- 1Institute of Public and Preventive Health, Augusta University, Augusta, GA, United States
- 2Department of Health Policy and Behavioral Sciences, School of Public Health, Georgia State University, Atlanta, GA, United States
- 3Department of Psychiatry and Behavioral Sciences, Medical College of Georgia, Augusta University, Augusta, GA, United States
- 4Medical University of South Carolina, Charleston, SC, United States
- 5Department of Pediatrics, McMaster University, Hamilton, ON, Canada
- 6Department of Psychiatry and Behavioral Neurosciences, McMaster University, Hamilton, ON, Canada
Introduction: Technology has been used in evidence-based child maltreatment (CM) programs for over a decade. Although advancements have been made, the extent of the application of technology in these programs, and its influence on parental and child outcomes, remains unclear within the context of changes that emerged because of the COVID-19 pandemic. This scoping review provides a contextualized overview and summary of the use of technology in evidence-based parenting and child programs serving families impacted by child maltreatment and the effects of technology-enhanced programs on target outcomes.
Materials and methods: Using Arksey and O'Malley's methodological framework, we searched seven databases to identify peer-reviewed and grey literature published in English from 2000 to 2023 on evidence-based programs, according to the California Evidence-Based Clearinghouse (CEBC), that included technological supports for two populations: at-risk parents for child maltreatment prevention, and children and youth 0–18 years exposed to child maltreatment. All study designs were included.
Results: Eight evidence-based parenting programs and one evidence-based child trauma program were identified as using technology across a total of 25 peer-reviewed articles and 2 peer-reviewed abstracts meeting inclusion criteria (n = 19 on parent-level programs; n = 8 on child-level programs). Four studies were published in the context of COVID-19. Two main uses of technology emerged: (1) remote programmatic delivery (i.e., delivering all or part of the program virtually using technology) and (2) programmatic enhancement (i.e., augmenting program content with technology). Improvements across parenting and child mental health and behavioral outcomes were generally observed.
Discussion: Technology use in evidence-based child maltreatment programs is not new; however, the small sample since the start of the COVID-19 pandemic in this review that met inclusion criteria highlight the dearth of research published on the topic. Findings also suggest the need for the inclusion of implementation outcomes related to adoption and engagement, which could inform equitable dissemination and implementation of these programs. Additional considerations for research and practice are discussed.
Introduction
Child maltreatment remains a national public health priority in the US with nearly 600,000 cases substantiated in 2021, and approximately 1,820 deaths related to singular or co-occurring incidents of physical abuse, sexual abuse emotional abuse, and neglect (1). More recent evidence suggests global physical abuse and psychological abuse rates of 18% and 39%, respectively, during the first years of the coronavirus pandemic, COVID-19 (2). Youth exposed to child maltreatment are vulnerable to a host of short- and long-term biological and psychosocial adverse outcomes (3–5). At-risk parents, the primary perpetrators of CM (1), may also be victims of trauma, and experience deficits in executive functioning and emotion regulation that amplify negative parenting behaviors (6–10). High-risk families experience several chronic stressors such as part-time employment, economic hardship, trauma history and mental health symptomology (8, 9). COVID-19 placed exceptional demands on high-risk minority families, who were at not only increased risk for contracting the virus, but at disproportionate risk of unemployment and psychosocial distress attributed to increases in financial and social support instabilities (11). Such disruptions to family routine and external resources have played a role in reports of increased burnout among caregivers (12), and the possibility of abuse against children (13–16).
An abundance of evidence exists for the effectiveness of evidence-based programs in addressing adverse outcomes among caregivers as well as child and youth victims. Of note, behaviorally-based child maltreatment prevention programs are founded on the assumption that child maltreatment risk resulting from parenting skill deficits can be improved by providing parents training in a repertoire of skills, using a specific instructional format that includes: (1) education or instruction on target skills, (2) behavioral modeling of target skills, (3) parent practice of skills through role plays and live practice with the child, and (4) feedback to parents (17). Importantly, these skills have been found to be critical to parent behavior change in a meta-analysis of parent training programs by Kaminski and colleagues (18). Research suggests that parenting programs for caregivers with increased risk of child maltreatment perpetration lead to reductions in child maltreatment potential, such as parental stress via self-report and biomarkers (19–21), as well as improvements in parent-child interactions, home safety, child healthcare skills, and other caregiver (e.g., maternal social support, maternal depression, non-violent discipline) and child outcomes (e.g., adaptive functioning, behavioral risk) (22–28).
Similar improvements are seen among youth engaged in evidence-based psychotherapeutic programs for child and youth trauma associated with child maltreatment exposure, which are often based in behavioral and cognitive restructuring frameworks as well as trauma-focused strategies to address the psychological impact of trauma among youth (29, 30). These programs may use multiple techniques over the course of treatment to change thoughts and behaviors of trauma-affected youth and their caregivers, such as psychoeducation and coping exercises (e.g., relaxation via breathing, meditation). For example, in the gold-standard child-sexual abuse intervention, Trauma-Focused Cognitive Behavioral Therapy (TF-CBT), providers implement components defined by the acronym “PRACTICE”: (1) psychoeducation and parenting, (2) relaxation, (3) affective expression and modulation, (4) cognitive coping, trauma narrative processing, (5) in vivo exposure, (6) conjoint parent-child sessions, and (7) enhancing safety (31). Such evidence-based programs are associated with notable changes across child behavior and mental health symptomology, including decreases in post-traumatic stress disorder symptomology, abuse-related fears, sexualized behavior, depression, anxiety, shame, and behavior problems among traumatized youth (29, 32–34).
Despite the proven effectiveness across these programs for both parents and children, reaching and retaining families in real-life practice is a substantial challenge in general. However, the availability and delivery of such scientifically supported programs were critical during the height of the pandemic, as the “pandemic paradox” (35) created by social distancing regulations to reduce spread of infection had unintended consequences for families; indeed, caregivers were placed at greater risk of stress in the household and child maltreatment perpetration. In response to national public health guidelines, agencies offering evidence-based practices rapidly adapted in-person delivery to a virtual delivery approach to prevent disruptions in service provision for vulnerable populations (36). In addition, telehealth guidelines were released for aforementioned well-supported behavioral treatment TF-CBT, which provided considerations for both providers and families on equipment, privacy, internet stability, and safety (37). As such, the pandemic heightened awareness of the utility and importance of digital platforms for services.
The field of child maltreatment prevention and treatment has considered technological platforms for program delivery and augmentation for over a decade prior to COVID-19 (the CDC first funded projects to explore such efforts in 2006), though dissemination and implementation of these approaches were very limited in standard practice (for examples, see the Introduction to the Special Issue on Using Technology to Address Child Maltreatment: Prevention, Intervention, and Research (38, 39). However, almost three years following the pandemic onset, it is unclear how the use of technology in practice has evolved to support child maltreatment evidence-based prevention and intervention program access and effectiveness. Because the pandemic necessitated the use of virtual program delivery, it is imperative that we learn from the data and information gathered prior to and during this period that can inform how we should move forward with leveraging telehealth and other technology to improve program access, efficiency, and effectiveness. For instance, preliminary data collected during 2020 suggest that virtual sessions are feasible for delivering child maltreatment programs typically delivered in the home (40, 41). Emerging evidence suggests that virtual and/or technology-augmented delivery of evidence-based child maltreatment programs originally designed to be delivered in person decrease program access barriers, improve program efficiency, increase family attendance and service completion, and lead to similar program outcomes as in-person delivery (41–44).
Yet, barriers exist for virtual delivery, including technology access, concerns about the quality of care, and how differing delivery approaches can impact program fidelity. Many questions remain, and thus, a comprehensive synopsis of technology use in practice across parent and child-level programs is needed to summarize evidence on not only these technological developments, but the effectiveness of these adaptations on measured outcomes among parent and child populations. This scoping review provides a contextualized overview and summary of the use technology in evidence-based parenting and child programs serving families impacted by child maltreatment, and the impact of technological methods, as available, on measured outcomes over the past two decades.
Materials and methods
Study design
A scoping review was chosen, in contrast to a systematic review, as the method of choice to synthesize and describe the breadth of available studies using various research methodologies without analytic comparisons, allowing for a comprehensive summary of the published literature that can guide future research directions as well as practice and policymaking (45). In accordance with Arksey and O'Malley's (46) framework, this scoping review included five stages of methodology: (1) development of specific review questions, including the definition of participants and establishment of inclusion criteria, (2) a comprehensive search of the published and grey literature; (3) selection of relevant studies; (4) charting of identified data; (5) summary and discussion of the results in the context of the field and future directions.
Identification of objectives and research questions
The objective of this research was to understand how technology can be better leveraged and understood to improve evidence-based child maltreatment programs. Our goals were to describe the evidence-based programs, the nature of technology incorporated, the nature of change across measured maltreatment-related outcomes.
As such, we posed the following questions:
(1) How has technology been used in evidence-based parenting and child/youth programs for child maltreatment from 2000 to 2023?
(2) What are the effects of technology-enhanced programs measured population outcomes?
Definitions
For the purposes of this review, evidence-based programs were defined as prevention programs at the parent level, or interventions at the child level rated as well-supported, supported, or promising through the Scientific Rating Scale established by the California Evidence-Based Clearinghouse (CEBC).
This review presents findings on two distinct populations affected by child maltreatment: parents and children. Parent populations were defined as the primary caregivers who are at-risk of perpetration or who have perpetrated child maltreatment. Child populations were defined as child or youth victims of child maltreatment, under 18 years of age.
Inclusion criteria
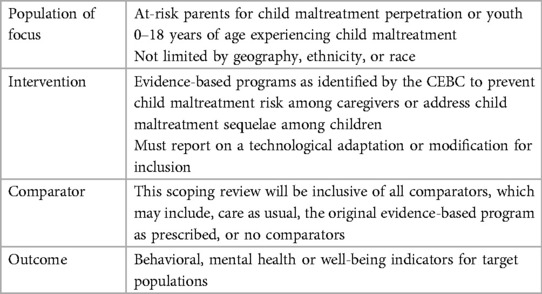
Eligibility criteria for studies were established using the PICO framework (i.e., participants, interventions, comparators, outcomes) as seen in Table 1. In general, this review included studies published in English from 2000 to 2023 on evidence-based programs for child maltreatment prevention among at-risk parents or evidence-based treatment for sequelae among children 0–18 years of age exposed to abuse. Of note, the year 2000 was chosen as a key period when close to 50% of Americans were using the internet (45), or likely used a cell phone (47), or owned a computer (48).
In addition, studies must have tested technological supports in the intervention for inclusion. Studies with provider informants reporting on population outcomes were also included in this work. All study designs were eligible for inclusion, such as pilot studies, qualitative accounts, cross-sectional studies, and effectiveness/efficacy trials. Exclusion criteria included protocol papers, discussion papers and field notes that did not include empirical data.
Identification of relevant published literature
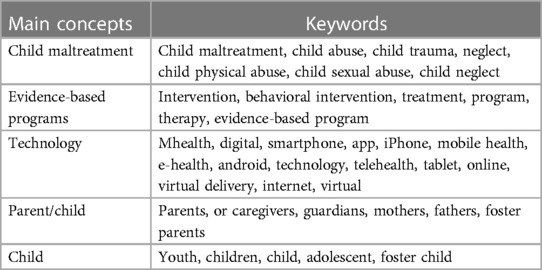
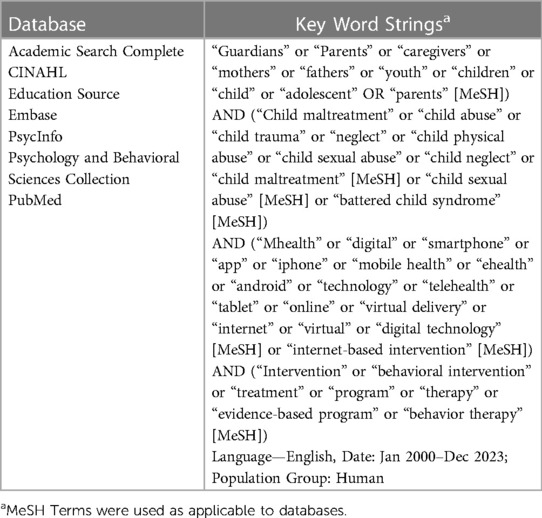
As mentioned, the review was designed to be inclusive of published peer-reviewed articles and select grey literature (e.g., conference abstracts, dissertations, reports) in the past two decades, between 2000 and 2023. The search extended across several subject areas including public health, psychology, medicine, education, and social work. Publications were identified using the following databases: Embase, Education Source, Academic Search Complete, PubMed, PsycINFO, CINAHL, and Psychology and Behavioral Sciences Collection. As recommended by Arksey and O'Malley (46), we worked with university librarians with expertise in scoping reviews to identify key words and execute a comprehensive search across databases. Searches were performed using identified key words and related MeSH terms across five domains of interest (see Tables 2, 3 for list of keywords and search strings, respectively).
Selection of relevant studies
A preliminary search of PubMed was conducted using key word string combinations and established MeSH terms. This step was taken to confirm the relevance of key terms in netting eligible articles. A comprehensive search across listed databases was conducted following the completion of the pilot literature search. Additional steps were taken to screen reference lists of retrieved and relevant publications. Special issues from leading family violence journals were also reviewed for completeness of search.
The research team uploaded retrieved citations into Endnote (49), a reference and citation manager, to facilitate organization of studies and duplicates removal. Following duplicates removal, the primary researcher created a comprehensive library that was used to screen relevant caregiver- and child-level publications. Screening procedures were conducted as follows: Three members of the research team (AT, MR, JG) independently screened titles and abstracts for eligibility criteria, keywords, and MeSH terms. All noted programs in publications were cross-compared to the CEBC for evidence-based intervention research ratings. Full-text articles were retrieved for all potentially relevant studies. We also retrieved full texts of articles with abstracts with ambiguous relevance during screening. At this stage, the three researchers screened retrieved articles for inclusion in results. Discrepancies were resolved by the lead researcher (AT) as they arose.
Data charting
Identical charting procedures were made for caregiver and child population findings as follows: Upon establishment of final eligible articles, two researchers used Microsoft Excel to first extrapolate study characteristics, including but not limited to: author information, publication year, publication type, population and sample size, location, intervention and evidence-based rating, technological adaptation identified, study design, and outcomes and/or key findings. Team members met as needed to discuss iterative changes as they emerged.
Results
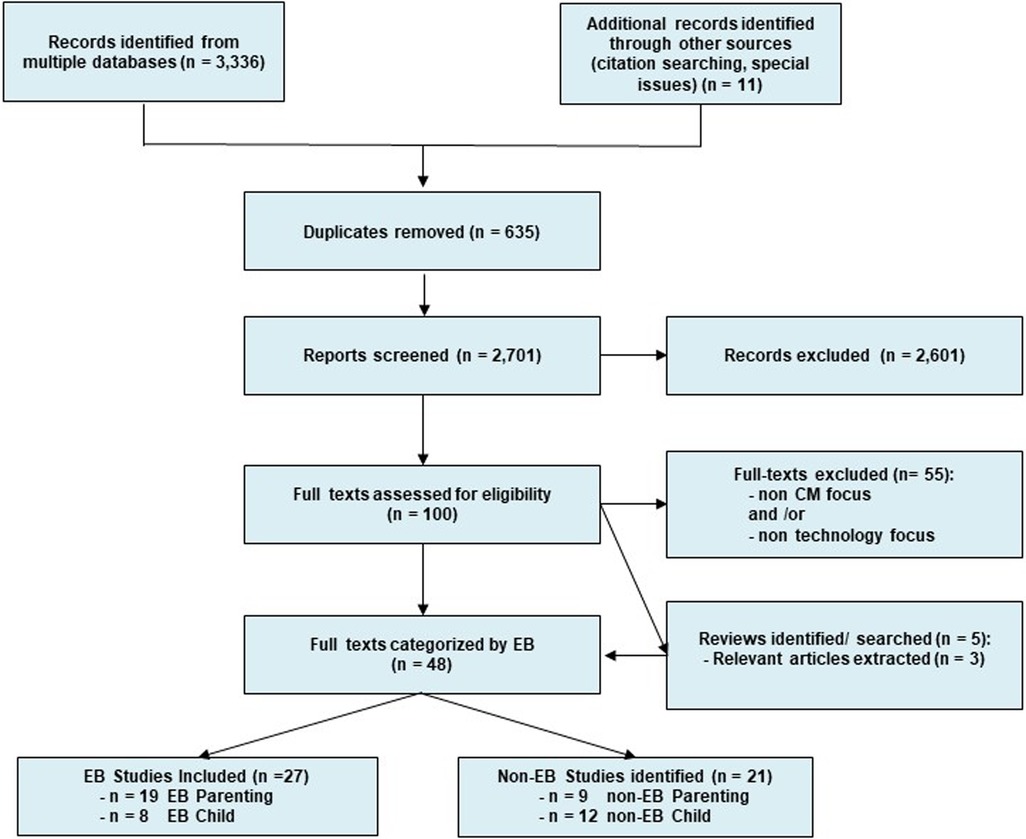
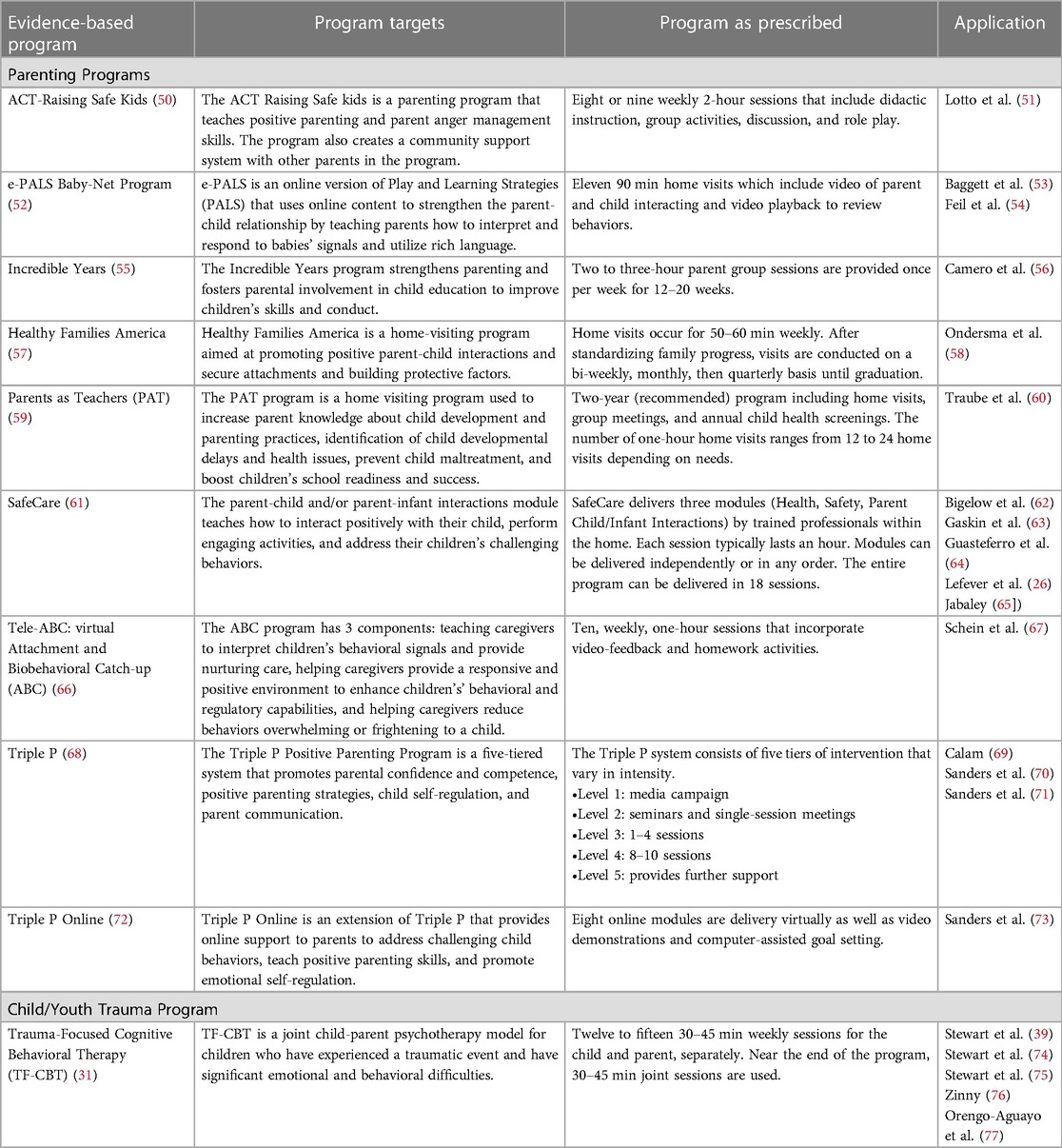
Figure 1 illustrates the flowchart of selection of final articles in the study. Using the previously mentioned key words, an initial search yielded 3,336 articles. Upon removal of 635 duplicate articles and an initial screening process removing 2,701 titles, we assessed 100 full text articles for eligibility criteria. Our final set of studies included 25 peer reviewed articles, and 2 peer-reviewed abstracts examining evidence-based parenting (n = 18 peer-reviewed articles; n = 1 peer-reviewed abstract), or child-level programs (n = 7 peer reviewed articles; n = 1 peer-reviewed abstract) using technology. Two major uses of technology across all programs emerged and were coded during data extraction—(1) remote programmatic delivery, or (2) programmatic enhancement. We define remote programmatic delivery as the complete, or hybrid use of virtual technology such as videos, recordings, or video conferencing platforms via data or internet channels to synchronously or asynchronously deliver all program components. Programmatic enhancements were defined as the use of technology to augment therapeutic content and goals in-person or between sessions. Below we summarize findings across the parent and child-level programs and report on the use or technology, and evaluation of program outcomes as available. An overview of all evidence-based parenting and youth/child programs identified can be found in Table 4.
Evidence-based parenting programs overview
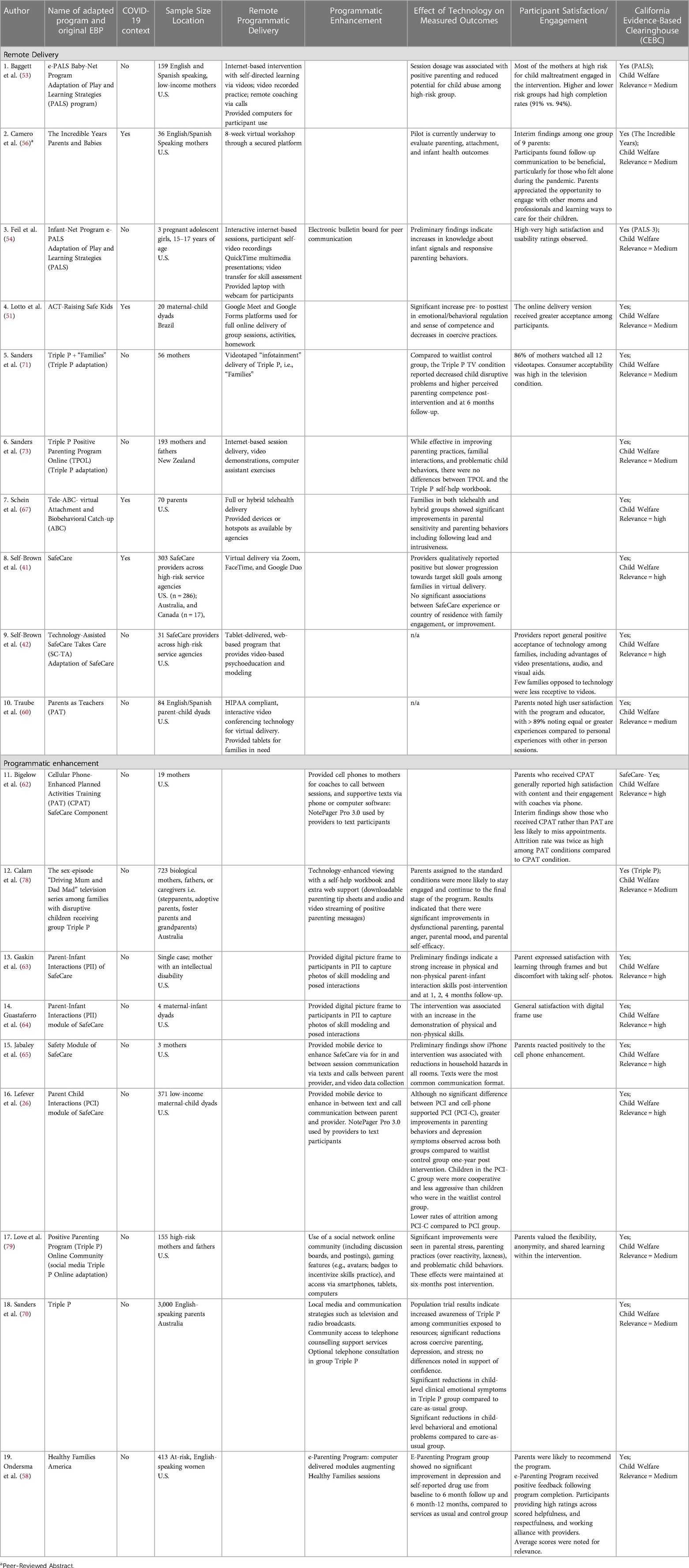
Nineteen studies (See Table 5) described or evaluated use of technology using data across the following eight evidence-based parenting programs: ACT Raising Safe Kids (n = 1), Attachment and Biobehavioral Catch-up (n = 1), Healthy Families America (n = 1), The Incredible Years (n = 1), Parents as Teachers (n = 1), Play and Learning Strategies (PALS) (n = 2), SafeCare (n = 7), and the Positive Parenting Program (Triple P) (n = 5). Data were available from five countries, including, the U.S., Australia, Brazil, Canada, and New Zealand, through single site and one multisite study. One study specifically focused on adolescent pregnant girls (54). Three studies provide reports in the context of the COVID-19 pandemic (41, 51, 56). Of these, two studies were conducted among providers engaged in parenting program delivery, who shared qualitative accounts of participant progress through the program (41, 42). A detailed description of findings across all studies is provided below, presented by type of technology used in programs.
Remote programmatic delivery
More than half of the included studies on evidence-based parenting programs (n = 10) reported on telehealth or online delivery of programmatic content. The majority of articles described full telehealth delivery of content. Only two described the use of hybrid, or asynchronous programmatic delivery to participants. Four studies noted provision of loaned equipment to facilitate remote delivery procedures to families (53, 54, 60, 67).
Measured improvements among participants following full telehealth program participation were noted across child maltreatment risk (51, 53, 65, 73), parenting skills and behaviors (51, 52, 63, 64, 67, 70, 71, 73), mental health (26, 60, 70), engagement in services (53, 62, 78) as well as child-level behaviors (26, 70, 71, 73, 79). Of note, two articles describe provider-level data, via qualitative inquiry, on parent acceptance or progression through remote delivery services. Self-Brown et al. (42) describe an early account of a web based SafeCare via tablet, in which providers noted positive reception among families, citing feasibility benefits to using audio and visual aids for programmatic delivery. Five years later, Self-Brown and colleagues (41) furthered virtual delivery work during the pandemic, citing virtual SafeCare delivery via web-based platforms among providers. While improvements across parental outcomes were noted, providers highlighted a slower progression towards targeted goals during virtual delivery compared to in-person sessions.
Among articles describing hybrid approaches and/or asynchronous delivery of services, Schein et al. (67) examined effects of telehealth as well as hybrid delivery of Attachment and Biobehavioral Catch-Up on parenting outcomes within the COVID-19 context, and cited significant improvements in parenting sensitivity and behaviors across both delivery formats. In a Triple P implementation study, Sanders et al. (70) cited the use of videotapes to facilitate content delivery, noting improvements across parenting confidence as well as child behavioral problems.
Enhancements
Eight studies on evidence-based parenting programs described alternative uses of technology, specifically to augment program delivery to families. Examples of technological enhancements included digital picture frames and mobile devices to facilitate in-person sessions, or direct external e-communication between parents and providers (26, 62, 64, 65), as well as web-supported audio and video content to supplement evidence-based program content (78). Of note, in many of these applications, participants were provided with needed technology devices during the intervention (26, 64, 65).
One additional technological enhancement was the optimization of the Healthy Families home visiting program though an internet-based, tablet delivered, eight session e-parenting program designed to address child maltreatment risk (58). The e-parenting program curriculum was grounded in three effective evidence-based models (i.e., SafeCare, motivational interviewing and cognitive retraining). Ondersma et al. (58) note the use of video-based skill modeling and feedback as part of the e-program. The enhancement demonstrated feasibility in its implementation, as well as positive reception among parents, but parent ratings of relevance were low. Improvements in maternal depression symptomology and perpetration risk were observed following intervention completion but were not maintained at 6 or 12 month follow up in comparison to services as usual and control groups (58).
Two studies also describe the use of online discussion forums as strategies for evidence-based programs to build group-based support systems among participating families (52, 79). One population-based study also described strategies for broad-based dissemination of programmatic material to increase program awareness in target communities (70).
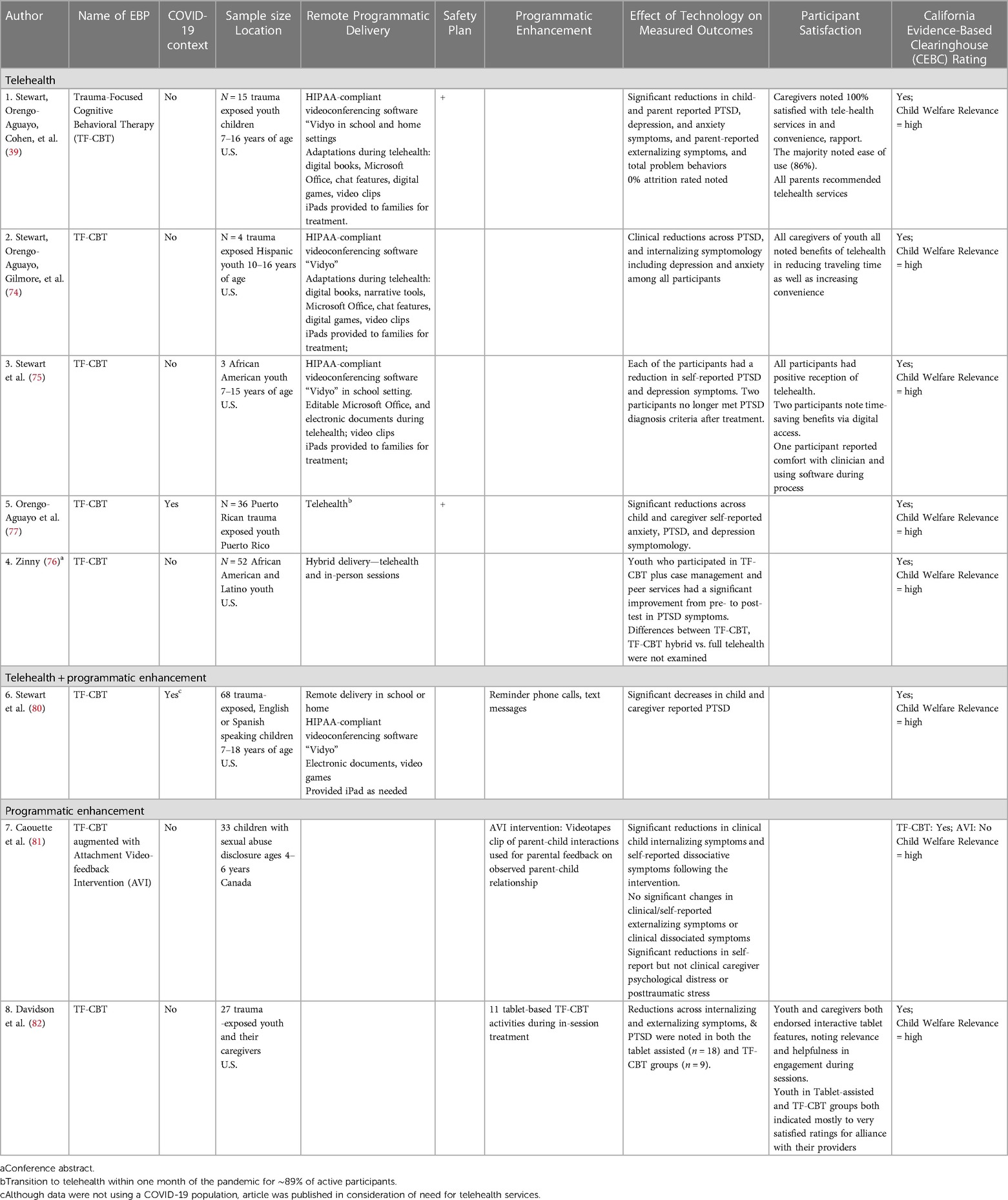
Evidence-based child focused trauma programs overview
Eight child-level intervention studies were identified for inclusion in this study (See Table 6), all examining effects of technology across one intervention, Trauma-Focused Cognitive Behavioral Therapy (TF-CBT). Data were collected from the U.S. (n = 6), Canada (n = 1), and Puerto Rico (n = 1). Importantly, only one study examined data collected during the pandemic COVID-19 context.
Remote programmatic delivery
Most studies (n = 6) described implementation of synchronous, virtual delivery via HIPAA compliant telehealth video conferencing software such as “Vidyo” to delivery program content (39, 74–77, 80). In several instances, families were provided with iPads during therapy to facilitate telehealth delivery [for examples, see: (74, 75, 80)]. As part of the TF-CBT telehealth process, several studies also cited the use of technological adaptations during delivery to meet the remote needs of children and youth. Sessions may have included use of digitized materials such as books, games, and video clips to convey content to clients. Additional software, including Microsoft Word and Adobe, were mentioned as applications allowing participants to make edits to documents that were shared with providers (39, 74, 75, 77, 80). Of note, one study also described the use of both remote delivery and supplemental enhancement strategies to increase engagement between sessions (80). In this work, providers contacted participants via calls and text messages for session and homework reminders.
Although safety assurance plans for youth were likely implemented during the pandemic, only two telehealth-based studies explicitly alluded to inclusion during implementation. For example, Orengo-Aguayo et al. (77) describe the use of consultation calls to review safety concerns among therapists as treatment sessions were conducted, whereas, Stewart and colleagues (39) detail strategies in school and home settings including regular communications and presence of school staff and presence of caregivers or trusted contacts during sessions.
Technological enhancements
Two studies were identified that presented unique augmentations to TF-CBT. Both studies were also published using data collected prior to the pandemic. While varying in approaches and purpose, both studies noted significant improvements across internalizing symptomology and post-traumatic stress disorder among participating youth. First, Davidson et al. (82) piloted “tablet TF-CBT”, which included 11 tablet-based activities targeting constructs within the TF-CBT model and general mental health programs, designed to increase provider-client engagement. These activities were built in consultation with providers and considered embedded under the category of “available tools for providers” in the fidelity monitoring process. Second, a Canadian study by Caouette et al. (81) piloted the embedment of an Attachment Video-feedback Intervention (AVI) with TF-CBT, to measure changes in parent-child relationships. AVI was integrated as a video-feedback component for caregivers during psychoeducation to address parent-child interactions. The authors describe that this discussion added half hour to session length, and that protocol for each intervention was followed as prescribed (81).
Discussion
This scoping review summarizes the use technology in evidence-based parenting child maltreatment prevention programs and child trauma therapy programs over the past two decades, inclusive of the recent COVID-19 pandemic years. We identified a total of eight parenting-focused programs, and one child-focused program across twenty-seven published works examining the use of technology in practice prior to, and since the onset of the pandemic. Our findings highlight the consistent presence of technology in remotely delivering services, and/or to enhance program content among target populations. Irrespective of the classification, technological advancements in practice were generally associated with positive parent and child mental health and behavioral outcomes in all geographic contexts and sample populations.
Although these results support the integration of technology in practice, the observed positive impact can be limited with low buy-in or feasibility in practice. However, review findings among parents and children across the 11 studies measuring participant satisfaction on the use of both telehealth and explored digital enhancements were generally encouraging. Indeed, these studies noted favorable reception or satisfaction rates among users, which may be a proxy indicator of perceived quality or engagement within these technologically advanced evidence-based programs. Conflicting findings, as with Ondersma et al. (58), may suggest otherwise, where positive reception to technology-based changes to programs did not equate to perceptions of relevance or positive program effects as observed. It is important to note; however, that the software included in this study, though very advanced at the time of the trial (2006–2009), holds very little relevance to the advancements that emerged in the last decade, and this could be a driver of the relatively poorer reception. Additionally, parent and child comfort and experience with using technology over the last decade has dramatically increased and has become standard in our social communications and general experiences with education, which could also substantially increase perceived relevance and satisfaction.
Other studies in this review, such as Baggett et al. (53) have shown that other feasibility indicators, such as increased session dosage, may be associated with stronger program outcomes. Collectively, these data emphasize that the investigation of associations between implementation measures and participant engagement, as well as with target outcomes among programs adopting technology is in its early stages at best, and even less explored in relation to specific uses such as telehealth and/or technological enhancements. Studies should include additional measured constructs across quality, dosage, and adherence for greater understanding of optimal approaches during program implementation.
While not a key focal population of this review, providers as the implementing agents of these evidence-based programs are a non-traditional but important group that can enhance our understanding of the feasibility and effectiveness of technological integration. Noting provider voice, in addition to clients, as part of development and testing of technology-based delivery approaches and augmentations is of utmost importance. Without provider or therapist buy-in to the use of technology as part of evidence-based practice delivery, there will be challenges with implementation. For example, Stewart et al. (74) described strong satisfaction amongst therapists with their telehealth delivery process, noting both comfort in using telehealth equipment as well as interactions with youth over digital technology. In contrast, in Self-Brown's (41) study on SafeCare implementation during the pandemic, providers described the logistic struggles faced by their families during telehealth delivery, as well as barriers in formatting program content and with conducting observational assessments using virtual delivery. General studies on therapist perspectives have also documented similar (83), as well as novel reflections on remote delivery considerations since the pandemic onset, such as quality and effectiveness of treatment (83–86), safety management in the home environment (85–87) and even provider virtual fatigue (83, 84). Such responses are key assessments that can shape directions for best practices for using technology in the context of human services.
COVID-19 context
An interesting observation from this review was the limited number of articles focused on technology use and effectiveness in the context of parenting and child programs published since the onset of the pandemic. This may be due in part to the arduous and lengthy process of peer-reviewed publication, which can take up to 2 years from time of submission to publication. However, the aforementioned recommendations across agencies to adopt telehealth suggests that many evidence-based programs were, indeed, utilizing such technology to meet the needs of families during the pandemic. The limited available evidence is promising, but more studies are sorely needed in this area.
Moreover, it is critical to explore how well these programs approached, or are approaching, implementation-related outcomes, especially fidelity monitoring, or protocol adherence measurement, in real-world practice as pragmatic adaptations during delivery were likely to occur. Fidelity is critical as programs implemented as designed are noted to achieve positive outcomes (88–90). Several of the parenting and child program studies published prior to the pandemic describe formal fidelity monitoring for telehealth as well as technological enhancements [data not shown; for examples, see: (42, 60, 82)]. Evidence-based parenting programs such as Parents as Teachers established support systems for technical assistance during telehealth delivery (60). In contrast, in their web-based application of SafeCare, Self-Brown and colleagues (42) note use of a provider fidelity checklist that accommodated adaptations made during the implementation of their web-based program. However, in the COVID-19 context, few have documented evidence of strong provider fidelity during implementation of a telehealth program (67, 77, 91, 92), and only one, included in the current study, with likely related effectiveness in improving parental outcomes (67).
Practice-based considerations
There is no dispute that real-time, digital delivery of programs can reduce geographic barriers for families who are likely burdened with numerous stressors. Our findings suggest that telehealth and programmatic enhancements are effective in increasing participation and improving outcomes among parent, youth, and child populations. Yet despite general satisfaction, positive indications of feasibility, and the unique position of telehealth options to alleviate geographic restrictions, developers and practitioners must continue to address formidable challenges around general program enrollment in addition to long waitlists as seen in child trauma programs, which may not be fixed with technology advents. Irrespective of how engaging a program may be, no observable effects will be noted without service-level supports and strong recruitment and retention strategies. Research must also focus on how well remotely delivered programs can effectively assess child safety, a hallmark of the child protection system in child maltreatment response. In other words, even in the presence of safety assurance plans, are providers able to accurately assess child safety and maltreatment risk, observing the home environment and key parent-child interactions?
Nonetheless, the use of various technological devices reflects the market of options available to assist with programmatic dissemination. As cell phones and tablets become more ubiquitous in use (47), these devices may become appropriate choices to engage with participants in and out of sessions and expand the reach of programmatic content. Uptake and incorporation of such technology in standard practice does come with caveats; as the question of digital equity regarding access to cellular data and connectivity remains (41), limiting the ecological validity of positive findings across highlighted efficacy studies in this review. We must continue to consider the present digital divide exacerbated by the pandemic (93), which faces many vulnerable families who are often the targets of these programs. One solution seen among studies was the provision of internet ready devices, which may assist with improving equity in access to care and higher engagement rates among parent and child populations. Yet, the removal of resource constraints among families will not address the logistic barriers seen at the provider level. For example, in the context of SafeCare during the pandemic, providers described logistic barriers with virtual translation of program content intended for in-person assessment, in which they experienced difficulties modeling skills and home assessments (41).
A key question regarding the inclusion of more technology-based applications in evidence-based programs then becomes, what information is potentially lost or enhanced in the process? In one school of thought, Mowbray et al. (94) classify essential programmatic content as structural (i.e., key components), or as process related (i.e., interactions, and rapport). If left unaddressed, logistic limitations could prohibit delivery of core program components and in turn, expected outcomes. It is encouraging to note that some programs are specifically addressing logistical limitations through tailoring of process-related content while maintaining structural content (i.e., fidelity to the model) when delivering interventions via telehealth (74). Promisingly, parent, youth and child accounts among included studies suggest that telehealth experiences and digital enhancements did not interfere with rapport building with providers (60). As we shift towards delivery with digital influences, programs should maintain some flexibility in delivery approaches, but rigor to the core components of the curriculum that is key to the mechanistic drivers of outcomes must be incorporated to ensure expected outcomes. Moving forward, technology could also be used in precision home visiting to strengthen the implementation of core components and efficiency of programs to serve the needs of diverse populations.
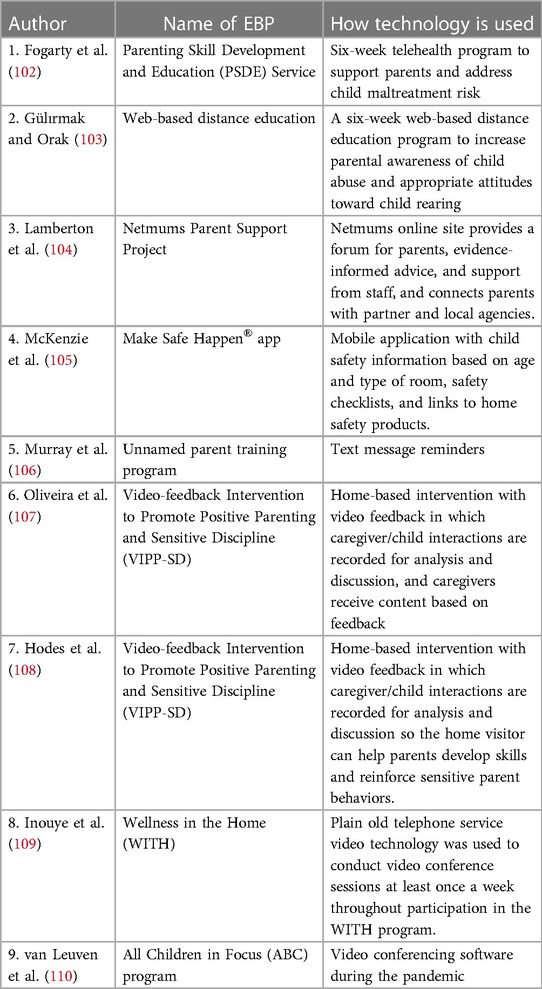
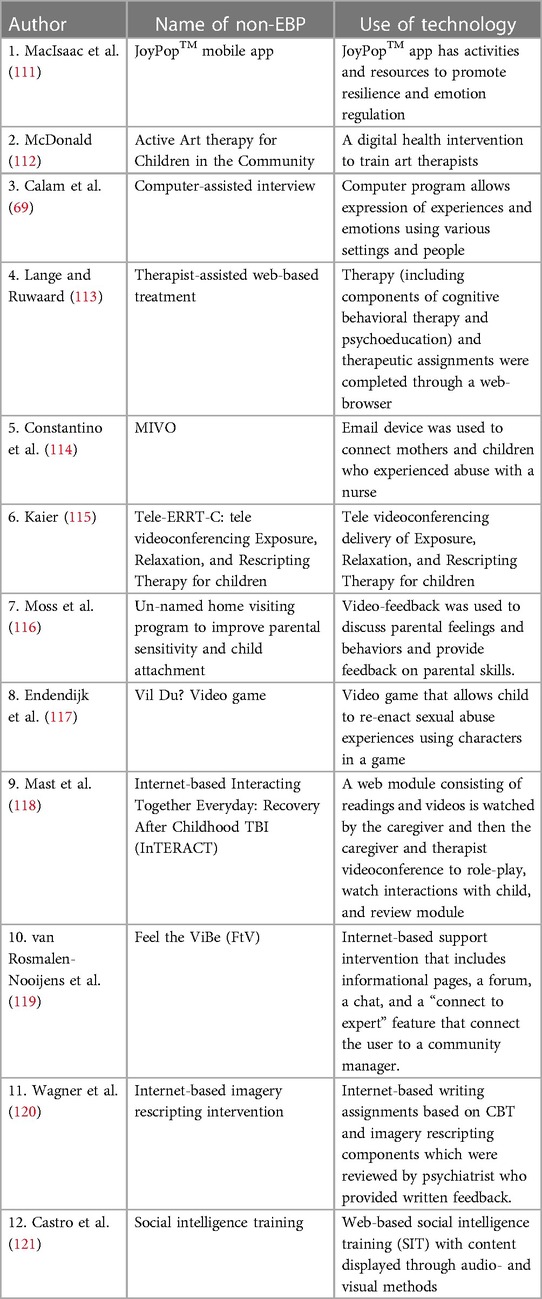
While our review captured the application of technology in evidence-based programs for child maltreatment, it is important to note additional existing literature in this area was not captured by through our search string or database selection. For example, artificial intelligence is a growing area of interest in data modeling of violence prevention to identify algorithms for perpetration and prevention (95). The current review did not include search parameters for this novel interface. However, with additional exploration, this technology will be important to assess within evidence-based programs in the future. Further, many established programs, with high relevance for preventing maltreatment and published technology research, were not captured because the technology-based modifications were applied to other target populations not captured in our search. For example, the Parent-Child Interaction Therapy (PCIT), an evidence-based program targeting child behavioral or externalizing mental health symptomology has been modified for remote delivery in its Internet delivered PCIT format, which uses comparable videoconferencing technology among families (96, 97). Though PCIT has also been shown to positive impact families at risk for child maltreatment (98) these studies focused on families with children experiencing significant behavioral issues (96). Several other non-evidence, based but emerging programs also describe digital advancements to promote outcomes, or are original digital interventions providing treatment (see Tables 7, 8). As one example, studies on smartphone app interventions, such as the JoyPop application which is based on trauma-informed principles, have demonstrated improvements in resilience and mental health symptomology and among young adult populations with a history of adverse childhood experiences. Preliminary evidence also supports the incorporation of JoyPop among both evidence-based parent (99, 100) and child programs (101). Such advancements represent new directions in technology providing rapid access to behavioral care.
In consideration of the increased use of technology-based applications in evidence-based practice, we must also assess whether the cost of these advents counterbalances the magnitude of benefits, and sustainability of programs, or contributes to the limitations observed in practice. Only through reliable evaluation of these programmatic advancements can we weigh the cost-effectiveness in comparison to program efficacy. However, researchers and practitioners encounter limitations through federal funding requirements and current grant infrastructure, which prohibit rapid dissemination of quality science in emergent situations such as the pandemic. Concurrently, published findings then become irrelevant as reported upon technology become obsolete in the face of newer technological innovations entering the field.
Conclusions
This scoping review is the first to provide a comprehensive examination of uses and effects programs through technology enhancements, as applicable, across evidence-based CM programs for both parent and child populations. The incorporation of technology presents exciting possibilities for program success for many models and the pandemic represents an era of novel directions for the field. However, the notably few available studies are an indication of the need for extensive exploration of the role of technology in practice. Only with such research can we definitively comment on its true utility. Further, the benefit of these programs is based on their effectiveness in achieving positive outcomes for parents, youth, and children. A prominent challenge of the field will be to identify effective means of implementing programs with technology in a sustainable manner. We have growing opportunities to explore innovative technologies in practice to meet the needs of families and must continue to explore methods to promote behavioral change through empirically validated research testing the rigor of technology-based strategies in practice.
Author contributions
AT, SS-B, and VE contributed to the conception of the study. AT, VE, MR, JG, RM, SD, KO, and EP contributed to the search process; AT, MR, and JG contributed to the screening and final inclusion process; AT wrote the first draft of the manuscript; SS-B, contributed to sections of the manuscript; AT, MR, and JG contributed to tabular creation. AT, MR, SS-B, RS, and CW contributed to the final review and edited the final draft of the submitted version. All authors contributed to the article and approved the submitted version.
Funding
This project was funded by the Substance Abuse and Mental Health Services Administration (SAMHSA) as part of a National Child Traumatic Stress Initiative- Cat III grant awarded to Project Director A.T. (6H79SM084946-01M001). The views and opinions contained in the publication do not necessarily reflect those of SAMHSA or the U.S. Department of Health and Human Services and should not be construed as such. RS's contribution to this manuscript was partially supported by the Health Resources and Services Administration (HRSA) of the U.S. Department of Health and Human Services (HHS) as part of the National Telehealth Center of Excellence Award (U66 RH31458). The contents are those of the author(s) and do not necessarily represent the official views of, nor an endorsement, by HRSA, HHS, or the U.S. Government.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. U.S. Department of Health & Human Services. Child Maltreatment 2021. Administration for Children and Families, Children’s Bureau (2023). Available at: https://www.acf.hhs.gov/cb/data-research/child-maltreatment
2. Lee H, Kim E. Global prevalence of physical and psychological child abuse during COVID-19: a systematic review and meta-analysis. Child Abuse Negl. (2023) 135:105984. doi: 10.1016/j.chiabu.2022.105984
3. Anda RF, Felitti VJ, Bremner JD, Walker JD, Whitfield C, Perry BD, et al. The enduring effects of abuse and related adverse experiences in childhood. Eur Arch Psychiatry Clin Neurosci. (2006) 256(3):174–86. doi: 10.1007/s00406-005-0624-4
4. Carr A, Duff H, Craddock F. A systematic review of reviews of the outcome of noninstitutional child maltreatment. Trauma Violence Abuse. (2018) 21(4):828–43. doi: 10.1177/1524838018801334
5. Cicchetti D, Rogosch FA, Gunnar MR, Toth SL. The differential impacts of early physical and sexual abuse and internalizing problems on daytime cortisol rhythm in school-aged children. Child Dev. (2010) 81(1):252–69. doi: 10.1111/j.1467-8624.2009.01393.x
6. Crouch JL, Davila AL, Holzman JB, Hiraoka R, Rutledge E, Bridgett DJ, et al. Perceived executive functioning in parents at risk for child physical abuse. J Interpers Violence. (2019) 36(17–18): 0886260519851185. doi: 10.1177/0886260519851185
7. Hiraoka R, Crouch JL, Reo G, Wagner MF, Milner JS, Skowronski JJ. Borderline personality features and emotion regulation deficits are associated with child physical abuse potential. Child Abuse Negl. (2016) 52:177–84. doi: 10.1016/j.chiabu.2015.10.023
8. Sidebotham P, Golding J. Child maltreatment in the “children of the nineties”: a longitudinal study of parental risk factors. Child Abuse Negl. (2001) 25(9):1177–200. doi: 10.1016/S0145-2134(01)00261-7
9. Stith SM, Liu T, Davies LC, Boykin EL, Alder MC, Harris JM, et al. Risk factors in child maltreatment: a meta-analytic review of the literature. Aggress Violent Behav. (2009) 14(1):13–29. doi: 10.1016/j.avb.2006.03.006
10. Whitaker DJ, Le B, Karl Hanson R, Baker CK, McMahon PM, Ryan G, et al. Risk factors for the perpetration of child sexual abuse: a review and meta-analysis. Child Abuse Negl. (2008) 32(5):529–48. doi: 10.1016/j.chiabu.2007.08.005
11. Substance Abuse and Mental Health Services Administration. Double jeopardy: COVID-19 and behavioral health disparities for black and latino communities in the US. Substance Abuse and Mental Health Services Administration. (2020). Available at: https://www.samhsa.gov/sites/default/files/covid19-behavioral-health-disparities-black-latino-communities.pdf
12. Griffith AK. Parental burnout and child maltreatment during the COVID-19 pandemic. J Fam Violence. (2022) 37(5):725–31. doi: 10.1007/s10896-020-00172-2
13. Connell CM, Strambler MJ. Experiences with COVID-19 stressors and Parents’ use of neglectful, harsh, and positive parenting practices in the northeastern United States. Child Maltreat. (2021) 26(3):255–66. doi: 10.1177/10775595211006465
14. Humphreys KL, Myint MT, Zeanah CH. Increased risk for family violence during the COVID-19 pandemic. Pediatrics. (2020) 146(1):e20200982. doi: 10.1542/peds.2020-0982
15. Lawson M, Piel MH, Simon M. Child maltreatment during the COVID-19 pandemic: consequences of parental job loss on psychological and physical abuse towards children. Child Abuse Negl. (2020) 110:104709. doi: 10.1016/j.chiabu.2020.104709
16. Wu Q, Xu Y. Parenting stress and risk of child maltreatment during the COVID-19 pandemic: a family stress theory-informed perspective. Dev Child Welf. (2020) 2(3):180–96. doi: 10.1177/2516103220967937
17. Shaffer A, Kotchick BA, Dorsey S, Forehand R. The past, present, and future of behavioral parent training: interventions for child and adolescent problem behavior. Behav Anal Today. (2001) 2(2):91. doi: 10.1037/h0099922
18. Wyatt Kaminski J, Valle LA, Filene JH, Boyle CL. A meta-analytic review of components associated with parent training program effectiveness. J Abnorm Child Psychol. (2008) 36(4):567–89. doi: 10.1007/s10802-007-9201-9
19. Hefti S, Pérez T, Fürstenau U, Rhiner B, Swenson CC, Schmid M. Multisystemic therapy for child abuse and neglect: do parents show improvement in parental mental health problems and parental stress?. J Marital Fam Ther. (2020) 46(1):95–109. doi: 10.1111/jmft.12367
20. Tiwari A, Self-Brown S, Lai BS, McCarty C, Carruth L. Effects of an evidence-based parenting program on biobehavioral stress among at-risk mothers for child maltreatment: a pilot study. Soc Work Health Care. (2018) 57(3):137–63. doi: 10.1080/00981389.2017.1371096
21. Toth SL, Sturge-Apple ML, Rogosch FA, Cicchetti D. Mechanisms of change: testing how preventative interventions impact psychological and physiological stress functioning in mothers in neglectful families. Dev Psychopathol. (2015) 27(4pt2):1661–74. doi: 10.1017/S0954579415001017
22. Branco MSS, Altafim ERP, Linhares MBM. Universal intervention to strengthen parenting and prevent child maltreatment: updated systematic review. Trauma Violence Abuse. (2021) 23(5):1658–76. doi: 10.1177/15248380211013131
23. Casillas KL, Fauchier A, Derkash BT, Garrido EF. Implementation of evidence-based home visiting programs aimed at reducing child maltreatment: a meta-analytic review. Child Abuse Negl. (2016) 53:64–80. doi: 10.1016/j.chiabu.2015.10.009
24. Chaffin M, Bard D, Bigfoot DS, Maher EJ. Is a structured, manualized, evidence-based treatment protocol culturally competent and equivalently effective among American Indian parents in child welfare? Child Maltreat. (2012) 17(3):242–52. doi: 10.1177/1077559512457239
25. Gallitto E, Romano E, Whitaker D. Investigating the impact of the SafeCare program on parenting behaviours in child welfare-involved families. Child Adolesc Soc Work J. (2021) 38(1):115–26. doi: 10.1007/s10560-020-00672-6
26. Lefever JEB, Bigelow KM, Carta JJ, Borkowski JG, Grandfield E, McCune L, et al. Long-term impact of a cell phone–enhanced parenting intervention. Child Maltreat. (2017) 22(4):305–14. doi: 10.1177/1077559517723125
27. Warren JM, Halpin SA, Hanstock TL, Hood C, Hunt SA. Outcomes of parent-child interaction therapy (PCIT) for families presenting with child maltreatment: a systematic review. Child Abuse Negl. (2022) 134:105942. doi: 10.1016/j.chiabu.2022.105942
28. Whitaker DJ, Self-Brown S, Hayat MJ, Osborne MC, Weeks EA, Reidy DE, et al. Effect of the SafeCare© intervention on parenting outcomes among parents in child welfare systems: a cluster randomized trial. Prev Med. (2020) 138:106167. doi: 10.1016/j.ypmed.2020.106167
29. Black PJ, Woodworth M, Tremblay M, Carpenter T. A review of trauma-informed treatment for adolescents. Can Psychol. (2012) 53:192–203. doi: 10.1037/a0028441
30. Leenarts L, Diehle J, Doreleijers T, Jansma E, Lindauer R. Evidence-based treatments for children with trauma-related psychopathology as a result of childhood maltreatment: a systematic review. Eur Child Adolesc Psychiatry. (2013) 22(5):269–83. doi: 10.1007/s00787-012-0367-5
31. Cohen JA, Mannarino AP, Deblinger E. Trauma-focused CBT for children and adolescents: Treatment applications. New York: Guilford Press (2012).
32. Hoogsteder LM, ten Thije L, Schippers EE, Stams GJJM. A meta-analysis of the effectiveness of EMDR and TF-CBT in reducing trauma symptoms and externalizing behavior problems in adolescents. Int J Offender Ther Comp Criminol. (2021) 66(6–7):735–57. doi: 10.1177/0306624X211010290
33. McTavish JR, Santesso N, Amin A, Reijnders M, Ali MU, Fitzpatrick-Lewis D, et al. Psychosocial interventions for responding to child sexual abuse: a systematic review. Child Abuse Negl. (2021) 116:104203. doi: 10.1016/j.chiabu.2019.104203
34. Thielemann JFB, Kasparik B, König J, Unterhitzenberger J, Rosner R. A systematic review and meta-analysis of trauma-focused cognitive behavioral therapy for children and adolescents. Child Abuse Negl. (2022) 134:105899. doi: 10.1016/j.chiabu.2022.105899
35. Bradbury-Jones C, Isham L. The pandemic paradox: the consequences of COVID-19 on domestic violence. J Clin Nurs. (2020) 29(13–14):2047–9. doi: 10.1111/jocn.15296
36. National SafeCare Training and Research Center. Utilizing Technology: How to Engage and Serve Families during the COVID-19 Pandemic (2020). Available at: https://safecare.publichealth.gsu.edu/files/2020/04/Engaging-Families-in-Virtual-SafeCare-Sessions-4.14.20.pdf (Retrieved May 18, 2020).
37. Stewart RW, Wallace M. Guide for transitioning to telehealth delivery of mental health: addressing barriers during the COVID-19 outbreak (2020). Available at: http://www.episcenter.psu.edu/sites/default/files/Telehealth%20Guide%20MUSC%20English%20%281%29.pdf
38. Self-Brown S, Whitaker DJ. Introduction to the special issue on using technology to address child maltreatment: prevention, intervention, and research. Child Maltreat. (2008) 13(4):319. doi: 10.1177/1077559508323764
39. Stewart RW, Orengo-Aguayo RE, Cohen JA, Mannarino AP, de Arellano MA. A pilot study of trauma-focused cognitive–behavioral therapy delivered via telehealth technology. Child Maltreat. (2017) 22(4):324–33. doi: 10.1177/1077559517725403
40. O'Neill K, Korfmacher J, Zagaja C, Duggan A. COVID-19’s early impact on home visiting. First report from a national HARC-beat survey of local home visiting programs. Home Visiting Appl Res Collaborative. (2020). Available at: https://library.first5center.org/wp-content/uploads/2020/06/COVID-19s-Early-Impact-on-Home-Visiting.pdf
41. Self-Brown S, Reuben K, Perry EW, Bullinger LR, Osborne MC, Bielecki J, et al. The impact of COVID-19 on the delivery of an evidence-based child maltreatment prevention program: understanding the perspectives of SafeCare® providers. J Fam Violence. (2022) 37(5):825–35. doi: 10.1007/s10896-020-00217-6
42. Self-Brown SC, Osborne M, Rostad W, Feil E. A technology-mediated approach to the implementation of an evidence-based child maltreatment prevention program. Child Maltreat. (2017) 22(4):344–53. doi: 10.1177/1077559516678482
43. Traube D, Gozalians S, Duan L. Transitions to virtual early childhood home visitation during COVID-19. Infant Ment Health J. (2022) 43(1):69–81. doi: 10.1002/imhj.21957
44. Watson AB, R L, Fong K, Self-Brown S. Virtual delivery in home visiting: insights from administrative, survey, and focus group data. American Public health association 2022 annual meeting and expo; Boston, MA (2022).
45. Daudt HML, van Mossel C, Scott SJ. Enhancing the scoping study methodology: a large, inter-professional team’s experience with arksey and O’Malley’s framework. BMC Med Res Methodol. (2013) 13(1):48. doi: 10.1186/1471-2288-13-48
46. Arksey H, O'Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. (2005) 8(1):19–32. doi: 10.1080/1364557032000119616
47. Pew Research Center. Mobile Fact Sheet (2021). Available at: https://www.pewresearch.org/internet/fact-sheet/mobile/ (Retrieved May 1, 2023).
48. U.S. Bureau of Labor Statistics. Focus of Prices and Spending. Consumer Expenditures: 2008 (2010). Available at: https://www.bls.gov/opub/btn/archive/more-than-75-percent-of-american-households-own-computers.pdf
49. Hupe M. Endnote X9. J Electron Resour Medical Libr. (2019) 16(3–4):117–9. doi: 10.1080/15424065.2019.1691963
50. Silva J. Parents raising safe kids: ACT 8-week program for parents. Washington, DC: American Psychological Association (2007).
51. Lotto CR, Altafim ERP, Linhares MBM. Feasibility and acceptability study of the online ACT-raising safe kids program. Child Youth Serv Rev. (2022) 141. doi: 10.1016/j.childyouth.2022.106591
52. Feil EG, Baggett KM, Davis B, Sheeber L, Landry S, Carta JJ, et al. Expanding the reach of preventive interventions: development of an internet-based training for parents of infants. Child Maltreat. (2008) 13(4):334–46. doi: 10.1177/1077559508322446
53. Baggett K, Davis B, Feil E, Sheeber L, Landry S, Leve C, et al. A randomized controlled trial examination of a remote parenting intervention: engagement and effects on parenting behavior and child abuse potential. Child Maltreat. (2017) 22(4):315–23. doi: 10.1177/1077559517712000
54. Feil EG, Baggett K, Davis B, Landry S, Sheeber L, Leve C, et al. Randomized control trial of an internet-based parenting intervention for mothers of infants. Early Child Res Q. (2020) 50:36–44. doi: 10.1016/j.ecresq.2018.11.003
55. Webster-Stratton C, Reid JM. The incredible years. Evidence-based parenting and child programs for families involved in the child welfare system. In: Rubin A, editor. Programs and interventions for maltreated children and families at risk. Hoboken, NJ: John Wiley & Sons, Inc. (2012). p. 11–30.
56. Camero KA, Castro J, Sepulveda A, Javier JR. Parenting during a pandemic: providing online parenting supportto mothers of infants. Pediatrics. (2022) 149:61.
57. Daro DA, Harding KA. Healthy families America: using research to enhance practice. Future Child. (1999) 9(1):152–76. doi: 10.2307/1602726
58. Ondersma SJ, Martin J, Fortson B, Whitaker DJ, Self-Brown S, Beatty J, et al. Technology to augment early home visitation for child maltreatment prevention: a pragmatic randomized trial. Child Maltreat. (2017) 22(4):334–43. doi: 10.1177/1077559517729890
59. Wagner MM, Clayton SL. The parents as teachers program: results from two demonstrations. Future Child. (1999) 9(1):91. doi: 10.2307/1602723
60. Traube D, Hsiao H-Y, Rau A, Hunt-O’Brien D, Lu L, Islam N. Advancing home based parenting programs through the use of telehealth technology. J Child Fam Stud. (2020) 29(1):44–53. doi: 10.1007/s10826-019-01458-w
61. Gershater-Molko RM, Lutzker JR, Wesch D. Project SafeCare: improving health, safety, and parenting skills in families reported for, and at-risk for child maltreatment. J Fam Violence. (2003) 18(6):377–86. doi: 10.1023/A:1026219920902
62. Bigelow KM, Carta JJ, Lefever JB. Txt u ltr: using cellular phone technology to enhance a parenting intervention for families at risk for neglect. Child Maltreat. (2008) 13(4):362–7. doi: 10.1177/1077559508320060
63. Gaskin E, Lutzker J, Crimmins D, Robinson L. Using a digital frame and pictorial information to enhance the SafeCare® parent-infant interactions module with a mother with intellectual disabilities: results of a pilot study. J Ment Health Res Intellect Disabil. (2012) 5(2):187–202. doi: 10.1080/19315864.2012.674871
64. Guastaferro KM, Lutzker JR, Graham ML. Using a technological augmentation to enhance parent-infant interactions with parents at risk. Child Fam Behav Ther. (2016) 38(1):15–31. doi: 10.1080/07317107.2016.1135698
65. Jabaley JJ, Lutzker JR, Whitaker DJ, Self-Brown S. Using iPhones™ to enhance and reduce face-to-face home safety sessions within SafeCare®: an evidence-based child maltreatment prevention program. J Fam Violence. (2011) 26(5):377–85. doi: 10.1007/s10896-011-9372-6
66. Dozier M, Bernard K, Roben CKP. Attachment and biobehavioral catch-up. In: Steele H, Steele M, editors. Handbook of attachment-based interventions. New York: Guilford Press (2017). p. 27–50.
67. Schein SS, Roben CKP, Costello AH, Dozier M. Assessing changes in parent sensitivity in telehealth and hybrid implementation of attachment and biobehavioral catch-up during the COVID-19 pandemic. Child Maltreat. (2022) 28(1):24–33. doi: 10.1177/10775595211072516
68. Sanders MR. Triple P-positive parenting program: towards an empirically validated multilevel parenting and family support strategy for the prevention of behavior and emotional problems in children. Clin Child Fam Psychol Rev. (1999) 2(2):71–90. doi: 10.1023/A:1021843613840
69. Calam R, Cox A, Glasgow D, Jimmieson P, Larsen SG. Assessment and therapy with children: can computers help?. Clin Child Psychol Psychiatry. (2000) 5(3):329–43. Available at: https://www.embase.com/search/results?subaction=viewrecord&id=L30644798&from=export doi: 10.1177/1359104500005003004
70. Sanders M, Calam R, Durand M, Liversidge T, Carmont SA. Does self-directed and web-based support for parents enhance the effects of viewing a reality television series based on the triple P—positive parenting programme? J Child Psychol Psychiatry. (2008) 49(9):924–32. doi: 10.1111/j.1469-7610.2008.01901.x
71. Sanders MR, Montgomery DT, Brechman-Toussaint ML. The mass Media and the prevention of child behavior problems: the evaluation of a television series to promote positive outcomes for parents and their children. J Child Psychol Psychiatry Allied Discip. (2000) 41(7):939–48. doi: 10.1111/1469-7610.00681
72. Sanders MR, Baker S, Turner KMT. A randomized controlled trial evaluating the efficacy of triple P online with parents of children with early-onset conduct problems. Behav Res Ther. (2012) 50(11):675–84. doi: 10.1016/j.brat.2012.07.004
73. Sanders M, Dittman C, Farruggia S, Keown L. A comparison of online versus workbook delivery of a self-help positive parenting program. J Prim Prev. (2014) 35(3):125–33. doi: 10.1007/s10935-014-0339-2
74. Stewart RW, Orengo-Aguayo RE, Gilmore AK, de Arellano M. Addressing barriers to care among hispanic youth: telehealth delivery of trauma-focused cognitive behavioral therapy. Behav Ther. (2017) 40(3):112–8.
75. Stewart RW, Orengo-Aguayo R, Wallace M, Metzger IW, Rheingold AA. Leveraging technology and cultural adaptations to increase access and engagement among trauma-exposed African American youth: exploratory study of school-based telehealth delivery of trauma-focused cognitive behavioral therapy. J Interpers Violence. (2021) 36(15/16):7090–109. doi: 10.1177/0886260519831380
76. Zinny A. 30.3 Peer-Assisted trauma-focused CBT for black and hispanic teens with traumatic stress reactions to COVID-19–related deaths. J Am Acad Child Adolesc Psychiatry. (2022) 61(10):S41–2. doi: 10.1016/j.jaac.2022.07.176
77. Orengo-Aguayo R, Dueweke AR, Nicasio A, de Arellano MA, Rivera S, Cohen JA, et al. Trauma-focused cognitive behavioral therapy with puerto rican youth in a post-disaster context: tailoring, implementation, and program evaluation outcomes. Child Abuse Negl. (2022) 129:1–9. doi: 10.1016/j.chiabu.2022.105671
78. Calam R, Sanders MR, Miller C, Sadhnani V, Carmont S-A. Can technology and the media help reduce dysfunctional parenting and increase engagement with preventative parenting interventions? Child Maltreat. (2008) 13(4):347–61. doi: 10.1177/1077559508321272
79. Love SM, Sanders MR, Turner KMT, Maurange M, Knott T, Prinz R, et al. Social media and gamification: engaging vulnerable parents in an online evidence-based parenting program. Child Abuse Negl. (2016) 53:95–107. doi: 10.1016/j.chiabu.2015.10.031
80. Stewart RW, Orengo-Aguayo R, Young J, Wallace MM, Cohen JA, Mannarino AP, et al. Feasibility and effectiveness of a telehealth service delivery model for treating childhood posttraumatic stress: A community-based, open pilot trial of trauma-focused cognitive–behavioral therapy . US: Educational Publishing Foundation (2020). doi: 10.1037/int0000225
81. Caouette J, Hébert M, Cyr C, Amédée LM. The attachment video-feedback intervention (AVI) combined to the trauma-focused cognitive behavioral therapy (TF-CBT) for sexually abused preschoolers and their parents: a pilot study examining pre- to post-test changes. Dev Child Welf. (2021) 3(2):119–34. doi: 10.1177/25161032211013820
82. Davidson TM, Bunnell BE, Saunders BE, Hanson RF, Danielson CK, Cook D, et al. Pilot evaluation of a tablet-based application to improve quality of care in child mental health treatment. Behav Ther. (2019) 50(2):367–79. doi: 10.1016/j.beth.2018.07.005
83. Beet N, Ademosu T. Keeping connected: family therapists’ experiences of working online during the COVID-19 pandemic. J Fam Ther. (2023) 45(2):223–41. doi: 10.1111/1467-6427.12421
84. Amorin-Woods D, Fraenkel P, Mosconi A, Nisse M, Munoz S. Family therapy and COVID-19: international reflections during the pandemic from systemic therapists across the globe. Aust N Z J Fam Ther. (2020) 41(2):114–32. doi: 10.1002/anzf.1416
85. Simons A, Noordegraaf M, Van Regenmortel T. ‘When it comes to relational trauma, you need people at the table': therapist experiences of online therapy for families with a prior disclosure of sibling sexual abuse during COVID-19 pandemic lockdowns. J Fam Ther. (2022) 44(4):490–503. doi: 10.1111/1467-6427.12397
86. Tener D, Marmor A, Katz C, Newman A, Silovsky JF, Shields J, et al. How does COVID-19 impact intrafamilial child sexual abuse? Comparison analysis of reports by practitioners in Israel and the US. Child Abuse Negl. (2021) 116:104779. doi: 10.1016/j.chiabu.2020.104779
87. Azzopardi C, Shih CS-Y, Burke AM, Kirkland-Burke M, Moddejonge JM, Smith TD, et al. Supporting survivors of child sexual abuse during the COVID-19 pandemic: an ecosystems approach to mobilizing trauma-informed telemental healthcare. Can Psychol. (2022) 63(1):43–55. doi: 10.1037/cap0000298
88. Durlak JA, DuPre EP. Implementation matters: a review of research on the influence of implementation on program outcomes and the factors affecting implementation. Am J Community Psychol. (2008) 41(3):327–50. doi: 10.1007/s10464-008-9165-0
89. Schoenwald SK, Garland AF, Chapman JE, Frazier SL, Sheidow AJ, Southam-Gerow MA. Toward the effective and efficient measurement of implementation fidelity. Adm Policy Ment Health Ment Health Serv Res. (2011) 38(1):32–43. doi: 10.1007/s10488-010-0321-0
90. Thijssen J, Albrecht G, Muris P, de Ruiter C. Treatment fidelity during therapist initial training is related to subsequent effectiveness of parent management training—oregon model. J Child Fam Stud. (2017) 26(7):1991–9. doi: 10.1007/s10826-017-0706-8
91. Caron EB, Kipp EC, Costello AH, Bernard K, Schein SS, Roben CKP, et al. Parent coaching fidelity trajectories of in-person and telehealth sessions during the COVID-19 pandemic. Evid Based Pract Child Adolesc Ment Health. (2022) 7(3):341–8. doi: 10.1080/23794925.2021.1996300
92. Roben CKP, Kipp E, Schein SS, Costello AH, Dozier M. Transitioning to telehealth due to COVID-19: maintaining model fidelity in a home visiting program for parents of vulnerable infants. Infant Ment Health J. (2022) 43(1):173–84. doi: 10.1002/imhj.21963
93. Lythreatis S, Singh SK, El-Kassar A-N. The digital divide: a review and future research agenda. Technol Forecast Soc Change. (2022) 175:121359. doi: 10.1016/j.techfore.2021.121359
94. Mowbray CT, Holter MC, Teague GB, Bybee D. Fidelity criteria: development, measurement, and validation. Am J Eval. (2003) 24(3):315–40. doi: 10.1177/109821400302400303
95. Hunt X, Tomlinson M, Sikander S, Skeen S, Marlow M, du Toit S, et al. Artificial intelligence, big data, and mHealth: the frontiers of the prevention of violence against children. Front Artif Intell. (2020) 3:1-16. doi: 10.3389/frai.2020.543305
96. Comer JS, Furr JM, Miguel EM, Cooper-Vince CE, Carpenter AL, Elkins RM, et al. Remotely delivering real-time parent training to the home: an initial randomized trial of internet-delivered parent–child interaction therapy (I-PCIT). J Consult Clin Psychol. (2017) 85(9):909. doi: 10.1037/ccp0000230
97. Funderburk BW, Ware LM, Altshuler E, Chaffin M. Use and feasibility of telemedicine technology in the dissemination of parent-child interaction therapy. Child Maltreat. (2008) 13(4):377–82. doi: 10.1177/1077559508321483
98. Chaffin M, Silovsky JF, Funderburk B, Valle LA, Brestan EV, Balachova T, et al. Parent-Child interaction therapy with physically abusive parents: efficacy for reducing future abuse reports. J Consult Clin Psychol. (2004) 72:500–10. doi: 10.1037/0022-006X.72.3.500
99. O'Hara K. Provider attitudes toward Mobile health app technology to augment child maltreatment prevention service delivery: An exploration of the integration of JoyPop™ with SafeCare®. Master's thesis. Atlanta: Georgia State University (2022).
100. O'Hara K, Recinos M, Tiwari A, Self-Brown S. Provider attitudes toward Mobile health application technology to augment child maltreatment prevention service delivery: An exploration of the integration of JoyPop™ with SafeCare®. Seattle, Washington: Society for Prevention Research (2022).
101. Recinos M, O'Hara K, Self-Brown S, Tiwari A. Augmenting evidence- based trauma therapy with mobile app technology: Trauma-focused cognitive behavioral therapists (TF-CBT) attitudes towards mobile app technology and reactions to the JoyPopTM app. New Orleans, Lousiana: American Professional Society on the Abuse of Children Colloquium (2022).
102. Fogarty A, Jones A, Seymour M, Savopoulos P, Evans K, O'Brien J, et al. The parenting skill development and education service: telehealth support for families at risk of child maltreatment during the COVID-19 pandemic. Child Fam Soc Work. (2022) 27(3):392–404. doi: 10.1111/cfs.12890
103. Gülırmak K, Orak OS. Effectiveness of web-based distance education for parents in the prevention of emotional neglect and abuse: a randomized controlled study. Perspect Psychiatr Care. (2021) 57(2):573–82. doi: 10.1111/ppc.12580
104. Lamberton L, Devaney J, Bunting L. New challenges in family support: the use of digital technology in supporting parents. Child Abuse Rev. (2016) 25(5):359–72. doi: 10.1002/car.2451
105. McKenzie LB, Roberts KJ, McAdams RJ, Abdel-Rasoul M, Kristel O, Szymanski A, et al. Efficacy of a mobile technology-based intervention for increasing parents’ safety knowledge and actions: a randomized controlled trial. Inj Epidemiol. (2021) 8(1):1–13. doi: 10.1186/s40621-021-00350-w
106. Murray K, Woodruff K, Moon C, Finney C. Using text messaging to improve attendance and completion in a parent training program. J Child Fam Stud. (2015) 24(10):3107–16. doi: 10.1007/s10826-015-0115-9
107. Oliveira P, Stevens E, Barge L, Comyn J, Langley K, Ramchandani P, et al. A modified video-feedback intervention for carers of foster children aged 6 years and under with reactive attachment disorder: a feasibility study and pilot RCT. Health Technol Assess. (2022) 26(35):1–106. doi: 10.3310/sliz1119
108. Hodes MW, Meppelder HM, Schuengel C, Kef S. Tailoring a video-feedback intervention for sensitive discipline to parents with intellectual disabilities: a process evaluation. Attach Hum Dev. (2014) 16(4):387–401. doi: 10.1080/14616734.2014.912490 (The use of video in attachment-based interventions)24972106
109. Inouye J, Cerny JE, Hollandsworth J, Ettipio A. Child abuse prevention program with POTS-based telehealth: a feasibility project. Telemed J E Health. (2001) 7(4):325–32. doi: 10.1089/15305620152814728
110. van Leuven L, Lalouni M, Forster M. “Will it work as well on zoom?” A natural experiment during the COVID-19 pandemic of delivering parenting groups via video conferencing or in person. J Child Fam Stud. (2022) 32:1–14. doi: 10.1007/s10826-022-02398-8
111. MacIsaac A, Mushquash AR, Mohammed S, Grassia E, Smith S, Wekerle C. Adverse childhood experiences and building resilience with the JoyPop app: evaluation study. JMIR Mhealth Uhealth. (2021) 9(1):e25087. doi: 10.2196/25087
112. McDonald A. Art therapy for children following adverse childhood experiences: an intervention development study. Arts Psychother. (2022) 77:1–10. doi: 10.1016/j.aip.2022.101880
113. Lange A, Ruwaard J. Ethical dilemmas in online research and treatment of sexually abused adolescents. J Med Internet Res. (2010) 12(5):e58. Available at: https://www.embase.com/search/results?subaction=viewrecord&id=L360285660&from=export doi: 10.2196/jmir.1455
114. Constantino R, Crane PA, Noll BS, Doswell WM, Braxter B. Exploring the feasibility of email-mediated interaction in survivors of abuse. J Psychiatr Ment Health Nurs. (2007) 14(3):291–301. doi: 10.1111/j.1365-2850.2007.01080.x
115. Kaier EE. Reaching a rural community: Feasibility of delivering a child posttraumatic nightmare treatment via televideoconferencing. Thesis. Tulsa: The University of Tulsa (2017).
116. Moss E, Tarabulsy GM, St-Georges R, Dubois-Comtois K, Cyr C, Bernier A, et al. Video-feedback intervention with maltreating parents and their children: program implementation and case study. Attach Hum Dev. (2014) 16(4):329–42. doi: 10.1080/14616734.2014.912486 (The use of video in attachment-based interventions)24972102
117. Endendijk JJ, Tichelaar HK, Deen M, Deković M. Vil du?! incorporation of a serious game in therapy for sexually abused children and adolescents. Child Adolesc Psychiatry Ment Health. (2021) 15(1):25. doi: 10.1186/s13034-021-00377-3
118. Mast JE, Antonini TN, Raj SP, Oberjohn KS, Cassedy A, Makoroff KL, et al. Web-based parenting skills to reduce behavior problems following abusive head trauma: a pilot study. Child Abuse Negl. (2014) 38(9):1487–95. doi: 10.1016/j.chiabu.2014.04.012
119. van Rosmalen-Nooijens K, Lo Fo Wong S, Prins J, Lagro-Janssen T. Young people, adult worries: randomized controlled trial and feasibility study of the internet-based self-support method “feel the ViBe” for adolescents and young adults exposed to family violence. J Med Internet Res. (2017) 19(6):e204. doi: 10.2196/jmir.6004
120. Wagner B, Grafiadeli R, Martin T, Böhm M. Internet-based imagery rescripting intervention for adult survivors of institutional childhood abuse in the former German democratic republic—a pilot study. Eur J Psychotraumatol. (2022) 13(2):2117222. doi: 10.1080/20008066.2022.2117222
Keywords: child maltreatment, technology, scoping review, at-risk parents, trauma treatment, child abuse, child trauma
Citation: Tiwari A, Recinos M, Garner J, Self-Brown S, Momin R, Durbha S, Emery V, O’Hara K, Perry E, Stewart R and Wekerle C (2023) Use of technology in evidence-based programs for child maltreatment and its impact on parent and child outcomes. Front. Digit. Health 5:1224582. doi: 10.3389/fdgth.2023.1224582
Received: 17 May 2023; Accepted: 26 June 2023;
Published: 6 July 2023.
Edited by:
Helen Cowie, University of Surrey, United KingdomReviewed by:
Rüdiger Christoph Pryss, Julius Maximilian University of Würzburg, GermanyHolger Muehlan, University of Greifswald, Germany
© 2023 Tiwari, Recinos, Garner, Self-Brown, Momin, Durbha, Emery, O'Hara, Perry, Stewart and Wekerle. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ashwini Tiwari QXRpd2FyaUBhdWd1c3RhLmVkdQ==
†These authors have contributed equally to this work and share last authorship
 Ashwini Tiwari
Ashwini Tiwari Manderley Recinos
Manderley Recinos Jamani Garner2
Jamani Garner2 Shannon Self-Brown
Shannon Self-Brown Rushan Momin
Rushan Momin Christine Wekerle
Christine Wekerle