- 1Endodontics and Restorative Dentistry, Graduate School of Dental Medicine, University of Siena, Siena, Italy
- 2Graduate School of Dental Medicine, University of Siena, Siena, Italy
- 3Faculty of Dentistry, University of Siena, Siena, Italy
- 4Department of Restorative Dentistry and Endodontics, Faculty of Dental Medicine, Lebanese University, Beirut, Lebanon
- 5Tuscan School of Dentistry, University of Siena, Siena, Italy
- 6Endodontics and Restorative Dentistry, Faculty of Dentistry, University of Siena, Siena, Italy
Introduction: The aim of this study was to compare the effect of two different access cavity designs on fracture strength of endodontically treated teeth and on cyclic fatigue resistance of Reciproc blue instruments.
Methods: Forty (40) maxillary central incisor teeth and forty (40) upper first premolars were selected and divided into 4 groups (n = 20/group): Group 1A, incisors prepared with conservative access cavity (CEC); group 1B, incisors prepared with traditional access cavity (TEC); group 2A, premolars prepared with CEC; group 2B, premolars prepared with TEC. After access cavity preparation, all teeth were endodontically treated, restored, and then loaded to fracture. A total of 80 Reciproc blue R25 files were used for root canal shaping and then tested for cyclic fatigue. Normality of data distribution was evaluated by Kolmogorov-Smirnov test. Data were statistically analyzed by Independent T-test and the significance level was set at p < 0.05.
Results: No statistically significant differences in fracture strength were found between the two tested access cavities both for incisors (P = 0.70) and premolars (0.422). Cyclic fatigue resistance of Reciproc blue R25 was significantly reduced in endodontically treated teeth with CEC (P < 0.001).
Conclusions: Within the limits of the present in vitro study, CEC does not increase fracture strength of endodontically treated teeth in comparison to TEC. Conservative Endodontic Cavity causes more cyclic fatigue of Reciproc blue R25 than Traditional Endodontic Cavity.
Introduction
Endodontically treated teeth (ETT) are more exposed to fracture risk than vital teeth during function (1–3). The goal of an endodontic treatment is to eliminate microorganisms from the root canal system while preserving as much dental substance as possible. The interest for the preservation of dental tissues in order to reduce the incidence of post-operative fractures inspired new trends oriented on the realization of minimal and extremely conservative endodontic access cavities.
Minimally invasive endodontics requires operator skills, in-depth knowledge of root canal anatomy, constant professional updating and the aid of instruments such as magnification systems, ultrasonic-assisted preparation technique, modern bur designs and file systems (4). Some Authors (5) proposed a new access cavity model respecting the minimally invasive dentistry concept, limiting the removal of peri-cervical, peri-cingular dentin, and part of the pulp chamber roof: the conservative (or contracted) access cavity (CEC). Many endodontists emphasized this concept by creating innovative models of access cavity design: the ninja access (NEC) and the truss access (TREC). NEC is based on opening a small hole oriented to the center of the pulp chamber from which all root canal treatment is carried out. TREC consists of a very small hole in correspondence of every single root canal, maintaining a large portion of the pulp chamber roof.
A recent study by Corsentino et al. (6) showed how TREC did not increase the fracture resistance of endodontically treated molars compared to CEC. Other Authors provided evidence that CEC resulted in higher fracture resistance compared to the traditional access cavity design (TEC) (7). However, a contracted cavity could create a non-linear access to root canals with a consequent increased fatigue of Ni-Ti instruments (8). There is no clear evidence concerning the impact of minimally invasive techniques on success rate of ETT; moreover, information about the fatigue resistance of instruments used to shape root canals with different cavity access designs is lacking. However, shaping root canal of teeth treated with TECs seems to lead to a better preservation of root canal geometry compared to CECs, particularly at the apical level (9).
A widely discussed clinical aspect regarding survival of ETT refers to the influence of the remaining residual coronal substance. Different authors found an increase in fracture strength of ETT with the increase of residual dentin height (10, 11); moreover, cavity wall thickness and width are related to teeth/restorations survival (12).
This study evaluated the fracture strength of endodontically treated maxillary central incisors and premolars with CEC and TEC and compared the effect of the two access cavity designs on fatigue resistance of Reciproc blue R25. The null hypothesis tested H0 was that there were no statistically significant differences on fracture strength of teeth treated with the two types of access cavity, and on fatigue resistance between the instruments used to shape teeth with CEC and TEC, respectively.
Materials and Methods
Teeth Collection and Selection
After local ethics approval and patients' informed consent, 40 recently human intact central maxillary incisors and 40 upper first premolars extracted for periodontal reasons were selected for the study. The exclusion criteria were the presence of caries, previous restorations, or visible fracture lines or cracks.
Bucco-lingual and mesio-distal dimensions of each crown were measured with the use of a Digital Caliper (Digimatic 500; Mitutoyo, Kanagawa, Japan); the cervico-incisal/cervico-occlusal dimensions were taken on all 4 sides of the crown for each tooth. In order to standardize the experimental procedure, central maxillary incisors with similar MD (6.72 ± 0.49 mm) and BL (6.07 ± 0.80 mm) dimensions at the cervical line and similar root length (12.59 ± 0.82 mm) and premolars with similar MD (5.84 ± 0.96 mm) and BL (7.84 ± 0.66 mm) dimensions at the cervical line and similar root length (14.18 ± 1.03 mm) were included in the present study.
Teeth were subsequently assigned to 4 test groups (n = 20):
Group 1A: maxillary incisors with conservative access cavity (CEC)
Group 1B: maxillary incisors with traditional access cavity (TEC)
Group 2A: upper first premolars with conservative access cavity (CEC)
Group 2B: upper first premolars with traditional access cavity (TEC)
A point of reference for each tooth was determined with teeth measurements and x-ray observation.
Samples were stored in saline solution (0.9%) at a temperature of 37°C to prevent dehydration until preparation.
Samples Preparation
In groups 1A and 2A teeth were prepared with CEC. In maxillary incisors, penetration was performed using a diamond bur (No.#12, Coltene) slightly above the cingulum area, with an initial inclination of the bur of ~45°, identifying the point of reference for each tooth on the palatal surface. Penetration of the bur was done up to the breaking of the chamber roof and root canal orifice location, with no subsequent correction of its inclination. The punctiform cavities obtained were slightly enlarged with the same bur in order to make them compatible with the instrument insertion, without the removal of coronal interferences (Figure 1). In upper premolars, penetration was performed using a diamond bur (No.#12, Coltene) until the breakthrough of the pulp chamber roof, with no subsequent removal of coronal interferences represented by dentinal triangles, obtaining slightly oval shaped minimal cavities (Figure 2A). Considering that the maximum diameter of Reciproc R25 is 1.05 mm (at the end of the working portion), size 1.2 mm was chosen as the minimum CECs diameter of the oval access for premolars and of the circular access for incisors, in order to allow free access of Reciproc instruments.
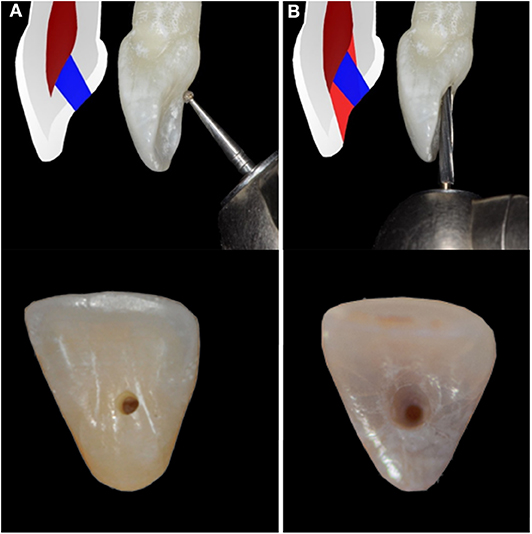
Figure 1. Opening the endodontic access cavity in maxillary incisors: in group 1 (A) conservative access cavity design was performed with the penetration of a diamond bur with an inclination of ~45°; in group 2 (B) the penetration phase was followed by an enlargement phase to realize traditional access cavity design (B).
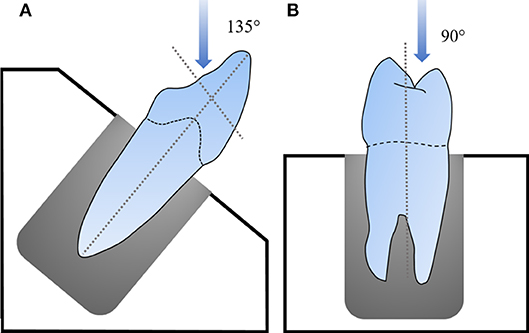
Figure 2. Example of a maxillary incisor (A) and an upper first premolar (B) positioned for the test.
TECs (groups 1B and 2B) were prepared following previously reported principles (13). In group 1B the penetration step was performed using a diamond bur (No.#12 Coltene, Whaladent, Altststten, Switzerland) mounted on a high-speed handpiece under water cooling. Access was created in the cingulum area, with an inclination of the bur of 45° and almost perpendicularly to the palatal surface up to the breaking of the chamber roof and root canal orifice location. Coronal interferences were removed using a Zekrya Endo Z bur (No.#152; Dentsply Sirona, York, USA). Also in premolars the penetration phase was followed by an enlargement phase in order to completely remove all coronal interferences and to allow a linear access to root canals. With TECs, cavities reflecting the anatomy of the pulp chamber were obtained. Access cavity preparation was performed by the same operator for all teeth.
After access cavities preparation, patency was checked for all root canals with a k-file #10.
Endodontic treatment was performed by a single operator for all teeth. Eighty new Reciproc blue R25 files (VDW GmbH, Munich, Germany) were used for endodontic treatment. Root canal shaping was performed following manufacturer's protocol. Instruments were then divided into 4 groups (n = 20):
Group 1a: instruments used for incisors with CEC
Group 1b: instruments used for incisors with TEC
Group 2a: instruments used for premolars with CEC
Group 2b: instruments used for premolars with TEC
Mechanical preparation was alternated with irrigation of 5% sodium hypochlorite solution; Root canal filling was performed according to the continuous wave of condensation technique. Restorations were realized with Prime&Bond Active Universal Adhesive (Dentsply srl Italy, Rome, IT), SDR (Dentsply Srl) as core material, and Ceram-X Duo E2 (Dentsply Srl) for the occlusal surface (2 mm).
Samples were stored in saline solution (0.9%) at a temperature of 37°C to prevent dehydration until test.
Fracture Strength Test
Teeth were positioned in an aluminum stub and embedded in self-curing resin (Gnathus cold self-curing acrylic resin; Zhermak, Badia Polesine, Italy) with the long axis perpendicular to the base of the block with the use of a parallelometer, leaving the roots exposed 2 mm apically from the CEJ to evaluate the type of fracture (14). A universal loading machine (Triaxal Tester T400 Digital; Controls Srl, Cernusco, Italy) was used. Incisors were inserted into the holding device with an inclination of 135° in relation to the horizontal plane and pressure was applied in correspondence of the peri-cingular area (Figure 2A). Premolars were inserted into the holding device perpendicularly to the horizontal plane; pressure of the rod tip was applied 2 mm from the apex of the palatal cusp in direction of the central fossa (Figure 2B) in order to simulate an occlusal vertical load. A controlled load was applied with a stainless steel rod with a tip diameter of 2 mm at a crosshead speed of 1 mm/min. All samples were loaded until fracture, and the maximum breaking load was recorded in Newton (N).
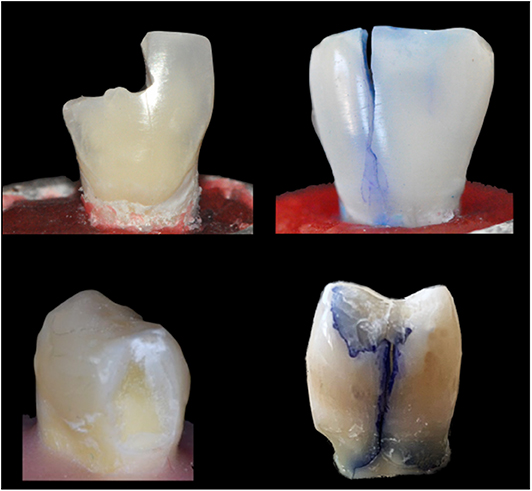
After the test, the specimens were observed under a stereomicroscope (SZR-10; Optika SRL, Ponetranica, Italy) at 80x to evaluate the type of fracture. Fractures were highlighted using an aqueous methylene blue solution (1%) and divided into: favorable (F), when involving the coronal portion without crossing the CEJ; unfavorable (UF), when involving the root (Figure 3).
Cyclic Fatigue Test
Reciproc blue R25 files were subjected to cyclic fatigue test after their use. The test was performed using a custom-made device which allowed a reproducible simulation of an instrument confined in a curved canal (15) with 60° angle of curvature and 5 mm radius of curvature to the center of the 1.5 mm wide canal. It ensured three dimensional alignment and positioning of all instruments at 19 mm in length. To reduce friction between instruments and metal canal walls, synthetic Oil WD-40 (WD 40 Company, San Diego, CA, USA) was sprayed into the artificial canal. Reciprocating movement was activated in an endodontic micromotor (X-SMART Plus; Dentsply Maillefer, Ballaigues, Switzerland) using RECIPROC ALL as a setting.
To eliminate the error related to the operator's reaction time, the procedure was recorded and timed on the video.
Statistical Analysis
Quantitative variables were expressed as mean (standard deviation) and Confidence Interval (95%). Normality distribution of data was tested according to Shapiro-Wilks's Test. Student t-test was performed to find significant differences between two independent groups. Homogeneity of variances was tested with the Levene's test and in the case of heteroscedasticity the Welch statistics were used. All analyses were performed using the SPSS software (v.20), setting the level of significance at p ≤ 0.05.
Results
No statistically significant differences were found between the two access cavity designs tested for fracture strength of endodontically treated maxillary central incisors (p = 0.70) and upper first premolars (p = 0.422); slightly higher values were observed in group 1A and 2A, treated with CEC (Tables 1, 2).
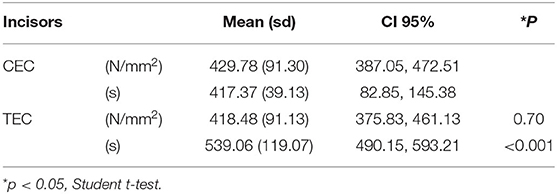
Table 1. Distribution of fracture strength values (N/mm2) and time of fracture variable(s) variable within groups (mean, sd, CI 95%).
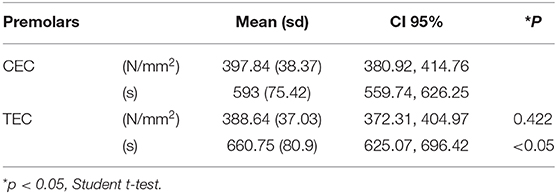
Table 2. Distribution of fracture strength values (N/mm2), time of fracture variable (s) within groups (mean, sd, CI 95%).
Occurrence frequency of each failure pattern was detected and calculated as percentage. In group 1A, favorable fractures occurred in 66% of cases, in group 1B favorable fractures occurred in 25% of cases; in group 2A favorable factures occurred in 80% of cases and in group 2B in 70% of cases. Statistically significant differences were observed between groups 1a and 1b (P < 0.001) and between groups 2a and 2b (P < 0.05) for cyclic fatigue resistance values. A significantly higher mean time to fracture was registered for instruments of groups 1b and 2b.
Discussion
The aim of this study was to evaluate how a conservative access (CEC) cavity could influence the fracture resistance of endodontically treated maxillary incisors and first premolars, and the cyclic fatigue resistance of Reciproc blue instruments. No significant differences were observed between the two different cavity designs for fracture strength of the two type of teeth tested, but cyclic fatigue resistance of instruments used with CEC was significantly lower. The null hypothesis tested H0 was partially rejected because, although the two types of access cavities did not affect the fracture strength of endodontically treated teeth, they influenced the fatigue resistance of endodontic instruments.
An ideal access cavity should guarantee the complete removal of the pulp chamber and the cleansing, shaping, filling of the canals. An excessive reduction of the access cavity size, however, could interfere with an adequate canal shaping and obturation (16); at the same time a too extensive access cavity and, therefore, an extensive removal of healthy tooth tissue, has been demonstrated to reduce fracture resistance (6, 17).
Consequently, conservative endodontic access cavity preparation (CEC) was proposed to preserve tooth structure maximally (18, 19). Literature has not yet well-defined answers that can lead us to approach these new trends in total safety. There are conflicting opinions regarding the fracture resistance of ETT prepared with size-reduced endodontic access cavities: some researchers showed how a conservative approach increased the strength of treated teeth, compared to a traditional approach (5, 14); other studies did not find significant differences (20, 21). Although minimal invasive intervention has been embraced in some area of dentistry (20), the CEC concept in endodontics has largely been opposed because it poses challenge not encountered with TECs.
The literature provides only one study (14) investigating fracture strength of maxillary incisors treated with CECs and TECs with which compare the results of this study. In this previous study the mean fracture load values were 1134.6 ± 109.2 N for CEC and 1305.2 ± 97.6 N for TEC, which are considerably greater than those recorded in the current study (429.78 ± 91.30 N for CEC and 418.48 ± 91.13 N for TEC). However, both studies concluded that CECs did not influence biomechanical behavior of anterior ETT, this is maybe because performing CECs in maxillary incisors determined a minimum coronal dentin conservation compared to TECs. Although dentin conservation was greater for CECs performed in premolars (14), the absence of significant difference between the two cavitary designs in terms of bond strength is maybe related to the maintenance, in both cases, of the two marginal ridges; marginal ridges of at least 2 mm thickness represent a reinforcing factor and their loss represents a risk factor for tooth fracture (22).
Different studies investigated the influence of endodontic access cavity design on fracture resistance of posterior ETT (6, 7, 20, 21, 23, 24), and also fracture strength values recorded for upper premolars in the current study are a little lower compared with those obtained in previous studies (7, 23).
This discrepancy in results is maybe due of different methodology features. There are no exact rules to prepare the CEC; the aim is to preserve as much as possible tooth structure and to locate the canal orifices. Furthermore, in this study a small 2 mm diameter ball herein was used for load test; with a larger diameter (7, 23) a greater force is needed to generate the critical pressure required to fracture the tooth.
Another important aspect is the type of fracture of ETT: previous studies revealed a higher frequency of vertical fractures (25, 26), most of them in the root area, reducing the possibility to save the teeth (25).
In the present study, a higher percentage of restorable fractures related to CEC was observed both in maxillary central incisors and first upper premolars; this is in agreement with other studies which related the volume of dentin removal with the increase probability of vertical fractures (26). Literature presents contradictory results also regarding root canal shaping of ETT with contracted access cavities. In fact, some authors (20) showed that small cavities did not interfere with shaping effectiveness and with the biomechanical characteristics of endodontically treated teeth; others (14) found substantial differences in root canal shaping of teeth with different sizes of access cavity design. The embedding of teeth was performed with the use of an acrylic self-curing resin according to previous studies (6, 20), other studies (27–29) used in addition a cushion material to simulate periodontal ligament and tooth mobility and also to amortize the load.
Other aspects should be considered, such as the increased separation risk of Ni-Ti instruments during canal preparation (30).
A study of Yahata et al. (31), conducted on 3D reproductions of maxillary central incisors, highlighted how an incisal shifted access cavity (similar to TEC) significantly reduces the percentage of iatrogenic damage such as apical transportation compared to a traditional lingual access (similar to CEC). These minimally invasive cavities actually managed to preserve more healthy dental tissue, but they could make the procedures of root canal treatment more difficult and less predictable.
The second part of this study revealed a lower cyclic fatigue resistance of Reciproc blue R25 used to shape CEC cavities compared to instruments used to shape TEC cavities. The results obtained can be explained with the absence of a straight access to canals orifices (32). Ni-Ti instruments touched a large area of root dentin and residual chamber roof; the torque generated during canal shaping proportionally increased to the increase of the contacted surface (33), thus reducing fatigue resistance of endodontic instruments. These results are in disagreement with a previous study (20) which detected no instrumentation efficacy risk associated with CECs in maxillary molars, but the authors suggested a careful application of CECs in these teeth presenting a particularly challenging root canal system.
The results of cyclic fatigue test could also be related to the type of instrument used. Yared in (34) proposed a single Ni-Ti instrument with reciprocating motion for clinical use. Reciprocating instruments are less subjected to torsional fracture because rotation angles are lower than “deflection angles,” defined as the maximum amount of rotation that an instrument can withstand before it exceeds its elastic limit and fails in torsional mode. Reciprocating instruments complete a 360° rotation in several movement cycles, minimizing the risk of “taper lock” (35). Many authors (36–38) have shown that alternate rotation increases the cyclic fatigue resistance about six times compared to continuous rotation. The number of cycles performed before separation during a test is cumulative and related to the stress intensity generated by compression/tension forces the curved portion of the canal (39). Many studies have shown that fracture time is also related to the rotation speed of the instrument. Although the rotational speed of the continuous rotation systems is lower than that of modern reciprocating systems (280 rpm against 300 rpm of the Reciproc system), reciprocating speed is not constant. The acceleration and deceleration process in both directions of rotation generates less stress on the instrument, providing greater resistance to cyclic fatigue. In addition, as observed by Gavini et al. (40), “Reciprocal All” mode accomplishes 10 cycles of reciprocating motion at the second and 3.33 revolutions per second. So the speed when reciprocating files are used is lower that the one indicated by the manufacturer's instructions.
In teeth presenting a complex root anatomy endodontic instruments are exposed to higher stress (33). Therefore, it should be advisable to realize traditional endodontic access cavities, rather than conservative ones. It is possible that CEC access hampers an adequate cleansing and disinfection of the root canal system, but no evidence is available yet (41).
Endodontic procedures must be planned according to a minimally invasive approach. The quantity of the residual tooth substance plays a fundamental role in the fracture resistance of ETT. An ideal access cavity should be minimally invasive but should allow adequate and safe cleaning, shaping and filling of the root canal system. A tooth that needs an endodontic treatment is probably a tooth with extensive carious lesion, fracture or previous restoration, therefore from a clinical point of view in most cases the shape and extent of the endodontic access cavity are guided by different factors and it is not always possible to perform extremely contracted access cavities.
The limitations of this study should be considered. The impossibility to assess the overall restorative scenarios ex vivo is due to the fact that clinical conditions cannot be simulated identically in vitro.
In this experimental study load was applied to upper central incisors at an angle of 135° from the longitudinal axis, considering both the mean values of the interincisal angle and the incisal guide (42), and a vertical occlusal load was applied to upper premolars. Teeth are normally subjected to a dynamic load: a continuous load as in maximum intercuspation and a cyclic load as in chewing (43); furthermore, load is transmitted in different directions. In case of malocclusion or parafunctions, the load is distributed differently than in physiological condition. In this study only a single direction load was examined.
Another aspect to take into account is the endodontic file used for canals shaping. In the present ex vivo study, all maxillary central incisors were shaped with Reciproc R25. Given the mean diameter at the apex of maxillary central incisors, R25 would not be the best clinical choice in order to remove the whole dentin layer in the apical region (44). On the other hand, teeth included in the present study were extracted for periodontal or orthodontic reasons. As a previous study demonstrated, the incidence of pulpal calcifications of periodontally involved teeth was 62% in histological and 30% in radiographic examinations (45). The incidence of calcified canals also correlates with age: almost all central incisors included in this study were extracted for periodontal reasons in subjects of age >60 years. Moreover, the emergence of necrotic tissue remnants can cause the formation of dystrophic calcifications in tissues that are susceptible to deposits of calcium (46). These calcifications cause a reduction in the root canal lumen.
Another point to take into account is the time lapse between the extraction and the analysis. The collection of 40 intact central maxillary incisors with similar MD and BL dimensions and similar root length, with no previous restorations or endodontic treatment, took months to complete. Therefore, although all teeth were stored in saline solution at 37°C before use, the time between the extraction and the laboratory phases was not the same for all teeth. For the above-mentioned reasons, Reciproc R25 was selected to shape the root canal of all extracted central maxillary incisors included in this study, in order to standardize the protocol.
Further in vitro and in vivo studies on anterior teeth, including various loading conditions, are necessary to confirm the results of this study and to evaluate all aspects involved in the use of contracted access cavities before recommending their use in daily clinical practice.
Within the limits of this in vitro study, we concluded that contracted endodontic access cavities do not represent a valid alternative to traditional endodontic access cavities, since they don't increase fracture resistance of endodontically treated teeth. Moreover, they also lead to greater cyclic fatigue of Reciproc blue R25 instruments compared to a traditional access cavity design.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by Comitato Etico Regione Toscana Area Vasta Sud Est (C.E.A.V.S.E). The patients/participants provided their written informed consent to participate in this study.
Author Contributions
VS participated in the experimental design, performed the experiments, performed statistical analysis, and wrote the manuscript. CM participated in the experimental design, wrote, and proofread the manuscript. DM participated in the experimental design and performed the experiments. MM and HO participated in the experimental design and proofread the manuscript. SG participated in the experimental design, supported the experiments, and proofread the manuscript. All authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. Reeh ES, Messer HH, and Douglas WH. Reduction in tooth stiffness as a result of endodontic and restorative procedures. J Endod. (1989) 15:512–16. doi: 10.1016/S0099-2399(89)80191-8
2. Tamse A, Fuss Z, Lusting J, and Kaplavi J. An evaluation of endodontically vertically fractured teeth. J Endod. (1999) 7:506–8. doi: 10.1016/S0099-2399(99)80292-1
3. Ferrari M, Mason PN, Goracci C, Pashley DH, and Tay FR. Collagen degradation in endodontically treated teeth after clinical function. J Dent Res. (2004) 83:414–9. doi: 10.1177/154405910408300512
4. Bürklein S, and Schäfer E. Minimally invasive in endodontics. Quintessence Int. (2015) 46:119–24. doi: 10.3290/j.qi.a33047
5. Clark D, and Khademi J. Modern molar endodontic access and directed dentin conservation. Dent Clin North Am. (2010) 54:249–73. doi: 10.1016/j.cden.2010.01.001
6. Corsentino G, Pedullà E, Castelli L, Liguori M, Spicciarelli V, Martignoni M, et al. Influence of access cavity preparation and remaining tooth substance on fracture strength of endodontically treated teeth. J Endod. (2018) 44:1416–21. doi: 10.1016/j.joen.2018.05.012
7. Plotino G, Grande NM, Isufi A, Ioppolo P, Pedullà E, Bedini R, et al. fracture strength of endodontically treated teeth with different access cavity designs. J Endod. (2017) 43:995–1000. doi: 10.1016/j.joen.2017.01.022
8. Alapati SB, Brantley WA, Svec TA, Powers JM, Nusstein JM, Daehn GS, et al. SEM observations of nickel-titanium rotary endodontic instruments that fractured during clinical use. J Endod. (2005) 31:40–3. doi: 10.1097/01.DON.0000132301.87637.4A
9. Alovisi M, Pasqualini D, Musso E, Bobbio E, Giuliano C, Mancino D, et al. Influence of contracted endodontic access on root canal geometry: an in vitro study. J. Endod. (2018) 44:614–20. doi: 10.1016/j.joen.2017.11.010
10. Santos Pantaleón D, Morrow BR, Cagna DR, Pameijer CH, and Garcia-Godoy F. Influence of remaining coronal tooth structure on fracture resistance and failure mode of restored endodontically treated maxillary incisors. J Prosthet Dent. (2018) 119:390–6. doi: 10.1016/j.prosdent.2017.05.007
11. Skupien JA, Luz MS, and Pereira-Cenci T. Ferrule effect: a meta-analysis. JDR Clin Trans Res. (2016) 1:31–9. doi: 10.1177/2380084416636606
12. Chai H, and Lawn BR. Fracture resistance of molar teeth with mesial-occlusal-distal (MOD) restorations. Dent Mater. (2017) 33:e283–9. doi: 10.1016/j.dental.2017.04.019
13. Ingle JI. Endodontic cavity preparation. In: Ingle J, Tamber J, editors. Endodontics. 3rd ed. Philadelphia, PA: Lea & Febiger (1985). p. 102–67.
14. Krishan R, Paquè F, Ossareh A, Kishen A, Dao T, and Friedman S. Impact of conservative endodontic cavity on root canal instrumentation efficacy and resistance to fracture assessed in incisors premolars and molars. J Endod. (2014) 40:1160–6. doi: 10.1016/j.joen.2013.12.012
15. Plotino G, Grande NM, Mazza C, Petrovic R, Testarelli L, and Gambarini G. Influence of size and taper of artificial canals on the trajectory of NiTi rotary instruments in cyclic fatigue studies. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. (2010) 109:e60–6. doi: 10.1016/j.tripleo.2009.08.009
16. Soares PV, Souza PG, Souza SC, de Queiroz Gonzaga RC, Faria VLG, de Lima Naves MF, et al. Effects of non-carious lesions coronary structure loss association on biomechanical behavior of maxillary premolars. J Res Dent. (2013) 1:140–53. doi: 10.19177/jrd.v1e22013140-153
17. Pereira JR, McDonald A, Petrie A, and Knowles JC. Effect of cavity design on tooth surface strain. J Prosthet Dent. (2013) 110:369–75. doi: 10.1016/j.prosdent.2013.08.004
18. Murdoch-kinch CA, and McLean ME. Minimally invasive dentistry. J Am Dent Assoc. (2003) 134:87–95. doi: 10.14219/jada.archive.2003.0021
19. Boveda C, and Kischen A. Contracted endodontic cavities: the foundation for less invasive alternatives in the management of apical periodontitis. Endod Topics. (2015) 33:169–86. doi: 10.1111/etp.12088
20. Moore B, Verdelis K, Kishen A, Dao T, and Friedman S. Impacts of contracted endodontic cavities on instrumentation efficacy and biomechanical responses in maxillary molars. J Endod. (2016) 42:1779–83. doi: 10.1016/j.joen.2016.08.028
21. Rover G, Belladonna FG, Bortoluzzi EA, de Deus G, Silva EJNL, and Teixeira CS. Influence of access cavity design on root canal detection, instrumentation efficacy, and fracture resistance assessed in maxillary molars. J Endod. (2017) 43:1657–62. doi: 10.1016/j.joen.2017.05.006
22. Shahrbaf S, Mirzakouchaki B, Oskoui SS, and Kahnamoui MA. The effect of marginal ridge thickness on the fracture resistance of endodontically-treated, composite restored maxillary premo- lars. Oper Dent. (2007) 32:285–90. doi: 10.2341/06-83
23. Chlup Z, ŽiŽka R, Kania J, and Pribyl M. Fracture behaviour of teeth with conventional and mini-invasive access cavity designs. J Eur Ceram Soc. (2017) 37:14. doi: 10.1016/j.jeurceramsoc.2017.03.025
24. Ivanoff CS, Marchesan MA, Andonov B, Hottel TL, and Dandarov Y. Fracture resistance of mandibular premolars withcontracted or traditional endodontic access cavities and class II temporary composite restorations. Endod Pract Today. (2017) 11:4–7.
25. Lagouvardos P, Sourai P, and Douvitsas G. Coronal fractures in posterior teeth. Oper Dent. (1989) 14:28–32.
26. Shemesh H, Roeleveld AC, Wesselink PR, and Wu MK. Damage to root dentin during retreatment procedures. J Endod. (2011) 37:63–6. doi: 10.1016/j.joen.2010.10.002
27. Sterzenbach G, Kalberlah S, Beuer F, Frankenberger R, and Naumann M. In-vitro simulation of tooth mobility for static and dynamic load tests: a pilot study. Acta Odontol Scand. (2011) 69:316–8. doi: 10.3109/00016357.2011.563244
28. von Stein-Lausnitz M, Bruhnke M, Rosentritt M, Sterzenbach G, Bitter K, Frankenberger R, et al. Direct restoration of endodontically treated maxillary central incisors: post or no post at all? Clin Oral Investig. (2019) 23:381–9. doi: 10.1007/s00784-018-2446-6
29. Abduljawad M, Samran A, Kadour J, Karzoun W, and Kern M. Effect of fiber posts on the fracture resistance of maxillary central incisors with Class III restorations: an in vitro study. J Prosthet Dent. (2017) 118:55–60. doi: 10.1016/j.prosdent.2016.09.013
30. Iqbal MK, Kohli MR, and Kim JS. A retrospective clinical study of incidence of root canal instrument separation in an endodontics graduate program: a PennEndo database study. J Endod. (2006) 32:1048–52. doi: 10.1016/j.joen.2006.03.001
31. Yahata Y, Masuda Y, and Komabayashi T. Comparison of apical centring ability between incisal-shifted access and traditional lingual access for maxillary anterior teeth. Aust Endod J. (2017)43:123–8. doi: 10.1111/aej.12190
32. Fan B, Cheung GS, Fan M, Gutmann JL, and Bian Z. C-shaped canal system in mandibular second molars: part I. Anatomical features. J Endod. (2004) 30:899–903. doi: 10.1097/01.don.0000136207.12204.e4
33. Blum JY, Cohen A, Machtou P, and Micallef JP. Analysis of forces developed during mechanical preparation of extracted teeth using Profile NiTi rotary instruments. Int Endod J. (1999) 32:24–31. doi: 10.1111/j.1365-2591.1999.tb01408.x
34. Yared G. Canal preparation using only one Ni-Ti rotary instrument: preliminary observations. Int Endod J. (2008) 41:339–44. doi: 10.1111/j.1365-2591.2007.01351.x
35. Kim HC, Kwak SW, Cheung GS, Ko DH, Chung SM, and Lee W. Cyclic fatigue and torsional resistance of two new nickel-titanium instruments used in reciprocation motion: reciproc versus waveone. J Endod. (2012) 38:541–4. doi: 10.1016/j.joen.2011.11.014
36. de Deus G, Moreira EJL, Lopes HP, and Elias CN. Extended cyclic fatigue life of F2 ProTaper instrument used in reciprocating movement. Int Endod J. (2010) 43:1063–8. doi: 10.1111/j.1365-2591.2010.01756.x
37. Kiefner P, Ban M, and de-Deus G. Is the reciprocating movement per se able to improve the cyclic fatigue resistance of instruments? Int Endod J. (2014) 47:430–6. doi: 10.1111/iej.12166
38. Pedulla E, Grande M, Plotino G, Gambarini G, and Rapisarda E. Influence of continuous or reciprocating motion on cyclic fatigue resistance of 4 different nickel-titanium rotary instruments. J Endod. (2013) 39:258–61. doi: 10.1016/j.joen.2012.10.025
39. Inan U, Aydin C, Uzun O, Topuz O, and Alacam T. Evaluation of the surface characteristcs of used and new ProTaper instruments: an atomic force microscopy study. J Endod. (2007) 33:1334–7. doi: 10.1016/j.joen.2007.07.014
40. Gavini G, Caldeira CL, Akisue E, Candeiro GT, and Kawakami DA. Resistance to flexural fatigue of Reciproc R25 files under continuous rotation and reciprocating movement. J Endod. (2012) 38:684–7. doi: 10.1016/j.joen.2011.12.033
41. Silva EJNL, Rover G, Belladonna FG, de Deus G, da Silveira Teixeira C, da Silva Fidaigo TK, et al. Impact of contracted endodontic cavities on fracture resistance of endodontically treated teeth: a systematic review of in vitro studies. Clin Oral Investig. (2018) 22:109–18. doi: 10.1007/s00784-017-2268-y
42. Heydecke G, Butz F, and Strub JR. Fracture strength and survival rate of endodontically treated maxillary incisors with approximal cavities after restoration with different post and core systems: an in-vitro study. J Dent. (2001) 2:427–33. doi: 10.1016/S0300-5712(01)00038-0
43. Larson TD. Part two: the restoration of non-vital teeth: structural, biological, and micromechanical issues in maintaining tooth longevity. Northwest Dent. (2006) 85:29.
44. Mizutani T, Ohno N, and Nakamura H. Anatomical study of the root apex in the maxillary anterior teeth. J Endod. (1992) 18:344–7. doi: 10.1016/S0099-2399(06)80486-3
45. Huang LG, and Chen G. A histological and radiographic study of pulpal calcification in periodontally involved teeth in a Taiwanese population. J Dent Sci. (2016) 11:405–10. doi: 10.1016/j.jds.2016.05.001
Keywords: conservative access cavity, traditional access cavity, fracture strength, cyclic fatigue, reciprocating instruments
Citation: Spicciarelli V, Marruganti C, Marzocco D, Martignoni M, Ounsi H and Grandini S (2020) Influence of Endodontic Access Cavity Design on Fracture Strength of Maxillary Incisors and Premolars and on Fatigue Resistance of Reciprocating Instruments. Front. Dent. Med. 1:575010. doi: 10.3389/fdmed.2020.575010
Received: 22 June 2020; Accepted: 17 August 2020;
Published: 17 September 2020.
Edited by:
Paulo Cesar, University of São Paulo, BrazilReviewed by:
Nicola Scotti, University of Turin, ItalyManoel Damião Sousa Neto, University of São Paulo, Brazil
Copyright © 2020 Spicciarelli, Marruganti, Marzocco, Martignoni, Ounsi and Grandini. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Crystal Marruganti, bWFycnVnYW50aUBnbWFpbC5jb20=
 Valentina Spicciarelli
Valentina Spicciarelli Crystal Marruganti
Crystal Marruganti Dario Marzocco
Dario Marzocco Marco Martignoni3
Marco Martignoni3 Simone Grandini
Simone Grandini