. The agreement between prehospital CUS findings and hospital imaging was substantial, with an 80.39% concordance rate, underscoring CUS's utility in enhancing prehospital diagnostic accuracy. We found no significant increase in on-scene time due to CUS usage, with most exams completed in <5 min.
Discussion: Our findings highlight the interesting role of CUS in HEMS, facilitating more informed and confident medical decision-making in prehospital emergency care. However, variability in CUS application emphasize the need for standardized guidelines to optimize its use. The study's limitations include its retrospective, monocentric design and the focus on on-scene ultrasound evaluations. Future research should aim at a more extensive, prospective analysis to further validate the benefits of CUS in emergency medical services.
Point-of-care ultrasonography (POCUS) usually refers to a multidisciplinary field of ultrasound use, defined as the acquisition, interpretation, and immediate clinical integration of ultrasonographic imaging performed by clinicians at the point of care (1). More specifically, the policy statement of the American College of emergency physicians defined clinical ultrasound as the medical use of ultrasound technology for bedside clinical evaluation of acute or critical medical conditions. As such, it is typically performed and interpreted by various clinicians, in the setting of emergency department (ED) or in pre-hospital settings. Indeed, clinical ultrasound (CUS) use in emergencies situations has expanded rapidly to become an integral aspect of emergency care (2). Consequently, the task force supporting the development of the Model of the clinical practice of emergency medicine, a collaboration of six major organizations in the field of emergency medicine, has recently recommended to focus on ultrasound as a procedure and integral skill to the practice of emergency medicine (3).
As expected, emergency ultrasound examination has also expanded to the prehospital field thanks to technological advances and the miniaturization of the main equipment, making its use realistic even in the most complex situations (4). In prehospital settings, CUS has been used as a decision-making support tool regarding diagnosis, treatment, or the choice of the most appropriate destination for the patient. However, according to Rudolph et al. more evidence still seems to be required to demonstrate its actual impact in clinical practice (5). Several authors have already pointed out the value of prehospital ultrasound in the context of polytrauma management (eFAST method), cardiac pathologies or cardiac arrest (transthoracic ultrasound), respiratory failure (BLUE protocol), shock (RUSH protocol), and assistance with airway management, vascular access, or musculoskeletal assessment (6, 7).
We therefore designed the present study with the primary aim to delineate the operational profile of CUS use in a HEMS in Belgium, which include indications and CUS characteristics (type, location, and duration of the exam). We further sought to evaluate its potential impact on therapeutic interventions, decisions regarding hospital destinations and the accuracy of prehospital ultrasound findings as regards hospital findings.
We designed a monocenter retrospective study in the helicopter medical center (CMH) of Bra sur Lienne in Belgium. The center was created in December 1986 to respond to the need for emergency care in underserved rural areas. The center is currently composed of 12 physicians (emergency physicians and anaesthesiologists), 11 emergency nurses and six pilots. All physicians involved in the center are specifically trained implying to be certified as specialized in emergency medicine, prehospital care and disaster medicine but also trained in CUS. CMH main activity is dedicated to helicopter medical services, but the center also provides ground emergency medical services when air transport is not feasible. The CMH is part of the Emergency Medical Service related to the 112 emergency dispatching number, in the Walloon region of Belgium. During the period covered by the study, the helicopter flew an average of 1,225 missions per year. The geographical area covered is large and extends mainly over three provinces of the country. Patients were sent to the nearest and most appropriate hospital. The majority of missions focus on pre-hospital emergency care, with a small percentage consisting of interhospital transfers. For the CUS examination portable, the devices used were Sonosite Iviz, Fujifilm Sonosite, Inc. These devices were available on a daily basis for the physician to perform any assessment needed.
All data were collected regarding the selected study period extending from January 1st, 2018, to December 31th, 2022.
Data related to the HEMS missions characteristics and patient population were obtained through a retrospective analysis of the CMH center's electronic and 112 dispatching center database and from the medical datafile of the Liege University Hospital Center.
Specifically, each mission culminates in a comprehensive digital medical report, which is stored within a specialized platform overseen by the CMH center. For each patient considered, emergency room management data were extracted from a review of the hospital medical electronic datafiles. The patient data were only available at the university hospital of Liège during they stay in emergency department. Data from the other hospitals weren't accessible.
All helicopter interventions carried out during the study period were selected, including inter-hospital transfers, even if these represent only an anecdotal part of the helicopter's activity. The CUS is always performed by the physician. Anesthesiologists and emergency physicians compose the medical team. The ultrasound machine used is an iVIZ type device from Fujifilm Sonosite that can be used with a cardiac probe, an abdominal probe or a high-frequency linear probe. The ultrasound of the trauma patient is always performed according to the extended FAST protocol (eFAST). Cardiac ultrasound is based on the simple “4F” protocol (Function, Form, Fluid, Filling). Lung ultrasound is based on the “blue protocol”. Ultrasound of the abdominal aorta is based on a simple five-section diagram (three transverse sections and one longitudinal section on the abdominal aorta as well as a transverse section on the iliac arteries just below the bifurcation).
The epidemiological assessment of CMH operations utilized data from interventions coordinated through the 112 medical dispatching. This research examined various aspects including the frequency of missions, the timing of these missions (daytime between 8:00 and 21:59 and after-hours between 22:00 and 7:59), patient transportation, factors leading to non-transport, and the destination of the patient. The characteristics of the population were collected: age, gender, National Advisory Committee for Aeronautics (NACA) score and the outcome of the patient at the end of emergency department care.
Data concerning CUS examination were collected through a retrospective exam of the intervention reports for the study period.
Several selected variables were collected:
• the number of CUS performed
• the type of CUS was classified into different categories:
- focused assessment by sonography for trauma or eFAST
- heart ultrasound
- lung ultrasound
- abdominal ultrasound
- cardiothoracic ultrasound
- cardiothoracic combined with abdominal ultrasound
- others
• the duration of the CUS and the place where the CUS was performed (air or ground).
Some medical files were incomplete and some datas were missing. We did not exclude cases with incomplete data.
As previously mentioned, at the conclusion of each urgent mission, the physician in charge completed a computerized intervention report detailing all aspects of the patient's care.
When a CUS was performed, the physician had to specify it's modality (eFAST, cardiac, pulmonary, abdominal, aortic, etc.), the duration of the examination and the location where it was conducted (on site or in flight). Comprehensive report of the exam was then written. Finally, two questions were asked:
1. did the physician change the hospital destination based on the CUS result? No need to specify the reason.
2. did the physician modify the treatment according to the CUS findings (therapeutic action or therapeutic abstention)? No further clarification required after completing the CUS.
A retrospective analysis of the physician's decisions following CUS was performed in view of the choice made in terms of therapeutic options (medical or interventional) and hospital destination. Thus, it was the investigator who, through a thorough review of the intervention reports, deduced the actions taken based based on the CUS finding.
Data analysis regarding the agreement between prehospital CUS and hospital findings was performed regarding the patients admitted to the University Hospital Center of Liège because the data for the other patients were not available retrospectively. To account for potential discrepancies between ultrasounds conducted on-scene vs. those performed in-flight, the study focused solely on ultrasounds executed on-scene (8). In-flight examinations were excluded because destination is defined as soon as the helicopter takes off. Furthermore, the CHU of Liège is typically the closest hospital to the interventions of the CMH of Bra-sur-Lienne, leading to very short flight durations. These brief flight times often did not allow sufficient time to perform ultrasounds in transit, which is why we ultimately could not include these data in the study.
All eligible files for the comparison were retrospectively assessed by one investigator who attributed an agreement score between the CUS results and the hospital imaging findings. These hospital images encompassed a range of radiological modalities, including CT scans, ultrasound, and other radiographic techniques, providing a comprehensive basis for comparison and assessment. The agreement score was categorized by three possibilities: full agreement, partial agreement, and no agreement. Partial agreement refers to the identification of multiple anomalies in the hospital findings that were not all described in the prehospital CUS. CUS images weren't recorded according to the General Data Protection Regulation rules in our country. However, the ultrasound reports from the CMH of Bra-sur-Lienne, along with all imaging reports from the CHU of Liège, were available to the researcher. The investigator was blinded to the outcome of the study.
The study was approved by the Ethics Board of the University of Liège (ref. 2023/139).
The results were encoded in a database and anonymized. The results were expressed as medians and percentiles (P25-P75) for quantitative variables and as counts and proportions (%) for qualitative variables. The analysis was carried out using R software.
From 1 January 2018 to 31 December 2022, the HEMS activity of the CMH accounted for 6,126 interventions: 5,471 during daytime (89.31%) and 655 out-of-hours (10.69%).
After on-scene assessment by the HEMS team, the patient was transported to the hospital in 5,369 interventions (87.64%). Among these, 2,727 (50.79%) patients were transported by the HEMS, 2,414 (44.96%) by ambulance alone, 159 (2.96%) by ambulance and ground emergency medical services, 62 (1.15%) by paramedical intervention team (PIT) and 7 (0.13%) by paramedical intervention team and emergency medical services.
In 757 interventions (12.36%), no transport was needed. The main reasons for non-transport were: patient death (75.56%; n = 572), transport not required (17.97%; n = 136), no patient on site (0.26%; n = 2), patient refusal (5.55%; n = 42), unspecified reasons (0.53%; n = 4), and the intervention cancel (0.13%; n = 1).
Among the 5,369 patients transported to the hospital, 3,741 (69.67%) were transported to the nearest hospital infrastructure, 1,311 (24.42%) were dispatched to another hospital for a specialized intervention, 253 (4.71%) were oriented to another hospital for unspecified reasons, 47 (0.88%) were transported to another hospital because of bed unavailability. Transport data were missing for 17 (0.32%) patients.
Among the 6,126 patients managed by the HEMS, the median age was 59.25 years-old (38.9–74.2). The interventions involved 3,793 males (61.92%) and 2,333 females (38.08%). The NACA scores of the patients were represented as follows: 1 patient (0.02%) with a NACA score of 0, 43 patients (0.70%) with a NACA score of 1, 389 patients (6.35%) with a score of 2, 2,132 patients (34.80%) with a score of 3, 1,688 patients (27.55%) with a score of 4, 1,074 patients (17.53%) with a score of 5, 219 patients (3.57%) with a score of 6, and 580 patients (9.47%) with a score of 7.
Regarding patient outcomes, 5,546 patients (90.53%) survived the prehospital phase of their care, whereas 564 (9.21%) were declared dead on scene, and 16 (0.26%) died in the emergency department. The main diagnoses suggested by the physician at the end of the intervention were related to trauma, wounds, or burns in 13.03% of the cases (N = 798), cardiac arrest (all causes) in 12.36% (N = 757) and respiratory failure in 10.01% (N = 613).
The detailed characteristics of the population are shown in Table 1.
Among the 6,126 interventions during the study period, 1,810 ultrasound exams were performed (29.55%). The predominant categories of ultrasounds performed included: eFAST for 551 patients (30.45%), cardiac for 471 patients (26.02%), and cardiothoracic for 225 patients (12.43%). The ultrasound duration predominantly fell under 5 min, accounting for 64.75% of cases, while durations between 5 and 10 min were observed in 6.96% of cases (N = 126), and a duration between 10 and 15 min was noted in a single case (0.006%). In 28.23% of cases, data on exam duration was missing due to incomplete information in the medical report. Most ultrasounds were conducted on-scene, comprising 65.64% of instances, as opposed to in-flight ultrasounds, which made up 6.46%. Data were missing in 27.90% of the cases.
The characteristics of the CUS are detailed in Table 2.
When CUS was performed (N = 1,810), it led to a therapeutic change (medication or technical procedure) in 30.88% of the cases (N = 559). Conversely, in 41.22% of the cases (N = 746), the treatment regimen remained unchanged. Data were missing in 27.90% of the cases (N = 505).
CUS examination led to a change in the hospital destination in 9% of the cases (N = 163) whereas in 63.09% of the cases (N = 1,142), no modification was suggested.
Data are missing in 27.90% of the cases (N = 505).
The subcohort for the analysis of the agreement between CUS findings and hospital findings was composed of 822 (45.4%) ultrasound exams. Among these exams, we noted 266 cardiac ultrasounds (32.36%), 231 eFAST (28.10%), 136 cardiothoracic ultrasounds (16.55%), 92 cardiothoracic and abdominal ultrasounds (11.19%), 45 lung ultrasounds (5.47%), 17 abdominal ultrasounds (2.07%), and 4 others (0.49%). Data were missing for 31 ultrasounds (3.77%).
Among the 822 ultrasounds, only 709 complete reports were available (86.25%).
The main anomalies are described in Table 3.
A full agreement was found in 570 cases of CUS (80.39%) whereas in 112 (15.80%) ultrasounds findings were not concordant. For 27 ultrasounds (3.81%) data were missing to assess the agreement. The agreement of CUS in the prehospital setting was then estimated at 80.39%. In the analysis of 112 instances where the findings from CUS ultrasound were not in agreement, we found false negative results in 65 cases (58.04%), when CUS didn't identified abnormal findings. Conversely, in 47 cases (41.96%), there were abnormal findings reported in the CUS findings that did not align with the hospital observations.
Partial agreement was found in 11 cases (1.55%) related to the eFAST type, cardiac ultrasound, cardiothoracic and cardiothoracic and abdominal ultrasounds.
The main findings are detailed in Table 4.
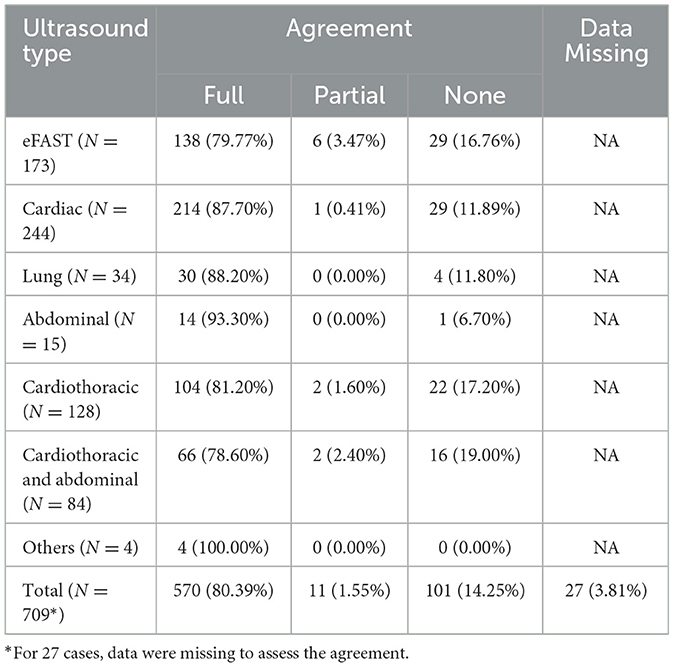
Table 4. Full agreement, partial agreement or no agreement between ultrasound findings and hospital findings.
Use of emergency ultrasound examination in helicopter emergency services has taken an important place in daily practice. However, evidence is still lacking regarding the impact, benefits, and risks of this practice (9).
In Europe, the practice of prehospital ultrasound within helicopter medical services (HEMS) seems particularly developed, as reported by a recent survey study by Hilbert-Carius et al. Indeed, these authors reported that 75% of HEMS organizations were currently using ultrasound in their daily practice (10). A second study by Naeem et al. suggested that, although physicians were interested and keen to use CUS, there was a lack of recognition of the practice (11).
One important point to evoke regarding CUS is the balance between the concrete benefits of its use compared with the potential pitfalls. A frequently reported caveat is that the use of ultrasound in the prehospital setting may slow down patient transport to the hospital and therefore potentially result in adverse events. In a study comparing the on-scene time of patients with or without ultrasound, Onotera et al. reported no significant difference in the time taken to manage patients who had received ultrasound (12).
While some authors are enthusiastic about the value of ultrasound in better dispatching patients in the prehospital setting, getting them to the most suitable hospital infrastructure, a lack of evidence persists, particularly regarding the benefit in terms of mortality reduction (13). Finally, several authors described CUS as a beneficial decision-making support tool in helping identify the correct diagnosis or to highlight abnormal findings (14).
The present results of our experience in the CMH service reveal that ultrasound examination is frequently used, as almost one-third of the interventions benefited from it, a higher rate than previously reported in HEMS (15, 16). The scope of CUS in CMH activities is vast, and different types of ultrasound examinations are performed in view of the various conditions encountered. For most of the extra hospital patients, clinical ultrasound does not provide immediate added value (e.g., isolated head trauma, isolated limb injury, stroke, altered state of consciousness, epilepsy, hypoglycemia, etc.) but for a part of them, CUS can provide the solution or, at the very least, valuable help hat can make the difference. It is for this category of patients that the rate of use of clinical ultrasound is important to consider.In a survey study among Canadian aeromedical service providers, Sedlakova et al. also reported that ultrasound examination was used for various reasons from abdominal free fluid to pneumothorax and cardiac arrest (17). In another survey in UK, HEMS providers perceived CUS as a technique to guide and enhance clinical management but also as a useful help in interventional procedures (11).
One question investigated in this study was the impact of CUS on therapeutic management and dispatching strategy. Indeed, as Sedlakova et al. reported in their survey, many providers believe that it could have a favorable impact on patient management and should thus be better deployed in the daily practice of HEMS (17). However, further evidence is needed to generalize its specific use in HEMS. In our study, we observed that CUS resulted in a change in therapeutic management in 30.88% of cases where data were available (data were missing in 27.90% of cases). In our practice, eFAST, cardiac, and pulmonary ultrasounds alone account for nearly 70% of the CUS performed. In another experiment regarding changes in patient management after prehospital ultrasound, CUS influenced the management of patients in 49.5% of the cases (18). Regarding specific conditions, prehospital ultrasound could have a different impact on patient management. Indeed, Ketelaars et al. reported that in cases of prehospital cardiac arrest the therapeutic decision can be influenced or supported by ultrasound exam in up to 88% of the cases (19).
We investigated the ability of the ultrasound to accurately identify abnormal findings in view of the hospital findings. Our study shows that prehospital ultrasound could represent an interesting technique to improve the accuracy of the diagnosis approach by identifying abnormalities as soon as the HEMS interventions. Indeed, the agreement between prehospital findings and hospital findings reached an 80.39% rate. This finding is similar to a recent study by Ienghong et al. reporting a 75.8% accuracy of the prehospital diagnosis using CUS compared to hospital findings (20). Another report estimated that the accuracy could reach up to 90%. This could be a benefit for the patient as the HEMS physician can inform the hospital team to deploy the human and technical resources required earlier and offer the most appropriate care.
In that view, it should be mentioned that the training of the physicians who performed the prehospital ultrasound seems to be a key factor influencing the accuracy of ultrasound findings compared to hospital ones (17, 18, 20). Regarding the dispatching strategy, in our experience, the CUS exam influenced patient's destination in 9% of the cases according to ultrasound findings. The hospital destination may be biased by the limited availability of landing options at all. Indeed, the helicopter often land at tertiary centers with advanced technical capabilities. This observation might represent another potential bias of our study, as a significant portion of patients were directed to the University Hospital of Liège, regardless of ultrasound use, either because it is the closest hospital or due to the impossibility of landing at an alternative hospital where the patient could have been taken otherwise.
This result might not be replicated in a road service scenario, where any hospital could be a potential destination. Similarly, a study in The Netherlands reported a 7.7% rate of changes regarding patient destination with the use of CUS for critically ill and injured patients. This too could be influenced by a bias, given the limited pre-hospital medicalization in The Netherlands. If an ultrasound is performed, it may indicate severe patient conditions, which would likely result in redirection to a major tertiary center over a closer destination hospital. These factors suggest that our findings and those from The Netherlands may not solely reflect the impact of CUS on patient dispatching but also the structural and operational peculiarities of emergency medical services in different regions.
Interestingly as concerns the impact of the CUS examination on the intervention time, we found that most ultrasound exam duration predominantly fell under 5 min. Similar results were reported in a recent study made in the Netherlands, where CUS was found not to prolong on-scene time. Indeed, it could often be performed simultaneously with other prehospital procedures like IV placement, monitoring and physical examination (21). Our study presents several limitations and some of its specificities need to be reported. We limited our study to ultrasounds performed on scene. We have not established criteria for deciding whether to use CUS. The physician decided by himself whether the ultrasound seemed useful and relevant for his patient. Our comparison focused on radiological findings rather than specific diagnoses, and we did not confine our analysis to any specific type of ultrasound or patient condition. Furthermore, the analysis regarding CUS accuracy only considered the patients who were admitted at one location, the University Hospital Center of Liège (CHU of Liège), because data were not available from other facilities. A single investigator was responsible for data collection. So there was no assessment of inter-rater reliability and the criteria used were based on clinical judgment, relying on the expertise of the clinicians. Furthermore, the nature of the therapeutic modifications proposed or withheld based on the CUS was not specified by the physician who performed the examination but was estimated by the investigator. A post-hoc comparison of the ultrasound examinations by an independent examiner was not possible. Only the written reports from the operators who performed the examinations could be compared because the ultrasound examinations performed were not recorded. We did not evaluate the mean time of interventions to investigate the impact of CUS on on-scene time.
Finally, this study is monocentric, has a retrospective design and several elements should be investigated more thoroughly in a prospective study. The descriptive nature of the study and the methodology used which the concordance between ultrasound findings and hospital results was determined by the investigator limitings the use of statistical tests. The results are expressed as a percentage of agreement, which does not formally exclude the possibility that part of this agreement may be due to chance.
Future research should focus more specifically on the nature of the therapeutic interventions prompted by CUS, moving beyond the mere observation that an action was taken in response to its findings. It would be valuable to identify which of these procedures had the greatest impact on patient care, particularly in terms of morbidity and mortality. Additionally, it is essential to explore the potential benefits of utilizing less conventional ultrasound modalities that are still being developed, such as optic nerve ultrasound in head trauma, bone ultrasound for limb fractures, and transcranial Doppler.
The retrospective analysis of the operational profile of CUS use within a Belgian HEMS for 5 years reveals that CUS examination was frequently performed by physicians to support their decisions in terms of therapeutic interventions. We found less impact on the decision regarding hospital destination mostly due to local operational constrains. The analysis of the agreement between pre-hospital CUS findings and hospital findings confirmed the pertinence of these examination and their potential to enhanced clinical diagnostic accuracy. Heterogeneity still exists in the practice of the daily use of CUS in HEMS. More recommendations could be useful to standardize daily practice of prehospital CUS.
The datasets presented in this article are not readily available because to comply with our ethics committee's regulations, the dataset must remain under the authors' discretion, as it contains sensitive patient information. Requests to access the datasets should be directed to the corresponding author.
The studies involving humans were approved by Ethics Board of the University of Liège (ref. 2023/139). The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants' legal guardians/next of kin in accordance with the national legislation and institutional requirements.
RB: Writing – review & editing, Writing – original draft. AGi: Writing – original draft. DM: Supervision, Writing – original draft, Writing – review & editing. LM: Validation, Writing – review & editing. MP: Methodology, Validation, Writing – review & editing. RL: Visualization, Writing – review & editing. OP: Resources, Validation, Writing – review & editing. AGh: Supervision, Validation, Writing – review & editing. SS: Formal analysis, Resources, Supervision, Validation, Writing – original draft, Writing – review & editing.
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Diaz-Gomez JL, Mayo PH, Koening SJ. Point-of-care ultrasonography. NEJM. (2021) 385:1593–602. doi: 10.1056/NEJMra1916062
2. American College of Emergency Physicians. Ultrasound guidelines: emergency, point-of-care, and clinical ultrasound guidelines in medicine. Ann Emerg Med. (2023) 82:e115–55. doi: 10.1016/j.annemergmed.2023.06.005
3. Beeson MS, Bhat R, Broder JS, Gaeta TJ, Janssen A, Karl ER, et al. The 2022 model of the clinical practice of emergency medicine. J Emerg Med. (2023) 64:659–95. doi: 10.1016/j.jemermed.2023.02.016
4. Nelson BP, Chason K. Use of ultrasound by emergency medical services: a review. Int J Emerg Med. (2008) 1:253–9. doi: 10.1007/s12245-008-0075-6
5. Rudolph SS, Sorensen MK, Svane C, Hesselfeldt R, Steinmetz J. Effect of prehospital ultrasound on clinical outcomes of non-trauma patients – A systematic review. Resuscitation. (2014) 85:21–30. doi: 10.1016/j.resuscitation.2013.09.012
6. Amaral CB, Ralston DC, Becker TK. Prehospital point-of-care ultrasound: a transformative technology. SAGE Open Med. (2020) 8:1–6. doi: 10.1177/2050312120932706
7. Ketelaars R, Hoogerwerf N, Jan Scheffer G. Prehospital chest ultrasound by a Dutch helicopter emergency medical service. J Emerg Med. (2013) 44:811–7. doi: 10.1016/j.jemermed.2012.07.085
8. Ketelaars R, Reijnders G, van Geffen GJ, Scheffer GJ, Hoogerwerf N. ABCDE of prehospital ultrasonography: a narrative review. Cri Ultrasound J. (2018) 10:17. doi: 10.1186/s13089-018-0099-y
9. Roantree AG, Furtado CS, Welch K, Lambert MJ. EMS Ultrasound Use. Treasure Island, FL: StatPearls Publishing (2022).
10. Hilbert-Carius P, Struck MF, Rudolp M, Knapp J, Rognas L, Adler J, et al. Point-of-care ultrasound (POCUS) practices in the helicopter emergency medical services in Europe: results of an online survey. Scand J Trauma Resusc Emerg Med. (2021) 29:124. doi: 10.1186/s13049-021-00933-y
11. Naeem S, Edmunds C, Hirst T, Williams J, Alzarrad A, Ronaldson J, et al. A national survey of prehospital care services of United Kingdom for use, governance and perception of prehospital point of care ultrasound. POCUS J. (2022) 7:232. doi: 10.24908/pocus.v7i2.15739
12. Onotera K, Ryan S, Jelic T. The effect of point-of-care ultrasound on helicopter EMS scene times. Ann Emerg Med. (2020) 76:S119. doi: 10.1016/j.annemergmed.2020.09.323
13. Bøtker MT, Jacobsen L, Rudolph SS, Knudsen L. The role of point of care ultrasound in prehospital critical care: a systematic review. Scand J trauma Resusc Emerg Med. (2018) 26:51. doi: 10.1186/s13049-018-0518-x
14. Partyka C, Coggins A, Bliss J, Burns B, Fiorentino M, Goorkiz P et al. A multicenter evaluation of the accuracy of prehospital eFAST by a physician-staffed helicopter emergency medical service. Emerg Radiol. (2022) 29:299–306. doi: 10.1007/s10140-021-02002-4
15. Weilbach C, Kobiella A, Rahe-Meyer N, Johanning K. Introduction of prehospital emergency ultrasound into an emergency medical service area. Anaesthesist. (2017) 66:21–7. doi: 10.1007/s00101-016-0248-2
16. Karfunkle B, Kit Chan H, Fisher B, Gill J, Bakunas C, Gordon R, et al. Prehospital ultrasound: nationwide incidence from the NEMSIS database. Prehosp Emerg Care. (2023) 28:515–30. doi: 10.1080/10903127.2023.2239353
17. Sedlakova A, Olszynski P, Davis P, Froh J. Prehospital ultrasound use among Canadian aeromedial service providers – A cross-sectional survey. CJEM. (2022) 22:338–41. doi: 10.1017/cem.2019.451
18. Scharonow M, Weilbach C. Prehospital point-of-care emergency ultrasound: a cohort study. Scand J Trauma Resuscit Emerg Med. (2018) 26:49. doi: 10.1186/s13049-018-0519-9
19. Ketelaars R, Beekers C, Van Geffen G, Scheffer G, Hoogerwerf N. Prehospital echocardiography during resuscitation impacts treatment in a physician-staffed helicopter emergency medical service: an observational study. Prehosp Emerg Care. (2018) 22:406–13. doi: 10.1080/10903127.2017.1416208
20. Ienghong K, Woon Cheung L, Tiamkao S, Bhudhisawasdi V, Apiratwarakul K. The utilization of handheld ultrasound devices in a prehospital setting. Prehosp Disaster Med. (2022) 37:355–9. doi: 10.1017/S1049023X22000644
21. Viannen NJ, Van Lieshout E, Vlasveld K, Maissan I, Gerritsen P, Den Hartog D et al. Impact of point-of-care ultrasound on prehospital decision making by HEMS physicians in critically ill and injured patients: a prospective cohort study. Prehosp Disast Med. (2023) 38:444–9. doi: 10.1017/S1049023X23006003
Keywords: clinical ultrasound, prehospital medicine, ultrasound, emergency medicine, helicopter medical services
Citation: Betz R, Gilbert A, Moens D, Marissiaux L, Paquay M, Lopez Iglesias R, Pirotte O, Ghuysen A and Stipulante S (2024) Prehospital point of care ultrasound in Helicopter Emergency Medical Services: a 5-year experience study in Belgium. Front. Disaster Emerg. Med. 2:1440545. doi: 10.3389/femer.2024.1440545
Received: 29 May 2024; Accepted: 29 September 2024;
Published: 28 October 2024.
Edited by:
Robert Ehrman, Wayne State University, United StatesReviewed by:
Lori Stolz, University of Cincinnati, United StatesCopyright © 2024 Betz, Gilbert, Moens, Marissiaux, Paquay, Lopez Iglesias, Pirotte, Ghuysen and Stipulante. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Romain Betz, ci5iZXR6QGNodWxpZWdlLmJl
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.