- Department of Psychology, Lakehead University, Thunder Bay, ON, Canada
Introduction: Mental health (MH) smartphone applications (MH apps) can support the increasing MH needs of postsecondary students and mitigate barriers to accessing support. Evaluating MH app acceptance using technology acceptance models is recommended to improve student engagement with MH apps. The JoyPopTM app was designed to improve youth resilience and emotion regulation. The JoyPopTM app is associated with improved student MH, but its acceptance has yet to be evaluated quantitatively. The present study used the Unified Theory of Acceptance and Use of Technology (UTAUT2) to evaluate and examine constructs and moderators influencing the acceptance (i.e., behavioural intention) and use of the JoyPopTM app.
Method: Participants were 183 postsecondary students attending a Canadian University who used the app for one week and completed measures before and after using the app. Relationships posited by the UTAUT2 were tested using partial least squares structural equation modelling (PLS-SEM).
Results: Most participants accepted the JoyPopTM app. The UTAUT2 model explained substantial variance in behavioural intention and app use. Performance expectancy, hedonic motivation, and facilitating conditions predicted behavioural intention, and behavioural intention and facilitating conditions predicted app use. Age moderated the association between facilitating conditions and behavioural intention. Experience moderated the relationship between performance expectancy, hedonic motivation, and social influence on behavioural intention.
Discussion: Results provide insight into factors influencing the acceptance of the JoyPopTM app and its ability to engage students. Results also provide valuable insights for evaluating and optimally designing MH apps.
Introduction
Despite the benefits and unique opportunities postsecondary education provides (1–3), mental health (MH) difficulties among Canadian students are high and increasing (4–6). A national survey examining the MH of 11,322 students across 32 Canadian colleges and universities found that many reported moderate to serious levels of psychological distress (85.4%), high levels of loneliness (58.6%), suicidal ideation (35.5%), and a diagnosis of an anxiety (32%) or mood (24.6%) disorder (4). Unaddressed MH difficulties can increase student distress and risk behaviours, negatively impact academic performance and well-being, and have long-lasting personal, social, and economic consequences (5, 7–9). Numerous stressors and challenges contribute to student MH difficulties, such as academic demands, concerns about the future, finances, and relationships (4, 5, 10). Students' abilities to cope with these stressors and the support they receive significantly impact MH and life outcome trajectories (5, 9, 11). In response to rising student MH needs, various discrete interventions (e.g., mindfulness interventions) and local, provincial, and national MH initiatives have been developed and implemented across Canadian postsecondary institutions (12, 13). However, students continue to face numerous structural and attitudinal barriers to accessing support, which reduces help-seeking and the adequacy of current MH services to meet student needs. Commonly reported barriers include minimal long-term therapy and off-site support, long wait times, lack of availability, time and financial constraints, and stigma (14–16). Consequently, there has been a growing interest in Canada in developing novel prevention and intervention efforts that expand the reach, scalability, affordability, and flexibility of MH supports (17).
Mobile Health (mHealth) smartphone applications designed to support MH (MH apps) are touted as a practical method to expand student MH support and mitigate barriers to accessing care (17, 18). MH apps are especially promising tools for students because of students' high rates of smartphone use and openness to using apps (17, 19, 20). MH apps are discussed as a solution to mitigate barriers to care because they are more scalable than traditional MH services and can provide 24-h on-demand support (12, 18). Further, integrating MH apps into existing services can increase availability and access to support and reduce stigma, costs, and MH disparities (17, 18, 21, 22). Among postsecondary students, research shows that MH apps are effective in improving outcomes, such as depression, anxiety, stress, well-being, and academic performance (23, 24). However, student engagement and long-term uptake of MH apps are low (25, 26). For example, a study in a sample of 742 postsecondary students found that among participants who had previously used a MH app, only 2.4% sustained use for four weeks or more (27). Evidence of effectiveness is also not a strong predictor of engagement and use (19, 28). Increasing user engagement is essential to increase the overall impact of MH apps for student MH (26, 28), and understanding user acceptance, which strongly affects engagement, is critical to improving engagement and use of MH apps (26, 28). Using technological acceptance frameworks to examine factors influencing user acceptance is recommended because of their utility in predicting and understanding engagement and continued use of mHealth apps (24, 28, 29–32).
The most prominent technology acceptance frameworks predicting acceptance and use of mHealth apps are the Technology Acceptance Model (TAM) (33), the Unified Theory of Acceptance and Use of Technology (UTAUT) (34), and the extended Unified Theory of Acceptance and Use of Technology (UTAUT2) (35). These frameworks are all based on psychological theories (e.g., Theory of Reasoned Action) (36) and conceptualize acceptance as users' behavioural intention to use technology, which is argued to influence use (35, 37). The UTAUT2 has become the leading framework because it captures the consumer/individual perspective, considers organizational, individual, and social factors, and explains more variance in behavioural intention and use of technologies (35, 38, 39).
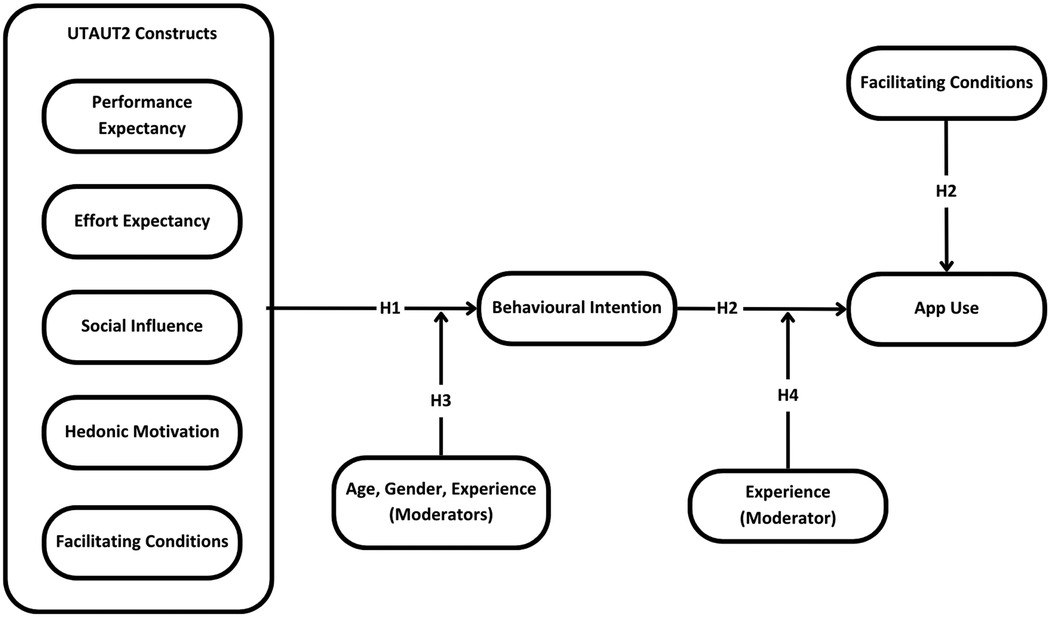
The UTAUT2 is an extension of the original UTAUT model (35). It includes seven core constructs (35). Performance expectancy refers to users' expectations that a technology is useful for its purpose. Effort expectancy relates to the ease of use and user-friendliness of technology. Social influence is the degree to which important people believe they should use technology. Facilitating conditions refers to the degree to which users believe they have sufficient organizational and technical infrastructure to use technology (34, 35). Hedonic motivation refers to the fun, pleasure, and enjoyment users experience with technology. Price value examines the influence of cost and pricing structure use. Habit refers to the automaticity with which people perform behaviours because of learning (35). All constructs in the model are purported to influence users' behavioural intention to use a technology. Behavioural intention, facilitating conditions and habit are posited to influence use directly. The UTAUT2 includes age, gender, and user experience with a specific technology as moderators of core constructs on behavioural intention, and experience is a moderator between behavioural intention and use (35). The UTAUT2 has been used and validated across diverse populations, countries, and contexts to evaluate and understand mHealth app acceptance (31, 39). UTAUT2 constructs and moderator variables significantly influence behavioural intention and use of mHealth apps in samples of postsecondary students (40–42).
Evaluating user acceptance, especially when guided by technology acceptance models, is critical in determining the relative importance of acceptance factors and informing app adaptations to increase user engagement and overall impact (24, 30, 43). However, among the many MH apps available on major marketplaces, few have been quantitatively evaluated regarding their acceptance (22, 26), and evaluations of MH app acceptance among postsecondary students are even more limited (22, 24, 26). Prior research implementing UTAUT2 constructs to quantitatively evaluate MH app acceptance is also cross-sectional, relies on retrospective reports of participants' experiences with groups of MH apps rather than gleaning users' experiences after using a specific app, and does not include all UTAUT2 constructs and moderators (40, 44, 45). Consequently, there is a significant need to quantitatively evaluate and understand the acceptance of specific MH apps among students, as the purpose and features of different MH apps are likely to vary. These evaluations can better assess the relative importance of acceptance factors to the unique characteristics of individual MH apps. These limitations informed the purpose of the present study, which is to evaluate and better understand factors influencing the acceptance of a resilience-building MH app (JoyPopTM) among a diverse student sample. This research will help determine whether the JoyPopTM app can be a valuable and engaging tool to support student MH, and results will inform future app adaptations.
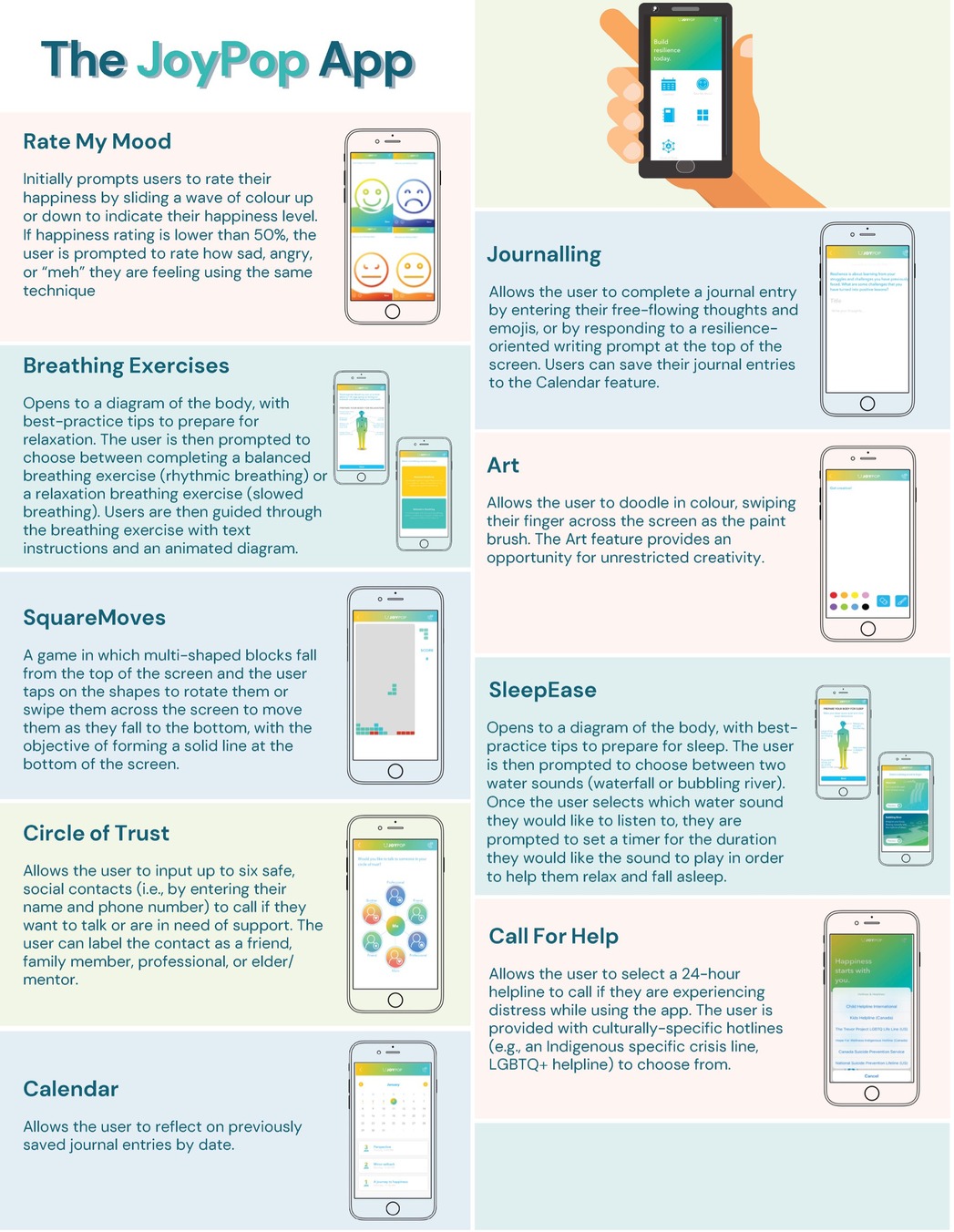
The JoyPopTM app was designed for youth (12+) and emerging adults (46). It contains multiple evidence-based features (see Figure 1) to support adaptive coping and emotion regulation (46, 47). The JoyPopTM app has a growing multimethod evidence base among diverse samples of youth and young adults in clinical and non-clinical settings (47–52). Research among postsecondary students suggests that using the app is associated with improved emotion regulation, stress, and depressive symptoms (47, 51). Students also perceive that the app increases self-regulation opportunities and self-awareness (52). However, the acceptance of the JoyPopTM app among students has yet to be quantitatively evaluated using an established technology acceptance model.
Considering this limitation in the JoyPopTM app literature, the paucity of quantitative MH acceptance evaluations among postsecondary students, and that no studies have incorporated the UTAUT2 model to quantitatively examine the acceptance of a specific MH app despite its utility in evaluating mHealth app acceptance, our objectives were to employ the UTAUT2 model to 1) quantitatively evaluate students’ acceptance of the JoyPopTM app and 2) examine factors influencing the app's acceptance and use. Because no study has examined the acceptance of a specific MH app using the UTAUT2, we based our hypotheses on the broader literature and the original UTAUT2 results (31, 35, 39). We did not include price value because the JoyPopTM app was freely available at the time of the study. We hypothesized that:
H1: Performance expectancy, effort expectancy, social influence, facilitating conditions, hedonic motivation, and habit would significantly predict behavioural intention to use the JoyPopTM app.
H2: Behavioural intention to use the JoyPopTM app, facilitating conditions, and habit would significantly predict use of the app.
H3: Age, gender, and experience with MH apps (“experience”) would moderate the relationship between UTAUT2 constructs and behavioural intention to use the JoyPopTM app.
H4: Experience would moderate the relationship between behavioural intention to use the JoyPopTM app and use of the app.
Method
Procedure
This study was reviewed and approved by the Research Ethics Board at Lakehead University. Students were eligible for the study if they were enrolled at Lakehead University and fluent in English. We selected this sample because students have increasing MH needs and face many barriers to accessing support, which makes them a relevant group to evaluate the utility of MH apps. We recruited students throughout the fall (2023) and winter (2024) academic semesters. Several measures were taken to increase the representativeness of our sample and minimize sampling bias. First, we used various recruitment methods to reach a wide range of students by posting flyers around campus, announcing our study to classes, providing postcards to students after class, emailing students in classes (e.g., through course instructors), and posting our study online via the Department of Psychology's undergraduate psychology participant pool site. Second, to improve the diversity of our sample, we had no restrictions on participant characteristics, such as year of study or program. Finally, to minimize biases of excluding participants without an iOS device, we participants without a suitable device with a refurbished iPhone containing only the app.
We used a one-week prospective design to ensure participants had sufficient time to use the app and provide informed evaluations regarding their acceptance. This study had three parts. For Part 1, participants attended an orientation session where they provided informed consent, completed demographic and MH app experience measures, and received the app. In Part 2, we reminded participants (via text/email) twice a day to use the app for one week. In Part 3, participants completed online measures assessing UTAUT2 constructs and app use. We compensated participants via cash/e-transfer or bonus course marks towards an eligible psychology course for completing measures ($10 for Part 1 or one bonus point; $20 for Part 3 or 1.5 bonus points).
Sample size estimation
In PLS-SEM, the ten times rule (i.e., sample size based on ten times the number of independent variables in the structural model) is often used to estimate the minimum required sample size. However, this approach underestimates the sample size needed for sufficient power and does not consider the entire model being assessed (53, 54). Thus, we followed the most recent recommendations and used the inverse square root method to determine the minimum sample size needed because it provides the most conservative and accurate estimate for PLS-SEM models (53, 54). This method bases sample size on the smallest path coefficient one expects to be significant, determined from research with similar conceptual models (53, 54). Past research employing the UTAUT2 to evaluate the acceptance of various types of mHealth apps (which included MH apps) found that the smallest significant path coefficient at the p < 0.05 level was 0.19 in the relationship between social influence and behavioural intention (40). Using minimum sample size requirement tables derived from the inverse square root method found in Hair et al. (53), to detect a minimum significant path coefficient between 0.11 and 0.20, we required a minimum sample size of 155 for 80% power at the 5% significance level. Considering ∼12% attrition rates in a similar JoyPopTM study conducted by MacIsaac et al. (47), we aimed to recruit at least 175 participants to account for estimated attrition throughout the study.
Participants
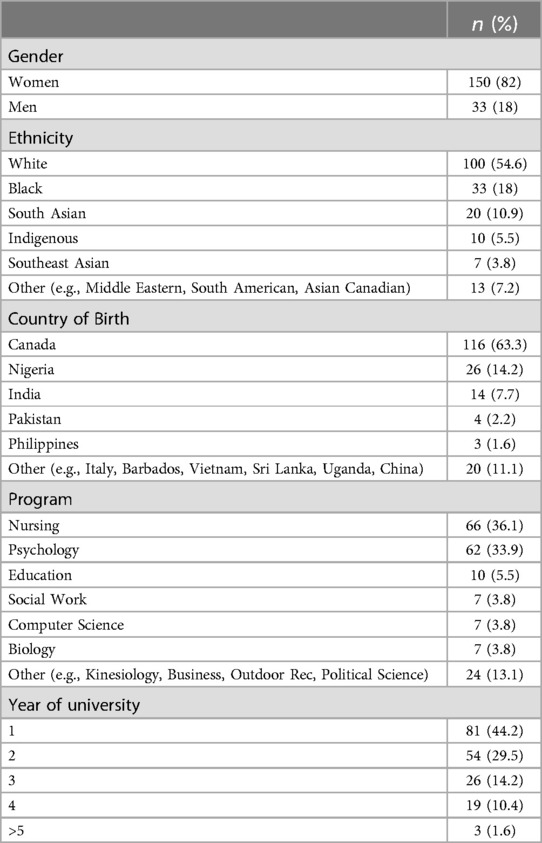
Our final sample consisted of 183 participants (see Table 1). Most participants were women (82%), with a mean age of 22.60 (SD = 7.08, 71% between 16 and 21, range = 16–56). Most participants identified as White (54.6%), followed by Black (18%) and South Asian (10.9%). Most participants were completing their first (42.6%) or second year (29.5%) in nursing (36.1%) or psychology programs (33.1%). Most participants used the app every day of the study period (M = 4.69, Mdn = 5, SD = 0.81).
Most participants had not used app-based MH care (80.9%). Of those who had used app-based MH care (19.1%), most used it for 0–6 months (62.9%), followed by not recalling the amount of time (20%) and 1–2 years (14.3%). Most participants had no MH apps on their phones/devices (86.3%). Among participants who reported having a MH app on their phone/device (13.7%), 88% had 1–3 apps, and 8% had more than seven apps. Frequency of use among these participants showed that 60% reported rarely using these apps, 12% reported using them once a week, 12% reported 2–3 times a week, and 16% used them once or twice a day.
Measures
UTAUT2 constructs
We used the UTAUT2 scale developed by Venkatesh et al. (35) to measure seven core constructs of the UTAUT2 model and behavioural intention to use the JoyPopTM app with 23 items slightly adapted to fit the context of the present study (see Supplementary File S1): Performance Expectancy (three items), Effort Expectancy (four items), Social Influence (three items), Facilitating Conditions (four items), Hedonic Motivation (three items), Habit (three items), and Behavioural Intention (three items). We adapted items where appropriate (i.e., changing “mobile internet” to “the JoyPopTM app”). We adapted one item from the Performance Expectancy construct to better fit the intended use of the JoyPopTM app (i.e., we changed “Using mobile internet increases my productivity,” to “Using the JoyPopTM app improves my mental health and/or productivity”). We adapted one item from the Habit construct based on a previous adaptation by Wu et al. (55) (i.e., we changed “I am addicted to using mobile internet” to “I am immersed in using/accepting the JoyPopTM app”). Participants rated items on a seven-point Likert scale ranging from 1 (strongly disagree) to 7 (strongly agree). We calculated scores for each construct by averaging corresponding items. We used participants' scores on the behavioural intention construct scale to evaluate the overall acceptance of the JoyPopTM app (32, 35).
Both the original and adapted versions of the UTAUT2 scale show strong psychometric properties in postsecondary student samples (35, 39, 40, 42). The internal consistency of construct scales in the present study were adequate (performance expectancy, α = .90; effort expectancy, α = .74; social influence, α = .91; facilitating conditions, α = .57; hedonic motivation, α = .91; habit, α = .81; behavioural intention, α = .94).
App use
To examine app use, we used an item (“How many times do you think you would use the JoyPopTM app in the next 12 months if it was relevant to you”) from the Subjective Quality scale of the User Version of the Mobile Application Rating Scale (uMARS) (56). Participants responded on a five-point scale ranging from 1 (None) to 5 (>50 times). We used this item because it is conceptually similar to the original use question on the UTAUT2 questionnaire and was developed to assess the frequency of mHealth app use.1
Data analysis
We coded whether participants had used app- or computer-based MH care as a binary categorical variable to examine the moderating effect of experience. We reported frequencies of participant scores on the behavioural intention construct scale to facilitate the interpretation of the app's overall acceptance.
PLS-SEM
We used the SmartPLS version 4 software (57) to conduct Partial Least Square Structural Equation Modelling (PLS-SEM) and examine hypothesized predictive-causal relationships (H1 to H4). We chose PLS-SEM because it is the preferred method of analysis when a study aims to test the predictive capability of a complex theoretical causal-predictive model that includes moderating effects and many constructs (six or more) and relationships (53, 58, 59). The causal-predictive nature makes PLS-SEM especially useful when deriving recommendations (53, 58), such as informing future adaptions to the JoyPopTM app to improve acceptance.
We evaluated two key components within the PLS-SEM model: a measurement model (outer model) and a structural model (inner model) (53). Throughout our analysis, we based our evaluation criteria and decision-making processes on the most recent PLS-SEM guidelines, recommendations, and research summarized by Hair et al. (53) and Sarstedt et al. (60).
Measurement model evaluation
We assessed the reliability of construct indicators (i.e., items used to measure constructs) and the internal consistency reliability, convergent validity, and discriminant validity of each construct in the model. We removed indicators and constructs that did not meet reliability and validity evaluation criteria to ensure that quality measures were used in the structural model (53). We evaluated indicator reliability by examining the outer loadings of constructs. Outer loadings should be >0.70 (53, 60). We removed indicators with outer loadings below 0.40 (53, 60). We considered indicators with outer loadings between ≥0.40 and <0.70 for removal if removing them increased construct reliability or validity to recommended thresholds and did not compromise content validity. We retained indicators with outer loadings within these ranges of values if the indicator's construct met the recommended thresholds for internal consistency reliability, convergent validity, and discriminant validity (53, 60).
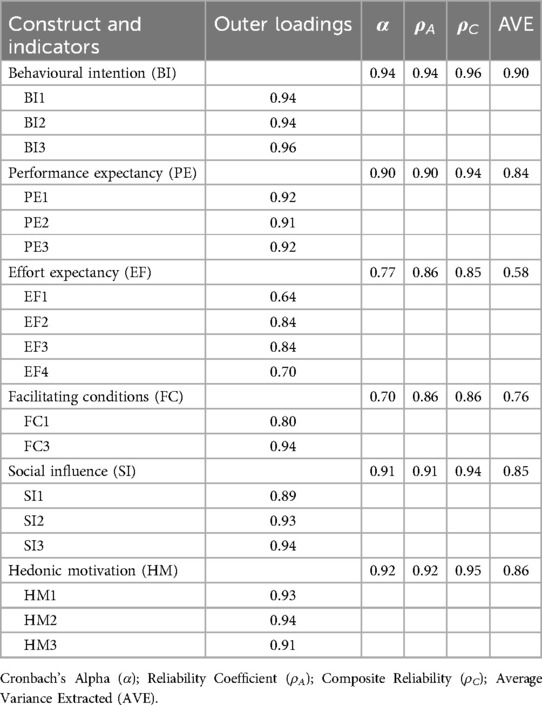
We assessed internal consistency reliability via Cronbach's α, composite reliability (ρC), and an exact reliability coefficient (ρA), which estimates the reliability of construct scores using the construct's weights rather than loadings (53, 60, 61). All internal consistency estimates should be ≥0.70 (53, 60). We assessed convergent validity by computing the average variance extracted (AVE) for all items for each construct. AVE's ≥ 0.50 are recommended (53, 60). We examined the discriminant validity of constructs via the heterotrait-monotrait ratio (HTMT) because it is more reliable and accurate than other common methods, such as the Fornell-Larcker criterion (53, 60). We used the <0.90 cut-off value, which is recommended when constructs are conceptually similar (60, 62).
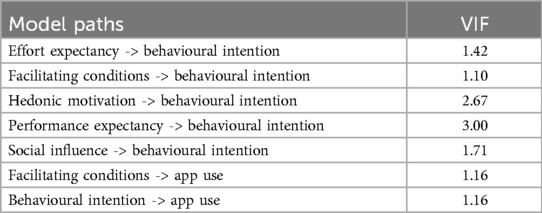
Structural model evaluation
We used the structural model to test our hypotheses that the UTAUT2 constructs would predict behavioural intention (H1), and facilitating conditions and behavioural intention would predict use of the JoyPopTM app (H2). We first checked for collinearity by examining the variance inflation factor (VIF). VIFs are recommended to be ≤3 because this indicates no collinearity issues (53, 60). We used the adjusted coefficient of determination (R2adj) to examine our structural model's explanatory power (53, 60). R2 values of 0.75, 0.50 and 0.25 are considered substantial, moderate, or weak (53, 58). We conducted a one-tailed test at the 5% significance level with PLS-SEM's nonparametric bootstrap procedure (10,000 iterations) to estimate path coefficients and their associated t values, p values, and confidence intervals (53, 63). We employed the Bias-Corrected and accelerated (BCa) bootstrap method to account for potential bias arising from asymmetrical bootstrap distributions for parameter estimates (60, 64). We examined the unique impact of predictors using f2 effect sizes. We used Cohen's (65) guidelines for interpreting the f2effect size, with values of 0.02, 0.15, and 0.25 representing small, medium, and large effects.
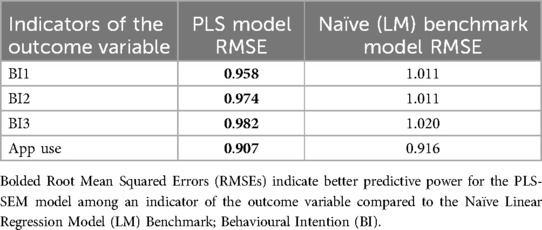
Because R2 values are derived from all data used for model estimation and do not provide information about the model's prediction power outside of the sample data included in the initial calculation of the model, they are not considered true estimates of predictive power (a model's utility in predicting new observations) (53, 59, 64). Consequently, if our hypothesized structural model was significant, we planned to test its out-of-sample prediction power using the novel and recommended PLSpredict procedure option in SmartPLS 4 (53, 66). The PLSpredict procedure first estimates the predictive power of a structural model by generating model estimates from a subset of observations (training sample). These estimates are applied to a subset of values on predictor variable indicators that have been omitted when generating parameter estimates (holdout sample), which are then used to predict dependent construct indicators within the holdout sample (64, 66). The strength of a model's out-of-sample prediction power is assessed by comparing prediction errors [the root mean squared errors (RMSEs)] produced by the PLS-SEM model to those made by a naïve linear regression model (LM) (64, 67). This method determines whether a theoretical model improves (or, at minimum, does not worsen) the predictive utility of available data among indicators (53, 67). See Supplementary Table S1 for guidelines for interpreting PLSpredict results [also see Shmueli et al. (67), for a thorough description of the PLSpredict method].
Moderation analysis
To test our hypothesis that age would moderate the relationships between the UTAUT2 constructs and behavioural intention (part of H3), we created interaction terms between age and relevant predictor variables using the recommended two-stage approach (53, 60, 68). Because gender and experience were grouping variables, our method to test the hypotheses that gender and experience would moderate the associations between UTAUT2 constructs and behavioural intention (part of H3), and experience would moderate the influence of behavioural intention on app use (H4) depended on whether there was full or partial measurement variance across groups (69). We employed the Measurement Invariance of Composite Models (MICOM) procedure in SmartPLS 4 to assess partial or full measurement invariance [see Henseler et al., (69) and Cheah et al., (70)]. If partial measurement invariance was confirmed, we planned to use the recommended multigroup analysis (MGA) procedure, to test whether there were significant differences between group-specific parameter estimates (53, 70). If full measurement invariance was confirmed, we followed suggestions to pool data from groups and account for structural heterogeneity by creating interaction terms between moderating variables and relevant latent constructs using the two-stage approach (53, 69, 70).
To determine the strength of the moderating effects, we calculated and interpreted the f2 effect sizes (53, 60). We interpreted f2 values as 0.005 (small), 0.01 (medium), and 0.025 (large) because standard cutoff values delineating f2effect sizes are less relevant when interpreting interaction terms (53, 71). We created simple slope plots to facilitate the interpretation of significant moderating effects (53, 72).
Results
Descriptives and overall acceptance
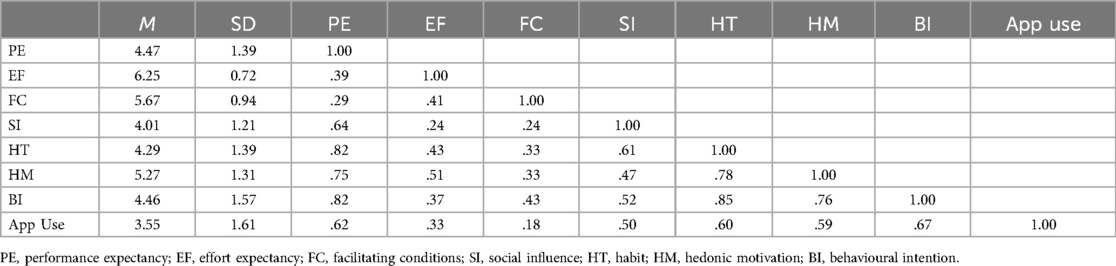
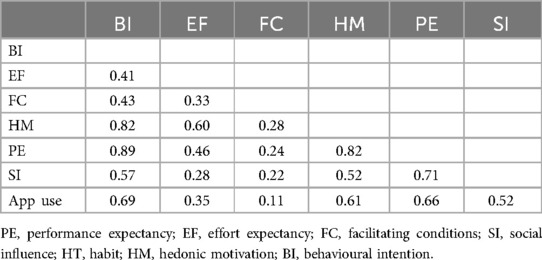
We present descriptive statistics and correlations for UTAUT2 constructs and app use in Table 2. Most participants showed moderate to strong acceptance of the JoyPopTM app. Specifically, 45.4% of participants indicated moderate (somewhat agree) to strong (strongly agree) acceptance of the app (range: 4.67–7), 25.1% showed low levels of acceptance (strongly disagree to somewhat disagree; range: 1–3.33), and 23% were unsure whether they intended to use the app (range: 3.67–4.33).
PLS-SEM
Measurement model
We removed two indicators on the facilitating conditions construct with outer loadings below 0.70 (0.39 and 0.66), which improved the reliability and convergent validity to recommended thresholds. We retained one indicator on the effort expectancy construct with an outer loading of 0.64 because the construct met all evaluation criteria for reliability and convergent validity. Discriminant validity was not established for the habit construct (HTMTs > 0.90), and we removed it from the model. Thus, we did not examine the hypothesized relationships between habit and behavioural intention (part of H1) and habit and use (part of H2) in the structural model. Our final model (see Figure 2) included performance expectancy, effort expectancy, facilitating conditions, social influence, hedonic motivation, behavioural intention, and app use because all constructs met the measurement model reliability and validity evaluation criteria. We present the outer loadings of indicators, the internal consistency reliability and convergent validity estimates of constructs in Table 3 and the discriminant validity of constructs in Table 4.
Structural model
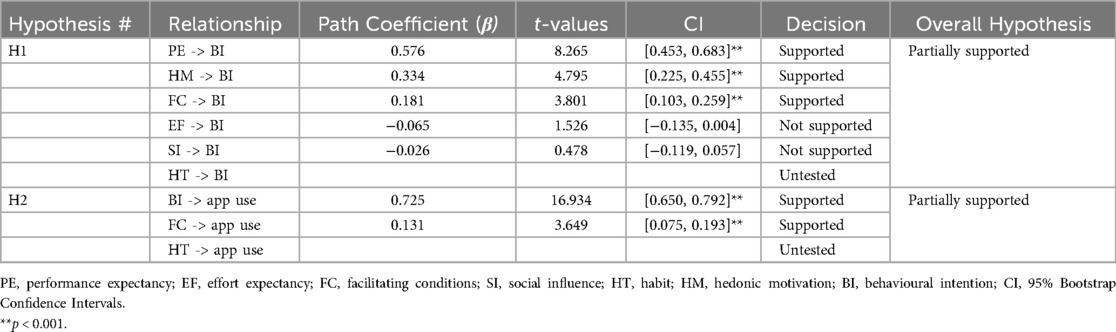
Once the measurement quality of the model was established, we evaluated and interpreted the structural model to test our hypotheses that each UTAUT2 construct would predict behavioural intention (H1), and facilitating conditions and behavioural intention would predict app use (H2). We found no collinearity issues (all VIFs ≤ 3; see Table 5). Overall, our model explained a significant and substantial amount of variance in behavioural intention [R2adjusted = 0.751, p < .001, 95% CI (0.679, 0.795)]. Performance expectancy (β = 0.576, p < .001, f2 = 0.457; large effect), hedonic motivation (β = 0.334, p < .001, f2 = 0.173; medium effect), and facilitating conditions (β = 0.181, p < .001, f2 = 0.124; small effect) significantly and positively predicted behavioural intention. Social influence and effort expectancy did not significantly predict behavioural intention. Therefore, we found partial support for H1.
Behavioural intention and facilitating conditions explained a moderate amount of variance in use [R2adjusted = 0.460, p < .001, 95% CI (0.367, 0.541)]. Behavioural intention (β = 0.725, p < 0.001, f2 = 0.849; large effect) and facilitating conditions (β = 0.131 p < .001, f2 = 0.038; small effect) significantly and positively predicted use. Thus, H2 was partially supported because we did not examine the influence of habit on use (see Table 6). Considering the significance of the structural model, we assessed the model's predictive power. Our model showed high predictive power because, compared to the naïve LM benchmark, lower RMSEs were produced by the PLS-SEM model on all indicators (see Table 7).
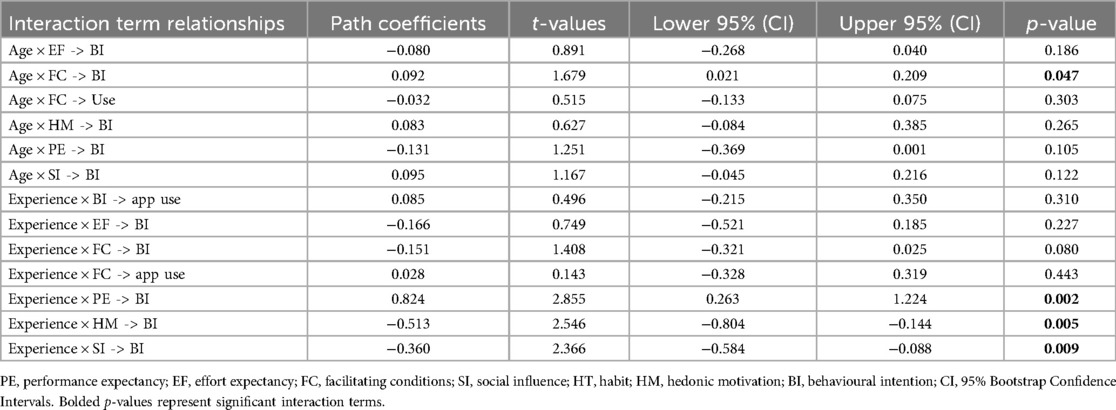
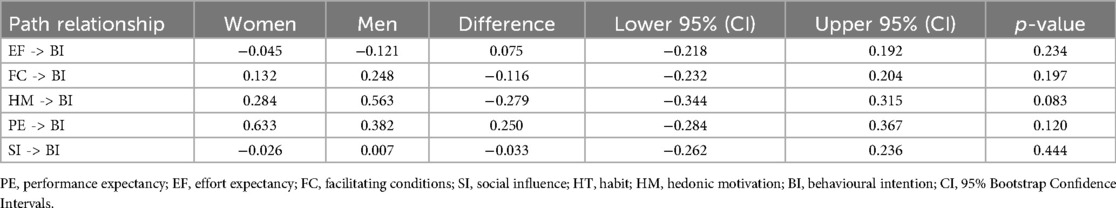
Moderation analysis
We first examined interaction effects for age to test our hypothesis that it would moderate associations between UTAUT2 constructs and behavioural intention. Age only showed a significant and large positive moderating effect on the relationship between facilitating conditions and behavioural intention (f2 = 0.032). We found full measurement invariance for experience and included it as an interaction effect to test our hypotheses that experience would moderate the relationship between UTAUT2 constructs and behavioural intention, as well as behavioural intention and use. Experience showed a significant and large positive effect on the relationship between performance expectancy and behavioural intention (f2 = 0.088) and significant and large negative effects on the relationships between hedonic motivation and behavioural intention (f2 = 0.059) and social influence and behavioural intention (f2 = 0.040; see Table 8). We found partial measurement invariance for gender and conducted a MGA to test our hypothesis that gender would moderate the relationship between UTAUT2 constructs and behavioural intention. We found no significant differences in path coefficients between women and men (see Table 9). In sum, H3 was partially supported because age, experience, and gender did not moderate all proposed hypothesized relationships between UTAUT2 constructs and behavioural intention. H4 was not supported because experience did not moderate the relationship between behavioural intention and use.
We created simple slope plots of significant interaction effects. As age increases, the positive relationship between facilitating conditions and behavioural intention becomes stronger, and as age decreases, this relationship gets slightly weaker (see Figure 3). The relationship between performance expectancy and behavioural intention was positive and stronger for participants without MH app experience. However, among those with MH app experience, the association between performance expectancy and behavioural intention was weak and negative (see Figure 4). The positive relationship between hedonic motivation and behavioural intention is stronger for participants with MH app experience and weaker for those without prior experience (see Figure 5). The relationship between social influence and behavioural intention is strong and positive among those with MH app experience compared to those without experience, in which the relationship is weak and negative (see Figure 6).
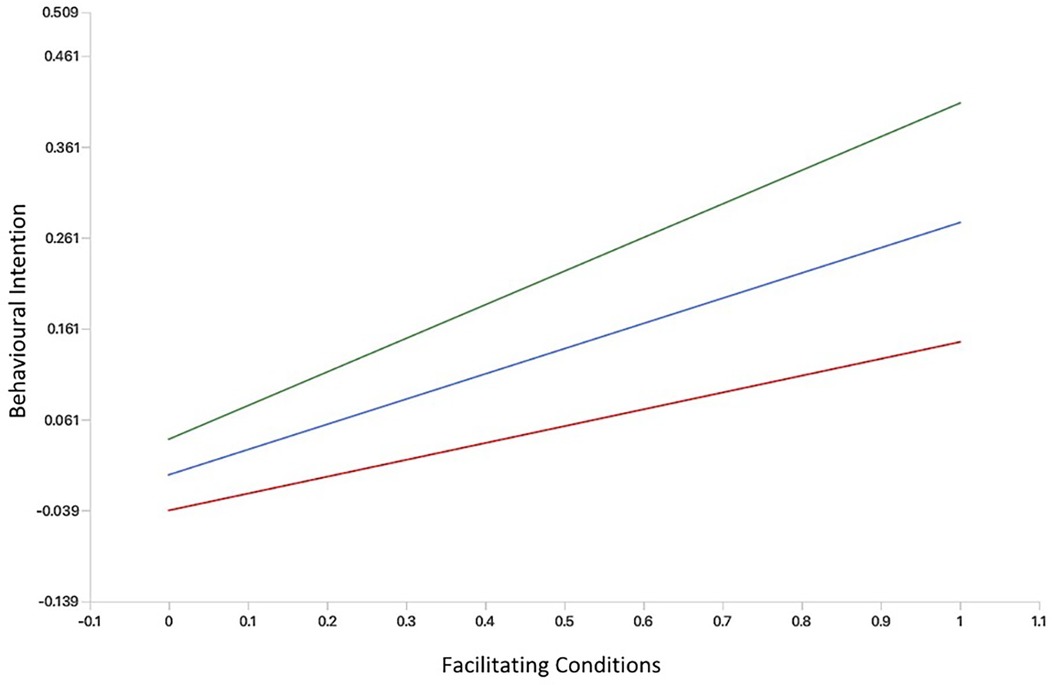
Figure 3. Simple slope plot showing moderating effect of Age on facilitating conditions. Green line (age = 1 SD above mean); Blue line (age = at mean); Red line (age = 1 SD below mean).
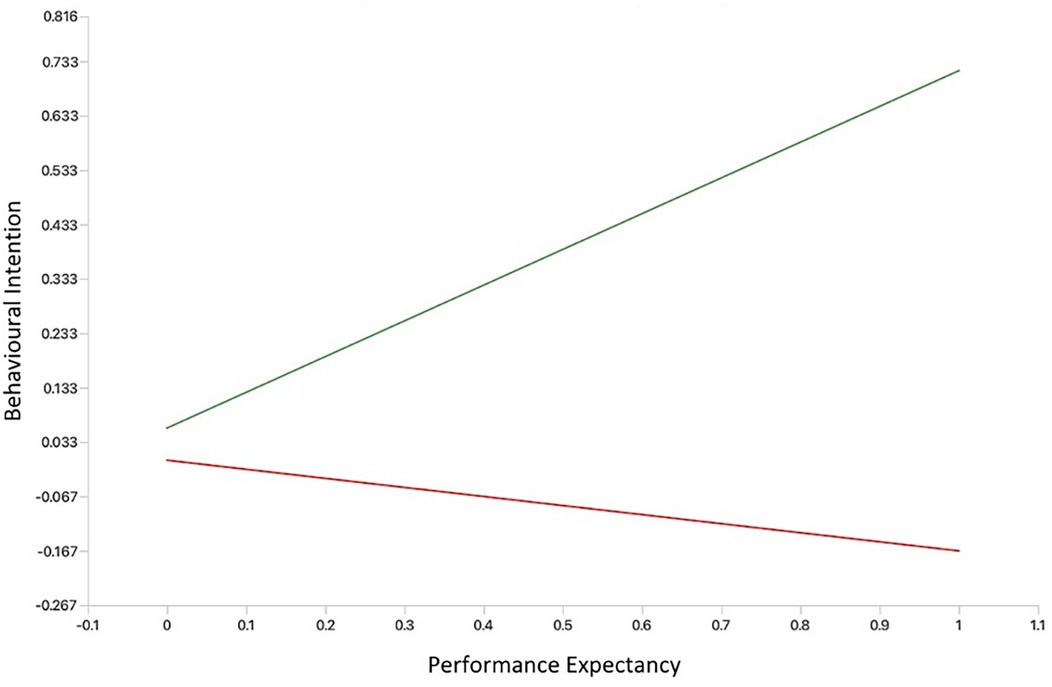
Figure 4. Simple slope plot showing moderating effect of experience on performance expectancy. Green line (No mental health app experience); Red line (Experience with mental health apps).
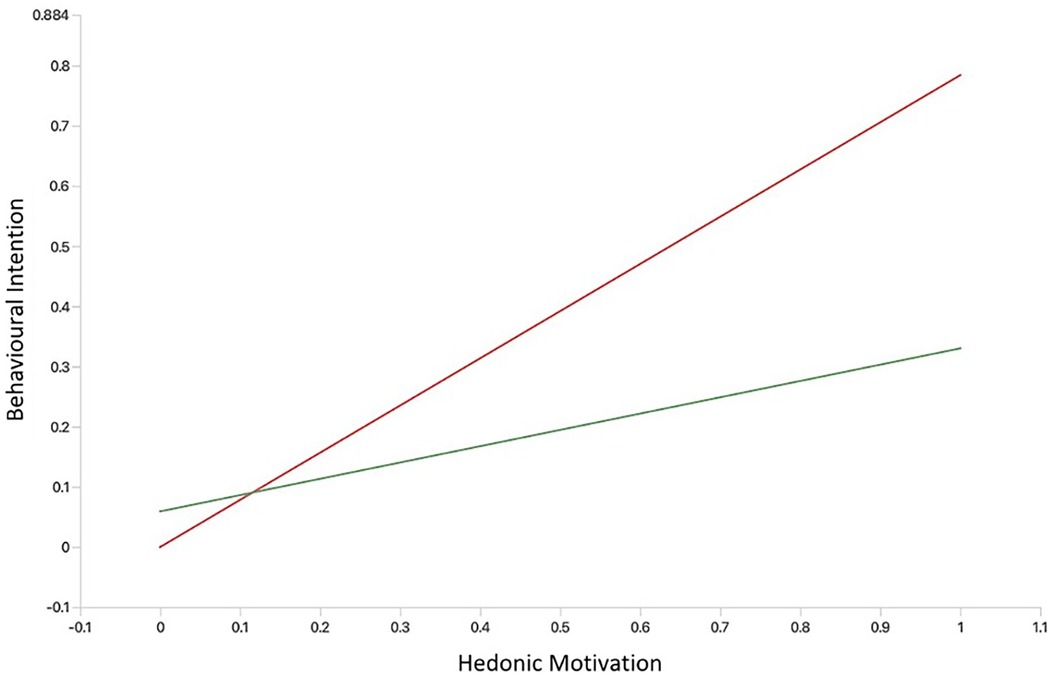
Figure 5. Simple slope plot showing moderating effect of experience on hedonic motivation. Green line (No mental health app experience); Red line (Experience with mental health apps).
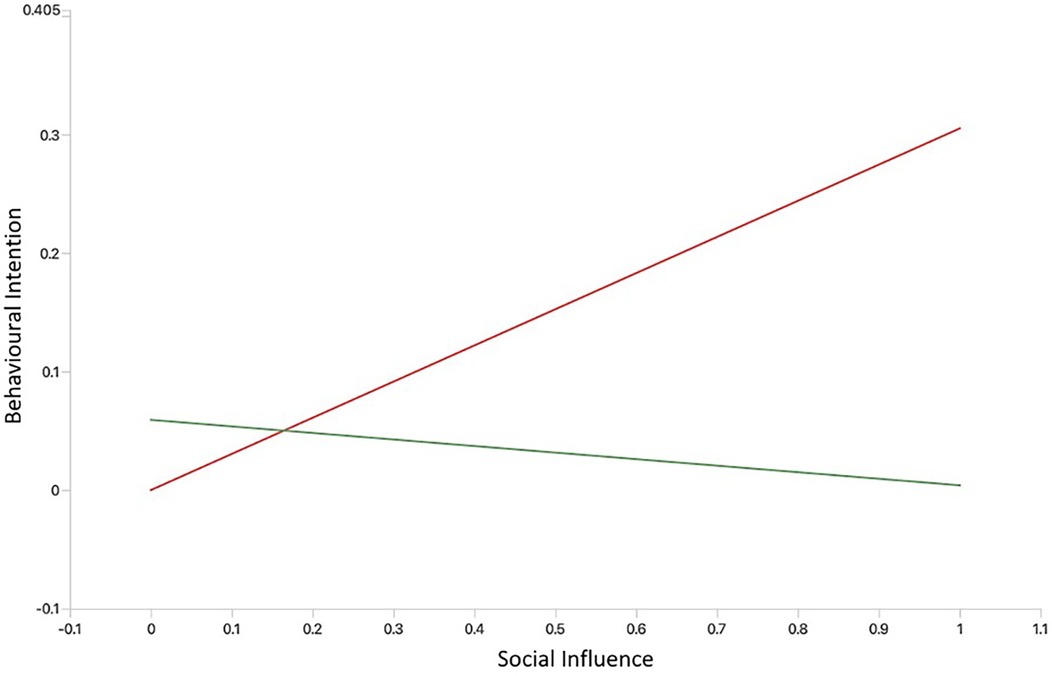
Figure 6. Simple slope plot showing moderating effect of experience on social influence. Green line (No mental health app experience); Red line (Experience with mental health apps).
Discussion
Using the UTAUT2 framework, we evaluated the acceptance (behavioural intention to use) of a resilience-building MH app (JoyPopTM) among postsecondary students and sought to better understand factors influencing its acceptance and use. We found that most students (45.4%) accepted the JoyPopTM app, which is consistent with past qualitative research on the app where users and healthcare providers reported high acceptance levels (via indicators such as usefulness and ease of use; 48, 49, 50, 52). Given that performance expectancy, facilitating conditions, and hedonic motivation significantly predicted students' intention to use the app, it is likely that students rated its acceptance highly because they had the resources necessary to use it and found it enjoyable and helpful for their MH and well-being.
Factors influencing acceptance and Use of the JoyPopTM App
We found that UTAUT2 constructs substantially influenced students' intentions to use the JoyPopTM app in the future (behavioural intention). Students’ intentions to use the app and whether they have sufficient resources (e.g., devices, time; facilitating conditions) moderately impacted app use. Our model showed strong out-of-sample predictive power (i.e., utility in predicting acceptance and use of the JoyPopTM app across the broader student population and similar research design contexts), supporting the external validity of our results. This pattern of results aligns with research highlighting the utility and importance of the UTAUT2 model in predicting the acceptance of mHealth apps across different contexts, populations, and countries (31, 32, 39, 73, 74).
Notably, our results also deviate from more recent, although limited, research regarding the predictive utility of the UTAUT2 model in determining users' intentions to use MH apps. For example, in past research, UTAUT2 constructs only had a minor influence on individuals' intentions to use lifestyle and therapy apps (40). Studies using the original UTAUT found that the constructs only had a small to moderate impact on whether postsecondary students intended to use popular MH apps (e.g., Headspace, Calm, Talkspace) (44). What may explain these conflicting findings is that each study was cross-sectional, and those by Schomakers et al. (40) and Holtz et al. (44) evaluated users' acceptance of groups of MH apps rather than specific apps. Further, Schomakers et al. (40) included many apps not designed explicitly for MH (e.g., diabetes-focused apps), and Holtz et al. (44) and Mitchell et al. (45) only examined the predictive utility of the original UTAUT constructs. More evaluations examining the acceptance of individual MH apps, such as the JoyPopTM app, using the UTAUT2 framework are needed to substantiate its predictive utility for MH app acceptance.
Upon examining the unique influence of individual UTAUT2 constructs, we found that students' perceptions about whether the JoyPopTM app could support their MH (performance expectancy) had the most substantial influence on their intentions to use the app in the future. Students' intentions were also affected by how fun and entertaining the app was perceived to be (hedonic motivation) and whether students felt they had the resources to use the app. Results are consistent with prior UTAUT2 mHealth app research among students and support the transferability and utility of the UTAUT2 in identifying and delineating the relative importance of acceptance factors across diverse student populations in different contexts and across various mHealth technologies (31, 45, 73). For instance, performance expectancy is routinely shown to be the most common and strongest predictor of mHealth app acceptance (including MH apps) among postsecondary students (31, 39, 44). mHealth and MH app acceptance among young adults and postsecondary students is also regularly shown to be influenced by hedonic motivation and facilitating conditions (31, 32, 39, 44, 45). In terms of use of the JoyPopTM app, we found that it was largely dependent on students’ intentions to use it, followed by whether they felt they had sufficient resources. These results align with the large body of research demonstrating that users' intentions are the strongest determinants of mHealth app use, followed by an essential but less impactful influence of having sufficient resources (31, 39).
Although past research employing the UTAUT2 to evaluate mHealth app acceptance found that the ease of using and learning an app (effort expectancy) is a consistent predictor of acceptance (28, 32, 44), effort expectancy did not predict acceptance of the JoyPopTM app. Students' skill and familiarity with smartphone apps (19, 20) and the finding that almost all participants found the JoyPopTM easy to use may explain the effort expectancy result. It may be that effort expectancy only becomes a determining factor in users' intention to use the app when it becomes significantly difficult to use. This finding makes it important for JoyPopTM app development teams to monitor effort expectancy levels while making adaptations to the app to ensure that the effort needed to use the app does not reach a point at which it negatively affects acceptance.
Also, we found that the opinions of important people in students' lives (social influence) did not predict acceptance of the JoyPopTM app, which was inconsistent with the extensive UTAUT2 literature demonstrating that social influence often predicts mHealth app acceptance (28, 32, 45). This finding could be attributed to students experiencing less stigma because seeking support for MH is widely promoted across postsecondary institutions, most being emerging adults and basing their decisions more on their own choices and agency (1), and that users can access MH apps privately and discretely in their own time. Prior qualitative research on the JoyPopTM app supports the privacy interpretation. Specifically, users perceived the app as helpful because it provided a safe and private tool to work on their MH (50). Although our moderation analysis provided important insight into the relationship between social influence and behavioural intention (discussed below), qualitative studies could be conducted to clarify why social influence does not influence students' acceptance of the JoyPopTM app.
Moderating effects of gender, age, and experience
Gender
Although the literature examining the influence of gender on mHealth app acceptance is mixed (28, 31), gender has an important pooled effect on UTAUT2 relationships (31, 39). We did not find moderating effects for gender in the present study, which might be attributed to the variety of features offered through the JoyPopTM app and its transdiagnostic focus on emotion regulation and resilience building. Although men and women differ on average in their coping strategies (75), the JoyPopTM app offers various ways to implement adaptive coping skills. It also includes features that can be used beyond coping (e.g., Journaling to plan activities). Thus, gender may be less important because the app allows users to create individualized methods to improve their MH and build resilience. This result should be interpreted cautiously, as there were more women than men in the present sample.
Age
We found age moderates the relationship between facilitating conditions and behavioural intention. Older students placed a stronger emphasis on ensuring they have sufficient resources to use the app. This result was inconsistent with prior studies showing that the relationship between users' knowledge and resources to use the app and their intentions to use the app is independent of their age (31, 76). However, previous studies have primarily evaluated the acceptance of general mHealth services (e.g., websites, telehealth, wearable technologies, computer systems) targeting broad medical and health issues (e.g., metabolic and cardiovascular diseases, fitness) among adults and healthcare providers (31, 39), and no studies have examined the acceptance of an individual MH app among postsecondary students. Older students may need to become more familiar with MH apps and have more responsibilities outside of school (e.g., children), thus placing more importance on ensuring they have the resources and knowledge required to use the JoyPopTM app effectively (77, 78). Older students may also be less inclined to use an app that is incompatible with the technologies they already use. Research finds that older adults are more hesitant about using novel technologies because they may be more inconvenienced by the effort required to use them, have more concerns about their utility, and may need more general awareness and knowledge about them (77, 78). Thus, older adults may need more information and support related to the utility, convenience benefits, and potential technical difficulties associated with newer technology (77, 78). This finding partly implies that to increase acceptance among older students, developers would benefit from ensuring that these students are provided with extra support and information about how to use the app (78).
Experience
MH app experience moderated the relationships between performance expectancy, social influence, hedonic motivation, and behavioural intention. This pattern of results is consistent with prior research showing that relationships between core UTAUT2 constructs and behavioural intention to use mHealth technologies depend on user experience (31, 35). Students with MH app experience placed less importance on how beneficial the JoyPopTM app was for their MH and more on the enjoyment and entertainment it offered. One interpretation of these findings is that those with MH app experience have previously found MH apps helpful for the benefits they can provide (e.g., increased access to support and improved MH) and developed a belief that apps like JoyPopTM can be valuable. Consequently, they may prioritize whether the app provides enough pleasure and fun to keep them engaged and promote continued use. Users with no MH app experience may be unsure whether the JoyPopTM app can fulfill its designed purpose and place less emphasis on whether it is fun and enjoyable and prioritize whether it provides any benefit to their MH and coping skills. It is important to consider that our indicator of experience was categorical (i.e., yes or no) and that the moderating influence of experience may change depending on the specific amount of experience a user has (e.g., number of months).
Although social influence had no significant main effect on behavioural intention, we found that the impact of social influence was moderated by experience. Consistent with past research (31, 35), participants with MH app experience placed more emphasis on the opinions of significant others in their intention to use the app compared to those with no experience, in which the opinions of others had a minimal negative effect. Self-stigma (e.g., perceiving oneself as socially undesirable because of seeking MH support) (79) may help explain why MH app experience influences the relationship between social influence and behavioural intention. Compared to individuals with no experience, those with experience may have developed higher levels of self-stigma from prior MH app use and thus be more sensitive to the opinions of others. However, being influenced by significant others is not always negative because they play an essential informal role in help-seeking (80, 81). Prior users of MH apps may be positively influenced by others who know them and have seen that MH supports, like MH apps, have been helpful for them (80, 81). Although more research is needed to fully explore how others influence experienced users' acceptance of the JoyPopTM app, strength-based supports, like the JoyPopTM app, can reduce the potential effects of self-stigma (82).
Taken together, our results examining the moderating effects of age, gender, and experience highlight the importance of including moderators posited by the UTAUT2 to understand the acceptance of MH apps. The influence of these moderating effects across mHealth acceptance studies is mixed and depends on the context, sample, setting, and specific apps evaluated (31, 32). Interestingly, the moderating effects of age, gender, and experience may occur via three-way interactions. For example, Venkatesh et al. (35) found that the effect of effort expectancy on behavioural intention was stronger among older women (age × gender × effort expectancy). Future studies would benefit from examining higher-order interaction effects among specific MH apps.
Limitations and suggestions for future research
The first limitation of this study is that we excluded the habit construct from the structural model because of inadequate discriminant validity. Research supports habit as a strong predictor of behavioural intention and use of mHealth apps (31, 32, 39). Our adaptations of items comprising the habit construct may have influenced discriminant validity. It will be important that future studies explore whether retaining the original items is beneficial.
A second limitation is our subjective measure of JoyPopTM app use. Although studies employing the UTAUT2 to examine mHealth app acceptance often use a subjective usage measure (39), recent recommendations suggest incorporating objective usage metrics (39, 43). While we tracked the number of days participants used the JoyPopTM app, we did not use this as an outcome measure and relied on a subjective measure of use because of high levels of actual usage (and lack of variation) among most of the sample. Future studies would benefit from examining acceptance over more extended periods to increase the likelihood that days used will vary enough to capture the relationship between behavioural intention and actual usage of the JoyPopTM app. It would be helpful for future research to include both subjective and objective measures of app usage.
A third limitation is that we used a convenience sample comprised primarily of women. Research finds that women are more likely to use mHealth apps designed to improve emotion regulation, while men prefer accessing health-related information mHealth apps that include gamification, goal-based, and built-in tracking features (83, 84). Although we accounted for this by including gender as a moderating variable, which showed no significant differences in estimated path coefficients, unequal sample sizes across groups warrant caution when interpreting this result. Thus, it is unknown whether the results will generalize to men and the broader Canadian postsecondary population (83, 84). Future acceptance research would benefit from recruiting more balanced proportions of men and women or conducting a similar study among only men. However, the generalizability of our results to the broader student population is supported by our assessment and demonstration of the model's strong predictive power and external validity and the commonalities between the demographics in our sample and the student population in Ontario (85).
A fourth limitation concerns our one-week prospective design. Technology acceptance is a staged and temporal process, and user engagement can be complex and vary over time (86). Although having participants use the JoyPopTM for one week facilitated informed perspectives regarding its acceptance, the relative importance of acceptance factors may change over extended periods of use. It will be important that future research assess acceptance at multiple time points over longer periods to better capture the process of technology acceptance and track its changing nature at varying stages of use.
Implications
Our results support the applicability of the UTAUT2 model in evaluating and understanding the acceptance and use of MH apps. Using the UTAUT2 can facilitate MH app comparisons to determine the most important constructs influencing app engagement while providing insight into the relative impact of constructs across different MH apps. The present study can also serve as an example for future researchers examining MH app acceptance and guide the initial selection of the most appropriate and established constructs and moderators. After an app undergoes an initial evaluation using the UTAUT2, additional constructs (e.g., perceived trust) and moderators (e.g., personality traits) shown to influence acceptance and use can be added to assess whether they add predictive value.
A key implication of this study is that it can provide a valuable process to facilitate optimal app design and ensure adaptations provide the most users with as helpful and engaging an experience as possible. After examining important UTAUT2 constructs and moderators (e.g., age) influencing app acceptance and use, apps can be tailored or adapted to tap into strongly predictive constructs and nuanced user characteristics. Further, understanding which constructs do not predict acceptance and use allows developers to potentially sacrifice attributes of an app at the expense of constructs with stronger predictive strength. For example, considering our results, JoyPopTM development teams could increase acceptance and use by adding a wider variety of features to improve the app's ability to enhance user resilience and adaptive coping (i.e., performance expectancy), incorporating gamification aspects and reward systems into features to increase the entertainment and enjoyability (i.e., hedonic motivation), and expanding the app to Android devices to ensure users have the resources to use the app (i.e., facilitating conditions). MH app development teams can then engage in an iterative process in which they evaluate factors influencing the acceptance of their app throughout all stages of development and implementation.
Finally, our results add to the literature suggesting that the JoyPopTM app can be an engaging and helpful tool for diverse students to build resilience and improve MH and well-being. Findings support the potential integration of the app into usual campus MH services to support increasing student MH needs and reduce common barriers to care. Results also provide critical information on the JoyPopTM app's acceptance, which will help inform future iterations to ensure changes address factors shown to influence its acceptance (or, at minimum, do not worsen it) to increase user engagement, long-term uptake, and the app's ability to meet the diverse needs of students.
Conclusion
The present study was the first to employ the UTAUT2 framework to evaluate and understand factors influencing the acceptance of a resilience-building MH app (JoyPopTM) among postsecondary students. Most students accepted the JoyPopTM app. Students' acceptance was significantly influenced by their perception of the app's utility in providing helpful and efficient MH support, how much they enjoyed and were entertained by it, and whether they had sufficient resources to use it. Findings highlight the utility and importance of employing the UTAUT2 to evaluate and understand factors influencing MH app acceptance. Results support the JoyPopTM app as a potentially helpful tool to integrate into postsecondary MH services, support student well-being, and reduce common barriers to care.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Lakehead University Research Ethics Board. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
IM: Conceptualization, Data curation, Formal Analysis, Investigation, Methodology, Project administration, Software, Writing – original draft, Writing – review & editing. AM: Conceptualization, Data curation, Formal Analysis, Investigation, Methodology, Project administration, Resources, Supervision, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. IM was supported by a grant from The Digital, Inclusive, Virtual, and Equitable Research Training in Mental Health Platform (DIVERT Mental Health): A Canadian Institutes of Health Research (CIHR) Research Training Platform Building a More Equitable and Accessible Mental Health System for Children, Youth, and Their Families.
Acknowledgments
We would like to acknowledge and thank Teagan Neufeld, Amelia Traer, Anastasia Ranta-Diegel, Jennifer Wyman, and Mackenzie McQueen for their hard work supporting this study as research assistants.
Conflict of interest
AM recently acquired intellectual property ownership rights for the JoyPop TM app (in June 2024). Prior to this time, intellectual property rights were owned by another researcher/institution. AM did not own any intellectual property rights when the study was developed, when data were collected, when data were analyzed, or when the initial draft of the manuscript was written.
The remaining author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fdgth.2025.1503428/full#supplementary-material
Footnote
1. ^Due to insufficient variation in the number of days participants used the app (i.e., the majority of participants used the app every day; see the participants section) across the study period, we did not include days used as our primary app use outcome variable.
References
1. Arnett JJ. College students as emerging adults: the developmental implications of the college context. Emerg Adulthood. (2016) 4(3):219–22. doi: 10.1177/2167696815587422
2. Borgonovi F. The relationship between education and levels of trust and tolerance in Europe: the relationship between education and levels of trust and tolerance. BJS. (2012) 63(1):146–67. doi: 10.1111/j.1468-4446.2011.01397.x
3. Brennan J, Durazzi N, Séné T. (2013). Report No.: BIS/13/1244. Things we know and don’t know about the wider benefits of higher education: a review of the recent literature. BIS Research Paper. London: Department for Business, Innovation and Skills.
4. American College Health Association (ACHA). American college health association-national college health assessment III: Canadian reference group executive summary spring 2022 (2022). Available online at: https://www.acha.org/wp-content/uploads/2024/07/NCHA-III_SPRING_2022_CANADIAN_REFERENCE_GROUP_EXECUTIVE_SUMMARY.pdf (accessed May 1, 2024).
5. Linden B, Stuart H. Post-secondary stress and mental well-being: a scoping review of the academic literature. Can J Community Ment Health. (2020) 39(1):1–32. doi: 10.7870/cjcmh-2020-002
6. Linden B, Boyes R, Stuart H. Cross-sectional trend analysis of the NCHA II survey data on Canadian post-secondary student mental health and wellbeing from 2013 to 2019. BMC Public Health. (2021) 21(1):590. doi: 10.1186/s12889-021-10622-1
7. Esmaeelzadeh S, Moraros J, Thorpe L, Bird Y. Examining the association and directionality between mental health disorders and substance use among adolescents and young adults in the US and Canada—a systematic review and meta-analysis. J. Clin. Med. (2018) 7(12):543. doi: 10.3390/jcm7120543
8. Evans TM, Bira L, Gastelum JB, Weiss LT, Vanderford NL. Evidence for a mental health crisis in graduate education. Nat Biotechnol. (2018) 36(3):282–4. doi: 10.1038/nbt.4089
9. Wood D, Crapnell T, Lau L, Bennett A, Lotstein D, Ferris M, et al. Emerging adulthood as a critical stage in the life course. In: Halfon N, Forrest C, Lerner R, Faustman E, editors. Handbook of Life Course Health Development. Cham: Springer (2018). p. 123–43. doi: 10.1007/978-3-319-47143-3_7
10. Burke TJ, Ruppel EK, Dinsmore DR. Moving away and reaching out: young adults’ relational maintenance and psychosocial well-being during the transition to college. J Fam Commun. (2016) 16(2):180–7. doi: 10.1080/15267431.2016.1146724
11. Byrd DR, McKinney KJ. Individual, interpersonal, and institutional level factors associated with the mental health of college students. J Am Coll Health. (2012) 60(3):185–93. doi: 10.1080/07448481.2011.584334
12. Mental Health Commission of Canada (MHCC). National standard of Canada for supporting the mental health and well-being of postsecondary students. (2020). Available online at: https://mentalhealthcommission.ca/wp-content/uploads/2021/05/PSS_Standard_Leaflet_eng.pdf (accessed May 1, 2024).
13. Okanagan Charter. Okanagan Charter: an international charter for health promoting universities and colleges. In: International Conference on Health Promoting Universities & Colleges. Kelowna, BC, Canada (2015). Available online at: https://open.library.ubc.ca/media/download/pdf/53926/1.0132754/7 (accessed May 1, 2024).
14. Moghimi E, Stephenson C, Gutierrez G, Jagayat J, Layzell G, Patel C, et al. Mental health challenges, treatment experiences, and care needs of post-secondary students: a cross-sectional mixed-methods study. BMC Public Health. (2023) 23(1):655. doi: 10.1186/s12889-023-15452-x
15. Ogrodniczuk JS, Kealy D, Laverdière O. Who is coming through the door? A national survey of self-reported problems among post-secondary school students who have attended campus mental health services in Canada. Couns Psychother Res. (2021) 21(4):837–45. doi: 10.1002/capr.12439
16. Robinson AM, Jubenville TM, Renny K, Cairns SL. Academic and mental health needs of students on a Canadian campus. Can J Couns Psychother. (2016) 50(2):108.
17. Mental Health Commission of Canada (MHCC). E-mental health in Canada: transforming the mental health system using technology. (2014). Available online at: https://www.mentalhealthcommission.ca/sites/default/files/MHCC_EMental_HealthBriefing_Document_ENG_0.pdf (accessed May 1, 2024).
18. Price M, Yuen EK, Goetter EM, Herbert JD, Forman EM, Acierno R, et al. Mhealth: a mechanism to deliver more accessible, more effective mental health care. Clin Psychol Psychother. (2014) 21(5):427–36. doi: 10.1002/cpp.1855
19. Bautista J, Schueller SM. Understanding the adoption and use of digital mental health apps among college students: secondary analysis of a national survey. JMIR Ment Health. (2023) 10(1):e43942. doi: 10.2196/43942
20. Statistics Canada. Table 22-10-0137-01. Selected online activities by gender, age group and highest certificate, diploma or degree completed. (2023). doi: 10.25318/2210013701-eng
21. Levin ME, Krafft J, Levin C. Does self-help increase rates of help seeking for student mental health problems by minimizing stigma as a barrier? J Am Coll Health. (2018) 66(4):302–9. doi: 10.1080/07448481.2018.1440580
22. Messner EM, Probst T, O’Rourke T, Stoyanov S, Baumeister H. Mhealth applications: potentials, limitations, current quality and future directions. In: Baumeister H, Montag C, editors. Digital Phenotyping and Mobile Sensing: New Developments in Psychoinformatics. Cham: Springer (2019). p. 235–48. doi: 10.1007/978-3-030-31620-4_15
23. Choudhury A, Kuehn A, Shamszare H, Shahsavar Y. Analysis of mobile app-based mental health solutions for college students: a rapid review. Healthcare (Basel). (2023) 11(2):272. doi: 10.3390/healthcare11020272
24. Oliveira C, Pereira A, Vagos P, Nóbrega C, Gonçalves J, Afonso B. Effectiveness of mobile app-based psychological interventions for college students: a systematic review of the literature. Front Psychol. (2021) 12:647606. doi: 10.3389/fpsyg.2021.647606
25. Linardon J, Fuller-Tyszkiewicz M. Attrition and adherence in smartphone-delivered interventions for mental health problems: a systematic and meta-analytic review. J Consult Clin Psychol. (2020) 88(1):1–13. doi: 10.1037/ccp0000459
26. Torous J, Nicholas J, Larsen ME, Firth J, Christensen H. Clinical review of user engagement with mental health smartphone apps: evidence, theory and improvements. BMJ Ment Health. (2018) 21(3):116–9. doi: 10.1136/eb-2018-102891
27. Kern A, Hong V, Song J, Lipson SK, Eisenberg D. Mental health apps in a college setting: openness, usage, and attitudes. Mhealth. (2018) 4:20. doi: 10.21037/mhealth.2018.06.01
28. Jacob C, Sezgin E, Sanchez-Vazquez A, Ivory C. Sociotechnical factors affecting patients’ adoption of mobile health tools: systematic literature review and narrative synthesis. JMIR Mhealth Uhealth. (2022) 10(5):e36284. doi: 10.2196/36284
29. Connolly SL, Hogan TP, Shimada SL, Miller CJ. Leveraging implementation science to understand factors influencing sustained use of mental health apps: a narrative review. J Technol Behav Sci. (2021) 6(2):184–96. doi: 10.1007/s41347-020-00165-4
30. Hajesmaeel-Gohari S, Khordastan F, Fatehi F, Samzadeh H, Bahaadinbeigy K. The most used questionnaires for evaluating satisfaction, usability, acceptance, and quality outcomes of mobile health. BMC Med Inform Decis Mak. (2022) 22(1):22. doi: 10.1186/s12911-022-01764-2
31. Calegari LP, Tortorella GL, Fettermann DC. Getting connected to m-health technologies through a meta-analysis. Int J Environ Res Public Health. (2023) 20(5):4369. doi: 10.3390/ijerph20054369
32. Philippi P, Baumeister H, Apolinário-Hagen J, Ebert DD, Hennemann S, Kott L, et al. Acceptance towards digital health interventions – model validation and further development of the unified theory of acceptance and use of technology. Internet Interv. (2021) 26:100459. doi: 10.1016/j.invent.2021.100459
33. Davis FD. Perceived usefulness, perceived ease of use, and user acceptance of information technology. MIS Q. (1989) 10(13):319–40. doi: 10.2307/249008
34. Venkatesh V, Morris M, Davis G, Davis F. User acceptance of information technology: toward a unified view. MIS Q. (2003) 27(3):425–78. doi: 10.2307/30036540
35. Venkatesh V, Thong JY, Xu X. Consumer acceptance and use of information technology: extending the unified theory of acceptance and use of technology. MIS Q. (2012) 36(1):157–78. doi: 10.2307/41410412
36. Ajzen I, Fishbein M. Attitude-behavior relations: a theoretical analysis and review of empirical research. Psychol Bull. (1977) 84(5):888–918. doi: 10.1037/0033-2909.84.5.888
37. Ammenwerth E. Technology acceptance models in health informatics: TAM and UTAUT. Stud Health Technol Inform. (2019) 263:64–71. doi: 10.3233/SHTI190111
38. Malatji WR, Eck RV, Zuva T. Understanding the usage, modifications, limitations and criticisms of technology acceptance model (TAM). Adv Sci Technol Eng Syst J. (2020) 5(6):113–7. doi: 10.25046/aj050612
39. Tamilmani K, Rana NP, Dwivedi YK. Consumer acceptance and use of information technology: a meta-analytic evaluation of UTAUT2. Inf Syst Front. (2021) 23(4):987–1005. doi: 10.1007/s10796-020-10007-6
40. Schomakers E-M, Lidynia C, Vervier LS, Calero Valdez A, Ziefle M. Applying an extended UTAUT2 model to explain user acceptance of lifestyle and therapy mobile health apps: survey study. JMIR Mhealth Uhealth. (2022) 10(1):e27095. doi: 10.2196/27095
41. Uncovska M, Freitag B, Meister S, Fehring L. Patient acceptance of prescribed and fully reimbursed mHealth apps in Germany: an UTAUT2-based online survey study. J Med Syst. (2023) 47:14. doi: 10.1007/s10916-023-01910-x
42. Yuan S, Ma W, Kanthawala S, Peng W. Keep using my health apps: discover users’ perception of health and fitness apps with the UTAUT2 model. Telemed E Health. (2015) 21(9):735–41. doi: 10.1089/tmj.2014.0148
43. Ng MM, Firth J, Minen M, Torous J. User engagement in mental health apps: a review of measurement, reporting, and validity. Psychiatr Serv. (2019) 70(7):538–44. doi: 10.1176/appi.ps.201800519
44. Holtz BE, Kanthawala S, Martin K, Nelson V, Parrott S. Young adults’ adoption and use of mental health apps: efficient, effective, but no replacement for in-person care. J Am Coll Health. (2023) 73(2):602–10. doi: 10.1080/07448481.2023.2227727
45. Mitchell KM, Holtz BE, McCarroll AM. Assessing college students’ perceptions of and intentions to use a mobile app for mental health. Telemed E Health. (2022) 28(4):566–74. doi: 10.1089/tmj.2021.0106
46. Wekerle C. JoyPopTM: A resilience intervention for youth mental health. (2021) Available online at: https://edition.pagesuite-professional.co.uk/html5/reader/production/default.aspx?pubname=&edid=b43e8d51-b6f4-48ca-9e31-d7936ed7a950 (accessed May 1, 2024).
47. MacIsaac A, Mushquash AR, Mohammed S, Grassia E, Smith S, Wekerle C. Adverse childhood experiences and building resilience with the JoyPop app: evaluation study. JMIR Mhealth Uhealth. (2021) 9(1):e25087. doi: 10.2196/25087
48. Au-Yeung A, Marfatia D, Beers K, General DA, McQueen KCD, Martin-Hill D, et al. Exploring the feasibility of a mental health application (JoyPopTM) for indigenous youth. Front Psychiatry. (2023) 14:1269347. doi: 10.3389/fpsyt.2023.1269347
49. Kim K, Au-Yeung A, Dagher D, Jacobs N, Martin-Hill D, Wekerle C, et al. Exploring the relevance of a psychology-based resilience app (JoyPop™) for indigenous youth. Child Abuse Negl. (2023) 148:106343. doi: 10.1016/j.chiabu.2023.106343
50. Malik I, Perez A, Toombs E, Schmidt F, Olthuis JV, Charlton J, et al. Female youth and mental health service providers’ perspectives on the JoyPop™ app: a qualitative study. Front Digit Health. (2023) 5:1197362. doi: 10.3389/fdgth.2023.1197362
51. Maurer K, Kimyaci M, Konyk K, Wekerle C. Building resilience through daily smartphone app use: results of a pilot study of the JoyPop app with social work students. Front Digit Health. (2023) 5:1265120. doi: 10.3389/fdgth.2023.1265120
52. Mushquash AR, Pearson ES, Waddington K, MacIsaac A, Mohammed S, Grassia E, et al. User perspectives on a resilience-building app (JoyPop): qualitative study. JMIR Mhealth Uhealth. (2021) 9(7):e28677. doi: 10.2196/28677
53. Hair JF, Hult GTM, Ringle CM, Sarstedt M. A Primer on Partial Least Squares Structural Equation Modeling (PLS-SEM). 3rd ed Thousand Oaks, CA: SAGE (2022).
54. Kock N, Hadaya P. Minimum sample size estimation in PLS-SEM: the inverse square root and gamma-exponential methods. Inf Syst J. (2018) 28(1):227–61. doi: 10.1111/isj.12131
55. Wu P, Zhang R, Zhu X, Liu M. Factors influencing continued usage behavior on mobile health applications. Healthcare (Basel). (2022) 10(2):208. doi: 10.3390/healthcare10020208
56. Stoyanov SR, Hides L, Kavanagh DJ, Wilson H. Development and validation of the user version of the mobile application rating scale (uMARS). JMIR Mhealth Uhealth. (2016) 4(2):e72. doi: 10.2196/mhealth.5849
57. Ringle CM, Wende S, Becker J. SmartPLS 4. Oststeinbek: SmartPLS. (2022). Available online at: https://www.smartpls.com (accessed May 1, 2024).
58. Hair JF, Risher JJ, Sarstedt M, Ringle CM. When to use and how to report the results of PLS-SEM. Eur Bus Rev. (2019) 31(1):2–24. doi: 10.1108/EBR-11-2018-0203
59. Sarstedt M, Hair JF, Ringle CM. “PLS-SEM: indeed a silver bullet” - retrospective observations and recent advances. J Mark Theory Pract. (2023) 31(3):261–75. doi: 10.1080/10696679.2022.2056488
60. Sarstedt M, Hair JF, Pick M, Liengaard BD, Radomir L, Ringle CM. Progress in partial least squares structural equation modeling use in marketing research in the last decade. Psychol Mark. (2022) 39(5):1035–64. doi: 10.1002/mar.21640
61. Dijkstra TK, Henseler J. Consistent partial least squares path modeling. MIS Q. (2015) 39(2):297–316. doi: 10.25300/MISQ/2015/39.2.02
62. Henseler J, Ringle CM, Sarstedt M. A new criterion for assessing discriminant validity in variance-based structural equation modeling. J Acad Mark Sci. (2015) 43(1):115–35. doi: 10.1007/s11747-014-0403-8
63. Streukens S, Leroi-Werelds S. Bootstrapping and PLS-SEM: a step-by-step guide to get more out of your bootstrap results. Eur Manag J. (2016) 34(6):618–32. doi: 10.1016/j.emj.2016.06.003
64. Hair J, Alamer A. Partial least squares structural equation modeling (PLS-SEM) in second language and education research: guidelines using an applied example. Res Methods Appl Linguist. (2022) 1(3):100027. doi: 10.1016/j.rmal.2022.100027
65. Cohen J. Statistical Power Analysis for the Behavioral Sciences. New York: Routledge Academic (1988).
66. Shmueli G, Ray S, Velasquez Estrada JM, Chatla SB. The elephant in the room: predictive performance of PLS models. J Bus Res. (2016) 69(10):4552–64. doi: 10.1016/j.jbusres.2016.03.049
67. Shmueli G, Sarstedt M, Hair JF, Cheah J-H, Ting H, Vaithilingam S, et al. Predictive model assessment in PLS-SEM: guidelines for using PLSpredict. Eur J Mark. (2019) 53(11):2322–47. doi: 10.1108/EJM-02-2019-0189
68. Henseler J, Chin WW. A comparison of approaches for the analysis of interaction effects between latent variables using partial least squares path modeling. Struct Equ Modeling. (2010) 17(1):82–109. doi: 10.1080/10705510903439003
69. Henseler J, Ringle CM, Sarstedt M. Testing measurement invariance of composites using partial least squares. Int Mark Rev. (2016) 33(3):405–31. doi: 10.1108/IMR-09-2014-0304
70. Cheah J-H, Amaro S, Roldán JL. Multigroup analysis of more than two groups in PLS-SEM: a review, illustration, and recommendations. J Bus Res. (2023) 156:113539. doi: 10.1016/j.jbusres.2022.113539
71. Aguinis H, Beaty JC, Boik RJ, Pierce CA. Effect size and power in assessing moderating effects of categorical variables using multiple regression: a 30-year review. J Appl Psychol. (2005) 90(1):94–107. doi: 10.1037/0021-9010.90.1.94
72. Dawson JF. Moderation in management research: what, why, when, and how. J Bus Psychol. (2014) 29(1):1–19. doi: 10.1007/s10869-013-9308-7
73. Duarte P, Pinho JC. A mixed methods UTAUT2-based approach to assess mobile health adoption. J Bus Res. (2019) 102:140–50. doi: 10.1016/j.jbusres.2019.05.022
74. Zhu Y, Zhao Z, Guo J, Wang Y, Zhang C, Zheng J, et al. Understanding use intention of mHealth applications based on the unified theory of acceptance and use of technology 2 (UTAUT-2) model in China. Int J Environ Res Public Health. (2023) 20(4):3139. doi: 10.3390/ijerph20043139
75. Lawrence J, Ashford K, Dent P. Gender differences in coping strategies of undergraduate students and their impact on self-esteem and attainment. Act Learn High Educ. (2006) 7(3):273–81. doi: 10.1177/1469787406069058
76. Nunes A, Limpo T, Castro SL. Individual factors that influence the acceptance of mobile health apps: the role of age, gender, and personality traits. In: Information and Communication Technologies for Ageing Well and e-Health: 4th International Conference, ICT4AWE 2018, Funchal, Madeira, Portugal, March 22–23, 2018, Revised Selected Papers 4. Cham: Springer International Publishing. (2019). p. 167–79. doi: 10.1007/978-3-030-15736-4_9
77. Gitlow L. Technology use by older adults and barriers to using technology. Phys Occup Ther Geriatr. (2014) 32(3):271–80. doi: 10.3109/02703181.2014.946640
78. Mitzner TL, Boron JB, Fausset CB, Adams AE, Charness N, Czaja SJ, et al. Older adults talk technology: technology usage and attitudes. Comput Hum Behav. (2010) 26(6):1710–21. doi: 10.1016/j.chb.2010.06.020
79. Vogel DL, Strass HA, Heath PJ, Al-Darmaki FR, Armstrong PI, Baptista MN, et al. Stigma of seeking psychological services: examining college students across ten countries/regions. Couns Psychol. (2017) 45(2):170–92. doi: 10.1177/0011000016671411
80. Rickwood DJ, Deane FP, Wilson CJ. When and how do young people seek professional help for mental health problems? Med J Aust. (2007) 187(S7):S35–9. doi: 10.5694/j.1326-5377.2007.tb01334.x
81. Rickwood DJ, Mazzer KR, Telford NR. Social influences on seeking help from mental health services, in-person and online, during adolescence and young adulthood. BMC Psychiatry. (2015) 15(1):40. doi: 10.1186/s12888-015-0429-6
82. Rashid T. Positive psychotherapy: a strength-based approach. J Posit Psychol. (2014) 10(1):25–40. doi: 10.1080/17439760.2014.920411
83. Antezana G, Venning A, Smith D, Bidargaddi N. Do young men and women differ in well-being apps usage? Findings from a randomised trial. Health Inform J. (2022) 28(1):14604582211064825. doi: 10.1177/14604582211064825
84. Smail-Crevier R, Powers G, Noel C, Wang J. Health-related internet usage and design feature preference for e-mental health programs among men and women. J Med Internet Res. (2019) 21(3):e11224. doi: 10.2196/11224
85. Statistics Canada. Table 98-10-0433-01. School attendance by visible minority and immigrant status: Canada, provinces and territories, census metropolitan areas and census agglomerations with parts (2022). doi: 10.25318/9810043301-eng
Keywords: mental health app, postsecondary students, acceptance, UTAUT2, JoyPopTM, mobile health, digital health, emotion regulation
Citation: Malik I and Mushquash AR (2025) Acceptance of a mental health app (JoyPopTM) for postsecondary students: a prospective evaluation using the UTAUT2. Front. Digit. Health 7:1503428. doi: 10.3389/fdgth.2025.1503428
Received: 28 September 2024; Accepted: 28 January 2025;
Published: 18 February 2025.
Edited by:
Rosa M. Baños, University of Valencia, SpainReviewed by:
Alexandru Vasincu, Grigore T. Popa University of Medicine and Pharmacy, RomaniaMarcin Golec, Heidelberg University Hospital, Germany
Copyright: © 2025 Malik and Mushquash. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Aislin R. Mushquash, YWlzbGluLm11c2hxdWFzaEBsYWtlaGVhZHUuY2E=
 Ishaq Malik
Ishaq Malik Aislin R. Mushquash
Aislin R. Mushquash