
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
OPINION article
Front. Dent. Med. , 22 September 2020
Sec. Endodontics
Volume 1 - 2020 | https://doi.org/10.3389/fdmed.2020.569225
This article is part of the Research Topic The Global Response to the SARS-CoV-2 Pandemic from Endodontists and Researchers View all 9 articles
Since the initial occurrence of COVID-19 in Wuhan, China, the number of infections has escalated tremendously, prompting the World Health Organization to declare it a pandemic and an international public health emergency (1). Governments around the world have been forced to undertake extensive measures in order to combat the spread of COVID-19, whilst medical professionals carry the burden of managing affected patients. This pandemic has not only exerted an economic impact on many industries but has also affected the safety and security of healthcare personnel, amongst which include dentists and dental students.
Hong Kong is home to one of the world's leading dental schools (2). The Faculty of Dentistry at the University of Hong Kong was founded in 1982 and is the only institution that provides dental education for both undergraduate and postgraduate training in Hong Kong. Currently there are over 2,500 registered dentists in Hong Kong, amongst which 20 of them are endodontic specialists.
The Bachelor of Dental Surgery (BDS) is the undergraduate program that paves the way to the dental profession in Hong Kong. The 6-year curriculum integrates both foundational knowledge and practical skills whilst emphasizing an inquiry-based educational experience. Starting from the second year, students enter the polyclinics in Prince Phillip Dental Hospital and begin treating patients. They develop their clinical competence through a combination of simulation laboratory courses and the comprehensive management of cases with interdisciplinary treatment considerations.
After obtaining their undergraduate degree, individuals may decide that they would like to pursue specialist training to further develop their skills in a specific discipline. For endodontics, the Faculty's taught postgraduate program, the Master of Dental Surgery (MDS) in Endodontics, provides a structured and comprehensive 3-year curriculum that incorporates three components: clinical practice, research, and teaching. This constitutes the Basic Training component of the specialist training pathway in Hong Kong.
There is no doubt that COVID-19 has shaken the lives of many across the world. Hong Kong is in a particularly precarious position given its proximity to China and the many portals of entry it shares with the mainland. However, given this city's history in regard to the 2003 SARS outbreak, Hong Kong was early to adopt preventative measures in order to combat and mitigate the spread of COVID-19. In April, several months after the initial outbreak, Hong Kong was able to suppress the daily number of infected cases with several consecutive weeks of no reported incidents of local transmission. This was likely due the collective compliance of its citizens coupled with the organized effort of the Hong Kong government. However, due to the volatile nature of this pandemic, Hong Kong is currently experiencing a resurgence in COVID-19 cases. The total number of infected cases in Hong Kong surpassed 3,300 on August 1st, with 33 of those cases proving to be fatal (3). The trend of the number of confirmed COVID-19 infections in Hong Kong is shown in Figure 1.
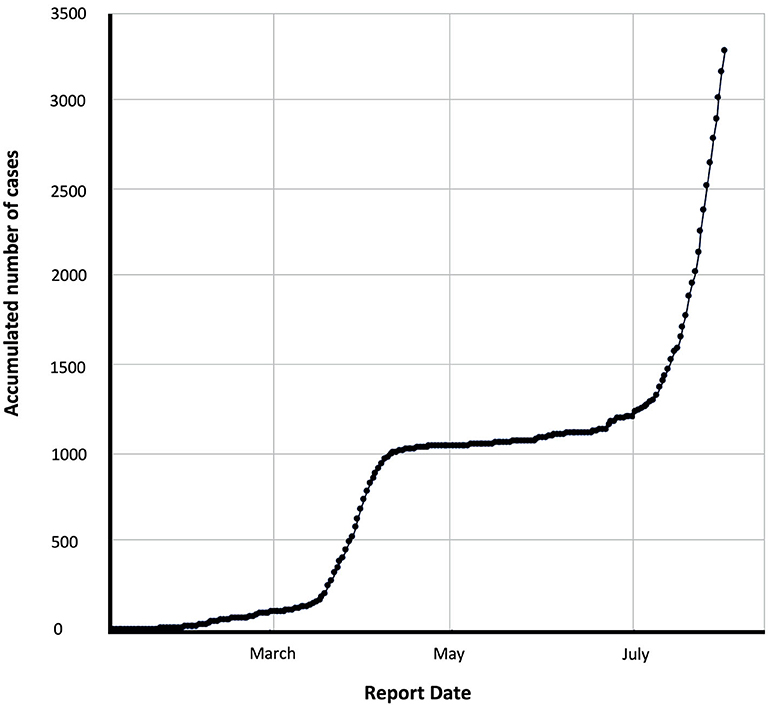
Figure 1. Number of confirmed COVID-19 infections in Hong Kong (modified from the HKSAR Government, COVID-19 Thematic Website).
The local spread of COVID-19 began with a first wave of cases of individuals traveling from Mainland China to Hong Kong in January, prompting the government to close the majority of border control points, impose 14-day quarantine orders on Hong Kong citizens who had been to Hubei province and restrict the entry of Hubei residents and non-local visitors of Hubei Province. Temperature checks and health-screening questionnaires were also enforced. Work from home orders were encouraged, major events were postposed and all primary to tertiary level educational institutes were closed. A second wave of imported cases occurred in March and was followed by more aggressive measures. All incoming Hong Kong citizens who had traveled overseas were subjected to initial COVID-19 testing and non-local travelers were denied entry into Hong Kong. Those who were found to be negative were subjected to a 14-day home or hotel quarantine whilst those who tested positive received medical attention. The government also mandated a closure of high-risk premises such as bars, gyms, and clubhouses, enforced strict social distancing measures by limiting the number of people gathered in a public space to four with exceptions for transport, work and other functions, and maintained school closures. Furthermore, contact tracing and accessible testing for suspected cases were implemented. Fourteen-day quarantine orders at designated quarantine centers were applied to those who have been in close contact with infected individuals. As the number of daily infections came to a halt, during the period of May and June the government relaxed social distancing measures permitting public gatherings of up to 50 people, allowed a gradual resumption of normal operations of the affected businesses and schools whilst implementing quarantine exemptions for a variety of personnel arriving from Mainland China and Macau such as officials on governmental duties as well as crew members of aircrafts, ships, and coaches. This saw the beginning of a gradual increase in daily reported cases of COVID-19, which was soon followed by a dramatic spike of locally transmitted infections in July. In response to this third wave, stringent policies were implemented once again, including tightened social distancing measures by limiting public gatherings to two people, a partial ban on dine-in services, compulsory mask-wearing in all indoor and outdoor public spaces, and the re-closure of high-risk premises, businesses and schools. In addition to existing quarantine measures and traveling restrictions, people arriving from several high-risk countries, including, but not limited to, India, Pakistan, the United States of America, and the Philippines, have been required to submit proof of negative test results for COVID-19 before their arrival in Hong Kong.
Although incidence of COVID-19 in Hong Kong has fluctuated since the start of the pandemic, the people of Hong Kong have largely maintained a watchful disposition. A survey found that 78.8% of Hong Kong citizens were concerned about contracting the disease. This likely fuelled the high level of cautiousness of the general public (4). It was reported that 98.8% of Hong Kong people complied with wearing a mask when in public, whilst 85.1% made a conscious effort to avoid crowded places. The comprehensive measures undertaken by the local government coupled with the collective effort of its citizens likely helped initially mitigate the more dire effects of the outbreak (5, 6). However, the recent spike in COVID-19 infections and clustered community outbreaks have been attributed to relaxed social distancing policies, an increase in social gatherings, asymptomatic spread, and transmission from imported cases (7). Furthermore, the mental and physical burn out from heightened stress levels, social isolation, and changes in routine have left many Hong Kong citizens fatigued and frustrated. This may have led to decreased alertness and compliance, which could have likewise contributed to the resurgence of infections (8).
Although early closure of schools may have helped reduce the spread of COVID-19 in Hong Kong, this has had a major impact on the education system. Dental education has been particularly affected given the importance of clinical, practical, and interactive learning.
Since late January, the majority of classes have moved online. Problem Based Learning (PBL) is a major component of the BDS curriculum and video-conferencing platforms allow for online interaction between students and facilitators. PBL enhances the ability of students to apply their dental knowledge in practical situations (9) but its effectiveness depends on student engagement. Interaction is sometimes hindered by technical difficulties and suboptimal audio and video quality. Pre-recorded video resources serve as another method to deliver information to dental students. E-learning was found to be an effective tool to enhance the learning experience (10), however, it has been reported that students considered online learning as a helpful adjunct and not a replacement for traditional educational methods (11). Despite the promise of E-learning, the one aspect of dental education that it cannot replace is the clinical skills aspect. Although instructional tutorials can offer guidance, the lack of hands-on practice may delay the development of students' manual dexterity and clinical competence.
As a result of prolonged school closures, the academic timeline has undergone several modifications. BDS examinations have been postponed until August and final year students may be required to attend several more months school in order to accumulate sufficient clinical experience before graduating. The examination requirements for graduating batches of dental students have been amended to take into consideration the impact of polyclinic closures. Some examinations will also take place online in order to maintain social distancing and accommodate international students who are unable to return to Hong Kong due to traveling restrictions. For example, students studying their MDS in Endodontics will be required to complete an online assessment followed by a presentation to the examiners.
Following the relaxation of government protocols in June, face-to-face and clinical teaching have partially resumed. Polyclinics are operating at a reduced capacity whilst the number of students per clinical session is strictly limited in order to maintain adequate social distancing. Clinical sessions have been arranged so that senior undergraduate and postgraduate students are prioritized. Precautionary protocols enforced in the endodontic postgraduate clinic include pre-treatment antiseptic mouth rinse, sodium hypochlorite disinfection of the rubber dam surface, mandatory high-volume suction during all restorative procedures and minimal use of aerosol generating instruments. Furthermore, all students and staff members of the Faculty are required to undergo weekly COVID-19 testing.
The outbreak of COVID-19 has prompted private clinics to undertake self-imposed limitations to the scope of practice or to cease operations all together. However, urgent cases are still seen with the aim to provide temporary pain relief measures for patients in need. In Hong Kong, more than 60% of adults visit the dentist only when they have symptoms such as toothaches or pain disturbing sleep (12). Endodontic diseases are indeed one of the more common dental problems affecting the general public (13) and because pains of pulpal and/or endodontic origin are often severe and acute (14), endodontic treatment becomes very relevant during this time as urgent dental care is given priority.
Dental professionals are particularly at risk of being exposed to infectious diseases given the nature of their practice. Many procedures involve coming into close contact with patients and aerosol generation. Aerosolized particles of viruses can be airborne and remain suspended in the air for hours, facilitating their transmission (15). Furthermore, high viral loads of COVID-19 were found in the respiratory tract of both symptomatic and asymptomatic patients (16) and were reported to be present in saliva of infected individuals (17). In response, the Department of Health (DH), the governmental body responsible for Hong Kong's healthcare system, and the Hong Kong Dental Association (HKDA), which represents and provides support to dentists in Hong Kong, have issued guidelines to ensure the safety of dental practices (18, 19).
Firstly, adequate personal protective equipment must be used at all times, with surgical masks, gloves, gowns, head caps, face shields, and eye protection as the bare minimum. Secondly, pre-treatment precautionary measures such as a health screening of patients and anti-septic mouth rinses should be carried out. The screening would include temperature measurements and questions about contact history, travel history, and relevant symptoms. It has been recommended that all non-urgent and elective dental treatment should be postponed however, there are no strict guidelines in regard to patient flow restrictions per se. All patients in the waiting area are required to wear masks and hand sanitizer should be readily available for their use whilst clinic staff are required to wear PPE at all times. Prior to dental treatment, the HKDA and DH have suggested the use of chlorohexidine, hydrogen peroxide and povidone iodine mouth rinses due to their potential to reduce the viral load of SARS-CoV-2 in saliva (20, 21). Patients treated in the undergraduate polyclinics are given a pre-procedural mouth rinse of povidone iodine, although the choice of antiseptic mouth rinse may vary in private practice. Thirdly, aerosol generating procedures should be avoided and largely limited to emergency treatment, even if rubber dam isolation is used. For endodontic treatment, it is the standard of practice to apply rubber dam isolation for reasons such as moisture control, ensuring an aseptic working field and protection of the patient's airway. In the context of infectious diseases, rubber dam isolation has been reported to be able to reduce the spread of airborne particles (22), albeit this is not specific to COVID-19. If aerosol generating procedures are to be performed, such as treatments that involve the use of high-speed and ultrasonic instruments, high-volume suction is mandatory in order to reduce the risk of contamination from the site of operation (23), with intra-oral modalities most commonly used in Hong Kong. Although negative pressure rooms can allow a more secure environment to treat and monitor patients with infectious diseases such as COVID-19 (24), its use for dental practices in Hong Kong has not been specifically recommended. Finally, all reusable dental instruments and equipment must be sterilized after use and changed between patients, whilst disposable items should be discarded after use. Thorough disinfection of frequently contacted and potentially contaminated surfaces should be carried out. It has been advised that surfaces contaminated with saliva are disinfected with one part 5.25% sodium hypochlorite to 49 parts water, whilst a concentration of one part 5.25% sodium hypochlorite to four parts water has been recommended for surfaces exposed to blood (18, 25). This is accordance to WHO guidelines, which suggests disinfectants such as diluted sodium hypochlorite, ethanol, and hydrogen peroxide are effective in cleaning surfaces and potentially reducing the presence of human coronavirus (26).
In summary, private dental clinics in Hong Kong and The Faculty of Dentistry have somewhat resumed operations, albeit with heightened levels of infection control and restrictions that limit the scope and capacity of everyday practices and procedures. Fortunately, despite the inherently high risk of exposure faced by dental professionals, there have been no reported instances of COVID-19 transmission between patients and dentists in Hong Kong. This suggests compliance to guidelines and strict infection control is of paramount importance in protecting the health of patients, dentists, and other dental personnel. Combating this pandemic will ultimately require the cooperation of the wider community. It affects all of us, from dental students to endodontic specialists. Although these trying times have pressed the pause button on many dental practices and the education system, adherence to social distancing, personal hygiene, and infection control may be able to see us through these volatile times. An optimistic outlook on the near future would be that Hong Kong will overcome the unpredictable challenges of this pandemic with the help of effective government policies and the cooperation of its citizens, and that dentists as well as educators will be able to maintain a cautious version of their normal practices.
All authors listed have made a substantial, direct and intellectual contribution to the work, and approved it for publication.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The authors would like to thank Professor Flemmig, Thomas Frank for generously taking the time to review the manuscript.
1. World Health Organization. WHO Director-General's Opening Remarks at the Media Briefing on COVID-19 World Health Organization. (2020). Available online at: https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19 (accessed March 11, 2020).
2. QS Top Universities. QS World University Rankings for Dentistry 2020: QS Quacquarelli Symonds Limited 1994-2020. (2020). Available online at: https://www.topuniversities.com/university-rankings/university-subject-rankings/2020/dentistry (accessed May 13, 2020).
3. HKSAR Government. COVID-19 Thematic Website - Together, We Fight the Virus. (2020). Available online at: https://www.coronavirus.gov.hk/eng/index.html (accessed May 13, 2020).
4. Hong Kong Institute of Asia-Pacific Studies at CUHK. Survey Findings on Views about COVID-19 Communications and Public Relations Office of The Chinese University of Hong Kong. (2020). Available online at: https://www.cpr.cuhk.edu.hk/en/press_detail.php?id=3260&t=survey-findings-on-views-about-covid-19-released-by-hong-kong-institute-of-asia-pacific-studies (accessed May 13, 2020).
5. Cowling BJ, Ali ST, Ng TWY, Tsang TK, Li JCM, Fong MW, et al. Impact assessment of non-pharmaceutical interventions against coronavirus disease 2019 and influenza in Hong Kong: an observational study. Lancet Publ. Health. (2020) 5:e279–e88. doi: 10.1016/S2468-2667(20)30090-6
6. Leung K, Wu JT, Liu D, and Leung GM. First-wave COVID-19 transmissibility and severity in China outside Hubei after control measures, and second-wave scenario planning: a modelling impact assessment. Lancet. (2020) 395:1382–93. doi: 10.1016/S0140-6736(20)30746-7
7. Leung KS-S, Ng TT-L, Wu AK-L, Yau MC-Y, Lao H-Y, Choi M-P, et al. A territory-wide study of early COVID-19 outbreak in Hong Kong community: a clinical, epidemiological and phylogenomic investigation. medRxiv.:2020.03.30.20045740 (2020). doi: 10.1101/2020.03.30.20045740
8. Sun F. Tired of the coronavirus? You're Not Alone, and Experts Worry ‘Pandemic Fatigue' is Driving Some in Hong Kong to Ignore Covid-19 Health Advice, Restrictions. (2020). Available online at: https://www.scmp.com/news/hong-kong/society/article/3094636/tired-coronavirus-youre-not-alone-and-experts-worry-pandemic (accessed May 13, 2020).
9. Bassir SH, Sadr-Eshkevari P, Amirikhorheh S, and Karimbux NY. Problem–based learning in dental education: a systematic review of the literature. J. Dent. Educ. (2014) 78:98–109. doi: 10.1002/j.0022-0337.2014.78.1.tb05661.x
10. Botelho MG. Evaluation of student use of videos to support learning in a simulation laboratory course: a perc “eption and analytics approach. J. Investig. Clin. Dent. (2019) 10:e12453. doi: 10.1111/jicd.12453
11. Asiry MA. Dental students' perceptions of an online learning. Saudi Dent. J. (2017) 29:167–70. doi: 10.1016/j.sdentj.2017.03.005
12. Department of Health HKSAR. Oral Health Survey 2011. Hong Kong (2013). Available online at: https://www.toothclub.gov.hk/en/en_pdf/Oral_Health_Survey_2011/Oral_Health_Survey_2011_WCAG_20141112_(EN_Full).pdf (accessed May 20, 2020).
13. Persoon IF, and Ozok AR. Definitions and epidemiology of endodontic infections. Curr. Oral Health Rep. (2017) 4:278–85. doi: 10.1007/s40496-017-0161-z
14. Pak JG, and White SN. Pain prevalence and severity before, during, and after root canal treatment: a systematic review. J. Endod. (2011) 37:429–38. doi: 10.1016/j.joen.2010.12.016
15. van Doremalen N, Bushmaker T, Morris D, Holbrook M, Gamble A, Williamson B, et al. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N. Engl. J. Med. (2020) 382:1564–67. doi: 10.1056/NEJMc2004973
16. Zou L, Ruan F, Huang M, Liang L, Huang H, Hong Z, et al. SARS-CoV-2 viral load in upper respiratory specimens of infected patients. N. Engl. J. Med. (2020) 382:1177–9. doi: 10.1056/NEJMc2001737
17. To KK, Tsang OT, Chik-Yan Yip C, Chan KH, Wu TC, Chan JMC, et al. Consistent detection of 2019 novel coronavirus in saliva. Clin. Infect Dis. (2020) 71:841–3. doi: 10.1093/cid/ciaa149
18. Hong Kong Dental Association. Updates of Current Studies on COVID-19 and Advice from the Hong Kong Dental Association (Press Release). Hong Kong Dental Association Ltd. (2020).
19. Lam W. Letters to Dentists Update on COVID-19. The Department of Health, The Government of the Hong Kong Special Administrative Region (2020).
20. Peng X, Xu X, Li Y, Cheng L, Zhou X, and Ren B. Transmission routes of 2019-nCoV and controls in dental practice. Int. J. Oral Sci. (2020) 12:9. doi: 10.1038/s41368-020-0075-9
21. O'Donnell VB, Thomas D, Stanton R, Maillard J-Y, Murphy RC, Jones SA, et al. Potential role of oral rinses targeting the viral lipid envelope in SARS-CoV-2 infection. Function. (2020) 1:zqaa002. doi: 10.1093/function/zqaa002
22. Samaranayake LP, Reid J, and Evans D. The efficacy of rubber dam isolation in reducing atmospheric bacterial contamination. ASDC J. Dent. Child. (1989) 56:442–4.
23. Harrel SK, and Molinari J. Aerosols and splatter in dentistry: a brief review of the literature and infection control implications. J. Am. Dent. Assoc. (2004) 135:429–37. doi: 10.14219/jada.archive.2004.0207
24. Centers for Disease Control and Prevention. Interim Infection Prevention and Control Recommendations for Healthcare Personnel During the Coronavirus Disease 2019 (COVID-19) Pandemic. U.S. Department of Health & Human Services (2020). Available online at: https://www.cdc.gov/coronavirus/2019-ncov/hcp/infection-control-recommendations.html (accessed May 13, 2020).
25. Centre for Health Protection. Guide to Infection Control in Clinic Setting. Department of Health, Hong Kong Special Administrative Region (2020).
Keywords: COVID-19, Hong Kong, endodontic practice, dental education, guidelines & recommendations
Citation: Wong J, Lee AHC and Zhang C (2020) Effect of COVID-19 on Dental Education and Endodontic Practice in Hong Kong. Front. Dent. Med. 1:569225. doi: 10.3389/fdmed.2020.569225
Received: 03 June 2020; Accepted: 17 August 2020;
Published: 22 September 2020.
Edited by:
Johnah Galicia, University of the Pacific, United StatesReviewed by:
Meetu R. Kohli, University of Pennsylvania, United StatesCopyright © 2020 Wong, Lee and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Chengfei Zhang, emhhbmdjZkBoa3UuaGs=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.