- Division of Pediatric Dentistry, College of Dentistry, The Ohio State University, Columbus, OH, United States
Introduction: Early childhood caries burdens children, their families, and the health care system. Utilizing fluoride varnish at medical well-child visits with non-dental primary care providers can be an interprofessional strategy to combat early childhood caries. The COVID-19 pandemic dramatically altered preventive health care delivery and the effects on preventive oral health care delivery have not been previously described.
Methods: This analysis used descriptive statistics and non-parametric Wilcoxon Mann-Whitney tests to compare preventive oral health utilization among 1 to 5-year old children in two state Medicaid agencies before and during the pandemic. Fluoride utilization rates at dental visits and medical well-child visits were calculated as number of users per 1,000 enrolled children. Additionally, the proportion of well-child visits that included fluoride application was calculated for each state.
Results: During the pandemic, the quarterly fluoride utilization rate significantly decreased at dental visits (pre-pandemic = 153.5 per 1,000 enrolled children; pandemic = 36.1 per 1,000 enrolled children, p < 0.001) and signficantly decreased at medical well-child visits (pre-pandemic = 72.2 per 1,000 enrolled children; pandemic = 32.3 per 1,000 enrolled children, p = 0.03) during the pandemic.
Conclusions: The findings highlight the importance of interprofessional collaboration among non-dental primary care providers and dental providers to provide access to preventive oral health services, particularly when access to dentists is limited. Future directions might include rigorous evaluations of co-located medical and dental services or the use of interprofessional telehealth technologies.
Introduction
Early childhood caries (ECC) is an age-defined condition of dental caries in children younger than 6 years old (1). For more than 25 years, professional guidelines have recommended establishing a dental home by age one (2). However, translating this recommendation into dental practices has lagged, so alternative venues have been explored. Children have significantly more medical visits than dental visits prior to age three (2). Accordingly, one intervention policymakers used to increase the proportion of early oral health visits was to reimburse physicians for oral health screening, counseling, and prevention (i.e., fluoride varnish) during medical well-child visits (3).
Many researchers have evaluated oral health prevention provided at early ages of life. Early evidence demonstrated clear increased access to care following implementation of reimbursement for preventive oral health services at well-child visits in physician offices (3, 4). Increased reimbursement also increased utilization of preventive services in dental offices, but it created gaps and exacerbated disparities for certain groups requiring comprehensive care (5–8). For example, children with autism or intellectual and developmental disability had lower preventive care utilization than their peers (8, 9).
Well-child visits can help improve the utilization of preventive oral health services among young children (10). Compared to children who received preventive oral health services during medical well-child visits, children who received preventive care from a dentist had greater caries related treatment (4). Recent analysis questions the long-term benefits of physician provided preventive oral health services because over long follow-up periods, differences in caries related treatment and expenditures tend to attenuate (4, 11–13).
Beyond the application of fluoride varnish, medical well-child visits include personalized anticipatory guidance for general health and safety topics. Both well-child visits and early dental visits provide an opportunity to improve parental oral health knowledge and practices for their children (14). Additionally, these early visits offer chances to coordinate care and referral to dentists for high risk children with extensive and severe disease (15, 16). Well-child visits play an important role in the oral health care system, especially when access to a dentist is severely limited (17).
The coronavirus pandemic exacerbated and created significant access to care issues, especially for young children and those who already had limited access to oral health care. The pandemic disrupted daily life and significantly altered health care delivery. Access to dental care was severely hampered when many offices were forced to shut down or reduce operations to non-aerosolizing, non-emergent procedures according to state regulations and federal guidelines (18). The guidance for routine pediatric medical care was less imposing. The CDC posted guidance emphasizing the importance of routine well-child visits and immunization shortly after the national emergency response was declared in March 2020 (19). As the pandemic progressed, well-child visits returned to 90% of historic averages through 6 months of the pandemic (20).
Preventive oral health services at dental visits and medical well-child visits during the pandemic has not been described. The objective of this analysis was to compare preventive oral health utilization before and during the pandemic. Specifically, fluoride varnish utilization rates at dental visits and well-child visits were compared using data from the Medicaid programs in Ohio and North Carolina.
Methods
The Ohio State University IRB determined this to be non-human subjects' research. Aggregate data from administrative claims were obtained from both North Carolina Medicaid and Partners for Kids, a pediatric accountable care organization managing the Medicaid program in southern and southeastern Ohio. For context, North Carolina Medicaid covers more than 1.2 million children, and Partners for Kids manages the Ohio Medicaid program for more than 325,000 children. North Carolina self-manages a fee-for-service dental program, and Ohio Medicaid primarily contracts with dental managed care organizations to operate its dental program which report to Partners for Kids. The Into the Mouths of Babes initiative in North Carolina was one of the first public health programs to reimburse physicians for preventive oral health services (3). At Partners for Kids, the program is comparatively newer, and physicians are encouraged to participate through the organization's quality improvement program. North Carolina limits reimbursement to physicians for preventive oral health services up to age 42 months, whereas Ohio continues reimbursement up to age 60 months, which aligns with the United States Preventive Health Services Task Force recommendation (21).
Monthly data summaries were requested for 1 to 5-year old children from January 2019 to June 2020. Limited to preventive visits, data for each age included:
• Number of dental visits with fluoride application.
• Number of well-child visits with fluoride application in physician offices.
• Total number of well-child visits.
Enrollment estimates for 1 to 5-year old children were approximately 76,000 in Ohio and 335,000 in North Carolina. Quarterly and monthly fluoride utilization rates were calculated separately for dental visits and well-child visits as the number of visits per 1,000 enrolled children per time period (i.e., quarter or month). The proportion of well-child visits that included fluoride application was also calculated. Although pandemic-imposed restrictions began in mid-March 2020, for analysis, the pandemic was defined as April–June 2020. Analysis relied on descriptive statistics and non-parametric Wilcoxon Mann-Whitney tests to compare utilization rates before and during the pandemic within each state. The level of significance was set at alpha equals 0.05, and all analysis was completed using Stata v.16.1 (STATACORP, LLC., College Station, TX, USA).
Results
Overall, the quarterly fluoride utilization rate at dental visits significantly decreased by 117.4 per 1,000 enrolled children during the pandemic (pre-pandemic = 153.5 per 1,000 enrolled children; pandemic = 36.1 per 1,000 enrolled children; p < 0.001). Quarterly fluoride utilization rate at medical well-child visits significantly decreased by 39.9 per 1,000 enrolled children during the pandemic (pre-pandemic = 72.2 per 1,000 enrolled children; pandemic = 32.3 per 1,000 enrolled children; p = 0.03). However, the proportion of well-child visits that included fluoride application did not significantly change (pre-pandemic = 26%; pandemic = 20%; p = 0.2).
Quarterly utilization rates for each state are summarized in Figure 1. North Carolina had higher fluoride utilization rates at dental visits and well-child visits than Ohio. The proportion of well-child visits that included fluoride application was more than double in North Carolina than in Ohio (40 vs. 18%, respectively). During the pandemic, fluoride utilization rates at dental visits significantly declined in both states. In Ohio, the difference was 116.8 per 1,000 enrolled children (p < 0.001) and in North Carolina, the difference was 118 per 1,000 enrolled children (p < 0.001). Changes in fluoride utilization rates at well-child visits differed in each state. In Ohio, fluoride utilization rate at well-child visits significantly decreased by 45 per 1,000 enrolled children per quarter (p = 0.007). In North Carolina, fluoride utilization rate at well-child visits decreased by 34.8 per 1,000 enrolled children per quarter (p = 0.3). The proportion of total well-child visits that included fluoride was not significantly different during pre-pandemic and pandemic periods. In Ohio, there was a 4 percentage point decrease (p = 0.3) and in North Carolina, there was a 0.1 percentage point decrease (p = 0.9).
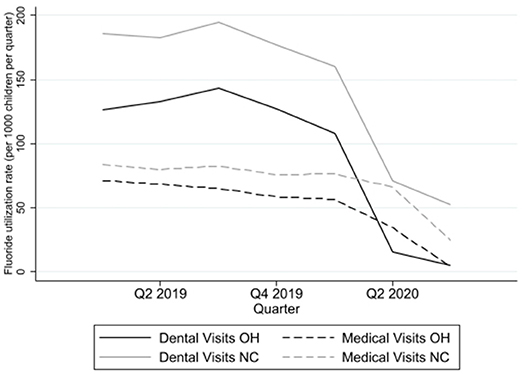
Figure 1. Quarterly fluoride utilization rates at dental visits and medical well-child visits in Ohio (OH) and North Carolina (NC) among Medicaid-enrolled children from January 2019 to June 2020. Q1: January–March. Q2: April–June. Q3: July–September. Q4: October–December. In this figure, the pandemic begins during Q2 2020.
The patterns of monthly utilization are shown in Figure 2. The two states had similar patterns of fluoride utilization rates at dental and well-child visits overall and across age strata. Fluoride utilization rates at dental visits essentially went to zero during March and April 2020, but has since rebounded. Consistently over the study period, 1-year-old children were the age group with the greatest proportion of recipients of fluoride varnish at well-child visits (Figure 2). The major source of professionally applied fluoride during the onset of the pandemic occurred in medical, rather than dental, settings.
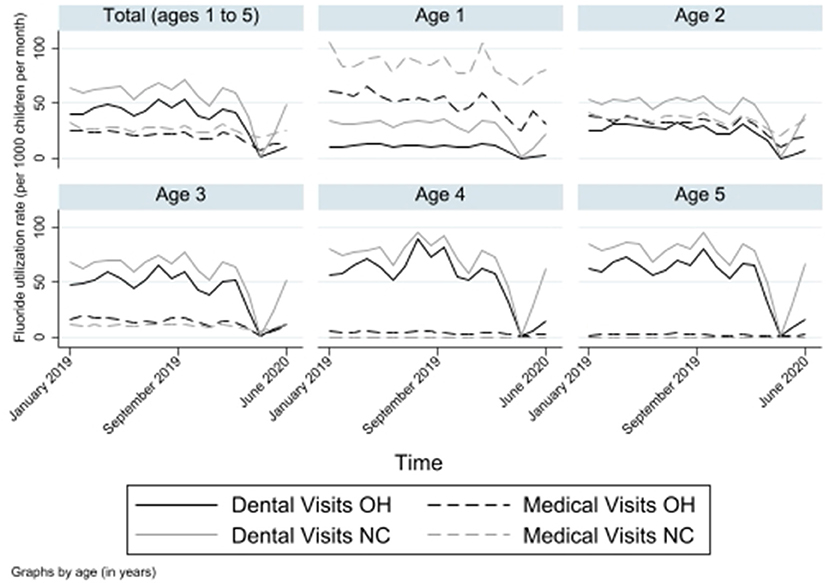
Figure 2. Monthly fluoride utilization rates at dental and medical well-child visits in Ohio (OH) and North Carolina (NC) among Medicaid-enrolled children from January 2019 to June 2020. Rates are plotted in total and by age from 1- to 5-years old. In this figure, the pandemic begins in March 2020.
Discussion
The results of this exploratory analysis highlight the importance of physician offices within the preventive oral health care safety net in two states during the first wave of the pandemic. For very young children, a physician's office may be the only source of professional oral health prevention. The sharp decrease noted in fluoride utilization rate at dental visits (75%) is especially dramatic when compared against the decline in vaccination visits among 0–2 year old children (25%) during the pandemic (22). When dental offices were closed or open only for emergency care during the early stages of the pandemic, physicians continued to provide preventive oral health care, albeit at a reduced rate, especially for 1- and 2-year old children.
Across the United States, only 8% of young children receive preventive oral health services at medical well-child visits (23). Additionally, recent analysis demonstrates that preventive oral health delivered at well-child visits complement, rather than replace, preventive dental visits (24). The two states examined in the present analysis compare favorably to the 8% reported average for preventive oral health delivered at well-child visits (Ohio = 6%; North Carolina = 8%) (23). Preventive oral health services at well-child visits have come a long way since their inception. While their use is increasing, a number of barriers and facilitators have provided insight to implementation. Lack of training during medical school, limited time with each patient, low reimbursement, poor implementation support, and non-integrated medical and dental records have prevented more widespread implementation, while having an office champion, implementation teams, good reimbursement policies from state public health programs, and a leader with a clear vision for how oral health will be included in the practice facilitate implementation (10, 25, 26).
The barriers noted above point to opportunities that can maximize delivery of preventive oral health services to very young children. The push toward interprofessional education and practice, as well as medical and dental integration has been well described (27–30). In addition to training physicians to provide oral health screening and apply fluoride varnish, two ideas that have been implemented at local and state levels include co-located services and care coordination. Colocation can facilitate many aspects of care coordination, particularly if the staffing model is optimized to use each workforce member to the highest level of their degree. Several versions of colocation models are available depending on state regulations governing the practice of dentistry and dental hygiene. Proposed models would include (1) the medical office hires a dental hygienist, (2) the dental hygienist practices independently, or (3) the dental hygienist serves as a spoke from a dentist-operated hub clinic (29). Colocation also demands full time staff from both professions so patients have continuous access to the elements of the medical and dental home. With the right staffing model and referral relationships, teledentistry workflows can farther facilitate colocation and care coordination (18). These innovative delivery models need support from reimbursement mechanisms, and as an accountable care organization, Partners for Kids may be able to engage its participating providers in different incentive plans based on performance against benchmark quality measures.
The implications of these findings must be considered in the context of barriers that families face as a result of the pandemic. In the dental office, many practices are asking fewer family members attend dental visits to maintain physical distancing recommendations. This may mean families with multiple children have to spread appointments over multiple days which can be cumbersome and subject the family to additional barriers. Whether individuals have new fears of getting sick, are burdened by school closures or looking after high-risk family members, or have become unemployed, the pandemic has altered how we interact with the health care system. For oral health, these changes are paradigm altering, and building collaborative relationships and care networks whether through referrals or telehealth consultations will become increasingly important. Interprofessional collaboration between non-dental medical and dental providers is critical. If infant oral health is to become the next great dental public health achievement (31), medical and dental collaborations, likely at well-child visits, will become a backbone of progress.
The present analysis was limited in scope. Differences in Medicaid administration, provider participation, training, and reimbursement, as well as state regulatory responses to the pandemic could partially explain the results. This analysis compared two different state-run health care systems, with system-level factors affecting medical well-child visits, dental visits, and preventive oral health service delivery. The pre-pandemic time period (January 2019–March 2020) also differs from the pandemic time period (April 2020–June 2020). Although visit utilization rates per 1,000 children per quarter were used for analysis, well-child visits and family engagement with medical and dental care may differ between the two time periods. The data and subsequent analysis could not assess the impact of the pandemic on dental outcomes or the quality of preventive oral health services provided at well-child visits. As aggregate data, the specific characteristics of the children receiving fluoride at dental visits and well-child visits could not be compared. The cost of personal protective equipment may play a more critical role in economic evaluations of early preventive oral health visits, but costs were not included in the present analysis. Conclusions from claims analysis are limited to system users, both participating providers and beneficiary users. The present analysis did not include specific provider or beneficiary data. Despite these limitations, the findings presented here underscore the importance of well-child visits in the preventive oral health safety net. Among the chaos imposed by the pandemic, fluoride utilization at well-child visits served as the primary source of preventive oral health for many young children.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
Author Contributions
BM was responsible for the study design, data collection, analysis, and interpretation, and manuscript preparation. DD was responsible for the data interpretation and manuscript preparation. BM and DD agree to be accountable for the content of the work. All authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The author would like to acknowledge the data and office of the Medical Director teams at Partners for Kids, and Dr. Mark Casey, Dental Officer, North Carolina Medicaid, Division of Health Benefits, North Carolina Department of Health and Human Services, for their input and insight into each program's administration.
References
1. Pitts NB, Baez RJ, Diaz-Guillory C, Donly KJ, Feldens CA, McGrath C, et al. Early childhood caries: IAPD Bangkok declaration. J Dent Child (Chic). (2019) 86:72. doi: 10.1111/ipd.12490
2. Section on Oral Health. Maintaining and improving the oral health of young children. Pediatrics. (2014) 134:1224–9. doi: 10.1542/peds.2014-2984
3. Rozier RG, Sutton BK, Bawden JW, Haupt K, Slade GD, King RS. Prevention of early childhood caries in North Carolina medical practices: implications for research and practice. J Dent Educ. (2003) 67:876–85. doi: 10.1002/j.0022-0337.2003.67.8.tb03674.x
4. Kranz AM, Rozier RG, Preisser JS, Stearns SC, Weinberger M, Lee JY. Preventive services by medical and dental providers and treatment outcomes. J Dent Res. (2014) 93:633–8. doi: 10.1177/0022034514536731
5. Taichman LS, Sohn W, Lim S, Eklund S, Ismail A. Assessing patterns of restorative and preventive care among children enrolled in Medicaid, by type of dental care provider. J Am Dent Assoc. (2009) 140:886–94. doi: 10.14219/jada.archive.2009.0282
6. Kaakko T, Skaret E, Getz T, Hujoel P, Grembowski D, Moore CS, Milgrom P. An ABCD program to increase access to dental care for children enrolled in Medicaid in a rural county. J Public Health Dent. (2002) 62:45–50. doi: 10.1111/j.1752-7325.2002.tb03420.x
7. Grembowski D, Milgrom PM. Increasing access to dental care for Medicaid preschool children: the Access to Baby and Child Dentistry (ABCD) program. Public Health Rep. (2000) 115:448–59. doi: 10.1093/phr/115.5.448
8. Craig MH, Scott JM, Slayton RL, Walker AL, Chi DL. Preventive dental care use for children with special health care needs in Washington's Access to Baby and Child Dentistry program. J Am Dent Assoc. (2019) 150:42–48. doi: 10.1016/j.adaj.2018.08.026
9. Chi DL, Momany ET, Mancl LA, Lindgren SD, Zinner SH, Steinman KJ. Dental homes for children with autism: a longitudinal analysis of Iowa Medicaid's I-smile program. Am J Prev Med. (2016) 50(5):609–15. doi: 10.1016/j.amepre.2015.08.022
10. Kranz AM, Ross R, Sorbero M, Kofner A, Stein BD, Dick AW. Impact of a Medicaid policy on preventive oral health services for children with intellectual disabilities, developmental disabilities, or both. J Am Dent Assoc. (2020) 151:255–64. doi: 10.1016/j.adaj.2019.12.001
11. Blackburn J, Morrisey MA, Sen B. Outcomes associated with early preventive dental care among Medicaid-enrolled children in Alabama. JAMA Pediatr. (2017) 171:335–41. doi: 10.1001/jamapediatrics.2016.4514
12. Bhaskar V, McGraw KA, Divaris K. The importance of preventive dental visits from a young age: systematic review and current perspectives. Clin Cosmet Investig Dent. (2014) 6:21–7. doi: 10.2147/CCIDE.S41499
13. Meyer BD, Wang R, Steiner MJ, Preisser JS. The effect of physician oral health services on dental use and expenditures under general anesthesia. JDR Clin Trans Res. (2020) 5:146–55. doi: 10.1177/2380084419870128
14. Thompson CL, McCann AL, Schneiderman ED. Does the Texas first dental home program improve parental oral care knowledge and practices? Pediatr Dent. (2017) 39:124–9.
15. Zilversmit L, Kane DJ, Rochat R, Rodgers T, Russell B. Factors associated with receiving treatment for dental decay among Medicaid-enrolled children younger than 12 years of age in Iowa, 2010. J Public Health Dent. (2015) 75:17–23. doi: 10.1111/jphd.12066
16. Pierce KM, Rozier RG, Vann WF. Accuracy of pediatric primary care providers' screening and referral for early childhood caries. Pediatrics. (2002) 109:E82–2. doi: 10.1542/peds.109.5.e82
17. Beil H, Rozier RG, Preisser JS, Stearns SC, Lee JY. Effects of early dental office visits on dental caries experience. Am J Public Health. (2014) 104:1979–85. doi: 10.2105/AJPH.2013.301325
18. Brian Z, Weintraub JA. Oral health and COVID-19: increasing the need for prevention and access. Prev Chronic Dis. (2020) 17:200266. doi: 10.5888/pcd17.200266
19. Santoli JM, Lindley MC, DeSilva MB, Kharbanda EO, Daley MF, Galloway L, et al. Effects of the COVID-19 Pandemic on routine pediatric vaccine ordering and administration—United States, 2020. MMWR Morb Mortal Wkly Rep. (2020) 69:591–3. doi: 10.15585/mmwr.mm6919e2
20. Macy ML, Huetteman P, Kan K. Changes in primary care visits in the 24 weeks after COVID-19 stay-at-home orders relative to the comparable time period in 2019 in metropolitan Chicago and Northern Illinois. J Prim Care Community Health. (2020) 11:1–7. doi: 10.1177/2150132720969557
21. Moyer VA. Prevention of dental caries in children from birth through age 5 years: US preventive services task force recommendation statement. Pediatrics. (2014) 133:1–10. doi: 10.1542/peds.2014-0483
22. Whaley CM, Pera MF, Cantor J, Chang J, Velasco J, Hagg HK, et al. Changes in health services use among commercially insured US populations during the COVID-19 pandemic. JAMA Netw Open. (2020) 3:e2024984. doi: 10.1001/jamanetworkopen.2020.24984
23. Geiger CK, Kranz AM, Dick AW, Duffy E, Sorbero M, Stein BD. Delivery of preventive oral health services by rurality: a cross-sectional analysis. J Rural Health. (2019) 35:3–11. doi: 10.1111/jrh.12340
24. Kranz AM, Rozier RG, Stein BD, Dick AW. Do oral health services in medical offices replace pediatric dental visits? J Dent Res. (2020) 99:891–7. doi: 10.1177/0022034520916161
25. Bernstein J, Gebel C, Vargas C, Geltman P, Walter A, Garcia RI, et al. Integration of oral health into the well-child visit at federally qualified health centers: study of 6 clinics, August 2014–March 2015. Prev Chronic Dis. (2016) 13:E58. doi: 10.5888/pcd13.160066
26. Quinonez RB, Kranz AM, Lewis CW, Barone L, Boulter S, O'Connor KG, et al. Oral health opinions and practices of pediatricians: updated results from a national survey. Acad Pediatr. (2014) 14:616–23. doi: 10.1016/j.acap.2014.07.001
27. Clark M, Quinonez R, Bowser J, Silk H. Curriculum influence on interdisciplinary oral health education and practice. J Public Health Dent. (2017) 77:272–82. doi: 10.1111/jphd.12215
28. Forbes J, Sierra T, Papa J. Advancing oral health knowledge and attitudes of physician assistant students using the smiles for life oral health curriculum. Fam Med. (2018) 50:775–8. doi: 10.22454/FamMed.2018.435186
29. Braun PA, Cusick A. Collaboration between medical providers and dental hygienists in pediatric health care. J Evid Based Dent Pract. (2016) 16(Suppl.):59–67. doi: 10.1016/j.jebdp.2016.01.017
30. Atchison KA, Weintraub JA, Rozier RG. Bridging the dental-medical divide: case studies integrating oral health care and primary health care. J Am Dent Assoc. (2018) 149:850–8. doi: 10.1016/j.adaj.2018.05.030
Keywords: Medicaid, dental public health, primary care, fluoride, pediatric dentistry, health services research, coronavirus, early childhood
Citation: Meyer BD and Danesh DO (2021) The Impact of COVID-19 on Preventive Oral Health Care During Wave One. Front. Dent. Med. 2:636766. doi: 10.3389/fdmed.2021.636766
Received: 02 December 2020; Accepted: 15 January 2021;
Published: 03 February 2021.
Edited by:
June Heather Nunn, Dublin Dental University Hospital, IrelandReviewed by:
Robert Schroth, University of Manitoba, CanadaArthur Musakulu Kemoli, University of Nairobi, Kenya
Copyright © 2021 Meyer and Danesh. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Beau D. Meyer, bWV5ZXIuNzgxQG9zdS5lZHU=
 Beau D. Meyer
Beau D. Meyer David O. Danesh
David O. Danesh