- Department of Emergency Medicine, Emergency Health Services, University of California, San Diego, La Jolla, CA, United States
Introduction
Emergency health services encompass a wide-ranging, diverse, and overarching impact on the health and well-being of individuals, communities, and large populations everywhere. The recent COVID-19 pandemic, during which emergency care providers played a leading and often heroic role in the response, highlights the critical importance of emergency healthcare staff and infrastructure (1, 2).
Emergency medicine is at the intersection of acute medical care at the individual level and public health at the population level. Moreover, the specialty is relatively new within the field of medicine, developing its specific training and areas of expertise only in the mid-to-late 20th century (3, 4). As such, the field of emergency health services faces both great challenges and unique opportunities as the specialty continues to grow and expand its impact.
Demographic challenges—aging populations
Improvements in living conditions and public health, as well as advances in medicine, have led to a remarkable increase in life expectancy over the past century. As a result, the world's population over the age of 60 will nearly double by 2050 (5). This remarkable demographic shift will present significant challenges throughout society and in particular for healthcare delivery systems, with the UN World Health Organization declaring a “Decade of Healthy Ageing” (6, 7).
Increasing physical frailty, multiple chronic comorbidities, and cognitive and social challenges mean that older adults will need increasing levels of acute unscheduled care through emergency health services (8, 9). A number of initiatives are underway to address this coming so-called “silver tsunami” (10). In the United States, the American College of Emergency Physicians launched the Geriatric ED Accreditation program in 2018 to recognize and certify emergency departments (EDs) committed to delivering appropriate, quality emergency care to the senior population, with over 400 such EDs now accredited at three levels (11–13). Assessment of the impact of these efforts in emergency health services is needed to guide and develop future initiatives and efforts to improve the care and well-being of older adults.
Resource challenges—capacity limitations
Emergency health services are resource-intense—where unscheduled care is available at all times for undifferentiated acute illness and injury, with the apt motto “Anyone, Anything, Anytime” (14, 15). Increasing reliance on EDs and emergency medical services (EMS) for essentially on-demand care now often exceeds the limited resources and capacity in many parts of the world, including developed countries with robust healthcare systems (16, 17).
Factors impacting this imbalance include the demographic changes and aging noted earlier; misaligned payment incentive systems, resulting in inefficient or inappropriate care; and overall insufficient capacity, particularly for inpatient care as demand grows (18, 19).
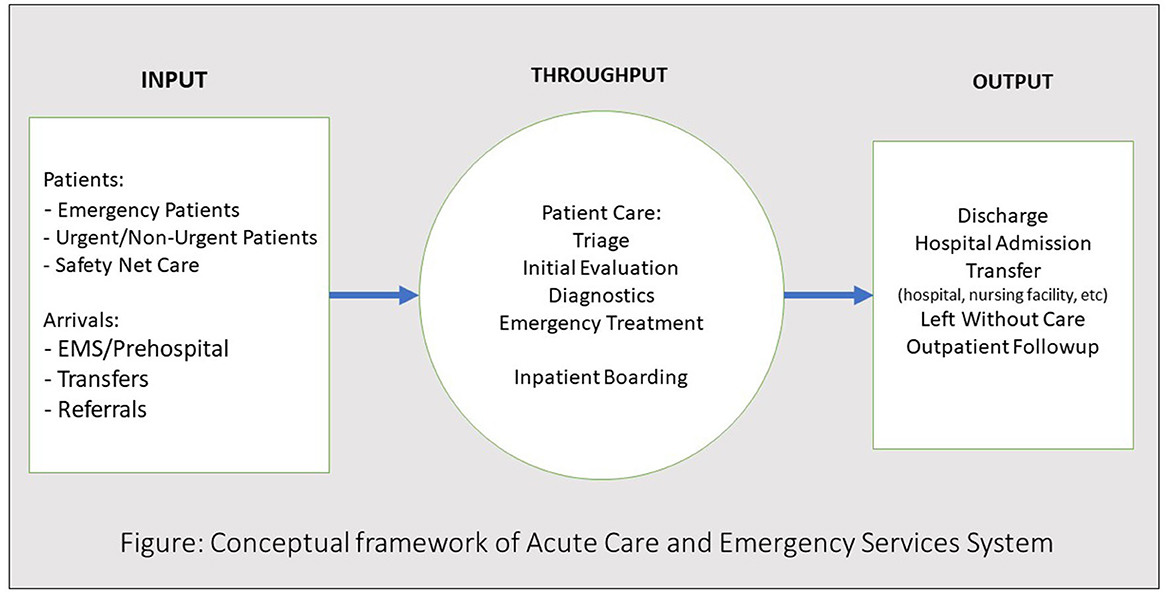
A conceptual model of emergency care patient flow and crowding developed by Asplin et al. (20) focuses on three key processes: input (or patient/care demand), throughput (care delivery, particularly in hospital EDs), and output (patient disposition—discharge, admission, or other; Figure 1) (21).
Despite efforts to address these processes in emergency health services, the problem has only worsened over the intervening decades (22). The result is long waits for care in overwhelmed hospitals and EDs, particularly for ED boarders—admitted inpatients waiting for patient beds—creating access issue challenges, and grave concerns regarding care quality when demand so greatly outpaces resources and capacity (23–25).
Another resource challenge is the shortage of healthcare workers and providers. Trends have accelerated following the COVID-19 pandemic, with significant impacts on staff wellness and burnout, as well as recruitment and attrition of critical personnel, particularly in emergency health services (26–29).
Technology challenges—advances in medicine
Like all fields, new technologies are rapidly advancing in medicine with both tremendous promise and risks. Rapid diagnostics that are both accurate and cost-effective have the potential to markedly improve the efficiency and quality of care in both high- and low-resourced communities. The widespread use of rapid diagnostic panels for gastrointestinal and respiratory pathogens is revolutionizing the evaluation and management of these conditions (30).
In addition, the advancement of new treatments for acute and chronic conditions, such as cancer, vascular diseases, and metabolic syndromes, is having an impact on emergency care in terms of both specific disease management and treatment complications (31). These medical advances will continue to provide great opportunities as well as challenges for emergency health service providers.
Similarly, the information technology revolution is having a profound impact on healthcare and emergency health services (32). The transition to electronic health records and the vast accumulation of personal health data will only accelerate this impact (33). Artificial intelligence, machine learning algorithms, and natural language processing are now readily being tested and adopted in healthcare. These advances have the potential to not only increase efficiency and reduce staff burden (like documentation) but also increase the risk of errors, bias, and overreliance on technology to deliver care (34). These risks are all the greater in the time-intensive emergency health services setting (35–37).
Challenges in disaster response and resilience—climate change
Over the last century, large-scale disasters have increased markedly in terms of both frequency and magnitude (38). Emergency health services are critical to the immediate response and resilience infrastructure and to mitigate the impact of these events on the health of humankind.
Climate change is accelerating disaster events, creating challenges for existing emergency care infrastructure and resources (39, 40). Extreme heat events, wildfires and smoke/particulate air pollution, and severe flooding are just a few climate-related impacts that result in mass injury and illnesses (41, 42). Current emergency health services are ill-prepared to handle this impact and must begin to prepare for a world in which these events are commonplace and frequent (43).
Expanding human development is also leading to new challenges, such as outbreaks of novel zoonotic infectious diseases in the human population. The worldwide COVID-19 pandemic is a reflection of the potential scale and devastating impact on an individual, community, and worldwide level, placing tremendous strain on our acute care infrastructure and emergency health services systems (44, 45).
Public and population health challenges
Emergency health services are at the nexus and intersection of individual patient care and community public health (46, 47). The remarkable reduction in trauma-related morbidity and mortality over the past several decades is the result of both improvements in acute trauma care and public health measures to prevent and reduce injury on a population level (48). Similar challenges and opportunities exist in other arenas including the immediate care of acute vascular diseases, metabolic syndromes, and cancer.
With its unique role within a community, emergency health services are vulnerable to the various social factors impacting health in a given region, the so-called social determinants of health. These include economic factors, access to shelter and nutrition, and critical equity issues that create underlying risks to certain individuals and specific communities (49).
These challenges represent a tremendous opportunity for emergency providers to play critical roles in not only providing acute care for communities but also addressing underlying issues and complexities on a public health and population health basis.
Emergency health services—the “availablists”
Emergency health services, focused on the core competency of acute care at any hour for those in need with critical illness or injury, are relatively new in the field of medicine. While traditionally based in hospital EDs and EMS prehospital systems, new opportunities and challenges are rising in the areas of on-demand medical care for a wide variety of healthcare needs in diverse settings. These include the rapid adoption of telemedicine and virtual care; express, urgent, and freestanding ED units outside of hospitals; progressive hospital at-home programs for post-acute care; and other remote virtual care settings (50–53).
Other innovations include social and psychiatric field teams for the prehospital setting, as well as community paramedicine programs now being adopted in many communities (54). All these opportunities leverage the so-called core competency of emergency providers—providing care across a wide range of specialties at any time in any setting—as Hollander and Sharma call it, being available, or “Availabilists” (55).
A significant challenge for emergency health services will be to demonstrate both the quality and value of these innovations. Emergency health services research efforts should focus on how these innovations improve emergency care for individuals in acute medical need and provide cost-effective, equitable care and access within communities and for public health.
Author contributions
TC: Conceptualization, Data curation, Formal analysis, Project administration, Supervision, Validation, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, et al. A novel coronavirus from patients with pneumonia in China, (2019). N Engl J Med. (2020) 382:727–33. doi: 10.1056/NEJMoa2001017
2. Yau SY, Lee CY, Lai HY, Lee CH. COVID-19-related stress among emergency physicians: a scoping review protocol on the stressors and coping strategies. BMJ Open. (2023) 13:e068085. doi: 10.1136/bmjopen-2022-068085
3. Huecker MR, Shreffler J, Platt M, O'Brien D, Stanton R, Mulligan T, et al. Emergency medicine history and expansion into the future: a narrative review. West J Emerg Med. (2022) 23:418–23. doi: 10.5811/westjem.2022.2.55108
4. Mackenzie R. Brief history of pre-hospital emergency medicine. Emerg Med J. (2018) 35:146–8. doi: 10.1136/emermed-2017-207310
5. World Health Organization. (2013). Available online at: https://www.who.int/data/maternal-newborn-child-adolescent-ageing/ageing-data/ageing—demographics (accessed October 6, 2023).
6. Christensen K, Doblhammer G, Rau R, Vaupel JW. Ageing populations: the challenges ahead. Lancet. (2009) 374:1196–208. doi: 10.1016/S0140-6736(09)61460-4
7. World Health Organization. (2023). Available online at: https://www.who.int/initiatives/decade-of-healthy-ageing (accessed October 6, 2023).
9. Clegg A, Young J, Iliffe S, Rikkert MO, Rockwood K. Frailty in elderly people. Lancet. (2013) 381:752–62. doi: 10.1016/S0140-6736(12)62167-9
10. Shadyab AH, Castillo EM, Chan TC, Tolia VM. Developing and implementing a geriatric emergency department (GED): overview and characteristics of GED visits. J Emerg Med. (2021) 61:131–9. doi: 10.1016/j.jemermed.2021.02.036
11. Gettel CJ, Hwang U, Janke AT, Rothenberg C, Tomasino DF, Schneider SM, et al. An outcome comparison between geriatric and nongeriatric emergency departments. Ann Emerg Med. (2023) 82:681–9. doi: 10.1016/j.annemergmed.2023.05.01
12. Kennedy M, Lesser A, Israni J, Liu SW, Santangelo I, Tidwell N, et al. Reach and adoption of a geriatric emergency department accreditation program in the United States. Ann Emerg Med. (2022) 79:367–73. doi: 10.1016/j.annemergmed.2021.06.013
13. A Practical Guide to Implementing a Geriatric Emergency Department by West Health UC San Diego Health - westhealth.org. Available online at: https://www.westhealth.org/resource/ged-implementation-guide/ (accessed October 6, 2023).
14. Zink B. Anyone, Anything, Anytime: A History of Emergency Medicine. Philadelphia, PA: Mosby, Inc. (2006).
15. Stadler DE, Donihoo RS, Brady MF. Bring ‘Em All. Chaos. Care. Stories from Medicine's Front Line. Dallas, TX: American College of Emergency Physicians. (2018).
16. Institute of Medicine. Hospital-Based Emergency Care: At the Breaking Point. Washington, DC: The National Academies Press. (2007).
17. Hsia RY, Zagorov S, Sarkar N, Savides MT, Feldmeier M, Addo N. Patterns in patient encounters and emergency department capacity in California, 2011-2021. JAMA Netw Open. (2023) 6:e2319438. doi: 10.1001/jamanetworkopen.2023.19438
18. Kellermann AL. Crisis in the emergency department. N Engl J Med. (2006) 355:1300–3. doi: 10.1056/NEJMp068194
19. Moskop JC, Sklar DP, Geiderman JM, Schears RM, Bookman KJ. Emergency department crowding, part 1–concept, causes, and moral consequences. Ann Emerg Med. (2009) 53:605–11. doi: 10.1016/j.annemergmed.2008.09.019
20. Asplin BR, Magid DJ, Rhodes KV, Solberg LI, Lurie N, Camargo CA Jr. A conceptual model of emergency department crowding. Ann Emerg Med. (2003) 42:173–80. doi: 10.1067/mem.2003.302
21. Moskop JC, Sklar DP, Geiderman JM, Schears RM, Bookman KJ. Emergency department crowding, part 2–barriers to reform and strategies to overcome them. Ann Emerg Med. (2009) 53:612–7. doi: 10.1016/j.annemergmed.2008.09.024
22. Kelen GD, Wolfe R, D'Onofrio G, et al. Emergency department crowding: the canary in the health care system. In: NEJM Catalyst. (2021). Available online at: https://catalyst.nejm.org/doi/full/10.1056/CAT.21.0217 (accessed October 6, 2023).
23. Berg LM, Ehrenberg A, Florin J, Östergren J, Discacciati A, Göransson KE. Associations between crowding and ten-day mortality among patients allocated lower triage acuity levels without need of acute hospital care on departure from the emergency department. Ann Emerg Med. (2019) 74:345–56. doi: 10.1016/j.annemergmed.2019.04.012
24. Verelst S, Wouters P, Gillet JB, Van den Berghe G. Emergency department crowding in relation to in-hospital adverse medical events: a large prospective observational cohort study. J Emerg Med. (2015) 49:949–61. doi: 10.1016/j.jemermed.2015.05.034
25. Bernstein SL, Aronsky D, Duseja R, Epstein S, Handel D, Hwang U, et al. Society for academic emergency medicine, emergency department crowding task force. The effect of emergency department crowding on clinically oriented outcomes. Acad Emerg Med. (2009) 16:1–10. doi: 10.1111/j.1553-2712.2008.00295.x
26. Poon YR, Lin YP, Griffiths P, Yong KK, Seah B, Liaw SY, et al. Global overview of healthcare workers' turnover intention amid COVID-19 pandemic: a systematic review with future directions. Hum Resour Health. (2022) 20:70. doi: 10.1186/s12960-022-00764-7
27. Gualano MR, Sinigaglia T, Lo Moro G, Rousset S, Cremona A, Bert F, et al. The burden of burnout among Healthcare Professionals of Intensive Care Units and emergency departments during the COVID-19 pandemic: a systematic review. Int J Environ Res Public Health. (2021) 18:8172. doi: 10.3390/ijerph18158172
28. Wahlster S, Sharma M, Lewis AK, Patel PV, Hartog CS, Jannotta G, et al. The Coronavirus Disease (2019). Pandemic's effect on critical care resources and health-care providers: a global survey. Chest. (2021) 159:619–33. doi: 10.1016/j.chest.2020.09.070
29. Zhang Q, Mu MC, He Y, Cai ZL, Li ZC. Burnout in emergency medicine physicians: a meta-analysis and systematic review. Medicine. (2020) 99:e21462. doi: 10.1097/MD.0000000000021462
30. Timbrook TT, Morton JB, McConeghy KW, Caffrey AR, Mylonakis E, LaPlante KL. The effect of molecular rapid diagnostic testing on clinical outcomes in bloodstream infections: a systematic review and meta-analysis. Clin Infect Dis. (2017) 64:15–23. doi: 10.1093/cid/ciw649
31. Hryniewicki AT, Wang C, Shatsky RA, Coyne CJ. Management of immune checkpoint inhibitor toxicities: a review and clinical guideline for emergency physicians. J Emerg Med. (2018) 55:489–502. doi: 10.1016/j.jemermed.2018.07.005
32. Naik N, Hameed BMZ, Sooriyaperakasam N, Vinayahalingam S, Patil V, Smriti K, et al. Transforming healthcare through a digital revolution: A review of digital healthcare technologies and solutions. Front Digit Health. (2022) 4:919985. doi: 10.3389/fdgth.2022.919985
33. Mullins A, O'Donnell R, Mousa M, Rankin D, Ben-Meir M, Boyd-Skinner C, et al. Health outcomes and healthcare efficiencies associated with the use of electronic health records in hospital emergency departments: a systematic review. J Med Syst. (2020) 44:200. doi: 10.1007/s10916-020-01660-0
34. Lee P, Bubeck S, Petro J. Benefits, limits, and risks of GPT-4 as an AI Chatbot for medicine. N Engl J Med. (2023) 388:1233–9. doi: 10.1056/NEJMsr2214184
35. Vearrier L, Derse AR, Basford JB, Larkin GL, Moskop JC. Artificial intelligence in emergency medicine: benefits, risks, and recommendations. J Emerg Med. (2022) 62:492–9. doi: 10.1016/j.jemermed.2022.01.001
36. Chenais G, Lagarde E, Gil-Jardiné C. Artificial intelligence in emergency medicine: viewpoint of current applications and foreseeable opportunities and challenges. J Med Internet Res. (2023) 25:e40031. doi: 10.2196/40031
37. Kirubarajan A, Taher A, Khan S, Masood S. Artificial intelligence in emergency medicine: a scoping review. J Am Coll Emerg Physicians Open. (2020) 1:1691–702. doi: 10.1002/emp2.12277
38. Institute for Economics & Peace. Ecological Threat Register 2020: Understanding Ecological Threats, Resilience Peace. Sydney, NSW (2020). Available online at: http://visionofhumanity.org/reports (accessed November 30, 2023).
39. The Economist: Weather-Related Diasters are Increasing. Available online at: https://www.economist.com/graphic-detail/2017/08/29/weather-related-disasters-are-increasing (accessed August 29, 2017).
40. Romanello M, Di Napoli C, Drummond P, Green C, Kennard H, Lampard P, et al. The 2022 report of the Lancet Countdown on health and climate change: health at the mercy of fossil fuels. Lancet. (2022) 400:1619–54. doi: 10.1016/S0140-6736(22)01540-9
41. Parks RM, Bennett JE, Tamura-Wicks H, Kontis V, Toumi R, Danaei G, et al. Anomalously warm temperatures are associated with increased injury deaths. Nat Med. (2020) 26:65–70. doi: 10.1038/s41591-019-0721-y
42. Aguilera R, Hansen K, Gershunov A, Ilango SD, Sheridan P, Benmarhnia T. Respiratory hospitalizations and wildfire smoke: a spatiotemporal analysis of an extreme firestorm in San Diego County, California. Environ Epidemiol. (2020) 4:e114. doi: 10.1097/EE9.0000000000000114
43. Sorensen CJ, Salas RN, Rublee C, Hill K, Bartlett ES, Charlton P, et al. Clinical implications of climate change on US emergency medicine: challenges and opportunities. Ann Emerg Med. (2020) 76:168–78. doi: 10.1016/j.annemergmed.2020.03.010
44. Morse SS, Mazet JA, Woolhouse M, Parrish CR, Carroll D, Karesh WB, et al. Prediction and prevention of the next pandemic zoonosis. Lancet. (2012) 380:1956–65. doi: 10.1016/S0140-6736(12)61684-5
45. Savitt A, Gerber-Chavez L, Montano S, Corbin T. Emergency management pandemic planning: an analysis of state emergency plans. J Emerg Manag. (2023) 21:97–109. doi: 10.5055/jem.0667
46. Bernstein E, Goldfrank LR, Kellerman AL, Hargarten SW, Jui J, Fish SS, et al. A public health approach to emergency medicine: preparing for the twenty-first century. Acad Emerg Med. (1994) 1:277–86 doi: 10.1111/j.1553-2712.1994.tb02446.x
47. Hauswald M, Gerson LW, Kerr NL. Public health and emergency medicine. Acad Emerg Med. (2009) 16:1040–3. doi: 10.1111/j.1553-2712.2009.00541.x
49. Anderson ES, Lippert S, Newberry J, Bernstein E, Alter HJ, Wang NE. Addressing social determinants of health from the emergency department through social emergency medicine. West J Emerg Med. (2016) 17:487–9. doi: 10.5811/westjem.2016.5.30240
50. Hollander JE, Davis TM, Doarn C, Goldwater JC, Klasko S, Lowery C, et al. Recommendations from the first national academic consortium of telehealth. Popul. Health Manag. 21:271–7. doi: 10.1089/pop.2017.0080
51. American College of Emergency Physicians: Freestanding Emergency Departments. Freestanding Emergency Departments | ACEP. (2014). Available online at: https://www.acep.org/patient-care/policy-statements/freestanding-emergency-departments/ (accessed October 6, 2023).
52. Leong MQ, Lim CW, Lai YF. Comparison of hospital-at-home models: a systematic review of reviews. BMJ Open. (2021) 11:e043285. doi: 10.1136/bmjopen-2020-043285
53. Hollander JE, Ranney ML, Carr BG. No patient left behind: patient-centered healthcare reform. Healthc. Transfor. (2016) 2016:115–119. doi: 10.1089/heat.2016.29016.hrc
55. Hollander JE, Sharma R. The availablists: emergency care without the emergency department. NEJM Catalyst. (2014). Available online at: https://catalyst.nejm.org/doi/full/10.1056/CAT.21.0310 (accessed October 6, 2023).
Keywords: emergency, disaster, challenge, healthcare services, acute care
Citation: Chan TC (2023) Specialty grand challenge: emergency health services. Front. Disaster Emerg. Med. 1:1310474. doi: 10.3389/femer.2023.1310474
Received: 09 October 2023; Accepted: 21 November 2023;
Published: 11 December 2023.
Edited and reviewed by: Charles Cairns, Drexel University, United States
Copyright © 2023 Chan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Theodore C. Chan, dGNjaGFuJiN4MDAwNDA7aGVhbHRoLnVjc2QuZWR1
 Theodore C. Chan
Theodore C. Chan