- 1Pediatric Dentistry, Dr. Sulaiman Al Habib Medical Group, Ar Rayyan, Riyadh, Makkah Province, Saudi Arabia
- 2School of Dentistry, The University of Western Australia, Nedlands, WA, Australia
- 3Department of Pediatric Dentistry, Virginia Commonwealth University School of Dentistry, Richmond, VA, United States
Objectives: To conduct a narrative review of the published literature on the localization techniques to identify the best technique for the localization of supernumerary teeth.
Methods: An extensive search of literature published in English between January 1966 and May 2024 was conducted using the “Medline via PubMed” and “Cochrane database” databases. The keywords included in the search were “localization” “radiographs”, and “impacted teeth”, or “un-erupted teeth”, or “supernumerary teeth” or “supernumerary tooth”. The citation lists from the included articles were examined to identify additional reports and a hand search was also conducted. Kappa statistics were used for intra-examiner reliability.
Results: The initial search yielded 4,864 citations, subsequently examined and supplemented by a hand search to find additional studies. Commonly used techniques for the localization of supernumerary teeth are the horizontal tube shift technique, vertical tube shift technique, vertex occlusal technique, and cone-beam computerized tomography.
Conclusion: The most commonly used localization techniques for supernumerary teeth are horizontal tube shift, vertex occlusal, vertical tube shift, and cone-beam computerized tomography. Conventional radiographs only provide two-dimensional views of 3-dimensional structures. Three-dimensional imaging alone can provide accurate data on impacted supernumerary teeth but, the need for this film has to be justified because of the higher radiation exposure.
1 Introduction
Supernumerary teeth are defined as “any tooth or odontogenic structure that is formed from a tooth germ in excess of the usual number for any given region of the dental arch” (1). They may be single or multiple, unilateral or bilateral in distribution, and can occur in both dental arches, and either in the primary mixed or permanent dentitions. The mesiodens is the most commonly occurring supernumerary tooth followed by mandibular premolars, which are the supernumerary teeth of the supplemental type (2–4). Males are more commonly affected than females, at a ratio of 2:1 (5, 6). Several hypotheses have been proposed to explain the occurrence of supernumerary teeth, but their etiology remains unclear (1, 7). According to one systematic review, the prevalence of supernumerary teeth ranges from 1.5% to 3% in the general population with a predilection to the mongoloid racial group (8). Early identification and appropriate management are critical to either limit or prevent the consequences of supernumerary teeth, which range from crowding to cyst formation. Clinical diagnosis is the primary and most important aid in the diagnosis of an impacted tooth (9, 10). Clinical localization includes visual inspection and palpation, while radiographic localization is based on different combinations of radiographs (11). Localization of supernumerary teeth plays a major role in diagnosis and treatment planning, especially if surgical intervention is required (12). Although early intervention can potentially prevent later complications, several authors have been cited as having anecdotally suggested that this approach is harmful due to the possible risk of damage to the developing tooth germs (1, 2). The location of supernumerary teeth can be confirmed by using a variety of imaging techniques. The interpretation principle “SLOB” (Same Lingual Opposite Buccal) rule is the most commonly used one when applying the concept of parallax (13). Localization of an un-erupted tooth is based on a combination of clinical and radiographic assessment (14). The more exact the localization of supernumerary teeth, potentially the less invasive the surgical procedure; therefore, the purpose of this paper was to conduct a narrative review of the available literature and to identify the best technique for the localization of supernumerary teeth.
2 Materials and methods
An extensive search of literature published in English between January 1966 and May 2024 was conducted using the “Medline via PubMed” and “Cochrane database” databases. The keywords included in the search were “localization” and “radiographs”, and “impacted teeth”, “un-erupted teeth”, or “supernumerary teeth” or “supernumerary tooth”. The citation lists from the included references were subsequently examined, in addition hand searching was performed in an attempt to identify additional papers. Kappa statistics were used for intra-examiner reliability.
3 Results
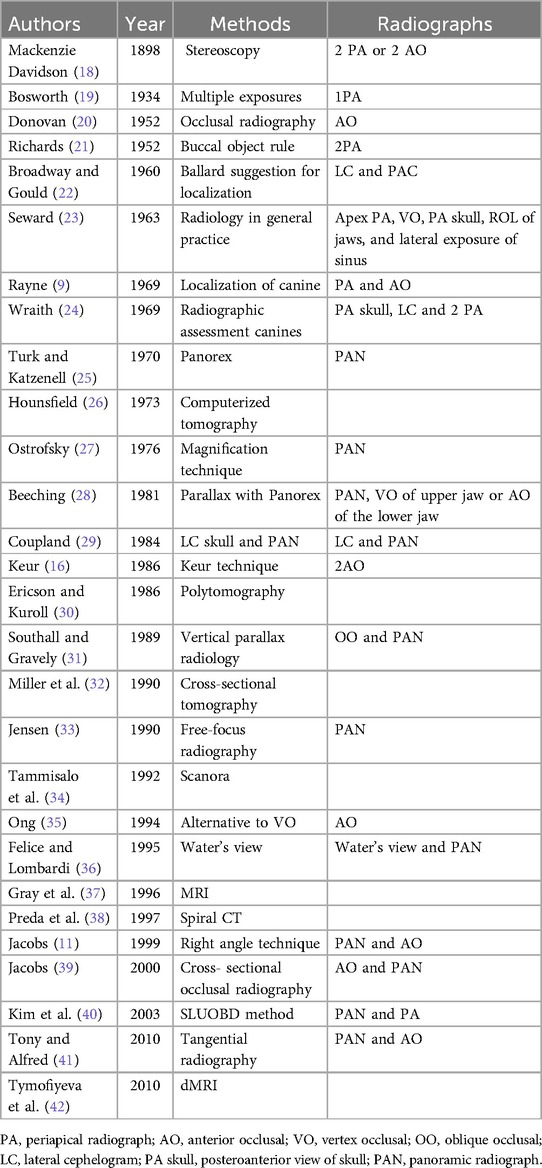
The initial search yielded 4,873 citations from PubMed Medline and 27 from Cochrane database, which were subsequently examined and supplemented by a hand search to find additional studies. Eighteen articles were available for final analysis on the localization of supernumerary teeth five related to horizontal tube shift technique (HTST) (5), six each related to vertical tube shift technique (VTST) and cone beam computerized tomography (CBCT) (6), and one related to computerized tomography (CT). No literature was evident for panoramic radiographs alone and magnetic resonance imaging (MRI) for the localization of supernumerary teeth. The most commonly used techniques for the localization of supernumerary teeth are Clark's technique (13), vertex occlusal (15), and Keur's technique (16), all of which involve the use of conventional radiographs (Table 1). Three-dimensional radiographs for localization and dimensional evaluation include CBCT, CT, MRI, Spiral computerized tomography (SCT), Scanora, and dental magnetic resonance imaging (dMRI), of which CBCT is most often used for the localization of un-erupted impacted/supernumerary teeth in the anterior region of the maxilla (Table 1). Only one reviewer was involved in the literature search and Kappa statistics showed good intra-examiner reliability (K = 0.89). Various localization techniques have been described in the literature (9, 11, 13, 15–42). The most commonly used ones for the localization of supernumerary teeth (13, 15–17), and all the other techniques used for localization of impacted teeth have been summarized in Table 2. The most frequently used localization techniques are described in detail in the text.
3.1 Horizontal tube shift technique (HTST)
Classically, this technique requires three periapical radiographs, one on the tooth of interest followed by one mesial and another distal to the first radiograph (13) see Figure 1. However, over the years, there has been a reduction in the number of films used for this technique, so presently only two periapical films are routinely used. While maintaining the same horizontal plane, a tube shift of 20° to 30° is made between each film. This technique is commonly referred to as Clark's technique and employs the principle of parallax to delineate the spatial relationships of an object.
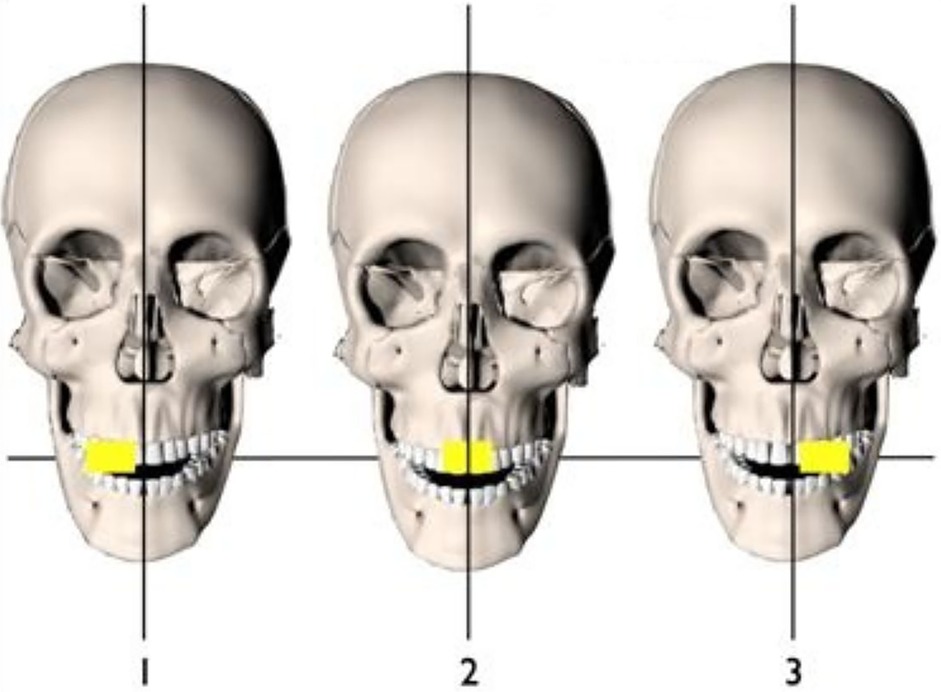
3.2 Vertex occlusal
Localization of an impacted tooth by radiographic means is dependent on the presence of fixed points apparent both visibly and radiographically (15). To obtain the accurate location of an impacted tooth, the central ray of the x-ray beam must be directed along the long axis of those teeth in the dental arch, which is to be used as reference points. An intraoral intensifying screen may be used to reduce the radiation dose. This technique is not recommended when the voltage of the dental x-ray set is less than 65 kV (43), and it is not acceptable when a long exposure time is needed. These results in a high patient dose and a film of low diagnostic quality because of fogging from scattered radiation see Figure 2. An alternative technique was proposed for the benefit of patients and clinicians, this involved an erect Potter Bucky diaphragm or a fine stationary radiographic grid that can be employed along with the occlusal film (35). However, this technique is not recommended for Class II division 2 malocclusion patients (44), where the retroclination of the maxillary incisors results in the frontal bone obscuring the incisor region. However, probably because of the dosage issues and the quality of the poor image, this method is no longer favored.
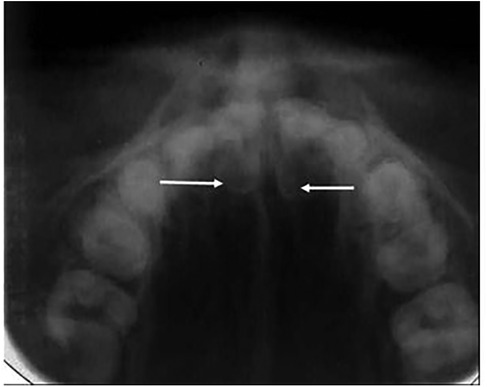
Figure 2. Two palatally located supernumerary teeth [arrows] on a vertex occlusal film, note the lack of clarity of images.
3.3 Vertical tube shift technique (VTST)
This method was introduced with the combination of panoramic and occlusal radiographs to localize an unerupted tooth in the anterior region of the maxilla (16). To obtain the panoramic radiography, the tube is positioned behind the patients’ head at an angle of −7° to the occlusal plane, and the film is placed in front of the head. Nevertheless, to aid the interpretation of tube shift, the tube can be considered to be in front of the patients' head at an effective angle of +7°, and the anterior occlusal radiograph is taken at an angle of +60° to 65° to the occlusal plane (Figure 3). Although a VTST using the PR and OR is usually not as easy to interpret, the PR-OR combination is traditionally preferred. This is because the PR, which contains information about all the teeth in both arches as well as about the jaws and surrounding structures, is often already available; it is usually taken as an initial radiograph, so only one additional exposure is required (anterior occlusal). Eventually, modifications were made in the angulations of VTST; the difference in the positioning of the tube for illustrations for occlusal radiographs 600 and 700 has been demonstrated. However, the recommendation is to increase the tube angle from 600 to 650 and 700 to 750 (11, 39). In a panoramic radiograph, the relationship between the images of the un-erupted ST with the reference objects is unaltered if the x-ray tube is considered to be on the facial side of the arches rather than on the lingual or buccal. The larger the distance between the impacted tooth and the image of an impacted tooth with a given x-ray tube movement, results in the easier determination of its position. Both the positions of the crown and of the root apex should be checked to gain a full picture of the position of the impacted tooth. Furthermore, it has been stated that this combination of radiographs should provide the clinician with a good diagnostic yield for the radiation dose given (44).
3.4 Cone beam computerized tomography [CBCT]
The CBCT respectively offers 3D- imaging of the maxillofacial region, providing the opportunity to study objectives in all standard plans with 3D reconstruction in multi-section views (17). The exact localization of supernumerary teeth is often difficult to assume by using conventional radiological techniques like PVTSAN or intra-oral dental films. A preoperative radiological investigation using CBCT on patients who are prepared to undergo surgery for impacted and supernumerary teeth in the frontal maxilla can more certainly indicate the nature of the pathology and hence enhance the surgical safety (Figure 4).
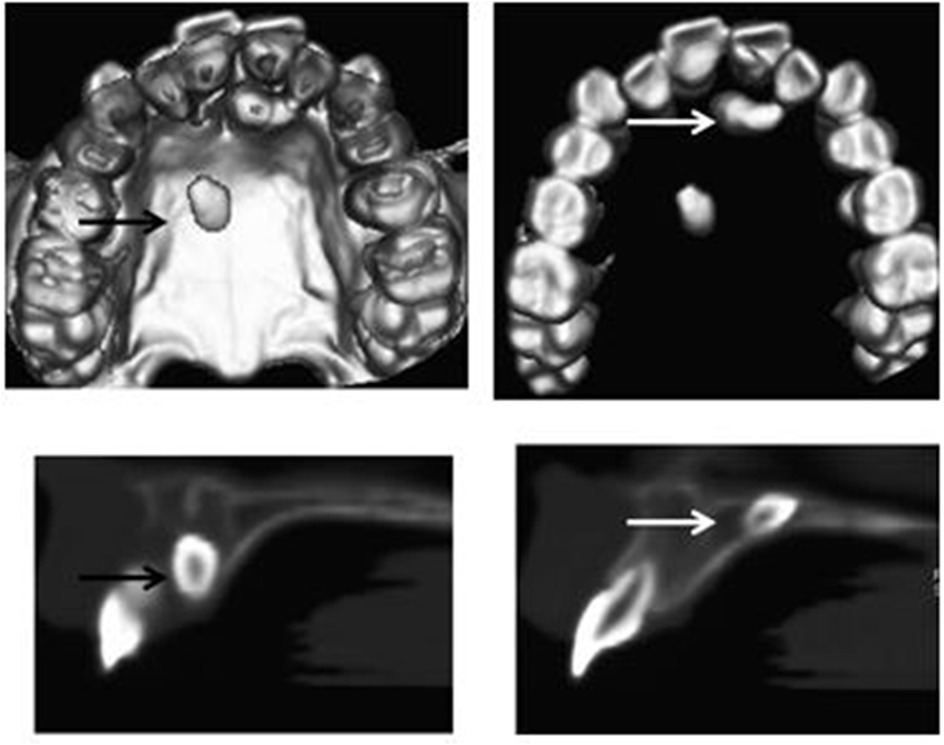
Figure 4. Cone beam computerized tomography 3D images are used for the localization of supernumerary teeth [arrows].
4 Discussion
A combination of clinical and radiological assessments is necessary for the diagnosis of supernumerary teeth. Most often, clinicians will take radiographs based on clinical information to confirm the diagnosis of supernumerary teeth. The localization of supernumerary teeth from radiographs is an important diagnostic adjunct to clinical assessment, diagnosis, and treatment planning. This is most important when surgical intervention is required. To evaluate the position and orientation of supernumerary teeth, the most commonly obtained radiographs are periapical, occlusal, panoramic, and lateral cephalograms. By localizing the supernumerary teeth, the site and extension of the flap margins and the amount of bone removal can be planned prior to surgical intervention. Although periapical, occlusal, and panoramic radiographs are usually able to provide the required information, these modalities do not always provide sufficient information concerning the 3-dimensional [3D] relationship of the supernumerary teeth and the surrounding structures for surgical planning (45, 46). One of the limitations of a single radiograph is its relative inability to demonstrate the relationship between two objects that are either side by side or superimposed (47). It is difficult to determine whether both are in the middle of the bone or buccal or lingual to each other. Furthermore, numerous alternative localization strategies have been articulated as a principle for interpreting buccal and lingual relationships in serial images produced from different techniques. However, different imaging modalities, ranging from intra-oral and extra-oral radiographs to computed tomography (CT) have been used for the evaluation of supernumerary teeth. The most frequently used localization techniques are the horizontal (13) and vertical tube shift (16) techniques using conventional radiographs. Stereoscopic methods (18) were used to localize the foreign bodies, such as bullets and impacted teeth prior to Clark's horizontal tube shift technique (13). Subsequently, based on this principle, various tube shift techniques have been proposed in the literature. However, the interpretation of both techniques enables the clinician to determine the relative position of the displaced tooth (48). The clinical signs provide preliminary information that later is confirmed by radiographic examination.
The treatment decisions have traditionally been based on planar 2-dimensional radiographs such as intraoral and extraoral radiographs (49). Although many localization techniques have been proposed using different combinations of radiographs, they just provide a 2-dimensional view of 3-dimensional structures. The introduction of cone-beam computerized tomography [CBCT] in dentomaxillofacial radiology has created new diagnostic possibilities, which includes evaluating supernumerary teeth (50). However, currently, CBCT has limited usage due to its high cost, low vertical resolution, and high radiation dosage (51). CBCT can be used to provide a 3-dimensional visualization of the oral maxillofacial complex, which aids in the formation of the treatment plan (52). This new imaging technique provides a rapid 3D volumetric image, with low radiation exposure than conventional CT. Using CBCT, the clinician can view the data in axial, sagittal, and coronal sections in three dimensions. Besides, it is possible to obtain periapical, panoramic, occlusal, and lateral cephalograms from a single cone beam scan. CBCT provides a 3-dimensional view with more detailed and accurate imaging compared to conventional and digital radiographs. Nevertheless, the clinician should determine the risks and benefits of imaging for each individual. Furthermore, some significant factors need to be considered; when deciding whether to purchase a CBCT device or to refer patients to imaging centers which include cost, the time required to generate images, training, data transmission and storage, knowledge about software, and accountability for the interpretation and review of the pathology. Many published studies and case reports have accepted the use of CBCT images in oral maxillofacial surgery, dental implantology, orthodontics, and pediatric dentistry because of measurement accuracy, comparisons between 2-D and 3-D images for diagnosis and treatment planning, and the clinical use of native 3-D information. The exposure dose for CBCT devices is typically in the range between 40 and 135 μSV, and the scan time generally from 5.7 to 40 s. The effective absorbed radiation dose for a complete cone beam volume tomographic image of the maxillofacial area is within the range for a full-mouth set of periapical films (53). There is controversy over the prophylactic removal of unerupted supernumerary teeth, which do not have any apparent pathological complications. It has been suggested that early removal prevents space loss and avoids extensive orthodontic treatment in the future (52). Alternatively, studies have reported an eruption rate of approximately 80% for supernumerary teeth positioned normally (54, 55). Accurate localization of supernumerary teeth is required to make a comprehensive diagnosis, determine the appropriate surgical access, and treatment planning. For a pediatric patient, knowing the exact position of supernumerary teeth is paramount to avoiding potential complications. The risk of problems associated with the supernumerary teeth in the anterior maxillary region, early diagnosis of disturbances, and proper management are considered to be important in factors growing children (56). A recent revolution of artificial intelligence (AI) when used in dentistry has given new scope for the identification of supernumerary teeth using various AI tools (57–59). The AI technologies, especially in dental imaging, enhance accuracy and efficiency to identification, and hence management of dental anomalies (57). The incorporation of artificial intelligence in dental practices is through enhancing diagnostic accuracy and making tailored treatment strategies possible. AI systems such as Diagnocat analyze, dental images used to identify supernumerary teeth and offer a comprehensive treatment planning option that demonstrates AI's capability to improve diagnostic accuracy and efficiency in dentistry (59). AI-powered tools that use deep learning neural networks are excellent at identifying and numbering teeth on panoramic x-rays, that is necessary for identifying supernumerary teeth (60, 61).
Although, CBCT and traditional radiographs are equally effective for the initial diagnosis of pathology. CBCT provides more information on the location of pathology and the presence of root resorption, which is crucial for treatment planning (62, 63). However, there has been limited research on various conventional radiographic methods for localizing impacted teeth (59, 62–64). Most of the reports in the literature focus on the localization of impacted canines and third molars, with only a few studies reporting on the localization of supernumerary teeth (65, 66). A recent study revealed that VTST outperforms HTST in accurately locating supernumerary teeth in the anterior region of the maxillary arch (65). However, the results are not statistically significant. The CBCT is better than traditional radiography because it offers accurate and authentic anatomical information with excellent surgical predictability without distortion or artifacts. It reduces costs and surgical challenges, enabling faster surgery completion (66). Researchers have reported no significant difference in localizing dilacerations, supernumerary teeth, and impacted incisors in the anterior region of the maxilla using a periapical film instead of an anterior occlusal film (2, 40). Most recently, several studies focused on using 3D imaging for the identification of the supernumerary teeth (61, 67). Toureno et al. (67) proposed a guideline for the identification and localization of supernumerary teeth in both two and three dimensions. The guideline aimed to minimize treatment errors and enhance communication among healthcare professionals and third-party administrators. CBCT provides clear 3D images that help doctors accurately locate missing teeth and other structures in the area (66–68). This is important for planning effective treatment and surgeries. Studies have shown that CBCT is more accurate at diagnosing than 2D radiographs, with an accurate preoperative finding rate (68–70). Recently various epidemiological studies used CBCT to report the prevalence of supernumerary teeth. It was truly evident that the trends of shifting from two-dimensional imaging to CBCT can better assess the number, location, shape, and position of supernumerary teeth, providing a comprehensive evaluation that is beneficial for preventing complications (69–72). Nevertheless, in situations involving multiple supernumerary teeth or when precise positioning is crucial, CBCT remains the preferred choice (72, 73). Even though CBCT excels in numerous facets, two dimensionals radiographs certain their significance in preliminary evaluations because of their economical nature and lower radiation risk (74). The is narrative review evaluates the available localization techniques when used to locate the position of impacted teeth, particularly supernumerary teeth.
5 Conclusion
The most commonly used localization techniques for supernumerary teeth are horizontal tube shift, vertex occlusal, vertical tube shift, and cone-beam computerized tomography. Unfortunately, conventional radiographs are only able to provide two-dimensional views of three-dimensional structures. Nevertheless, three-dimensional imaging alone can provide precise and accurate data on impacted supernumerary teeth however, the need for this film has to be justified because of the higher radiation exposure. The paper also describes the trends in the use of other various techniques for the localization of supernumerary teeth.
Author contributions
SM: Conceptualization, Data curation, Formal Analysis, Investigation, Methodology, Visualization, Writing – original draft, Writing – review & editing. RA: Conceptualization, Funding acquisition, Investigation, Project administration, Resources, Supervision, Writing – original draft, Writing – review & editing. JJ: Methodology, Software, Validation, Visualization, Writing – original draft, Writing – review & editing. NK: Funding acquisition, Project administration, Resources, Supervision, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Omer RS, Anthonappa RP, King NM. Determination of the optimum time for surgical removal of unerupted anterior supernumerary teeth. Pediatr Dent. (2010) 32:14–20.20298648
2. Seehra J, Mortaja K, Wazwaz F, Papageorgiou SN, Newton JT, Cobourne MT. Interventions to facilitate the successful eruption of impacted maxillary incisor teeth due to the presence of a supernumerary: a systematic review and meta-analysis. Am J Orthod Dentofacial Orthop. (2023 May) 163(5):594–608. doi: 10.1016/j.ajodo.2023.01.004
3. King NM, Lee AM, Wan PK. Multiple supernumerary premolars: their occurrence in three patients. Aust Dent J. (1993) 38:11–6. doi: 10.1111/j.1834-7819.1993.tb05445.x
4. Khalaf K, Brook AH, Smith RN. Genetic, epigenetic and environmental factors influence the phenotype of tooth number, size and shape: anterior maxillary supernumeraries and the morphology of mandibular incisors. Genes. (2022) 13(12):2232. doi: 10.3390/genes13122232
5. Brook AH. Dental anomalies of number, form and size: their prevalence in British schoolchildren. J Int Assoc Dent Child. (1974) 5:37–53.4535299
6. Anthonappa RP, Omer RS, King NM. Characteristics of 283 supernumerary teeth in southern Chinese children. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. (2008) 105:48–54. doi: 10.1016/j.tripleo.2008.01.035
7. Anthonappa RP, King NM, Rabie AB. Aetiology of supernumerary teeth: a literature review. Eur Arch Paediatr Dent. (2013) 14:279–88. doi: 10.1007/s40368-013-0082-z
8. Anthonappa RP, King NM, Rabie AB. Prevalence of supernumerary teeth based on panoramic radiographs revisited. Pediatr Dent. (2013) 35:257–61.23756311
10. Williams BH. Diagnosis and prevention of maxillary cuspid impaction. Angle Orthod. (1981) 51:30–40.6939352
11. Jacobs SG. Radiographic localization of unerupted maxillary anterior teeth using the vertical tube shift method. The history and application of the method with some case reports. Am J Orthod Dentofac Orthop. (1999) 116:415–23. doi: 10.1016/S0889-5406(99)70226-X
12. Anthonappa RP, King NM, Rabie AB, Mallineni SK. Reliability of panoramic radiographs for identifying supernumerary teeth in children. Int J Paediatr Dent. (2012) 22:37–43. doi: 10.1111/j.1365-263X.2011.01155.x
13. Clark C. A method of ascertaining the position of unerupted teeth by means of film radiographs. Proc R Soc Med. (1910) 3:87–90.19974610
14. Counihan K, Al-Awadhi EA, Butler J. Guidelines for the assessment of the impacted maxillary canine. Dent Update. (2013) 40:770–7. doi: 10.12968/denu.2013.40.9.770
16. Keur JJ. Radiographic localization techniques. Aust Dent J. (1986) 31:86–90. doi: 10.1111/j.1834-7819.1986.tb02566.x
17. Mozzo P, Procacci C, Tacconi A, Martini PT, Andreis IAB. A new volumetric CT machine for dental imaging based on the cone-beam technique: preliminary results. Eur Radiol. (1998) 8:1558–64. doi: 10.1007/s003300050586
18. Davidson JM. Roentgen rays and localisation: an apparatus for exact measurement and localisation by means of roentgen rays. Br Med J. (1898) 1:10–3. doi: 10.1136/bmj.1.1931.10
20. Donovan MH. Occlusal radiography of the mandibular third molar. Dent Radiogr Photogr. (1952) 25:53–5.
21. Richards AG. Roentgenographic localization of the mandibular canal. J Oral Surg. (1952) 10:325–9.12991124
22. Broadway RT, Gould DG. Surgical requirements of the orthodontist. Br Dent J. (1960) 108( ):1187–90.
23. Seward GR. Radiology in general dental practice: unerupted maxillary canines, central incisors and supernumeries. Br Dent J. (1963) 115:85–9.
24. Wraith KW. Methods of repositioning the misplaced canine. Dent Pract Dent Rec. (1969) 19:387–93.5255837
25. Turk MH, Katzenell J. Panoramic localization. Oral Surg Oral Med Oral Pathol Endod. (1970) 29:212–5. doi: 10.1016/0030-4220(70)90084-8
26. Hounsfield GN. Computerised transverse axial scanning [tomography]. Br J Radiol. (1973) 46:1016–22. doi: 10.1259/0007-1285-46-552-1016
27. Ostrofsky MK. Localization of impacted canines with Status-X radiography. Oral Surg Oral Med Oral Pathol. (1976) 42:529–33. doi: 10.1016/0030-4220(76)90301-7
28. Beeching BW. Parallax with the panorex. Br Dent J. (1981) 151:369–73. doi: 10.1038/sj.bdj.4804707
29. Coupland MA. Localisation of misplaced maxillary canines: orthopantomograph and P.A. Skull views compared. Br J Orthod. (1984) 11:27–32. doi: 10.1179/bjo.11.1.27
30. Ericson S, Kurol J. Radiographic assessment of maxillary canine eruption in children with clinical signs of eruption disturbance. Eur J Orthod. (1986) 8:133–40. doi: 10.1093/ejo/8.3.133
31. Southall PJ, Gravely JF. Vertical parallax radiology to localize an object in the anterior part of the maxilla. Br J Orthod. (1986) 16:79–83. doi: 10.1179/bjo.16.2.79
32. Miller CS, Nummikoski PV, Barnett DA, Langlais RP. Cross-sectional tomography. A diagnostic technique for determining the buccolingual relationship of impacted mandibular third molars and the inferior alveolar neurovascular bundle. Oral Surg Oral Med Oral Pathol. (1990) 70:791–7. doi: 10.1016/0030-4220(90)90023-L
33. Jensen TW. Fine-detail panoramic radiography by free-focus radiography. A clinical demonstration of diagnostic radiographs. Oral Surg Oral Med Oral Pathol. (1990) 70:502–15. doi: 10.1016/0030-4220(90)90219-I
34. Tammisalo E, Hallikainen D, Kanerva H, Tammisalo T. Comprehensive oral x-ray diagnosis: scanora multimodal radiography. A preliminary description. Dentomaxillofac Radiol. (1992) 21:9–15. doi: 10.1259/dmfr.21.1.1397455
35. Ong A. An alternative technique to the vertex/true occlusal view. Am J Orthod Dentofacial Orthop. (1994) 106:621–6. doi: 10.1016/S0889-5406(94)70087-7
36. Di Felice R, Lombardi T. Ectopic third molar in the maxillary sinus: case report. Aust Dent J. (1995) 40:236–7. doi: 10.1111/j.1834-7819.1995.tb04802.x
37. Gray CF, Redpath TW, Smith FW. Pre-surgical dental implant assessment by magnetic resonance imaging. J Oral Implantol. (1996) 22:147–53.9151637
38. Preda LA, La Fianza A, Di Maggio EM, Dore R, Schifino MR, Campani R, et al. The use of spiral computed tomography in the localization of impacted maxillary canines. Dentomaxillofac Radiol. (1997) 26:236–41. doi: 10.1038/sj.dmfr.4600258
39. Jacobs SG. Radiographic localization of unerupted teeth: further findings about the vertical tube shift method and other localization techniques. Am J Orthod Dentofacial Orthop. (2000) 118:439–47. doi: 10.1067/mod.2000.108782
40. Kim JD, Lee CY, You CH. The radiographic localization of unerupted maxillary incisors and supernumeraries. Korean J Oral Maxillofac Radiol. (2003) 33:217–21.
41. Tony A. Localization of impacted maxillary anterior tooth with tangential radiograph. H K Dent J. (2009) 6:46–8.
42. Tymofiyeva O, Rottner K, Jakob PM, Richter EJ, Proff P. Three-dimensional localization of impacted teeth using magnetic resonance imaging. Clin Oral Investig. (2010) 14:169–76. doi: 10.1007/s00784-009-0277-1
43. McNicol A, Stirrups DR. Radiation dose during the dental radiographic techniques most frequently used during orthodontic treatment. Eur J Orthod Dentomaxillofac Radiol. (2012) 41:444–9. doi: 10.1259/dmfr/19442214
44. Langlais RP, Langland OE, Morris CR. Radiographic localization techniques. Dent Radiogr Photogr. (1979) 52:69–77.292601
45. Gavel V, Dermaut L. The effect of changes in tooth position of unerupted canines on cephalograms. Eur J Orthod. (2003) 25:49–56. doi: 10.1093/ejo/25.1.49
46. Frederiksen NL. Guidelines for prescribing dental radiographs. United states food and drug administration. Tex Dent J. (1995) 112:63–7.8633307
47. Schulze D, Heiland M, Thurmann H, Adam G. Radiation exposure during midfacial imaging using 4- and 16-slice computed tomography, cone beam computed tomography systems, and conventional radiography. Dentomaxillofac Radiol. (2004) 33:83–6. doi: 10.1259/dmfr/28403350
48. Ludlow JB, Davies-Ludlow LE, Brooks SL. Dosimetry of two extraoral direct digital imaging devices: NewTom cone beam CT and orthophos plus DS panoramic unit. Am J Orthod Dentofacial Orthoped. (2005) 128:418–23. doi: 10.1016/j.ajodo.2004.04.033
49. Howerton WB Jr, Mora MA. Advancements in digital imaging: what is new and on the horizon? J Am Dent Assoc. (2008) 139:20–4. doi: 10.14219/jada.archive.2008.0354
50. Mah JK, Danforth RA, Bumann A, Hatcher D. Radiation absorbed in maxillofacial imaging with a new dental computed tomography device. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. (2003) 96:508–13. doi: 10.1016/S1079-2104(03)00350-0
51. Ludlow LE, Brooks SL, Howerton WB. Dosimetry of 3 CBCT devices for oral and maxillofacial radiology: CB Mercuray, NewTom 3G, and i-CAT. Dentomaxillofac Radiol. (2006) 35:219–26. doi: 10.1259/dmfr/14340323
52. Mallineni SK, Alassaf A, Almulhim B, Alghamdi S. Dental anomalies in primary dentition among Arabian children: a hospital-based study. Children. (2024) 11(3):366. doi: 10.3390/children11030366
53. Kau CH, Richmond S, Palomo JM, Hans MG. Three-dimensional cone beam computerized tomography in orthodontics. J Orthod. (2005) 32:282–3. doi: 10.1179/146531205225021285
54. Pescia R, Kiliaridis S, Antonarakis GS. Spontaneous eruption of impacted maxillary incisors after surgical extraction of supernumerary teeth: a systematic review and meta-analysis. Clin Oral Investig. (2020) 24(11):3749–59. doi: 10.1007/s00784-020-03369-3
55. Mallineni SK, Aldhuwayhi S, Deeban Y, Almutairi KS, Alhabrdi SN, Almidaj MA, et al. Prevalence, occurrence, and characteristics of supernumerary teeth among the Saudi Arabian population using panoramic radiographs. Diagnostics. (2024) 14(22):2542. doi: 10.3390/diagnostics14222542
56. Brinkmann JC, Martínez-Rodríguez N, Martín-Ares M, Sanz-Alonso J, Marino JS, Suárez García MJ, et al. Epidemiological features and clinical repercussions of supernumerary teeth in a multicenter study: a review of 518 patients with hyperdontia in Spanish population. Eur J Dent. (2020) 14(3):415–22. doi: 10.1055/s-0040-1712860
57. Hayashi-Sakai S, Nishiyama H, Hayashi T, Sakai J, Shimomura-Kuroki J. Deep learning with convolution neural network detecting mesiodens on panoramic radiographs: comparing four models. Odontology. (2025) 113(1):448–55. doi: 10.1007/s10266-024-00980-8
58. Kaya E, Güneç HG, Ürkmez EŞ, Aydın KC, Fehmi H. Deep learning for diagnostic charting on pediatric panoramic radiographs. Int J Comput Dent. (2024 Oct 15) 27(3):225–33. doi: 10.3290/j.ijcd.b4200863
59. Mladenovic R, Arsic Z, Velickovic S, Paunovic M. Assessing the efficacy of ai segmentation in diagnostics of nine supernumerary teeth in a pediatric patient. Diagnostics. (2023) 13(23):3563. doi: 10.3390/diagnostics13233563
60. Mine Y, Iwamoto Y, Okazaki S, Nakamura K, Takeda S, Peng TY, et al. Detecting the presence of supernumerary teeth during the early mixed dentition stage using deep learning algorithms: a pilot study. Int J Paediatr Dent. (2022) 32(5):678–85. doi: 10.1111/ipd.12946
61. Katheria BC, Kau CH, Tate R, Chen JW, English J, Bouquot J. Effectiveness of impacted and supernumerary tooth diagnosis from traditional radiography versus cone beam computed tomography. Pediatr Dent. (2010) 32:304–49.20836949
62. Henninger E, Friedli L, Makrygiannakis MA, Zymperdikas VF, Papadopoulos MA, Kanavakis G, et al. Supernumerary tooth patterns in non-syndromic white European subjects. Dent J. (2023) 11(10):230. doi: 10.3390/dj11100230
63. Hadziabdic N, Haskic A, Mujkic A, Hasic-Brankovic L, Dzankovic A, Korac S, et al. Epidemiological, clinical and radiographic features of supernumerary teeth in nonsyndromic Bosnian and Herzegovinian population: a monocentric study. Med Arch. (2022) 76(5):348–53. doi: 10.5455/medarh.2022.76.348-353
64. He L, Que G, Yang X, Yan S, Luo S. Prevalence, clinical characteristics, and 3-dimensional radiographic analysis of supernumerary teeth in Guangzhou, China: a retrospective study. BMC Oral Health. (2023) 23(1):351. doi: 10.1186/s12903-023-03032-9
65. Mallineni SK, Anthonappa RP, King NM. Reliability of horizontal and vertical tube shift techniques in the localisation of supernumerary teeth. Eur Arch Paediatr Dent. (2016) 17(6):455–60. doi: 10.1007/s40368-016-0253-9
66. Ziegler CM, Klimowicz TR. A comparison between various radiological techniques in the localization and analysis of impacted and supernumerary teeth. Indian J Dent Res. (2013) 24(3):336–41. doi: 10.4103/0970-9290.117998
67. Toureno L, Park JH, Cederberg RA, Hwang EH, Shin JW. Identification of supernumerary teeth in 2D and 3D: review of literature and a proposal. J Dent Educ. (2013) 77(1):43–50. doi: 10.1002/j.0022-0337.2013.77.1.tb05441.x
68. Jiang Y, Ma X, Wu Y, Li J, Li Z, Wang Y, et al. Epidemiological, clinical, and 3-dimentional CBCT radiographic characterizations of supernumerary teeth in a non-syndromic adult population: a single-institutional study from 60,104 Chinese subjects. Clin Oral Investig. (2020) 24(12):4271–81. doi: 10.1007/s00784-020-03288-3
69. Ma X, Jiang Y, Ge H, Yao Y, Wang Y, Mei Y, et al. Epidemiological, clinical, radiographic characterization of non-syndromic supernumerary teeth in Chinese children and adolescents. Oral Dis. (2021) 27(4):981–92. doi: 10.1111/odi.13628
70. Liu X, Ren Q, Bai J, Kang P, Ren G, Li X, et al. Imaging analysis of 1 138 supernumerary teeth by using cone-beam computed tomography. Hua Xi Kou Qiang Yi Xue Za Zhi. (2023) 41(6):671–7.38597032
71. Gurler G, Delilbasi C, Delilbasi E. Investigation of impacted supernumerary teeth: a cone beam computed tomograph (CBCT) study. J Istanb Univ Fac Dent. (2017) 51(3):18–24.29114426
72. Gurgel CV, Costa AL, Kobayashi TY, Rios D, Silva SM, Machado MA, et al. Cone beam computed tomography for diagnosis and treatment planning of supernumerary teeth. Gen Dent. (2012) 60(3):e131–5.22623467
73. Kapila SD, Nervina JM. CBCT In orthodontics: assessment of treatment outcomes and indications for its use. Dentomaxillofac Radiol. (2015) 44(1):20140282. doi: 10.1259/dmfr.20140282
Keywords: localization, radiographs, impacted teeth, supernumerary teeth, CBCT
Citation: Mallineni SK, Anthonappa RP, Jayaraman J and King NM (2025) Radiographic localization of supernumerary teeth: a narrative review. Front. Dent. Med 6:1495025. doi: 10.3389/fdmed.2025.1495025
Received: 11 September 2024; Accepted: 3 January 2025;
Published: 10 February 2025.
Edited by:
Ali Mentes, Marmara University, TürkiyeReviewed by:
Rosa Helena Wanderley Lacerda, Federal University of Paraíba, BrazilAlessandro Venditti, University of Rome Tor Vergata, Italy
Copyright: © 2025 Mallineni, Anthonappa, Jayaraman and King. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Sreekanth Kumar Mallineni, ZHJtYWxsaW5lbmlAZ21haWwuY29t
 Sreekanth Kumar Mallineni
Sreekanth Kumar Mallineni Robert Prashanth Anthonappa
Robert Prashanth Anthonappa Jayakumar Jayaraman
Jayakumar Jayaraman Nigel Martyn King2
Nigel Martyn King2