- 1Psychiatric and Neurodevelopmental Genetics Unit, Center for Genomic Medicine, Massachusetts General Hospital, Boston, MA, United States
- 2Department of Psychiatry, Harvard Medical School and the Massachusetts General Hospital, Boston, MA, United States
- 3Henry and Allison McCance Center for Brain Health, Massachusetts General Hospital, Boston, MA, United States
- 4Department of Oral and Craniofacial Sciences, University of California, San Francisco, San Francisco, CA, United States
- 5Mathematics and Statistics Research Group, University of the West of England, Bristol, United Kingdom
- 6Department of Psychiatry and Behavioral Sciences, University of California, San Francisco, San Francisco, CA, United States
- 7Forsyth Institute, Cambridge, MA, United States
- 8Department of Developmental Biology, Harvard School of Dental Medicine, Boston, MA, United States
- 9Department of Pediatrics, University of California, San Francisco, San Francisco, CA, United States
Mental disorders are among the most disabling health conditions globally. However, there remains a lack of valid, reliable, noninvasive, and inexpensive biomarkers to identify (at an early age) people who are at the greatest risk of experiencing a future mental health condition. Exfoliated primary teeth, when used in combination with established and emerging tools (e.g., family history, imaging, genetics, epigenetics), may provide important additional insights about vulnerability to mental illness. Teeth are especially promising because they develop in parallel with the brain and maintain a permanent record of environmental insults occurring during prenatal and perinatal development. Despite their potential, few empirical studies have investigated features of exfoliated teeth in relation to mental health. Here, we used micro-CT imaging to test the hypothesis that measures derived from exfoliated primary incisors associated with psychopathology symptoms in a community-based sample of children (n = 37). We found that enamel volume (β = −0.77, 95% CI, −1.35 to −0.18, P = 0.01) had large negative associations with internalizing symptoms, and enamel mineral density (β = 0.77, 95% CI, 0.18–1.35, P = 0.01) had large positive associations with internalizing behavioral symptoms, even after stringent control for multiple testing. Pulp volume (β = −0.50, 95% CI, −0.90 to −0.09, P = 0.02) had a moderately-large negative association with externalizing behavioral symptoms, though these associations did not survive multiple testing correction. These results support the ongoing investigation of teeth as potential novel biomarkers of mental health risk.
Introduction
Mental disorders constitute ~13% of the global burden of disease and are one of the most disabling groups of health conditions worldwide (1, 2). Mental disorders often begin early in life; in 50% of people with a mental disorder, the condition was diagnosed by early adolescence (3). In children, mental health problems are often classified into two symptom clusters (4): internalizing symptoms, meaning emotional and behavior problems that are inwardly-directed, such as depression or anxiety and externalizing symptoms, meaning emotional and behavior problems that are outwardly-directed, such as conduct problems or attention deficit hyperactivity difficulties (5, 6). High levels of internalizing and externalizing symptoms in childhood, in turn, have been found to predict a variety of poor outcomes in adulthood, including a 2- to 6-fold increase in risk for adult psychiatric diagnoses (7), as well as increased risk for academic failure (8), substance abuse problems (9), and even suicidality (10). Such poor outcomes may be attributable, in part, to the fact that people with early-onset psychopathology symptoms often delay seeking care, by as much as a decade, at which point symptoms have progressed and become more severe (11–13). Together, these findings emphasize the importance of identifying youth who may be at high future risk of psychopathology so they can be directed to early interventions, which have been shown to be effective in reducing psychopathology symptoms [see reviews by (14, 15)].
Recent advances in biomarker science are starting to identify new objective tools, such as neuroimaging, genetic, and epigenetic markers, which show promise in being able to one day help guide population-based risk stratification efforts and possibly even identify individual youth at-risk. Neuroimaging studies, for example, have identified associations between structural and functional markers (e.g., cortical thinning, decreased amygdala activity) and poor psychiatric outcomes in children (16–19). Genome-wide association studies (GWAS) have led to the creation of disease-specific and cross-disorder polygenic risk scores, which themselves have been associated in the population with up to about 5% of the variability in risk for psychopathology symptoms or neurodevelopmental phenotypes (20–22). Relative to self-reports of family history or children's current psychopathology symptoms, biomarkers have a number of advantages. For instance, they are objective (rather than subjective) indicators and therefore might be more precise in characterizing population-level risk. Moreover, they could provide more precise information about underlying biological mechanisms shaping disease risk than broader self-report tools. Yet many biomarkers are currently limited due to their invasive nature and costly implementation on a population scale. New noninvasive and cost-effective biomarkers are therefore needed. With a broader suite of available tools, both researchers and clinicians would have more information (beyond family histories and symptom or diagnostic measures) to identify children who may benefit from early intervention.
Recently, we outlined a conceptual model—Teeth Encoding Experiences and Transforming Health (TEETH)—wherein we proposed that exfoliated primary teeth (also referred to as baby, deciduous, or milk teeth) could provide a new tool to guide primary prevention efforts in the fields of pediatrics as well as child and adolescent mental health (23). Our conceptual model was grounded in the observation that primary teeth develop on a parallel timeline with the brain and preserve a permanent record of prenatal and perinatal insults (23–25), which are potent risk factors for mental illness, per the prenatal programming hypothesis (26–28). Thus, we argued that inexpensive and non-invasive markers derived from exfoliated primary teeth—when used alongside existing tools—might serve as an additional early-warning sign for vulnerability to future psychopathology. If true, such insights could facilitate efforts to direct children who are vulnerable toward targeted interventions at the time when teeth are initially exfoliated, starting around age 6, which is years before the typical onset of many early life psychiatric disorders. Directing exfoliated teeth for such purposes therefore provides a possible alternative relative to throwing teeth away or storing them, as most parents often do (29).
By our review of the literature, several dozen studies have explored the properties of teeth as indicators of mental health risk, in a mixture of clinical, community-based, and population-based samples of youth (see Table 1). The overwhelming majority of research on teeth and mental health has investigated the associations of early life toxicants measured in primary teeth and risk for autism (30–36, 46) in particular, as well as internalizing and externalizing problems (40, 41), ADHD (37), schizophrenia (42, 43), and neurodegenerative disorders (38, 39) [see reviews by (47, 48)]. The most recent generation of these toxicant teeth studies, which date back to the early 2010s, use mass-spectrometry technology paired with laser ablation. This methodology, which requires sectioning the teeth to expose tooth structures, has identified time-specific windows in development when uptake of heavy metals (e.g., lead, manganese, etc.) differentiated cases with psychiatric disease from controls without disease. For example, in one of the largest and most robust studies, Mora and colleagues (40) found in a study of exfoliated primary teeth from 248 school-aged children that higher pre- and post-natal levels of magnesium in dentin were associated with worse internalizing and externalizing symptoms in young children, but improved cognitive abilities in young boys.
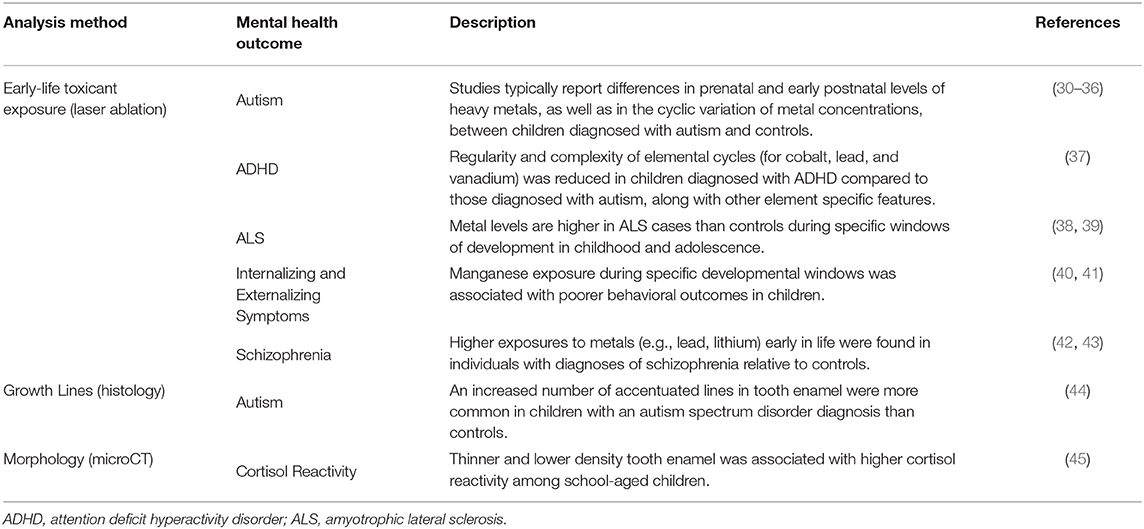
Table 1. Examples of empirical research reporting associations between properties of teeth and mental health outcomes.
Outside of research on toxicants, a smaller body of research on teeth and mental health risk also exists, revealing connections between other aspects of primary teeth and psychopathology risk. For instance, adopting an approach focusing on the histology of the tooth (meaning, its structure) rather than its chemical composition, Kurek and colleagues (44) investigated how the presence of tooth growth lines, which are similar to the rings in a tree marking its age, associated with risk for autism in a sample of boys. The authors found that boys with autism were more likely than their peers without autism to have a greater number of a certain type of growth line, called accentuated growth marks or stress lines, which indicate some type of stressor occurred during enamel formation. Similarly, Boyce et al. (45) found markers of reactivity in the stress hormone cortisol associated with reduced average thickness and less mineralized enamel in a community-based sample of youth. Notably, sample sizes of studies examining toxicants or other features of teeth in relation to mental health studies are small by the standards of clinical or epidemiological studies (varying from n of 12 to 248); however, these sample sizes are considered typical in size for anthropological work. Though limited in total number, this collection of observational studies collectively suggest opportunities to bridge the fields of pediatric dentistry with child and adolescent psychiatry.
In the current study, we empirically tested the tooth-to-mental health risk part of our conceptual model (23) by analyzing data from a community-based study of kindergarten-aged youth. We used nondestructive micro-CT imaging to investigate the extent to which children's exfoliated primary teeth associated with levels of child internalizing and externalizing symptoms. In this report, we provide the first evidence that basic morphological properties of children's exfoliated primary teeth may serve as indicators of vulnerability to child psychopathology.
Methods
Participants
We analyzed exfoliated primary mandibular central incisors from 37 kindergarten-aged children (20 boys; 17 girls; ranging in age from 5.9 to 6.8 years) enrolled in the Peers and Wellness Study (PAWS), a longitudinal school-based study of children attending public school in the California Bay Area (49, 50). The original PAWS study (n = 338) was designed to investigate the role of social dominance status, family environment, and biological responses to adversity on child physical and mental health. In 2004-2006, a dental tissue sub-study was launched, which recruited a subsample of PAWS children during their first grade year who had lost a tooth during the 9 months of the academic year, and donated at least one tooth to the study. All children donated incisors, which are typically the first primary teeth to exfoliate and begin forming during the second trimester of prenatal life and reach full maturation by the end of the first year of life. Incisors are comprised of three dental compartments: enamel (the white outermost part of the tooth), dentin (the layer below enamel), and pulp (the center part of a tooth consisting of connective tissue, blood vessels, and cells). Each child donated one or more incisors. However, only one tooth per child was included in this analysis (teeth were selected for analysis randomly). The teeth were free of dental cavities or developmental dental anomalies.
Measures
Tooth Measures
Using micro-CT and Amira 6.5 analysis software (Thermo Fisher Scientific), we derived six measures from each incisor: (1) tooth size (micrometers; mm2), (2) enamel volume (mm3), (3) enamel density (Hounsfield units; HU), (4) dentin density (HU), (5) pulp volume (mm3), and (6) pulp shape (mm).
After micro-CT scanning, images were uploaded into Amira and all teeth were spatially aligned against a reference tooth, using a Euclidean metric algorithm, allowing for consistent comparison between samples. A 3D Gaussian filter was applied to define the boundaries between the dental compartments (i.e., enamel, dentin, pulp). In the segmentation editor, the tooth root was cropped along the cementoenamel junction (CEJ) and analysis was performed on the tooth crown. Each dental compartment was assigned by relative density and compartment edges were refined with single voxel erosion and smoothing to clearly define each dental compartment (Figure 1A).
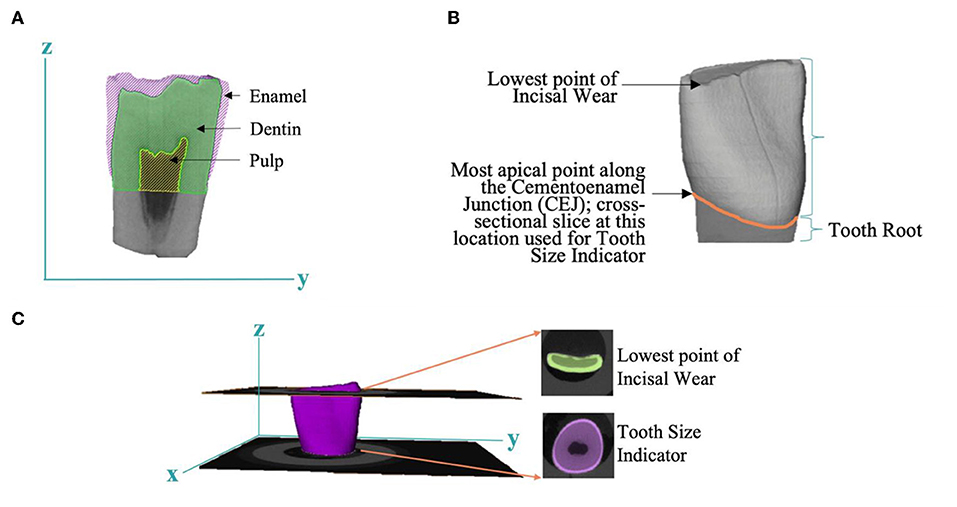
Figure 1. Tooth-based measures derived by micro-CT. (A) A 2D image highlighting the anatomy of the dental compartments: enamel, dentin, and pulp. (B) Estimation of tooth size based on most apical point along the cementoenamel junction (CEJ). (C) Evaluation of bruxing factor, or tooth wear, derived from lowest point of incisal wear and tooth size indicator.
Enamel and pulp volume were measured by simple voxel counting within the enamel and pulp compartment, respectively. Relative density of enamel and dentin were assessed by averaging voxel intensity in each separate dental tissue. Pulp shape was calculated by a 3D sphere filling method which averages the diameters of the largest spheres that fit within the boundaries of the pulp chamber.
We observed loss of incisal tooth structure on 98% of the sampled teeth. This loss was likely associated with bruxing, or grinding, and is a common feature of pediatric dentition. The varying amounts of incisal wear did not allow for the direct use of total volume as the most accurate measure of tooth size. Therefore, we used the cross sectional area of the dentin and pulp at the most apical point of the cervical margin of the crown as a relative measure of tooth size (Figure 1B). Enamel, pulp volume, and pulp shape measures were normalized by tooth size. An index of bruxing (bruxing factor) was measured by taking the cross-sectional area of a slice through the lowest point of occlusal wear on each tooth and dividing this by tooth size (Figure 1C).
Internalizing and Externalizing Symptom Measures
Psychopathology symptoms were assessed with the parent- and teacher-reported MacArthur Health and Behavior Questionnaire (51) and children's self-report on the Berkeley Puppet Interview (52). Both of these measures are commonly-used, have excellent psychometric properties, and were designed specifically for children ages 4–8 years. Due to the benefits offered by multiple informants when evaluating children's psychological symptoms, we used procedures outlined by Kraemer et al. (53) to conduct principal component analysis of potentially orthogonal reports from parents, teachers, and children and derive two multi-reporter indices of children's internalizing and externalizing symptoms. The first component that was extracted reflected a trait dimension (individual differences in children's internalizing or externalizing emotional and behavioral symptoms). This approach has been extensively used in prior studies (49, 54–56), including studies using both survey instruments (49).
Covariates
We also analyzed data on the following social-demographic factors, which as described below were considered as possible covariates in our regression models: (1) child sex (coded as male vs. female), (2) child racial/ethnic background (coded as White vs. Other Race/Ethnicity); (3) family socioeconomic status; (4) children's body mass index (kg/m2 evaluated at age 9), and (5) tooth wear (due to bruxing or chewing). Family socioeconomic status was measured as the standardized average (ranging from −3.13–1.64 in the total sample) of parental education and family income (57). Parental education was measured in 8 categories, from 1 = some grade school, to 8 = graduate or professional degree. Family income was measured in 15 categories (as a continuous variable), from 1 = < $10,000, to 15 = $400,000–499,999.
Data Analysis
We first performed univariate analyses to understand the distribution of each study variable and then performed bivariate analyses to understand the pair-wise associations between each variable. We then evaluated associations between the six tooth-based measures and two psychopathology outcomes (internalizing and externalizing symptoms) using multiple regression performed in R 4.0.0. Multiple regression was preferable to univariate regression, because preliminary analysis confirmed the six tooth-based measures were reasonably correlated (see details below); thus, a given marker should be examined after controlling for the other markers. Covariates were selected for inclusion in regression models based on their having an association with at least one outcome, as we report below.
We included all tooth measures and selected covariates in each model; thus, each beta coefficient captures the estimated effect of that variable after controlling for the other teeth measures and covariates. To aid in interpretation and assist in the future reproducibility of our study results, we present results from both unstandardized and standardized regression models. Unstandardized regression models refer to analyses performed with the raw variables. Standardized regression models refer to analyses performed on standardized variables calculated by subtracting the variable mean and dividing by the standard deviation.
Partial R2 (meaning the amount of variability explained by the predictors above that explained by the covariates) are also presented and were adjusted for the number of predictors in model.
To ensure study rigor, we used 2-sided P (< 0.05) to define statistical significance and implemented false discovery rate corrections (FDR) to adjust for multiple comparisons. We calculated variance inflation factors to assess whether our regression models were affected by multicollinearity.
Results
Sample Descriptives
In the PAWS analytic sample of n = 37, 62.2% of children were White. The analytic sample also varied with respect to socioeconomic status (derived SES measure median = 0.4; SD: 0.8; min= −2.05; max = 1.1). Compared to children in the total PAWS sample, children in our analytic sample were more likely to be White (41% White in the total PAWS sample), and of higher SES (mean SES score = −0.01; SD: 0.88; min = −3.13; max = 1.64 in total PAWS sample) (57).
There was considerable variability in each of the tooth markers: (1) tooth size (mean = 9.42 mm2; SD = 1.33; min = 7.18; max = 13.39); (2) enamel volume (mean = 4.39 mm3; SD = 0.87; min = 2.42; max = 7.21); (3) enamel density (mean = 13,556 HU; SD=377.5; min = 12,704; max = 14,148); (4) dentin density (mean = 8,207 HU; SD = 192.9; min = 7,755; max = 8,577); (5) pulp volume (mean = 1.19 mm3; SD = 0.54; min = 0.28; max = 3.04); and (6) pulp shape (mean-0.66; SD = 0.26; min = 0.02; max = 0.98). Internalizing (mean = −0.21; SD = 0.86; min = −1.72; max = 1.61) and externalizing symptoms scores were also variable (mean = −0.17; SD = 0.73; min = −1.23; max = 1.22).
Bivariate Associations Between All Study Variables
Table 2 presents the pair-wise correlation between the six tooth markers, the five possible socio-demographic covariates, and the two psychopathology outcome measures. As shown there, no tooth measure individually showed an association with either psychopathology measure. However, the significant correlations between the tooth measures mean it is inappropriate to consider univariate regression with single tooth measures. Hence, we proceeded to conduct multiple regression. Because socioeconomic status and racial/ethnic background were associated with internalizing symptoms, we included both of these variables as covariates in our multiple regression analyses.
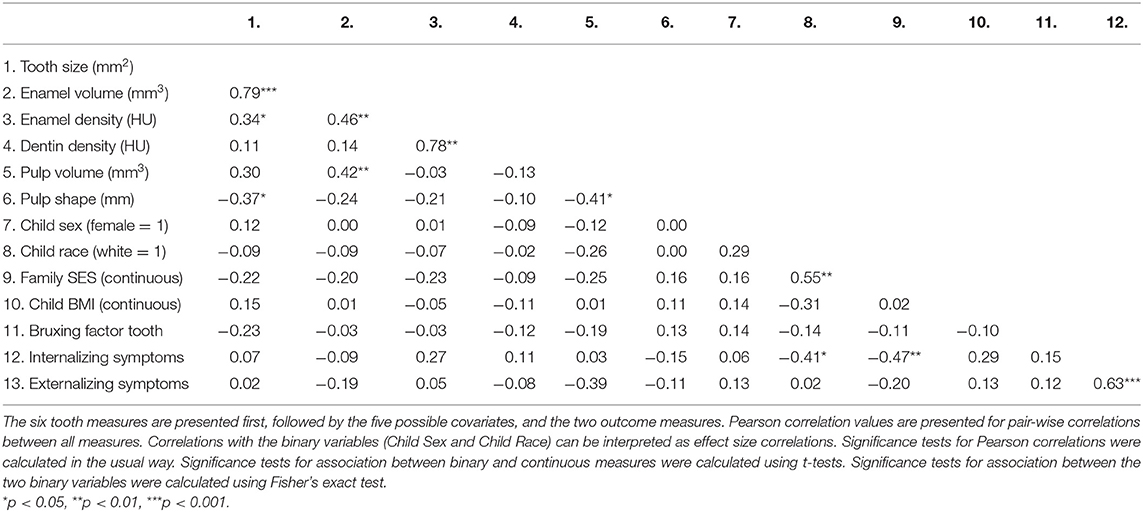
Table 2. Correlations between the six tooth measures, the five possible covariates, and the two outcomes (n = 37).
Multiple Regression Results
As shown in Table 3, several noteworthy findings emerged from our multiple regression analysis. First, enamel volume was negatively associated with internalizing symptoms, after adjusting for other predictors and sociodemographic covariates (standardized β = −0.77, 95% CI, −1.35 to −0.18, P = 0.01). The standardized regression coefficient suggested that internalizing symptoms decreased, on average, by 0.77 standard deviations per 1 standard deviation increase (equivalent to 0.87 mm3) in enamel volume, if all other predictors and covariates remain fixed.
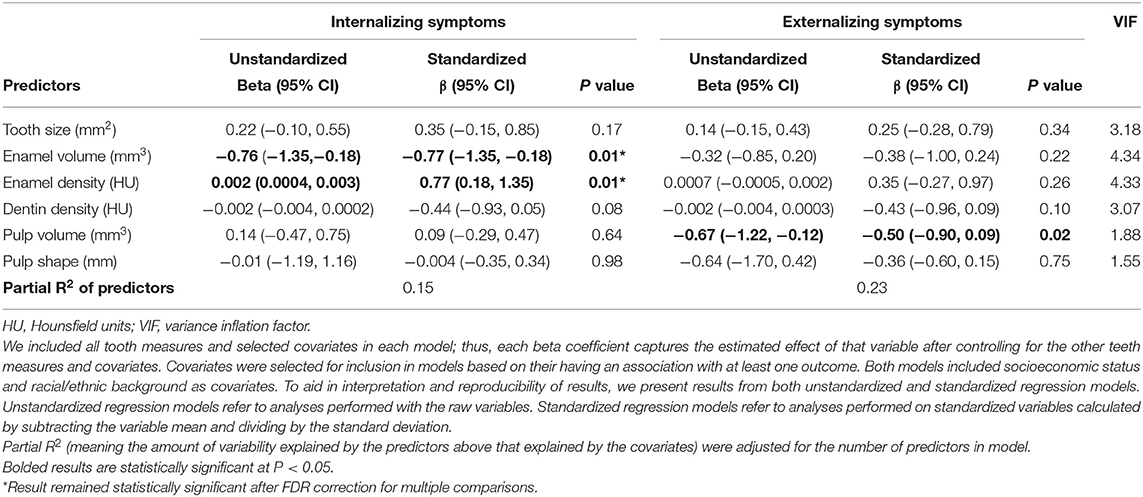
Table 3. Results of multiple linear regression analyses examining the association between tooth measures and levels of internalizing and externalizing symptoms, adjusted for socioeconomic status, race/ethnicity, and other tooth-based measures (n = 37).
Second, enamel density had a positive association with internalizing symptoms (standardized β = 0.77, 95% CI, 0.18–1.35, P = 0.01), suggesting internalizing symptoms increased, on average, by 0.77 standard deviations units per 1 standard deviation increase (equivalent to 378HU) in enamel density.
Of note, both of these standardized regression coefficients indicate a medium-sized effect (adjusted partial correlation = ± 0.42 for both, Cohens f2 = 0.21 for both). Moreover, both of these results were statistically significant, even after FDR correction for multiple testing.
Third, pulp volume had a negative association with externalizing symptoms (standardized β = −0.50, 95% CI, −0.90 to −0.09, P = 0.02) that would be considered a medium-sized effect (adjusted partial correlation = −0.39, Cohens f2 = 0.18). However, this association was not statistically significant after correction for multiple testing.
Collectively, these six tooth markers explained a further 15% and 20% of the variation in internalizing and externalizing symptoms, respectively, above that already explained by socioeconomic status and racial/ethnic background, two of the strongest predictors of child psychopathology (58). These findings were also detected after correcting for tooth size, thus were not explained by bruxing.
The largest variance inflation factor was 4.34, indicating multicollinearity was of minimal concern. We confirmed our regression models did not violate multiple regression assumptions, including the linearity assumption, by checking basic and partial scatterplots, and residual plots.
Discussion
The main conclusion of this study is that micro-CT-based measures from exfoliated primary teeth may provide new insights about child psychopathology symptoms, consistent with our TEETH conceptual model (23). Our results demonstrate for the first time that easily derived macro-level measures from children's exfoliated primary teeth may provide new clues to help characterize children's mental health risk. We showed that primary enamel volume was negatively associated with children's internalizing symptoms, while enamel density was positively associated with internalizing symptoms. Furthermore, primary pulp volume was negatively associated with children's externalizing symptoms.
Findings from the current study add to the existing literature by focusing on morphological properties in relation to child internalizing and externalizing symptoms. By our review of the literature, our study is the first of its kind. The current study is also an advancement of prior work, given our focus on investigating micro-CT-based macro-level measures of tooth features. Prior studies have primarily used other techniques to derive exposure data from teeth, including mass-spectrometry technology paired with laser ablation (33) or light microscopy (44). A major advantage of micro-CT measures is that they can be derived without destroying the tooth. Thus, micro-CT-based data has more potential to be incorporated into research, because it will allow for other future analyses of the collected teeth. Moreover, deriving data from micro-CT may be more cost-effective than other approaches. Although costs for lab procedures are variable and can change over time, depending on the research environment and its set-up (e.g., labs could have microCT covered as part of start-up; there are differences in core facility pricing based on internal versus external pricing for equipment time and the resolution of the scan), a “going rate” for the micro-CT we used is currently at about $100 per tooth.
What could explain our findings regarding the negative association between enamel volume and internalizing symptoms, and the positive association between enamel density and internalizing symptoms? We hypothesize these findings may reflect several biological processes in development. Primary tooth enamel is formed in stages, beginning during the second trimester of prenatal life and ending during the first year of postnatal life for incisors (59, 60). The full thickness of the enamel matrix is first laid down in the secretory stage, and then the matrix mineralizes to reach its full density in the maturation stage (61, 62). The rate of enamel matrix apposition is associated with the circadian rhythm (63); thus, the association between reduced enamel volume and internalizing symptoms suggests either an earlier end to the secretory stage or possibly circadian rhythm-related effects. The association between increased enamel density and internalizing symptoms indicates changes in either the onset and duration of maturation, or other mechanisms that affect how much mineral is formed and how much the enamel crystals grow during the maturation process. Because mandibular primary incisors are formed primarily in utero (64), these findings therefore reflect some type of aberrations occurring during prenatal development.
Should this work be replicated in future studies, these findings have potential important implications for both timely intervention and increasing our understanding of the etiology of psychopathology. For example, depressive and anxiety problems generally arise by 7 years of age in 1.1 and 8.5% of children, respectively (65). Children begin losing their first teeth by around age 6. Thus, if validated as a biomarker, primary teeth could potentially be used to identify high risk children, before the first signs of psychopathology symptoms are likely to emerge. These macro-level measures derived from microCT imaging of the exfoliated tooth may also one day be applicable to less precise but more accessible forms of tooth-based measurement, such as X-rays, which are routinely performed by dental professionals during pediatric primary care visits. Further, as primary teeth develop in an incremental manner during sensitive periods of development, they may preserve an important record of insults and their timing that could shed light on the causes of psychopathology symptoms (23).
There were several strengths of this study. For one, our measure of psychopathology symptoms came from a composite of scores from multiple reporters. Prior studies have shown multiple reporters often provide more information about child psychopathology symptoms than a single reporter alone (66). Second, we assess tooth morphology using non-destructive means. The possibility to acquire information about psychopathology risk from intact teeth might enable more parents to donate teeth to science (because the tooth could be returned to the parent, if desired, to hold as a keepsake). Moreover, intact teeth can also be further interrogated for other analyses in the future, though radiation through microCT must be noted. Third, our study was able to correct for tooth size, ensuring that our results were not explained by between-child differences in the size of dentition. Finally, we were rigorous in our analysis: we controlled for potential covariates, tested for regression model assumptions, evaluated the possibility of multicollinearity, and adjusted for multiple testing.
This study had several limitations. First, children in this study were identified in first grade, thus we lacked information about children's prenatal and perinatal life. If available, such data could have enabled us to evaluate the extent to which tooth abnormalities reflected the biological imprints of maternal pregnancy (e.g., social support; maternal history of psychopathology; stressors) or child factors during prenatal or early development (e.g., gestational age; exposure to medications or exposure to toxicants) (67). Indeed, we recently showed in a population-based sample of 70 youth that maternal depression and perceptions of social support were associated with the thickness of the neonatal line, a prominent growth marker in exfoliated teeth thought to be indicative of stressful birth conditions (67). Caution is therefore warranted in interpreting these results, as our findings would be biased away from the null if early life factors shaped both tooth formation and child psychopathology. Second, we did not have information on the potential biological mechanisms linking tooth measures with child psychiatric symptoms. Although establishing an initial association between two factors is a key first step, future studies are needed to both replicate these associations and further unravel what biological mechanisms in development could be explaining those associations. Third, our study was limited in sample size, but comparable to prior work exploring the relationship between tooth-markers and mental health (42). Our study was also comprised of mostly European-ancestry children and thus was not representative of more racially/ethnically diverse groups of youth, limiting the generalizability of these findings. Finally, data were originally collected more than two decades ago from a sample of children who were not followed longitudinally to adolescence. Funding for the study concluded and data collection did not continue beyond first grade. Thus, we lack any information on specific psychiatric diagnoses children may have developed later in life. However, early in life, children often move dynamically in and out of diagnostic classifications of mental disorders (68) and intermediate behavioral risk factors are important and robust predictors of psychopathology in adulthood. In fact, a recent systematic review concluded that elevated symptomatology in childhood was more strongly associated with adult mental health disorders than childhood diagnoses (69).
Exfoliated primary teeth hold great appeal as potential biomarkers. Exfoliated primary teeth can be collected easily, as nearly every child globally exfoliates primary teeth. Exfoliated teeth can also provide nuanced data on the occurrence and timing of otherwise hard to measure retrospective events. The early age of natural tooth shedding also means insights gained from exfoliated teeth could help guide risk-stratification and/or prevention efforts for youth at-risk (23). However, as we have reported (29), teeth are different from other biospecimens: they are finite; parents view tooth exfoliation as a developmental milestone bearing nostalgic value, and parents practice a variety of rituals with their children once their teeth are exfoliated. These and other factors may determine if parents donate their children's teeth to science, and if so which and how many teeth they donate.
As with any emerging biomarker, high standards for scientific rigor are needed when conducting and reporting research on teeth. Such scientific rigor should exist across all stages of the research process, including unbiased study designs, data analysis, as well as the interpretation and reporting of results. Through such rigor, we can help ensure findings are reproducible and in what populations and contexts such findings are validated. Further, as research on primary teeth also progresses, researchers can incorporate the valuable lessons learned from other biomarkers to avoid the pitfalls that prior work encountered, including the importance of extending studies to more diverse samples, and help determine the extent to which markers from teeth provide distinct or similar information to other measures.
We hope the results of the current study will encourage researchers to test our TEETH conceptual model more fully and characterize potential links in this “tooth-brain-axis,” including the impact of early life stress on tooth formation. Replication and validation of these findings are needed, which can help determine the usefulness of teeth as indicators of mental health risk. Through such work, teeth could one day be used as an additional tool—alongside information on family history and other biomarkers—to identify children at high-risk for future mental disorders.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by University of California San Francisco. Written informed consent to participate in this study was provided by the participants' legal guardian/next of kin.
Author Contributions
ECD, PD, and WTB conceived of the study. RVM, KAD, and ADACS conducted the statistical analysis. RVM and KAD wrote early drafts of the manuscript. ECD and RVM wrote later drafts of the manuscript. IS and PD oversaw the derivation of microCT data. DSR and WTB provided data on the PAWS study. FBB helped interpret results from the analysis. All authors reviewed and edited the manuscript. All authors contributed to the article and approved the submitted version.
Funding
The PAWS study was supported by Grant R01 MH62320 from the National Institute of Mental Health (to WTB and Nancy Adler, Co-Principal Investigators), the MacArthur Foundation Research Network on Psychopathology and Development, and the Canadian Institute for Advanced Research (CIFAR). Support for this manuscript was provided by the Bezos Foundation to Dr. Takao Hensch (PI; Co-Investigator: ECD). ECD also received funding under an administrative supplement from the National Institute of Mental Health of the National Institutes of Health under Award Number R01MH113930. Tooth analyses were supported by a T32DE007306 grant from the National Institute of Dental and Craniofacial Research (NIDCR) to PD, and a F30 DE029399 from NIDCR to IS. FBB acknowledges funding from NIDCR through 1 R01-DE025865-01A1.
Author Disclaimer
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
The authors thank the school principals, teachers, children, and families who participated in the PAWS study and the numerous research assistants who collected and scored these data. The authors also thank Ms. Yiwen Zhu for her early input on statistical analysis, Ms. Susan T. Landry for her assistance in copyediting this manuscript, and Dr. Takao Hensch for helpful early discussions about the study design.
References
1. Collins PY, Patel V, Joestl SS, March D, Insel TR, Daar AS, et al. the Executive Committee of the Grand Challenges on Global Mental H, Anderson W, Dhansay MA, Phillips A, Shurin S, Walport M, Ewart W, et al. Grand challenges in global mental health. Nature. (2011) 475:27–30. doi: 10.1038/475027a
2. World Health Organization. Depression and Other Common Mental Disorders: Global Health Estimates. (World Health Organization, Geneva, 2017).
3. Kim-Cohen J, Caspi A, Moffitt T, Harrington H, Milne B, Poulton R. Prior juvenile diagnoses in adults with mental disorder: Developmental follow-back of a prospective-longitudinal cohort. Arch Gen Psychiatry. (2003) 60:709–17. doi: 10.1001/archpsyc.60.7.709
4. Kotov R, Krueger RF, Watson D, Achenbach TM, Althoff RR, Bagby RM, et al. The Hierarchical Taxonomy of Psychopathology (HiTOP): A dimensional alternative to traditional nosologies. J Abnorm Psychol. (2017) 126:454–77. doi: 10.1037/abn0000258
5. Cicchetti D, Toth SL. A developmental perspective on internalizing and externalizing disorders. In: Cicchetti D, Toth SL, editors. Rochester Symposium on Developmental Psychopathology, Vol. 2. Hillside, NJ: Erlbaum (1991). p. 1–19.
6. Cohen NJ, Gotlieb H, Kershner J, Wehrspann W. Concurrent validity of the internalizing and externalizing profile patterns of the Achenbach Child Behavior Checklist. J Consult Clin Psychol. (1985) 53:724. doi: 10.1037/0022-006X.53.5.724
7. Hofstra MB, Van Der Ende J, Verhulst FC. Child and Adolescent Problems Predict DSM-IV Disorders in Adulthood: A 14-Year Follow-up of a Dutch Epidemiological Sample. J Am Acad Child Adolesc Psychiatry. (2002) 41:182–9. doi: 10.1097/00004583-200202000-00012
8. Masten AS, Roisman GI, Long JD, Burt KB, Obradovic J, Riley JR, et al. Developmental Cascades: Linking Academic Achievement and Externalizing and Internalizing Symptoms Over 20 Years. Dev Psychol. (2005) 41:733–46. doi: 10.1037/0012-1649.41.5.733
9. Miettunen J, Murray GK, Jones PB, Mäki P, Ebeling H, Taanila A, et al. Longitudinal associations between childhood and adulthood externalizing and internalizing psychopathology and adolescent substance use. Psychol Med. (2014) 44:1727–38. doi: 10.1017/S0033291713002328
10. Peyre H, Hoertel N, Stordeur C, Lebeau G, Blanco C, McMahon K, et al. Contributing Factors and Mental Health Outcomes of First Suicide Attempt During Childhood and Adolescence: Results From a Nationally Representative Study. J Clin Psychiatry. (2017) 78:e622–30. doi: 10.4088/JCP.16m10876
11. Wang PS, Angermeyer M, Borges G, Bruffaerts R, Tat Chiu WAI, De Girolamo G, et al. For The Who World Mental Health Survey, C. Delay and failure in treatment seeking after first onset of mental disorders in the World Health Organization's World Mental Health Survey Initiative. World Psychiatry. (2007) 6:177–85. Available online at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2174579/
12. Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. (2005) 62:593–602. doi: 10.1001/archpsyc.62.6.593
13. Raven D, Jorg F, Visser E, Oldehinkel AJ, Schoevers RA. Time-to-treatment of mental disorders in a community sample of Dutch adolescents. A TRAILS study. Epidemiol Psychiatr Sci. (2017) 26:177–88. doi: 10.1017/S2045796016000226
14. Dougherty LR, Leppert KA, Merwin SM, Smith VC, Bufferd SJ, Kushner MR. Advances and directions in preschool mental health research. Child Dev Perspect. (2015) 9:14–9. doi: 10.1111/cdep.12099
15. Whalen DJ, Sylvester CM, Luby JL. Depression and anxiety in preschoolers: a review of the past 7 years. Child Adolesc Psychiatr Clin N Am. (2017) 26:503–22. doi: 10.1016/j.chc.2017.02.006
16. Sandman CA, Curran MM, Davis EP, Glynn LM, Head K, Baram TZ. Cortical Thinning and neuropsychiatric outcomes in children exposed to prenatal adversity: a role for placental CRH? Am J Psychiatry. (2018) 175:471–9. doi: 10.1176/appi.ajp.2017.16121433
17. Park A, Leonard J, Saxler PK, Cyr AB, Gabrieli J, Mackey AP. Amygdala-medial prefrontal cortex connectivity relates to stress and mental health in early childhood. Soc Cogn Affect Neurosci. (2018) 13:430–9. doi: 10.1093/scan/nsy017
18. Satterthwaite TD, Wolf DH, Calkins ME, Vandekar SN, Erus G, Ruparel K, et al. Structural Brain Abnormalities in Youth With Psychosis Spectrum Symptoms. JAMA Psychiatry. (2016) 73:515–24. doi: 10.1001/jamapsychiatry.2015.3463
19. Wolf DH, Satterthwaite TD, Calkins ME, Ruparel K, Elliott MA, Hopson RD, et al. Functional neuroimaging abnormalities in youth with psychosis spectrum symptoms. JAMA Psychiatry. (2015) 72:456–65. doi: 10.1001/jamapsychiatry.2014.3169
20. Lussier AA, Hawrilenko M, Wang MJ, Choi KW, Cerutti J, Zhu Y. Major Depressive Disorder Working Group of the Psychiatric Genomics Consortium & Dunn, E. C Genetic susceptibility for major depressive disorder associates with trajectories of depressive symptoms across childhood and adolescence. J Child Psychol Psychiatry. (2021) 62:895–904. doi: 10.1111/jcpp.13342
21. Clarke TK, Lupton MK, Fernandez-Pujals AM, Starr J, Davies G, Cox S, et al. Common polygenic risk for autism spectrum disorder (ASD) is associated with cognitive ability in the general population. Mol Psychiatry. (2016) 21:419–25. doi: 10.1038/mp.2015.12
22. Wray NR, Lee SH, Mehta D, Vinkhuyzen AA, Dudbridge F, Middeldorp CM. Research review: Polygenic methods and their application to psychiatric traits. J Child Psychol Psychiatry. (2014) 55:1068–87. doi: 10.1111/jcpp.12295
23. Davis KA, Mountain RV, Pickett OR, Den Besten PK, Bidlack FB, Dunn EC. Teeth as Potential New Tools to Measure Early-Life Adversity and Subsequent Mental Health Risk: An Interdisciplinary Review and Conceptual Model. Biol Psychiatry. (2020) 87:502–13. doi: 10.1016/j.biopsych.2019.09.030
24. Agarwal KN, Narula S, Faridi MMA, Kalra N. Deciduous dentition and enamel defects. Indian Pediatr. (2003) 40:124.
25. Chaves AMB, Rosenblatt A, Oliveira OFB. Enamel defects and its relation to life course events in primary dentition of Brazilian children: a longitudinal study. Commun Dent Health. (2007) 24:31.
26. Susser E, Clair DS, He L. Latent effects of prenatal malnutrition on adult health: the example of schizophrenia. Ann N Y Acad Sci. (2008) 1136:185–92. doi: 10.1196/annals.1425.024
27. Bilbo SD, Schwarz JM. Early-life programming of later-life brain and behavior: a critical role for the immune system. Front Behav Neurosci. (2009) 3:14. doi: 10.3389/neuro.08.014.2009
28. Roffman J, Sipahi K, Dowling K, Hughes D, Hopkinson C, Lee H, et al. Association of adverse prenatal exposure burden with dimensional child psychopathology in the Adolescent Brain Cognitive Development (ABCD) Study. PLoS ONE. (2021) 16:e0250235. doi: 10.1371/journal.pone.0250235
29. Parsons CLB, Mountain RV, Lau A, Troulis MJ, Bidlack FB, Dunn EC. The Meaning and Purpose of Primary Tooth Disposal Rituals: Implications for Pediatric Dental Professionals. Front Dent Med. (2021) 2:44. doi: 10.3389/fdmed.2021.698144
30. Adams JB, Romdalvik J, Ramanujam VMS, Legator MS. Mercury, Lead, and Zinc in Baby Teeth of Children with Autism Versus Controls. J Toxicol Environ Health A. (2007) 70:1046–51. doi: 10.1080/15287390601172080
31. Abdullah MM, Ly AR, Goldberg WA, Clarke-Stewart KA, Dudgeon JV, Mull CG, et al. Heavy metal in children's tooth enamel: related to autism and disruptive behaviors? J Autism Dev Disord. (2012) 42:929–36. doi: 10.1007/s10803-011-1318-6
32. Palmer RF, Heilbrun L, Camann D, Yau A, Schultz S, Elisco V, et al. Organic Compounds Detected in Deciduous Teeth: A Replication Study from Children with Autism in Two Samples. J Environ Public Health. (2015) 2015:862414. doi: 10.1155/2015/862414
33. Arora M, Reichenberg A, Willfors C, Austin C, Gennings C, Berggren S, et al. Fetal and postnatal metal dysregulation in autism. Nat Commun. (2017) 8:15493. doi: 10.1038/ncomms15493
34. Curtin P, Austin C, Curtin A, Gennings C, Arora M, Tammimies K, et al. Dynamical features in fetal and postnatal zinc-copper metabolic cycles predict the emergence of autism spectrum disorder. Sci Adv. (2018) 4:eaat1293. doi: 10.1126/sciadv.aat1293
35. Frye RE, Cakir J, Rose S, Delhey L, Bennuri SC, Tippett M, et al. Early life metal exposure dysregulates cellular bioenergetics in children with regressive autism spectrum disorder. Transl Psychiatry. (2020) 10:1–12. doi: 10.1038/s41398-020-00905-3
36. Yalçin SS, Çak T, Yalçin S. Lower strontium in two different body matrices in neurodevelopmental disorders: a preliminary report. J Trace Elem Med Biol. (2020) 62:126553. doi: 10.1016/j.jtemb.2020.126553
37. Austin C, Curtin P, Curtin A, Gennings C, Arora M, Tammimies K, et al. Dynamical properties of elemental metabolism distinguish attention deficit hyperactivity disorder from autism spectrum disorder. Transl Psychiatry. (2019) 9:238. doi: 10.1038/s41398-019-0567-6
38. Curtin P, Austin C, Curtin A, Gennings C, Figueroa-Romero C, Mikhail KA, et al. Dysregulated biodynamics in metabolic attractor systems precede the emergence of amyotrophic lateral sclerosis. PLoS Comput Biol. (2020) 16:e1007773. doi: 10.1371/journal.pcbi.1007773
39. Figueroa-Romero C, Mikhail KA, Gennings C, Curtin P, Bello GA, Botero TM, et al. Early life metal dysregulation in amyotrophic lateral sclerosis. Ann Clin Transl Neurol. (2020). doi: 10.1002/acn3.51006
40. Mora AM, Arora M, Harley KG, Kogut K, Parra K, Hernández-Bonilla D, et al. Prenatal and postnatal manganese teeth levels and neurodevelopment at 7, 9, and 105 years in the CHAMACOS cohort. Environ Int. (2015) 84:39–54. doi: 10.1016/j.envint.2015.07.009
41. Horton MK, Hsu L, Henn BC, Margolis A, Austin C, Svensson K, et al. Dentine biomarkers of prenatal and early childhood exposure to manganese, zinc and lead and childhood behavior. Environ Int. (2018) 121:148–58. doi: 10.1016/j.envint.2018.08.045
42. Modabbernia A, Velthorst E, Gennings C, De Haan L, Austin C, Sutterland A, et al. Early-life metal exposure and schizophrenia: a proof-of-concept study using novel tooth-matrix biomarkers. Eur Psychiatry. (2016) 36:1–6. doi: 10.1016/j.eurpsy.2016.03.006
43. Velthorst E, Smith L, Bello G, Austin C, Gennings C, Modabbernia A, et al. New Research Strategy for Measuring Pre- and Postnatal Metal Dysregulation in Psychotic Disorders. Schizophr Bull. (2017) 43:1153–7. doi: 10.1093/schbul/sbx112
44. Kurek M, Borowska B, Lubowiedzka-Gontarek B, Rosset I, Zadzińska E. Disturbances in primary dental enamel in Polish autistic children. Sci Rep. (2020) 10:12751. doi: 10.1038/s41598-020-69642-3
45. Boyce WT, Den Besten PK, Stamperdahl J, Zhan L, Jiang Y, Adler NE, et al. Social inequalities in childhood dental caries: The convergent roles of stress, bacteria and disadvantage. Soc Sci Med. (2010) 71:1644–52. doi: 10.1016/j.socscimed.2010.07.045
46. Kaur K, Suneja B, Jodhka S, Kaur J, Singh A, Singh SR. Metallic insignia in primary teeth: A biomarker for Autism Spectrum Disorders. J Indian Soc Pedod Prev Dent. (2021) 39:61. doi: 10.4103/jisppd.jisppd_485_20
47. Arora M, Austin C. Teeth as a biomarker of past chemical exposure. Curr Opin Pediatr. (2013) 25:261–7. doi: 10.1097/MOP.0b013e32835e9084
48. Liu W, Xin Y, Li Q, Shang Y, Ping Z, Min J, et al. Biomarkers of environmental manganese exposure and associations with childhood neurodevelopment: A systematic review and meta-analysis. Environ Health. (2020) 19:1–22. doi: 10.1186/s12940-020-00659-x
49. Obradović J, Bush NR, Stamperdahl J, Adler NE, Boyce WT. Biological Sensitivity to Context: The Interactive Effects of Stress Reactivity and Family Adversity on Socioemotional Behavior and School Readiness. Child Dev. (2010) 81:270–89. doi: 10.1111/j.1467-8624.2009.01394.x
50. Bush NR, Alkon A, Obradovic J, Stamperdahl J, Boyce WT. Differentiating Challenge Reactivity from Psychomotor Activity in Studies of Children's Psychophysiology: Considerations for Theory and Measurement. J Exp Child Psychol. (2011) 110:62–79. doi: 10.1016/j.jecp.2011.03.004
51. Armstrong JM, Goldstein LH. The MacArthur working group on outcome assessment: Manual for the MacArthur health and behavior questionnaire (HBQ 1.0). In: Kupfer DJ, editor. MacArthur Foundation Research Network on Psychopathology and Development. Pittsburgh, PA: University of Pittsburgh (2003).
52. Ablow JC, Measelle JR. The MacArthur Working Group on Outcome Assessment: MacArthur Foundation Research Network on Psychopathology and Development. Manual for the Berkeley Puppet Interview: Symptomatology, Social, and Academic Modules (BPI 1.0). Pittsburgh, PA: University of Pittsburgh Press (2003).
53. Kraemer HC, Measelle JR, Ablow JC, Essex MJ. Boyct, Kupfer DJ. A new approach to integrating data from multiple informants in psychiatric assessment and research: Mixing and matching contexts and perspectives. Am J Psychiatry. (2003) 160:1566–77. doi: 10.1176/appi.ajp.160.9.1566
54. Goulter N, Roubinov DS, McMahon RJ, Boyce WT. Bush, NR. Externalizing and Internalizing Problems: Associations with Family Adversity and Young Children's Adrenocortical and Autonomic Functioning. Res Child Adolesc Psychopathol. (2021) 49:629–42. doi: 10.1007/s10802-020-00762-0
55. Roubinov DS, Boyce WT, Bush NR. Informant-specific reports of peer and teacher relationships buffer the effects of harsh parenting on children's oppositional defiant disorder during kindergarten. Dev Psychopathol. (2020) 32:163–74. doi: 10.1017/S0954579418001499
56. Roubinov DS, Boyce WT, Lee MR, Bush NR. Evidence for discrete profiles of children's physiological activity across three neurobiological system and their transitions over time. Dev Sci. (2021) 24:e12989. doi: 10.1111/desc.12989
57. Boyce WT, Obradović J, Bush NR, Stamperdahl J, Kim YS, Adler N. Social stratification, classroom climate, and the behavioral adaptation of kindergarten children. Proc Nat Acad Sci. (2012) 109:17168–73. doi: 10.1073/pnas.1201730109
58. Anderson ER, Mayes LC. Race/ethnicity and internalizing disorders in youth: A review. Clin Psychol Rev. (2010) 30:338–48. doi: 10.1016/j.cpr.2009.12.008
59. Logan W, Kronfeld R. Development of the human jaws and surrounding structures from birth to the age of fifteen years (Table). J Am Dent Assoc. (1933) 20:379–427. doi: 10.14219/jada.archive.1933.0080
60. Schuurs A. In:Pathology of the Hard Dental Tissues Ch. 1, 431-431. Hoboken, NJ: John Wiley & Sons, Ltd. (2013).
62. Lunt RC, Law DB. A review of the chronology of calcification of deciduous teeth. J Am Dent Assoc. (1974) 89:599–606. doi: 10.14219/jada.archive.1974.0446
63. Lacruz RS, Hacia JG, Bromage TG, Boyde A, Lei Y, Xu Y, et al. The Circadian Clock Modulates Enamel Development. J Biol Rhythms. (2012) 27:237–45. doi: 10.1177/0748730412442830
64. Lunt RC, Law DB. A review of the chronology of eruption of deciduous teeth. J Am Dent Assoc. (1974) 89:872–9. doi: 10.14219/jada.archive.1974.0484
65. Vasileva M, Graf RK, Reinelt T, Petermann U, Petermann F. Research review: A meta-analysis of the international prevalence and comorbidity of mental disorders in children between 1 and 7 years. J Child Psychol Psychiatry. (2021) 62:372–81. doi: 10.1111/jcpp.13261
66. Makoi BA, Youngstrom EA, Racz SJ, Qasmieh N, Glenn LE, De Los Reyes A. Integrating multiple informants' reports: How conceptual and measurement models may address long-standing problems in clinical decision-making. Clin Psychol Sci. (2020) 8:953–70. doi: 10.1177/2167702620924439
67. Mountain RV, Zhu Y, Pickett OR, Lussier AA, Goldstein J, Roffman JL, et al. Association of maternal stress and social support during pregnancy with growth marks in children's primary tooth enamel. JAMA Network Open. (2021) 4:e2129129. doi: 10.1001/jamanetworkopen.2021.29129
68. Bush NR, Boyce WT. Differential sensitivity to context: Implications for developmental psychopathology. In: Cicchetti D, editor. Developmental Psychopathology: Developmental Neuroscience. John Wiley and Sons, Inc (2016). p. 107–37. doi: 10.1002/9781119125556.devpsy203
Keywords: teeth, biomarkers, prevention, pediatric, internalizing symptoms, externalizing symptoms
Citation: Dunn EC, Mountain RV, Davis KA, Shaffer I, Smith ADAC, Roubinov DS, Den Besten P, Bidlack FB and Boyce WT (2022) Association Between Measures Derived From Children's Primary Exfoliated Teeth and Psychopathology Symptoms: Results From a Community-Based Study. Front. Dent. Med. 3:803364. doi: 10.3389/fdmed.2022.803364
Received: 30 October 2021; Accepted: 13 January 2022;
Published: 29 March 2022.
Edited by:
Jayakumar Jayaraman, Virginia Commonwealth University, United StatesReviewed by:
Anshad Mohamed Abdulla, King Khalid University, Saudi ArabiaThalyta Pinheiro Ferreira, University of California, Los Angeles, United States
Sivakumar Nuvvula, Narayana Dental College and Hospital, India
Copyright © 2022 Dunn, Mountain, Davis, Shaffer, Smith, Roubinov, Den Besten, Bidlack and Boyce. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Erin C. Dunn, ZWR1bm4yQG1naC5oYXJ2YXJkLmVkdQ==
†These authors have contributed equally to this work
 Erin C. Dunn
Erin C. Dunn Rebecca V. Mountain
Rebecca V. Mountain Kathryn A. Davis1
Kathryn A. Davis1 Ida Shaffer
Ida Shaffer Danielle S. Roubinov
Danielle S. Roubinov Pamela Den Besten
Pamela Den Besten Felicitas B. Bidlack
Felicitas B. Bidlack W. Thomas Boyce
W. Thomas Boyce