
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Digit. Health , 24 August 2023
Sec. Health Technology Implementation
Volume 5 - 2023 | https://doi.org/10.3389/fdgth.2023.1176130
This article is part of the Research Topic Intelligent Approaches to Smart Mental Health Monitoring and Management: Implementation, Validation and Promotion View all 8 articles
Introduction: Mental disorders are often underdiagnosed in routine diagnostic procedures due to the use of unstandardized assessments; this can result in people either not receiving necessary treatment or receiving ineffective treatment for their condition. Klenico is an online diagnostic software system that facilitates diagnosis of mental disorders in adults through the use of standardized procedures. The procedure encompasses two modules, self-report and clinical validation. The current study aimed to confirm the validity of the Klenico assessment in a large clinical sample.
Methods: Fully anonymized data from 495 adult inpatients were used. ICD-10 diagnoses were made during an initial interview by the clinical staff. Afterwards, patients filled out self-report questionnaires (BDI-II, BSI, EDE-Q, OCI-R, PHQ-D, and Y-BOCS) and completed the Klenico self-report module, which involves selecting and rating the severity of applicable symptoms. Finally, in the clinical validation module, mental health professionals validated the symptoms endorsed in the self-report module. Six Klenico domains were tested against patient self-reports and routine ICD-10 diagnoses by following the multitrait-multimethod approach. Internal consistency was assessed by calculating Cronbach's alpha.
Results: The Klenico depressive disorders, OCD, and somatoform disorders domains revealed high correlations with the congruent questionnaires (i.e., those pertaining to these specific disorders) and revealed low correlations with the noncongruent questionnaires (i.e., those pertaining to other disorders), therefore evidencing construct validity. For the eating disorders and psychotic disorders domains, divergent validity was demonstrated. For the anxiety disorders domain, although analysis mostly indicated construct validity, this should be further confirmed.
Discussion: Overall, the results largely confirmed the construct validity of the Klenico assessment, demonstrating its use as an easy-to-use, valid, standardized, and comprehensive instrument for diagnosing mental disorders.
Mental disorders are widespread across the globe. Estimates suggest that the general population has a 25% 12-month prevalence (1) and that one in three people will develop a mental disorder at some point in their life (2). Mental disorders have profound detrimental effects beyond individual suffering. Patients with mental disorders show significantly higher rates of mortality (3), which results in a substantial reduction in life expectancy of about 10–20 years (4). In addition, mental disorders impose substantial economic costs on the individual as well as on society. While individuals experience less income due to their disability, societies are faced with substantial health care costs and are additionally impacted by the loss of productivity from reduced labor, the loss of income tax revenue, and increased government support payments (5–7).
Further aggravating the burdens on an individual and societal level is the comorbidity commonly seen in mental disorders (8–12). For instance, a representative study with 9,282 adult respondents revealed that in more than 40% of 12-month cases, patients with mental disorders had comorbid diagnoses (12). Comorbidity in mental disorders is of great clinical importance because it is strongly related to overall disorder severity (12). Patients with multiple, comorbid mental disorders are likely to have poorer treatment outcome and prognosis as well as increased levels of suicidality (13, 14).
In routine clinical practice, however, comorbidity is often underrecognized (15) and mental disorders in general are often under- or misdiagnosed (16, 17). For instance, misdiagnosis rate in primary care has been shown to reach up to 66% for major depression (16) and up to 50% for bipolar disorders (17). This underdiagnosis is often the result of the use of unstandardized instruments (18). A meta-analysis based on 39 primary studies with more than 15,000 participants comparing the results of standardized diagnostic interviews and unstandardized interviews by clinical experts demonstrated that a significant portion of diagnoses are missed if unstandardized interviews are used (19). Moreover, diagnostic agreement between the two approaches was only low to moderate for most diagnoses. Consequently, there are considerable differences in the outcome of the diagnostic assessment when interviews are conducted by different methods (19). These findings highlight the importance of standardized diagnostic procedures.
However, in routine clinical practice, standardized instruments are rarely used. For example, only 15% of patients are diagnosed by using structured interviews. One reason for this low use of structured assessments is that mental health professionals consider these too time-consuming. Moreover, familiarity with such instruments is lacking, while clinical utility of unstructured clinical interviews is overestimated (20). For these reasons, a standardized yet time-efficient diagnostic software program, which is easy to implement in everyday clinical practice, could have the potential to fill this gap in current diagnostic procedures.
To address this challenge, Klenico was developed (21). Klenico is an online diagnostic software tool for routine mental health care based on the 10th revision of the International Classification of Diseases (ICD-10) (22). Klenico uses standardized procedures and involves two modules. First, in the self-report module, patients select and rate applicable symptoms. Second, in the clinical validation module, mental health professionals validate the symptoms endorsed in the self-report module by means of a semi-structured interview. Based on the information obtained in these two modules, mental health professionals are guided toward ICD-10 diagnoses.
Klenico covers the following mental disorders and aggregated disorder domains: anxiety disorders [agoraphobia, generalized anxiety disorder (GAD), panic disorder, social pobias, specific phobias]; disorders of adult personality and behavior; eating disorders (anorexia nervosa, bulimia nervosa); mental and behavioral disorders due to psychoactive substance use; mood (affective) disorders (depressive disorders, mania); obsessive-compulsive disorder (OCD); reaction to severe stress and adjustment disorders; and psychotic disorders (schizophrenia, schizotypal and delusional disorders). Additionally, aspects of autism spectrum disorder, attention deficit hyperactivity disorder (ADHD), and dementia were included. Furthermore, Klenico screens for self-harm, potential harm to others, and suicidal ideation.
Klenico was developed in collaboration with clinical experts, including psychologists and psychiatrists, to ensure high content validity. For additional information on how the Klenico system was developed, including the selection of disorders and symptoms, as well as the development and selection of items, see Lustig et al. (23).
Preliminary validity of the Klenico self-report module has been confirmed in a study comparing the results of Klenico to the gold-standard Structured Clinical Interview for DSM-IV (SCID) in an outpatient sample. Klenico led to similar diagnostic results as the SCID, demonstrating criterion validity. Moreover initial convergent and divergent validity were shown (Reutimann et al., in press1). Evidence for factorial validity and sensitivity to change for the Klenico depression domain was demonstrated in a sample of inpatients from the same clinic as the sample used in the current study (Reutimann et al., submitted manuscript2).
The current study seeks to confirm the above-mentioned preliminary results in a larger sample and with more fine-grained analyses. The aim of this study was to test construct validity in a routine clinical inpatient sample by focusing on both self-report and clinical validation modules of Klenico. In the present study, all those Klenico domains were tested for which congruent routine self-report questionnaires were available.
Data were collected between 2019 and 2022 in a psychotherapeutic inpatient clinic that treats patients with a wide range of mental disorders, particularly those with eating disorders, OCD, and depressive disorders. Patients receive cognitive-behavioral therapy both individually and in group settings.
All patients underwent the clinic's routine diagnostic procedure, from which the data in this study originated. The Klenico system was temporarily integrated into this routine as an add-on to usual care.
Upon admission, patients were informed about the procedures by the clinical staff and asked for written consent that their data may be used for scientific studies. On the day of admission, patients received their routine diagnosis according to ICD-10 after an initial unstructured interview by the clinic's mental health professionals. Afterwards, patients were given routine self-report questionnaires (BDI-II, PHQ, and BSI were given to all patients; Y-BOCS, OCI-R, and EDE-Q disorder specific) and access to the Klenico self-report module by clinic staff.
Within the first two weeks of their stay, patients completed the routine questionnaires and responded to the Klenico self-report module on a device of their choice (computer or tablet). Finally, the clinic's mental health professionals completed the Klenico clinical validation module with each patient. The timing of the clinical validation depended on the availability of the professionals.
Before conducting their first Klenico clinical validation, professionals received an introduction and a demo on how to use the system, as well as an explanation of how to interpret and explain the results. Most of the professionals were psychotherapists in training for cognitive behavioural therapy under supervision with a minimum of one year professional experience. In addition, a co-therapist with several years of professional experience was part of the team. All of these professionals exhibited the required competence to make diagnoses in Germany. On average, the professionals conducted 2–3 clinical validations per week, and the average duration of the clinical validations was 66 min.
The BDI-II (24) is a valid and reliable questionnaire (25) to assess depressive symptoms. It consists of 21 items on a four-point Likert scale ranging from 0 (symptom absent) to 3 (severe symptom) with a maximum score of 63. The sum score was calculated for each participant. Cronbach's alpha was 0.75.
The PHQ-D (26) is based on the Diagnostic and Statistical Manual of Mental Disorders, 4th Edition (DSM-IV) and has good psychometric properties (27). Its short form consists of nine items for depression (PHQ-9), seven items for generalized anxiety (PHQ-GAD-7), both with a four-point Likert scale ranging from 0 (not at all) to 3 (nearly every day), and 15 items for somatoform symptoms (PHQ-15) with a three-point Likert scale ranging from 0 (not bothered at all) to 2 (bothered a lot). Sum scores of PHQ-9 (maximum score = 27), PHQ-15 (maximum score = 30), and PHQ-GAD-7 (maximum score = 21) were calculated for each participant. Cronbach's alpha was 0.84, 0.80 and 0.83, respectively.
The BSI (28) consists of 53 items on nine subscales (somatization, obsession-compulsion, interpersonal sensitivity, depression, anxiety, hostility/aggression, phobic anxiety, paranoid ideation, and psychoticism) with a five-point Likert scale ranging from 0 (not at all) to 4 (extremely). The BSI shows satisfactory psychometric properties. Its factor structure is questionable (29). The sum score was calculated for each subscale for each participant. Cronbach's alpha was between 0.70 and 0.83.
The Y-BOCS (30) consists of a symptom checklist to quantify different obsessions and actions. Impairment in everyday life, suffering, and resistance and control over the symptoms are recorded separately for obsessions and compulsions on a five-point scale ranging from 0 (no symptoms) to 4 (extreme symptoms). The sum score was calculated for each participant, with a maximum of 40. The Y-BOCS is a valid and reliable instrument for assessing OCD symptoms (31, 32). Cronbach's alpha was 0.76.
The OCI-R (33) is a self-assessment tool with 18 items recording the most common OCD symptom areas on six subscales (washing, checking, ordering, neutralizing, obsessing, and hoarding) with a five-point Likert scale ranging from 0 (not at all) to 4 (extremely). It is a reliable and valid questionnaire (34). The sum score was calculated (maximum score = 168). Cronbach's alpha was 0.90.
The EDE-Q (35), comprising 28 items and four subscales (restraint, eating concern, weight concern, shape worries), is a screening tool that measures the range and severity of eating disorder symptoms on a seven-point scale, ranging from 0 (never) to 6 (every day). It has good psychometric properties (36). However, the number of its underlying factors is questionable (37). The sum score was calculated for each participant, with a maximum of 168. Cronbach's alpha was 0.76.
After the initial, unstructured interview, the treating mental health professionals provided diagnoses based on the patients' current symptoms and coded them according to ICD-10. Compared to structured interviews, unstructured interviews lack validity (38), which can affect the quality of the diagnoses made (15).
In Klenico's self-report module, patients were presented with 379 items based on ICD-10. The items were randomly displayed in groups of nine per screen, of which patients selected applicable ones (i.e., the symptoms that applied to them). Patients then rated the symptom severity by dragging and dropping the previously selected items onto a visual analogue scale ranging from 1 to 100. In the clinical validation module, mental health professionals confirmed or re-rated patients' self-reports. They also assessed additional items that required external perspective and therefore, did not occur in the self-report module (97 items). In this study, all those Klenico domains were tested for which congruent routine self-report questionnaires were available (anxiety disorders, depressive disorders, eating disorders, OCD, psychotic disorders, and somatoform disorders). These domains contain a total of 176 items in the self-report module. The mean score for each Klenico domain tested was calculated.
Anonymized data from 495 adults [n = 336 female, n = 159 male, mean age = 38.9 (SD = 15.0)] were used. Of these, 443 datasets included the full assessment because 52 patients only completed the self-report module.
Table 1 reports the frequencies of the given routine ICD-10 diagnoses by the clinic's mental health professionals using routine diagnostic procedures. Most frequent were depressive disorders followed by eating disorders. The mean number of diagnoses was 1.9.
The software RStudio was used for data analysis (Version 2021.9.1.372, Boston, MA, USA). P-values < 0.05 were considered statistically significant.
Cronbach's alpha values of the tested Klenico domains were calculated for evaluation of internal consistency.
To determine convergent and divergent validity, a multitrait-multimethod (MTMM) matrix approach was used. This approach allows for concurrent inclusion of multimodal instruments and is a common method for evaluating psychological measurements (39).
To ensure a comprehensive evaluation of the Klenico system and obtain significant insights, all instruments used in the clinic's routine diagnostic procedures, such as the routine self-report questionnaires and routine ICD-10 diagnoses, were included in the analysis despite their limitations.
The MTMM contains three different types of correlations: Monotrait-heteromethod (associations between Klenico domains and corresponding self-report questionnaires as well as ICD-10 diagnoses), heterotrait-heteromethod (associations between Klenico domains and noncorresponding self-report questionnaires as well as ICD-10 diagnoses), and heterotrait-monomethod (associations between Klenico domains themselves).
By convention (40), convergent validity is demonstrated if the monotrait-heteromethod correlations are significantly high. Divergent validity is demonstrated if the heterotrait-monomethod correlations are lower than the monotrait-heteromethod correlations, the heterotrait-heteromethod correlations are lower than the monotrait-heteromethod correlations, and the correlation coefficients are comparably large, both within a method and between the different methods (40).
Pearson's correlation coefficients were calculated for associations between interval scaled variables, point-biserial correlations (rpb) were calculated for associations between interval scaled and dichotom variables, and Phi coefficients were calculated for associations between dichotom variables.
Correlation coefficients between 0.10 and 0.29 were considered as small, between 0.30 and 0.49 as medium, and ≥0.50 as large correlations (41).
Klenico domains demonstrated sufficient Cronbach's alpha coefficients of 0.70 or higher, except for the psychotic disorders (0.47) domain. For further details see Table 2.
Correlations in the MTMM matrix must meet the following criteria to fulfill construct validity: (I) the monotrait-heteromethod correlations are significantly high; (II) the heterotrait-monomethod correlations are lower than the monotrait-heteromethod correlations; (III) the heterotrait-heteromethod correlations are lower than the monotrait-heteromethod correlations; and (IV) the correlation coefficients are approximately equal both within a method and between the different methods. Findings pertaining to these criteria are indicated in the descriptions below.
Depressive disorders. (I) This domain revealed significantly high monotrait-heteromethod correlations with the compared routine self-report questionnaire scales (ranging from r = 0.68 to r = 0.71) but a low correlation with the corresponding ICD-10 diagnosis of depression (r = 0.18). (II), (III) The monotrait-heteromethod correlations (ranging from r = 0.68 to r = 0.71) were all higher than both the heterotrait-monomethod correlations (ranging from r = 0.23 to r = 0.60) and the heterotrait-heteromethod correlations (ranging from r = −0.02 to r = 0.60), except for the correlation with the corresponding ICD-10 diagnosis.
Eating disorders. (I) This domain showed significantly high monotrait-heteromethod associations with the congruent ICD-10 diagnosis (r = 0.70) but no significant correlation with the EDE-Q (r = 0.26). (II), (III) Apart from this nonsignificant association with the EDE-Q, all heterotrait correlations of the Klenico eating disorders domain (ranging from r = 0.00 to r = 0.32) are lower than the monotrait correlation with the compared ICD-10 diagnosis (r = 0.70).
Anxiety disorders. (I) This domain showed high monotrait-heteromethod correlations with the BSI (phobic) anxiety scales (ranging from r = 0.57 to r = 0.64), medium correlations with the BSI interpersonal sensitivity (r = 0.43) and the PHQ-GAD-7 (r = 0.45) scales, and weak correlations with the ICD-10 diagnosis (r = 0.23). (II) Its heterotrait-monomethod correlation with the Klenico somatoform disorders domain (r = 0.66) was higher than the monotrait-heteromethod correlations. (III) However, it showed particularly higher heterotrait-heteromethod correlations with the OCI-R (r = 0.61) than the monotrait-heteromethod correlations with the PHQ-GAD-7, the BSI (social) anxiety scales, and the ICD-10 diagnosis.
Somatoform disorders. (I) The somatoform disorder domain revealed significantly high monotrait-heteromethod correlations with the compared routine self-report questionnaire scales (ranging from r = 0.59 to r = 0.61) but low associations with the corresponding ICD-10 diagnoses (r = 0.21). (II) Again, the heterotrait-monomethod correlation between the somatoform disorders and anxiety disorders domains was higher (r = 0.66) than the monotrait-heteromethod correlations for the somatoform disorders domain. (III) However, it showed higher monotrait-heteromethod correlations (ranging from r = 0.59 to 0.61) than heterotrait-heteromethod correlations (ranging from r = 0.01 to r = 0.51), except for the association with the corresponding ICD-10 diagnosis (r = 0.21).
OCD. (I) This domain showed high correlations with the congruent ICD-10 diagnosis (r = 0.52) and the Y-BOCS (r = 0.73), a weak correlation with the BSI OCD scale (r = 0.29), and a nonsignificant correlation with the OCI-R (r = 0.31). (II) Further, the Klenico OCD domain revealed higher monotrait-heteromethod correlations (ranging from r = 0.52 to r = 0.73) than heterotrait-monomethod correlations (ranging from r = 0.23 to r = 0.39), except for the correlations with the OCI-R (r = 0.31) and BSI OCD (r = 0.29), which were lower. (III) Monotrait-heteromethod correlations (ranging from r = 0.52 to r = 0.73) were higher than heterotrait-heteromethod correlations (ranging from r = 0.02 to r = 0.34), except for the correlation with the BSI OCD scale (r = 0.29) and the nonsignificant correlation with the OCI-R (r = 0.31).
Psychotic disorders. (I) The Klenico psychotic disorders scale revealed only low monotrait-heteromethod correlations with the compared BSI psychoticism and paranoid ideation scales (ranging from r = 0.10 to r = 0.13) and no significant correlations with the given routine diagnosis (r = 0.03). (II), (III) Its monotrait-heteromethod correlations with the congruent questionnaires and ICD-10 diagnoses were lower (ranging from r = 0.10 to r = 0.13) than the heteromethod correlations (ranging from r = 0.02 to r = 0.16).
Correlations within and between methods. (IV) The heterotrait-heteromethod correlations of the Klenico domains are comparable to the monotrait-heteromethod correlations for the respective domains. For example, the Klenico OCD domain showed a correlation coefficient of r = 0.23 with the Klenico depressive disorders domain and coefficients of r = 0.14, r = 0.14, and r = 0.18 with the BDI depression scale, the PHQ-9, and the BDI-II, respectively.
Correlation coefficients for all Klenico domains are presented in Table 3. The full MTMM can be found in the Supplementary Materials.
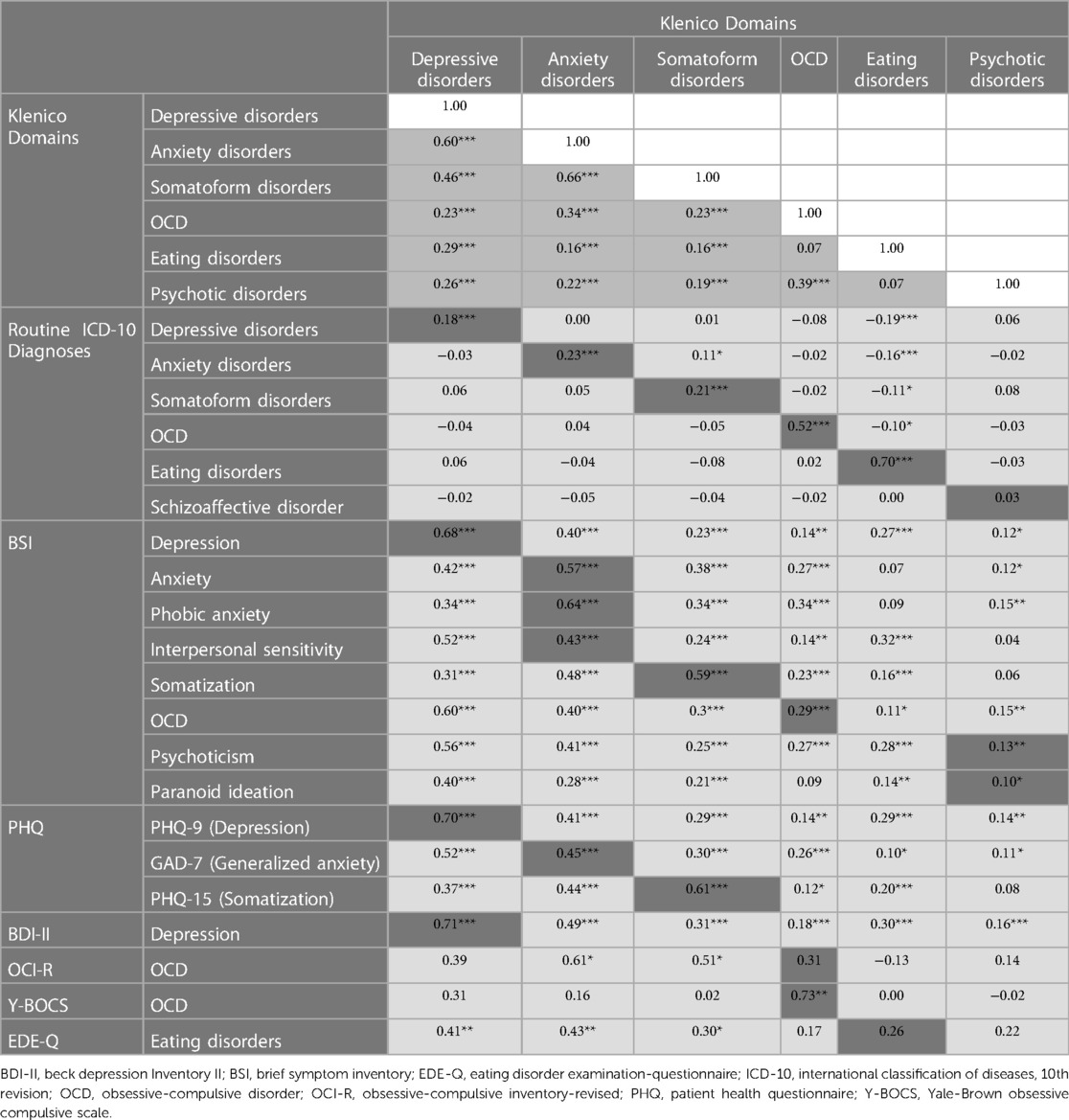
Table 3. Correlation coefficients of the tested Klenico domains with the compared methods of the MTMM approach. The full MTMM matrix can be found in the Supplementary Material.
This current study aimed to confirm the construct validity of the Klenico assessment by using a MTMM approach to compare the results of the Klenico domain scores with standard self-report questionnaires and routine ICD-10 diagnoses in a large clinical inpatient sample.
While the Klenico anxiety disorders domain demonstrated strong congruent associations with the BSI (phobic) anxiety scales, correlations with the BSI interpersonal sensitivity scale and the PHQ-GAD-7 were in the medium range, and the correlation with the congruent ICD-10 diagnosis was in the low range. The heterotrait-monomethod correlation between this domain and the Klenico somatoform disorders domain was higher than the correlations with the congruent questionnaire scales, and the correlations with the rest of the Klenico domains were lower. The heterotrait-heteromethod correlation with the OCI-R was in the high range and higher than the monotrait-heteromethod correlations, except for the correlation with the BSI phobic anxiety scale. Furthermore, the heterotrait-heteromethod correlations with the BDI-II and the BSI somatization scale were higher than the medium-range monotrait-heteromethod correlations with the BSI interpersonal sensitivity scale and the PHQ-GAD-7.
Reasons for the low associations of the anxiety disorders domain with the corresponding ICD-10 diagnosis might be inherent in routine diagnostic procedures. Diagnoses were made by the inpatient clinic professionals using unstructured interviews, which often lack validity and reliability, thus compromising the quality of the compared ICD-10 diagnoses (42). This counts for the anxiety disorders domain and all other Klenico domains tested. Therefore, the ICD-10 diagnoses are not used as a decisive criterion for the construct validity of the Klenico domains, but rather provide additional indications.
The same applies to the comparison to the BSI. The construction of the BSI was aimed at the assessment of symptom dimensions. Consequently, it demonstrates considerable heterogeneity in its underlying constructs and has questionable factorial validity (43). Therefore, the BSI is not used as a main criterion but delivers additional indications on construct validity. In the case of anxiety disorders, the BSI interpersonal sensitivity scale includes symptoms that reflect aspects of depression rather than of social anxiety disorder, which explains the medium-range correlation with the Klenico anxiety disorders domain. This is reflected by a recent study (29).
The medium-range correlation between the Klenico anxiety disorders domain and the PHQ-GAD-7 can be attributed to the fact that the PHQ was developed based on the diagnostic criteria of the DSM (26). However, the items included in the Klenico anxiety disorders domain are derived from the ICD-10 diagnostic criteria, which differ substantially from those in the DSM (44).
One possible explanation for the high correlation of the Klenico anxiety disorders domain with the OCI-R is that the OCI-R may measure certain aspects of anxiety. A previous validation study has already shown an association of the OCI-R total score with anxiety questionnaires, albeit in the medium range (45). Additionally, the OCD subscale of the OCI-R revealed large associations with a compared anxiety measure in another study (46).
Finally, the high heterotrait-monomethod correlation between the Klenico anxiety disorders and somatoform disorders domains and also the medium-range heterotrait-heteromethod correlation with the BSI somatization scale is not surprising, as both disorder domains are highly comorbid (47) and show substantial symptom overlap; anxiety disorders in particular are represented by a wide range of somatic symptoms (48). The same applies to the medium-range heterotrait-heteromethod correlation with the BDI-II because of the highly frequent comorbidity of anxiety and depressive disorders (49).
Overall, although results partially indicate construct validity for the Klenico anxiety disorders domain, this could not be definitively confirmed. The fact that the anxiety disorders were analyzed together as a whole domain and not as individual disorders may have influenced the results. Nonetheless, this summary analysis makes sense due to the partly shared symptomatology and etiology as well as the frequent comorbidities between the different anxiety disorders (50). However, the various disorders still have unique features and distinctions, which can limit a summary analysis (51, 52). Therefore, the anxiety disorders should be analyzed again individually in order to fully confirm the construct validity of the Klenico anxiety disorders domain.
The Klenico depressive disorders domain revealed high correlations with the compared depression measures (BDI-II and PHQ-9) but low correlations with the congruent ICD-10 diagnosis. Consequently, the monotrait-heteromethod correlations for this domain were higher than all the heterotrait correlations, with the exception of the nonsignificant monotrait-heteromethod correlation with the ICD-10 diagnosis.
Due to the high correlations with the well validated PHQ-9 and BDI-II and the low correlations with the noncongruent questionnaires, convergent and divergent validity are established. Accordingly, construct validity of the Klenico depressive disorders domain was demonstrated.
The Klenico eating disorders domain revealed strong correlations with the ICD-10 diagnosis for eating disorders but low correlations with the congruent questionnaire, the EDE-Q. Consequently, while all heteromethod correlations were lower than the monotrait-heteromethod correlation with the ICD-10 diagnosis for eating disorders, they were higher than the monotrait-heteromethod correlation with the EDE-Q.
This nonsignificant correlation between the Klenico eating disorders domain and the EDE-Q is not striking. First, the EDE-Q does not include certain important ICD-10 diagnostic criteria, such as self-initiated vomiting, binge eating, amenorrhea, or loss of libido (53). And secondly, previous studies have failed to establish a one-factor model of the EDE-Q (54), which challenges the calculation of an overall sum score.
Thus, the nonsignificant correlation of the EDE-Q sum score with the Klenico eating disorders domain does not compromise the domain's convergent or divergent validity. Based on the low correlations with the noncongruent questionnaires, divergent validity can be confirmed for the Klenico eating disorders domain. Even the domain's convergent validity is indicated by the high correlation with the ICD-10 eating disorders diagnosis, additional research is needed to compare the domain with other more congruent measurements than the EDE-Q to fully confirm its convergent validity.
The Klenico psychotic disorders domain revealed low correlations with the two corresponding BSI scales, psychoticism and paranoid ideation, and a nonsignificant monotrait-heteromethod correlation with the ICD-10 diagnosis. Although the heterotrait-monomethod correlations with the other Klenico domains were in the medium range, they were higher than the monotrait-heteromethod correlations, except for the eating disorders domain. The heterotrait-heteromethod correlations were all nonsignificant or in the low range. However, the correlations with the BSI phobic anxiety and OCD scales, as well as with the PHQ-9 and BDI-II depression questionnaires, were minimally higher than the monotrait-heteromethod correlations, but all in the low range.
Again, the low correlations between the Klenico psychotic disorders domain and both BSI scales, paranoid ideation and psychoticism, can be attributed to their underlying constructs. These two scales, in particular, have been criticized for representing constructs too heterogeneously (55). Also, the low correlation with the ICD-10 diagnosis is not striking as there was only one corresponding diagnosis for the Klenico psychotic disorders domain, namely schizoaffective disorder.
Although divergent validity for the Klenico psychotic disorders domain is not met based on the MTMM, it was suggested by the finding that all correlations with the noncongruent questionnaires were low. Nevertheless, the convergent validity of the Klenico psychotic disorders domain still needs to be demonstrated in a more suitable sample, for instance from a psychiatric setting, and against more standard questionnaires representing more appropriate constructs.
The Klenico OCD domain revealed high monotrait-heteromethod correlations with the corresponding ICD-10 diagnosis and the Y-BOCS. However, although significant, the associations between the Klenico OCD domain and the BSI OCD scale were low, and correlations with the OCI-R were nonsignificant. All monotrait-heteromethod and heterotrait-monomethod correlations were lower than the monotrait-heteromethod correlations with the ICD-10 diagnosis and the Y-BOCS, but higher than the monotrait-heteromethod correlations with the BSI OCD scale and the OCI-R.
The low correlation of the Klenico OCD domain with the OCI-R can be attributed to this questionnaire's measured OCD construct. Earlier studies found only a medium correlation between the Y-BOCS and the OCI-R (45). This may be because the OCI-R, in contrast to the Klenico OCD domain, tends to measure the stress related to specific OCD conditions rather than measuring overall symptom severity based on diagnostic criteria (56).
The apparent lack of associations between the Klenico OCD domain and the BSI OCD scale can be explained by the properties of the BSI. Half of the items of the OCD scale measure nonspecific symptoms that can also be attributed to depression (57).
Taken together, neither the low correlation with the OCI-R nor the low correlation with the BSI OCS compromises the Klenico OCD domain's construct validity, as the results could be well reasoned on the properties and measured constructs of the two tools. The high correlations with the Y-BOCS, as well as the low correlations with the noncongruent questionnaires and diagnoses, therefore demonstrates its construct validity.
The Klenico somatoform disorders domain showed high correlations with the congruent questionnaire scales (BSI somatization and PHQ-15) but low correlations with the corresponding ICD-10 diagnosis. Consequently, the monotrait-heteromethod correlations with the BSI somatization and the PHQ-15 were higher than all of the heterotrait-heteromethod correlations. Finally, the heterotrait-monomethod correlations were lower than the monotrait-heteromethod correlations, except for the high monotrait-heteromethod correlation with the Klenico anxiety disorders domain.
Again, the high heterotrait-monomethod correlation between the Klenico somatoform disorders and anxiety disorders domains can be explained by the frequent comorbidities between the two domains (47) and the wide range of somatic symptoms common in anxiety disorders (48).
Consequently, convergent and divergent validity are demonstrated according to conventions; therefore, construct validity of the somatoform disorders domain could be confirmed.
All but one of the Klenico domains reached good internal consistency, providing evidence for reliability. The exception was the psychotic disorders domain. This might be explained by the fact that psychotic disorders were insufficiently represented in the sample, as patients with psychotic disorders will more likely be referred to psychiatric instead of psychotherapeutic clinics. It therefore requires further investigation.
As previously mentioned, low correlations between the Klenico anxiety disorders, depressive disorders, and somatoform disorder domains and their corresponding routine ICD-10 diagnoses should not undermine the construct validity of these domains. The low correlations are likely attributable to the quality of the diagnoses, which were based on unstructured interviews conducted by clinic staff. Previous research has indicated that such assessments may lack reliability and validity (38, 42), potentially resulting in incorrect diagnoses (15).
Although it is possible that the properties of the Klenico domains contribute to the low correlations, there are arguments against this. Firstly, the routine ICD-10 diagnoses also showed low or non-significant associations with other well-validated self-report measures, such as the BDI-II and PHQ subscales in our current analysis. Additionally, in a previous study, the Klenico domains showed criterion validity according to the SCID, the gold standard in diagnostics, indicating Klenico's high diagnostic potential (24).
The high correlations observed between the Klenico eating disorders and OCD domains and their respective ICD-10 diagnoses suggest that the quality of diagnoses made via unstructured interview may vary between different disorders and depend on the experience and specialization of the clinical professional.
Consequently, the results of this study once again implies the weaknesses of diagnoses using unstructured interviews and emphasizes the need for standardized assessments. However, since structured tools such as the SCID are rarely used in clinical practice—because, among other reasons, they are considered too time-consuming (20)—new solutions are needed. Diagnostic software such as Klenico, which enables efficient diagnostic procedures, can therefore offer a solution.
The standard diagnosis and the Klenico clinical validation were conducted by psychotherapists (in training), which is a common practice in Germany. Psychotherapists undergo rigorous training and have a licence and therefore, have the competence to diagnose mental disorders.
In Germany, the education of psychotherapy is regulated by law, and the professional title is protected. The provision of psychotherapy is limited to certified psychologists and physicians, including psychiatrists, who have completed extensive specialized training and received official recognition in the field of psychotherapy. Psychologists, for instance, must successfully complete a comprehensive three-year full-time practical training program, totaling 4,200 h. This training includes a year-long internship at an accredited psychiatric institution, six months of clinical work at an outpatient facility, a minimum of 600 h of supervised psychotherapy in an outpatient setting, and attendance of at least 600 h of theoretical seminars.
These characteristics distinguishes Germany from many other countries in Europe and around the world. For instance, in the UK the title of psychotherapist is not protected, and the training is not regulated by law. Instead, professional associations set their own standards for training. As a result, a more diverse range of professional backgrounds, including nursing, social work, and teaching, can access psychotherapist training in the UK and similarly in other countries like Australia.
Overall, the results revealed evidence for construct validity of the Klenico depressive disorders, OCD, and somatoform disorders domains and for reliability of the majority of the tested Klenico domains. Exceptions were the eating disorders and psychotic disorders domains, where only divergent validity was indicated, and the anxiety disorders domain. Validity of these domains needs further confirmation.
Consequently, this study partially confirms the results of previous studies of construct validity of the Klenico in psychotherapeutic in- and outpatient settings (24, 25) and extends previous findings to demonstrate validity of the entire Klenico system, including both the self-report and clinical validation module. Accordingly, Klenico offers high potential for improving diagnostic accuracy by utilizing standardized procedures. Furthermore, the inclusion of all relevant mental disorders can support mental health professionals in comprehensive diagnostics and therefore help reliably identify comorbidities. This is crucial as comorbid mental disorders are highly frequent (58) but often missed in clinical practice, again due to the use of unstructured interviews (15). Thus, only comprehensive, valid diagnoses, which Klenico enables, can lead to effective and evidence-based therapeutic interventions and, ultimately, to successful therapeutic outcomes.
A major strength of the study is the large sample, collected in the routine diagnostic procedures of a psychotherapeutic inpatient clinic, thus reflecting the implementation of the Klenico system in everyday clinical practice while presenting high ecological validity. For those reasons, results are well generalizable to psychotherapeutic inpatient and comparable settings. However, since there are likely fewer patients with severe mental illness in psychotherapeutic compared to psychiatric settings, this may limit the generalizability to psychiatric settings, and therefore requires further investigation.
Due to the design of the MTMM approach and the types of routine self-report questionnaires available for comparison, the individual disorders had to be grouped into domains for this study and not all the Klenico domains were tested. The analysis of the whole domains may have led to certain limitations. This applies in particular to anxiety disorders, which should be examined again separately.
Secondly, since the data for this study were collected in routine diagnostic assessments, we had no influence on which questionnaires were used in the procedure. Therefore, appropriate questionnaires were not available for all Klenico domains, which partially limited the demonstration of convergent validity. For instance, the BSI, which has heterogeneity in the underlying constructs and questionable validity for certain scales, was used for the analysis. Therefore, the conclusions drawn from its comparison must be taken with caution. The same applies to the routine ICD-10 diagnoses used in the comparison because, as already discussed, they may lack reliability and validity given their basis on unstructured interviews. Further investigation is needed for certain Klenico domains, such as addictive disorders or ADHD, due to the lack of suitable questionnaires available for assessment.
Finally, although testing Klenico under real-life clinical conditions had the great advantage of high ecological validity, it also meant that the data collection was not standardized. Therefore, it is not known if and how many patients dropped out of treatment and how the different settings used in the study may vary. Because the interrater agreement of the clinical validation module could not be calculated, heterogeneity in the diagnostic quality of the individual professionals is possible.
In summary, this analysis confirms the earlier preliminary findings for the Klenico self-report module and demonstrates construct validity for the entire Klenico system. These results demonstrate that Klenico has the potential to close the gap of unstandardized diagnostic procedures. The system can support mental health professionals in making accurate diagnoses, which, in turn, can help them to select appropriate, evidence-based treatment for their patients.
Regarding future research, Klenico domains—in particular the eating disorders and psychotic disorders domains—need to be tested against more appropriate questionnaires to confirm their convergent validity. Moreover, future studies should focus on structural models to generate further insights into the factorial and structural validity of the Klenico system.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethical approval was not required for the studies because according to German law, no ethical approval was required for the use of the Klenico in routine diagnostic procedures. With reference to German legislation [Medizinprodukttet-Durchführungsgesetz (MPDG) §47] the test-related use of a medical device with certification (CE marking) does not require an ethics vote if it is carried out within the scope of its intended purpose. Furthermore, the use of Klenic in routine diagnostic procedures falls within the scope of the responsibility of the attending physician (Berufsordnung der Ärztekammern §15). According to the ethics committee of the Ludwig Maximilian University Munich, such data collection with the aim of evaluating the performance of an accepted, evidence-based practice (quality assurance) do not require an ethical approval. Finally no ethical approval was required for analysis of the data, since retrospective studies using already-available, anonymized data are exempt from needing ethics approval, according to the guidelines of the institutional review board at the Ludwig Maximilian University Munich. The study was conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
All authors listed have made a substantial, direct, and intellectual contribution to the work and approved it for publication. All authors contributed to the article and approved the submitted version.
SR, JS, NH, and MA are employed by Klenico Health AG. We declare that this did not affect the collection or the analysis of the data. UV declares the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fdgth.2023.1176130/full#supplementary-material
1Reutimann S, Milanovic D, Gulewtisch MD, Augsburger M. Preliminary validation of the Klenico diagnostic software self-report module through comparison with the diagnostic gold standard in an outpatient routine clinical sample. Health Psychol Behav Med. (in press).
2Reutimann S, Steiner J, Hübscher N, Milanovic D, Voderholzer U, Meule A, et al. Assessing construct validity and sensitivity to change of the Klenico depression scale. (2022). Manuscript submitted for publication.
1. Ten Have M, Tuithof M, van Dorsselae S, Schouten F, Luik AI, de Graaf R. Prevalence and trends of common mental disorders from 2007–2009 to 2019–2022: results from the Netherlands Mental Health Survey and Incidence Studies (NEMESIS), including comparison of prevalence rates before vs. during the COVID-19 pandemic. World Psychiatry. (2023) 22(2):275–85. doi: 10.1002/wps.21087
2. Steel Z, Marnane C, Iranpour C, Chey T, Jackson JW, Patel V, et al. The global prevalence of common mental disorders: a systematic review and meta-analysis 1980–2013. Int J Epidemiol. (2014) 43:476–93. doi: 10.1093/ije/dyu038
3. Lawrence D, Kisely S, Pais J. The epidemiology of excess mortality in people with mental illness. Can J Psychiatry. (2010) 55:752–60. doi: 10.1177/070674371005501202
4. Chesney E, Goodwin GM, Fazel S. Risks of all-cause and suicide mortality in mental disorders: a meta-review. World Psychiatry. (2014) 13:153–60. doi: 10.1002/wps.20128
5. Vigo D, Thornicroft G, Atun R. Estimating the true global burden of mental illness. Lancet Psychiatry. (2016) 3:171–8. doi: 10.1016/S2215-0366(15)00505-2
6. Schofield DJ, Shrestha RN, Percival R, Passey ME, Callander EJ, Kelly SJ. The personal and national costs of mental health conditions: impacts on income, taxes, government support payments due to lost labour force participation. BMC psychiatry. (2011) 11:1–7. doi: 10.1186/1471-244X-11-72
7. Christensen M, Lim C, Saha S, Plana-Ripoll O, Cannon D, Presley F, et al. The cost of mental disorders: a systematic review. Epidemiol Psychiatr Sci. (2020) 29:e161. doi: 10.1017/S204579602000075X
8. Avenevoli S, Swendsen J, He J-P, Burstein M, Merikangas KR. Major depression in the national comorbidity survey–adolescent supplement: prevalence, correlates, and treatment. J Am Acad Child Adolesc Psychiatry. (2015) 54:37–44.e2. doi: 10.1016/j.jaac.2014.10.010
9. Fried EI, van Borkulo CD, Cramer AO, Boschloo L, Schoevers RA, Borsboom D. Mental disorders as networks of problems: a review of recent insights. Soc Psychiatry Psychiatr Epidemiol. (2017) 52:1–10. doi: 10.1007/s00127-016-1319-z
10. Beard C, Millner AJ, Forgeard MJ, Fried EI, Hsu KJ, Treadway M, et al. Network analysis of depression and anxiety symptom relationships in a psychiatric sample. Psychol Med. (2016) 46:3359–69. doi: 10.1017/S0033291716002300
11. Boschloo L, van Borkulo CD, Rhemtulla M, Keyes KM, Borsboom D, Schoevers RA. The network structure of symptoms of the diagnostic and statistical manual of mental disorders. PLoS One. (2015) 10:e0137621. doi: 10.1371/journal.pone.0137621
12. Kessler RC, Chiu WT, Demler O, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the national comorbidity survey replication. Arch Gen Psychiatry. (2005) 62:617–27. doi: 10.1001/archpsyc.62.6.617
13. Nock MK, Hwang I, Sampson NA, Kessler RC. Mental disorders, comorbidity and suicidal behavior: results from the national comorbidity survey replication. Mol Psychiatry. (2010) 15:868–76. doi: 10.1038/mp.2009.29
14. Schoevers RA, Deeg DJH, van Tilburg W, Beekman ATF. Depression and generalized anxiety disorder: co-occurrence and longitudinal patterns in elderly patients. Am J Geriatr Psychiatry. (2005) 13:31–9. doi: 10.1097/00019442-200501000-00006
15. Zimmerman M. A review of 20 years of research on overdiagnosis and underdiagnosis in the Rhode Island methods to improve diagnostic assessment and services (MIDAS) project. Can J Psychiatry. (2016) 61:71–9. doi: 10.1177/0706743715625935
16. Vermani M, Marcus M, Katzman MA. Rates of detection of mood and anxiety disorders in primary care: a descriptive, cross-sectional study. Prim Care Companion CNS Disord. (2011) 13:27211. doi: 10.4088/PCC.10m01013
17. Rakofsky JJ, Dunlop BW W. The over-under on the misdiagnosis of bipolar disorder: a systematic review. Curr Psychiatry Rev. (2015) 11:222–34. doi: 10.2174/1573400512666151117211523
18. Zimmerman M, Chelminski I. Clinician recognition of anxiety disorders in depressed outpatients. J Psychiatr Res. (2003) 37:325–33. doi: 10.1016/S0022-3956(03)00020-7
19. Rettew DC, Lynch AD, Achenbach TM, Dumenci L, Ivanova MY. Meta-analyses of agreement between diagnoses made from clinical evaluations and standardized diagnostic interviews. Int J Methods Psychiatr Res. (2009) 18:169–84. doi: 10.1002/mpr.289
20. Bruchmüller K, Margraf J, Suppiger A, Schneider S. Popular or unpopular? Therapists’ use of structured interviews and their estimation of patient acceptance. Behav Ther. (2011) 42:634–43. doi: 10.1016/j.beth.2011.02.003
21. Klenico Health AG. Available at: https://www.klenico.com/
22. World Health Organization. The ICD-10 classification of mental and behavioural disorders : clinical descriptions and diagnostic guidelines. Classification internationale des troubles mentaux et des troubles du comportement : descriptions cliniques et directives pour le diagnostic (1992) Available at: https://apps.who.int/iris/handle/10665/37958
23. Lustig L. Die Klenico-Items: theoretische Herleitung und empirische Fundierung eines neuen Ansatzes in der psychiatrischen Diagnostik. (2020). Available at: https://www.zora.uzh.ch/id/eprint/189882/
25. Sprinkle SD, Lurie D, Insko SL, Atkinson G, Jones GL, Logan AR, et al. Criterion validity, severity cut scores, and test-retest reliability of the beck depression inventory-II in a university counseling center sample. J Couns Psychol. (2002) 49:381–5. doi: 10.1037/0022-0167.49.3.381
27. Gräfe K, Zipfel S, Herzog W, Löwe B. Screening psychischer störungen mit dem “gesundheitsfragebogen für patienten (PHQ-D)”. Diagnostica. (2004) 50:171–81. doi: 10.1026/0012-1924.50.4.171
28. Derogatis L. Brief symptom inventory (BSI) administration, scoring, and procedures manual. Minneapolis, MN: National Computer Systems, Inc (1993).
29. Prinz U, Nutzinger D, Schulz H, Petermann F, Braukhaus C, Andreas S. Die symptom-checkliste-90-R und ihre kurzversionen: psychometrische analysen bei patienten mit psychischen erkrankungen. Phys Rehab Kur Med. (2008) 18:337–43. doi: 10.1055/s-0028-1093323
30. Goodman W, Rasmussen S, Price L, Mazure L, Heninger G, Charney D. Yale-Brown obsessive compulsive scale (Y-BOCS). Verhaltenstherapie. (1991) 1:226–33. doi: 10.1159/000257973
31. Goodman WK, Price LH, Rasmussen SA, Mazure C, Delgado P, Heninger GR, et al. The Yale-Brown obsessive compulsive scale. II. Validity. Arch Gen Psychiatry. (1989) 46:1012–6. doi: 10.1001/archpsyc.1989.01810110054008
32. Taylor S. Assessment of obsessions and compulsions: reliability, validity, and sensitivity to treatment effects. Clin Psychol Rev. (1995) 15:261–96. doi: 10.1016/0272-7358(95)00015-H
33. Foa EB, Kozak MJ, Salkovskis PM, Coles ME, Amir N. The validation of a new obsessive-compulsive disorder scale: the obsessive-compulsive inventory. Psychol Assess. (1998) 10:206–14. doi: 10.1037/1040-3590.10.3.206
34. Gönner S, Leonhart R, Ecker W. Das zwangsinventar OCI-R—die deutsche version des obsessive-compulsive inventory-revised. Psychother Psych Med. (2007) 57:395–404. doi: 10.1055/s-2007-970894
35. Fairburn CG, Beglin SJ. Assessment of eating disorders: interview or self-report questionnaire? Intl J Eating Disorders. (1994) 16:363–70. doi: 10.1002/1098-108X(199412)16:4<363::AID-EAT2260160405>3.0.CO;2-%23
36. Mond JM, Hay PJ, Rodgers B, Owen C, Beumont PJV. Validity of the eating disorder examination questionnaire (EDE-Q) in screening for eating disorders in community samples. Behav Res Ther. (2004) 42:551–67. doi: 10.1016/S0005-7967(03)00161-X
37. Lichtenstein MB, Haastrup L, Johansen KK, Bindzus JB, Larsen PV, Støving RK, et al. Validation of the eating disorder examination questionnaire in danish eating disorder patients and athletes. JCM. (2021) 10:3976. doi: 10.3390/jcm10173976
38. Miller PR, Dasher R, Collins R, Griffiths P, Brown F. Inpatient diagnostic assessments: 1. Accuracy of structured vs. unstructured interviews. Psychiatry Res. (2001) 105:255–64. doi: 10.1016/S0165-1781(01)00317-1
39. Raykov T. Evaluation of convergent and discriminant validity with multitrait-multimethod correlations: convergent and discriminant validity. Br J Math Stat Psychol. (2011) 64:38–52. doi: 10.1348/000711009X478616
40. Campbell DT, Fiske DW. Convergent and discriminant validation by the multitrait-multimethod matrix. Psychol Bull. (1959) 56:81–105. doi: 10.1037/h0046016
41. Cohen J. Statistical power analysis for the behavioral sciences. 0 ed. New York: Routledge (2013). doi: 10.4324/9780203771587
42. Miller PR. Inpatient diagnostic assessments: 2. Interrater reliability and outcomes of structured vs. unstructured interviews. Psychiatry Res. (2001) 105:265–71. doi: 10.1016/S0165-1781(01)00318-3
43. Bolbeth A, Ziegler M, Fehm L. Störungsübergreifende fragebogendiagnostik in der psychotherapie: ein vergleich des brief symptom inventorys und des ICD-10 symptom rating. Psychother Psychosom Med Psychol. (2021) 71:202–8. doi: 10.1055/a-1264-0348
45. Gönner S, Leonhart R, Ecker W. The obsessive–compulsive inventory-revised (OCI-R): validation of the German version in a sample of patients with OCD, anxiety disorders, and depressive disorders. J Anxiety Disord. (2008) 22:734–49. doi: 10.1016/j.janxdis.2007.07.007
46. Wootton BM, Diefenbach GJ, Bragdon LB, Steketee G, Frost RO, Tolin DF. A contemporary psychometric evaluation of the obsessive compulsive inventory—revised (OCI-R). Psychol Assess. (2015) 27:874–82. doi: 10.1037/pas0000075
47. Piontek K, Shedden-Mora MC, Gladigau M, Kuby A, Löwe B. Diagnosis of somatoform disorders in primary care: diagnostic agreement, predictors, and comaprisons with depression and anxiety. BMC Psychiatry. (2018) 18:361. doi: 10.1186/s12888-018-1940-3
48. Meuret AE, Tunnell N, Roque A. Anxiety disorders and medical comorbidity: treatment implications. In: Kim Y-K, editors. Anxiety disorders. Advances in experimental medicine and biology. Singapore: Springer Singapore (2020). p. 237–61. doi: 10.1007/978-981-32-9705-0_15
49. ter Meulen WG, Draisma S, van Hemert AM, Schoevers RA, Kupka RW, Beekman ATF, et al. Depressive and anxiety disorders in concert–A synthesis of findings on comorbidity in the NESDA study. J Affect Disord. (2021) 284:85–97. doi: 10.1016/j.jad.2021.02.004
50. Bandelow B, Michaelis S. Epidemiology of anxiety disorders in the 21st century. Dialogues Clin Neurosci. (2015) 17:327–35. doi: 10.31887/DCNS.2015.17.3/bbandelow
51. Newman MG, Shin KE, Zuellig AR. Developmental risk factors in generalized anxiety disorder and panic disorder. J Affect Disord. (2016) 206:94–102. doi: 10.1016/j.jad.2016.07.008
52. Na K-S, Cho S-E, Cho S-J. Machine learning-based discrimination of panic disorder from other anxiety disorders. J Affect Disord. (2021) 278:1–4. doi: 10.1016/j.jad.2020.09.027
53. Hilbert A, Tuschen-Caffier B. Eating disorder examination. 2. Auflage. Tübingen: dgvt-Verlag (2016).
54. Calugi S, Milanese C, Sartirana M, El Ghoch M, Sartori F, Geccherle E, et al. The eating disorder examination questionnaire: reliability and validity of the Italian version. Eat Weight Disord. (2017) 22:509–14. doi: 10.1007/s40519-016-0276-6
55. Pedersen G, Urnes Ø, Kvarstein EH, Karterud S. The three factors of the psychoticism scale of SCL-90-R: factors of the psychoticism scale of SCL-90-R. Personal Ment Health. (2016) 10:244–55. doi: 10.1002/pmh.1278
56. Abramowitz JS, Deacon BJ. Psychometric properties and construct validity of the obsessive–compulsive inventory—revised: replication and extension with a clinical sample. J Anxiety Disord. (2006) 20:1016–35. doi: 10.1016/j.janxdis.2006.03.001
57. Tritt K, Heymann F, Zaudig M, Loew T, Söllner W, Fischer F, et al. Das ICD-10-symptom-rating (ISR): zusammenhänge mit der SCL-90-R. Klinische Diagnostik und Evaluation. (2010) 3:22–37.
Keywords: Klenico, ICD-10, multitrait-multimethod, validation, diagnostic procedures, construct validity, digital mental health
Citation: Reutimann S, Hübscher N, Steiner J, Voderholzer U and Augsburger M (2023) Assessing validity of the Klenico diagnostic software system in a large psychotherapeutic inpatient sample. Front. Digit. Health 5:1176130. doi: 10.3389/fdgth.2023.1176130
Received: 28 February 2023; Accepted: 31 July 2023;
Published: 24 August 2023.
Edited by:
Kwok Leung Tsui, Virginia Tech, United StatesReviewed by:
Michael Musker, University of South Australia, Australia© 2023 Reutimann, Hübscher, Steiner, Voderholzer and Augsburger. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Stefan Reutimann c3RlZmFuLnJldXRpbWFubkBrbGVuaWNvLmNvbQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.