- 1Department of Health Informatics, College of Medicine and Health Science, Debre Markos University, Debre Markos, Ethiopia
- 2Department of Health System and Policy, Institute of Public Health, College of Medicine and Health Science, University of Gondar, Gondar, Ethiopia
- 3Department of Health Education and Behavioral Sciences, Institute of Public Health, College of Medicine and Health Science, University of Gondar, Gondar, Ethiopia
- 4Department of Health Informatics, Institute of Public Health, College of Medicine and Health Science, University of Gondar, Gondar, Ethiopia
Introduction: Currently, mortality by non-communicable diseases is increasing alarmingly. They account for approximately 35 million deaths each year, of which 14% are due to cardiovascular disease and 9.2% occur in Africa. Patients do not have access to healthcare services outside the healthcare setting, resulting in missed follow-ups and appointments and adverse outcomes. This study aimed to assess the willingness to use remote monitoring among cardiovascular patients in a resource-limited setting in Ethiopia.
Method: An institution-based cross-sectional study was conducted from April to June 2021 among cardiovascular patients at referral hospitals in Ethiopia. A structured interview questionnaire was used to collect the data. A systematic random sampling technique was used to select 397 study participants. Binary and multivariable logistic regression analyses were employed and a 95% confidence level with a p-value <0.05 was used to determine the level of association between variables.
Result: In total, 81.61% of the study participants were willing to use remote patient monitoring [95% confidence interval (CI) = 77.4%–85.1%]. Age [adjusted odds ratio (AOR) = 0.94; 95% CI: 0.90–0.98], having a mobile phone (AOR = 5.70; 95% CI: 1.86–17.22), and perceived usefulness (AOR = 1.50; 95% CI: 1.18–1.82) were significantly associated with willingness to use remote patient monitoring among cardiovascular patients.
Conclusion: Cardiovascular patients had a high willingness to use remote patient monitoring. Age, perceived usefulness of remote patient monitoring, and having a mobile phone were significantly associated with a willingness to use remote patient monitoring.
Introduction
In the 21st century, mortality due to non-communicable diseases (NCDs) has been increasing alarmingly and it has been the leading threat to human health and development (1). NCDs account for approximately 35 million deaths each year, of which 14% were due to cardiovascular diseases (CVDs) (2) and 9.2% of the total mortality occurred in Africa (3).
CVDs are a cluster of disorders of the heart and blood vessels that include but are not limited to ischemic heart disease (IHD), heart failure, rheumatic heart disease (RHD), peripheral arterial disease (PAD), and stroke (4) In a study conducted in Ethiopia, more than 3 million people were found to affected by CVDs. Of these cases, 33.7% were RHD, followed by IHD (22.5%) and stroke (11.4%) (5).
NCDs accounted for 34% of deaths in Ethiopia in 2011, 31% in 2014, and 39% in 2018. Of these, CVDs contributed 15% to NCD-related deaths in 2011, 9% in 2014, and 16% in 2018.
In addition to this, the age-standardized CVD prevalence was 5,534 per 100,000 population in Ethiopia (6, 7). A study conducted in Tikur Anbessa referral hospital showed that 70% of RHD affects mainly the working-age group (18–40 years) (8).
According to the World Health Organization (WHO), the healthcare system is experiencing a rapid digital transformation to deliver healthcare services remotely using broadcast communications innovation (8) through an automated web, electronic, or phone-based information transmission of diagnosis, treatment of diseases, injuries, and physiological data such as heart rate, blood pressure, oxygen saturation, and weight where healthcare providers and patients are spatially separated (9–11), thus using audio, video, and other telecommunication technologies to monitor vital parameters of patient status (9).
In developed countries, remote patient monitoring (RPM) has been used to monitor the health status of patients outside the healthcare setting and as an alternative approach to reduce geographical barriers and optimize healthcare service access where in-person visits are difficult. Evidence shows that remote monitoring allows for better communication between the patient and the physician for timely treatment (12, 13). Remote patient monitoring benefits the patients with immediate feedback at the earliest sign of health treatment (14).
However, implementing remote patient monitoring in resource-limited settings can present several challenges, such as a lack of the necessary infrastructure and technology, a shortage of financial resources, ensuring patient data privacy and security, and training healthcare professionals to monitor and interpret patient data remotely (15). Successful RPM implementation relies on patient engagement and adherence to monitoring protocols, where patients may have limited health literacy or cultural beliefs that affect their willingness to participate in RPM programs (16).
Integrating RPM into existing healthcare systems can be complex, particularly in resource-limited settings where the healthcare infrastructure may be fragmented or underdeveloped for interoperability, and data integration with electronic health records (EHRs) may pose challenges (17). Addressing these challenges requires a multi-faceted approach involving collaboration between healthcare providers, technology vendors, policymakers, community stakeholders, and patients (18). It is critical to adapt RPM solutions to the unique context of resource-limited settings, taking into account the available resources, infrastructure, and cultural factors (14, 19, 20).
An RPM system reduces the healthcare personnel burden and medico-legal issues (13, 21). For instance, mobile phone-based remote monitoring is a relatively cheap and convenient way to improve heart failure patient management (22). Remotely managing the patient using telemedicine has emerged as an alternative to optimize therapy, improve quality of life, prevent readmission, and self-manage their condition (13, 20–22). Wireless remote monitoring allows clinicians to make clinical decisions on time rather than in the office (14). The use of remote monitoring reduces hospitalization by 44%and prevents secondary cause mortality (23). In the USA, RPM for patients with cardiovascular heart failure (CHF) was cost-effective (24), reducing the need for hospitalization and mortality (22, 25).
Tele-monitoring in the Netherlands of patients with COVID-19 enabled them to recover in their homes, improved satisfaction, reduced hospitalization, and reduced healthcare costs (13). Efficiency and satisfaction resulted from remote monitoring of patients in the COVID-19 watch program at the University of Pennsylvania (26). In sub-Saharan Africa (SSA), tele-health interventions in the diagnosis, tracking, and care of patients with COVID-19 were effective (27) and remote monitoring of patients with human immunodeficiency virus (HIV) and tuberculosis (TB) contributed to the reduction of healthcare costs, waiting time, hospital visits, and improved patients’ quality of life (22).
Patients are constrained by unnecessary transportation, long waiting times, and healthcare costs (27, 28). These challenges to providing health services in rural and urban communities in Ethiopia are due to limited health facilities and health personnel (29). The WHO emphasized designing different models to manage NCD (30).
The Ethiopian Ministry of Health (MoH) has set key strategic directions for digital health technology to enhance the healthcare system, such as strengthening health information systems (HIS), implementing EHR, and telemedicine and remote healthcare (28). However, there is limited evidence on the acceptance and willingness of cardiovascular (CV) patients to use RPM services. Therefore, this study aimed to assess the willingness to use remote monitoring and associated factors among cardiovascular patients in a resource-limited setting.
Method and materials
Study design and setting
An institutional-based cross-sectional study was conducted among 423 cardiovascular patients. The study was conducted at specialized teaching hospitals in the Amhara region from April to June 2021. These hospitals have been used as teaching and referral centers for a population of more than 10 million in the catchment area.
Inclusion and exclusion criteria
Patients who were 18 and older and had a follow-up in the hospitals during data collection were included in the study. However, patients who were seriously ill and unable to respond were excluded from the study.
Operational definitions
Cardiovascular disease
Patients with cardiac disease (ischemic, rheumatic, chronic heart failure), stroke, PAD, or deep vein thrombosis (DVT).
Willingness to use remote patient monitoring
A patient who responded “yes” was considered to be willing to use remote monitoring for their disease management, and those who responded “no” were unwilling to use remote monitoring (31).
Attitude to use remote patient monitoring
A 5-point Likert scale was used ranging from “strongly disagree” to “strongly agree” with eight items and classified into favorable and unfavorable attitudes using Bloom's cut-off point. An attitude score of less than 79% (<32 points) was grouped into an unfavorable attitude, while a score of greater than 80% (32–40 points) was considered a favorable attitude toward using remote monitoring (32).
Perceived usefulness
Perceived usefulness was measured using a 5-point Likert scale ranging from “strongly disagree” to “strongly agree” by three items. A higher usefulness score implied a patient perceived remote monitoring to be more useful as compared to a patient with a lower usefulness score (33).
Perceived ease of use
Perceived ease of use was measured using a 5-point Likert scale that ranged from “strongly disagree” to “strongly agree” by four items. A higher ease of use score meant a patient perceived remote monitoring to be easy to use (34, 35).
Sample size and sampling procedures
The sample size was determined using the single population proportion formula by considering the 95% confidence interval (CI), 5% marginal error (d = 0.05), and 50% of the magnitude of willingness to use remote patient monitoring since there has been no previous study done in the same population among CV patients (p = 0.5). After accounting for a 10% non-response rate, the total final sample size was 423. A systematic random sampling technique was used to select the study participants. The expected number of patients during the data collection period was 917, which was obtained from two referral hospitals. An interval was calculated as k = N/n, where N is the expected number of CV patients during the data collection period and n is the sample of CV patients (423), thus k = 917/423 = 2. Thus with an interval of 2, CV patients were selected based on their order of registration and this continued until the sample number was reached.
Data collection tools and procedures
A structured administrative questionnaire was adapted and modified from various literature studies to collect data including socio-demographic characteristics, attitude toward RPM, technological factors, clinical factors, healthcare access, and willingness to use remote monitoring (35–37). The content validity of the questionnaire was checked, and the reliability was calculated using Cronbach's alpha coefficient (=0.70), which was acceptable. The questionnaire was first prepared in English and then translated into the local Amharic language and back into English by experts to ensure consistency.
Data quality control
A pre-test was conducted outside the actual study sites among 10% of CV patients; before the actual data collection, modifications were made based on the pre-test. Two interns and two bachelor of science (BSC) nurses participated as data collectors and supervisors, respectively. The data collectors and the supervisor were trained before participating in the actual data collection process. To create awareness of the purpose of the study, their rights, and confidentiality issues, sufficient time was given to respondents to read and fill in materials carefully. There was continuous supervision up to the end of data collection. After collecting the data, the supervisor and the investigator checked its consistency and completeness.
Data management and analysis
The data were collected using the KoboCollect tool and then checked, cleaned, and exported into Excel to reduce error and incompleteness. The data was exported and analyzed using STATA 14. The descriptive statistics results were expressed as mean, standard deviation, percentage, and frequency. Binary logistic regression was employed to identify factors associated with RPM use. Variables with a p-value ≤0.2 from the bi-variable analysis were considered during multivariable analysis. The multivariable logistic regression analysis was used to control potential confounders and identify significant factors associated with willingness to use RPM. The magnitude of the association between different independent variables and dependent variables was measured using adjusted odds ratios (AORs). The Hosmer–Lemeshow goodness of fit was used to test the model's fitness. Multi-collinearity between independent variables was assessed by checking their tolerance and variable inflation factors (VIF). A 95% CI and a p-value <0.05 were used to declare statistical significance.
Results
Socio-demographic characteristics
In total, 81.61% of the study participants had a willingness to use remote patient monitoring (95% CI = 77.4%–85.1%). A total of 397 cardiovascular patients participated in the study, with a response rate of 94%. The mean age of the study participants was 49 ± 13.19 years. More than half (51.64%) of the participants were males, and approximately 65% (258) were from urban areas. One-third of (31.7%) the participants had not received any formal education (Table 1).
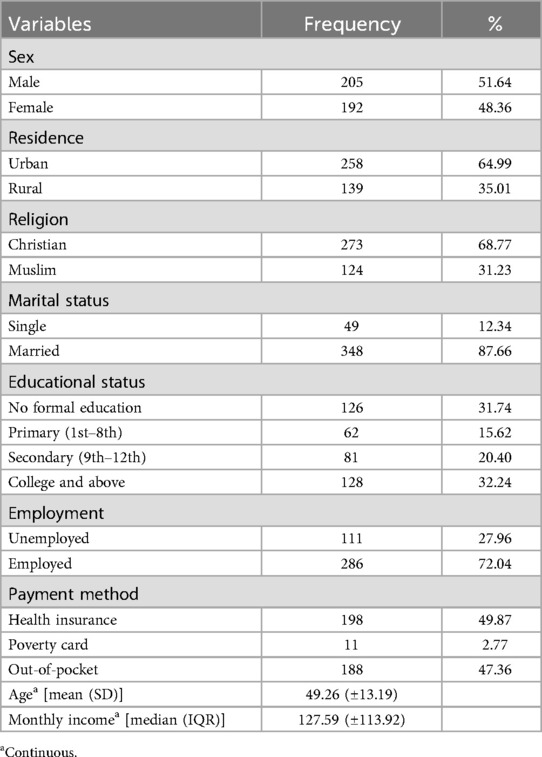
Table 1. Socio-demographic characteristics of cardiovascular patients in the referral hospitals, 2021 (n = 397).
Clinical characteristics of participants
In total, 55.92% of the study participants were classified as cardiac and 16.12% were hypertensive. More than half of the total participants (51.89%) were found to have comorbidities, of which 56.31% of the patients were found to have hypertension, 93.7% of patients were taking their medication orally, and 59.00% of the patients missed their follow-up due to COVID-19 (Table 2).
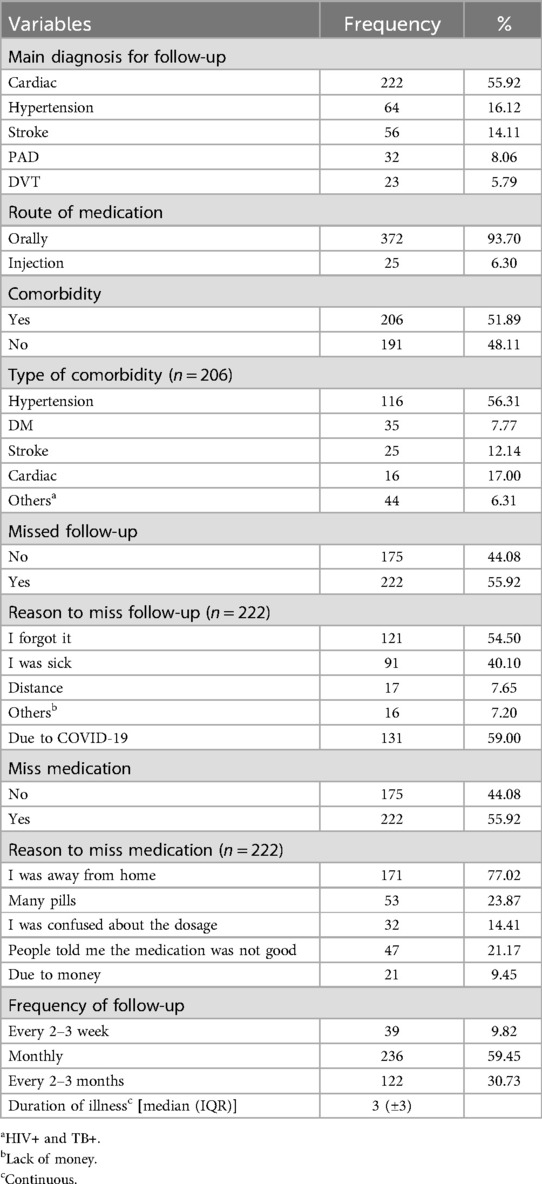
Table 2. Clinical characteristics of cardiovascular patients in the referral hospitals in 2021 (n = 397).
Technological factors
Of the total study participants, 80.86% were mobile phone users of which 52.03% were smartphone users (Table 3).
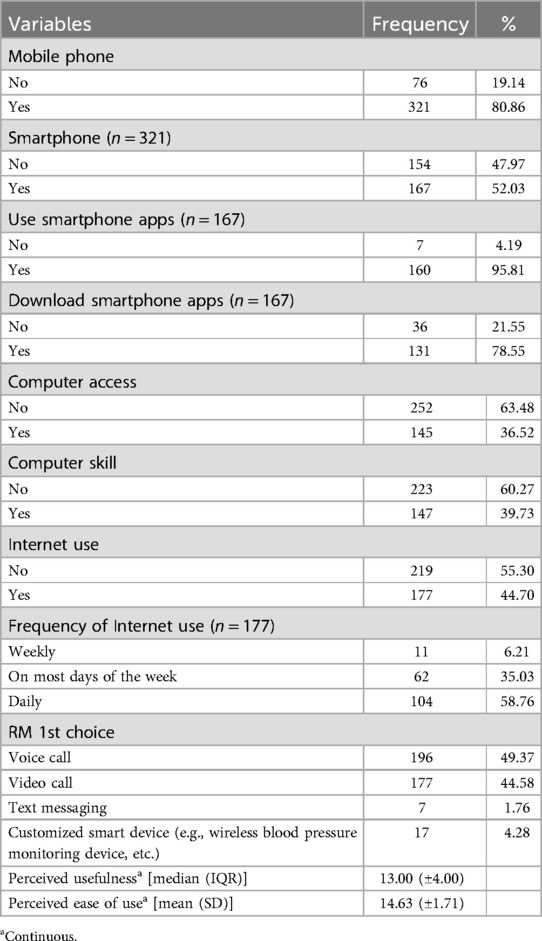
Table 3. Technological factors of cardiovascular patients in the referral hospitals, 2021 (n = 397).
Healthcare access
Of the total participants, 63.73% reported that traveling from home to the hospital was convenient, and of the study participants, 62.97% reported a bus as their mode of transport. Of the participants, the median traveling time was 1.5 h from home to the hospital to access healthcare services, and patients were waiting for more than 2 h during their follow-up day (Table 4).
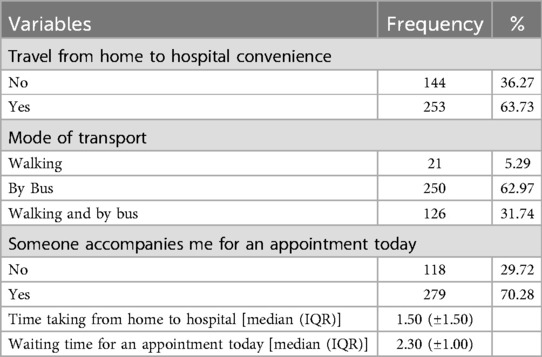
Table 4. Healthcare access factors of cardiovascular patients in the referral hospitals, 2021 (n = 397).
Factors associated with willingness to use remote patient monitoring
The study participant's age, perceived usefulness of RPM, and use of a mobile phone were significant factors associated with willingness to use remote patient monitoring among cardiovascular patients.
A year increase in the age of the patients decreased the odds of being willing to use remote monitoring by 6% (AOR = 0.94, 95% CI: 0.90–0.98). Cardiovascular patients who had mobile phones were five times more likely to use remote monitoring (AOR = 5.00 95% CI: 1.65–14.55). For a unit increase in a cardiovascular patient’s score of perceived usefulness of RPM, the odds of being willing to use remote monitoring increased by a factor of 1.5 (AOR = 1.50, 95% CI: 1.16–1.76) (Table 5).
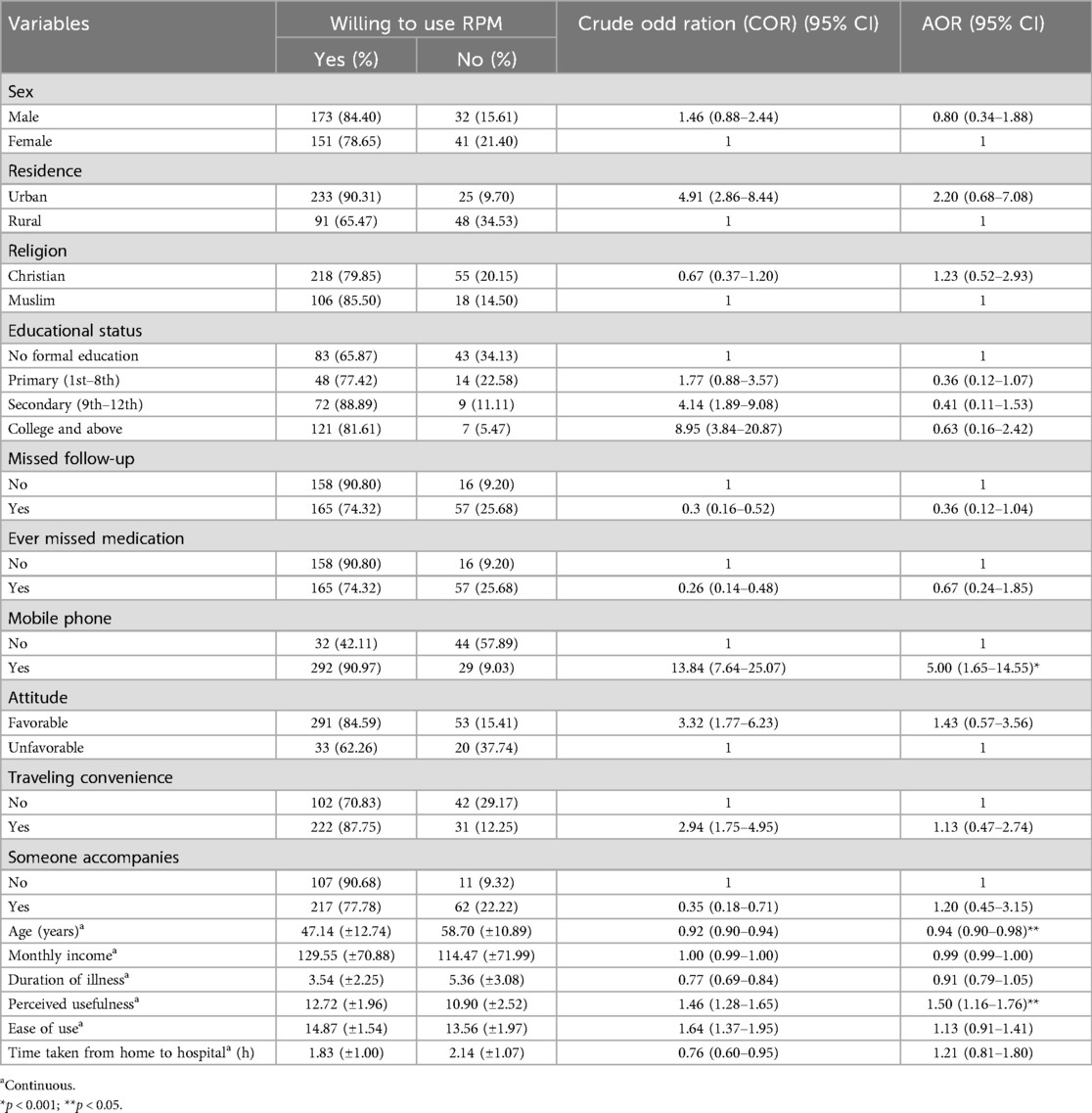
Table 5. Bi-variable multivariable logistic regression analysis of factors with the willingness to use remote monitoring among cardiovascular patients in the referral hospitals, 2021 (n = 397).
Discussion
Telemedicine has made significant strides in improving patient-to-provider communication, expanding access to previously underserved populations and places, and improving the delivery of healthcare. The study participant's age, the perceived usefulness of RPM, and the use of a mobile phone were significant factors associated with willingness to use remote patient monitoring among cardiovascular patients.
The study showed that 81.61% of cardiovascular patients were willing to use remote monitoring for their follow-up. This finding was in line with studies conducted in Honduras (38), Santiago (39), and Poland (40). However, this figure was higher than the findings from Nigeria (40), Singapore (38), and Canada (41). The discrepancies might be due to differences in socio-demographic variations. For instance, in the study conducted in Singapore, the participants were patients with diabetes mellitus type 2 (DM-2), whereas in our study, the participants were cardiovascular patients. In the study from Nigeria, the educational status of the participants was lower than that of the participants in our study. As for the difference in study setting, the studies mentioned above were conducted in primary care clinics, whereas the current study was done at teaching hospitals. Moreover, study period variation may be another possible reason for the observed discrepancies since technologies are improving over time (35, 38), which explains the increased use of remote monitoring in the current study compared to studies done in previous years. However, the current finding is lower than a study done in the USA (42). This variation might be due to patients’ experience with technology in the USA being higher than the current study’s participants (43).
Age, perceived usefulness of RPM, and having a mobile phone were significantly associated factors with the willingness to use remote patient monitoring. Our study showed that the odds of using remote monitoring decreased by 6% in response to a year increase in the age of the patients. A patient's willingness to use remote monitoring decreases as age increases. A possible reason for this might be that older patients are less willing to use technology than younger patients (due to lower intention toward technology, anxiety to use, concern about the security of information, and cost) which was evident in studies conducted in Germany (44, 45), Australia (46), China (47), and Canada (22).
The current finding showed that cardiovascular patients who had mobile phones were five times more likely to use remote monitoring. This finding is supported by studies done in Australia (46), China (47), Greece (48), and Kenya (49). We found that more than two-thirds of cardiovascular patients had mobile phones. The widespread use of mobile phones suggests an increase in the tendency to use remote monitoring (50). Currently, mobile phones are the preferable way to communicate with healthcare providers directly via text messaging or voice calls regardless of where they are located. This implies that patients may be willing to use remote monitoring for their health service demands if those services are launched.
Ethiopia has struggled to implement digital health for managing chronic disease to improve the health of society and effectively facilitate the delivery of healthcare services (51, 52). The current study showed that cardiovascular patients with higher perceived usefulness of RPM were 1.5 times more likely willing to use remote monitoring. However, scholars have shown that there are Internet connectivity issues or data transmission errors, privacy concerns, patient compliance issues, and the need for healthcare professionals to interpret and act upon the data effectively (53). Clinically, the data obtained through remote monitoring can be utilized in various ways. It can provide valuable insights into a patient's health status, allowing for early detection of potential issues, monitoring treatment effectiveness, and facilitating personalized healthcare management, which can aid in making informed clinical decisions and designing individualized interventions (54).
Different types of healthcare providers may follow such data, depending on the specific condition being monitored. It can be used by primary care physicians, specialists, nurses, and other healthcare professionals involved in the patient's care (55). The influence of remote monitoring data on interventions can be significant. It enables healthcare providers to intervene promptly and make timely adjustments to treatment plans based on real-time information. For example, if abnormal vital signs are detected, healthcare providers can initiate the appropriate interventions (56).
This finding is supported by studies conducted in Singapore (36), Sweden (57), and Taiwan (32), where patients’ willingness to use remote monitoring was found to be associated with their perception of the usefulness of the RPM technology. This may be because if patients perceive remote monitoring as useful, they have a propensity to use remote monitoring to manage their disease conditions to improve their health. The perceived usefulness of remote monitoring indicates one's acceptance and the perceived utility of remote monitoring and this will have a positive influence on a patient's willingness to use RPM (33).
Digital infrastructure, including strong network connectivity, and the development of different digital platforms to effectively collect and process data from cardiac patients to manage their healthcare conditions, will be crucial for evidence-based planning and decision-making (58, 59).
Conclusion
The study participants had a high willingness to use remote patient monitoring to maintain their health and quality of life and showed a substantial willingness to use remote patient monitoring. Age, the perceived usefulness of remote monitoring, and the use of a mobile phone were significantly associated with a willingness to use remote monitoring among cardiovascular patients.
This enabling finding should inspire policymakers, particularly the Ministry of Health, to enhance and broaden the use of remote monitoring technologies in healthcare services by encouraging cardiovascular patients to utilize remote patient monitoring technology for disease management.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Author contributions
MK: Conceptualization, Formal Analysis, Funding acquisition, Project administration, Validation, Visualization, Writing – original draft, Writing – review & editing. GA: Conceptualization, Funding acquisition, Investigation, Project administration, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. KS: Conceptualization, Supervision, Writing – original draft, Writing – review & editing. BT: Conceptualization, Funding acquisition, Investigation, Methodology, Project administration, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. BA: Conceptualization, Data curation, Formal Analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing.
Funding
The authors declare financial support was received for the research, authorship, and/or publication of this article. This study was supported by the University of Gondar (DDCF project) for data collection. University of Gondar (DDCF project) has no role in the design of the study, data collection, analysis, or interpretation of data, in the decisions on where, how, or when to publish in the peer-reviewed press, or preparation of the manuscript. The authors are entirely responsible for this paper's content.
Acknowledgments
We acknowledge the University of Gondar’s Institute of Public Health for giving us the chance to conduct this research and Doris Duke Charitable Foundation's (DDCF) financial support for data to improve the quality of people's lives through grants supporting the performing arts, environmental conservation, medical research, and child wellbeing, and through the preservation of the cultural and environmental legacy of Doris Duke's properties.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
AOR, adjusted odds ratio; CI, confidence interval; CV, cardiovascular; OR, odds ratio; UoG, University of Gondar; RPM, remote patient monitoring; NCD, non-communicable disease; WHO, World Health Organization.
References
1. Partridge EE, et al. Creating a 21st century global health agenda: the general assembly of the United Nations high level meeting on non-communicable diseases. Circulation. (2011) 123(25):3012–4. doi: 10.1161/CIR.0b013e31821c36ab
2. Balakumar P, Maung-U K, Jagadeesh G. Prevalence and prevention of cardiovascular disease and diabetes mellitus. Pharmacol Res. (2016) 113:600–9. doi: 10.1016/j.phrs.2016.09.040
3. World Health Organization. 2008–2013 action plan for the global strategy for the prevention and control of noncommunicable diseases: prevent and control cardiovascular diseases, cancers, chronic respiratory diseases and diabetes (2009). https://iris.who.int/bitstream/handle/10665/44009/9789241597418_jpn.pdf
4. Yuyun MF, et al. Cardiovascular diseases in sub-Saharan Africa compared to high-income countries: an epidemiological perspective. Glob Heart. (2020) 15(1).
5. Ali S, et al. The burden of cardiovascular diseases in Ethiopia from 1990 to 2017: evidence from the global burden of disease study. Int Health. (2021) 13(4):318–26. doi: 10.1093/inthealth/ihaa069
6. Girum T, et al. The burden of noncommunicable diseases in Ethiopia, 2000–2016: analysis of evidence from global burden of disease study 2016 and global health estimates 2016. Int J Chronic Dis. (2020) 2020(1):3679528.32149073
7. Misganaw A, et al. National mortality burden due to communicable, non-communicable, and other diseases in Ethiopia, 1990–2015: findings from the global burden of disease study 2015. Popul Health Metr. (2017) 15:1–17. doi: 10.1186/s12963-016-0118-9
8. Asmare MH, et al. Prevalence of rheumatic heart disease in a major referral cardiology clinic in Ethiopia: a retrospective cross-sectional study. PLoS One. (2021) 16(2):e0246519. doi: 10.1371/journal.pone.0246519
9. Nick JM, Roberts LR, Petersen AB. Effectiveness of telemonitoring on self-care behaviors among community-dwelling adults with heart failure: a quantitative systematic review. JBI Evid Synth. (2021) 19(10):2659–94. doi: 10.11124/JBIES-20-00329
10. Mcgonagle D. Since January 2020 Elsevier has created a COVID-19 resource centre with free information in English and Mandarin on the novel coronavirus COVID-19. The COVID-19 resource centre is hosted on Elsevier Connect, the company’s public news and information (2020). https://cir.nii.ac.jp/crid/1370576118741734285
11. Vlahu-Gjorgievska E, Nagapuri S, Win KT. Tele-monitoring technology as a tool for monitoring and management of patients with congestive heart failure. Australas J Inf Syst. (2019) 23. doi: 10.3127/ajis.v23i0.1816
12. Kulshreshtha A, et al. Use of remote monitoring to improve outcomes in patients with heart failure: a pilot trial. Int J Telemed Appl. (2010) 2010(1):870959.20508741
13. Grutters L, et al. Home telemonitoring makes early hospital discharge of COVID-19 patients possible. J Am Med Inform Assoc. (2020) 27(11):1825–7. doi: 10.1093/jamia/ocaa168
14. Crossley GH, et al. The CONNECT (clinical evaluation of remote notification to reduce time to clinical decision) trial: the value of wireless remote monitoring with automatic clinician alerts. J Am Coll Cardiol. (2011) 57(10):1181–9. doi: 10.1016/j.jacc.2010.12.012
15. Gous N, et al. The impact of digital technologies on point-of-care diagnostics in resource-limited settings. Expert Rev Mol Diagn. (2018) 18(4):385–97. doi: 10.1080/14737159.2018.1460205
16. Landolina M, et al. Remote monitoring reduces healthcare use and improves quality of care in heart failure patients with implantable defibrillators: the evolution of management strategies of heart failure patients with implantable defibrillators (EVOLVO) study. Circulation. (2012) 125(24):2985–92. doi: 10.1161/CIRCULATIONAHA.111.088971
17. Shull JG. Digital health and the state of interoperable electronic health records. JMIR Med Inform. (2019) 7(4):e12712. doi: 10.2196/12712
18. Condry MW, Quan XI. Remote patient monitoring technologies and markets. IEEE Eng Manag Rev. (2023) 51(3):59–64. doi: 10.1109/EMR.2023.3285688
19. Yong J, Lin D, Tan X-R. Primary prevention of cardiovascular disease in older adults in China. World J Clin Cases. (2017) 5(9):349. doi: 10.12998/wjcc.v5.i9.349
20. Yah CS, et al. Impact of telemonitoring approaches on integrated HIV and TB diagnosis and treatment interventions in sub-Saharan Africa: a scoping review. Health Promot Perspect. (2017) 7(2):60. doi: 10.15171/hpp.2017.12
21. Koehler F, et al. Efficacy of telemedical interventional management in patients with heart failure (TIM-HF2): a randomised, controlled, parallel-group, unmasked trial. Lancet. (2018) 392(10152):1047–57. doi: 10.1016/S0140-6736(18)31880-4
22. Seto E, et al. Attitudes of heart failure patients and healthcare providers towards mobile phone-based remote monitoring. J Med Internet Res. (2010) 12(4):e1627. doi: 10.2196/jmir.1627
23. Brahmbhatt DH, Cowie MR. Remote management of heart failure: an overview of telemonitoring technologies. Card Fail Rev. (2019) 5(2):86. doi: 10.15420/cfr.2019.5.3
24. Asch DA, Muller RW, Volpp KG. Automated hovering in health care—watching over the 5000 h. N Engl J Med. (2012) 367(1):1–3. doi: 10.1056/NEJMp1203869
25. Jiang X, Yao J, You JH. Telemonitoring versus usual care for elderly patients with heart failure discharged from the hospital in the United States: cost-effectiveness analysis. JMIR Mhealth Uhealth. (2020) 8(7):e17846. doi: 10.2196/17846
26. Morgan AU, et al. Remote monitoring of patients with COVID-19: design, implementation, and outcomes of the first 3,000 patients in COVID watch. NEJM Catal Innov Care Deliv. (2020) 1(4).
27. Manyati TK, Mutsau M. Exploring the effectiveness of telehealth interventions for diagnosis, contact tracing and care of Corona virus disease of 2019 (COVID19) patients in sub Saharan Africa: a rapid review. Health Technol (Berl). (2021) 11(2):341–8. doi: 10.1007/s12553-020-00485-8
28. Alebachew A, et al. Costs and resource needs for primary health care in Ethiopia: evidence to inform planning and budgeting for universal health coverage. Front Public Health. (2023) 11:1242314. doi: 10.3389/fpubh.2023.1242314
29. Little A, et al. Meeting community health worker needs for maternal health care service delivery using appropriate mobile technologies in Ethiopia. PLoS One. (2013) 8(10):e77563. doi: 10.1371/journal.pone.0077563
30. Nolte E, Knai C, Saltman R. Assessing chronic disease management in European health systems. Concepts and approaches (2014). https://researchonline.lshtm.ac.uk/id/eprint/2530940
31. Chang E, et al. Feasibility and acceptability of using a telehealth platform to monitor cardiovascular risk factors in hematopoietic cell transplantation survivors at risk for cardiovascular disease. Biol Blood Marrow Transplant. (2020) 26(6):1233–7. doi: 10.1016/j.bbmt.2020.02.027
32. Syed-Abdul S, et al. Virtual reality among the elderly: a usefulness and acceptance study from Taiwan. BMC Geriatr. (2019) 19:1–10. doi: 10.1186/s12877-019-1218-8
33. Holden RJ, Karsh B-T. The technology acceptance model: its past and its future in health care. J Biomed Inform. (2010) 43(1):159–72. doi: 10.1016/j.jbi.2009.07.002
34. Nayak A, et al. Remote patient monitoring (RPM) with biosensors: reforming healthcare beyond walls of hospital. In: 2024 International Conference on Advancements in Smart, Secure and Intelligent Computing (ASSIC) (2024). IEEE.
35. Liljeroos M, Thylén I, Strömberg A. Patients’ and nurses’ experiences and perceptions of remote monitoring of implantable cardiac defibrillators in heart failure: cross-sectional, descriptive, mixed methods study. J Med Internet Res. (2020) 22(9):e19550. doi: 10.2196/19550
36. Sin DYE, et al. Assessment of willingness to tele-monitoring interventions in patients with type 2 diabetes and/or hypertension in the public primary healthcare setting. BMC Med Inform Decis Mak. (2020) 20:1–11. doi: 10.1186/s12911-019-1002-x
37. Gorst SL, et al. Home telehealth uptake and continued use among heart failure and chronic obstructive pulmonary disease patients: a systematic review. Ann Behav Med. (2014) 48(3):323–36. doi: 10.1007/s12160-014-9607-x
38. Piette JD, et al. Access to mobile communication technology and willingness to participate in automated telemedicine calls among chronically ill patients in Honduras. Telemed J E Health. (2010) 16(10):1030–41. doi: 10.1089/tmj.2010.0074
39. Piette JD, et al. Use of telephone care in a cardiovascular disease management programme for type 2 diabetes patients in Santiago, Chile. Chronic Illn. (2006) 2(2):87–96. doi: 10.1177/17423953060020020401
40. Kowalska M, et al. Readiness for voice technology in patients with cardiovascular diseases: cross-sectional study. J Med Internet Res. (2020) 22(12):e20456. doi: 10.2196/20456
41. Edgar MC, et al. Telerehabilitation in stroke recovery: a survey on access and willingness to use low-cost consumer technologies. Telemed J E Health. (2017) 23(5):421–9. doi: 10.1089/tmj.2016.0129
42. Wiseman JT, et al. Conceptualizing smartphone use in outpatient wound assessment: patients’ and caregivers’ willingness to use technology. J Surg Res. (2015) 198(1):245–51. doi: 10.1016/j.jss.2015.05.011
43. Leonardsen A-CL, et al. Patient experiences with technology enabled care across healthcare settings—a systematic review. BMC Health Serv Res. (2020) 20:1–17. doi: 10.1186/s12913-019-4778-6
44. Illiger K, et al. Mobile technologies: expectancy, usage, and acceptance of clinical staff and patients at a university medical center. JMIR Mhealth Uhealth. (2014) 2(4):e3799. doi: 10.2196/mhealth.3799
45. Albrecht U-V, et al. Expectancy, usage and acceptance by general practitioners and patients: exploratory results from a study in the German outpatient sector. Digital Health. (2017) 3:2055207617695135.29942582
46. Bonner A, et al. Evaluating the prevalence and opportunity for technology use in chronic kidney disease patients: a cross-sectional study. BMC Nephrol. (2018) 19:1–8. doi: 10.1186/s12882-018-0830-8
47. Dai M, et al. Willingness to use mobile health in glaucoma patients. Telemed J E Health. (2017) 23(10):822–7. doi: 10.1089/tmj.2016.0254
48. Doupis J, et al. Smartphone-based technology in diabetes management. Diabetes Ther. (2020) 11(3):607–19. doi: 10.1007/s13300-020-00768-3
49. Miller CW, Himelhoch S. Acceptability of mobile phone technology for medication adherence interventions among HIV-positive patients at an urban clinic. AIDS Res Treat. (2013) 2013(1):670525.23997948
50. Logan AG, et al. Mobile phone–based remote patient monitoring system for management of hypertension in diabetic patients. Am J Hypertens. (2007) 20(9):942–8. doi: 10.1016/j.amjhyper.2007.03.020
51. Manyazewal T, et al. The potential use of digital health technologies in the African context: a systematic review of evidence from Ethiopia. NPJ Digit Med. (2021) 4(1):125. doi: 10.1038/s41746-021-00487-4
52. Getachew E, Woldeamanuel Y, Manyazewal T. Capacity and readiness assessment of healthcare facilities for digital health interventions against tuberculosis and HIV in Addis Ababa, Ethiopia. Front Digit Health. (2022) 4:821390. doi: 10.3389/fdgth.2022.821390
53. Uddin MA, et al. Continuous patient monitoring with a patient centric agent: a block architecture. IEEE Access. (2018) 6:32700–26. doi: 10.1109/ACCESS.2018.2846779
54. Cancela J, et al. Digital health in the era of personalized healthcare: opportunities and challenges for bringing research and patient care to a new level. Digit Health. (2021):7–31. doi: 10.1016/B978-0-12-820077-3.00002-X
55. Van Grootven B, et al. Experiences with the implementation of remote monitoring in patients with COVID-19: a qualitative study with patients and healthcare professionals. J Nurs Scholarsh. (2023) 55(1):67–78. doi: 10.1111/jnu.12814
56. Alanazi H, Daim T. Health technology diffusion: case of remote patient monitoring (RPM) for the care of senior population. Technol Soc. (2021) 66:101662. doi: 10.1016/j.techsoc.2021.101662
57. Lundell S, et al. Perceptions of home telemonitoring use among patients with chronic obstructive pulmonary disease: qualitative study. JMIR Mhealth Uhealth. (2020) 8(6):e16343. doi: 10.2196/16343
58. Konopik J, Blunck D. Development of an evidence-based conceptual model of the health care sector under digital transformation: integrative review. J Med Internet Res. (2023) 25:e41512. doi: 10.2196/41512
Keywords: cardiovascular disease, remote patient monitoring, non-communicable diseases, willingness, Ethiopia
Citation: Kassaw M, Amare G, Shitu K, Tilahun B and Assaye BT (2024) Willingness to use remote patient monitoring among cardiovascular patients in a resource-limited setting: a cross-sectional study. Front. Digit. Health 6:1437134. doi: 10.3389/fdgth.2024.1437134
Received: 23 May 2024; Accepted: 22 August 2024;
Published: 17 September 2024.
Edited by:
Saam Iranmanesh, Imperial College London, United KingdomReviewed by:
Panagiotis Katrakazas, Zelus_GR P.C., GreeceJoseph Hadaya, University of California, Los Angeles, United States
Copyright: © 2024 Kassaw, Amare, Shitu, Tilahun and Assaye. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mitiku Kassaw, YmF5dV90aWxhaHVuQGRtdS5lZHUuZXQ=
 Mitiku Kassaw1*
Mitiku Kassaw1* Getasew Amare
Getasew Amare Kegnie Shitu
Kegnie Shitu Bayou Tilahun Assaye
Bayou Tilahun Assaye