
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Digit. Health , 17 September 2024
Sec. Health Communications and Behavior Change
Volume 6 - 2024 | https://doi.org/10.3389/fdgth.2024.1404646
Background: A staff e-learning course was developed to prepare for scaling up a national take-home naloxone (THN) program in Norway. The aims of the study were to (a) describe participant characteristics for those that completed a THN e-learning course, (b) compare opioid overdose knowledge scores before and after e-learning course completion, and (c) to explore subsequent THN distribution by those trained.
Methods: This was a quasi-experimental pre-test, post-test longitudinal cohort study of individuals completing a THN e-learning course from April 2021 to May 2022. Frequency analyses were performed for participant characteristics and subsequent naloxone distributions at 1-week and 1-month follow-up. The opioid overdose knowledge scale (OOKS) was used to measure pre-test-post-test knowledge among participants. Wilcoxon signed-rank test was performed for comparison between pre-test and post-test. Effect size was calculated using Cohen criteria.
Results: In total, 371 individuals were included in this study. Most were either nurses or social workers (n = 277, 75%). Participant knowledge increased by medium or large effect for all items measured. At 1-month follow-up, 15% reported naloxone distribution. During the study period, 94 naloxone kits were distributed. Major reasons for not distributing were “clients not interested”, “workplace not distributing” and “workplace in process of distributing”.
Conclusions: Our findings suggest that an e-learning course is equally effective in terms of knowledge transfer as an in-person classroom setting, and may provide engagement in terms of naloxone distribution. However, our findings also emphasize the importance of clear implementation routines, including support from central coordinators to optimize the implementation process.
Over the last 30 years, take-home naloxone (THN) programs have been implemented in various settings globally, and are considered an important public health intervention to reduce opioid overdose harm including mortality (1, 2). While THN programs have been found effective in reducing overdose deaths when optimized and implemented on a large-scale (3, 4), researchers argue that THN programs still have not reached their full potential (1, 5, 6). This has been attributed to among other things as not being sufficiently widely implemented throughout communities, too modest distribution compared to the clinical need and lack of adequate pre-supplied naloxone (1, 5, 6). Further, increasing overdose mortality rates underline the importance of continuing to scale up efficient THN implementation strategies (7–10).
Scaling-up evidence-based public health interventions may reduce behavioral health problems on a population level (11). While researchers and implementers have developed guides, models, and frameworks for scaling-up public health interventions (11–15), the subject is still one of the major questions in prevention science (11). Zomahoun et al. (16) describe six potential pitfalls associated with the scaling-up of evidence-based interventions, including cost-effectiveness, top-down implementation and contextual issues. Facilitators for success have been identified as strong leadership, broad engagement among implementers, and tailoring to local contexts (17). Specific THN implementation barriers are related to workflow, logistics, staff roles and responsibilities, education, engagement and trainings (18, 19). Among facilitators for success were leadership support, basic education and training efforts, and simple access to the actual naloxone kit for clients at no cost (18).
The emergence of digital tools in public health have provided new possibilities for infrastructure and outreach (20, 21). The use of digital technologies in health promotion provide inexpensive means to collect and assess health data on an individual level, and may influence behavioral change on a population level (20). By applying digital technology to reinforce health and health care, e-health has become a significant part of the healthcare system, providing more efficient services and accuracy (21, 22). Like e-health, “e-learning” (learning facilitated by the application of information technology, communication, and electronic media) has been applied to numerous settings within healthcare (23–25). E-learning is regarded as a cost-effective facilitator for both learning and knowledge integration into practice (23, 26, 27). In addition, e-learning is accessible to a large audience, and thus may be an appropriate tool for scaling-up public health interventions (20, 25, 28).Other potential benefits are related to potential of unlimited access to complete, and repeat courses, and the consistency and streamlining of trainings.
While e-learning is a promising invention with an almost unlimited reach, there is limited research on the use of e-learning while scaling up staff trainings for THN. Simmons et al. (29) found that an online opioid overdose prevention training was both feasible and acceptable among first responders in Pennsylvania, and a well-suited tool for rapid expansion. Lai Joyce Chun et al. (30) found that most community pharmacists in Australia preferred online trainings or webinars to face-to-face sessions. However, neither assessed pre-test post-test knowledge, or the training's impact on engagement and subsequent naloxone distribution. While widespread access and acceptability from stakeholders (such as staff members and health professionals) is important when scaling up, subsequent naloxone distribution is a main desirable outcome (31, 32). In-person train-the-trainer courses have shown to increase knowledge among stakeholders and engage in subsequent THN distribution (33–35). However, the use of e-learning in healthcare has come with concerns related to the quality of knowledge in different disciplines and settings, loss of traditional face-to-face interactions, and poor engagement (20, 23, 36).
In Norway, a government-funded THN program has gradually expanded to increase naloxone accessibility throughout the country. When preparing for scaling-up of the THN program for national availability, an e-learning course was developed to replace the previous in-person staff training course. The objective was to improve staff training availability, and ultimately to improve naloxone accessibility on a national level. The aims of this paper are (a) to describe participant characteristics for those that completed a THN e-learning course, (b) compare opioid overdose knowledge scores before and after e-learning course completion, and (c) explore subsequent THN distribution by those trained.
This is a quasi-experimental, longitudinal study with pre-tests and post-tests of individuals who completed the Norwegian THN program's e-learning course. The recruitment period was from April 2021 to May 2022, with a 1-week and 1-month follow-up period for each participant.
In 2014, the Norwegian government funded a multifaceted overdose prevention strategy (37). One of the main measures in the strategy was the introduction of a THN program. At the time of initiation, the THN program was piloted in the two cities with the highest overdose mortality rates in Norway: Oslo and Bergen. The objective was to implement THN in existing low-threshold services for people who use drugs, primarily among those outside of formal treatment services. Central coordinators would approach relevant services, facilitating them for distribution by conducting trainings and provide them with naloxone kits. Naloxone kits were distributed without individual prescription and were free of charge for clients. A face-to-face train-the-trainer course was developed to facilitate for large-scale distribution, and any staff members who were trained could distribute (33). Central coordinators conducted the 90-min staff trainings and provided guidance and support for new distribution sites through the implementation stage (33).
The program had continuous geographical expansion from 2016, and new municipalities were prioritized and included based on their annual overdose mortality numbers. By 2021, 63 municipalities were included in the program. At the time of this study, over 100 distribution sites were included, and approximately 1,500 staff members had attended the face-to-face train-the-trainer course since program initiation (38). Distribution sites expanded to include additional low-threshold facilities, treatment centers, street outreach, and prisons. Throughout the expansion, the face-to-face train-the-trainer trainings became unsustainable to meet the growing program's needs. The program therefore introduced an e-learning course to improve staff training availability, and ultimately to improve naloxone accessibility on a national level.
The original in-person train-the-trainer course was adapted into a seven-module e-learning course. Each module covered different topics: (1) introduction, (2) the scope of the overdose problem, (3) opioid overdoses and naloxone, (4) overdose prevention, (5) overdose response, (6) summary and practical information, (7) project documentation. Quizzes were embedded throughout. When all modules were completed, a final exam became available. The exam was adapted from the opioid overdose knowledge scale (OOKS) and consisted of a multiple choice and checkbox questionnaire, examining course participants in opioid overdose knowledge. Completing the course and the exam would take an estimated 30–50 min. Completing the exam was a prerequisite for a staff member to distribute naloxone. Those who completed the exam received a course completion certificate.
The e-learning course is available through the THN website for anyone to participate. When the e-learning course was launched, project coordinators recruited potential participants by informing both existing and future distribution sites via e-mail. Information on the new e-learning course was also posted on the THN program's Facebook page. All course participants had to register with an e-mail address and a mobile phone number to access the course.
During the study period, all course participants were directed to the study information sheet and consent form. Consenting participants were directed to the initial study questionnaire and the OOKS pre-test before they were directed to the e-learning course. Participants were not informed whether their answers were correct or incorrect. All modules were accessible for repetitions at any time. The integrated exam (accessible after all modules were completed) had to be passed (80% correct answers) for the post-test and follow-up questionnaires to be sent out. If a participant did not pass the exam, they could retake it as many times they wanted in order to pass.
A link with the OOKS post-test and 1-week follow-up questionnaire were sent out via email 1 week after the exam was passed. A link with the 1-month follow-up questionnaire was sent out 1 month after the exam was passed. Those who did not complete the 1-week follow-up would still receive the 1 month-follow-up questionnaire.
Participants in this study were individuals who completed the e-learning course (with the integrated exam) and completed pre- and post- tests. Participation was voluntary and anyone who accessed the e-learning course could complete the training.
The OOKS was used for the pre-test, the exam and the post-test. The OOKS assesses knowledge using the following items: risk factors for overdose, signs of an overdose, response to an overdose, and naloxone use. The questionnaire has proven to be internally reliable (39). The OOKS was translated into Norwegian by the first author in close cooperation with the other authors. Two questions were removed from the original questionnaire as they applied to injectable naloxone, whereas this project uses only intranasal naloxone. This adjustment removed six points off the original scale, and consequently resulted in scores between 0 and 39 [risks (0–9), signs (0–10), action (0–11), naloxone use (0–9), and knowledge total (0–39)].
The initial questionnaire included the following variables: age, gender, region (by municipality), profession (nurse, social worker, physician, psychologist, other), employment sector (municipality health service, specialist health service, non-profit organization, private, prison, police/security, other), previous THN training (no, yes), and if yes: time since previous training (never, more than 6 months, last 6 months).
The follow-up questionnaire explored naloxone distribution 1 week and 1 month following e-learning completion. Those who reported naloxone distribution were asked to provide the number of kits distributed. If they reported no distribution, they were asked “why” choosing from the following alternatives: workplace not distributing, clients not interested, I do not feel competent and other. Those who answered “other” were asked to elaborate in a free-text box.
The free-text responses were systematically coded and grouped into the following additional categories: “workplace in process of distributing”, “naloxone use for staff only”, “not relevant for our clients”, “not relevant for job position”, “other colleagues have distributed”.
Frequency analyses were performed for participants completing the initial questionnaire and for those completing the follow-up questionnaire at 1 week and 1 month. For the free text responses, thematic analyses were used. The responses were coded into categories and included in the results for the follow-up questionnaire. Wilcoxon signed-rank test was performed for comparison between pre-test and post-test OOKS for all four items and total. Effect size was calculated using Cohen criteria (small effect 0.1, medium effect 0.3, and large effect 0.5) (40). All analyses were completed in IBM SPSS Statistics 28.
Further, considering that a proportion of those consenting for the study were lost to follow-up throughout the stages of the follow-up period, we conducted chi-square tests of differences between those completing and non-completers’ demographical variables gender, work sector, previous training and profession. This was also the case for the follow-up-losses between 1 week and 1 month. No significantly differences were measured, therefore analysis were not presented in the manuscript.
The Norwegian Centre for Research Data (project number: 614874) confirmed that the project processed personal data in accordance with data collection legislation.
Of the 1,122 people registered for the e-learning course during the study period, 733 (65%) consented to participate in the study. Of the 733, 21 (3%) did not complete the pre-test, 106 (15%) did not complete the course (Four due to not passing the exam), and 235 (21%) did not complete the post-test. Thus, 371 (33%) persons completed the course, pre-test, and post-test and were included in the study (Figure 1).
The majority of the participants were female (n = 293, 79%) with a mean age of 41 years old (SD = 11.5) (Table 1). Nurses and social workers made up the two largest groups of professions (n = 277, 75%). Most of the participants were either employed within the municipality health service or the specialist health service (n = 310, 84%). Most had never previously attended a naloxone course (n = 321, 87%). Of those who previously attended a naloxone course, most reported that it was more than 6 months ago (n = 43, 86%).
There was a significant increase in knowledge for all items (Table 2). The items with the most improvement were “naloxone use” (r = −0.50) and “knowledge total” (r = −0.54), which both exhibited a large effect size. For the remaining items (risks, signs and action), the improved effect size was medium. The total average of correct answers increased from 85% in the pre-test to 94% in the post-test.
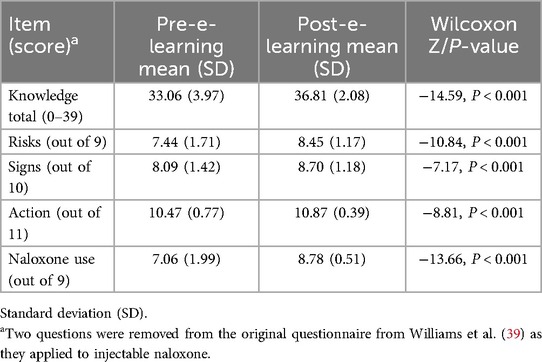
Table 2. Participant responses to opioid overdose knowledge scale, prior to and 1 week following e-learning course (n = 371).
There were 5% (n = 20) who reported naloxone distribution at 1-week follow-up, and 14.6% (n = 27) who reported naloxone distribution at 1-month follow-up (Table 3). Among those who reported no naloxone distribution at 1 week (n = 347, 94%), 5% (n = 19) reported to have distributed naloxone at 1 month. In addition, 60% (n = 12) of those who reported naloxone distribution at 1 week, did not respond to follow-up at 1 month. Consequently, though 27 individuals reported naloxone distribution at the 1-month follow-up, the total number of individuals reporting naloxone distribution during the follow-up period was 39 (10.5%). At 1-week follow-up, 20 participants reported to have distributed 50 naloxone kits. Further, at one-month follow-up an additional 44 kits had been distributed. Those who reported naloxone distribution at either time point reported a total of 94 naloxone kits distributed.
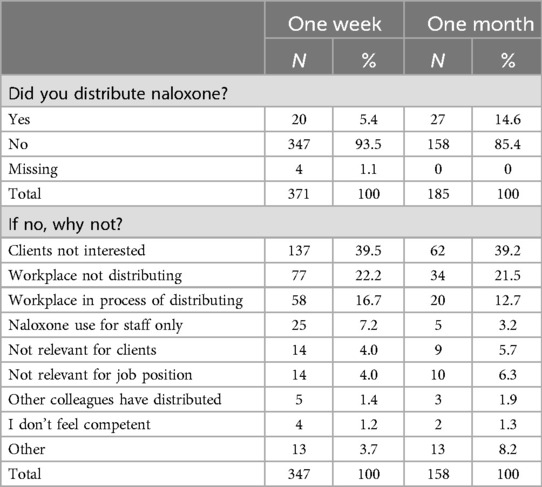
Table 3. Participant naloxone distribution and reasons for not distributing, at 1 week and 1-month follow-up.
Several reasons for not distributing were reported and listed in Table 3. After 1 week, 40% (n = 137) reported that “no clients had wanted naloxone”, and 39% reported either that “workplace not distributing” or “workplace in process of distributing”.
We found that a THN staff e-learning course reached out to relevant stakeholders, and that participants increased opioid overdose knowledge scores for all items, particularly for items relating to naloxone use. The mean overall knowledge scores increased by 9% points from pre-test to post-test (from 85% to 94%). At 1-week follow-up 20 participants reported to have distributed 50 naloxone kits. Further, at 1-month follow-up an additional 44 kits had been distributed. Consequently, within the 1-month follow-up period, 39 participants reported to have distributed 94 naloxone kits.
In 13 months, the e-learning course reached out to three quarters of what the preceding face-to-face train-the-trainer-course did in 4 years (n = 1,122 vs. n = 1,500) (38). Most of the participants were either social workers or nurses (n = 277, 75%) within the health service, suggesting that the e-learning course reached out to relevant target groups (32, 41). In an earlier stage of the program, Madah-Amiri, Clausen and Lobmaier (33) found that 69% of those trained in the in-person train-the-trainer course were either nurses or social workers. While the wide-reach potential of e-learning is a key element when scaling-up, concerns related to the quality of knowledge transfer in different disciplines and settings have been raised (23). In this study, we found similar increase in participant pre- test, post-test knowledge as described by others when assessing similar trainings in classroom settings (33, 34). While Madah-Amiri, Clausen and Lobmaier (33) found a slightly larger effect size in the items “naloxone use” and “overall knowledge”, participants in our study exhibited higher mean knowledge level in both pre-test and post-test. The high pre-test knowledge scores may indicate an accumulation of opioid overdose knowledge among professional health workers due to 7 years of the ongoing national overdose prevention strategy. Unlike Madah-Amiri, Clausen and Lobmaier (33) and Dahlem et al. (34) who measured post-test scores immediately after course completion, our findings found a high degree of knowledge retained 1 week after course completion.
In addition to train relevant target groups, reaching sufficient naloxone coverage is important for naloxone programs to make an impact (3, 31, 42, 43). We found that 39 (10.4%) participants reported to have distributed 94 naloxone kits within the follow-up month, which totals 36% of the monthly distribution rates in the THN program during the same period1. At the 1-month follow-up 15% of respondents reported to have distributed naloxone, threefold the proportion reporting distribution after 1 week. These findings are similar to what others have found elsewhere assessing in-person settings; Orfaly et al. (44) found that 20% of those trained in a train-the-trainer program conducted trainings within a 6 months follow-up period. Further, in relation to number of kits distributed, Dahlem et al. (34) found that training 109 participants in their train-the-trainer scheme resulted in a total of 137 naloxone kit distributions within a 6 month follow-up period.
We found that the most frequent reasons for not distributing naloxone were “clients not interested”, “workplace not distributing” and “workplace in process of distributing”. The former suggests that enquires have been made, implying some level of site interest. However, the proportion of participants reporting “workplace not distributing” and “workplace in process of distributing” may indicate a need to better streamline the training and implementation processes. The importance of role clarity, tailoring into local contexts, and in-hand naloxone-accessibility have been described by others as facilitating factors for implementation, staff engagement and subsequent naloxone distribution (17, 18, 45). Taken into account our findings, we support the importance of robust preparation, local adjustments, and particularly in-hand naloxone availability at e-learning completion. Further, through the expansion of the program, the coordinator role changed with the introduction of the e-learning course. The loss of face-to-face interactions due to the shift from in-person trainings to e-learning, seem to have led to less robust hands on support and implementation planning. Thus, our findings echo the benefit of a central facilitator, as suggested by others, to provide both guidance and support at the implementation stage, and to add flexibility to the e-learning (23, 46). Additionally, to further improve the scaling-up process, it has been recommended that the use of digital tools should be accompanied by resources for supplies and staffing, monitoring of overdose events to predict potential naloxone demand and provide support for people with lived experiences to become naloxone trainers (47).
There are several limitations to this study. The recruitment strategy was a nonrandom convenience sample, with no inclusion criteria in terms of professional background, and the e-learning course was open for anyone to take, which may have affected, representativeness, test-scores and subsequent naloxone distribution rates. Further, considering that a notable proportion of those consenting were lost either before course completion, or during the follow-up period, the study may have been prone to a loss-to-follow-up bias. However, no demographical differences between completers and non-completers were found when conducting chi-square tests, thus loss-to-follow-up bias was not likely to distort the results in a major way. Secondly, the relatively large proportion of participants reporting either “workplace not distributing” or “workplace in process of distributing”, may suggest that a longer follow-up period may have captured a more complete picture on subsequent staff engagement. Further, the validated OOKS-questionnaire was subject to some changes; we translated the questionnaire into Norwegian and removed two questions not relevant to the nasal device used in the program. In terms of translation, there are no validated OOKS-questionnaire in Norwegian. but validity have been tested for other languages than English (48). Despite these limitations, the study also had several strengths. The study was able to reach out to a large number of relevant stakeholders and staff members. Our pre-test-post-test longitudinal cohort design allowed us to assess data at three different time points. While others have assessed train-the-trainer classroom settings, our study provide novel information on both knowledge transfer and subsequent naloxone distribution succeeding an e-learning course. Further, by assessing reasons for not distributing naloxone, the findings may be used to inform future implementation and practices.
This study found that an e-learning course reached out to relevant stakeholders such as nurses and social workers working at relevant services for PWUD. Additionally, the participants who completed the THN e-learning course increased their knowledge in all items, to near completely correct levels. Our findings suggest that an e-learning course is equally effective in terms of knowledge transfer as an in-person classroom setting, and may provide engagement in terms of naloxone distribution. Further, our findings support that the e-learning delivery model effectively contributed staff education for the scaling-up of a national THN program. However, our findings also emphasize the importance of clear implementation routines, including support from central coordinators to optimize the implementation process.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving humans were approved by The Norwegian Centre for Research Data (project number: 614874) (SIKT) who confirmed that the project processed personal data in accordance with data collection legislation. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
ØE: Conceptualization, Data curation, Formal Analysis, Investigation, Writing – original draft, Writing – review & editing. DE: Conceptualization, Methodology, Supervision, Writing – review & editing. HB: Conceptualization, Methodology, Software, Supervision, Writing – review & editing. PL: Conceptualization, Methodology, Supervision, Writing – review & editing. TC: Conceptualization, Methodology, Supervision, Writing – review & editing.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. The first author holds a position as a PhD-student funded by the Directory of health as part of the national overdose prevention strategy.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
OOKS, opioid overdose knowledge scale; THN, take-home naloxone.
1. ^Norwegian Take-Home Naloxone Program. Naloxone Distribution Data. Oslo: University of Oslo (2014–2022). (retrieved December 04, 2022).
1. McDonald R, Campbell ND, Strang J. Twenty years of take-home naloxone for the prevention of overdose deaths from heroin and other opioids-conception and maturation. Drug Alcohol Depend. (2017) 178:176–87. doi: 10.1016/j.drugalcdep.2017.05.001
2. Moustaqim-Barrette A, Dhillon D, Ng J, Sundvick K, Ali F, Elton-Marshall T, et al. Take-home naloxone programs for suspected opioid overdose in community settings: a scoping umbrella review. BMC Public Health. (2021) 21(1):597. doi: 10.1186/s12889-021-10497-2
3. Walley AY, Xuan Z, Hackman HH, Quinn E, Doe-Simkins M, Sorensen-Alawad A, et al. Opioid overdose rates and implementation of overdose education and nasal naloxone distribution in Massachusetts: interrupted time series analysis. Br Med J. (2013) 346:f174. doi: 10.1136/bmj.f174
4. Townsend T, Blostein F, Doan T, Madson-Olson S, Galecki P, Hutton DW. Cost-effectiveness analysis of alternative naloxone distribution strategies: first responder and lay distribution in the United States. Int J Drug Policy. (2020) 75:102536. doi: 10.1016/j.drugpo.2019.07.031
5. Chimbar L, Moleta Y. Naloxone effectiveness: a systematic review. J Addict Nurs. (2018) 29(3):167–71. doi: 10.1097/JAN.0000000000000230
6. Black L, Connolly I, Getty M, Hogan C, Lennon P, Mc Cusker M, et al. Poor implementation of naloxone needs to be better understood in order to save lives. Addiction. (2017) 112(5):911–2. doi: 10.1111/add.13778
7. EMCDDA. European Drug Report 2022: Trends and Developments. Luxembourg: Publications Office of the European Union (2022).
8. Razaghizad A, Windle SB, Filion KB, Gore G, Kudrina I, Paraskevopoulos E, et al. The effect of overdose education and naloxone distribution: an umbrella review of systematic reviews. Am J Public Health. (2021) 111(8):e1–12. doi: 10.2105/AJPH.2021.306306
9. Kerensky T, Walley AY. Opioid overdose prevention and naloxone rescue kits: what we know and what we don’t know. Addict Sci Clin Pract. (2017) 12(1):4. doi: 10.1186/s13722-016-0068-3
10. Wenger LD, Doe-Simkins M, Wheeler E, Ongais L, Morris T, Bluthenthal RN, et al. Best practices for community-based overdose education and naloxone distribution programs: results from using the Delphi approach. Harm Reduct J. (2022) 19(1):55. doi: 10.1186/s12954-022-00639-z
11. Fagan AA, Bumbarger BK, Barth RP, Bradshaw CP, Cooper BR, Supplee LH, et al. Scaling up evidence-based interventions in US public systems to prevent behavioral health problems: challenges and opportunities. Prev Sci. (2019) 20(8):1147–68. doi: 10.1007/s11121-019-01048-8
12. Catalano RF, Fagan AA, Gavin LE, Greenberg MT, Irwin CE, Ross DA, et al. Worldwide application of prevention science in adolescent health. Lancet. (2012) 379(9826):1653-64. doi: 10.1016/S0140-6736(12)60238-4
13. Barker PM, Reid A, Schall MW. A framework for scaling up health interventions: lessons from large-scale improvement initiatives in Africa. Implement Sci. (2016) 11(1):12. doi: 10.1186/s13012-016-0374-x
14. Hawkins JD, Jenson JM, Catalano R, Fraser MW, Botvin GJ, Shapiro V, et al. Unleashing the power of prevention. Am J Med Res. (2016) 3(1):39. doi: 10.22381/AJMR3120162
15. World Health O, ExpandNet. Nine Steps for Developing a Scaling-Up Strategy. Geneva: World Health Organization (2010).
16. Zomahoun HTV, Ben Charif A, Freitas A, Garvelink MM, Menear M, Dugas M, et al. The pitfalls of scaling up evidence-based interventions in health. Glob Health Action. (2019) 12(1):1670449. doi: 10.1080/16549716.2019.1670449
17. Milat A, Newson R, King L, Rissel C, Wolfenden L, Bauman A, et al. A guide to scaling up population health interventions. Public Health Res Pract. (2016) 26(1):e2611604. doi: 10.17061/phrp2611604
18. Drainoni M-L, Koppelman EA, Feldman JA, Walley AY, Mitchell PM, Ellison J, et al. Why is it so hard to implement change? A qualitative examination of barriers and facilitators to distribution of naloxone for overdose prevention in a safety net environment. BMC Res Notes. (2016) 9(1):465. doi: 10.1186/s13104-016-2268-z
19. Davis CS, Walley AY, Bridger CM. Lessons learned from the expansion of naloxone access in Massachusetts and North Carolina. J Law Med Ethics. (2015) 43(Suppl 1):19–22. doi: 10.1111/jlme.12208
20. Koh A, Swanepoel DW, Ling A, Ho BL, Tan SY, Lim J. Digital health promotion: promise and peril. Health Promot Int. (2021) 36(Supplement_1):i70–80. doi: 10.1093/heapro/daab134
21. Ossebaard HC, Van Gemert-Pijnen L. eHealth and quality in health care: implementation time. Int J Qual Health Care. (2016) 28(3):415–9. doi: 10.1093/intqhc/mzw032
22. da Fonseca MH, Kovaleski F, Picinin CT, Pedroso B, Rubbo P. E-Health practices and technologies: a systematic review from 2014 to 2019. Healthcare (Basel). (2021) 9(9):1192. doi: 10.3390/healthcare9091192
23. Regmi K, Jones L. A systematic review of the factors—enablers and barriers—affecting e-learning in health sciences education. BMC Med Educ. (2020) 20(1):91. doi: 10.1186/s12909-020-02007-6
24. Guri-Rosenblit S. “Distance education” and “e-learning”: not the same thing. High Educ. (2005) 49(4):467–93. doi: 10.1007/s10734-004-0040-0
25. Ruggeri K, Farrington C, Brayne C. A global model for effective use and evaluation of e-learning in health. Telemed E-Health. (2013) 19(4):312–21. doi: 10.1089/tmj.2012.0175
26. Frehywot S, Vovides Y, Talib Z, Mikhail N, Ross H, Wohltjen H, et al. E-learning in medical education in resource constrained low- and middle-income countries. Hum Resour Health. (2013) 11(1):4. doi: 10.1186/1478-4491-11-4
27. Gunasekaran A, McNeil RD, Shaul D. E-learning: research and applications. Ind Commer Train. (2002) 34(2):44–53. doi: 10.1108/00197850210417528
28. Bitanihirwe BK. Scaling-up innovation as a means of tackling health inequalities. Commentary. Ann Ist Super Sanita. (2016) 52(2):143–5. doi: 10.4415/ANN_16_02_01
29. Simmons J, Rajan S, Goldsamt L, Elliott L. Implementation of online opioid overdose prevention, recognition and response trainings for professional first responders: year 1 survey results. Drug Alcohol Depend. (2016) 169:1–4. doi: 10.1016/j.drugalcdep.2016.10.003
30. Lai Joyce Chun K, Olsen A, Taing MW, Clavarino A, Hollingworth S, Dwyer R, et al. How prepared are pharmacists to provide over-the-counter naloxone? The role of previous education and new training opportunities. Res Social Adm Pharm. (2019) 15(8):1014–20. doi: 10.1016/j.sapharm.2019.03.003
31. Madah-Amiri D. Opioid Overdoses and Overdose Prevention: The Establishment of Take-Home Naloxone in Norway. Oslo: University of Oslo (2017).
32. Wilder CM, Brason FW 2nd, Clark AK, Galanter M, Walley AY, Winstanley EL. Development and implementation of an opioid overdose prevention program within a preexisting substance use disorders treatment center. J Addict Med. (2014) 8(3):164–9. doi: 10.1097/ADM.0000000000000032
33. Madah-Amiri D, Clausen T, Lobmaier P. Utilizing a train-the-trainer model for multi-site naloxone distribution programs. Drug Alcohol Depend. (2016) 163:153–6. doi: 10.1016/j.drugalcdep.2016.04.007
34. Dahlem CH, Scalera M, Chen B, McCabe SE, Boyd CJ. Impact of the take ACTION train-the-trainer model of opioid overdose education with naloxone distribution– who benefits? Subst Abus. (2020) 41(4):485–92. doi: 10.1080/08897077.2019.1671946
35. Monds LA, Bravo M, Mills L, Malcolm A, Gilliver R, Wood W, et al. The overdose response with take home naloxone (ORTHN) project: evaluation of health worker training, attitudes and perceptions. Drug Alcohol Rev. (2022) 41(5):1085–94. doi: 10.1111/dar.13474
36. Sinclair PM, Kable A, Levett-Jones T, Booth D. The effectiveness of internet-based e-learning on clinician behaviour and patient outcomes: a systematic review. Int J Nurs Stud. (2016) 57:70–81. doi: 10.1016/j.ijnurstu.2016.01.011
37. Norwegian Directorate of Health. [Translated from Norwegian] National Overdose Prevention Strategy 2014–2017: “Sure you can be Drug Free, but First you Must Survive.” Oslo: Norwegian Directorate of Health (2014).
38. Norwegian Directorate of Health. [Translated from Norwegian] National Overdose Prevention Strategy 2019–2022: “Sure you can be Drug Free, but First you Must Survive”. Oslo: Norwegian Directorate of Health (2019).
39. Williams AV, Strang J, Marsden J. Development of opioid overdose knowledge (OOKS) and attitudes (OOAS) scales for take-home naloxone training evaluation. Drug Alcohol Depend. (2013) 132(1–2):383–6. doi: 10.1016/j.drugalcdep.2013.02.007
40. Tomczak M, Tomczak E. The need to report effect size estimates revisited. An overview of some recommended measures of effect size. Trends Sport Sci. (2014) 21:19–25.
41. WHO. Community Management of Opioid Overdose. Geneva: World Health Organization (2014). Report No.: 92-4-154881-9.
42. Bird SM, Parmar MK, Strang J. Take-home naloxone to prevent fatalities from opiate-overdose: protocol for Scotland’s public health policy evaluation, and a new measure to assess impact. Drugs (Abingdon Engl). (2015) 22(1):66–76. doi: 10.3109/09687637.2014.981509
43. Wheeler E, Jones TS, Gilbert MK, Davidson PJ. Opioid overdose prevention programs providing naloxone to laypersons—United States, 2014. MMWR Morb Mortal Wkly Rep. (2015) 64(23):631–5.26086633
44. Orfaly RA, Frances JC, Campbell P, Whittemore B, Joly B, Koh H. Train-the-trainer as an educational model in public health preparedness. J Public Health Manag Pract. (2005) 11:S123–7. doi: 10.1097/00124784-200511001-00021
45. Thylstrup B, Hesse M, Jørgensen M, Thiesen H. One opioid user saving another: the first study of an opioid overdose-reversal and naloxone distribution program addressing hard-to-reach drug scenes in Denmark. Harm Reduct J. (2019) 16(1):66. doi: 10.1186/s12954-019-0328-0
46. Gray M, Joy E, Plath D, Webb SA. Implementing evidence-based practice: a review of the empirical research literature. Res Soc Work Pract. (2012) 23(2):157–66. doi: 10.1177/1049731512467072
47. Young S, Williams S, Otterstatter M, Lee J, Buxton J. Lessons learned from ramping up a Canadian take home naloxone programme during a public health emergency: a mixed-methods study. BMJ Open. (2019) 9(10):e030046. doi: 10.1136/bmjopen-2019-030046
Keywords: staff training, overdose prevention, e-health, public health, scaling up
Citation: Ericson ØB, Eide D, Brendryen H, Lobmaier P and Clausen T (2024) Scaling up! Staff e-learning for a national take-home naloxone program. Front. Digit. Health 6:1404646. doi: 10.3389/fdgth.2024.1404646
Received: 21 March 2024; Accepted: 4 September 2024;
Published: 17 September 2024.
Edited by:
Dari Alhuwail, Kuwait University, KuwaitReviewed by:
Hannah Knudsen, University of Kentucky, United StatesCopyright: © 2024 Ericson, Eide, Brendryen, Lobmaier and Clausen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Øystein Bruun Ericson, by5iLmVyaWNzb25AbWVkaXNpbi51aW8ubm8=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.