- 1Research Unit Inclusive Society, University College Leuven Limburg, Leuven, Belgium
- 2Research Units Sustainable Resources and Smart Organizations, University College Leuven Limburg, Diepenbeek, Belgium
- 3Brain and Cognition, KU Leuven, Leuven, Belgium
- 4School of Educational Studies, UHasselt, Hasselt, Belgium
Introduction: Computer-mediated care is becoming increasingly popular, but little research has been done on it and its effects on emotion-related outcomes. This systematic literature review aims to create an overview that addresses the research question: “Is there a relationship between computer-mediated care and emotional expression, perception, and emotional and (long-term) emotion outcomes?”
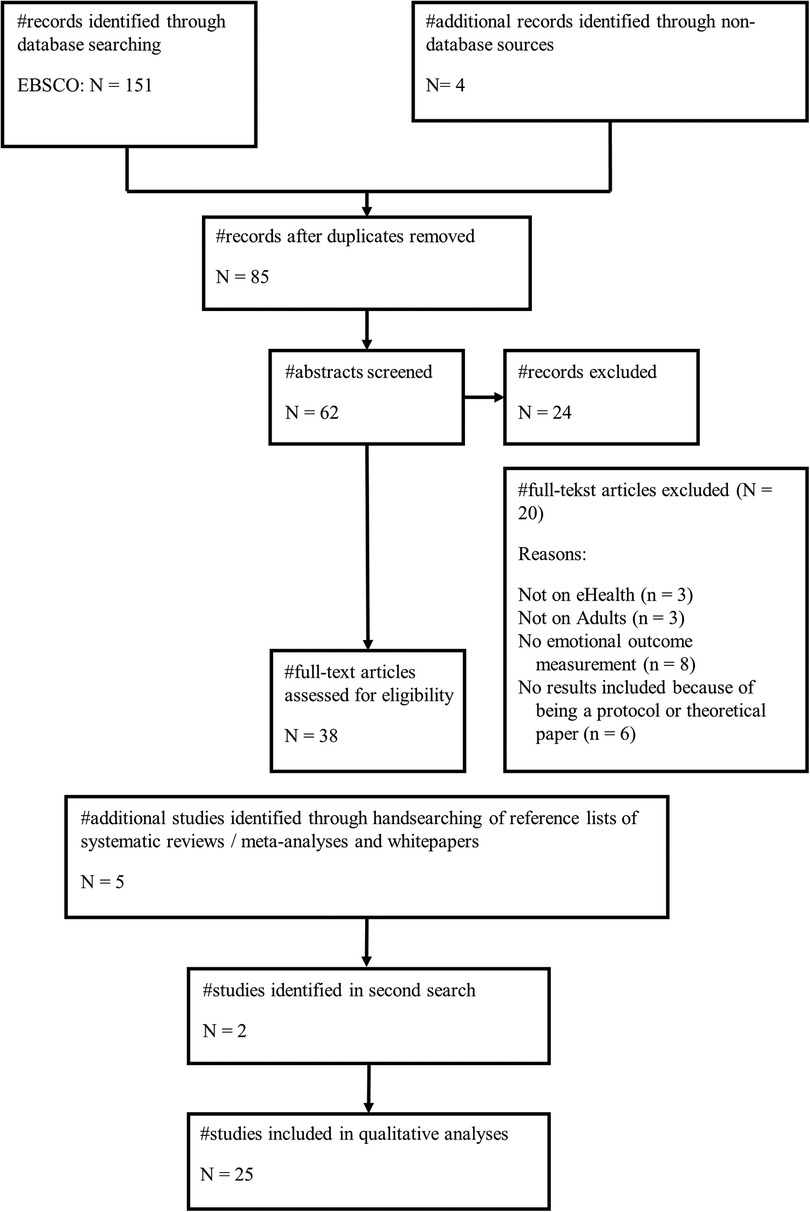
Method: This systematic literature review was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines and used five eligibility criteria, namely, (1) participants: adults seeking support; (2) intervention: eHealth; (3) diagnostic criteria: transdiagnostic concept of difficulty identifying, expressing, and/or regulating emotions (e.g., alexithymia); (4) comparator: either face-to-face care or no comparator; and (5) study design: quantitative studies or qualitative studies. Quality was assessed using the QualSyst tool.
Results: The analysis includes 25 research papers. Self-paced interventions appear to have a positive effect on emotion regulation. Videoconferencing interventions improved emotion regulation from before to after treatment but worsened emotion regulation compared with face-to-face treatment.
Discussion: The lack of variation in the modalities studied and the emotion measurements used make it difficult to draw responsible conclusions. Future research should examine how different modalities affect the real-time communication of emotions and how non-verbal cues influence this.
1. Introduction
The mediation of social and health services by computers and other digital devices is becoming increasingly popular (e.g., (1)). In 2017, over 10,000 mental health apps were available (2). Moreover, considering the COVID-19 pandemic, legislation has been rapidly changing to increase the availability of computer-mediated care (3, 4).
Available effectiveness research focuses mainly on care via videoconferencing and shows that it is feasible and effective for a wide range of psychopathologies (5–8). Two studies found a better treatment response or faster decrease in symptoms when treatment for children and their parents was delivered via the Internet compared with face-to-face (9, 10). The treatment response and the bond between a therapist and their client appear to be unchanged when video conferencing is compared with face-to-face interactions (11). Despite these findings, clinicians report a decrease in the ability to express empathy online (12). Both empathy skills and the number of empathic interactions appear lower in online sessions compared with face-to-face interactions (13, 14).
In their seminal work, Grondin et al. (15) developed a theoretical framework to elucidate the concept of computer-mediated empathy. This article follows the work of Grondin and colleagues and will discuss the phenomenon of computer-mediated empathy, which involves individuals seeking and/or providing support online. It will examine the dynamics between a counselor and their client, as well as the roles of the “target” and “observer” in this context. The concept of computer-mediated empathy encompasses a sequential interaction process comprising four distinct stages, namely, the transmission of social–emotional signals, the experience of empathy, the transfer of empathy, and the perception of empathy. The initiation of an empathic interaction involves the target expressing their emotional state to the observer. The extent to which non-verbal signals are filtered depends on the specific modality employed, such as videoconferencing or text-based communication. Therefore, it is necessary to modify the message to communicate emotions effectively. According to Barak et al. (16), the individual being studied has the option to explicitly express their emotional state by stating phrases such as “I'm crying” or “I feel sad.” In addition, textual paralanguage cues, such as symbols, images, or emoticons, can be employed to convey emotions (17–19). Furthermore, emotions can also be expressed using character repetitions or punctuation, as exemplified by phrases such as “This is taking soooooo loooooong,” [blank message], and “He never talks about IT” (18, 19).
Subsequently, the individual at the receiving end of the computer interface must adeptly discern the emotional state of the target and cultivate a sense of empathy. The subsequent phase entails the transmission of empathetic sentiments by the observer, as also outlined by Grondin et al. (15). The ability to convey empathy is influenced by both verbal and non-verbal cues, as suggested by previous research (20, 21). Therefore, filtering non-verbal cues affects one's ability to express empathy. Observers can directly inquire about the emotional state of the individual in question, specifically regarding feelings of sadness. However, they encounter limitations in effectively communicating subtle variations in facial expressions or body language. According to Grondin et al. (15), the target must interpret the response as empathetic. It is crucial to establish this differentiation when expressing empathy, as research has shown that the perceived level of empathy is a more accurate indicator of therapeutic outcomes compared with the observer's assessment of the therapist’s own experience of empathy (22).
Figure 1 shows the complicated target–observer relationship in computer-mediated care. The target, who needs emotional assistance, sends social–emotional signals using a computer. Their SMS messages may express their ideas, feelings, and experiences. “I feel overwhelmed with work deadlines” or “I'm going through a difficult time and need someone to talk to” are sample statements of emotional support requests. The observer, who provides empathy and emotional support, deciphers these social–emotional indicators and responds with compassion. Virtual hugs, encouraging words, and supporting texts convey this response. The observer may say, “I'm here for you. You can get through this,” or “I understand how difficult that must be for you.” The target's emotions are affected by the observer's empathy. Computer-mediated empathy can boost the target's mood with the observer's pleasant words. Computer-mediated empathy helps moderate interpersonal emotions even after participation. Zaki and Williams (23) found that computer-mediated routes can provide emotional support to the target.
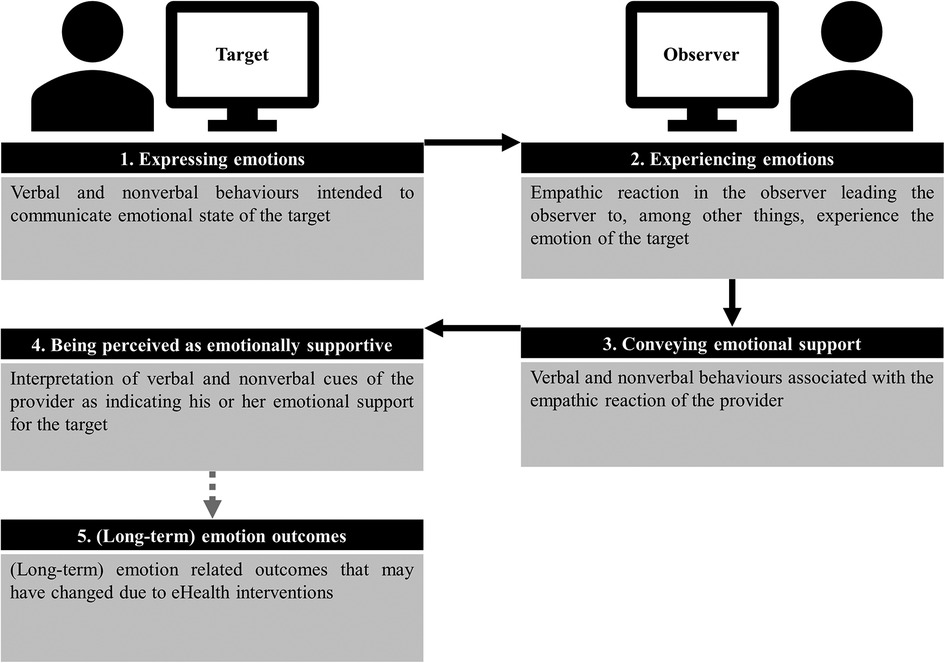
Figure 1. Framework for expressing and experiencing emotions and emotional support via computer-mediated interaction based on the framework of computer-mediated empathy by Grondin et al. (15).
Little is known about the ability to express and experience emotions and emotional support through computer-mediated care. An overview of the effects of computer-mediated communication on emotion-related outcomes is also lacking. Little is known about how other modalities influence emotion-related outcomes, given that most available research focuses on videoconferencing. Thus, this systematic literature review addresses the following research questions:
(1) Is there a link between computer-mediated care and (a) emotional expression, (b) emotional experience, and (c) emotional support during the interaction?
(2) Is there a link between computer-mediated care and emotion-related outcomes after the interaction?
2. Methods
The present study employed a systematic literature review approach, following a protocol developed a priori, adhering to the guidelines outlined in the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA). Five specific eligibility criteria were employed in the selection process. The assessment of quality was conducted utilizing the QualSyst tool.
2.1. Literature search
Papers were searched following a pre-developed protocol in EBSCO using keywords such as “eHealth” and “Emotio* identification” (for the complete search string, see Supplementary File S1, Table 1). All relevant databases (e.g., The Cochrane Library, Google Scholar, PubMed, PsychInfo, CINAHL, ERIC, ProQuest Dissertations, and EBSCO) were searched to include academic and gray literature. The reference lists of retrieved studies, (systematic) reviews, meta-analyses, and eHealth whitepapers and reports were searched as well. No ethnic or geographic limits were adopted. No client or ethical approval was required.
2.2. Screening and eligibility criteria
All studies have been screened for publication year (2000 to date) and adopted language (English or Dutch), and the records were deduplicated. The eligibility criteria include (1) participants: adults seeking support; (2) intervention: eHealth; (3) diagnostic criteria: transdiagnostic concept of difficulty identifying, expressing, and/or regulating emotions (e.g., alexithymia); (4) comparator: either face-to-face care or no comparator; and (5) study design: quantitative or qualitative studies. Quality was assessed using the QualSyst tool.
2.3. Data extraction
Data were extracted based on a pre-developed protocol. Study characteristics included the country in which the study was conducted, the intervention(s), the comparator(s), the target population, and the sample size. For each study, the instruments used for data collection, the method of delivery of the intervention, and the results of the measurements were reviewed to analyze the effect of the intervention.
2.4. Quality assessment
The two authors individually critically appraised the quality of the studies using the standard quality assessment criteria for evaluating primary research documents (QualSyst tool) (24). Supplementary File S4, Tables 4, 5 report two separate tables indicating the quality for the quantitative and qualitative studies.
3. Results
3.1. Literature search
A total of 151 studies were identified based on the search string, with 66 duplicates excluded. The two reviewers screened 85 titles and abstracts independently. The selection underwent thorough approval by the author team, wherein any disagreements were addressed through constructive discussions, accompanied by well-founded arguments, ultimately leading to a consensus. The inter-assessor reliability was 0.70. Figure 2 shows the full flowchart of this systematic literature review. A total of 25 papers were included in the analysis.
3.2. Study characteristics
Included studies are internationally dispersed, with most of the studies originating in the USA (e.g., (25–27)) (see Supplementary File S2, Table 2). Some studies were conducted internationally through an online community (e.g., (28–30)).
Study designs include six qualitative studies (e.g., (25, 31)), three surveys (e.g., (32–34)), and one case study (35), but the majority of the studies are RCTs (e.g., (36–38)).
The study populations vary but have a predominant medical focus, such as breast cancer patients (e.g., (25, 26, 39)), traumatic brain injury patients (e.g., (40)), patients with mental health problems (e.g., (28, 41)), and employees (e.g., (42–44)).
3.3. Quality of the included studies
All 19 quantitative studies were of good quality overall. Results in Supplementary File S4, Table 4 show that the range is from 0.64 (min) to 1.00 (max), with an average score of 0.85, and show seven studies of good quality (0.70–0.90) (e.g., (26, 36, 37)) and nine studies with excellent quality (>0.90) (e.g., (27, 28, 42)).
The scores for the qualitative studies were calculated similarly (24). The quality of the qualitative studies is low, showing a minimum of 0.35 (e.g., (45, 46)) and a maximum of 0.80 (e.g., (31)), with a score average of 0.55 (see Supplementary File S4, Table 5).
3.4. Modalities used
There was significant variability in the modalities used in the included studies. Five studies used a synchronous communication mode (e.g., (26, 35, 37)), meaning that the interaction took place in real time, while the majority of studies used an asynchronous communication mode (e.g., (25, 31, 36)).
In total, 12 interventions were text-based (e.g., (25, 31, 47)), 5 made use of videoconferencing (e.g., (26, 35, 37)), and 8 used a communication mix (e.g., (28, 36, 38)).
3.5. Is there a connection between eHealth and emotional expression, experience, support, and (long-term) emotion outcomes?
3.5.1. Expressing emotions
The studies on emotional expression mostly investigate text-based online support communities (e.g., (25, 31, 47)) (see Supplementary File S3, Table 3a). Qualitative analysis of messages posted in online support groups indicates that emotions are regularly expressed verbally in these communities (e.g., (25, 31, 47)). Online bereavement and cancer communities predominantly feature emotional communications (25, 45). While emotions are expressed online, it seems necessary to modulate the intensity of these emotions instead of presenting them in its raw form, for example, by using humor and storytelling (46) or sharing more positive than negative emotions (25, 27).
There seems to be a discrepancy between online and real-life emotional expressions. A questionnaire administered to participants in online breast cancer communities revealed that individuals expressed more emotions online than in face-to-face interactions (33). This finding is supported by a qualitative analysis of messages in an online support group for men with eating problems (47). This is in accordance with the online disinhibition effect, which claims that people are inclined to express themselves more openly online (48).
3.5.2. Experiencing the emotions of the user on the other side of the screen
No studies have investigated whether users experienced the emotions of another user during computer-mediated interactions. However, one study indicates that using positive emotions is associated with a lower chance of response (27). Another study suggests that too much unmodulated emotion reduces group interaction and individual involvement (46) (see Supplementary File S3, Table 3b). This reduced interaction may indirectly indicate a difficulty in experiencing the emotions of the target after reading positive emotions or too much unmodulated emotion.
3.5.3. Conveying emotional support
Two studies describe how emotional support can be provided, namely, by sharing certain feelings, supporting each other’s well-being, and showing sympathy, compassion, and understanding (31, 47). Moreover, empathy was the main emotion expressed in a bereavement community (45.6% (45)) (see Supplementary File S3, Table 3c).
3.5.4. Perceived emotional support
Self-report surveys on online cancer communities showed that perceived emotional support led to less perceived life stress (34) and that participants experienced less emotional support online than in face-to-face interactions (33) (see Supplementary File S3, Table 3d).
3.5.5. Emotion outcomes after the interaction
Results concerning emotion outcomes after the interaction are inconsistent and relate to different modalities of computer-mediated care and different emotion outcomes (see Supplementary File S3, Table 3e). One study found that the emotion perception of participants increased after web-based training when compared with a waitlist control group (49).
As mentioned earlier, men with eating disorders reported expressing fewer emotions face-to-face and instead sought anonymous support online (47). After spending more time in the online group, they reported becoming less secretive in real-life meetings, suggesting a possible effect of the online environment on emotional expression. In contrast, another study of a video conference group found no effect on emotional expression before and after participation (26).
Emotion regulation improved from pre- to post-treatment in individuals suffering from dissociative disorder (28) and women with a BMI over 25 (38) after a self-paced intervention. In addition, compared with a waitlist control, emotion regulation increased in stress-sensitive employees (42), women with postpartum depression (50), business students (49), and women with a BMI over 25 (38) following the same intervention. Moreover, a self-paced intervention for breast cancer patients decreased emotional suppression from pre- to post-treatment but had no effect on cognitive reappraisal (30). Employees with high-risk drinking experienced less emotional irritation compared with waitlist control after a web-based intervention (36). In contrast, employees with work-related stress showed less emotional exhaustion after a web-based intervention from pre- to post-treatment compared with waitlist control (44).
Contrary to these results, a self-paced web-based stress management intervention for employees showed no effects on emotion regulation (43), and a text-based cancer support group showed higher emotional suppression after the intervention (39).
Videoconferencing interventions resulted in a lower degree of reappraisal and higher emotional suppression compared with face-to-face treatment for persons with medically unexplained pain (37). However, for female veterans who have experienced military sexual trauma (41) and people with traumatic brain injuries (40), videoconferencing interventions improved post-treatment emotion-regulatory skills. In a case study involving a man suffering from intermittent explosive disorder, mindfulness-based cognitive behavioral therapy delivered via videoconferencing showed a decline in aggressive episodes (35).
4. Discussion
This systematic literature review aimed to investigate whether emotions can be expressed, experienced, and supported effectively through computer-mediated care and the effects thereof on emotion-related outcomes.
4.1. Context and quality of the studies
The study characteristics show significant variations in the international context, study design, and study population, making it impossible to draw overall conclusions. The majority of the studies originate in the USA (e.g., (25–27)), making it difficult to generalize results to other regions of the world.
Overall, all quantitative studies were of good quality, but the quality of the qualitative studies was low. In contrast to this finding, the ratings of quantitative and qualitative studies by the developers of Qualsyst seem to be relatively similar (24), suggesting that the qualitative studies included in this review are of poor quality (e.g., (45, 46)). Qualitative studies are gaining popularity because they provide an in-depth picture of social health problems and individual experiences. However, the lack of information about the study standards for qualitative studies in the health sector leads to poorly conducted, analyzed, or reported studies (51).
4.2. Emotion expression
The studies on emotion expression are all considered text-based online support communities (e.g., (31)) and describe how much of the conversation contains explicit emotional expression (e.g., (25)). Interestingly, there seems to be some support for a possible disinhibition effect (48), where anonymity lowers the threshold to share emotional experiences online (47). However, no studies investigate whether an observer on the other end of the computer recognizes emotion expression.
4.3. Experiencing emotional support
The studies on experiencing emotional support solely look at text-based message boards. While emotions are regularly expressed online, participants experience less emotional support compared with face-to-face interactions (33). This finding might indicate that computer-mediated empathy online is lacking beyond the initial expression of emotions.
4.4. Emotion outcomes after the interaction
The results concerning emotion outcomes after the interaction are quite heterogeneous. Different intervention modalities lead to different results on emotion expression, making it impossible to draw any general conclusions.
The results are somewhat more evident when looking at emotion regulation. Emotion regulation seems enhanced after going through self-paced online interventions (28, 30, 42, 50) and interventions via videoconferencing (e.g., (40)). However, comparisons with face-to-face treatment are still lacking. Only one study compared face-to-face treatment with videoconferencing, which found lower emotion regulation skills after the videoconferencing condition (37).
4.5. Modalities
It is difficult to compare the modalities of the included studies with those of other studies, as the field is rapidly evolving and different taxonomies exist (e.g., (6, 52)). However, keeping in mind the framework on computer-mediated empathy (15), the characteristics of the online modality that are most relevant for the expression and experience of emotions are (1) communication richness, (2) synchronicity of the modality, (3) transmission quality, and (4) communication content. While communication richness and synchronicity are specific to the modality used, transmission quality is specific to the internet connection, and communication content can be altered by user customization (e.g., using emoticons and avatars and adjusting the webcam position). Therefore, a description of the modality is insufficient to establish these characteristics for the described interventions. Moreover, some studies used a communication mix (e.g., (28, 36, 42, 50)), making it even more difficult to determine the influence of the modality used on emotional expression, experience, and support.
In addition, no studies on text-based interventions looked at the effects of using symbols, images, emoticons (17–19), or textual paralanguage cues (18, 19) to convey emotions, limiting the conclusions that can be drawn.
4.6. Limitations and future directions
The research discussed in this paper can yield significant findings regarding the correlation between computer-mediated care and emotional consequences. Nevertheless, it is imperative to acknowledge the presence of limitations. Firstly, this systematic literature review focused on the eligibility criteria, including adults seeking help with transdiagnostic emotional identification, expression, and regulation. The narrow focus of this study may limit its relevance to other demographics or emotional concerns. In addition, the study explored a restricted number of modalities, such as self-paced interventions and videoconferencing, so it may limit the variety of computer-mediated care options. Chat-based therapies and virtual reality therapy may create different emotional effects.
Furthermore, the available studies show methodological shortcomings. Few studies with quantitative data allowed for statistical comparison of the data (e.g., (28, 34)), and the included qualitative studies were of low quality (e.g., (45, 46)). Furthermore, few studies compared computer-mediated interaction to face-to-face encounters, while no studies compared different technologies with each other.
Future research should describe the modalities used, situational factors, and end-user alterations in sufficient detail to determine the amount of filtering of verbal and non-verbal signals. In addition, studies that investigate how expressing emotions influence how an observer on the other end of the computer experiences these emotions and gives an emotionally supportive response are needed. Moreover, more in-depth analyses of how different verbal and non-verbal cues influence these steps of computer-mediated empathy are lacking.
5. Conclusions
Computer-mediated care is rising, especially in light of the current COVID-19 pandemic. Thus, research on how emotion is expressed and experienced and how to be emotionally supportive during online interactions is crucial. Currently, the study is too limited to draw general conclusions. Self-paced interventions seem to enhance emotion regulation, but research on emotional expression, experience, and support during online interactions is limited.
More in-depth analysis of computer-mediated interaction is needed, which involves looking at the effects of verbal and non-verbal cues and describing the modality used in detail, including any situational factors and end-user modifications.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Author contributions
SC was involved in the conceptualization, formal analysis, investigation, writing the original draft, and reviewing and editing the manuscript. EE contributed to the methodology, formal analysis, investigation, reviewing and editing of the manuscript, and supervision. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by the “Agentschap innoveren en ondernemen” (grant number TETRA HBC.2017.0064).
Acknowledgments
We would like to thank the research group that made this review possible.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fdgth.2023.1216268/full#supplementary-material
References
1. Shore J. The evolution and history of telepsychiatry and its impact on psychiatric care: current implications for psychiatrists and psychiatric organizations. Int Rev Psychiatry. (2015) 27(6):469–75. doi: 10.3109/09540261.2015.1072086
2. Torous J, Roberts LW. Needed innovation in digital health and smartphone applications for mental health: transparency and trust. JAMA Psychiatry. (2017) 74(5):437–8. doi: 10.1001/jamapsychiatry.2017.0262
3. American Psychiatric Association. Practice guidance for COVID-19. (2020). Available at: https://www.psychiatry.org/psychiatrists/covid-19-coronavirus/practice-guidance-for-covid-19.
4. American Telemedicine Association. State of the states report: coverage and reimbursement. (2019).
5. Backhaus A, Agha Z, Maglione ML, Repp A, Ross B, Zuest D, et al. Videoconferencing psychotherapy: a systematic review. Psychol Serv. (2012) 9(2):111–31. doi: 10.1037/a0027924
6. Barak A, Hen L, Boniel-Nissim M, Shapira N. A comprehensive review and a meta-analysis of the effectiveness of internet-based psychotherapeutic interventions. J Technol Hum Serv. (2008) 26(2–4):109–60. doi: 10.1080/15228830802094429
7. Bee PE, Bower P, Lovell K, Gilbody S, Richards D, Gask L, et al. Psychotherapy mediated by remote communication technologies: a meta-analytic review. BMC Psychiatry. (2008) 8(1):60. doi: 10.1186/1471-244X-8-60
8. Hilty DM, Ferrer DC, Parish MB, Johnston B, Callahan EJ, Yellowlees PM. The effectiveness of telemental health: a 2013 review. Telemed J E Health. (2013) 19(6):444–54. doi: 10.1089/tmj.2013.0075
9. Comer JS, Furr JM, Miguel EM, Cooper-Vince CE, Carpenter AL, Elkins RM, et al. Remotely delivering real-time parent training to the home: an initial randomized trial of Internet-delivered parent–child interaction therapy (I-PCIT). J Consult Clin Psychol. (2017) 85(9):909–17. doi: 10.1037/ccp0000230
10. Nelson E-L, Barnard M, Cain S. Treating childhood depression over videoconferencing. Telemed J E Health. (2003) 9(1):49–55. doi: 10.1089/153056203763317648
11. Simpson SG, Reid CL. Therapeutic alliance in videoconferencing psychotherapy: a review: alliance in videoconferencing psychotherapy. Aust J Rural Health. (2014) 22(6):280–99. doi: 10.1111/ajr.12149
12. Bambling M, King R, Reid W, Wegner K. Online counselling: the experience of counsellors providing synchronous single session counselling to young people. Couns Psychother Res. (2008) 8:110–6. doi: 10.1080/14733140802055011
13. Carrier LM, Spradlin A, Bunce JP, Rosen LD. Virtual empathy: positive and negative impacts of going online upon empathy in young adults. Comput Human Behav. (2015) 52:39–48. doi: 10.1016/j.chb.2015.05.026
14. Liu X, Sawada Y, Takizawa T, Sato H, Sato M, Sakamoto H, et al. Doctor-patient communication: a comparison between telemedicine consultation and face-to-face consultation. Intern Med. (2007) 46(5):227–32. doi: 10.2169/internalmedicine.46.1813
15. Grondin F, Lomanowska AM, Jackson PL. Empathy in computer-mediated interactions: a conceptual framework for research and clinical practice. Clin Psychol Sci Pract. (2019) 26(4):1–17. doi: 10.1111/cpsp.12298
16. Barak A, Klein B, Proudfoot JG. Defining internet-supported therapeutic interventions. Ann Behav Med. (2009) 38(1):4–17. doi: 10.1007/s12160-009-9130-7
17. Derks D, Fischer AH, Bos AER. The role of emotion in computer-mediated communication: a review. Comput Human Behav. (2008) 24(3):766–85. doi: 10.1016/j.chb.2007.04.004
18. Luangrath AW, Peck J, Barger VA. Textual paralanguage and its implications for marketing communications. J Consum Psychol. (2017) 27(1):98–107. doi: 10.1016/j.jcps.2016.05.002
19. Rodríguez-Hidalgo C, Tan ESH, Verlegh PWJ. Expressing emotions in blogs: the role of textual paralinguistic cues in online venting and social sharing posts. Comput Human Behav. (2017) 73:638–49. doi: 10.1016/j.chb.2017.04.007
20. Hall JA, Harrigan JA, Rosenthal R. Nonverbal behavior in clinician—patient interaction. Appl Prev Psychol. (1995) 4(1):21–37. doi: 10.1016/S0962-1849(05)80049-6
21. Riess H, Kraft-Todd G. E.M.P.A.T.H.Y.: a tool to enhance nonverbal communication between clinicians and their patients. Acad Med. (2014) 89(8):1108–12. doi: 10.1097/ACM.0000000000000287
22. Elliott R, Bohart A, Watson J, Greenberg L. Empathy. Psychotherapy (Chic). (2011) 48:43–9. doi: 10.1037/a0022187
23. Zaki J, Williams WC. Interpersonal emotion regulation. Emotion. (2013) 13(5):803–10. doi: 10.1037/a0033839
24. Kmet LM, Lee RC, Cook LS, Alberta Heritage Foundation for Medical Research. In: Standard quality assessment criteria for evaluating primary research papers from a variety of fields. Edmonton, Alberta, Canada: Alberta Heritage Foundation for Medical Research (2004). Available at: http://ra.ocls.ca/ra/login.aspx?inst=centennial&url=https://www.deslibris.ca/ID/200548
25. *Blank TO, Adams-Blodnieks M. The who and the what of usage of two cancer online communities. Comput Human Behav. (2007) 23(3):1249–57. doi: 10.1016/j.chb.2004.12.003
26. *Collie K, Kreshka M, Ferrier S, Parsons R, Graddy K, Avram S, et al. Videoconferencing for delivery of breast cancer support groups to women living in rural communities: a pilot study. Psychooncology. (2007) 16:778–82. doi: 10.1002/pon.1145
27. *Lewallen AC, Owen JE, Bantum EO, Stanton AL. How language affects peer responsiveness in an online cancer support group: implications for treatment design and facilitation. Psychooncology. (2014) 23(7):766–72. doi: 10.1002/pon.3477
28. *Brand BL, Schielke HJ, Putnam KT, Putnam FW, Loewenstein RJ, Myrick A, et al. An online educational program for individuals with dissociative disorders and their clinicians: 1-year and 2-year follow-up. J Trauma Stress. (2019) 32(1):156–66. doi: 10.1002/jts.22370
29. *Foster D. “Keep complaining til someone listens”: exchanges of tacit healthcare knowledge in online illness communities. Soc Sci Med. (2016) 166:25–32. doi: 10.1016/j.socscimed.2016.08.007
30. *Villani D, Cognetta C, Repetto C, Serino S, Toniolo D, Scanzi F, et al. Promoting emotional well-being in older breast cancer patients: results from an eHealth intervention. Front Psychol. (2018) 9:1–12. doi: 10.3389/fpsyg.2018.02279
31. *Aho AL, Paavilainen E, Kaunonen M. Mothers’ experiences of peer support via an Internet discussion forum after the death of a child. Scand J Caring Sci. (2012) 26(3):417–26. doi: 10.1111/j.1471-6712.2011.00929.x
32. *Setoyama Y, Yamazaki Y, Namayama K. Benefits of peer support in online Japanese breast cancer communities: differences between lurkers and posters. J Med Internet Res. (2011) 13(4):e122. doi: 10.2196/jmir.1696
33. *Setoyama Y, Yamazaki Y, Nakayama K. Comparing support to breast cancer patients from online communities and face-to-face support groups. Patient Educ Couns. (2011) 85(2):95–100. doi: 10.1016/j.pec.2010.11.008
34. *Wright K. Social support within an on-line cancer community: an assessment of emotional support, perceptions of advantages and disadvantages, and motives for using the community from a communication perspective. J Appl Commun Res. (2002) 30(3):195–209. doi: 10.1080/00909880216586
35. *Osma J, Crespo E, Castellano C. Multicomponent cognitive-behavioral therapy for intermittent explosive disorder by videoconferencing: a case study. Ann Psychol. (2016) 32(2):424–32. doi: 10.6018/analesps.32.2.211351
36. *Boß L, Lehr D, Schaub MP, Paz Castro R, Riper H, Berking M, et al. Efficacy of a web-based intervention with and without guidance for employees with risky drinking: results of a three-arm randomized controlled trial. Addiction. (2018) 113(4):635–46. doi: 10.1111/add.14085
37. *Chavooshi B, Mohammadkhani P, Dolatshahi B. Telemedicine vs. in-person delivery of intensive short-term dynamic psychotherapy for patients with medically unexplained pain: a 12-month randomized, controlled trial. J Telemed Telecare. (2016) 23:133–41. doi: 10.1177/1357633X15627382
38. *Czepczor-Bernat K, Brytek-Matera A, Staniszewska A. The effect of a web-based psychoeducation on emotional functioning, eating behaviors, and body image among premenopausal women with excess body weight. Arch Womens Ment Health. (2020) 24:423–35. doi: 10.1007/s00737-020-01077-1
39. *Lieberman MA, Golant M, Giese-Davis J, Winzlenberg A, Benjamin H, Humphreys K, et al. Electronic support groups for breast carcinoma: a clinical trial of effectiveness. Cancer. (2003) 97(4):920–5. doi: 10.1002/cncr.11145
40. *Tsaousides T, Spielman L, Kajankova M, Guetta G, Gordon W, Dams-O'Connor K. Improving emotion regulation following web-based group intervention for individuals with traumatic brain injury. J Head Trauma Rehabil. (2017) 32(5):354–65. doi: 10.1097/HTR.0000000000000345
41. *Weiss BJ, Azevedo K, Webb K, Gimeno J, Cloitre M. Telemental health delivery of skills training in affective and interpersonal regulation (STAIR) for rural women veterans who have experienced military sexual trauma. J Trauma Stress. (2018) 31(4):620–5. doi: 10.1002/jts.22305
42. *Ebert DD, Lehr D, Heber E, Riper H, Cuijpers P, Berking M. Internet- and mobile-based stress management for employees with adherence-focused guidance: efficacy and mechanism of change. Scand J Work Environ Health. (2016) 42(5):382–94. doi: 10.5271/sjweh.3573
43. *Glück TM, Maercker A. A randomized controlled pilot study of a brief web-based mindfulness training. BMC Psychiatry. (2011) 11(1):1–12. doi: 10.1186/1471-244X-11-175
44. *Ruwaard J, Lange A, Bouwman M, Broeksteeg J, Schrieken B. E-mailed standardized cognitive behavioural treatment of work-related stress: a randomized controlled trial. Cogn Behav Ther. (2007) 36:179–92. doi: 10.1080/16506070701381863
45. *Döveling K. Emotion regulation in bereavement: searching for and finding emotional support in social network sites. New Rev Hypermedia Multimed. (2015) 21:106–22. doi: 10.1080/13614568.2014.983558
46. *Nicholas DB, McNeil T, Montgomery G, Stapleford C, McClure M. Communication features in an online group for fathers of children with spina bifida: considerations for group development among men. Soc Work Groups. (2004) 26(2):65–80. doi: 10.1300/J009v26n02_06
47. *Doran J, Lewis C. Posting incognito … males with eating problems: online emotional expression and support. J Cyber Rehab. (2011) 4:341.
48. Suler J. The online disinhibition effect. Cyberpsychol Behavior. (2004) 7:321–6. doi: 10.1089/1094931041291295
49. *Köppe C, Held MJ, Schütz A. Improving emotion perception and emotion regulation through a web-based emotional intelligence training (WEIT) program for future leaders. Int J Emot Educ. (2019) 11(2):17–32. doi: 10.20378/irb-46523
50. *Fonseca A, Monteiro F, Alves S, Gorayeb R, Canavarro MC. Be a mom, a web-based intervention to prevent postpartum depression: the enhancement of self-regulatory skills and its association with postpartum depressive symptoms. Front Psychol. (2019) 10:1–10. doi: 10.3389/fpsyg.2019.00265
51. Collingridge DS, Gantt EE. The quality of qualitative research. Am J Med Qual. (2008) 23(5):389–95. doi: 10.1177/1062860608320646
52. Slattery BW, Haugh S, O’Connor L, Francis K, Dwyer CP, O’Higgins S, et al. An evaluation of the effectiveness of the modalities used to deliver electronic health interventions for chronic pain: systematic review with network meta-analysis. J Med Internet Res. (2019) 21(7):1–18. doi: 10.2196/11086
Keywords: eHealth, computer-mediated care, emotion regulation, empathy, emotional support, emotion expression
Citation: De Coninck S and Emmers E (2023) “Online, the counselor can't see me cry”: a systematic literature review on emotion and computer-mediated care. Front. Digit. Health 5:1216268. doi: 10.3389/fdgth.2023.1216268
Received: 3 May 2023; Accepted: 31 July 2023;
Published: 1 September 2023.
Edited by:
Uffe Kock Wiil, University of Southern Denmark, DenmarkReviewed by:
Rüdiger Christoph Pryss, Julius Maximilian University of Würzburg, GermanyLucia Luciana Mosca, Scuola di Specializzazione in Psicoterapia Gestaltica Integrata (SIPGI), Italy
© 2023 De Coninck and Emmers. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Sarah De Coninck c2FyYWguZGVjb25pbmNrQHVjbGwuYmU=
 Sarah De Coninck
Sarah De Coninck Elke Emmers
Elke Emmers