- 1Department of Social Sciences, University of Luxembourg, Esch-sur-Alzette, Luxembourg
- 2Department of Health, IU Internationale Hochschule, Erfurt, Germany
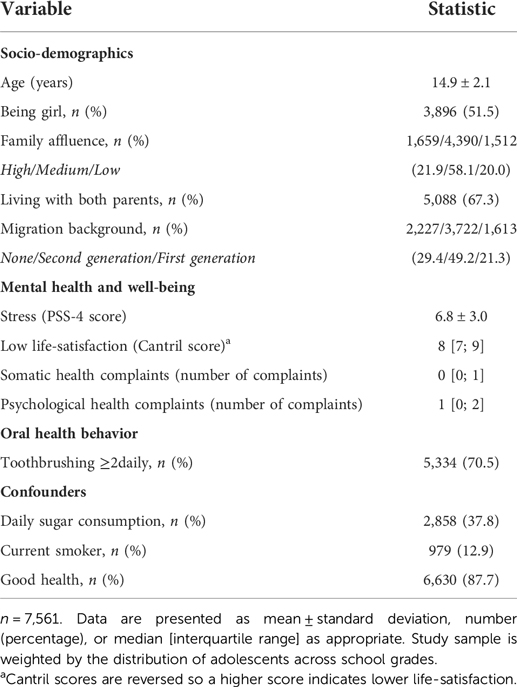
Oral health remains a global health problem. Mental health has been linked to oral health behavior. However, studies among adolescents in high-income countries are limited. This study aimed to investigate the association between adolescent mental health and well-being with regular toothbrushing. We used data from the 2018 Luxembourg Health Behavior in School-Aged Children study (n = 7,561; n = 3,896 [51.5%] girls; mean [standard deviation] age = 14.9 [2.1] years). Multiple logistic regression analyses were performed to assess the associations of self-reported stress levels, life-satisfaction, somatic health complaints, and psychological health complaints with regular toothbrushing (≥2 daily). Analyses were adjusted for gender, age, family affluence, family structure, migration background, daily sugar consumption, smoking behavior, and general health. 70.5% of the adolescents regularly brushed their teeth. Adolescents who reported higher levels of stress (odds ratio [OR], 95% confidence interval [CI]; 0.97 [0.95;0.99] per one-point increase), low life-satisfaction (OR = 0.92 [0.89;0.95] per one-point increase), and psychological health complaints (OR = 0.95 [0.91;0.99] per complaint) were less likely to regularly brush their teeth. No association was found between somatic health complaints and regular toothbrushing (OR = 1.00 [0.94;1.06] per complaint). Adolescents with poor mental health and well-being are less likely to regularly brush their teeth and may have an increased risk for oral diseases. Interventions focused on lifestyle modification in adolescents with mental health problems should include regular toothbrushing to prevent dental caries and other oral diseases.
Introduction
Toothbrushing is the most effective oral hygiene method and a major modifiable risk factor for oral diseases (1, 2). Oral diseases, which are mostly preventable, are an important global health problem affecting more than 3.5 billion people (3, 4). They may have a significant impact on the individual's daily life. Oral diseases have been related to pain, chronic diseases, poorer general health, reduced quality of life and well-being, and problems with eating, chewing, and communication because of missing, discolored or damaged teeth (5). The loss of productivity caused by reduced school, work and household activities places a large burden on the society (5). Untreated dental caries is the most prevalent disease worldwide according to the Global Burden of Disease 2019 (6). In 2015, 573 million children had untreated dental caries (7). The prevalence of untreated caries in permanent teeth peaks during adolescence (15–19 years), affecting almost one in two adolescents (8). Oral health behavior during adolescence is crucial for the prevention of dental caries and other oral diseases and forms the basis of oral health behavior throughout adulthood. During adolescence, many behaviors that can affect oral health, including toothbrushing, are established (9).
Studies have shown an association between mental health and oral health among adults. A meta-analysis including 334,503 participants has shown an association of common mood and anxiety disorders and dental phobia, with dental caries and tooth loss (10). Furthermore, symptoms of depression and anxiety have been related to lower frequency of toothbrushing (11). Evidence for a relationship between mental health and oral health among adolescents is more limited. Research conducted in mainly low- and middle-income countries has related poor mental health to inadequate toothbrushing among adolescents. The World Health Organization (WHO) recommends toothbrushing twice daily with fluoride-containing toothpaste (2, 12). Poor mental health, including anxiety, no close friends, loneliness, depression, symptoms of post-traumatic stress disorder, suicidal ideation and suicide attempt, has been related to irregular toothbrushing among adolescents (13–18). However, contrasting results have been reported. Loneliness, suicidal ideation, sadness, and anxiety were not related to regular toothbrushing among African and Asian adolescents (14–17).
Only two studies in high-income countries have reported on the association of mental health and well-being with toothbrushing (19, 20). Finnish adolescents who reported symptoms of social phobia and generalized anxiety disorder were less likely to regularly brush their teeth compared to adolescents without these symptoms (19). Life-satisfaction was related to regular toothbrushing in the French Health Behavior in School-Aged Children (HBSC) study (20). However, both European studies did not adjust for important confounders like sugar consumption and smoking behavior (3).
The above studies suggest that adolescent mental health is related to oral health behavior. However, the association between adolescent mental health and well-being with oral health behavior in high-income countries needs further investigation. The aim of this study was to investigate the association between adolescent mental health and well-being with regular toothbrushing in Luxembourg. Because socio-demographic differences among adolescents have been reported in relation to both mental health and toothbrushing (21), it was investigated whether potential associations of mental health and well-being with toothbrushing differ by gender, age, and family affluence.
Materials and methods
Study population and design
Data from the 2018 wave of the Luxembourg Health Behavior in School-Aged Children (HBSC) study were used. The HBSC study is a World Health Organization (WHO) collaborative cross-national survey study that is conducted every four years across 50 countries and regions in Europe, Asia, and North America. The rationale and methodology of the 2018 Luxembourg HBSC study have been described previously (21). In brief, the study collected nationally representative data from adolescents aged 11–18 years old. Primary and secondary school classes were selected at random as primary sampling units. Schools that did not teach according to the national curriculum and special needs schools were excluded from sampling. Students from special needs schools were not surveyed because it could not be ensured that they would be able to complete the questionnaire without assistance. Schools that teach according to international curricula were excluded because these students are taught in different languages. This would have made the survey very time-consuming and would have made it possible to identify students retrospectively. Data were collected using paper–pencil questionnaires. Ethical approval was granted by the Comité National d'Ethique de Recherche (CNER, Avis N201711/02) and the Ethics Review Panel of the University of Luxembourg (ERP 17–059 HBSC 2018). All participants and parents were informed about the study and the right to refuse participation. Parents gave opt-out written consent.
Figure 1 shows the flowchart of the study sample. 13,001 adolescents were invited to participate, of whom 9,738 participated (74.9%). Adolescents with missing data on the age variable (n = 315) or who were too young or too old to participate (n = 691) were excluded. Data on other confounders were missing in 1,143 adolescents and toothbrushing data were incomplete in 18 participants. Exclusion of adolescents with unavailable stress (n = 420), life-satisfaction (n = 114), and health complaints (n = 140) data, resulted in a total study sample of n = 7,561 participants. Our analytical sample ranged between n = 7,457 and n = 7,151 participants, depending on the assessed mental health variable.
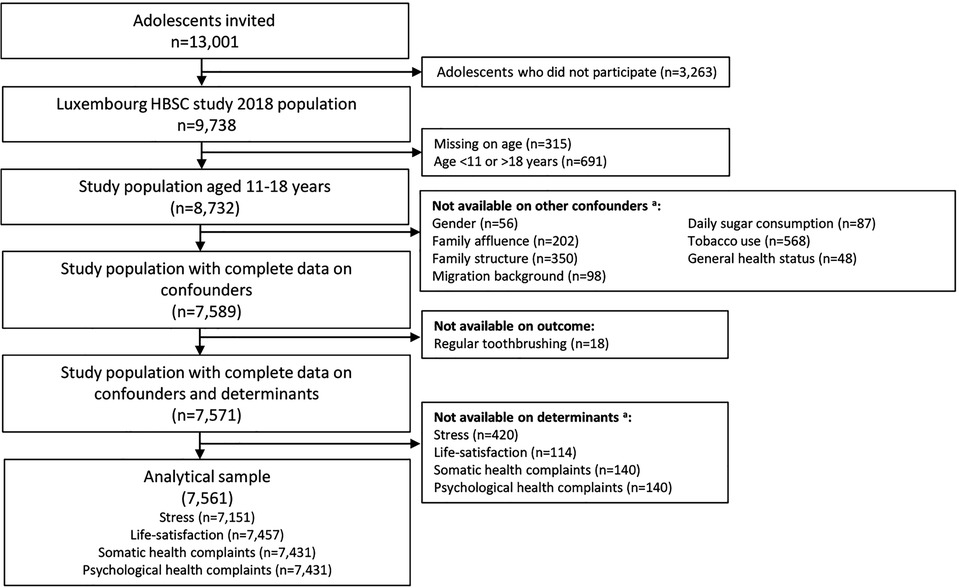
Figure 1. Flowchart HBSC indicates Health Behavior in School-Aged Children. Numbers are weighted by the distribution of adolescents across school grades. aUnavailable data are not mutually exclusive.
Mental health and well-being
The shortened 4-item version of the Cohens’ Perceived Stress Scale-4 (PSS-4) was used to assess general perceived stress (22). Participants were asked how unpredictable, uncontrollable, and overloaded their lives were during the last month, e.g., “How often have you felt confident about your ability to handle your personal problems?”. Items were scored on a 5-point Likert scale with a total score range from 0 to 16. The internal consistency of the scale in this sample was satisfactory (Cronbach's alpha = 0.57).
Life-satisfaction was measured using the Cantril Ladder (23, 24). Participants rated how they feel about their life on a visual analogous scale ranging from 0 (worst possible life) to 10 (best possible life). The Cantril scores were reversed so a higher score indicates lower life-satisfaction.
Subjective psychosomatic health complaints were assessed using the self-reported HBSC-Symptom Checklist (25, 26). The frequency of four somatic complaints (headaches, abdominal pain, backache, and dizziness) and four psychological complaints (feeling low, irritability, nervousness, and sleeping difficulties) during the last six months were assessed. Scores on somatic and psychological complaints ranged between 0 and 4.
Regular toothbrushing
Adolescents were asked how often they brush their teeth. This question was developed by the HBSC network to measure dental care. A dichotomous variable was created to compare adolescents who brush their teeth at least 2 times a day and those who brush their teeth less often. This dichotomization is based on the recommendation of the WHO (2).
Confounders
Adolescents reported their gender and year and month of birth. Socioeconomic status was assessed through the 6-item HBSC Family Affluence Scale (27). Relative family affluence was categorized into low (lowest 20%), medium (medium 60%) and high (highest 20%). Adolescents were asked about the people with whom they lived in their main or only home. Adolescents living with both parents were identified and compared to those with other family structures. Migration background was assessed by country of birth of the participant and their parents, and categorized into native, first-generation immigrant or second-generation immigrant. The frequency of sweets and soft drink consumption was assessed. Participants who consumed sweets and/or soft drinks daily were identified and compared to those who did not consume sweets and/or soft drinks daily. Participants were asked how often they used tobacco over the past 30 days. This question was adapted by the HBSC network from the 1975 Monitoring the Future project (28) and the 1995 European School Survey Project on Alcohol and other Drugs (29). A dichotomous variable was created to identify adolescents who used tobacco during the past 30 days (yes/no). Participants were asked to rate their general health on a four-point Likert-scale (poor, fair, good, and excellent) (30). In line with previous studies from the HBSC network, response options were dichotomized into those who reported their health as excellent or good and those who reported their health as fair or poor (31).
Statistical analyses
Analyses were performed using IBM SPSS version 27. Multiple logistic regression analyses were used to assess the associations of mental health and well-being with regular toothbrushing. Analyses were adjusted for gender, age, family affluence, family structure, migration background, daily sugar consumption, smoking behavior, and general perceived health. The data were weighted by the distribution of adolescents across school grades. Accordingly, the distribution of the adolescents across school grades in the weighted sample was in line with the distribution in the population. To test whether the associations differ among gender, age, and family affluence, interactions of sociodemographic factors with mental health and well-being on regular toothbrushing were tested. A 2-sided P-value <0.05 was considered statistically significant.
Results
General characteristics of the study sample
Table 1 shows the general characteristics of the study sample. Participants had a mean age of 14.9 ± 2.1 years and 51.5% were girls. Regular toothbrushing was reported in 70.5% of the participants and most adolescents had good health (87.7%).
Associations of mental health and well-being with regular toothbrushing
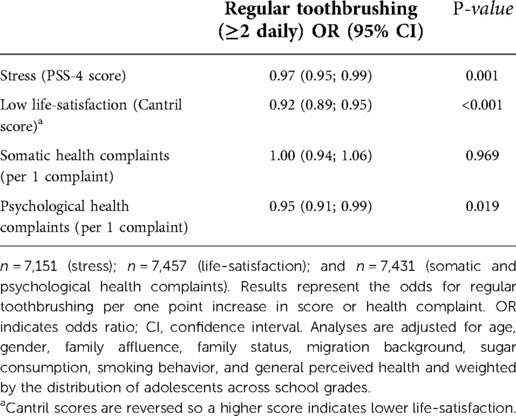
The associations of mental health and well-being with regular toothbrushing are presented in Table 2. Adolescents who reported higher stress levels were less likely to regularly brush their teeth (odds ratio [OR], 95% confidence interval [CI]; 0.97 [0.95;0.99], p = 0.001 per one-point increase in stress level). Furthermore, a one-point increase in low life-satisfaction was associated with lower odds for regular toothbrushing (OR = 0.92 [0.89;0.95], p < 0.001). No association was found between somatic health complaints and regular toothbrushing (OR = 1.00 [0.94; 1.06], p = 0.969 per increase in the number of complaints), while there was an association between psychological health complaints and regular toothbrushing (OR = 0.95 [0.91;0.99], p = 0.019 per increase in the number of complaints).
Socio-demographic differences
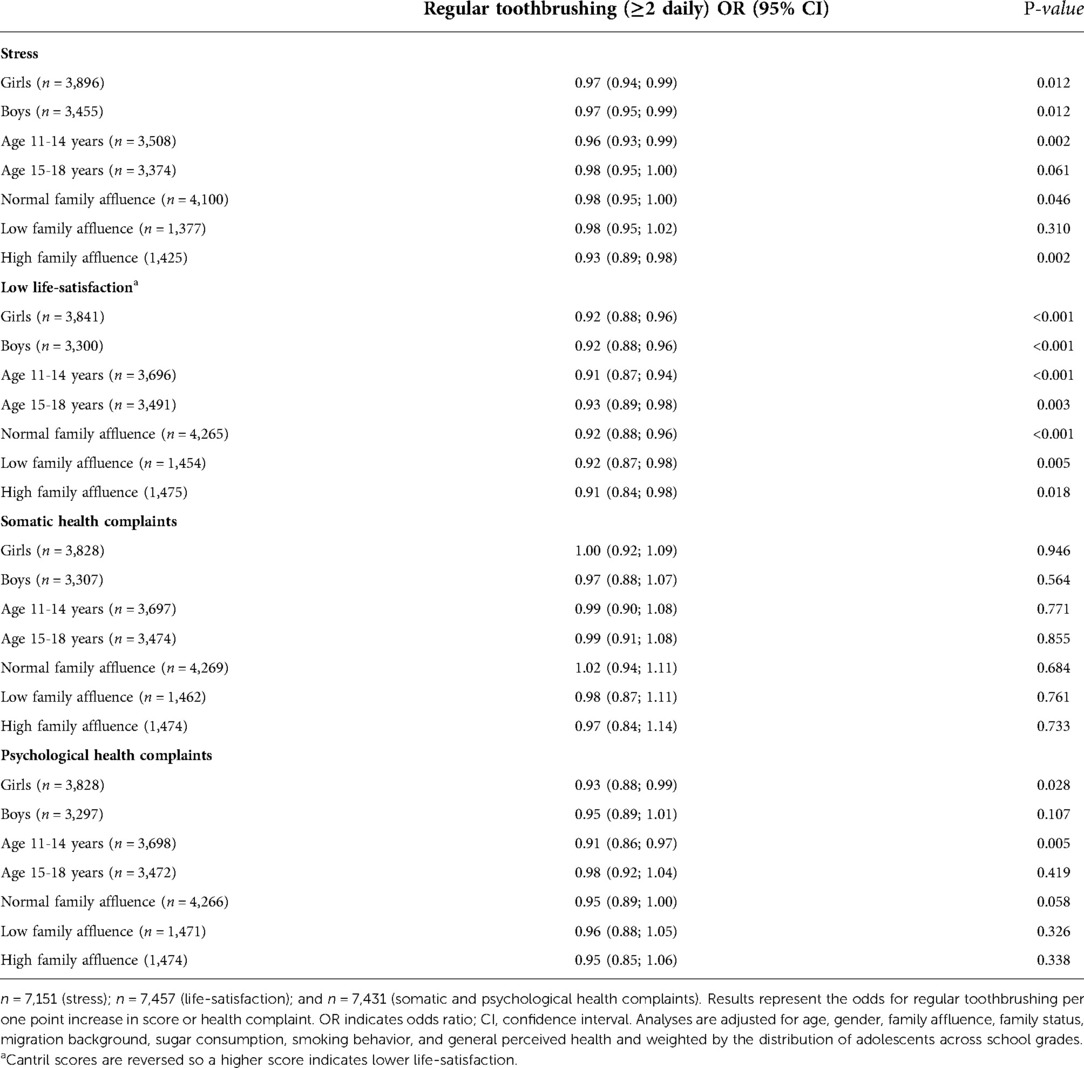
Several interactions of mental health and well-being with sociodemographic factors on regular toothbrushing were found. Table 3 shows the associations of stress, low life-satisfaction, and psychosomatic health complaints with regular toothbrushing stratified by sex, age, and family affluence. Stress, low life-satisfaction, and psychosomatic health complaints showed an interaction with age on regular toothbrushing (p-interaction = 0.023, p-interaction = 0.016, and p-interaction = 0.003, respectively). Stronger associations were observed in adolescents aged 11–14 years compared to adolescents aged 15–18 years (stress: OR = 0.96 [0.93;0.99], p = 0.002 vs. OR = 0.98 [0.95;1.00], p = 0.061; low life-satisfaction: OR = 0.91 [0.87;0.94], p < 0.001 vs. OR = 0.93 [0.89;0.98], p = 0.003; and psychological health complaints: 0.91 [0.86;0.97), p = 0.005 vs. OR = 0.98 [0.92;1.04], p = 0.419). Although the difference in the associations between the younger and older subgroups was marginal (<10%), the associations of stress and psychological health complaints with regular toothbrushing in the older age group became non-significant.
An interaction with high family affluence on regular toothbrushing was found for stress (p-interaction = 0.041). Slightly stronger associations were found in adolescents with a high family affluence (stress: OR = 0.93 [0.89;0.98], p = 0.002) compared to adolescents with a normal family affluence (stress: OR = 0.98 [0.95;1.00], p = 0.046, Table 3).
Other interactions of stress, low life-satisfaction, somatic health complaints, and psychological health complaints with gender, age, and family affluence on regular toothbrushing were non-significant.
Discussion
This study aimed to investigate whether adolescents' mental health and well-being is associated with regular toothbrushing in a high-income country. Adolescents who experienced higher levels of stress, lower levels of life-satisfaction, and more psychological health complaints were less likely to regularly brush their teeth. Somatic health complaints did not decrease the likelihood for regular toothbrushing. Differences in sociodemographic characteristics were observed, in which associations were more pronounced in younger adolescents compared to older adolescents. In addition, adolescents with high family affluence who experience higher stress levels were less likely to regularly brush their teeth than those with normal family affluence.
The current findings are in line with a previous Finnish study that found an association of social phobia and elevated anxiety levels with regular toothbrushing (19). Furthermore, our results are in line with a French study that observed an association of low life-satisfaction and with regular toothbrushing (20). Our results extend these findings by observing that the association of mental health and well-being is independent of important confounders like daily sugar consumption and smoking behavior. Furthermore, this study found that the association between mental health and oral health is already evident in subtle markers of poor mental health and well-being, i.e., subjective continuous measures of stress, life-satisfaction, and health complaints were used, instead of dichotomous markers of for example high or low depression. This underscores the importance of regular toothbrushing over the whole continuum of mental health and well-being.
More qualitative and longitudinal studies are needed to investigate the mechanisms underlying the association of poor mental health and well-being with irregular toothbrushing. One explanation for irregular toothbrushing is that adolescents with mental health problems have less motivation to regularly brush their teeth due to their mental state (32), i.e., adolescents with symptoms of apathy and stress might be less motivated to follow the recommendation for toothbrushing twice a day. There are also social factors that motivate toothbrushing. Clean teeth look attractive, create a feeling of freshness and strengthen one's self-confidence (33). A reduction in social contacts may reduce the motivation for regular toothbrushing. Aside from motivation, adolescents with a mental disease who receive pharmacological treatment have an increased risk for dental caries and oral diseases due to side-effect of their medication. A decrease or increase in salivation, taste problems, and abnormal involuntary movements have been related to dental caries and other oral diseases (34). Longitudinal research may provide more insights into the direction of the association between mental health and regular toothbrushing.
The prevalence and disease burden of highly preventable oral diseases demands for a radical change in the oral health systems and public health policies (7). The current treatment approach in high-income countries, that is characterized by technology, interventions, and specialism, does not deal with the underlying causes of oral diseases (3). Oral health care should not be a luxury and needs to be more integrated in other health care setting, particularly in primary care and mental health care settings. This demands action from academics, clinicians, dental health associations, governments, and international organizations as the FDI World Dental Federation and WHO, to promote oral health and place it back on the public health agenda. The World Health Assembly approved a Resolution on oral health in 2021 that proposes a change from the traditional curative approach towards a preventive approach that includes promotion of oral health behavior within the family, schools and workplaces, and includes timely, comprehensive and inclusive care within the primary care (2). The Resolution also declares the inclusion of oral health within the noncommunicable disease agenda and inclusion of oral health interventions in the universal health coverage programs (2). Promotion of regular toothbrushing is a major step in this. School oral health programs have shown to be effective in the improvement of oral health knowledge, status, and behavior, including frequency of toothbrushing (35). The government of the United Kingdom sets a good example by providing supervised toothbrushing programs in schools (36).
Other easy and inexpensive prevention approaches for oral diseases overlap with cardiovascular risk management, like a reduction in sugar, tobacco, and alcohol consumption. An introduction of sugar tax, restrictions on advertisements of sugary products, the reduction of sugar in existing products, and water fluoridation are recommended (7). Research has shown that adolescent demographics, mental health factors, and oral health behavior are interrelated. Therefore, promotion and intervention strategies should be developed using a multi-faceted approach (37). Clinicians in both primary care and mental health settings should include oral health behavior as part of a healthy lifestyle promotion and facilitate dental referrals if needed. Patients should be stimulated to brush their teeth regularly and clinicians should provide education about oral health behavior, like sugar consumption and smoking behavior. Clinicians should consider the side-effect of pharmacological treatment and advise patients to drink water regularly throughout the day and chew sugar-free chewing gum to reduce the side-effects of reduced salivation (34).
Strengths of this study include its large representative and random sample size, which make the results generalizable to the adolescent population in Luxembourg; the inclusion of both negative and positive mental health factors, which allows investigation into both negative and positive associations with regular toothbrushing; the adjustment of important behavioral confounders like sugar consumption and smoking behavior; the inclusion of interactions with sociodemographic factors, which consents research into sociodemographic differences; and the comparability of the 2018 data with future 2022 international data, which makes it possible to investigate cross-national changes due to Covid-19 with regards to mental health and oral health behavior.
The current study is limited by its cross-sectional design. Therefore, no conclusions can be drawn about causality. A previous study has observed an association between oral health symptoms and an increased risk of suicide-related factors (38). Although reversed causality cannot be ruled out, the poor oral hygiene in adolescents with poor mental health and well-being is relevant for both disciplines and demands for an integrated health care approach. Furthermore, data is based on self-reports. However, previous research has shown that self-reported toothbrushing frequency is a reliable proxy measure for clinical oral hygiene indices. Gil et al. (39) investigated the associations between oral hygiene measures and dental caries. Results of their study revealed that toothbrushing frequency was a better predictor for dental caries than the Simplified Oral Hygiene Index and the Plaque Index, two clinical measures for oral hygiene.
In conclusion, adolescents with poor mental health and well-being are less likely to brush their teeth regularly and may have an increased risk for oral diseases. Interventions focused on lifestyle modification in adolescents with mental health problems should include regular toothbrushing to prevent dental caries and other oral diseases.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary materials, further inquiries can be directed to the corresponding author/s.
Ethics statement
The studies involving human participants were reviewed and approved by Ethical approval was granted by the Comité National d’Ethique de Recherche (CNER, Avis N201711/02) and the Ethics Review Panel of the University of Luxembourg (ERP 17-059 HBSC 2018). Written informed consent from the participants’ legal guardian/next of kin was not required to participate in this study in accordance with the national legislation and the institutional requirements.
Author contributions
A.F.J.G: Contributed to conception and design, data analysis and interpretation, and drafted and critically revised the manuscript. A.H: Contributed to conception and design, data acquisition and interpretation, and critically revised the manuscript. All authors gave their final approval and agreed to be accountable for all aspects of the work. All authors contributed to the article and approved the submitted version.
Funding
The analysis of the data and open access publication were funded by the Université du Luxembourg; the Ministère de la Santé (Luxembourg) and the Ministère de l’Éducation nationale, de l’Enfance et de la Jeunesse (Luxembourg). The funders were not involved in the data analysis or interpretation, neither in the writing of this article nor the decision to submit the article for publication.
Acknowledgments
Health Behaviour in School-Aged Children (HBSC) is an international study carried out in collaboration with World Health Organization Regional Office for Europe. The International Coordinator of the 2017/2018 survey was Jo Inchley from the University of Glasgow, United Kingdom, and the Data Bank Manager was Oddrun Samdal from Bergen University, Norway. For details, see http://www.hbsc.org. The HBSC Luxembourg study was a collaboration between the University of Luxembourg, the Ministère de la Santé and the Ministère de l'Éducation nationale, de l'Enfance et de la Jeunesse. The authors would like to acknowledge the HBSC international research network, the HBSC Luxembourg team, the Ministère de la Santé and the Ministère de l'Éducation nationale, de l'Enfance et de la Jeunesse. The researchers are indebted to the participants and school staff for their willingness to participate in the study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Löe H. Oral hygiene in the prevention of caries and periodontal disease. Int Dent J. (2000) 50:129–39. doi: 10.1111/J.1875-595x.2000.Tb00553.X
2. World Health Organization. Oral Health (2022) Available at: https://www.who.int/news-room/fact-sheets/detail/oral-health [Cited 2022 Mar 24].
3. Watt R, Daly B, Allison P, Macpherson L, Venturelli R, Listl S, et al. Ending the neglect of global oral health: time for radical action. The Lancet. (2019) 394:261–72. doi: 10.1016/S0140-6736(19)31133-X
4. Hugo F, Kassebaum N, Marcenes W, Bernabé E. Role of dentistry in global health: challenges and research priorities. J Dent Res. (2021) 100:681–5. doi: 10.1177/0022034521992011
5. Petersen P, Bourgeois D, Ogawa H, Estupinan-Day S, Ndiaye C. The global burden of oral diseases and risks to oral health. Bull W H O. (2005) 83:661–9. PMID: 16211157; PMCID: PMC2626328
6. Global Burden Of Disease Collaborative Network. Global Burden Of Disease Study 2019 (Gbd 2019). Seattle (2020) [Cited 2022 Mar 24]. Available From: http://ghdx.healthdata.org/gbd-results-tool
7. The Lancet Child & Adolescent Health. Oral health: oft overlooked. The Lancet Child & Adolescent Health. (2019) 3:663. doi: 10.1016/S2352-4642(19)30275-5
8. Kassebaum N, Smith A, Bernabé E, Fleming T, Reynolds A, Vos T, et al. Global, regional, and national prevalence, incidence, and disability-adjusted life years for oral conditions for 195 countries, 1990-2015: a systematic analysis for the global burden of diseases, injuries, and risk factors. J Dent Res. (2017) 96:380–7. doi: 10.1177/0022034517693566
9. Frech A. Healthy behavior trajectories between adolescence and young adulthood. Adv Life Course Res. (2012) 17:59–68. doi: 10.1016/J.Alcr.2012.01.003
10. Kisely S, Sawyer E, Siskind D, Lalloo R. The oral health of people with anxiety and depressive disorders - A systematic review and meta-analysis. J Affect Disord. (2016) 200:119–32. doi: 10.1016/J.Jad.2016.04.040
11. Anttila S, Knuuttila M, Ylöstalo P, Joukamaa M. Symptoms of depression and anxiety in relation to dental health behavior and self-perceived dental treatment need. Eur J Oral Sci. (2006) 114:109–14. doi: 10.1111/J.1600-0722.2006.00334.X
12. Walsh T, Worthington H, Glenny A-M, Marinho V, Jeroncic A. Fluoride toothpastes of different concentrations for preventing dental caries. Cochrane Database Syst Rev. (2019) 3:Cd007868. doi: 10.1002/14651858.Cd007868.Pub3
13. Peltzer K, Pengpid S. Oral health behaviour and social and health factors in university students from 26 low, middle and high income countries. Ijerph. (2014) 11:12247–60. doi: 10.3390/Ijerph111212247
14. Folayan M, Arowolo O, Mapayi B, Chukwumah N, Alade M, Rh Y, et al. Associations between mental health problems and risky oral and sexual behaviour in adolescents in A sub-urban community in southwest Nigeria. Bmc Oral Health. (2021) 21:1–11. doi: 10.1186/S12903-021-01768-W
15. Folayan M, Tantawi M, Oginni O, Oziegbe E, Mapayi B, Arowolo O, et al. Oral health practices and oral hygiene Status as indicators of suicidal ideation among adolescents in southwest Nigeria. Plos One. (2021) 16:E0247073. doi: 10.1371/Journal.Pone.0247073
16. Ranasinghe S, Ramesh S, Jacobsen KH. Hygiene and mental health among middle school students in India and 11 other countries. J Infect Public Health. (2016) 9:429–35. doi: 10.1016/J.Jiph.2015.11.007
17. Pengpid S, Peltzer K. Hygiene behaviour and associated factors among in-school adolescents in nine african countries. Int J Behav Med. (2011) 18:150–9. doi: 10.1007/S12529-010-9109-6
18. Pengpid S, Peltzer K. Hand and oral hygiene practices among adolescents in Dominican republic, Suriname and Trinidad and Tobago: prevalence, health, risk behavior. Mental Health and Protective Factors. Ijerph. (2020) 17:7860. doi: 10.3390/Ijerph17217860
19. Pohjola V, Nurkkala M, Virtanen J. Psychological distress, oral health behaviour and related factors among adolescents: finnish school health promotion study. Bmc Oral Health. (2021) 21:6. doi: 10.1186/S12903-020-01357-3
20. Fernandez De Grado G, Ehlinger V, Godeau E, Arnaud C, Nabet C, Benkirane-Jessel N, et al. Changes in tooth brushing frequency and its associated factors from 2006 to 2014 among French adolescents: results from three repeated cross sectional hbsc studies. Plos One. (2021) 16:E0249129. doi: 10.1371/Journal.Pone.0249129
21. Heinz A, Kern M, Van Duin C, Catunda C, Willems H. Gesundheit Von schülerinnen und schülern in luxemburg-bericht zur luxemburgischen hbsc-befragung 2018. Esch-Sur-Alzette. (2020). http://hdl.handle.net/10993/46653 [Accessed September 20, 2022].
22. Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. (1983) 24(4):385–96. doi: 10.2307/2136404
24. Ka L, Currie C. Reliability and validity of an adapted version of the cantril ladder for use with adolescent samples. Soc Indic Res. (2014) 119:1047–63. doi: 10.1007/S11205-013-0507-4
25. Ravens-Sieberer U, Torsheim T, Hetland J, Vollebergh W, Cavallo F, Jericek H, et al. Subjective health, symptom load and quality of life of children and adolescents in Europe. Int J Public Health. (2009) 54:151–9. doi: 10.1007/s00038-009-5406-8
26. Haugland S, Wold B, Stevenson J, Aaroe L, Woynarowska B. Subjective health complaints in adolescence: a cross-national comparison of prevalence and dimensionality. Eur J Public Health. (2001) 11:4–10. doi: 10.1093/eurpub/11.1.4
27. Torsheim T, Cavallo F, Levin K, Schnohr C, Mazur J, Niclasen B, et al. Psychometric validation of the revised family affluence scale: a latent Variable approach. Child Ind Res. (2016) 9:771–84. doi: 10.1007/S12187-015-9339-X
28. Johnston L, Bachman JG, O'Malley PM. Drug use among American high school students, 1975–1977. National Institute on Drug Abuse. Division of Research (1977).
29. Hibell B, Andersson B, Ahlström S, Balakireva O, Bjarnason T, Kokkevi A, Morgan M. The 1999 ESPAD report: in alcohol and other drug use among students in 30. (2000). p. 1–383
30. Idler E, Benyamini Y. Self-Rated health and mortality: a review of twenty-seven community studies. J Health Soc Behav. (1997) 38(1):21–37. doi: 10.2307/2955359
31. Torsheim T, Nygren J, Rasmussen M, Arnarsson A, Bendtsen P, Schnohr C, et al. Social inequalities in self-rated health: a comparative cross-national study among 32,560 nordic adolescents. Scand J Public Health. (2018) 46:150–6. doi: 10.1177/1403494817734733
32. Choo A, Delac D, Messer L. Oral hygiene measures and promotion: review and considerations. Aust Dent J. (2001) 46:166–73. doi: 10.1111/J.1834-7819.2001.Tb00277.X
33. Koivusilta L, Honkala S, Honkala E, Rimpelä A. Toothbrushing as part of the adolescent lifestyle predicts education level. J Dent Res. (2003) 82:361–6. doi: 10.1177/154405910308200507
34. Cockburn N, Pradhan A, Taing M, Kisely S, Ford P. Oral health impacts of medications used to treat mental illness. J Affect Disord. (2017) 223:184–93. doi: 10.1016/J.Jad.2017.07.037
35. Geetha Priya P, Asokan S, Janani R, Kandaswamy D. Effectiveness of school dental health education on the oral health Status and knowledge of children: a systematic review. Indian J Dent Res. (2019) 30:437–49. doi: 10.4103/Ijdr.Ijdr_805_18
36. Public Health England. Improving Oral Health: A Toolkit To Support Commissioning Of Supervised Toothbrushing Programmes In Early Years And School Settings (2016) [Cited 2022 Apr 05]. Available From: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/574835/phe_supervised_toothbrushing_toolkit.pdf
37. Chun J-Y, Lee K-H. The correlation between oral health factors and mental health factors in Korean adolescents. J Korean Soc Dent Hyg. (2017) 17:669–80. doi: 10.13065/Jksdh.2017.17.04.669
38. Lee K-H, Lee W-K, Jung E-S, Choi Y-Y. Associations between mental health and oral health among Korean adolescents: analysis of the national surveys (2008–2017). Ijerph. (2021) 18:10660. doi: 10.3390/ijerph182010660
39. Gil G, Morikava F, Santin G, Pintarelli T, Fraiz F, Ferreira F. Reliability of self-reported toothbrushing frequency as an indicator for the assessment of oral hygiene in epidemiological research on caries in adolescents: a cross-sectional study. BMC Med Res Methodol. (2015) 15:14. doi: 10.1186/S12874-015-0002-5
Keywords: oral health & hygiene, toothbrushing, epidemiology, mental health, adolescence, health promotion
Citation: Geraets AFJ and Heinz A (2022) The association between adolescent mental health and oral health behavior: The Luxembourg Health Behavior in School-Aged Children study. Front. Dent. Med 3:979192. doi: 10.3389/fdmed.2022.979192
Received: 27 June 2022; Accepted: 23 September 2022;
Published: 12 October 2022.
Edited by:
Helen Weiss, University of London, United KingdomReviewed by:
Shailesh Lele, Consultant, Academic Development & Quality Assurance, IndiaJuliana Balbinot Hilgert, Federal University of Rio Grande do Sul, Brazil
© 2022 Geraets and Heinz. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Anouk Francine Jacqueline Geraets, YW5vdWsuZ2VyYWV0c0B1bmkubHU=
Specialty Section: This article was submitted to Pediatric Dentistry, a section of the journal Frontiers in Dental Medicine
 Anouk Francine Jacqueline Geraets
Anouk Francine Jacqueline Geraets Andreas Heinz
Andreas Heinz