- 1Private Practitioner, Waterford, MI, United States
- 2Private Practitioner, Chicago, IL, United States
- 3Private Practitioner, Greenville, NC, United States
- 4Adams School of Dentistry, University of North Carolina at Chapel Hill, Chapel Hill, NC, United States
- 5Dental School, University of Texas Health San Antonio, San Antonio, TX, United States
Vital pulp therapy (VPT) is a viable treatment option for carious teeth with exposed pulps. To our knowledge, no study has examined the correlation between postoperative pain and the outcome of VPT on asymptomatic permanent teeth. The aim of this study was to examine whether odontogenic pain experienced after VPT on asymptomatic teeth with a carious pulp exposures is correlated with the progression of pulpal disease into a more inflamed or necrotic state. Direct pulp caps or partial pulpotomies using a tricalcium silicate (MTA Angelus, Angelus, Londrina, Brazil) were performed on asymptomatic permanent teeth using a standardized protocol. Patients were contacted at 24 h, 1 week, and 3 months following treatment and data was collected on post-operative pain and analgesic intake using a standardized questionnaire. At 6 months after treatment, an in-person clinical exam was performed which included standard vitality tests along with exposure of a periapical radiograph. Success was defined as an asymptomatic, functional tooth without any clinical or radiographic pathology. Data was analyzed using logistic regression. VPT was successful in 84.3% of patients at the 6 months timepoint. The percentage of patients that experienced pain at 24-h, 1 week, and 3-month time periods was 38, 22, and 12%, respectively. Pain at 3 months was significantly correlated with decreased outcome (p = 0.028). This data suggests that postoperative pain in the first 3 months after VPT is predictive of a poor treatment outcome.
Introduction
Developing minimally invasive biologically based therapies is an emerging theme in dentistry. Pulp capping and partial pulpotomy procedures are minimally invasive and are designed to manage the bacterial contamination, stimulate formation of reparative dentin, and restore homeostasis in the pulp. The long-term goal of these procedures is the preservation of functional teeth with healthy pulps and periapical tissues.
The traditional treatment for teeth with carious pulp exposures is to perform non-surgical root canal treatment. Justification for this treatment is often based on the American Association of Endodontists' definition of asymptomatic irreversible pulpitis- “A clinical diagnosis based on subjective and objective findings indicating that the vital inflamed pulp is incapable of healing” (1). While vital pulp therapy has always been an option for teeth with carious pulp exposures, it is rarely performed due to lack of predictability. Recent publications provide evidence that vital pulp therapy is a viable and predictable treatment option (2–6).
The reported success of vital pulp therapy, specifically partial pulpotomies and pulp capping procedures, ranges from as low as 37% to as high as 97% (2, 3, 7–11). Much of the variability in success rates across these studies is likely due to differences in study design and the materials used. Earlier studies on vital pulp therapy used calcium hydroxide, while more recent studies used tricalcium silicates (2–5, 7–12). It is clear from these studies that the use of tricalcium silicates is associated with higher success rates than calcium hydroxide (4, 6, 12). Data from these studies also suggests that factors such as age, gender, tooth type, and location of pulp exposure may influence the outcome of this treatment (2, 4, 6–10, 12–14).
A report on the outcomes of randomized clinical trials on the management of deep carious lesions noted that patients who experienced pretreatment pain were less likely to have a successful outcome as compared to those who had no pain (P = 0.03) (15). Studies on conventional root canal treatment also show that pain before and during treatment is strongly associated with a less optimal treatment outcome (16, 17). Thus, suggesting that pain is a predictor for pulpal and periapical healing following dental interventions. This prospective, observational study tests the hypothesis that pain experienced after partial pulpotomy and pulp-capping procedures is correlated to the treatment outcome.
Materials and Methods
This study was approved by the office of Human Ethics and Research at our Institution (#15-2275). Written informed consent was obtained from 73 healthy patients (aged 15 years or older) who met the study criteria. Inclusion criterion were carious pulp exposure on an asymptomatic mature, permanent tooth. Exclusion criteria included severe systemic disease determined as American Society of Anesthesiologists score of ≥ 3, a history of pain indicative of irreversible pulpitis (e.g., patient presents with or reports history of spontaneous pain and/or exaggerated pain to thermal stimuli), presence of periapical disease (pain on percussion or a periapical radiolucency) and inability to obtain hemostasis at the pulpal exposure site.
Partial pulpotomy and pulp capping procedures were performed by 3rd- and 4th-year dental students under the direct supervision of study investigators (MS-A, TT, and WY). The first step in the standardized protocol was to isolate the tooth with either a rubber dam or Isolite (Isolite Systems, Santa Barbara, Calif) after obtaining local anesthesia. Caries removal was then completed and verified by the use of a caries dye indicator (Sable Seek, Ultradent Products, South Jordan, UT, USA). Next, if hemorrhage was noted a partial pulpotomy was performed with a sterile 1 mm diameter round diamond bur (Endo-Access Bur, Dentsply Maillefer, WoodBridge, ON, Canada) and a sterilized cotton pellet soaked in 4.25% sodium hypochlorite was placed with firm pressure for 60 s over the exposure site. If hemorrhage was noted from the pulp upon removal of the cotton pellet, the procedure was repeated for up to three times to obtain hemostasis. The tooth was excluded from the study if hemorrhage continued after three attempts. If hemostasis was achieved, a 3 mm thick layer of a tricalcium silicate (MTA Angelus, Angelus, Londrina, Brazil) was placed over the exposure site with a Dovgan carrier (Quality Aspirators, Duncanville, Texas). A resin-modified glass ionomer (Vitrebond™, 3M, Maplewood, MN) was placed over the tricalcium silicate and light cured. Amalgam (Dispersalloy, Denstply Sirona, Charlotte, NC) or a resin based restorative material (Filtek Universal Restorative, 3M, Maplewood, MN) was used to restore the tooth and a periapical radiograph was exposed. If no hemorrhage had been noted on caries removal, then a direct pulp cap was placed as described above. Data on intra-operative variables such as tooth type, location of pulpal exposure, size of the exposure (> or <1 mm; measured using a 1 mm round bur), number of attempts needed to obtain hemostasis and type of permanent restoration were recorded.
Patients were contacted via phone call at 24 h, 1 week, and 3 months after the procedure and a standardized questionnaire was used to collect data on the incidence and intensity of post-operative pain (on a 11-point numerical scale) and on analgesic use. Pain intensity rated as <3 was defined as mild pain, 4–6 was defined as moderate pain and, that more than seven was defined as severe pain. Patients experiencing moderate to severe pain were re-evaluated and additional treatments (pulpectomy or extraction) performed if indicated. Six months after the procedure patients returned for a clinical examination. The exam included standard diagnostic tests such as percussion, palpation, mobility, and periodontal probing. Pulp vitality was determined by using a cold stimulus (EndoIce, Coltène Whaledent, Cuyahoga Falls, Ohio) as well as the electric pulp tester (Vitality ScannerTM, Kerr, Brea CA). A periapical radiograph was also exposed. The treatment outcome was determined to be successful if the tooth was asymptomatic, responded normally to all diagnostic tests and, was not associated with any radiographic pathology. If any additional endodontic treatment had been performed on the tooth after the vital pulp therapy procedure, it was considered a failure. All clinical examinations were performed by standardized operators (M S-A, TT, and WY).
Data Analysis
Sample size analysis was based on prior studies on vital pulp therapy (7–9). The main outcome variable for this study was success or failure. The “R” function “glm” for generalized linear model with family (success/failure) as “binomial” was used to analyze the data. We also examined the data for associations between selected peri-operative predictors and post-treatment pain. For size of the exposure, the data was log transformed and linear regression was fit with the predictor and outcome variable. Significance was set at p < 0.05. All the statistical analysis was performed in R statistical software (version 3.2.3, www.cran.r-project.org).
Results
Seventy-three patients were recruited to the study of which seventy-one patients were available for the 24-h and 1-week follow-up phone calls. Fifty-five patients were available for 3-month phone calls and 51 patients presented for the 6-month clinical follow-up. Patients ranged in age from 15 to 78 years old (median age was 45). Sixty-seven percent of patients were female. Forty-seven percent of the teeth treated were anterior teeth, 26% were premolars and the remaining 47% were molars.
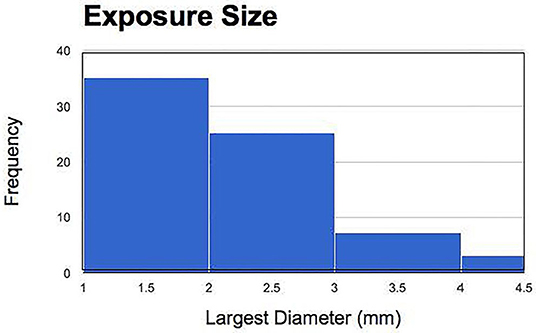
Regarding hemorrhage control, it was noted that in 78% of teeth hemostasis was immediately achieved without the need for partial pulpotomy, 21% of teeth needed a single attempt of partial pulpotomy to achieve pulpal hemostasis, and 1% of teeth needed two attempts of partial pulpotomy to achieve pulpal hemostasis. Regarding the locations of the pulpal exposure sites in 14 teeth it was on the buccal/lingual surface, in 16 teeth it was on the occlusal surface and in 40 teeth it involved the interproximal surfaces. The size of the exposure ranged from 1 to 4.5 mm (Figure 1).
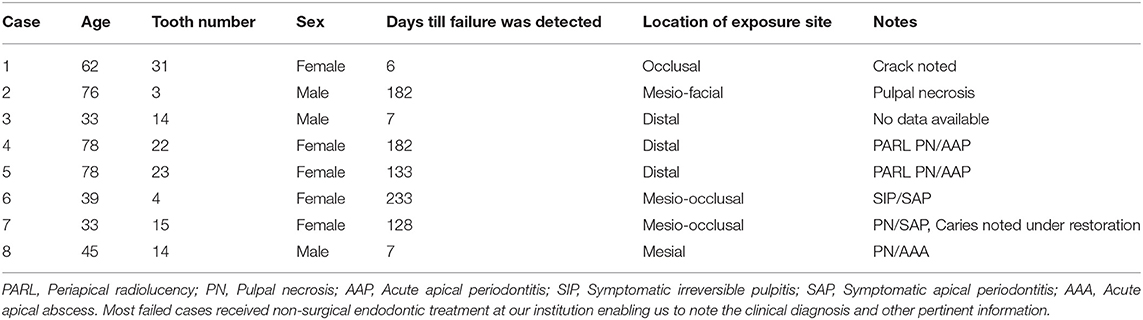
Sixty-five percent of patients experienced pain in the 24-h post-treatment period. The incidence of post-operative pain as well as the intensity of pain decreased over time with most (83%) patients being pain free after 3 months (Figures 2, 3). A similar trend was noted with analgesic intake (Figure 4). The study patients took a wide variety of analgesics including ibuprofen (200–800 mg) and acetaminophen (500 mg). Only 1 patient used hydrocodone with acetaminophen (5 mg/325 combination) and one other patient took codeine with acetaminophen (30 mg/300 mg combination) for post-operative pain relief. Both narcotics were taken at the 24-h time point. Analgesic intake decreased in a time-dependent manner from 30% to 19% to 9% at the 24-h, 1 week, and 3-month time points, respectively. Detailed information on cases which failed to heal is shown in Table 1.
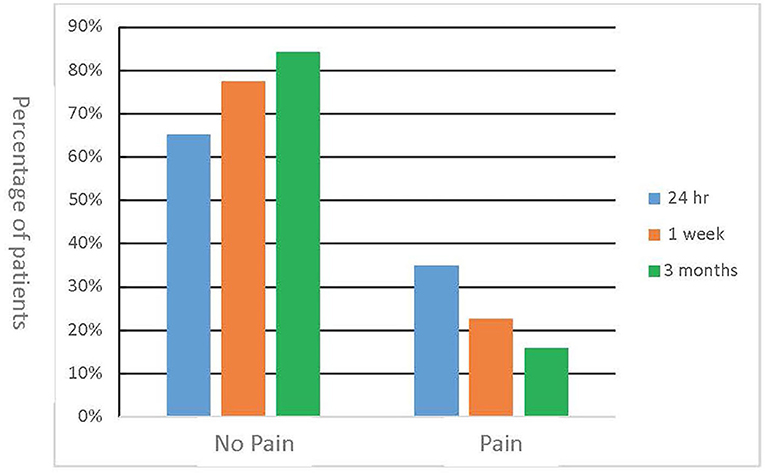
Figure 2. Incidence of post-operative pain. Patients were contacted via phone call at 24 h, 1 week, and 3 months after the procedure and a standardized questionnaire was used to collect data on the incidence of post-operative pain.
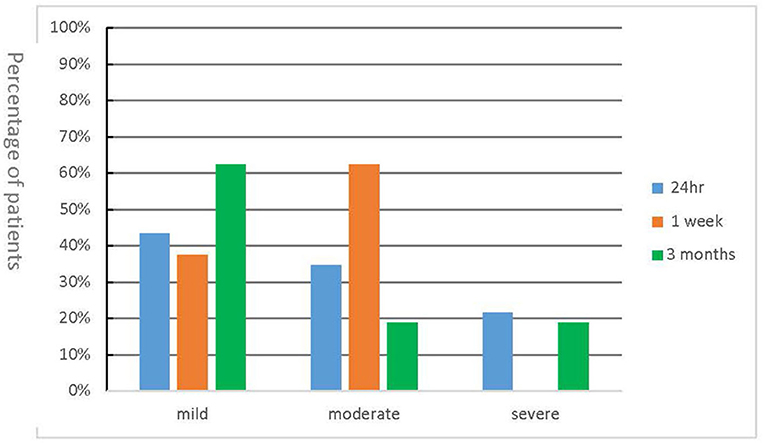
Figure 3. Intensity of post-operative pain. Patients were contacted via phone call at 24 h, 1 week, and 3 months after the procedure and asked to rate their pain intensity on a 11-point numerical scale.
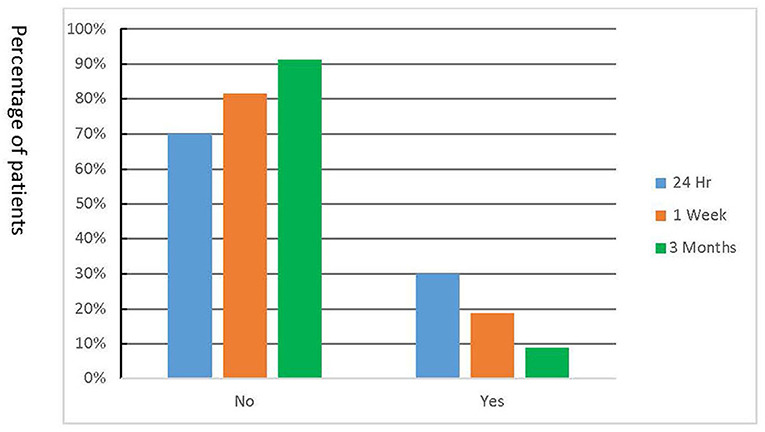
Figure 4. Analgesic use during the post-treatment period. Data on analgesic use was collected by calling the patients at 24 h, 1 week, and 3 months after the treatment.
The success rate at 6 months after treatment was 84.3%. Using the generalized linear model with predictors—pain at 24 h, pain at 1 week and pain at 3 months, tooth type and Patients' age, we found that pain at 3 months is significantly associated with failure (p = 0.028). We also noted marginal significance between patients' age and failure (p = 0.059) with failure rates being higher in older patients. On analyzing our data for an association between exposure size and post-treatment pain, a marginal significance (p = 0.0596) was noted between exposure size and pain at 24 h. No associations were noted between the other factors evaluated (gender, tooth type, and exposure site) and treatment outcome or perioperative pain. The two additional factors evaluated, gender type and exposure site, were not associated with treatment outcome.
Discussion
Within the specialty of endodontics, information on pain is used to make the diagnosis, and to anticipate the need for additional anesthetics and post-operative analgesics. However, it is rarely used a predictor for treatment outcome. To our knowledge, this is the first pragmatic study to evaluate the relationship between post-treatment pain and treatment outcome in endodontic patients. Our results suggest that contacting patients in the first 3 months after treatment to inquire on post-operative pain will help in early recognition of treatment failures.
Several trends were noted on the post-operative pain reported. First, approximately one-third of patients who underwent the procedure experienced some level of postoperative pain. In a majority of the patients the pain was most intense in the first 24 h and resolved completely after 1 week. Second, the data shows that mild to moderate pain in the immediate postoperative time period is not associated with failure. Lastly, while most patients did not feel the need to take analgesics after VPT, those that did, took them in the earlier postoperative periods. This is valuable information for clinicians who can use it to inform their patients on what to expect after pulp capping or partial pulpotomy procedures.
With a p-value of 0.028, there is a significant association between continued pain at the 3-month time point and the unfavorable outcome of VPT. Conversely a lack of pain may indicate continued improvement in the pulpal status. This data suggests that the 3-month post-treatment evaluation point is critical for predicting long term prognosis, and that complete endodontic evaluation should be undertaken at that time. Reevaluation of the prognosis at 3 months, may be an indication that additional restorative or prosthetic treatment on the tooth can proceed. Thus, the dentist and patient can confidently proceed with additional treatment if, at 3 months, the tooth still exhibits lack of clinical and radiographic pathology, while also being asymptomatic.
This pragmatic study on the outcome of vital pulp therapy is unique in that the treatment procedures were performed by dental students. While these students had been trained on the protocol and were supervised by dental faculty, their skills were still being developed at the time of the study. In spite of this, the treatment had a high success rate in maintaining pulp vitality. Thus, providing evidence of the short learning curve needed to learn how to perform this treatment.
VPT is an excellent treatment option to address pulpal involvement during restorative procedures and to increase the likelihood of preserving pulpal vitality. It is an important third option in addition to root canal treatment or extraction for asymptomatic teeth with cariously exposed pulps. Patients with limited financial resources who often choose extraction over root canal treatment, now have the option to maintain their vital teeth.
Pain associated with pulpitis results from activation and/or sensitization of nociceptors by inflammatory and immune mediators released in response to microbial infections or injury. Post-treatment pain after a pulp capping procedure is also a result of similar mechanisms. It is also likely that the treatment procedures themselves induce a transient inflammatory response. Pulpitis pain is inflammatory and does respond to anti-inflammatory drugs such as NSAIDs and steroids. As evidenced by this and other studies, NSAIDs were very effective in attenuating the post-treatment pain. In conclusion, this study provides evidence that post-treatment pain is a predictor of treatment outcome after VPT procedures in asymptomatic teeth with carious pulpal exposure. Our data also support the high success rate of VPT, and the short learning curve required to perform this procedure with a high degree of confidence.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by Institutional Review Board, University of North Carolina-Chapel Hill. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
MS-A, TT, and WY contributed to the execution of the clinical study, data collection, and manuscript preparation. PT and CH contributed to study design and data interpretation. DW and CH contributed to sample size calculation and data analysis. AK contributed to hypothesis generation, supervision of the clinical study, data interpretation, and manuscript preparation. All authors contributed to the article and approved the submitted version.
Funding
This work was funded by the Foundation for Endodontics.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The results of this study were presented as oral presentations and poster presentations at the 2017 annual meeting of the American Association of Endodontists and the abstracts were published in the Journal of Endodontics (18–20).
References
1. Levin LG, Law AS, Holland GR, Abbott PV, and Roda RS. Identify and define all diagnostic terms for pulpal health and disease states. J Endod. (2009) 35:1645–57. doi: 10.1016/j.joen.2009.09.032
2. Jang Y, Song M, Yoo I-S, Song Y, Roh B-D, and Kim E. A randomized controlled study of the use of proroot mineral trioxide aggregate and endocem as direct pulp capping materials: 3-month versus 1-year outcomes. J Endod. (2015) 41:1201–6. doi: 10.1016/j.joen.2015.03.015
3. Marques MS, Wesselink PR, and Shemesh H. Outcome of direct pulp capping with mineral trioxide aggregate: a prospective study. J Endod. (2015) 41:1026–31. doi: 10.1016/j.joen.2015.02.024
4. Li Z, Cao L, Fan M, and Xu Q. Direct pulp capping with calcium hydroxide or mineral trioxide aggregate: a meta-analysis. J Endod. (2015) 41:1412–7. doi: 10.1016/j.joen.2015.04.012
5. Taha NA, Ahmad MB, and Ghanim A. Assessment of Mineral Trioxide Aggregate pulpotomy in mature permanent teeth with carious exposures. Int Endod J. (2017) 50:117–25. doi: 10.1111/iej.12605
6. Çalişkan MK, and Güneri P. Prognostic factors in direct pulp capping with mineral trioxide aggregate or calcium hydroxide: 2- to 6-year follow-up. Clin Oral Investig. (2017) 21:357–67. doi: 10.1007/s00784-016-1798-z
7. Barthel CR, Rosenkranz B, Leuenberg A, and Roulet JF. Pulp capping of carious exposures: treatment outcome after 5 and 10 years: a retrospective study. J Endod. (2000) 26:525–8. doi: 10.1097/00004770-200009000-00010
8. Haskell EW, Stanley HR, Chellemi J, and Stringfellow H. Direct pulp capping treatment: a long-term follow-up. J Am Dent Assoc. (1978) 97:607–12. doi: 10.14219/jada.archive.1978.0356
9. Matsuo T, Nakanishi T, Shimizu H, and Ebisu S. A clinical study of direct pulp capping applied to carious-exposed pulps. J Endod. (1996) 22:551–6. doi: 10.1016/S0099-2399(96)80017-3
10. Eghbal MJ, Asgary S, Baglue RA, Parirokh M, and Ghoddusi J. MTA pulpotomy of human permanent molars with irreversible pulpitis. Aust Endod J J Aust Soc Endodontology Inc. (2009) 35:4–8. doi: 10.1111/j.1747-4477.2009.00166.x
11. Bogen G, Kim JS, and Bakland LK. Direct pulp capping with mineral trioxide aggregate: an observational study. J Am Dent Assoc. (2008) 139:305–15. doi: 10.14219/jada.archive.2008.0160
12. Mente J, Hufnagel S, Leo M, Michel A, Gehrig H, Panagidis D, et al. Treatment outcome of mineral trioxide aggregate or calcium hydroxide direct pulp capping: long-term results. J Endod. (2014) 40:1746–51. doi: 10.1016/j.joen.2014.07.019
13. Cho S-Y, Seo D-G, Lee S-J, Lee J, Lee S-J, and Jung I-Y. Prognostic factors for clinical outcomes according to time after direct pulp capping. J Endod. (2013) 39:327–31. doi: 10.1016/j.joen.2012.11.034
14. Aguilar P, and Linsuwanont P. Vital pulp therapy in vital permanent teeth with cariously exposed pulp: a systematic review. J Endod. (2011) 37:581–7. doi: 10.1016/j.joen.2010.12.004
15. Bjørndal L, Fransson H, Bruun G, Markvart M, Kjældgaard M, Näsman P, et al. Randomized clinical trials on deep carious lesion: 5 year follow-up. JDR. (2017) 96:747–53. doi: 10.1177/0022034517702620
16. Polycarpou N, Ng YL, Canavan D, Moles DR, and Gulabivala K. Prevalence of persistent pain after endodontic treatment and factors affecting its occurrence in cases with complete radiographic healing. Int Endodontic J. (2005) 38:169–78. doi: 10.1111/j.1365-2591.2004.00923.x
17. Yu VS, Messer HH, Yee R, and Shen L. Incidence and impact of painful exacerbations in a cohort with post-treatment persistent endodontic lesions. J Endodo. (2012) 38:41–6. doi: 10.1016/j.joen.2011.10.006
18. Yeung W, Shallal-Ayzin M, Trinh T, Tawil P, Haggerty C, Wu D, et al. Prospective analysis of prognostic indicators of direct pulp caps on mature permanent teeth. J Endod. (2017) 43:e7. doi: 10.1016/S0099-2399(17)30169-3
19. Shallal-Ayzin M, Yeung W, Trinh T, Tawil P, Haggerty C, Wu D, et al. Prospective analysis of perioperative pain following VPT on permanent teeth with mature apices. J Endod. (2017) 43:e38. doi: 10.1016/S0099-2399(17)30169-3
Keywords: vital pulp therapy, caries, pain, predictors, treatment outcome
Citation: Shallal-Ayzin M, Trinh T, Yeung W, Tawil PZ, Haggerty CL, Wu D and Khan AA (2021) A Prospective Analysis of the Correlation Between Postoperative Pain and Vital Pulp Therapy. Front. Dent. Med. 2:647417. doi: 10.3389/fdmed.2021.647417
Received: 29 December 2020; Accepted: 15 February 2021;
Published: 23 March 2021.
Edited by:
Emi Shimizu, Rutgers, The State University of New Jersey, United StatesReviewed by:
Vasudev Ballal, Manipal Academy of Higher Education, IndiaNatalino Lourenço Neto, Universidade de São Paulo, Brazil
Copyright © 2021 Shallal-Ayzin, Trinh, Yeung, Tawil, Haggerty, Wu and Khan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Asma A. Khan, a2hhbmEyQHV0aHNjc2EuZWR1
†These authors have contributed equally to this work and share first authorship
 Mark Shallal-Ayzin1†
Mark Shallal-Ayzin1† Asma A. Khan
Asma A. Khan