
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Disaster Emerg. Med. , 25 July 2024
Sec. Emergency Health Services
Volume 2 - 2024 | https://doi.org/10.3389/femer.2024.1397597
This article is part of the Research Topic Advancing Health Equity in Emergency Medicine: Addressing Disparities for Equity-Deserving Populations View all articles
 Melanie Walker1,2*
Melanie Walker1,2* Meredith MacKenzie3,4
Meredith MacKenzie3,4 Stuart L. Douglas1,5
Stuart L. Douglas1,5 Amanda Collier1
Amanda Collier1 Jodie Pritchard1
Jodie Pritchard1 Sharleen Hoffe1
Sharleen Hoffe1 Patrick A. Norman2,6
Patrick A. Norman2,6 Eva Purkey2,3
Eva Purkey2,3 David Messenger1,5
David Messenger1,5 Susan A. Bartels1,2
Susan A. Bartels1,2Background: Equity-deserving groups (EDGs) have increased emergency department (ED) use, and often report negative ED care. Past studies have largely been qualitative and suffer from methodological bias and lack of comparison groups, thereby limiting their identification of interventions to ensure equitable care among equity-deserving populations. This study sought to better understand ED care experiences among EDGs in our local setting.
Materials and methods: We conducted a community-engaged, mixed-methods cross-sectional study using sensemaking methodology at the Kingston Health Sciences Centre's ED and Urgent Care Centre (Ontario, Canada), as well as at community partner organizations. From June-August 2021, eligible participants were invited to complete a survey about an ED care experience within the previous 24 months. Multiple-choice questions collected demographic/ED visit information including self-identification with up to three EDGs (Indigenous; having a disability; experiencing mental health concerns; persons who use substances (PWUS); 2SLGBTQ+; people who experience homelessness (PWEH); a visible minority; or having experienced violence). We evaluated differences in overall ED care experiences by EDG self-identification using chi-squared tests. Quantitative analysis of survey questions disaggregated by EDG status, and a thematic analysis of participant experiences are presented.
Results: Overall, 1,973 unique participants completed the survey (949 controls and 994 EDGs) sharing 2,114 ED care experiences in total. Participants who identified as PWUS, having mental health concerns, 2SLGBTQ+, PWEH, or having a disability, reported more negative overall experiences (p < 0.001). Compared with controls, each of the eight EDGs were statistically more likely to report feelings of judgement/disrespect, that there was too little attention paid to their needs (p < 0.001), and that it was more important to be treated with kindness/respect than to receive the best possible care (p < 0.001). Thematic analysis supported quantitative findings and identified four themes: stigma/judgement, poor staff communication, lack of compassionate care, and patients feeling unsupported.
Discussion: Negative ED care experiences were pervasive among EDGs including feelings of judgement/stigma and a perception that a better understanding of personal situation/identity/culture was needed to improve care. Qualitative findings identified the following future interventions: universal trauma-informed care, improved care for addiction/substance use, and improved access to mental health care resources.
The Emergency Department (ED) plays an essential role in healthcare provision, particularly in settings where primary care access is limited, and its 24/7 open-door policy makes the ED a critical safety net for injured, ill, and otherwise unwell patients (1–3). Equity-deserving groups (EDGs) are defined as those who face significant challenges participating in society due to attitudinal, historic, social, and environmental barriers based on age, ethnicity, disability, economic status, gender, race, and sexual orientation, among others (4). EDGs, including those who experience unstable housing, poverty, social isolation, and marginalization, are known to more frequently access and rely upon emergency care in comparison to other groups (1–3, 5).
Patients from a variety of EDGs have reported negative ED care experiences including judgement, stigma, racism, and provider misconceptions about reasons for accessing the ED (6, 7). For example, people who use substances (PWUS) have reported that their ED care is negatively impacted by a variety of factors including persistent stigma and miscommunication, leading to reduced treatment efficacy (8–14). Similarly, patients facing mental health issues experience discriminatory attitudes (15–19), poor communication from ED staff (15, 17, 19–21), and challenges with systemic factors, such as long wait times (22) and inadequate discharge procedures (15, 23). Likewise, the literature demonstrates that people who experience homelessness (PWEH) face many interpersonal and structural barriers to receiving quality care in the ED (1, 5, 15–27), including stigma and discrimination, dismissal of concerns, physician stereotyping, and barriers to communication. PWEH have also been shown to face other constraints, such as care-associated costs, wait times, and poorly coordinated care (26–31). Further, 2SLGBTQ+ patients have reported negative ED experiences due to insufficient health care provider knowledge concerning diverse identities and health issues (32–34) as well as a lack of culturally competent care (35), leading to discomfort and discrimination with negative impacts on care-seeking behavior and disclosure (36). Additionally, Indigenous patients have reported judgement by staff and feel their health issues are dismissed or diminished because they are “read” by providers as being poor and having addictions (7). In at least one well-publicized Canadian case, racism directly contributed to an Indigenous patient's death in the ED (37).
While some empirical evidence on ED care experiences among EDGs exists, it is largely confined to qualitative studies, which have methodological limitations including selection bias, small sample sizes, narrow generalizability, and the inability to assess causal associations due to a lack of comparison groups. Further, data collection in earlier studies often relied solely on focus groups or interviews, which are susceptible to self-reporting and interviewer biases. Thus, existing data may be limited in its ability to help identify needed interventions to ensure equitable and high-quality ED care among equity-deserving community members.
To address these knowledge gaps and design limitations, we conducted a community-engaged, mixed-methods study at the Kingston Health Sciences Centre (KHSC) to better understand the ED care experiences among those who identify as equity-deserving compared with those who do not. The quantitative findings from this work comparing all EDGs with controls have been published elsewhere (38). Quantitative data demonstrated that compared to controls, members of EDGs reported more negative experiences, expressed feelings of judgement and disrespect, and felt that staff paid too little attention to their needs. Further, EDGs overall felt that more attention needed to be paid to their personal situation/identity/culture and that it was more important to be treated with kindness and respect than to receive the best medical care (38). The objective for the current analysis was to present the quantitative results among each unique EDG contextualized with findings from the participants' qualitative data and community focus groups to identify targeted interventions for ED care quality improvement.
We conducted a community-engaged, mixed-methods cross-sectional study using “sensemaking” (SM) methodology, an innovative narrative capture approach that is founded on the premise that storytelling is an inherent method for conveying complex information, which individuals use to make sense of their experiences (39–42). A mixed-methods approach allowed us to collect rich quantitative and qualitative data grounded in the lived experiences of participants (43). SM, specifically, provides a comprehensive understanding of complex issues by using indirect prompting questions to elicit more revealing responses (39, 44). Compared to other qualitative methods, such as interviews, SM greatly reduces both social desirability bias, as no one response is more socially acceptable than another within any given question, and interpretation bias, because participants, not researchers, interpret their own experiences. SM is also a highly efficient method for gathering hundreds of self-interpreted micronarratives.
Using a SM approach, between June to August 2021, participants were asked to audio-record an anonymous micronarrative in response to an open-ended prompt asking about an ED care experience within the previous 24 months, thereby generating the qualitative data. Participants then interpreted that experience by plotting their perspectives between three options (triads) or two options (sliders). SM then quantified each of the plotted points, providing the quantitative data backed up by the accompanying qualitative narratives (39). Multiple-choice questions collected demographic information and allowed patients to self-identify as a member of up to three EDGs. Participants could share more than one ED care experience from the previous 24 months, thus generating more survey responses than participants. Data was collected in English using the Spryng.io app on handheld tablets. Survey questions were informed and piloted by several community partners and their clients prior to data collection (see Appendix 1).
Data were collected from participants attending the KHSC ED and urgent care center (UCC). KHSC provides care for over 120,000 ill and injured patients per year as both a regional trauma and tertiary care center. It also serves as the sole points of hospital-based emergency care provision in Kingston, Ontario, a city recognized for its income and quality of living disparities (45). A team of trained Research Assistants (RAs) were on site from 9 a.m.−9 p.m. Monday to Friday during the three months of data collection. In addition, data collection occurred at several Kingston-based community organizations that provide support to equity-deserving populations (see Appendix 2).
Individuals aged 16 years or older with proficiency in English, who had attended the ED or UCC within the preceding 24 months were eligible for participation. Within the hospital, medically stable patients registering in the ED/UCC during study hours were invited to complete the survey. Clients accessing services through collaborating community partners were offered the same survey. Interviewing in the community supported the inclusion of equity-deserving individuals, and helped to reach those who may not be accessing ED care due to previous negative experiences. Equity-deserving individuals were defined as those who identified as (1) Indigenous; (2) having a disability; (3) experiencing mental health concerns; (4) persons who use substances (PWUS); (5) 2SLGBTQ+; (6) people who experience homelessness (PWEH); (7) a visible minority; and/or (8) having experienced violence.
The primary outcome measure was a comparison of self-described ED/UCC care experiences (positive, negative, or mixed) among each of the eight primary EDGs as well as among those who did not identify as equity-deserving.
Descriptive statistics with chi-squared tests identified differences in participant and ED visit characteristics between each of the eight EDGs and the control group (IBM SPSS Statistics V.26.0.0.0). Results were considered statistically significant at p < 0.05 and do not include missing data (including prefer not to say/do not know responses).
Quantitative data were exported into Tableau (V.2020.4) where collective plots were visually inspected to identify patterns in the data (46). Triad and slider data were disaggregated based on self-identification into each of the eight primary EDGs as well as those who did not identify as equity-deserving (controls). For the triad data, geometric means for each subgroup were produced in R Scripts (R V.3.4.0) as were the generated 95% confidence intervals, which are presented graphically as 95% confidence ellipses (47, 48). Two geometric means were considered statistically significantly different if their 95% confidence ellipses did not overlap. Slider data were generated graphically as histograms and the collective areas under the bars for each subgroup was analyzed in SPSS (IBM SPSS Statistics V.26.0.0.0) using the Kruskal-Wallis H test and chi-squared tests to determine if the bar areas were statistically different between groups (p < 0.05 considered statistically significant) (49, 50). Violin plots present the distributions of responses for the slider questions, with an asterisk demarcating the overall mean for each sub-group.
Qualitative data in the form of shared micronarratives of ED care experiences were imported into NVivo (v.12.7.0) for thematic analysis. A master codebook based on current evidence and the study survey was developed and used as a framework for the thematic analysis while also allowing new codes to be added inductively based on the shared experiences. Qualitative data was reviewed by at least two independent reviewers with regular meetings to compare coding, establish inter-rater reliability, and reach consensus. Codes were then organized into emerging themes with selection of representative quotes to highlight findings.
As described by Creswell and Clark (51), we used triangulation to look at the quantitative and qualitative data, assigning an equal weight to both, to build a coherent pattern from the data. This approach provides the advantage of corroborating quantitative findings with more nuanced qualitative results, thereby ensuring that the research yields more well-substantiated conclusions.
Service providers at community partner organizations and clients identifying as equity-deserving with lived experience visiting the local ED/UCC were invited to participate in focus group discussions (FGDs). These discussions were intended to help interpret study results, advise on whether findings aligned with their experiences, and identify strategies to improve KHSC ED/UCC care. FGDs were audio-recorded (in all but the Indigenous sharing circle) with participants' permission and transcribed for analysis.
This study was approved by the Queen's University Health Sciences and Affiliated Teaching Hospitals Research Ethics Board (6029400). Informed consent was obtained from all study participants prior to survey completion. No identifying information was collected; data were anonymous from the point of collection. Participants were offered a $5 coffee gift card in appreciation of their time. Participants in focus group discussions provided verbal consent and were each provided with a $10 coffee gift card in addition to light refreshments during the discussion. The project was led by OCAP (Ownership, Control, Access, and Possession) Principles and Indigenous partners were involved in the entire research process.
Overall, 1,973 unique participants completed the survey, including 994 individuals from EDGs and 949 controls, sharing a total of 2,114 ED care experiences. Those who identified as PWUS (p < 0.0001), having mental health concerns (p < 0.0001), 2SLGBTQ+ (p = 0.01), or PWEH (p < 0.0001) reported more negative overall experiences, whereas participants who identified as having a disability reported more mixed ED care experiences (p < 0.01). Participants who did not identify as equity-deserving were more likely to report positive experiences (p < 0.0001). Irrespective of EDG status, more negative experiences were reported by participants who identified as women or non-binary (p < 0.001), struggled more frequently to make ends meet (p < 0.0001), had more visits to the ED in the previous 24 months (p < 0.0001), and who experienced judgement/disrespect in the ED (p < 0.0001) (Table 1).
Compared with those who did not identify as equity-deserving, COVID-19 made it harder to access ED care for those who identified as PWUS (p < 0.01), having disabilities (p < 0.001), PWEH (p = 0.02), 2SLGBTQ+ (p = 0.04), or having mental health concerns (p < 0.001). Further, each of the eight EDGs were statistically more likely to report overall negative feelings about their ED visit, that their personal situation/identity/culture negatively affected care, and that they were treated without respect compared with controls (data not shown).
Participants were able to self-identify with up to three EDGs. Table 2 shows the intersectionality among study participants who identified as equity deserving, with more than half of each EDG identifying with two or more EDGs, except for those who identified as a visible minority.
Quantitative findings were triangulated with the thematically analyzed qualitative micronarratives shared by EDGs and are presented in aggregate below to present a fulsome account of the participants' experiences. Four overall themes were identified and related to: stigma/judgement, poor staff communication, lack of compassionate care, and patients feeling unsupported.
Participants across all eight EDGs were statistically more likely to report feelings of judgement during their ED visit compared with controls. As an example, Figure 1 illustrates that participants with mental health concerns were more likely to feel judged in comparison to controls who did not identify as equity-deserving.
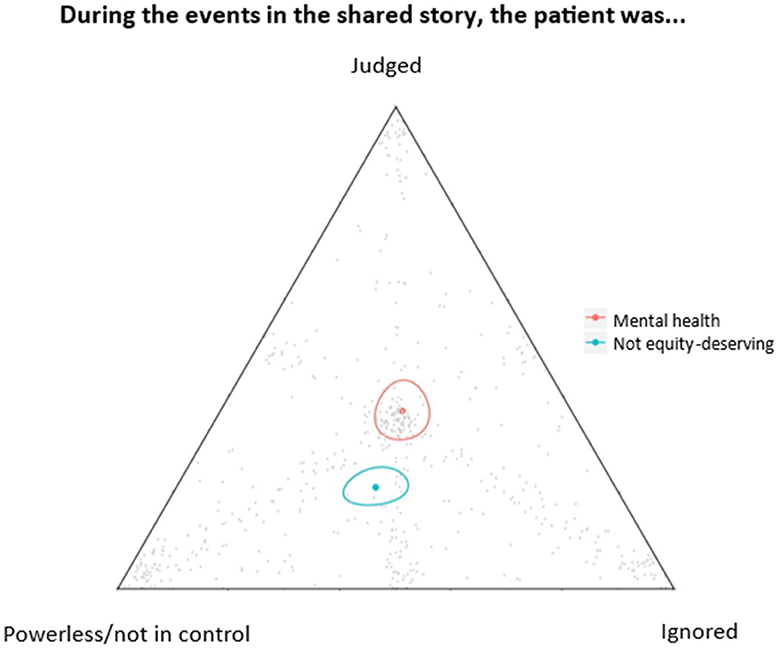
Figure 1. Geometric means with surrounding 95% confidence ellipses are provided. Responses were statistically different between participants with mental health concerns compared to controls, with participants with mental health concerns more likely to feel judged in the ED.
Participants shared ED care experiences about feelings of judgement based on clothing/appearance as well as past or presumed mental health or substance use. Participants also expressed concern over lack of appropriate symptom management, especially pain, due to assumptions about drug use/addiction.
As one man aged 26–45, who identified as having mental health concerns, Indigenous, and as a PWEH, stated,
“The security and nurses at triage judged me by my look assuming I am an addict when I was actually sober for couple months by then. […] Although I was in for an infection on my finger, they automatically assumed I was there for something else asking tons of questions related to my mental concerns and history of substance use.”
Further, as one Indigenous woman aged 46–65, who also identified as having mental health concerns and a PWUS, shared,
“They saw in my chart that I am a cannabis user […] and attributed my vomiting to cannabis use. […] The last time I went, the Dr did not even come in my room all the way, just stuck her head in and said its from using cannabis and we will give you meds. She never once asked me anything, or even made an attempt at an exam. This combined with rough treatment from a nurse when I was in a high anxiety state on the previous visit (her manor made it very clear she doesn't understand mental health issues, she was very dismissive) has made it not a safe spot for me to return to […] I am convinced that this treatment is in large part due to my Indigenous heritage and my use of cannabis, even though I am using with my Drs approval.”
In contrast to these negative ED care experiences, participants also shared positive experiences such as the below:
“… The doctors and nurses went above and beyond to help me and take the time to listen to me. They were patient and non-judgemental. It was one of the better experiences I've had because the doctor allowed my husband to call in and be a part of the conversation.”—woman with a disability, aged 26–45
Feelings of stigma and judgement strongly resonated with FGD participants. Disrespectful interactions with security based on identity was recurrently mentioned as a source of negative ED care experiences. Patients with disabilities and those who identified as visible minorities, on the other hand, shared less stigmatizing and judgemental ED care experiences.
Participants who identified as Indigenous, having mental health concerns, or PWUS were more likely to indicate that the events in their shared micronarratives were about the ED staff (p < 0.001). Figure 2 provides one example comparing Indigenous participants with control participants.
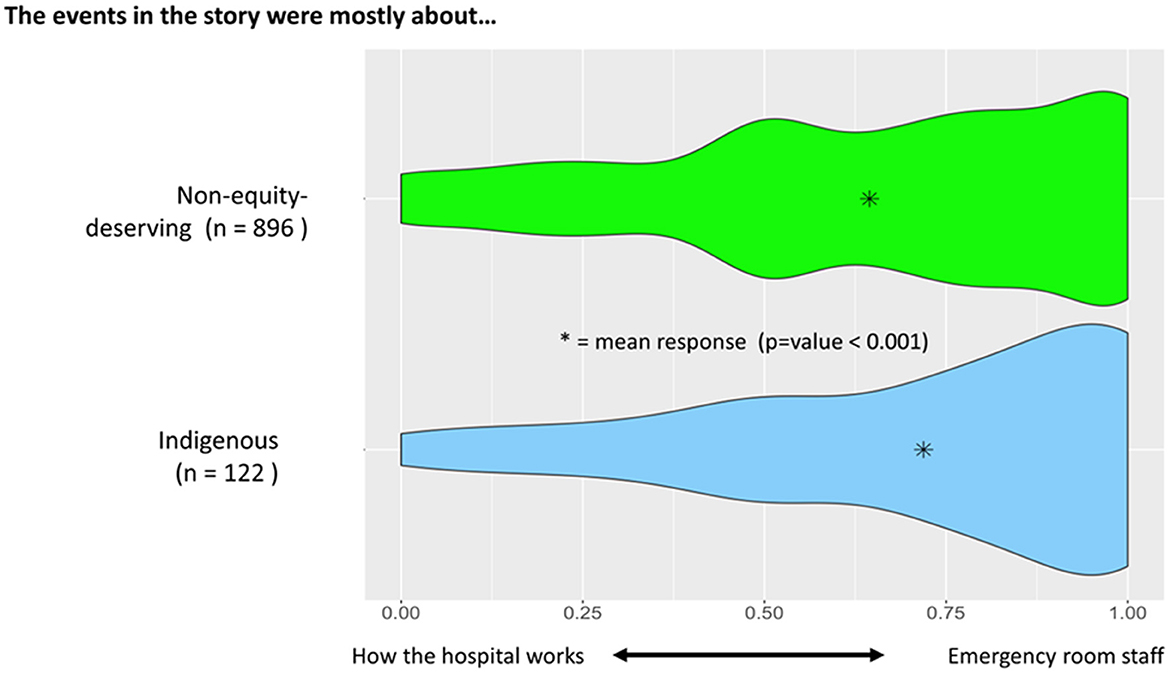
Figure 2. Violin plots with asterisks indicating the overall mean for each group are provided. Results highlight that participants who identified as Indigenous were more likely to indicate that their shared experiences were about the emergency room staff (p < 0.001).
Complementary qualitative data analysis highlighted the ways in which emergency room staff (physicians, nurses, and other allied health care providers) impacted patient care experiences. Identified themes included a lack of understanding by staff, disrespectful communication, poor communication about their diagnosis or treatment, a lack of privacy, and a lack of patient involvement in decision-making.
As one man, aged 46–65, who identified as gender diverse shared,
“I was asked by the triage nurse if I had ever had any surgeries. There were quite a few people in the waiting area, all within ear shot of the triage area. I asked the nurse if I could wait to tell the doctor this information and continued to persist. […] I can't recall how many times she asked me about surgeries, perhaps three […] My eyes welled with tears until I could no longer hold them back. […] there must be other ways to ask this question in a trans sensitive manner or at least in a more private area.”
Another participant, aged 26–45, who accompanied a man with a disability and mental health concerns noted,
“…. Since he can't communicate at all for himself it was a pretty negative experience. He has a trach and they wanted to do suction but he wasn't there for that. There was a miscommunication because he had aspirated blood and didn't need it.”
In contrast to these negative ED care experiences, some participants described positive staff communication. For instance, a woman who identified as a PWEH, aged 26–45, shared the following micronarrative:
“And they were really nice to give me some supplies, you know to take back. And they asked me if everything is all right being homeless. And if there's anything that they can help with. And do you want me to contact any organization or anything to help me out. Do I have a place to stay at night? And they were very, very helpful.”
Community participants also felt poor/inadequate staff communication and a feeling of being “rushed out” was a common experience when they sought ED care. Individuals shared distressing experiences of insufficient privacy when discussing personal information, feeling uninformed/lacking regular updates particularly around wait times, concerns with communication between patients and staff and between staff, a lack of clear instructions, and language barriers impacting care. Others discussed leaving the ED before completing treatment due to a lack of communication. Participants also reported positive experiences when health care providers listened to their concerns, expressed empathy/care about their personal wellbeing, and presented treatment options in a respectful manner. Overall, participants felt staff communication about wait times, their care plan, and clear discharge instructions strongly influenced their ED care experiences.
Participants across all eight EDGs were statistically more likely to indicate that future ED care would be improved by a better understanding of their personal situation/identity/culture compared with controls. This trend is illustrated in Figure 3A with PWEH participants as an example in comparison to control participants.
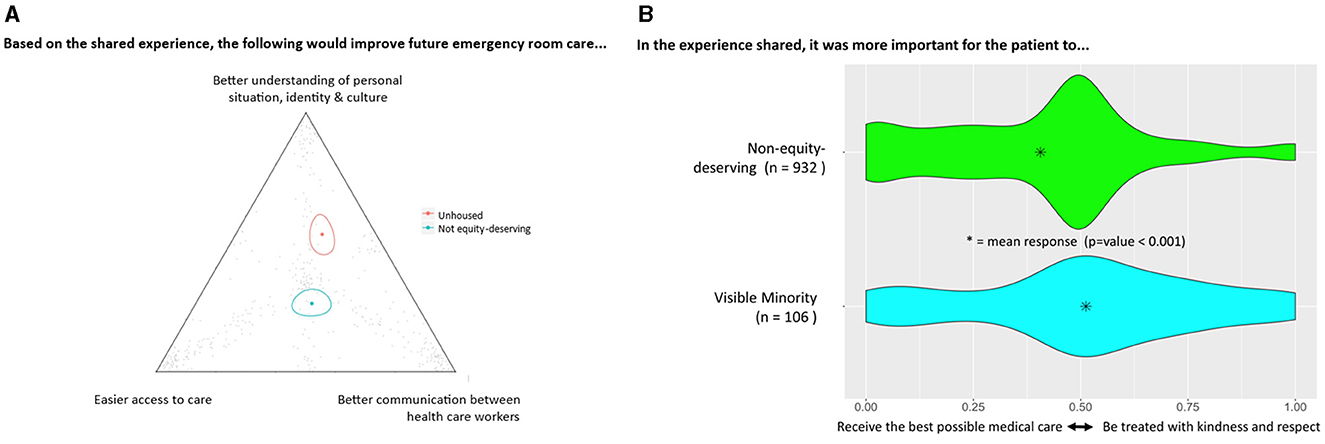
Figure 3. (A) Geometric means with 95% confidence ellipses were statistically different between participants who identified as PWEH compared with controls, with PWEH indicating that future emergency care would be improved with a better understanding of one's personal situation/identity/culture; (B) Violin plots illustrate that participants who identified as visible minorities thought it was more important to be treated with kindness and respect than to receive the best possible care (p < 0.001).
Further, compared with controls, members of each of the eight EDGs indicated it was more important to be treated with kindness and respect than to receive the best possible care (p < 0.001). Figure 3B illustrates one example comparing participants who identified as visible minorities with control participants.
Participants shared ED care experiences about their personal identities being dismissed, assumed, or not being taken into consideration by treating health care providers. Equity-deserving participants also reported concerns about security being called in absence of violent behavior contributing to feeling unsafe.
As one man aged 18–25 who identified as a PWUS, 2SLGBTQ+, and PWEH stated,
“And after I was sick, um, they kind of just kicked me out right away. They didn't really give me a chance to recover. So, then I was homeless at that time. So I was, I was forced to be on the street, and I was sick, and I had nowhere to go. And it was the middle of winter too.”
Another man, aged 18–25, who identified as 2SLGBTQ+ and having mental health concerns, and had recently had gender-affirming surgery shared the following,
“I […] ended up in the hospital due to lots of bruising and swelling no one wanted to call me by my preferred name or pronouns were very short for me […] I felt very uncomfortable and upset that the people working at KGH weren't compassionate or accepting of a transgender person or knew about transition surgeries”.
Compassionate care experiences, including feelings of kindness, understanding, and showing care were also shared by some participants, including the following:
“I arrived at the hospital. I didn't have any ID. They were extremely nice. I was really, really upset. I didn't know where I was going or nothing. They did everything for me. They got me a bus pass. They sent me to where I should go for help. And I just thought it was great. And I appreciate all of the help that they did for me.”—and Indigenous woman aged 46–65 who identified as a PWEH
Community participants emphasized that while the overall medical care received was good, there was a lack of personal care that was respectful and unrushed. Some participants shared that they avoided discussing their mental health history due to a fear of not receiving medical treatment for presenting physical complaints or for gender-affirming care. Participants valued when health care providers introduced themselves, advocated for their needs, recognized their culture/identity, and asked what they could do to make them feel more comfortable. Overall, kind and compassionate care was felt to be important in determining the best care plan and additionally reduced feelings of stigma and discrimination.
Participants who identified as Indigenous, having mental health concerns, PWUS, PWEH, having experienced violence, and/or 2SLGBTQ+ were statistically more likely than controls to report feeling unsupported in coping with their health concern when they left the ED. Figure 4A illustrates that PWUS were more likely to feel unsupported in comparison to controls.
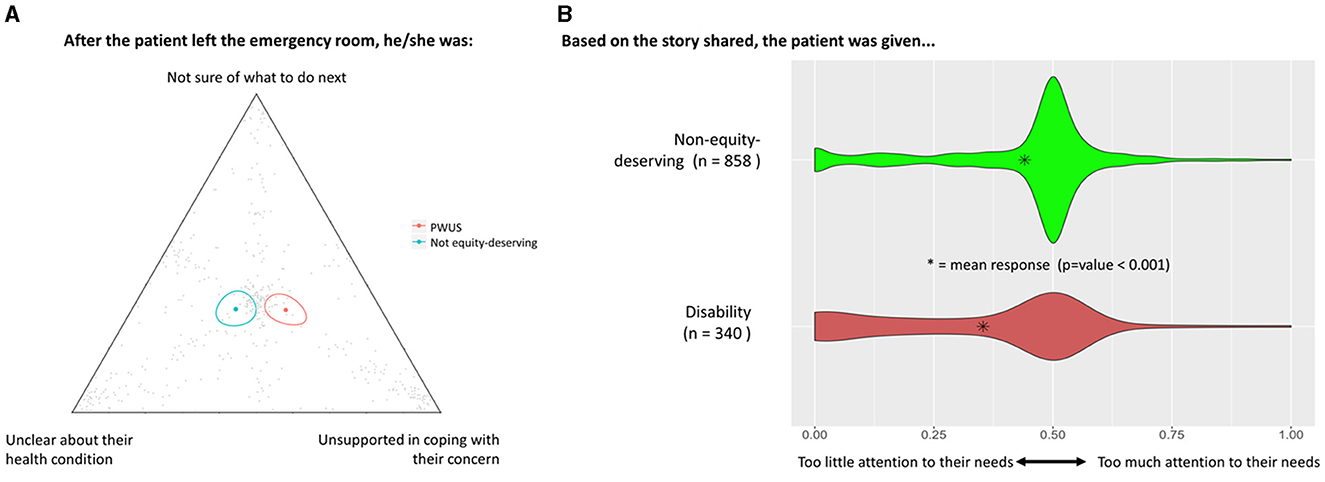
Figure 4. (A) Geometric means with 95% confidence ellipses were statistically different between participants who identified as PWUS compared with controls, with PWUS reporting feeling unsupported in coping with their health concerns when they left the ED; (B) Violin plots illustrate that participants who identified as having a disability felt that they received too little attention to their needs during ED care (p < 0.001).
Members of each of the eight EDGs were more likely than controls to indicate that they received too little attention to their needs during ED care (p < 0.001). Figure 4B provides one example comparing participants who identified as having disabilities with control participants.
Participants shared ED experiences about their health concerns not being taken seriously, that health care providers did not pay attention to their needs, and that they did not receive support in coping with health concerns. Further, EDG participants reported inadequate mental health care and staff knowledge in treating mental health problems in particular.
As one non-binary participant, who identified as 2SLGBTQ+, PWEH, and having mental health concerns, expressed,
“I've recently visited the [Kingston General Hospital], for suicidal ideation and actions. […] At the hospital I spent the majority of the time waiting, being moved around, and feeling my anxiety get worse and worse. I feel stupid and wasted and like I don't matter because of my status as a person, I don't feel important. I don't feel like I was heard in the hospital and I don't know if my own fault or if the hospital didn't understand me well enough.”
Another man, aged 26–45, who identified as having a disability, a PWUS, and having mental health concerns shared,
“But there was supposed to be a follow-up. So, I am quite distressed about the lack of concern for my safety and there, um, they didn't address it at all, the medication thing. And I remember specifically telling them that I want to see a psychiatrist and get that Prozac thing addressed. And they said no that will have to be done at a later date in the community. So, I feel just left. Lost with it.”
Some EDG participants also shared positive ED care experiences including feeling supported with their health concerns and being taken seriously.
As one woman who identified as a visible minority, aged under 18, shared,
“The doctor that was treating me was very calming and assuring, despite it being so late at night. He was very kind and explained everything that was going on and answered all the questions I had.”
Community participants also often felt unsupported in their ED care and discussed experiences of being discharged too fast and before they felt their health concerns were properly addressed. Further, participants recalled experiences of being discharged without referral to inpatient services, such as psychiatry, or community resources for further support. As one participant said, “discharge is the most problematic aspect of the ER…patients are discharged with nowhere to go or are referred to community resources they have little knowledge about.”
Negative ED care experiences were pervasive among the more than 950 surveys shared across the eight primary EDGs in our local setting. These included feelings of judgement/stigma, too little attention to needs, and a need for better understanding of personal situation/identity/culture to improve care. Participants from each EDG reported that it was more important to be treated with kindness and respect than to receive the best possible medical care. Thematic analysis of the qualitative data and FGDs with providers and clients with lived experience supported quantitative findings and identified four overall themes related to stigma/judgement, poor staff communication, lack of compassionate care, and patients feeling unsupported.
That many EDGs report more negative ED care experiences is consistent with the literature, particularly among those who identify as a PWUS (16, 52–54), PWEH (31, 55, 56), experiencing mental health concerns (18, 57–59), having a disability (60, 61), and/or 2SLGBTQ+ (62–65). Smaller scale studies consistently demonstrate that people who face the greatest social and health inequities experience the most negative ED care experiences (15, 16, 31, 60, 63). This, in turn, has been shown to result in EDGs disproportionately leaving the ED before completing care, having no/limited follow-up care, and to overall care avoidance (31, 63, 66, 67).
At the level of patient-provider interactions, three identified themes are consistent with past research and highlight barriers to positive ED care experiences among EDGs including feelings of stigma/judgement (31, 52–56, 58, 62, 68–71), poor staff communication (52, 54, 58, 63, 72–75), and a lack of compassionate care (69, 76–79). Some studies have shown that unconscious bias, the often unrecognized association or attitudes that unknowingly alter one's perceptions of others, has been shown to be related to such patient-provider interactions, as well as treatment decisions, treatment adherence, and patient health outcomes (80).
Contrary to other findings (27, 31, 81, 82), we did not observe quantitative differences between EDG-identifying and non-identifying participants regarding perceived wait times. This may be more reflective of the waiting “culture” with ED services and overall negative patient perceptions regarding a lack of timely and adequate information about expected wait times that is not inherently unique to EDGs (83–86). In addition, and unlike other studies (7, 87–90), participants who identified as Indigenous, a visible minority, and/or having experienced violence did not quantitatively report more overall negative vs. positive ED care experiences in the current study. Shared micronarratives revealed more subtle rather than overt microaggressions, leaving participants feeling uncertain as to whether bias and stigma had played a role in their ED care, and this may have contributed to the discrepant quantitative findings. Participants who identified as Indigenous, a visible minority, and/or having experienced violence also shared more positive experiences about their ED care than other EDGs including kind and empathetic care, compassionate care, having their medical issues taken seriously, and being listened to and respected.
Taken together, results suggest that stigmatizing attitudes and behaviors are more prominently experienced by some EDGs who may be perceived as being responsible or blameworthy for their social circumstances (91, 92). Attribution theory holds that “observers make judgements about the cause and controllability of someone's circumstance/illness and assume how responsible the person is for their condition” (93, 94). Persons with mental health illness, PWEH, and PWUS have been shown to have an increase in “blameworthiness” that often results in discriminatory care and behavior. These differences in assumptions regarding the causes of an individual's problems or social conditions can lead to emotional reactions that can alter one's willingness or motivation to help (93, 94).
The additional theme identified, patients feeling unsupported, which included inadequate mental health care resources, may reflect broader limitations of our current health care system (57, 65, 95–97). For example, health care providers have reported low skill in managing mental health needs (58) as well as limited knowledge of and connections to community service providers, which acts as barriers to providing appropriate referrals (57). Conversely, the availability of mental health services has been associated with more positive care experiences for both patients and providers (58). Furthermore, data collection in the current study occurred during the COVID-19 pandemic which itself exacerbated many pre-existing health care inequities and had an enormous toll on our health care system, with unprecedented rates of burnout among frontline health care providers and systemic issues including staff shortages. Combined, this may result in burnout-associated detachment, depersonalization, and a sense of ineffectiveness among frontline providers which may contribute to negative patient experiences and disproportionately affect those who identify as equity-deserving (98–100).
Our study findings should be interpreted in consideration of several limitations. Selection bias is a potential concern given that only individuals who were visiting the ED/UCC during study hours, had sufficient English proficiency, were medically stable, and had the capacity to consent were approached for participation. This systematically excludes EDGs who are non-English speaking and who are disproportionately racialized people within the Kingston area. Further, participants who may not have been actively seeking ED care due to prior negative experiences were not included, although this was mitigated through recruitment of EDGs at community partner organizations. There is a large amount of data missing at random from early in the data collection due to a failed software update on some of the tablets. However, study findings were presented to both service providers and community members who identified with each of the eight EDGs and no new themes were identified. Recall bias is also a possibility given that ED experiences could be shared from the previous two years, although the triangulation of quantitative with qualitative findings minimizes this concern. Lastly, this is a single study center with a convenience sample and the results consequently may not be widely generalizable.
Our study has several noteworthy strengths. This is the first large, mixed-methods study to include a diverse number of EDGs, analyzed by disaggregated groups, and a comparison group who did not identify as equity-deserving. The sensemaking tool reduces social desirability bias, given that all triads/slider response options are all positive, negative, or neutral. It also reduces interpretation bias, as participants interpret their own shared experiences. Lastly, this community-engaged research design included community partners and clients representing the cross section of EDGs from study conceptualization to survey design to results interpretation, thereby increasing the validity of study findings.
Study findings support the need for interventions at both the level of the health care provider and the health care system. At the level of the provider, education on the delivery of universal trauma-informed care that recognizes and responds to the signs/symptoms/risks of trauma and adversity would be useful to better support the health needs of patients, as would improved care for addiction/substance use. FGDs with EDGs also highlighted a desire for culturally competent care, improved staff communication regarding wait times and updates on care, and better discharge planning including ensuring patients have somewhere safe to go, referral to community organizations, and clear instructions on follow-up. At the level of the health care system, findings strongly supported the need for improved access to mental health care resources in the ED setting, privacy when disclosing personal information, and ED social supports including patient advocates or peer support persons.
This study supports the use of SM-produced quantitative data as specific outcome measures to direct quality improvement programs addressing the bias and stigma ingrained in institutional culture (101). At the patient level, research is needed to look more closely at intersectionality given the high prevalence of EDGs who self-identified as belonging to multiple EDGs, and ED care experiences to better meet patient needs (66, 102). At the provider level, cultural competence training (103) and universal trauma-informed care (104, 105) have been shown to improve knowledge, attitudes, and skills of health care workers and improve patient experiences. Lastly, the development of innovative medical education curricula and training on health advocacy and ways of addressing unconscious bias are needed. For instance, the Equipping Health Care for Equity (EQUIP) model, a multi-component, organizational-level intervention has demonstrated improved staff confidence and comfort in providing equity-oriented health care and improved patient outcomes. EQUIP includes a focus on staff education (i.e., trauma-informed care and harm reduction) and organizational integration/tailoring (i.e., shifts in funding, structures, and practices). Additional studies that include the perspectives of ED staff and implement/evaluate intervention models such as EQUIP are needed (106, 107).
EDGs face intrapersonal, interpersonal, and structural barriers to accessing equitable ED care, and their care experiences are negatively impacted by stigmatizing attitudes and behaviors. Findings suggest that future quality improvement strategies should focus on universal culturally competent and trauma-informed care, improved care for addiction/substance use, and improved education on and access to mental health care resources. Future studies that include the perspectives of ED staff including registration clerks, nurses, physicians, and security would help inform future intervention studies.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
This study was approved by the Queen's University Health Sciences and Affiliated Teaching Hospitals Research Ethics Board (6029400). Informed consent was obtained from all study participants prior to survey completion. No identifying information was collected; data were anonymous from the point of collection. Participants were offered a $5 coffee gift card in appreciation of their time. Participants in focus group discussions provided verbal consent and were each provided with a $10 coffee gift card in addition to light refreshments during the discussion. The project was led by OCAP (Ownership, Control, Access, and Possession) Principles and Indigenous partners were involved in the entire research process.
MW: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Writing – original draft, Writing – review & editing. MM: Conceptualization, Methodology, Writing – review & editing. SD: Conceptualization, Methodology, Writing – review & editing. AC: Conceptualization, Methodology, Writing – review & editing. JP: Conceptualization, Methodology, Writing – review & editing. SH: Conceptualization, Methodology, Writing – review & editing. PN: Formal analysis, Methodology, Writing – review & editing. EP: Conceptualization, Methodology, Writing – review & editing. DM: Conceptualization, Methodology, Writing – review & editing. SB: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Writing – review & editing.
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. We acknowledge the funders who supported this work: Queen's University Catalyst Fund (PI SB), Clinical Teachers' Association of Queen's University (PI SD), and Queen's University Fund for Scholarly Research and Creative Work and Professional Development (PI MW). None of the funders played any role in study design/implementation, data analysis or interpretation of study findings, or in manuscript writing.
Many thanks to all study participants who shared their ED care experiences with us. We are also grateful to the team of research associates for their help in survey development and piloting as well as those involved in participant recruitment in the KHSC ED/UCC and at community partner organizations: Caroline Navas, Cadence Harris, Alex Shammas, Aisha Nathoo, Gillian Forster, Lewis Forward, Kellina Pittman, and Nicole Morris, Eva Lim, Sidonie Chard, Laura Wells, Gillian Forster, Cortney Clark, Jenn Campbell, and Sonal Gupta. We appreciate Laurie Webster's assistance (QED Insight) with the analysis and Reyana Jayawardena and Nicole Morris' assistance in manuscript preparation. A special thanks to Grandmother Kathy Brant at the Kingston Community Health Centre for her review of the manuscript. Queen's University is situated on traditional Haudenosaunee and Anishinaabe territory. We are grateful to be able to live, learn, and play on these lands.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/femer.2024.1397597/full#supplementary-material
1. Malone RE. Whither the almshouse? Overutilization and the role of the emergency department. J Health Polit. (1998) 23:795–832. doi: 10.1215/03616878-23-5-795
2. Richardson LD, Hwang U. Access to care a review of the emergency medicine literature. Acad Emerg Med. (2001) 8:1030–6. doi: 10.1111/j.1553-2712.2001.tb01111.x
3. Ragin DF, Hwang U, Cydulka RK, Holson D, Haley LL Jr., Richards CF, et al Reasons for using the emergency department: results of the EMPATH Study. Acad Emerg Med. (2005) 12:1158–66. doi: 10.1197/j.aem.2005.06.030
4. Canada Council for the Arts. Equity-Seeking Groups. (2021). Available online at: https://canadacouncil.ca/glossary/equity-seeking-groups (accessed December 7, 2021).
5. Ionescu-Ittu R, McCuskter J, Ciampi A, Vadeboncoeur A-M, Roberge D, Larouche D, et al. Continuity of primary care and emergency department utilization among elderly people. CMAJ. (2007) 177:1362–8. doi: 10.1503/cmaj.061615
6. Graham B, Endacott R, Smith JE, Latour JM. ‘They do not care how much you know until they know how much you care': a qualitative meta-synthesis of patient experience in the emergency department. Emerg Med J. (2019) 36:355–63. doi: 10.1136/emermed-2018-208156
7. Browne AJ, Smye VL, Rodney P, Tang SY, Mussell B, O'Neil J. Access to primary care from the perspective of aboriginal patients at an urban emergency department. Qual Health Res. (2011) 21:333–48. doi: 10.1177/1049732310385824
8. Islam MM, Topp L, Day CA, Dawson A, Conigrave KM. The accessibility, acceptability, health impact and cost implications of primary healthcare outlets that target injecting drug users: a narrative synthesis of literature. Int J Drug Policy. (2012) 23:94–102. doi: 10.1016/j.drugpo.2011.08.005
9. Henderson S, Stacey CL, Dohan D. Social stigma and the dilemmas of providing care to substance users in a safety-net emergency department. J Health Care Poor Underserv. (2008) 19:1336–49. doi: 10.1353/hpu.0.0088
10. Ti L, Voon P, Dobrer S, Montaner J, Wood E, Kerr T. Denial of pain medication by health care providers predicts in-hospital illicit drug use among individuals who use illicit drugs. Pain Res Manag. (2015) 20:84–8. doi: 10.1155/2015/868746
11. Ti L, Milloy MJ, Turje RB, Montaner J, Wood E, Kerr T. The impact of an HIV/AIDS adult integrated health program on leaving hospital against medical advice among HIV-positive people who use illicit drugs. J Public Health. (2017) 39:e33–e9. doi: 10.1093/pubmed/fdw057
12. Strike C, Robinson S, Guta A, Tan DH, O'Leary B, Cooper C, et al. Illicit drug use while admitted to hospital: patient and health care provider perspectives. PLoS ONE. (2020) 15:1–16. doi: 10.1371/journal.pone.0229713
13. Paterson B, Hirsch G, Andres K. Structural factors that promote stigmatization of drug users with hepatitis C in hospital emergency departments. Int J Drug Policy. (2013) 24:471–8. doi: 10.1016/j.drugpo.2013.01.008
14. Cox J, Graves L, Marks E, Tremblay C, Stephenson R, Lambert-Lanning A, et al. Knowledge, attitudes and behaviours associated with the provision of hepatitis C care by Canadian family physicians. J Viral Hepat. (2011) 18:332–40. doi: 10.1111/j.1365-2893.2010.01426.x
15. Digel Vandyk A, Young L, MacPhee C, Gillis K. Exploring the experiences of persons who frequently visit the emergency department for mental health-related reasons. Qual Health Res. (2018) 28:587–99. doi: 10.1177/1049732317746382
16. Wise-Harris D, Pauly D, Kahan D, Tan de Bibiana J, Hwang SW, Stergiopoulos V. “Hospital was the Only Option”: experiences of frequent emergency department users in mental health. Adm Policy Ment Health. (2017) 44:405–12. doi: 10.1007/s10488-016-0728-3
17. Cerel J, Currier GW, Conwell Y. Consumer and family experiences in the emergency department following a suicide attempt. J Psychiatr Pract. (2006) 12:341–7. doi: 10.1097/00131746-200611000-00002
18. Carstensen K, Lou S, Groth Jensen L, Konstantin Nissen N, Ortenblad L, Pfau M, et al. Psychiatric service users' experiences of emergency departments: a CERQual review of qualitative studies. Nord J Psychiatry. (2017) 71:315–23. doi: 10.1080/08039488.2017.1288759
19. Harris B, Beurmann R, Fagien S, Shattell MM. Patients' experiences of psychiatric care in emergency departments: a secondary analysis. Int Emerg Nurs. (2016) 26:14–9. doi: 10.1016/j.ienj.2015.09.004
20. Thomas KC, Owino H, Ansari S, Adams L, Cyr JM, Gaynes BN, et al. Patient-centered values and experiences with emergency department and mental health crisis care. Administr Policy Mental Health Mental Health Serv Res. (2018) 45:611–22. doi: 10.1007/s10488-018-0849-y
21. Wong AH, Ray JM, Rosenberg A, Crispino L, Parker J, McVaney C, et al. Experiences of individuals who were physically restrained in the emergency department. JAMA Netw Open. (2020) 3:e1919381. doi: 10.1001/jamanetworkopen.2019.19381
22. Clarke D, Usick R, Sanderson A, Giles-Smith L, Baker J. Emergency department staff attitudes towards mental health consumers: a literature review and thematic content analysis. Int J Ment Health Nurs. (2014) 23:273–84. doi: 10.1111/inm.12040
23. Fleury MJ, Grenier G, Farand L, Ferland F. Reasons for emergency department use among patients with mental disorders. Psychiatr Q. (2019) 90:703–16. doi: 10.1007/s11126-019-09657-w
24. Innes K, Morphet J, O'Brien AP, Munro I. Caring for the mental illness patient in emergency departments - an exploration of the issues from a healthcare provider perspective. J Clin Nurs. (2014) 23:2003–11. doi: 10.1111/jocn.12437
25. Fleury MJ, Grenier G, Farand L, Ferland F. Use of emergency rooms for mental health reasons in Quebec: barriers and facilitators. Administr Policy Mental Health Mental Health Serv Res. (2019) 46:18–33. doi: 10.1007/s10488-018-0889-3
26. Haley RJ, Woodward KR. Perceptions of individuals who are homeless. Adv Emerg Nurs J. (2007) 29:346–55. doi: 10.1097/01.TME.0000300117.17196.f1
27. McCallum R, Medved MI, Hiebert-Murphy D, Distasio J, Sareen J, Chateau D. Fixed nodes of transience: narratives of homelessness and emergency department use. Qual Health Res. (2020) 30:1183–95. doi: 10.1177/1049732319862532
28. Ramsay N, Hossain R, Moore M, Milo M, Brown A. Health care while homeless: barriers, facilitators, and the lived experiences of homeless individuals accessing health care in a Canadian regional municipality. Qual Health Res. (2019) 29:1839–49. doi: 10.1177/1049732319829434
29. Fine AG, Zhang T, Hwang SW. Attitudes towards homeless people among emergency department teachers and learners: a cross-sectional study of medical students and emergency physicians. BMC Med Educ. (2013) 13:112. doi: 10.1186/1472-6920-13-112
30. Gabet M, Grenier G, Cao Z, Fleury MJ. Predictors of emergency department use among individuals with current or previous experience of homelessness. Int J Environ Res Public Health. (2019) 16:4965. doi: 10.3390/ijerph16244965
31. Nicholas DB, Newton AS, Calhoun A, Dong K, Dejong-Berg MA, Hamilton F, et al. The experiences and perceptions of street-involved youth regarding emergency department services. Qual Health Res. (2016) 26:851–62. doi: 10.1177/1049732315577605
32. Chisolm-Straker M, Jardine L, Bennouna C, Morency-Brassard N, Coy L, Egemba MO, et al. Transgender and gender nonconforming in emergency departments: a qualitative report of patient experiences. Transgend Health. (2017) 2:8–16. doi: 10.1089/trgh.2016.0026
33. Lee A, Kanji Z. Queering the health care system: experiences of the lesbian, gay, bisexual, transgender community. Can J Dental Hyg. (2017) 51:80−9.
34. Lerner JE, Robles G. Perceived barriers and facilitators to health care utilization in the United States for transgender people: a review of recent literature. J Health Care Poor Underserv. (2017) 28:127–52. doi: 10.1353/hpu.2017.0014
35. Kano M, Silva-Ban-Uelos AR, Sturm R, Willging CE. Stakeholders' recommendations to improve patient-centered “lGBTQ” primary care in rural and multicultural practices. J Am Board Fam Med. (2016) 29:156–60. doi: 10.3122/jabfm.2016.01.150205
36. Jaffee KD, Shires DA, Stroumsa D. Discrimination and delayed health care among transgender women and men. Med Care. (2016) 54:1010–6. doi: 10.1097/MLR.0000000000000583
37. Puxley C. Woman in ER Where Man Died After Lengthy Wait Says it was Obvious he Needed Help. MacLean's (2013). Available online at: https://www.macleans.ca/general/woman-in-er-where-man-died-after-lengthy-wait-says-it-was-obvious-he-needed-help/ (accessed February 28, 2022).
38. Bartels SA, MacKenzie M, Douglas SL, Collier A, Pritchard J, Purkey E, et al. Emergency department care experiences among members of equity-deserving groups: quantitative results from a cross-sectional mixed methods study. BMC Emerg Med. (2023) 23:21. doi: 10.1186/s12873-023-00792-z
39. Edge C. SenseMaker (2017). Available online at: http://cognitive-edge.com/sensemaker/ (accessed April 8, 2021).
40. Koenig Kellas J, Trees AR. Finding meaning in difficult family experiences: sense-making and interaction processes during joint family storytelling. J Fam Commun. (2006) 6:49–76. doi: 10.1207/s15327698jfc0601_4
41. Brown AD. A narrative approach to collective identities*. J Manag Stud. (2006) 43:731–53. doi: 10.1111/j.1467-6486.2006.00609.x
42. Fivush R, Habermas T, Waters T, Zaman W. The making of autobiographical memory: intersections of culture, narratives and identity. Int J Psychol. (2011) 46:321–45. doi: 10.1080/00207594.2011.596541
43. Wisdom J, Creswell JW. Mixed Methods: Integrating Quantitative and Qualitative Data Collection and Analysis While Studying Patient-Centered Medical Home Models. Rockville, VIC: Agency for Healthcare Research and Quality (2013). p. 1–5.
44. Hub G. Using SenseMaker to Understand Girls' Lives: Lessons Learnt from Girl Hub (2014). Available online at: http://old.cognitive-edge.com/wp-content/uploads/2015/04/GH-SenseMaker-brief.pdf (accessed April 8, 2021).
45. Jay C. Living Wage Kingston Update - October 2016 Report (2016). Available online at: http://www.livingwagecanada.ca/files/4014/7824/8360/LW2016_Report.final1_Kingston.pdf (accessed February 22, 2022).
46. Cognitive Edge. SenseMaker (2017). Available online at: https://sensemaker.cognitive-edge.com (accessed April 8, 2021).
47. DeLong S. Statistics in the Triad, Part I: Geometric Mean (2016). Available online at: http://qedinsight.com/2016/03/28/geometric-mean/ (accessed April 20, 2021).
48. DeLong S. Statistics in the Triad, Part IV: Confidence Regions (2017). Available online at: http://qedinsight.com/2017/07/08/confidence-regions/ (accessed April 8, 2022).
49. Webster L. Using Statistics to Help Interpret Patterns: Are My Eyes Tricking Me? (2015). Available online at: http://qedinsight.com/2015/06/04/are-my-eyes-tricking-me/ (accessed April 20, 2021).
50. Webster L, Carroll M. November 2014 Webinar: The Art and Science of Story Patterns (2014). Available online at: http://qedinsight.com/resources/library/november-2014-webinar/ (accessed April 20, 2021).
51. Creswell JW, Clark VLP. Designing and Conducting Mixed Methods Research: SAGE Publications; 2011.
52. Chan Carusone S, Guta A, Robinson S, Tan DH, Cooper C, O'Leary B., et al. “Maybe if I stop the drugs, then maybe they'd care?”-hospital care experiences of people who use drugs. Harm Reduct J. (2019) 16:16. doi: 10.1186/s12954-019-0285-7
53. Ellis K, Walters S, Friedman SR, Ouellet LJ, Ezell J, Rosentel K, et al. Breaching trust: a qualitative study of healthcare experiences of people who use drugs in a rural setting. Front Sociol. (2020) 5:593925. doi: 10.3389/fsoc.2020.593925
54. Hawk K, McCormack R, Edelman EJ, Coupet E Jr., Toledo N, Gauthier P, et al. Perspectives about emergency department care encounters among adults with opioid use disorder. JAMA Netw Open. (2022) 5:e2144955. doi: 10.1001/jamanetworkopen.2021.44955
55. Weber JJ, Lee RC, Martsolf D. Experiences of care in the emergency department among a sample of homeless male veterans: a qualitative study. J Emerg Nurs. (2020) 46:51–8. doi: 10.1016/j.jen.2019.06.009
56. Liu M, Hwang SW. Health care for homeless people. Nat Rev Dis Prim. (2021) 7:5. doi: 10.1038/s41572-020-00241-2
57. Navas C, Wells L, Bartels SA, Walker M. Patient and provider perspectives on emergency department care experiences among people with mental health concerns. Healthcare. (2022) 10:1297. doi: 10.3390/healthcare10071297
58. Sacre M, Albert R, Hoe J. What are the experiences and the perceptions of service users attending emergency department for a mental health crisis? A systematic review. Int J Ment Health Nurs. (2022) 31:400–23. doi: 10.1111/inm.12968
59. Roennfeldt H, Wyder M, Byrne L, Hill N, Randall R, Hamilton B. Subjective experiences of mental health crisis care in emergency departments: a narrative review of the qualitative literature. Int J Environ Res Public Health. (2021) 18:9650. doi: 10.3390/ijerph18189650
60. Morris MA. Striving toward equity in health care for people with communication disabilities. J Speech Lang Hear Res. (2022) 65:3623–32. doi: 10.1044/2022_JSLHR-22-00057
61. York J, Wechuli Y, Karbach U. Emergency medical care of people with intellectual disabilities: a scoping review. Open Access Emerg Med. (2022) 14:441–56. doi: 10.2147/OAEM.S361676
62. Ayhan CHB, Bilgin H, Uluman OT, Sukut O, Yilmaz S, Buzlu S, et al. Systematic review of the discrimination against sexual and gender minority in health care settings. Int J Health Serv. (2020) 50:44–61. doi: 10.1177/0020731419885093
63. Bauer GR, Ayden, Scheim I, Deutsch MB, Massarella C. Reported emergency department avoidance, use, and experiences of transgender persons in Ontario, Canada: results from a respondent-driven sampling survey. Ann Emerg Med. (2014) 63:713–20. doi: 10.1016/j.annemergmed.2013.09.027
64. Vermeir E, Jackson LA, Marshall EG. Barriers to primary and emergency healthcare for trans adults. Cult Health Sex. (2018) 20:232–46. doi: 10.1080/13691058.2017.1338757
65. Campbell J, Nathoo A, Chard S, Messenger D, Walker M, Bartels SA. Lesbian, gay, bisexual, transgender and or queer patient experiences in Canadian primary care and emergency departments: a literature review. Cult Health Sex. (2023) 25:1707–24. doi: 10.1080/13691058.2023.2176548
66. Varcoe C, Browne AJ, Bungay V, Perrin N, Wilson E, Wathen CN, et al. Through an equity lens: illuminating the relationships among social inequities, stigma and discrimination, and patient experiences of emergency health care. Int J Health Serv. (2022) 52:246–60. doi: 10.1177/00207314221075515
67. Purkey E, MacKenzie M. Experience of healthcare among the homeless and vulnerably housed a qualitative study: opportunities for equity-oriented health care. Int J Equity Health. (2019) 18:101. doi: 10.1186/s12939-019-1004-4
68. Lloyd C. The stigmatization of problem drug users: a narrative literature review. Drugs Educ Prev Policy. (2013) 20:85–95. doi: 10.3109/09687637.2012.743506
69. Muncan B, Walters SM, Ezell J, Ompad DC. “They look at us like junkies”: influences of drug use stigma on the healthcare engagement of people who inject drugs in New York City. Harm Reduct J. (2020) 17:53. doi: 10.1186/s12954-020-00399-8
70. Gilmer C, Buccieri K. Homeless patients associate clinician bias with suboptimal care for mental illness, addictions, and chronic pain. J Prim Care Commun Health. (2020) 11:2150132720910289. doi: 10.1177/2150132720910289
71. Flike K, Hayman LL, Byrne T, Song Q, Aronowitz T. The impact of patient-centred care on the relationship between access to care and subjective health outcomes amongst people experiencing homelessness: a mediation analysis. Health Soc Care Commun. (2022) 30:e5755–64. doi: 10.1111/hsc.14007
72. Drumm RD, McBride DC, Metsch L, Page JB, Dickerson K, Jones B. “The rock always comes first”: drug users' accounts about using formal health care. J Psychoactive Drugs. (2003) 35:461–9. doi: 10.1080/02791072.2003.10400493
73. Bull C, Latimer S, Crilly J, Spain D, Gillespie BM. 'I knew I'd be taken care of': Exploring patient experiences in the Emergency Department. J Adv Nurs. (2022) 78:3330–44. doi: 10.1111/jan.15317
74. Sharby N, Martire K, Iversen MD. Decreasing health disparities for people with disabilities through improved communication strategies and awareness. Int J Environ Res Public Health. (2015) 12:3301–16. doi: 10.3390/ijerph120303301
75. Hemsley B, Balandin S, Worrall L. The “Big 5” and beyond: nurses, paid carers, and adults with developmental disability discuss communication needs in hospital. Appl Nurs Res. (2011) 24:e51–8. doi: 10.1016/j.apnr.2010.09.001
76. Gordon J, Sheppard LA, Anaf S. The patient experience in the emergency department: a systematic synthesis of qualitative research. Int Emerg Nurs. (2010) 18:80–8. doi: 10.1016/j.ienj.2009.05.004
77. Mautner DB, Pang H, Brenner JC, Shea JA, Gross KS, Frasso R, et al. Generating hypotheses about care needs of high utilizers: lessons from patient interviews. Popul Health Manag. (2013) 16 (Suppl. 1):S26–33. doi: 10.1089/pop.2013.0033
78. Welch SJ. Twenty years of patient satisfaction research applied to the emergency department: a qualitative review. Am J Med Qual. (2010) 25:64–72. doi: 10.1177/1062860609352536
79. Martins DC. Experiences of homeless people in the health care delivery system: a descriptive phenomenological study. Public Health Nurs. (2008) 25:420–30. doi: 10.1111/j.1525-1446.2008.00726.x
80. Hall WJ, Chapman MV, Lee KM, Merino YM, Thomas TW, Payne BK, et al. Implicit racial/ethnic bias among health care professionals and its influence on health care outcomes: a systematic review. Am J Public Health. (2015) 105:e60–76. doi: 10.2105/AJPH.2015.302903a
81. Nelson SE. “They Seem to Want to Help Me”: Health, Rights, and Indigenous Community Resurgence in Urban Indigenous Health Organizations. University of Toronto (2019).
82. Ignored to Death - Brian Sinclair Working Group. Brian Sinclair: Killed by Racism (2017). Available online at: http://ignoredtodeathmanitoba.ca (accessed February 22, 2022).
83. Hassankhani H, Soheili A, Vahdati SS, Amin Mozaffari F, Wolf LA, Wiseman T. “Me First, Others Later” A focused ethnography of ongoing cultural features of waiting in an Iranian emergency department. Int Emerg Nurs. (2019) 47:100804. doi: 10.1016/j.ienj.2019.100804
84. Nyce A, Gandhi S, Freeze B, Bosire J, Ricca T, Kupersmith E, et al. Association of emergency department waiting times with patient experience in admitted and discharged patients. J Patient Exp. (2021) 8:23743735211011404. doi: 10.1177/23743735211011404
85. de Steenwinkel M, Haagsma JA, van Berkel ECM, Rozema L, Rood PPM, Bouwhuis MG. Patient satisfaction, needs, and preferences concerning information dispensation at the emergency department: a cross-sectional observational study. Int J Emerg Med. (2022) 15:5. doi: 10.1186/s12245-022-00407-7
86. Göransson KE, von Rosen A. Patient experience of the triage encounter in a Swedish emergency department. Int Emerg Nurs. (2010) 18:36–40. doi: 10.1016/j.ienj.2009.10.001
87. Browne AJ, Fiske J-A, Thomas G. First Nations Women's Encounters With Mainstream Health Care Services & Systems. Vancouver, BC: British Columbia Centre of Excellence for Women's Health (2000).
88. Larsen MM, Krohn J, Püschel K, Seifert D. Experiences of health and health care among women exposed to intimate partner violence: qualitative findings from Germany. Health Care Women Int. (2014) 35:359–79. doi: 10.1080/07399332.2012.738264
89. Reisenhofer S, Seibold C. Emergency healthcare experiences of women living with intimate partner violence. J Clin Nurs. (2013) 22:2253–63. doi: 10.1111/j.1365-2702.2012.04311.x
90. Wallin Lundell I, Eulau L, Bjarneby F, Westerbotn M. Women's experiences with healthcare professionals after suffering from gender-based violence: an interview study. J Clin Nurs. (2018) 27:949–57. doi: 10.1111/jocn.14046
91. Pilla D. Stereotypes and Public Stigma Against People Experiencing Homelessness (Ph.D. thesis). New York, NY: Fordham University (2023).
92. Yang LH, Wong LY, Grivel MM, Hasin DS. Stigma and substance use disorders: an international phenomenon. Curr Opin Psychiatry. (2017) 30:378–88. doi: 10.1097/YCO.0000000000000351
93. Markowitz FE, Syverson J. Race, Gender, and homelessness stigma: effects of perceived blameworthiness and dangerousness. Deviant Behav. (2021) 42:919–31. doi: 10.1080/01639625.2019.1706140
94. Witte TH, Wright A, Stinson EA. Factors influencing stigma toward individuals who have substance use disorders. Subst Use Misuse. (2019) 54:1115–24. doi: 10.1080/10826084.2018.1560469
95. Mayer S, Langheimer V, Nolan S, Boyd J, Small W, McNeil R. Emergency department experiences of people who use drugs who left or were discharged from hospital against medical advice. PLoS ONE. (2023) 18:e0282215. doi: 10.1371/journal.pone.0282215
96. De Hert M, Cohen D, Bobes J, Cetkovich-Bakmas M, Leucht S, Ndetei DM, et al. Physical illness in patients with severe mental disorders. II Barriers to care, monitoring and treatment guidelines, plus recommendations at the system and individual level. World Psychiatry. (2011) 10:138–51. doi: 10.1002/j.2051-5545.2011.tb00036.x
97. Semlyen J, King M, Varney J, Hagger-Johnson G. Sexual orientation and symptoms of common mental disorder or low wellbeing: combined meta-analysis of 12 UK population health surveys. BMC Psychiatry. (2016) 16:67. doi: 10.1186/s12888-016-0767-z
98. Mercuri M, Clayton N, Archambault P, Wallner C, Boulos ME, Chan TM, et al. Canadian emergency medicine physician burnout: a survey of Canadian emergency physicians during the second wave of the COVID-19 pandemic. CJEM. (2022) 24:288–92. doi: 10.1007/s43678-021-00259-9
99. Tran A, Wallner C, de Wit K, Gérin-Lajoie C, Ritchie K, Mercuri M, et al. Humans not heroes: Canadian emergency physician experiences during the early COVID-19 pandemic. Emerg Med J. (2023) 40:86–91. doi: 10.1136/emermed-2022-212466
100. Patel RS, Bachu R, Adikey A, Malik M, Shah M. Factors related to physician burnout and its consequences: a review. Behav Sci. (2018) 8:98. doi: 10.3390/bs8110098
101. Rao D, Elshafei A, Nguyen M, Hatzenbuehler ML, Frey S, Go VF, et al. systematic review of multi-level stigma interventions: state of the science and future directions. BMC Med. (2019) 17:41. doi: 10.1186/s12916-018-1244-y
102. Bauer GR. Incorporating intersectionality theory into population health research methodology: challenges and the potential to advance health equity. Soc Sci Med. (2014) 110:10–7. doi: 10.1016/j.socscimed.2014.03.022
103. Beach MC, Price EG, Gary TL, Robinson KA, Gozu A, Palacio A, et al. Cultural competence: a systematic review of health care provider educational interventions. Med Care. (2005) 43:356–73. doi: 10.1097/01.mlr.0000156861.58905.96
104. Brown T, Ashworth H, Bass M, Rittenberg E, Levy-Carrick N, Grossman S, et al. Trauma-informed care interventions in emergency medicine: a systematic review. West J Emerg Med. (2022) 23:334–44. doi: 10.5811/westjem.2022.1.53674
105. Li Y, Cannon LM, Coolidge EM, Darling-Fisher CS, Pardee M, Kuzma EK. Current state of trauma-informed education in the health sciences: lessons for nursing. J Nurs Educ. (2019) 58:93–101. doi: 10.3928/01484834-20190122-06
106. Varcoe C, Browne AJ, Perrin N, Wilson E, Bungay V, Byres D, et al. EQUIP emergency: can interventions to reduce racism, discrimination and stigma in EDs improve outcomes? BMC Health Serv Res. (2022) 22:1113. doi: 10.1186/s12913-022-08475-4
Keywords: Emergency Medicine, equity-deserving groups, health equity, care experiences, substance use disorder, Indigenous health, mental health, people who experience homelessness
Citation: Walker M, MacKenzie M, Douglas SL, Collier A, Pritchard J, Hoffe S, Norman PA, Purkey E, Messenger D and Bartels SA (2024) “I feel like I don't matter because of my status as a person”— A mixed-methods, cross-sectional study of emergency department care experiences among equity-deserving groups in Ontario, Canada. Front. Disaster Emerg. Med. 2:1397597. doi: 10.3389/femer.2024.1397597
Received: 07 March 2024; Accepted: 26 June 2024;
Published: 25 July 2024.
Edited by:
Muhammad Waseem, Lincoln Medical Center, United StatesReviewed by:
Samad Shams Vahdati, Tabriz University of Medical Sciences, IranCopyright © 2024 Walker, MacKenzie, Douglas, Collier, Pritchard, Hoffe, Norman, Purkey, Messenger and Bartels. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Melanie Walker, bWVsYW5pZS53YWxrZXJAa2luZ3N0b25oc2MuY2E=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.