- Department of Electrical and Systems Engineering, University of Pennsylvania, Philadelphia, PA, United States
Introduction: Certain behavioral practices, such as wearing masks, practicing social distancing, and accepting vaccines, play a crucial role in impeding the spread of COVID-19 and reducing the severity of symptoms. Opinions regarding whether to observe such behavioral practices evolve over time through interactions via networks that overlap with but are not identical to the physical interaction networks over which the disease progresses. This necessitates the joint study of the dynamics of COVID-19 and opinion evolution.
Methods: We develop a mathematical model that can be easily adapted to a wide range of behavioral practices and captures in a computationally tractable manner the joint evolution of the disease and relevant opinions in populations of large sizes. Populations of large sizes are typically heterogeneous in that they comprise individuals of different age groups, genders, races, and underlying health conditions. Such groups have different propensities to imbibe severe forms of the disease, different physical contact, and social interaction patterns and rates. These lead to different disease and opinion dynamics in them. Our model is designed to effectively capture such diversities.
Results: Computations using our model reveal that opinion dynamics have a strong impact on fatality and hospitalization counts and the number of man-days lost due to symptoms both in the regular form of the disease and the extended forms, more commonly known as long COVID. We show that opinion dynamics in certain groups have a disproportionate impact on the overall public health attributes because they have high physical interaction rates, even when they have the lowest propensity to imbibe severe forms of the disease. This identifies a social vulnerability that malactors can utilize to inflict heavy public health damages through opinion campaigns targeting specific segments. Once such vulnerabilities are identified, which we accomplish, adequate precautions may be designed to enhance resilience to such targeted attacks and better protect public health.
Discussion: By recognizing and understanding the vulnerabilities, appropriate precautions can be developed to enhance resilience against targeted attacks and safeguard public health. Our study underscores the importance of considering opinion evolution alongside disease dynamics, providing insights into the interplay between behavioral practices, opinions, and disease outcomes. We believe that our model is a valuable tool for understanding the joint dynamics of COVID-19 and opinions. We hope that our findings will help to inform public health policy and facilitate evidence-based decision-making for public health interventions.
1. Introduction
The novel coronavirus, COVID-19, was first detected in the United States in January 2020 (1). Most of the detected COVID-19 in the early days were from travelers returning from high-risk countries or their close contacts. Thereafter, widespread community transmission of the disease began to occur in Washington, New York, and California communities (2). On March 11, 2020, the World Health Organization (WHO) declared COVID-19 a pandemic (3). Since then, there have been approximately 97 million cases and 1.06 million fatalities in the United States (4).
Behavioral patterns heavily influence both the spread and evolution of COVID-19. For example, a large-scale randomized trial involving 350,000 people in 600 villages in Bangladesh has shown that the use of surgical masks impedes the spread of COVID-19 (5). Observing isolation when exposed or infected also impedes the spread. Vaccines reduce the severity of symptoms, including hospitalization and death, and also the spread rates (6). Opinions regarding whether to observe behavioral patterns conducive to containment of COVID-19 evolve over time through social exchanges via networks that overlap with but are not identical to the COVID-19 propagation networks. Thus, the biological and information contagion spread simultaneously and necessitate a joint investigation of the two phenomena. The joint investigation is yet to be studied for COVID-19, despite enormous progress in research on COVID-19 in the last 3 years. However, certain distinguishing characteristics of COVID-19 necessitate an investigation of the joint spread focusing on COVID-19.
Several behavioral patterns, such as willingness to wear surgical masks and observing social distance, affect the spread of COVID-19. Next, whether an individual is vaccinated affects the severity of symptoms in infected individuals (7,8). Furthermore, the severity of COVID-19 symptoms and fatality rates depend on age (9–11), underlying health conditions (obesity, cancer, heart conditions, chronic liver disease, chronic lung disease, chronic kidney disease, HIV infection, etc.) (12, 13), race (14), and gender of individuals (15), while propensity to spread COVID-19 depends on the contact patterns of individuals. More specifically, old individuals and those with certain underlying diseases, hitherto referred to as comorbidity, are at greater risk to develop a severe form of the disease and even die from it; the risk factor is higher for males and for certain ethnic groups. However, old individuals are also least likely to spread the disease because their contact rates are limited (16). Young individuals who are in good health usually have high contact rates among themselves, and also with other groups, and are therefore more likely to spread the disease. Nevertheless, they are also least likely to develop a severe form of the disease. Given this divergence between groups who are at greater risk from the disease and who are most likely to spread it, there may also be a divergence between opinions regarding the behavioral patterns between them. That is, given that their risk factors for developing a severe form of the disease are lower, young and healthy individuals may more easily subscribe to opinions that undervalue behavioral patterns that are conducive to the containment of the disease. Opinion spread rates can be different in different groups too. For example, young individuals may be more active on social media and may therefore circulate their opinions faster than others. The groups are often clustered in that the contact rates (both proximity and social contacts) are often higher within groups than across groups. For example, residential neighborhoods and social circles are often racially segregated (17)—according to a poll conducted in 2013 by Reuters/Ipsos, about 40% of White Americans and about 25% of non-White Americans are surrounded exclusively by friends of their own race (18). Thus, the joint disease and opinion spread need to be studied considering different forms of behavioral patterns that affect the spread and different types and rates of information and disease spread based on age, underlying health conditions, gender, race, etc. Note that the divergences in question need not be as pronounced for other infectious diseases as COVID-19.
The emergence of a new infectious disease always opens up the possibility of a new bioterrorist attack that utilizes the respective contagion. It is possible to create synthetic strains of COVID-19 that are more virulent and has higher transmissibility than the existing strains through gain-of-function (GOF) research. One such strain has already been created by a group of researchers at Boston University (BU) by combining two features of different existing COVID-19 strains (19). GOF research may help researchers better understand the evolving pathogenic landscape, pandemic response, treatment, and countermeasures and develop new technologies, but may lead to synthetic variants that can be leaked accidentally or deliberately as part of a bioterrorist attack. In the event of the latter, opinions may be manipulated to induce behaviors conducive to the spread of the disease. The divergence between groups that are at the greatest risk and can spread the most facilitates such behavior manipulation through opinion spread. For example, simultaneously with the deliberate seeding of synthetic strains in the populace, behavior conducive to the spread may be promoted among young individuals citing their low risk of the disease. Due to connection across age groups, the disease may spread to old and at-risk individuals leading to high casualty. Thus, the characteristics of COVID-19 may be exploited to launch lethal attacks through the spread of opinions along with the spread of disease. The potential of malevolent actors to inflict damage by exploiting the above characteristics needs to be investigated.
In this paper, we develop a computationally tractable mathematical model that jointly captures the evolution of a COVID-19 outbreak and the evolution of opinion pertaining to behavioral patterns pertinent to the spread and severity of the disease. The model captures (1) the distinguishing characteristics of COVID-19, namely, different risk factors and contact patterns of different sections of the populace classified through age, underlying health conditions (comorbidity), race, and gender; (2) different opinion dynamics and rates of spreads of opinions within these groups and across the groups. The model is flexible enough to capture the dynamics of different kinds of behavior, namely, wearing surgical masks and receiving vaccines. We consider the reality that in the age of social media, opinions regarding behavioral dynamics rapidly evolve, through social networks that overlap with but are not identical to biological networks. In particular, during physical interactions, both disease and opinions may spread, whereas only opinions may spread through remote (e.g., electronic) interactions, and only the disease might spread when individuals share the same physical space (e.g., public spaces like beaches, parks, public transports) without engaging in social interactions. We consider the long-term effects of COVID-19 infection, otherwise known as long COVID or post-COVID conditions (PCC). As per WHO, long COVID occurs when coronavirus symptoms persist or return 3 months after an individual develops symptoms, and the symptoms last for at least 2 months and cannot be explained by an alternative diagnosis (20). Common symptoms of PCC include fatigue, shortness of breath, and cognitive dysfunction. According to the CDC, unvaccinated individuals who get infected with COVID-19 might be at higher risk of developing long COVID compared to people who get infected after receiving the vaccine (21). Thus, PCC is correlated with behavioral choice and therefore opinion dynamics. The model captures the essence of stochastic evolution, but retains computational tractability, in that it easily scales to typical target population sizes for infectious diseases encompassing millions of individuals. We utilize the model to quantify the impact of the opinion dynamics on metrics that capture the overall health of the system such as the total number of fatalities, hospitalization, and the number of days the populace suffers from symptoms. This provides a quantitative foundation for public health discourse pertaining to the relationship between disease and opinion spreads that have only been conducted in the qualitative sphere for COVID-19 thus far. The quantifications confirm several commonplace intuitions and go beyond by unearthing the exact nature of the dependence of the above public health metrics on several key parameters. Our work helps identify how potential bioterrorist attacks can strategically exploit the specific characteristics of COVID-19 to undermine public health.
2. Materials and methods
In this section, we progressively describe the dynamics of COVID-19 progression and spread (Section 2.1), the spread of opinions pertaining to different behavioral patterns that affect the severity of symptoms and the rate of spread (Section 2.2), state transitions in the joint spread of disease and opinions (Section 2.3), and a mathematical formulation that captures the dynamics of the joint spread (Section 2.4).
2.1. Dynamics of the infectious disease
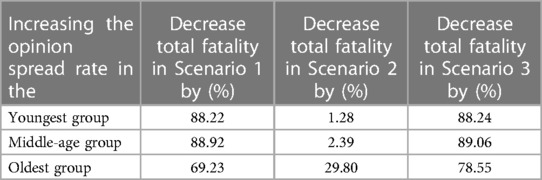
SARS-CoV-2 propagates through spatial proximity. When a susceptible individual, , gets in spatial proximity of an infected individual, , the former contracts the disease with a certain probability and becomes exposed. We denote the exposed stage by . The virus incubates and grows during the exposed stage but the exposed individual neither shows any symptoms nor is contagious. From the exposed stage, an individual either becomes presymptomatic, stage denoted by , or asymptomatic, stage denoted by . During both stages, the individual does not show symptoms but is infectious, though he may transmit the disease with different probabilities. From the former stage, he moves on to show symptoms while from the latter stage, he directly recovers without ever showing symptoms. If he shows symptoms, he transitions into the symptomatic stage after which he either recovers or is hospitalized. When he is hospitalized, he cannot transmit the infection further because he is under quarantine. A hospitalized individual, stage , can recover, stage , or die, stage . We assumed that an individual who recovers from COVID-19 does not get reinfected. Refer to Figure 1 for a pictorial illustration of the different stages of the disease.
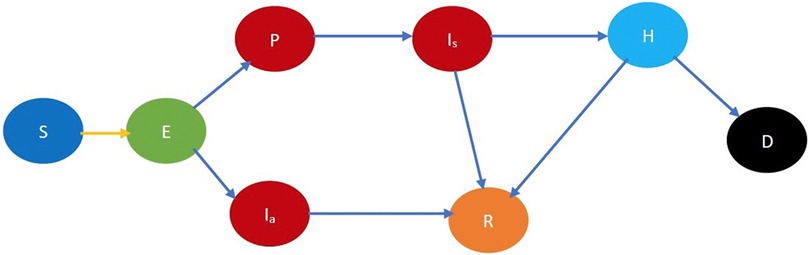
Figure 1. Fundamental COVID-19 state diagram. The states in blue color are the susceptibles (not yet infected but they are prone to infection) while those in light green color are exposed (still in the incubation period, hence they are not infectious). The states in dark red are infected and therefore infectious while those in gold have recovered, those in light blue are hospitalized, and black denotes dead. In addition, the yellow arrow shows susceptibles transitioning to the exposed state after contracting the virus. The blue arrows indicate the natural progression of the disease.
One of the distinguishing characteristics of COVID-19 is that different segments of the populace exhibit a substantially different propensity to severe forms of COVID-19, and death when they imbibe it. First, once infected, older adults are more likely to need hospitalization, intensive care admission, or a ventilator to help them breathe (10). Older patients also have a higher fatality rate (11). Next, male patients are more at risk for worse outcomes and death (15). Also, in the United States once infected, African Americans have higher duration of hospital stays, as compared to White people (14). Finally, risks for a severe form of the disease are substantially higher when patients have certain underlying health conditions. These underlying conditions include obesity [body mass index, i.e., a person’s weight in kilograms divided by the square of height in meters, over 30 is considered obese (22)], cancer treatment, HIV/AIDS positive, heart and lung disease, diabetes, etc. (12). Risks increase manifold for comorbid patients, i.e., those who suffer from two or more conditions.
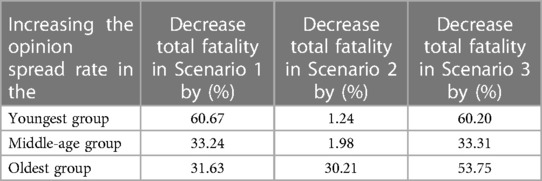
To model different risk factors for different sections of the population, we will classify individuals in different stages of COVID-19 further according to their age, gender, race, and underlying health conditions. Specifically, we classify individuals into three different age groups: (i) youngest group—for individuals who are in the age range of 0–24 years; (ii) middle-age group—for individuals who are 25–49 years old; (iii) oldest group—for those who are 50 years and above. We classify individuals into male and female; African American, Hispanic, and White; and healthy and immunocompromised. Individuals who do not have any underlying health conditions that accentuate the risk of imbibing a severe form of COVID-19 are classified as healthy, the rest are immunocompromised. For simplicity, we have considered the races which together constitute of the population of the Commonwealth state of Pennsylvania, United States. Table 5 in the Supplementary material shows the demographic characteristics of Pennsylvania with respect to age and race (23).
Refer to Figure 2 for a pictorial illustration of the evolution when only age-based classification is resorted to. Note how the state evolution shown in Figure 1 is being replicated due to age-based classification. Consideration of further classification based on gender, race, and underlying health replicates the state evolution shown in Figure 2 further. We consider this further classification in the mathematical formulation but not in the pictorial representation owing to the large number of states introduced due to the full-fledged classification.
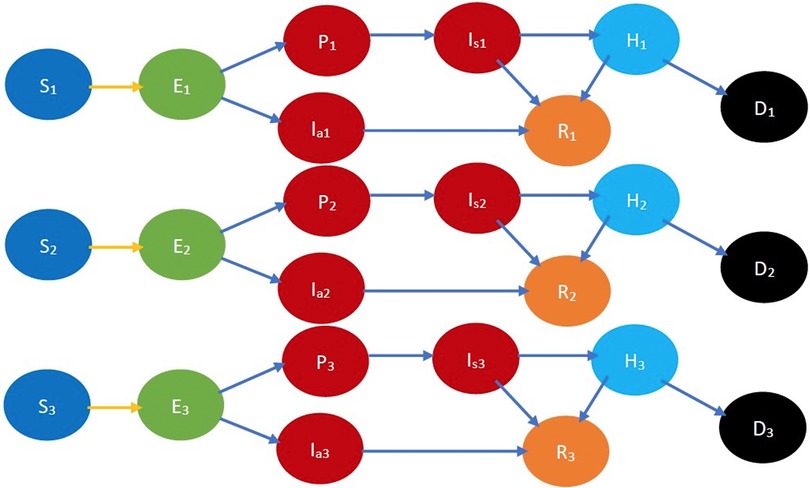
Figure 2. COVID-19 state diagram divided into various age groups. The subscripts 1, 2, and represent the youngest group, middle-age group, and oldest group, respectively. Every state and transition has the same meaning as described in the caption forand Figure 1. Note that there is no transition between states indexed 1, 2, and 3, e.g., between , , and , as we do not consider transitions between age groups in the time frame under consideration.
Different sections exhibit different contact rates and patterns, both within and across sections. For example, in many parts of the United States, neighborhoods are racially segregated, through living preferences and economic conditions. Accordingly, people of different races also largely attend different schools, and utilize different services and shops (17). According to a poll conducted in 2013 by Reuters/Ipsos, about 40% of White Americans and about 25% of non-White Americans befriend exclusively from their own race (18). Thus, contact rates across the categories we considered in the previous paragraph are lower than those within the same category. Finally, contact rates also depend on age. Specifically, older people have less social contact than younger people, and other things being equal, higher age is correlated with a lesser amount of time spent with others (16). Different contact rates and patterns can be incorporated by classifying individuals based both on the stage of the disease and age, gender, race, overall health, etc.
2.2. Opinion dynamics
We now describe how we characterize the opinion dynamics leading to a characterization of the joint evolution of COVID-19 and opinions.
An individual is cooperative if he follows the behavioral practices that reduce (1) the probability of the spread of COVID-19 in the event of spatial proximity between an infectious and a susceptible individual; (2) the severity of symptoms if he imbibes the disease. Such behavioral practices include some or all of the following: maintaining appropriate physical distancing, wearing appropriate protective gear, getting vaccinated, frequent hand washing, etc. A non-cooperative individual does not observe these norms. Thus, an individual ought to be classified as cooperative or non-cooperative, in addition to his stage of the disease, age, gender, race, and overall health. For example, in the classified COVID-19 state diagram (Figure 3), and , respectively, denote cooperative and non-cooperative susceptible individuals. This additional classification enables the modeling of the joint evolution of the disease and opinions. Refer to Supplementary Table 3 for all the notations.
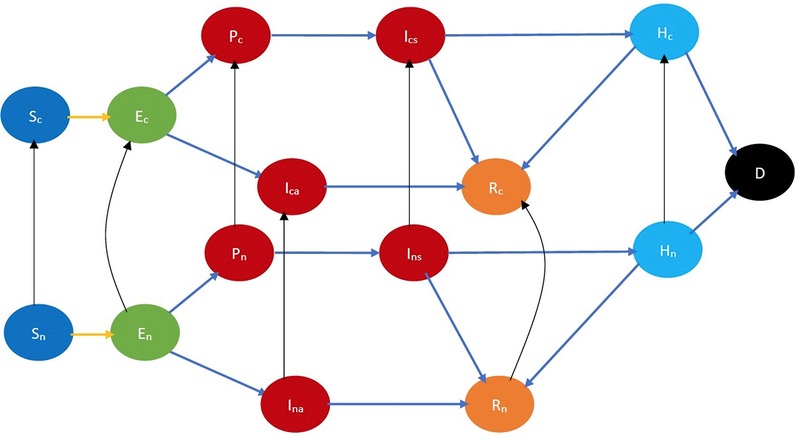
Figure 3. COVID-19 state diagram incorporating cooperativity. The black arrows indicate opinion evolution. The subscripts and , respectively, denote cooperative and non-cooperative individuals. Thus, the black arrow from to represents the conversion of a susceptible non-cooperative to a susceptible cooperative, i.e., evolution of opinion of a susceptible. Every state and transition has the same meaning as described in the caption for Figure 1.
Opinions pertaining to the observance of the above behavioral practices evolve through the influence of social contacts and through exposure to independently accessible information such as reading material, TV, radio, billboards, Internet advertisements, etc. We consider that a cooperative converts a non-cooperative to become a cooperative with a certain probability during an exchange of ideas between the duo. Such exchanges may happen in person or remotely. A non-cooperative may also be converted by reading about what reduces the spread of the disease or by watching or hearing public awareness programs on TV, radio, billboards, social media, etc. The conversion may happen during any stage of the disease. We assume that when an individual is hospitalized, he is quarantined, then he does not convert anyone or is converted by anyone but may be converted by exposure to public awareness campaigns (which may have a stronger impact because the individual might be infected and he experiences the symptoms acutely). Our default assumption is that the non-cooperatives change their opinions, but we later generalize the model to incorporate change of opinions in the reverse direction as well.
Refer to Figure 3 for a pictorial illustration of the evolution when only cooperativity-based classification is resorted to. Note how the state evolution shown in Figure 1 is being replicated due to the cooperativity-based classification. Figure 4 shows classification based on both age and cooperativity. Further classification based on age, gender, race, and underlying health, which we consider in the mathematical formulation, replicates the state evolution shown in Figure 3 further. The fundamental difference between classifications based on cooperativity and those based on age, gender, race, and underlying health is that an individual can transition from cooperative to non-cooperative or vice versa but does not transition across the other attributes in the time frame we consider. Thus, in Figure 2, there is no transition between , , and , but in Figure 3, there is a transition from to .
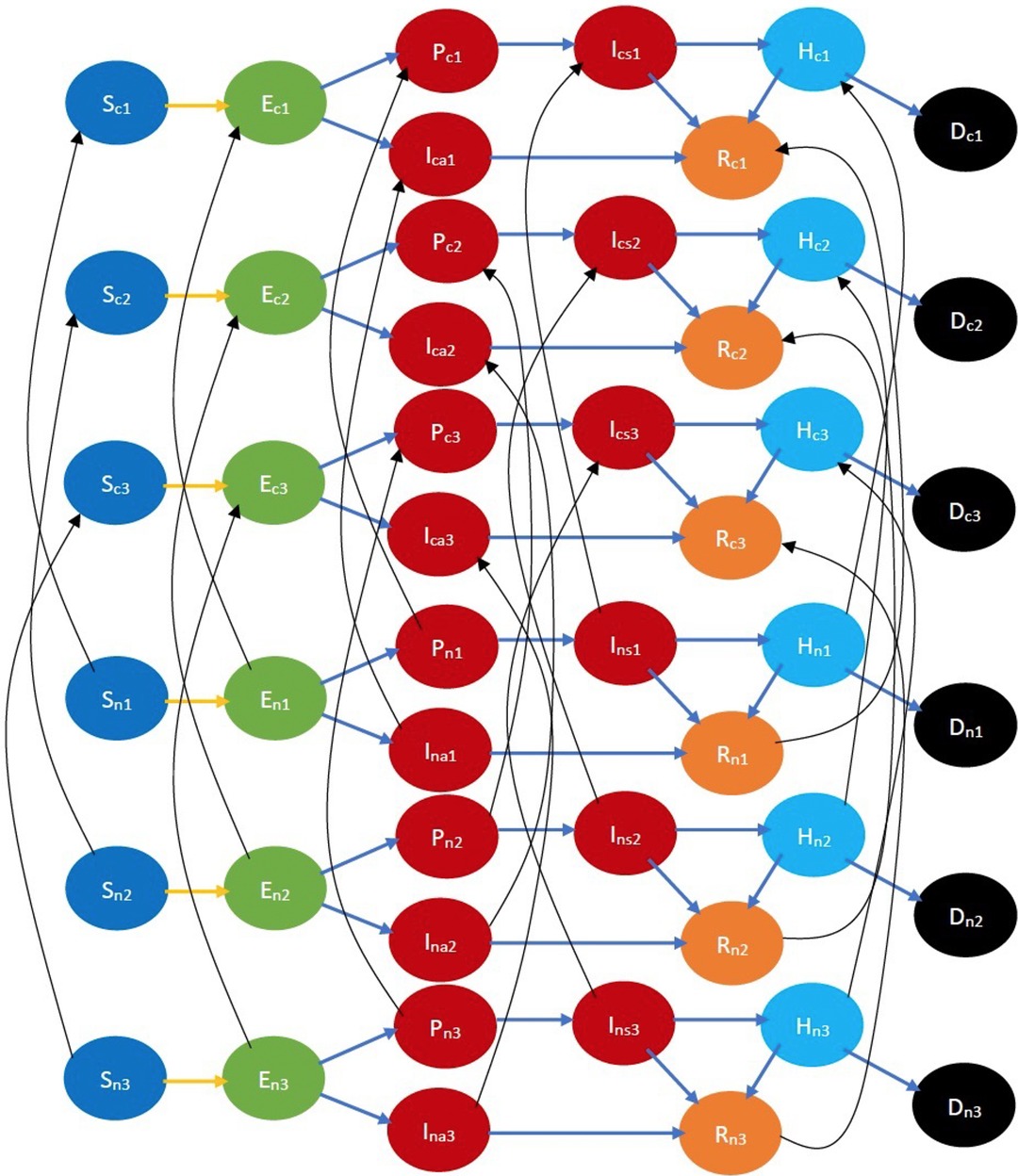
Figure 4. COVID-19 state diagram classified by ages and cooperativities. The subscripts and , respectively, denote cooperative and non-cooperative individuals. Similarly, subscripts , , and represent the youngest group, the middle-age group, and the oldest group, respectively. Note that there is no transition across age groups, but there is a transition across opinion groups, e.g., there is a transition from to , but no transition between or . Every state and transition has the same meaning as described in the caption for Figure 1.
We have considered different behavioral practices pertaining to the evolution of COVID-19, namely, maintaining appropriate physical distancing, wearing appropriate protective gear, frequent hand washing, getting vaccinated, etc. All except the last reduce the probability of spread of the disease from an infectious individual to a susceptible, while the last reduces the severity of symptoms, probability of hospitalization, and death once the disease is imbibed (though the last may also reduce the probability of transmission of the disease from the infectious to the susceptible). We now illustrate how minor adaptations of the model can help cater to these distinctions in the impact of different behavioral precautions. We first consider the behavioral practices that only reduce the spread. When cooperativity is used to denote observance of these, we assume that when an infectious individual is in physical proximity of a susceptible one, the probability of the spread of the disease from the infectious to the susceptible is higher if both are non-cooperatives than if both are cooperatives. If only one is non-cooperative, the probability of the spread is somewhere in-between (the in-between can also equal one of the two ends, i.e., the probability when both are cooperative and when both are non-cooperative). We now consider the behavioral practice to be vaccinated, i.e., a cooperative is willing to be vaccinated while a non-cooperative is not. We assume that vaccines are available as soon as one is willing, which is currently the case in most of the United States and Europe. Thus, considering that the vaccine in question requires only one dose, as soon as an individual becomes cooperative, he is vaccinated. Then, we incorporate the impact of vaccination by considering that a cooperative has a lower probability of developing symptoms, a lower probability of needing hospitalization even when he develops symptoms (i.e., the symptoms are mostly mild), and a lower probability of dying even when hospitalized. We can simultaneously consider that cooperatives spread the disease with a lower probability, as described above if vaccines also lower the probability of the spread. Our default assumption is that the vaccine needs only one dose, though we describe in Section 4 how our model can be generalized to incorporate vaccines that need multiple doses.
The model can incorporate different opinion dynamics and interactions involving exchange of ideas in different sections of the populace based on age, gender, race, and health conditions, by considering different rates of conversion of opinions in different groups representing the above classifications.
2.3. State transitions in the joint evolution of disease and opinions
There are two kinds of transitions in joint evolution: (1) interactional and (2) non-interactional. Interactional transitions happen when a susceptible imbibes the disease from an infectious individual or a cooperative converts a non-cooperative. Thus, during interactional transition, both disease and opinions may spread from one individual to another. The natural progression of the disease in the infected individuals and conversion of opinion due to access to information in reading material or mass awareness campaigns constitute non-interactional transitions.
We now provide a taxonomy of the interactional transitions [which is similar to that in (24)]. Interaction between individuals can be classified as (i) physical interactions with an exchange of opinion and biological contagion (e.g., friends and acquaintances visiting homes of each other, etc.); (ii) physical interactions without any exchange of ideas (e.g., people commuting on a train, bus, etc.); (iii) virtual interactions with an exchange of ideas (e.g., telehealth, counseling over the phone or Internet, etc.). Whereas the first case can cause infection and a change in opinion, the second case can only cause infection, while the third case can only cause a change of opinion.
2.4. The clustered epidemiological differential equation model
A joint investigation of infectious disease and opinion dynamics naturally leads to a computationally complex model involving (1) a multiplicity of states representing a combination of stages of the disease, gender, age group, race, health condition, and cooperativity; and (2) a multiplicity of state transitions representing interactional transitions due to spread of the disease and opinions, as well as non-interactional transitions due to the natural progression of the disease in the infected individuals and alteration of opinions due to exposure to public awareness campaigns. Following our recent work on modeling the joint spread of Smallpox and vaccine hesitancy (24), we model these attributes by adapting the metapopulation epidemiological model (25, 26) which relies on a set of differential equations. We describe the adaptations in the Supplementary material and refer to the resulting model as clustered epidemiological differential equations or the CEDE, given that each state is decomposed into groups or clusters. In general, estimating the spread of infectious diseases is computationally challenging because it involves millions of individuals in population sizes one needs to consider. Metapopulation models alleviate this challenge by relying on differential equations, which can be solved using readily available and computationally efficient numerical techniques. The differential equations capture the evolution of states of different fractions of the total population. Thus, the computational time does not increase with the increase in the size of the populace (24).
Each variable in the CEDE represents the fraction of the population who are in a particular system state. Meanwhile, each state represents the combination of the stage of the disease, age group, gender, health conditions, and cooperativity of an individual. Each differential equation captures the evolution of a particular variable. Thus, the solution of the CEDE provides the fraction of individuals in different states at given times. In other words, the solutions of the differential equation provide the distribution of the disease and opinion spread across groups and time. The terms in the CEDE are either linear or quadratic. The quadratic terms represent the interactional transitions (refer to the yellow and black arrows in Figure 3) and the linear terms represent the non-interactional transitions (refer to the blue arrows in Figure 3). This distinction arises because interactions always involve two individuals, while non-interactional transitions involve only one individual. This arises in all epidemiological models starting from the classical Kermack–McKendrick formulation (27) and onward to the metapopulation models (24–26, 28, 29). But our work differs from the metapopulation epidemiological models because it captures two different evolving contact processes spreading simultaneously (disease, opinion), whose overlap is only partial (only certain interactions spread both the disease and opinion, while others can only spread one of the two). The spread of the two processes involves two broad categories of interactional transitions: (1) susceptible to exposed state; (2) non-cooperative to cooperative and vice versa. Metapopulation models typically capture only one evolving process, namely, the disease, spreading through physical proximity and therefore need only the first kind of interactional transitions. Since interactional transitions are represented by quadratic terms, the second kind produces additional quadratic terms in our model.
We now provide more details on the computation time of the CEDE. Let there be variables and thus differential equations. The computation time depends only on and increases linearly with it. For instance, with three age groups, two genders, three races, cooperative–non-cooperative, healthy–immunocompromised classifications, . And, regardless of the population size, the average computation time to obtain one data point is approximately min using MATLAB 2022a and Macbook Pro 2.9 GHz Dual-Core Intel Core i5 Processor with 8 GB Memory Laptop.
A question that arises for the CEDE is that it is a deterministic model, while many of the state transitions are stochastic. We resolved this dilemma in our earlier work (24) through an application of a classical result of probability theory. Under some commonly made assumptions on the stochastic evolutions, we have shown that as the number of individuals increases, the fractions of individuals in different system states in the stochastic system converge to the solutions of the CEDE, and the convergence becomes exact in the limit that the number of individuals is infinity (24). Thus, the CEDE approximates the stochastic process better with an increase in the number of individuals. The convergence guarantee holds when the stochastic evolutions are Markov, that is, the amount of time an individual spends in each system state is exponentially distributed, which is what we assume to estimate the parameters of the system (Supplementary material). Note that such Markovian assumptions are commonplace in modeling the spread of infectious diseases [e.g., as noted in Chapter 2, p. 28, (30)].
Our CEDE model is naturally flexible in that it can accommodate opinion dynamics, different behavioral practices, arbitrary age groups, gender, health conditions, and countermeasure application strategies. The CEDE remains computationally tractable and provides an analytical convergence guarantee while providing the above modeling flexibility.
3. Results
We utilized our COVID-19 model to investigate the impact of opinion dynamics on various public health attributes such as fatalities, number of man-days lost because of symptoms, hospitalizations, etc. We consider three different scenarios: (1) cooperatives observe behavioral practices (e.g., wearing surgical masks, observing social distancing, hygiene such as repeated hand washing) that reduce the spread of the biological contagion (Scenario 1, Section 3.2); (2) cooperatives take vaccines which reduce the severity of symptoms (Scenario 2, Section 3.3); (3) cooperatives observe both healthy behavioral practices and take vaccines (Scenario 3, Section 3.4). Recall that consistent with reported statistics, we have assumed that vaccines only reduce the severity of symptoms. Thus, in Scenario 1, cooperatives only impede the spread, while in Scenario 2, they only have a lower propensity of severe symptoms, and in Scenario 3 they impede the spread and have a lower propensity of severe symptoms (5–8). The first scenario corresponds to the case in which vaccines are not available because then no one (i.e., neither cooperatives nor non-cooperatives) accepted vaccines. The second and third scenarios correspond to the phase in which vaccines are available. When we consider the second and third scenarios, we start from an initial distribution of cooperatives, which correspond to the people who had become willing to accept vaccines at the start of the availability of vaccines. The willingness may be attributed to trust in the public health system, fear and panic about the pandemic, etc. In the first and third scenarios, our default assumption is that cooperative susceptible (respectively cooperative infectious) individuals are infected (respectively infect) during physical proximity with an infectious (respectively susceptible) individual at a rate that is half that of a non-cooperative individual. We also deviate from the default assumption and consider the scenario in which when a susceptible is in physical proximity of an infectious and (1) both are cooperatives, the disease transmits at the lowest rate; (2) only one is a cooperative, the disease transmits at an intermediate rate; and (3) both are non-cooperatives, the disease transmits at the highest rate. We consider that the lowest and the intermediate are respectively and of the highest rate. We denote this scenario as second-transmission-rate-scenario. We consider different durations for COVID-19 symptoms: (1) regular durations in which symptoms do not exist after an individual recovers; (2) long COVID in which symptoms last for months after recovery (we consider 2 months in this case). We consider different fatality and hospitalization rates, ranging from those seen in natural variants (default choice) to extremely high values which have been reported for synthetic variants. As to opinion dynamics, we consider that cooperatives convert non-cooperatives during information exchange (default), but we also consider the scenario whereby non-cooperatives convert cooperatives.
We start with a sanity check in which we show that several commonly used variables such as the number of infected, hospitalized, and recovered individuals vary with time in an expected manner (Section 3.1). This suggests that the model is functioning as per expectations and instills confidence in the results that the model yields. We subsequently report our findings for the above-mentioned variations in Sections 3.2–3.4. In all the variations, we observe that opinion exchange between cooperatives and non-cooperatives has a significant effect on the public health attributes we consider. Specifically, information exchange among the younger population has a disproportionate impact on public health attributes, though statistically speaking the symptoms are the mildest among them. The disproportionate impact arises because the younger section is in physical proximity to each other and with the rest of the society more often than other age groups, because of their naturally active lifestyle. Unless otherwise mentioned, all parameters are at their default values specified in Section II in the Supplementary material. Figures 16–20 are supplementary figures in the Supplementary material.
3.1. Sanity check
We plot the number of infected, hospitalized, and recovered individuals as a function of time (Scenario 1, Supplementary Figure 16; Scenario 2, Supplementary Figure 17; Scenario 3, Figure 5). We plot these attributes separately for the youngest and the oldest age groups we considered. As expected, the first two increase with time initially and then decrease, as individuals either recover or die. The number of recovered individuals initially increases with time and finally saturates as the system reaches a steady state in which all individuals have either recovered or died. Finally, as expected, more individuals in the youngest group are infected per day than individuals in the oldest group (Supplementary Figures 16A, 17A, and Figure 5A). This is because younger individuals are more often in physical proximity with others than those in the oldest group. As expected, the number of hospitalized individuals is higher for the oldest group because the hospitalization rate increases with age (Supplementary Figures 16B, 17B, and Figure 5B). The number of recovered individuals is higher for the youngest group because the fatality rate is lowest for them and in the steady state an individual is either dead or recovered (Supplementary Figures 16C, 17C, 5C). The number of infected and hospitalized are the least and the number of recovered is the maximum in Scenario 3, intermediate in Scenario 1, and respectively the maximum and the minimum in Scenario 2 (Figures 16, 17, and Figure 5). This is because the cooperatives observe all the desirable behavioral practices in Scenario 3 and different subsets of behavioral practices in the other two scenarios. A comparison between Scenarios 1 and 2 suggests that impeding the spread is more effective than reducing the severity of symptoms for all public health attributes (Figures 16 and 17).
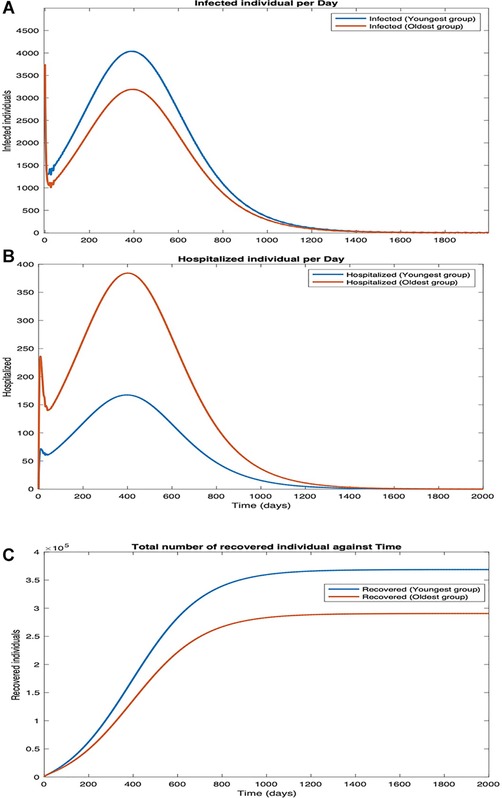
Figure 5. Scenario 3. Plots in the time domain for sanity check. (A) Infection per day, (B) hospitalization per day, and (C) number of recovered individuals.
3.2. Impact of opinion dynamics when behavioral practices affect spread of COVID-19: scenario 1
3.2.1. The default scenario
We consider that cooperatives observe behavioral practices that reduce the spread of biological contagion, while non-cooperatives do not observe such practices. Also, no individual takes vaccines. In Figure 6, we plot the overall fatality and hospitalization counts against the opinion spread rate for different values of the fraction of individuals who are cooperative initially. As cooperatives exchange opinions with non-cooperatives, the latter is converted. In general, the conversion happens faster as the rate of exchange of opinions, i.e., the opinion spread rate, increases. The conversion does not happen if all individuals are cooperatives or non-cooperatives initially. Thus, the number of deaths does not change with the opinion spread rate when the initial cooperativity is either 0 or 1. The fatality counts, however, decrease rapidly with an increase in opinion spread rates for initial cooperativities between 0 and 1. For instance, for an initial cooperativity of , , , and , the number of deaths decreases by , , , and , respectively, as the opinion spread rate increases from through . Similarly, the number of hospitalized individuals decreases by , , , and respectively as the opinion spread rate increases from through . The percentage decrease in fatality and hospitalization counts show that opinion dynamics have a strong impact on these public health attributes; the impact is strongest when the initial cooperativity values are moderate to low as then there are more non-cooperatives to convert with an increase in opinion exchange rates. The variations of the fatality and hospitalization counts against the opinion spread rate follow similar patterns.
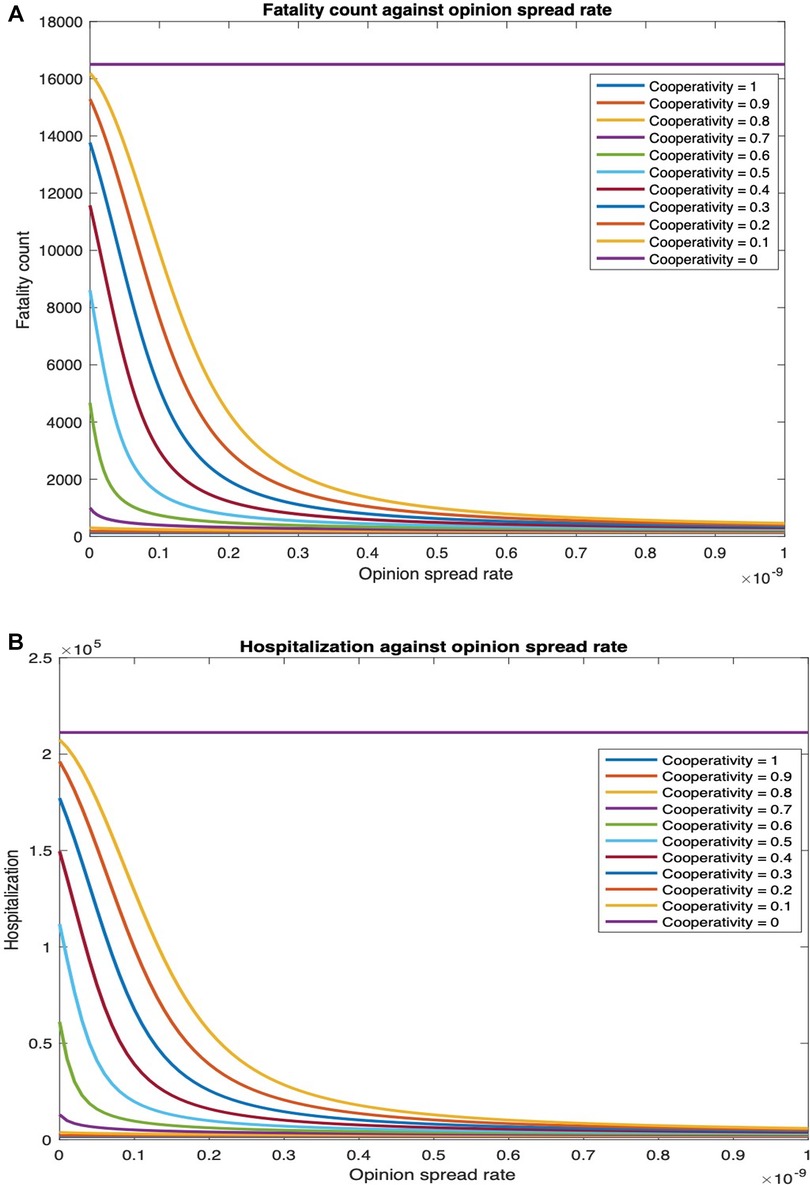
Figure 6. Fatality and hospitalization counts against opinion spread rate for various initial cooperativities. (A) Fatalities count against opinion spread rate for various initial cooperativities. (B) Hospitalization count against opinion spread rate for various initial cooperativities.
We next examine how fatality and hospitalization counts are affected if only the opinion exchange rate in one age group is increased and also if there is any difference depending on which age group that is. We examine this for two different values of physical contact rates among the youngest population: the default value () and thrice the default value (). For , the fatality count in all, youngest, middle-age, and oldest groups, respectively, decrease by , , , and as the opinion spread rate of the youngest group increases from through (Figure 7A). Also, the hospitalization count in all, youngest, middle-age, and oldest groups, respectively, decreased by , , , and (Supplementary Figure 18A). For , the number of deaths in all, youngest, middle age, and oldest groups will respectively decrease by , , , and . Similarly, hospitalization count in all, youngest, middle-age, and oldest groups will, respectively, decrease by , , , and . Thus, an increase in the rate at which individuals physically interact reduces the percentage decrease in fatalities and hospitalization and thereby the efficacy of the opinion exchange. Note that the fatality and hospitalization counts for the oldest group are significantly affected by the opinion exchange within the youngest group. We now examine the impact of opinion exchange within the oldest group (Figure 7B). For , fatality count for all, youngest, middle-age, and oldest groups decrease by , , , and respectively, as the opinion spread rate of the oldest group increases from through . Also, the hospitalization count for all, youngest, middle-age, and oldest groups will, respectively, decrease by , , , and . Next, for , the fatality count for all, youngest, middle-age, and oldest groups will, respectively, decrease by , , , and . Similarly, the hospitalization count for all, youngest, middle-age, and oldest groups will, respectively, decrease by , , , and . Thus, in all cases, the fatality and hospitalization counts decrease more when the opinion exchange rates are enhanced in the youngest group than when they are enhanced in the oldest group. Thus, converting younger individuals to cooperatives decreases fatality and hospitalization counts more across all age groups. That is, the behavioral practices of the youngest group impact the whole population more than those of the others. As expected, simultaneously converting opinions across all age groups have the most impact. For instance, for the fatality count for all, youngest, middle-age, and oldest groups, respectively, decreased by , , and as the opinion spread rate increases from through (Figure 7C). Also, the hospitalization count for all, youngest, middle-age, and oldest groups, respectively, decreased by , , and . Similarly, for , the number of deaths for all, youngest, middle-age, and oldest groups, respectively, decreases by , , and . Also, the hospitalization count for all, youngest, middle-age, and oldest groups, respectively, decreased by , , and . We do not present separate plots for overall fatality counts as the numbers can be obtained by adding the fatality counts in the three age groups; we just provide the numbers in the text. Yet again, we observe from Figure 7 and Supplementary Figure 18 that the variation of hospitalization and fatality follows the same pattern. We, therefore, omit the plots for the latter subsequently.
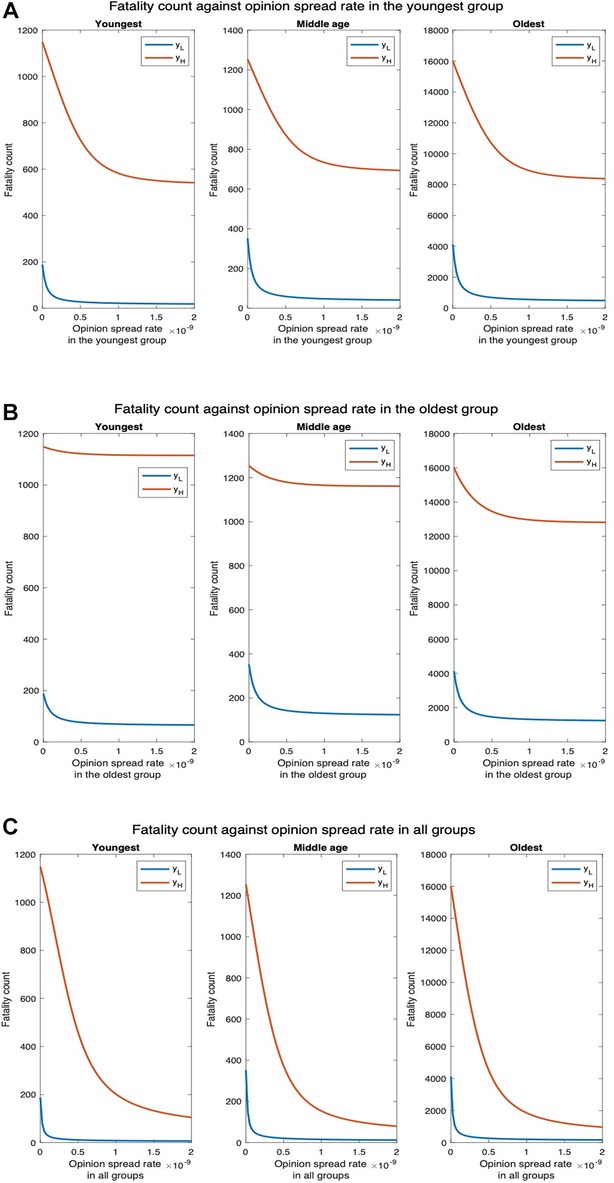
Figure 7. Fatality count for various interaction rates of the youngest group. denotes the default interaction rates of the youngest group while represents when the youngest group’s interaction rates are tripled (other groups’ interaction rates remain the same). (A) Opinion spread rate varied for the youngest group. (B) Opinion spread rate varied for the oldest group. (C) Opinion spread rate varied for all the groups.
To understand why the opinion exchange rate in the youngest group has the greatest impact on the fatality rates, we plot the fatality vs. the opinion spread rate when the physical interaction rates are the same in the youngest and the oldest groups. This would clearly not arise in practice but has been selected so as to understand the reason underlying the phenomenon reported in the previous paragraph. We observe that the number of deaths for all, youngest, middle-age, and oldest groups, respectively, decrease by , , , and as the opinion spread in the youngest group is increased from to (Figure 8A). Similarly, the number of hospitalized in all, youngest, middle-age, and oldest groups, respectively, decrease by , , and as the opinion spread in the oldest group is increased in the same range (Figure 8B). The numbers are now in the same ballpark; if at all now fatalities decrease more by converting a greater number of cooperatives in the oldest group because death rates are higher here (the oldest group has a high-risk factor). Thus, in the scenarios that arise in practice, the impact of the opinion spread in the youngest age group is the most because the physical interaction rate in this group is the highest. Consequently, disease spreads in this group at the highest rate and this group spreads the disease to other groups. Thus, converting individuals in this group to cooperatives in effect contains the carriers.
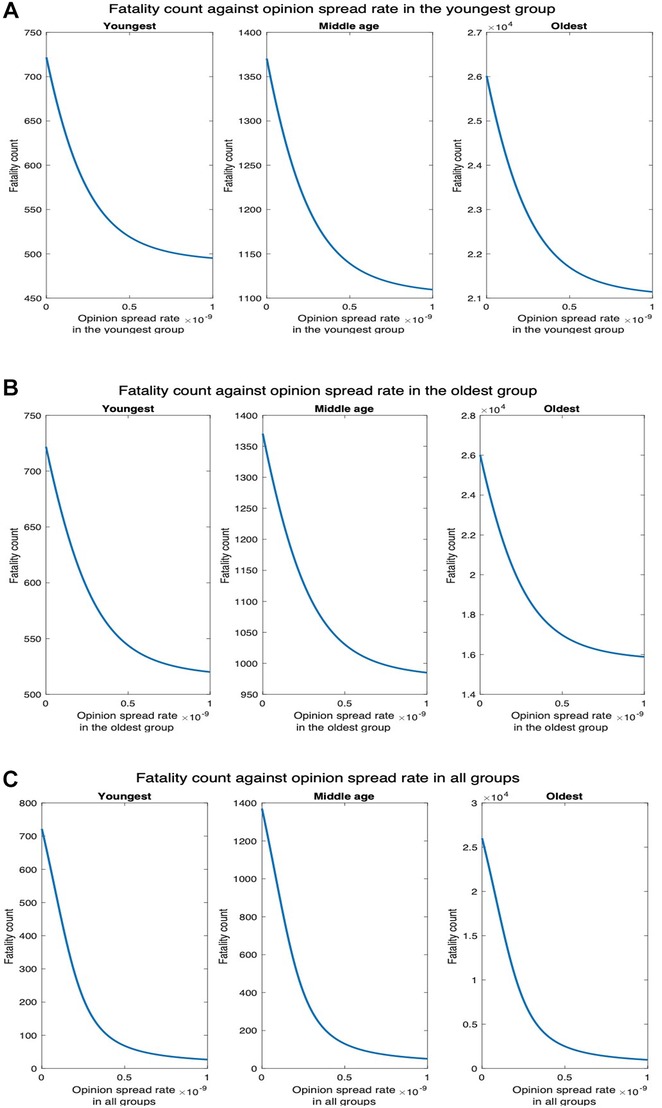
Figure 8. Fatality count when the interaction rates of the oldest group equal that of the youngest group. (A) Opinion spread rate varied for the youngest group. (B) Opinion spread rate varied for the oldest group. (C) Opinion spread rate varied for all the groups.
3.2.2. Second transmission rate scenario
Next, we consider the case whereby the disease spread rate is at its default value when only one of the interacting pair is cooperative; when both the interacting individuals are non-cooperative, the disease spread rate is twice the default value; and when both the interacting individuals are cooperative, the disease spread rate is half the default value. Figure 9A shows that the fatality counts for all, youngest, middle-age, and oldest groups, respectively, decrease by , , and as the opinion spread rate of the youngest group increases from through . Figure 9B shows that the fatality counts for all, youngest, middle-age, and oldest group, respectively, decrease by , , , and , as the opinion spread rate of the oldest group increases from through . Thus, the pattern of variation remains the same as before. Figure 9C shows that the fatality counts for all, youngest, middle- age, and oldest groups, respectively, decrease by , , , and as the opinion spread rate for all the groups increases from through . Finally, even when the interaction rate of the youngest group is tripled, the fatality count for all, youngest, middle-age, and oldest groups, respectively, decrease by , , and . Thus, the impact of the opinion spread rate across all the groups is quite significant even when the disease spread rate is increased.
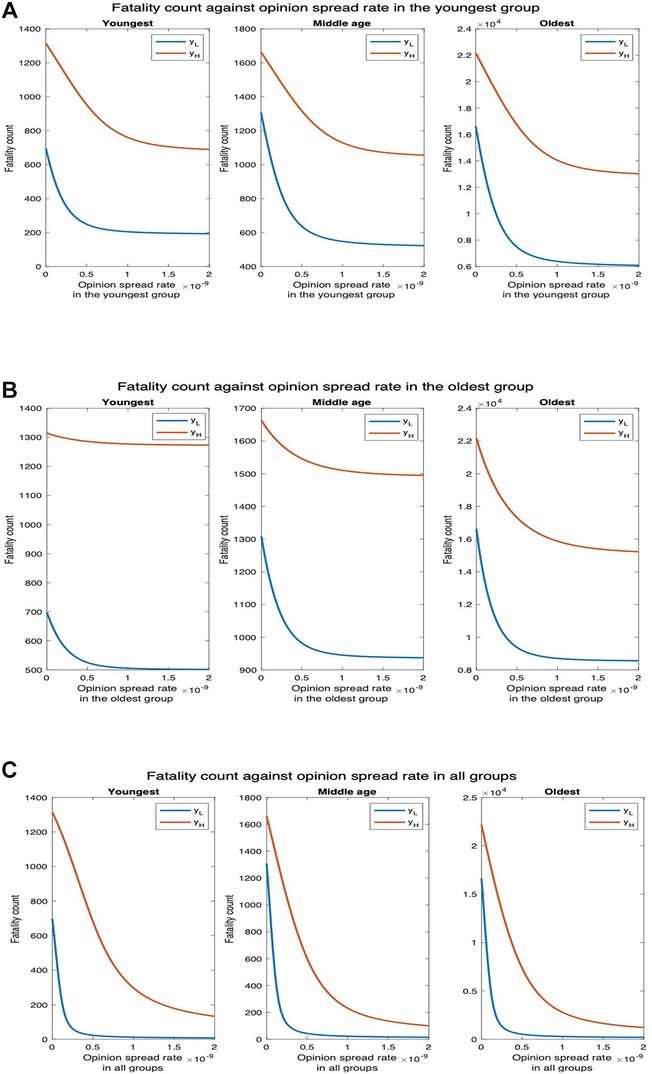
Figure 9. Fatality count for various interaction rates of the youngest group. denotes the default interaction rates of the youngest group while represents when the youngest group’s interaction rates are tripled (other groups’ interaction rates remain the same). (A) Opinion spread rate varied for the youngest group. (B) Opinion spread rate varied for the oldest group. (C) Opinion spread rate varied for all groups.
3.2.3. Impact of long COVID
Next, we evaluate the impact of opinion dynamics in the presence of long COVID. Recall that long COVID occurs when coronavirus symptoms persist for at least 60 days or return 3 months after an individual becomes ill from SARS-CoV-2. We consider only the former here; in effect, this increases the duration of symptoms for patients or a fraction thereof and decreases the productivity of the populace. We consider the number of man-days patients suffer from symptoms, i.e., the number of days each patient suffers from symptoms summed up over all patients. This attribute is the sum of two components: (1) man-days lost due to symptoms during the symptomatic phase of COVID-19 infection; (2) man-days lost due to patients experiencing symptoms after recovering. Due to the second component, a section of the patients experiences symptoms even after transitioning to the recovered state when they are no longer infectious. The first component is , where is the number of days we consider, is the number with symptoms, and the number hospitalized on day . The second component is , where is the number of cooperatives who recover on day , is the number of non-cooperatives who recover on day , is the fraction of cooperatives who suffer long COVID, and is the fraction of non-cooperatives who suffer long COVID. In the current section, neither cooperatives nor non-cooperatives are vaccinated. We consider as of unvaccinated individuals suffer from long COVID (31, 32). We now plot the number of man-days patients experience symptoms against the rate of spread of opinion (Figure 10).
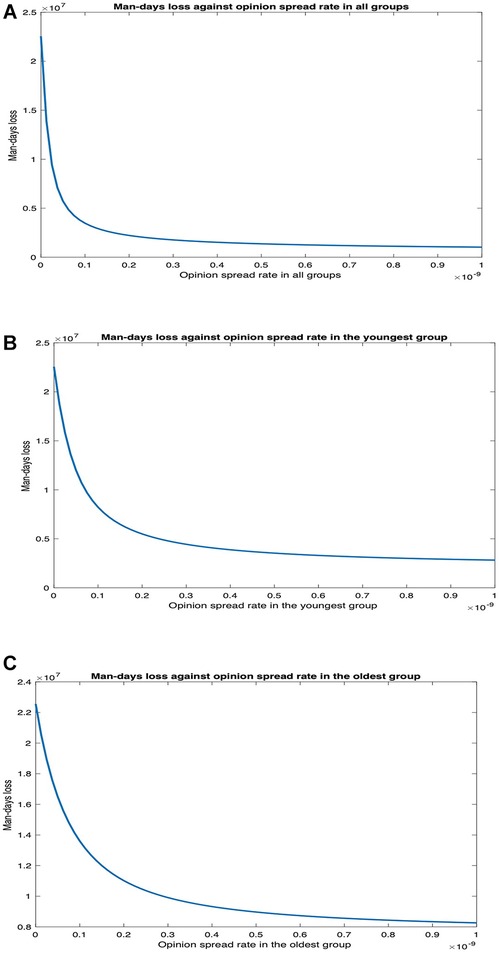
Figure 10. Impact of opinion dynamics on long COVID in Scenario 1. (A) Number of man-days of patients suffering symptoms vs. opinion spread rate in all the groups. (B) Number of man-days of patients suffering symptoms vs. opinion spread rate in only the youngest group. (C) Number of man-days of patients suffering symptoms vs. opinion spread rate in only the oldest group.
We observe that man-days lost decreases as the opinion spread rate increases. The decrease is most when the opinion spread rate for all the groups increases, intermediate when the rate of spread of opinion increases only for the youngest group, and least when the rate of spread of opinion only increased for the oldest group. When the rate of spread of opinion for all the groups, only the youngest group, and only the oldest group increases, man-days lost due to long COVID decreases by , , and , respectively. Thus, the impact of opinion dynamics is pronounced in this case as a higher rate of spread of opinion tantamount to non-cooperatives converting to cooperatives at a higher rate, which in turn leads to a lower rate of spread of the disease in the populace and, therefore, a lower number of man-days individuals experience symptoms. Again, the opinion dynamics in the youngest group have a much greater impact than that in the oldest group.
3.2.4. Synthetic variant with high fatality rate
Next, we consider higher values of fatality rate motivated by the recent creation by BU researchers of a synthetic variant of COVID-19, a recombinant virus called Omi-S, that causes fatality rate in mice (19). Figure 11 shows that fatality count increases by a factor of as compared to when the fatality rate is at the default value (Figure 7). In addition, the decrease in fatality with the increase in the opinion spread rate follows the same pattern as in the default case. For instance, when the opinion spread rates for the youngest group increase from to , the fatality counts for all, youngest, middle-age, and oldest groups, respectively, decrease by , , , and as against , , , and in the default case. Similarly, when the opinion spread rates for the oldest group increase from to , the fatality counts for all, youngest, middle-age, and oldest groups, respectively, decrease by , , , and as against , , , and in the default case.
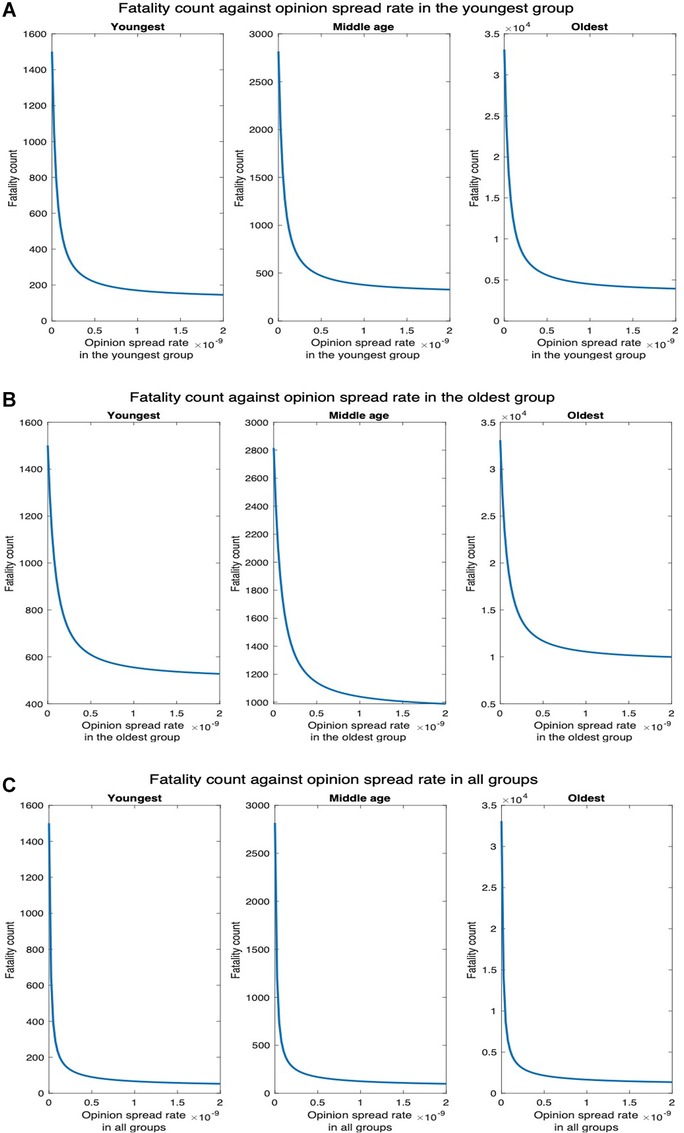
Figure 11. Synthetic variant with high fatality rate. (A) Fatality count vs. opinion spread rate when the latter is increased in all groups for high fatality rate. (B) Fatality count vs. opinion spread rate when the latter is increased in the youngest group for high fatality rate. (C) Fatality count vs. opinion spread rate when the latter is increased in the oldest group for high fatality.
3.2.5. When non-cooperatives convert cooperatives
We finally consider the case that non-cooperatives convert cooperatives while exchanging opinions. Now, as expected, unlike in the former case where cooperatives convert non-cooperatives, fatality increases with an increase in the opinion spread rate. We consider two values of the physical interaction rate in the youngest group: default value and thrice the default value (Figure 12). We observe that for , the fatality counts in all, youngest, middle-age, and oldest groups, respectively, increase by , , , and as the opinion spread rate in the youngest group increases from through (Figure 12A). For , the fatality counts for all, youngest, middle-age, and oldest groups will, respectively, increase by , , and as the opinion spread rate in the youngest group increases from through . Similarly, for , the fatality counts for all, youngest, middle-age, and oldest group, respectively, increase by , , , and as the opinion spread rate of the oldest group increases from through (Figure 12B). For , the fatality counts for all, youngest, middle-age, and oldest groups, respectively, increase by , , , and as the opinion exchange rate in the oldest group increases from to . In addition, for , the fatality counts for all, youngest, middle-age, and oldest group, respectively, increase by , , , and as the opinion spread rate in all the groups increases from through (Figure 12C). Similarly, for , the respective increases in this case are , , , and We observe that as before, the highest increase in fatalities occurs when the opinion spread rate increase for all the groups, and if the opinion spread rates were to increase in only one age group, the increase in the youngest one has the maximum impact over all the groups.
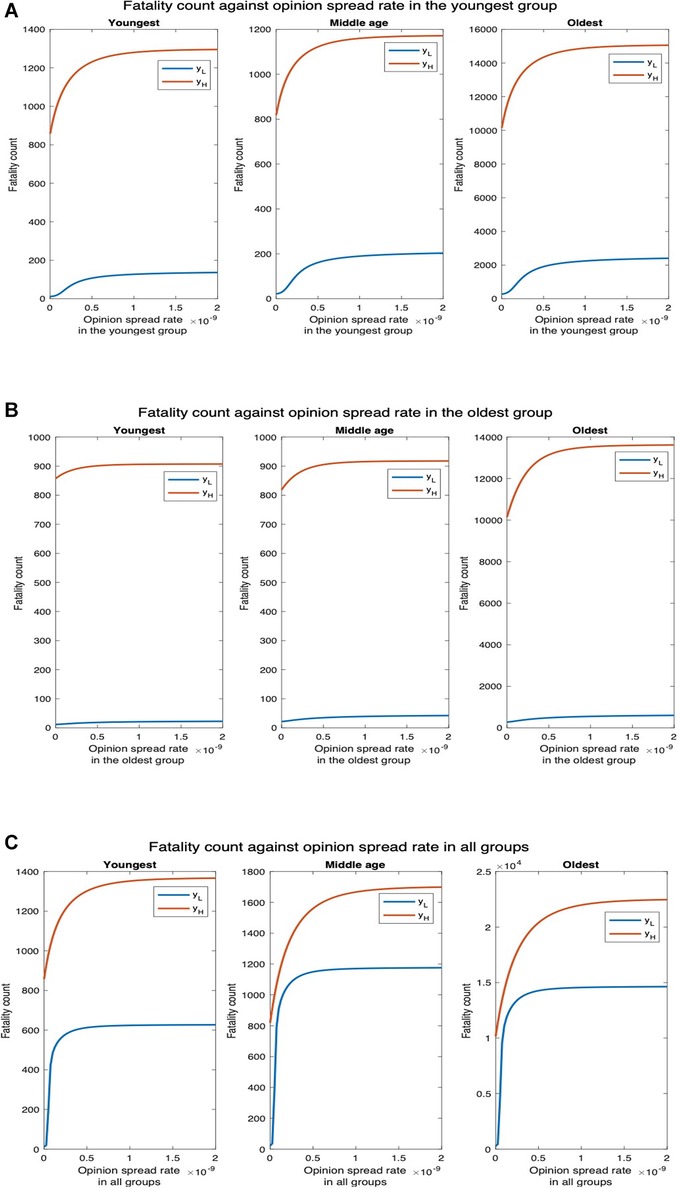
Figure 12. Non-cooperatives convert cooperatives during interactions. denotes the default interaction rates of the youngest group while represents when the youngest group interaction rates are tripled (other groups’ interaction rates remain the same). (A) Opinion spread rate varied for the youngest group. (B) Opinion spread rate varied for the oldest group. (C) Opinion spread rate varied for all the groups.
3.3. Impact of opinion dynamics when behavioral practices affect the severity of symptoms of COVID-19: scenario 2
We consider that cooperatives are willing to receive vaccines but observe no other behavioral precaution; non-cooperatives refuse all behavioral precautions including receiving vaccines. We assumed that COVID-19 vaccination in the United States is now readily available across the country and the vaccines need only one dose. Thus, an individual is vaccinated right after he becomes willing to be vaccinated, i.e., cooperative. According to Wilder-Smith (6), the secondary attack rate (SAR) among household contacts exposed to fully vaccinated index cases was similar to household contacts exposed to unvaccinated index cases. Thus, vaccination does not affect the rate of transmission of the disease, and cooperatives spread the disease at the same rate as non-cooperatives. However, it has been established that vaccines reduce the severity of symptoms, including hospitalization and death. For example, vaccines reduce non-intensive care unit (ICU) hospitalizations and deaths by and , respectively (33). Thus, infected cooperatives experience lower hospitalization and death rates as compared to infected non-cooperatives.
Since cooperatives transmit the disease at the same rate as non-cooperatives, conversion to cooperative does not affect the rate of spread of the disease. Thus, increasing the rate of spread of opinions in one age group affects the fatality count only in that group. As the rate of spread of opinion in the youngest group increases from through , the fatality count for the middle-age and oldest groups remain unchanged; the fatality count in the youngest group, however, decreases by (Figure 13A). For , the disease spreads faster among the young and subsequently to the other groups. Thus, the fatality counts increase in all age groups in this case, but the fatality counts decrease with an increase in the opinion exchange rate only in the youngest group, the fatality counts do not change in other age groups. Similarly, when the opinion exchange rate increases only in the oldest group, the fatality count remains constant in other age groups but decreases by in the oldest group (Figure 13B). Thus, opinion dynamics in one group do not affect public health attributes among others.
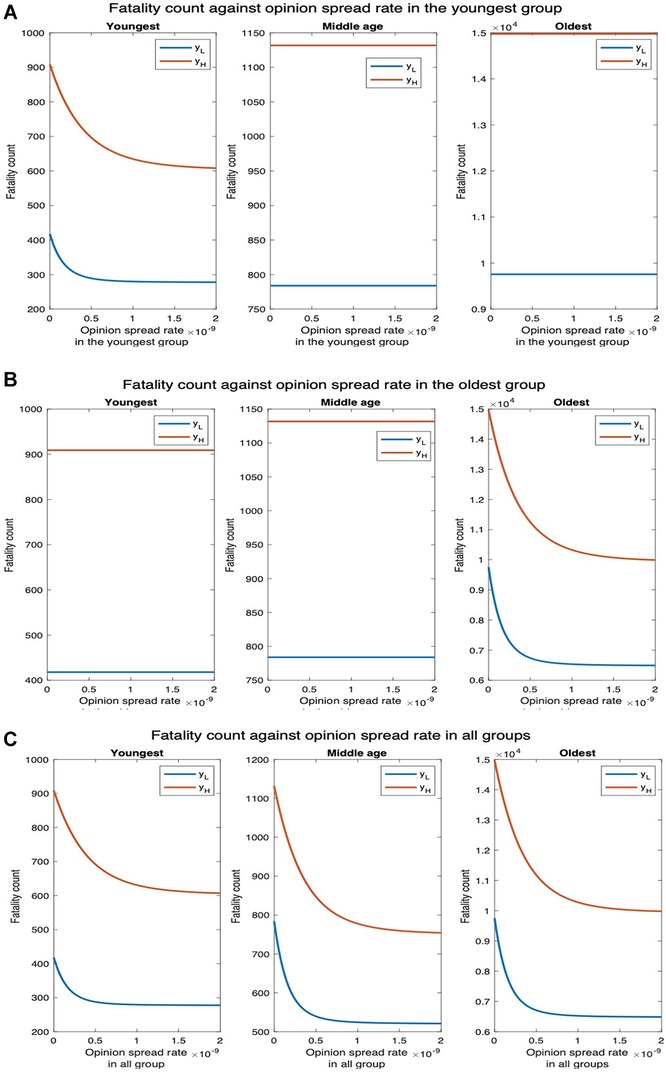
Figure 13. Impact of vaccination on fatality. denotes the default interaction rates of the youngest group while represents when the youngest group interaction rates are tripled (other groups’ interaction rates remain the same). (A) Opinion spread rate varied for the youngest group. (B) Opinion spread rate varied for the oldest group. (C) Opinion spread rate varied for all the groups.
Next, we consider the impact of long COVID. For multidose vaccine, the prevalence of long COVID in vaccinated individuals is after one dose, after two doses, and after a single dose. Since we consider only single-dose vaccines, we consider the overall prevalence to be the average, i.e. (31, 32). The number of man-days of symptoms can be computed similarly to that for Scenario 1, with the difference that in this case as different fractions of vaccinated and unvaccinated experience long COVID. The fraction of cooperatives and non-cooperatives who suffer long COVID are and , respectively (31, 32). The man-days lost due to COVID decrease as the opinion spread rate increases (Figure 19). The decrease is most when the opinion spread rate increases in all groups, intermediate when the rate of spread of opinion increases only for the youngest group, and least when it increases only in the oldest group. When the rate of spread of opinion increases in all groups, only in the youngest group, and only in the oldest group, the number of man-days decreases by , , and , respectively. In the presence of long COVID, the man-days lost when cooperatives only accept vaccines is observed to be lower when compared to the case in which cooperatives observe the behavioral practices that impede COVID but do not accept vaccines.
3.4. Impact of opinion dynamics when behavioral practices affect both spread and severity of symptoms of COVID-19: scenario 3
We now consider that cooperatives follow behavioral practices that impede the spread of COVID-19 and reduce the severity of symptoms if one imbibes the disease (i.e., accepts vaccines). The fatality counts for all, youngest, middle-age, and oldest groups, respectively, decrease by , , , and as the opinion spread rate of the youngest group increases from through (Figure 14A). The fatality counts for all, youngest, middle-age, and oldest group decrease by , , , and , respectively, as the opinion spread rate of the oldest group improves from through (Figure 14B). Similarly, the fatality counts for all, youngest, middle-age, and oldest group ,respectively, decrease by , , , and as the opinion spread rate in all groups improves from through (Figure 14C). Thus, opinion exchange in all groups has the greatest impact, if opinions are to be exchanged in only one group, selecting the youngest group has the maximum impact. For , the number of deaths for all, youngest, middle-age, and oldest groups will, respectively, decrease by , , , and , as the opinion spread rate in the youngest group is varied (Figure 14A). Similarly, the number of deaths for all, youngest, middle-age, and oldest groups will, respectively, decrease by , , , and , as the opinion spread rate in the oldest group is varied (Figure 14B). In addition, the number of deaths for all, youngest, middle-age, and oldest groups will, respectively, decrease by , , , and , as the opinion spread rate in all groups is increased (Figure 14C).
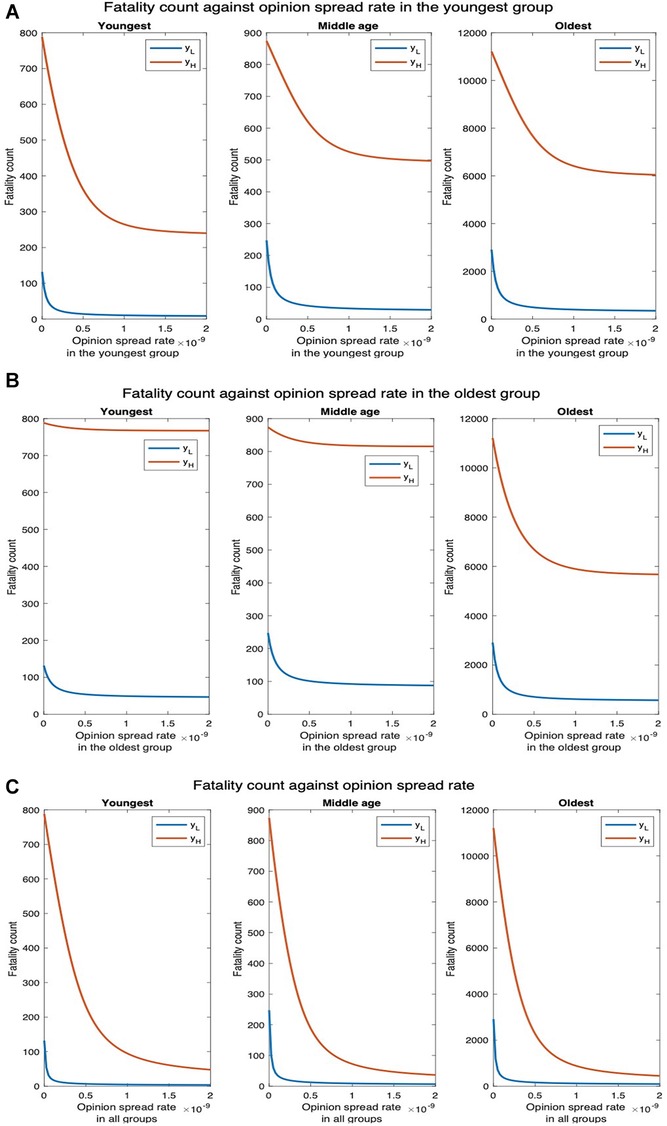
Figure 14. Joint implementation of vaccines and behavioral practices. denotes the default interaction rates of the youngest group while represents when the youngest group interaction rates are tripled (other groups’ interaction rates remain the same). (A) Opinion spread rate varied for the youngest group. (B) Opinion spread rate varied for the oldest group. (C) Opinion spread rate varied for all the groups.
We now consider the impact of opinion dynamics in the presence of long COVID. The number of man-days lost due to COVID-19 decrease as the opinion spread rate increases (Figure 20). The decrease is most when the opinion spread rate for all the groups improve, intermediate when the rate of spread of opinion increases only for the youngest group, and least when the rate of spread of opinion only increases for the oldest group. When the rate of spread of opinion for all the groups, the youngest group only, and oldest group only increases from through , the above attribute decreases by , , and , respectively. These decreases are considerably higher compared to that when cooperatives only accept vaccines and do not adopt other behavioral precautions; the decreases are only , , and in this case (Scenario 2, Section 3.3). This is because we had considered that vaccines do not reduce the rate of transmission of disease (based on the cited literature). If vaccines reduced the transmission of the disease as well, at the same rate as behavioral practices, the results in this section will be obtained even when cooperatives only accept vaccines.
3.5. A comparative analysis of the three scenarios: summary
Scenario 1
Scenario 1: The decrease in the total fatality count when opinion spread rates are increased in individual groups, as reported in Tables 1 and 2, shows that the impact of increasing opinion exchange rate in a group depends on (1) physical contact rate for it; and (2) risk factor for it. Increasing opinion spread rates in the youngest and middle-age groups decrease the total fatality by the same amount when they have the same contact rates (Table 1). The decrease is significantly higher for the youngest group as compared to the middle-age group when the physical contact rate for the former is twice that of the latter (Table 2). The physical contact rate for the oldest group is the lowest, but increasing the opinion spread rate in it still decreases the overall fatality because the risk factor in the oldest group is highest. The decrease is still the lowest when we increase the opinion exchange rate in the oldest group alone because the infections in the other groups reach the oldest group because of the high physical contact rates of the other two.
Scenario 2
Scenario 2: Recall that in this case, cooperatives receive vaccines (and therefore have lower risk of developing severe forms of the disease if infected), but they do not follow behavioral practices that reduce the chances of contracting the disease. Thus, increasing the opinion exchange rate in one group reduces fatality in only that group and does not have any impact on another group. Thus, the decrease in total fatalities as the opinion spread rates are increased will be more significant if the increment occurs in the group with the highest risk factor. The risk factors are highest for the oldest group, intermediate in the middle age group but only slightly higher than the youngest group, and least for the youngest group. Thus, increasing the opinion exchange rate in only the oldest group decreases the total fatality count significantly, and increasing the opinion exchange rate in only the middle-age group decreases the overall fatality count only slightly more than increasing the opinion exchange rate in only the youngest group. The opinion dynamics has the least overall impact in this scenario as cooperativity does not decrease spread at all.
Scenario 3
Scenario 3: The trends are similar in this scenario as in Scenario 1 because cooperativity reduces the spread in both. The only difference is that increasing the opinion exchange rate in only the oldest group decreases the overall fatality count more in Scenario 3. This is because cooperativity additionally decreases the probability of developing a severe form of the disease in the infected in this scenario and the oldest age group has the greatest risk of developing a severe form of the disease.
4. Discussion
We summarize the important findings from our work and the implications thereof to practice. We have presented a mathematical model that can be easily adapted to model the impact of a wide range of behaviors on public health attributes during the spread of COVID-19. Our model is therefore flexible and also computationally tractable in that the size of the population does not affect the computation time. Thus, the model can scale to large population sizes, which is an important strength given that the target population for a pandemic is typically large and easily in the order of millions considering populations of large cities and even mid-size provinces. Some of our findings from the model reinforce prior expectations by quantifying the impact. For example, we show that following a combination of behavioral practices that impede the spread of COVID-19 and partaking in vaccines that reduce the severity of symptoms together substantially reduce both the fatalities and the number of man-days lost due to symptoms from long COVID. This conclusion is only expected but our findings quantify the improvements that accompany good health practices. The quantifications are useful in comparing different scenarios and impact of opinions of different groups, which can help public health/government agencies formulate necessary rules and guidance. Next, we show that opinion dynamics pertaining to the observance of behavioral practices that impede the spread have a substantial impact on fatality count and man-days lost due to symptoms. In particular, a higher rate of exchange of opinions that convert (respectively dissuade) individuals to observing such practices substantially decreases (respectively increases) the fatality count and man-days lost due to symptoms. Our work is the first to quantify the impact of behavioral dynamics and the spread of opinions pertaining to the observance of desired behaviors on public health damages inflicted by COVID-19. We also show that opinion dynamics in groups that have the highest rate of physical interaction have the maximum impact on overall fatalities and man-days lost due to symptoms even though such groups are least likely to imbibe severe forms of the disease. Specifically, if the rate of spread of opinion that conforms to desirable behavioral practices increases among the youngest groups, fatality for all the groups decreases. If the rate of spread of similar opinions increases among the oldest age group, then the positive impact due to the spread is largely confined to the same age group. We show that this disparity arises because young individuals physically interact among themselves and across age groups at a higher rate than others. The consequence of this finding is that it reveals how mal-actors can undermine public health in society by deliberately targeting young individuals with a propaganda campaign that dissuades them from observing desirable health practices. Note that such dissuading may be relatively simple because their own risk of imbibing a severe form of the disease is low. Appropriate precautions involving a counter-information campaign can be undertaken once this vulnerability is identified and its impact quantified which our work has accomplished.
For simplicity, we have considered that individuals are not reinfected. Thus, different waves of infection were not captured in the current research. This constitutes an important direction for future research.
In conclusion, we discuss a generalization of our model. We have so far assumed that vaccines require only one dose. But, according to CDC, there are four approved or authorized vaccines in the United States, namely, Pfizer-BioNTech, Moderna, Johnson & Johnson’s Janssen, and Novavax COVID-19 vaccines; and Johnson & Johnson’s Janssen requires one dose but all the rest require two doses 3–4 weeks apart. We now describe how our model can be generalized to accommodate two doses. Refer to Figure 15 for a pictorial illustration of the state diagram that captures this generalization while considering classification based only on opinions. The only difference with the previous versions (i.e., Figure 3) is that we introduce a new vaccinated state () and cooperative susceptibles and exposed transition to this state after they receive the second dose. When an individual becomes cooperative, we consider that he has received the first dose because currently in many countries the first dose can be received without any administering delay. The transition time between the cooperative and vaccinated state is the delay mandated between the two doses. According to the CDC, people who tested positive for COVID-19 (symptomatic or asymptomatic) should wait to be vaccinated until they have recovered from their illness and have met the criteria for discontinuing isolation (34). We, therefore, do not include any transition from symptomatic or asymptomatic states to vaccinated. Thus, a vaccinated individual can get infected and transition to the exposed state , then to either the presymptomatic or asymptomatic stage at a certain probability. The asymptomatic vaccinated recovers after some days while the presymptomatic vaccinated experiences symptoms after about 2 days. Thereafter, the symptomatic vaccinated either get hospitalized at a reduced hospitalization rate or recover. The hospitalized individual eventually recovers or dies. The hospitalization and fatality rates for vaccinated individuals are much lower compared to those for unvaccinated individuals. These can be incorporated by appropriately choosing the transition probabilities from the vaccinated state.
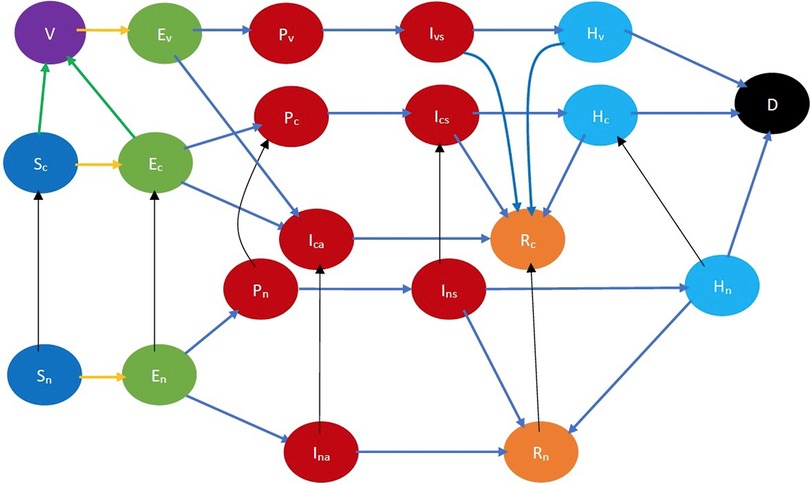
Figure 15. COVID-19 state diagram for two-dose vaccine. The state in purple color is the vaccinated state. The states in blue color are the susceptibles while those in light green color are exposed (still in the incubation period). The states in dark red are infected and therefore infectious while those in gold have recovered, those in light blue are hospitalized, and black denotes dead. In addition, the green arrows denote transition to the vaccinated state after receiving the vaccine, the yellow arrows show susceptibles transitioning to the exposed state after contracting the virus, the black arrows indicate opinion evolution, and the blue arrows indicate the natural progression of the disease. The yellow arrows show susceptibles transitioning to the exposed state after contracting the virus.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics statement
Ethical review and approval was not required for this study in accordance with the local legislation and institutional requirements.
Author contributions
RA and SS contributed to the formulation of the model. RA wrote the codes, generated the plots, and drafted the manuscript. SS reviewed and updated the manuscript. All authors critically reviewed the final version of the manuscript. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fdgth.2023.1146178/full#supplementary-material
References
1. Centers for Disease Control, Prevention (CDC). First travel-related case of 2019 novel coronavirus detected in United States. 2020 January. Available from: https://www.cdc.gov/media/releases/2020/p0121-novel-coronavirus-travel-case.html (Accessed November 1, 2022).
2. Zeller M, Gangavarapu K, Anderson C, Smither AR, Vanchiere JA, Rose R, et al. Emergence of an early SARS-CoV-2 epidemic in the United States. Cell. (2021) 184(19):4939–52. doi: 10.1016/j.cell.2021.07.030
3. World Health Organization (WHO). WHO Director-General’s opening remarks at the media briefing on COVID-19-11 March 2020. Available from: https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19—11-march-2020 (Accessed November 1, 2022).
4. Centers for Disease Control, Prevention (CDC). CDC Covid data tracker. Available from: https://covid.cdc.gov/covid-data-tracker/datatracker-home (Accessed November 1, 2022).
5. Abaluck J, Kwong LH, Styczynski A, Haque A, Kabir MA, Bates-Jefferys E, et al. Impact of community masking on COVID-19: a cluster-randomized trial in Bangladesh. Science. (2022) 375(6577):eabi9069. doi: 10.1126/science.abi9069
6. Wilder-Smith A. What is the vaccine effect on reducing transmission in the context of the SARS-CoV-2 delta variant? Lancet Infect Dis. (2022) 22(2):152–3. doi: 10.1016/S1473-3099(21)00690-3
7. Centers for Disease Control and Prevention (CDC). Summary of guidance for minimizing the impact of COVID-19 on individual persons, communities, and health care systems—United States, August 2022. Available from: https://www.cdc.gov/mmwr/volumes/71/wr/mm7133e1.htm (Accessed November 1, 2022).
8. Thompson MG, Stenehjem E, Grannis S, Ball SW, Naleway AL, Ong TC, et al. Effectiveness of COVID-19 vaccines in ambulatory and inpatient care settings. N Engl J Med. (2021) 385(15):1355–71. doi: 10.1056/NEJMoa2110362
9. Calafiore GC, Fracastoro G. Age structure in SIRD models for the covid-19 pandemic—a case study on italy data and effects on mortality. PLoS One. (2022) 17(2):e0264324. doi: 10.1371/journal.pone.0264324
10. Centers for Disease Control and Prevention (CDC). COVID-19 risks and vaccine information for older adults. 2021 August. Available from: https://www.cdc.gov/aging/covid19/covid19-older-adults.html (Accessed November 1, 2022).
11. Centers for Disease Control and Prevention. COVID-19 pandemic planning scenarios. Available from: https://www.cdc.gov/coronavirus/2019-ncov/hcp/planning-scenarios.html (Accessed December 10, 2020).
12. Chandler RF. COVID19 and the commonwealth: vulnerable populations in Pennsylvania: health risks & factors. Pennsylvania Population Network, Pennsylvania State University, University Park, PA. Issue 05 | Apr 2020 https://pop.psu.edu/sites/pri/files/COVIDSmoking&Obesity.pdf
13. Centers for Disease Control and Prevention (CDC). People with certain medical conditions. Available from: https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-with-medical-conditions.html (Accessed January 2, 2023).
14. DeSimone DC. Why are people of color more at risk of being affected by COVID-19? October 2022. Available from: https://www.mayoclinic.org/diseases-conditions/coronavirus/expert-answers/coronavirus-infection-by-race/faq-20488802 (Accessed November 1, 2022).
15. Jin J-M, Bai P, He W, Wu F, Liu X-F, Han D-M, et al. Gender differences in patients with COVID-19: focus on severity and mortality. Front Public Health. (2020) 8:152. doi: 10.3389/fpubh.2020.00152
16. Marcum CS. Age differences in daily social activities. Res Aging. (2013) 35(5):612–40. doi: 10.1177/0164027512453468
17. Vaidyanathan R. Why don’t black, white Americans live together? British Broadcasting Corporation (2016). https://www.bbc.com/news/world-us-canada-35255835
18. Dunsmuir L. Many Americans have no friends of another race: poll. New York: Reuters (2013). https://www.reuters.com/article/ususa-poll-race/many-americans-have-no-friends-of-another-race-poll-idUSBRE97704320130808
19. Chen D-Y, Kenney D, Chin C-V, Tavares AH, Khan N, Conway HL, et al. Role of spike in the pathogenic, antigenic behavior of SARS-CoV-2 BA.1 Omicron. bioRxiv (2022).
20. Soriano JB, Murthy S, Marshall JC, Relan P, Diaz JV. A clinical case definition of post-covid-19 condition by a Delphi consensus. Lancet Infect Dis. (2022) 22(4):e102–7. doi: 10.1016/S1473-3099(21)00703-9
21. Centers for Disease Control, Prevention (CDC). Long COVID or post-COVID conditions. Available from: https://www.cdc.gov/coronavirus/2019-ncov/long-term-effects/index.html (Accessed November 7, 2022).
22. Centers for Disease Control and Prevention (CDC). Defining adult overweight & obesity. Available from: https://www.cdc.gov/obesity/basics/adult-defining.html (Accessed February 6, 2021).
23. The Demographic Statistical Atlas of the United States—Statistical Atlas. Available from: https://statisticalatlas.com/state/Pennsylvania/Age-and-Sex (Accessed: July 20, 2021).
24. Ali RN, Rubin H, Sarkar S. Countering the potential re-emergence of a deadly infectious disease—information warfare, identifying strategic threats, launching countermeasures. PLoS One. (2021) 16(8):e0256014. doi: 10.1371/journal.pone.0256014
25. Apolloni A, Poletto C, Ramasco JJ, Jensen P, Colizza V. Metapopulation epidemic models with heterogeneous mixing, travel behaviour. Theor Biol Medical Model. (2014) 11(1):3. doi: 10.1186/1742-4682-11-3
26. Colizza V, Vespignani A. Epidemic modeling in metapopulation systems with heterogeneous coupling pattern: theory, simulations. J Theor Biol. (2008) 251(3):450–67. doi: 10.1016/j.jtbi.2007.11.028
27. Ogilvy Kermack W, McKendrick AG. A contribution to the mathematical theory of epidemics. Proc R Soc Lond A. (1927) 115(772):700–21. doi: 10.1098/rspa.1927.0118
28. Eshghi S, Preciado VM, Sarkar S, Venkatesh SS, Zhao Q, D’Souza R, et al. Spread, then target, and advertise in waves: optimal budget allocation across advertising channels. IEEE Trans Netw Sci Eng. (2018) 7(2):750–63. doi: 10.1109/TNSE.2018.2873281
29. Kim J, Sarkar S, Venkatesh SS, Smirti Ryerson M, Starobinski D. An epidemiological diffusion framework for vehicular messaging in general transportation networks. Trans Res B Methodol. (2020) 131:160–90. doi: 10.1016/j.trb.2019.11.004
30. Kiss IZ, Miller JS, Simon P. Mathematics of epidemics on networks: from exact to approximate models. Springer (2017). https://scholar.google.com/scholar?hl=en&as_sdt=0%2C39&q=Mathematics+of+Epidemics+on+Networks%3AFrom+Exact+to+Approximate+Models&btnG=
31. Van Beusekom M. Two or 3 vaccine doses may cut risk of long COVID. Center for Infectious Disease Research & Policy. Available from: https://www.cidrap.umn.edu/two-or-3-vaccine-doses-may-cut-risk-long-covid (Accessed January 7, 2023).
32. Azzolini E, Levi R, Sarti R, Pozzi C, Mollura M, Mantovani A, et al. Association between BNT162b2 vaccination and long COVID after infections not requiring hospitalization in health care workers. JAMA. (2022) 328(7):676–8. doi: 10.1001/jama.2022.11691
33. Moghadas SM, Vilches TN, Zhang K, Wells CR, Shoukat A, Singer BH, et al. The impact of vaccination on coronavirus disease 2019 (COVID-19) outbreaks in the United States. Clin Infect Dis. (2021) 73(12):2257–64. doi: 10.1093/cid/ciab079
34. Centers for Disease Control and Prevention (CDC). COVID-19—frequently asked questions about COVID-19 vaccination. Available from: https://www.cdc.gov/coronavirus/2019-ncov/vaccines/faq.html (Accessed January 10, 2023).
Keywords: COVID-19, COVID-19 dynamics, opinion dynamics, behavioral practice, opinion spread rate, cooperativity, long Covid, disease and opinion dynamics
Citation: Ali RN and Sarkar S (2023) Impact of opinion dynamics on the public health damage inflicted by COVID-19 in the presence of societal heterogeneities. Front. Digit. Health 5:1146178. doi: 10.3389/fdgth.2023.1146178
Received: 17 January 2023; Accepted: 24 April 2023;
Published: 8 June 2023.
Edited by:
Constantinos S. Pattichis, University of Cyprus, CyprusReviewed by:
Parimita Roy, Thapar Institute of Engineering & Technology, India,Tiantian Zhang, Fudan University, China
© 2023 Ali and Sarkar. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Rex N. Ali YWxpcmV4QHNlYXMudXBlbm4uZWR1
 Rex N. Ali
Rex N. Ali Saswati Sarkar
Saswati Sarkar