
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Digit. Health, 07 April 2022
Sec. Digital Mental Health
Volume 4 - 2022 | https://doi.org/10.3389/fdgth.2022.814248
This article is part of the Research TopicDesigning and Evaluating Games for Health and WellbeingView all 9 articles
 Manuela Ferrari1,2*
Manuela Ferrari1,2* Judith Sabetti2
Judith Sabetti2 Sarah V. McIlwaine2,3
Sarah V. McIlwaine2,3 Sahar Fazeli1,2
Sahar Fazeli1,2 S. M. Hani Sadati2,4
S. M. Hani Sadati2,4 Jai L. Shah1,2,3
Jai L. Shah1,2,3 Suzanne Archie5
Suzanne Archie5 Katherine M. Boydell6
Katherine M. Boydell6 Shalini Lal2,7,8
Shalini Lal2,7,8 Joanna Henderson9
Joanna Henderson9 Mario Alvarez-Jimenez10,11
Mario Alvarez-Jimenez10,11 Neil Andersson12,13
Neil Andersson12,13 Rune Kristian Lundedal Nielsen14
Rune Kristian Lundedal Nielsen14 Jennifer A. Reynolds15
Jennifer A. Reynolds15 Srividya N. Iyer1,2,3
Srividya N. Iyer1,2,3Nearly all young people use the internet daily. Many youth with mental health concerns, especially since the Covid-19 pandemic, are using this route to seek help, whether through digital mental health treatment, illness prevention tools, or supports for mental wellbeing. Videogames also have wide appeal among young people, including those who receive mental health services. This review identifies the literature on videogame interventions for young people, ages 12-29, and maps the data on game use by those with mental health and substance use problems, focusing on evidence for the capacity of games to support treatment in youth mental health services; how stakeholders are involved in developing or evaluating games; and any potential harms and ethical remedies identified. A systematic scoping review methodology was used to identify and assess relevant studies. A search of multiple databases identified a total of 8,733 articles. They were screened, and 49 studies testing 32 digital games retained. An adapted stepped care model, including four levels, or steps, based on illness manifestation and severity, was used as a conceptual framework for organizing target populations, mental health conditions and corresponding digital games, and study results. The 49 selected studies included: 10 studies (20.4%) on mental health promotion/prevention or education for undiagnosed youth (Step 0: 7 games); 6 studies (12.2%) on at-risk groups or suspected mental problems (Step 1: 5 games); 24 studies (49.0%) on mild to moderate mental conditions (Steps 2-3: 16 games); and 9 studies (18.4%) focused on severe and complex mental conditions (Step 4: 7 games). Two interventions were played by youth at more than one level of illness severity: the SPARX game (Steps 1, 2-3, 4) and Dojo (Steps 2-3 and 4), bringing the total game count to 35 with these repetitions. Findings support the potential integration of digital games in youth services based on study outcomes, user satisfaction, relatively high program retention rates and the potential usefulness of most games for mental health treatment or promotion/prevention. Most studies included stakeholder feedback, and involvement ratings were very high for seven games. Potential harms were not addressed in this body of research. This review provides an important initial repository and evaluation of videogames for use in clinical settings concerned with youth mental health.
International research identifies adolescence and early adulthood as critical periods for first-time mental illness (1–5), with potentially devastating consequences when education and other developmental activities are disrupted. Serious mental illness is associated with further risks for co-occurring physical illnesses, as well as poverty and homelessness (6). Adolescents and young adults have also been especially hard hit by deteriorating mental health during the Covid-19 pandemic (7–10). Yet, despite the risks and burdens of mental illness, many young people delay or avoid seeking mental health treatment (11) for reasons that are complex. They include difficulties recognizing symptoms (12), negative perceptions of mental health services and professionals (13), and concerns about the stigma of mental illness (14–16). Fewer than 20% of young people with mental health problems use mental health services at all (17, 18). Rather, some 70-80% have turned to online sources for mental health information or help with emotional problems (19, 20), preferring the privacy, easy access and greater control over help-seeking afforded by virtual mental health care (21).
With nearly all young people using the internet (1, 22), research interest in digital mental health interventions has accelerated in response to their mental health needs and preferences, particularly since the pandemic (8, 23). Digital technologies including telehealth, internet, virtual reality, artificial intelligence, smartphones, and videogames (24–28) have been evaluated, showing comparable effectiveness among them (26). Digital interventions using cognitive-behavioral therapy (CBT) are especially effective in treating depression and anxiety (24, 26, 29, 30). Moreover, digital game interventions are frequently used by youth recovering from psychosis (31), who are receptive to the use of technology for receiving mental health interventions (32). Digital game interventions also show promise for improving user engagement in mental health care (23, 33). Serious games, defined as computerized games for educational purposes or for changing experience or behavior patterns (34), are used as therapeutic tools in treating anxiety, depression, autism, post-traumatic stress disorder (PTSD), attention-deficit/ hyperactivity disorder (ADHD) and alcohol use (33, 35–40). Game interventions promote improved memory, attention span, problem-solving, emotion management and socialization (41), better information retention (42), and learning (43), while supporting behavior change (44). Research also supports the benefits of integrating patient/staff and peer-to-peer interaction, and stakeholder collaboration into game designs (45).
By contrast, some studies have identified links between videogame use and depression, aggression, addiction, and negative moods (46–48). The risks of excessive internet use have also intensified during the pandemic due to worldwide school closures and prolonged confinement of youth at home (48). Gaming disorder, identified in the World Health Organization International Classification of Diseases, 11th Revision, is characterized by extreme investment of time (8-12 h/day) in gaming to the detriment of real-world relationships, daily routines, and life responsibilities (49). Prevalence rates for gaming disorder among youth have also been estimated at 10-15% in Asian countries and 1-10% in Western countries (50). Research presenting a proper assessment of gaming disorder is at an early stage. Some researchers have identified theoretical and methodological issues (51), while others still believe that solid evidence on gaming disorder as anything but a symptom of other disorders has yet to be produced (52, 53).
Youth mental health services are a rapidly developing field with a focus on prevention, early identification, treatment innovation and service development (54–56). Amid the crisis provoked by Covid-19 and its disproportionate psychosocial effects for young people (57), opportunities exist to deploy and scale up digital services to support mental health for this population (58). Yet, competing perspectives also exist around videogame technology as a tool for mental health treatment and education. However, little is known about how games have been used in clinical mental health services for youth, the experiences of young service users, families and service providers with videogame interventions, or strategies to assess possible harms (33, 59, 60) and pathways to gaming disorder (61). This “gaming my way to recovery” review aims to identify the existing literature on digital games for youth and map the evidence on the broad aims of these games and their use by young people with a full range of mental health and substance use problems.
The age range for this study includes “youth” (ages 12-19) and “young adults” (ages 20-29) as defined in Canadian public health (62). Five research questions (RQ) are addressed:
1) How have digital game interventions for mental health promotion and treatment been implemented in youth mental health services? What barriers and facilitators affected their implementation?
2) What were the outcomes of implementing digital game interventions and what evidence exists for the capacity of digital games to support mental health services in caring for youth?
3) What is known about youth, family, and service provider involvement in the development and implementation of digital interventions in youth mental health services?
4) What is known about youth, family, and service provider involvement in the evaluation of digital interventions in youth mental health services?
5) What are the potential harms and ethical practices related to use of digital interventions in youth mental health services?
Scoping review methodology was chosen as best suited to knowledge synthesis involving an array of evidence, publication types and research approaches. The five-stage methodological framework for scoping reviews by Arksey and O'Malley (63) was used in developing the study protocol (IRRID: PRR1-10.2196/13834) (64) and search strategy. An additional consultation stage (65) was added to the framework so that insights about the research could be gathered from partners (youth mental health services) and knowledge users (youth experiencing mental health problems). The information presented in this manuscript follows the PRISMA Extension for Scoping Reviews (PRISMA-ScR) Checklist (66) (see Appendix 1 in Supplementary Material).
The stepped care model, used increasingly to guide clinical practice and evaluate complex interventions in community-based mental health programs (67–69), was chosen as the conceptual framework for the study. Model 1, published in the “gaming my way to recovery” protocol (64), presents an adapted version of the traditional stepped care model for categorizing target populations and mental health conditions. This model organizes mental health, mental conditions and illness according to four levels of mental health condition severity (or steps), from at-risk groups or those with suspected mental health problems (Step 1), mild-moderate mental health conditions (Steps 2-3), combining mild and moderate levels of severity that are not always easy to disaggregate, to severe mental illness (Step 4). Step 0 was added to the original stepped care model, to include population-based interventions for mental health prevention/promotion and education for asymptomatic youth. The second column in the model was reserved for corresponding digital game interventions (focus and types) and the third column for evidence on contributions to knowledge by digital games at each step, in terms of processes, impact, effectiveness, sustainability, equity, engagement, and ethical practices.
Members of mental health services participated in the design of this scoping review project which led to the development of the published protocol (64). Project team members included service providers and researchers from Canada, Australia, and Denmark, who represented several international youth mental health networks (ACCESS Open Minds, Youth Wellness Hubs Ontario, Frayme, Orygen, and the Black Dog Institute). An advisory group was also established, meeting weekly during the project. Meetings were facilitated by a young peer researcher and self-identified gamer with lived experience of mental illness. The advisory group provided feedback on the data extraction form and helped to adapt the Ladder of Children's Participation (70) for the tool used to assess user engagement in studies under review. The advisory group was also involved in project dissemination activities (e.g., webinars).
The search strategy was constructed in collaboration with a health services librarian and reviewed by a second librarian following the Peer Review of Electronic Search Strategies checklist (71). The 23 strings in the search included terms related to mental health, mental disorders and a range of common/serious conditions as listed in section Study Identification and Selection (e.g., depressive disorders, anxiety disorders, schizophrenia, psychotic disorders, alcohol and substance-related disorders, mood disorders); game-related terms (e.g., video games, serious games, virtual reality, gamification); and a section of keywords related to platforms (e.g., online, internet, web, digital or computer, phone, apps, console, handheld). Initial searches were performed using multiple databases (e.g., Ovid MEDLINE, EMBASE, PsycINFO, the Cochrane Library) from inception to November 30, 2018; the search was later updated to April 2021. Only published, peer-reviewed studies were included. Duplicate citations were removed using EndNote citation software (Clarivate Analytics). The search strategy was published with the study protocol (64).
Study identification criteria were as follows: (1) digital game interventions delivered on any technical platform, including personal computers, consoles (handheld or not), mobile devices and virtual reality; (2) interventions targeting mental health or substance use disorders or symptomatology, including depression, bipolar disorders, anxiety disorders, obsessive-compulsive disorder (OCD), schizophrenia and related psychotic disorders, eating disorders, PTSD, ADHD, specific phobia and interventions focused on mental health prevention, promotion or education; and (3) studies using any quantitative, qualitative or mixed methodologies. Review articles were not subject to data extraction and synthesis but were reserved for secondary reference searches.
The two-phase screening process included title-abstract and full-text reviews. First, four trained screeners, working in teams of two, independently assessed studies for inclusion in the review following a preliminary selection using the Rayyan (Qatar Computing Research Institute) screening tool (72). The following exclusion criteria were applied: (1) dissertations or theses; (2) articles with missing abstracts; (3) conference presentations; (4) interventions targeting physical illnesses (e.g., cancer, dementia, chronic pain); (5) interventions delivered by telemedicine; (6) board games or commercial videogames used for entertainment only. Specifically, commercial video games designed for entertainment were excluded, except where they were used in clinical samples for therapeutic purposes. Second, the two raters read the full texts of articles that met the inclusion/exclusion criteria and made a final selection. Differences in ratings were resolved by consensus, or by the project lead in cases where consensus could not be reached.
The four raters performed the data extraction, which was validated by senior researchers (MF, JS). A data extraction table was developed based on study characteristics and variables related to the research objective and questions. Data were extracted from articles in the final selection for the following categories: (1) study characteristics: aims/hypotheses, country, setting, methodology, theoretical framework/model, interventions, model and stakeholder participation ratings; (2) participant characteristics: age, sex, ethnicity; (3) game characteristics: object/description, type of game, digital platform, guidance (y/n), target diagnoses; (4) stakeholder engagement: ratings on participation in game development and evaluation by youth, family and service providers; (5) outcome measures; and (6) findings: quantitative, qualitative, player satisfaction, barriers/facilitators to implementation, adherence/attrition, and loss to follow-up (see Study Data file, Appendix 2 in Supplementary Material). Data were extracted for each article, synthesized, and entered by category for use in revising Model 1 (see the “gaming my way to recovery” protocol) (64).
A PRISMA flow diagram (73) summarizing the search results was produced (see Figure 1). Of a total 8,733 articles screened from the original and updated searches, 40 met the inclusion criteria, four were identified in the updated search, and five were identified through other methods for a total of 49 studies in the final review. These studies represented 12 different countries: over half from the USA (n = 10), the Netherlands (n = 9) and New Zealand (n = 8); followed by Spain (n = 5), Ireland and Romania (four studies each), Australia, Hong Kong, and South Korea (two studies each) and Chile, India, and Germany (one study each) (see Study Data file, Appendix 2 in Supplementary Material).
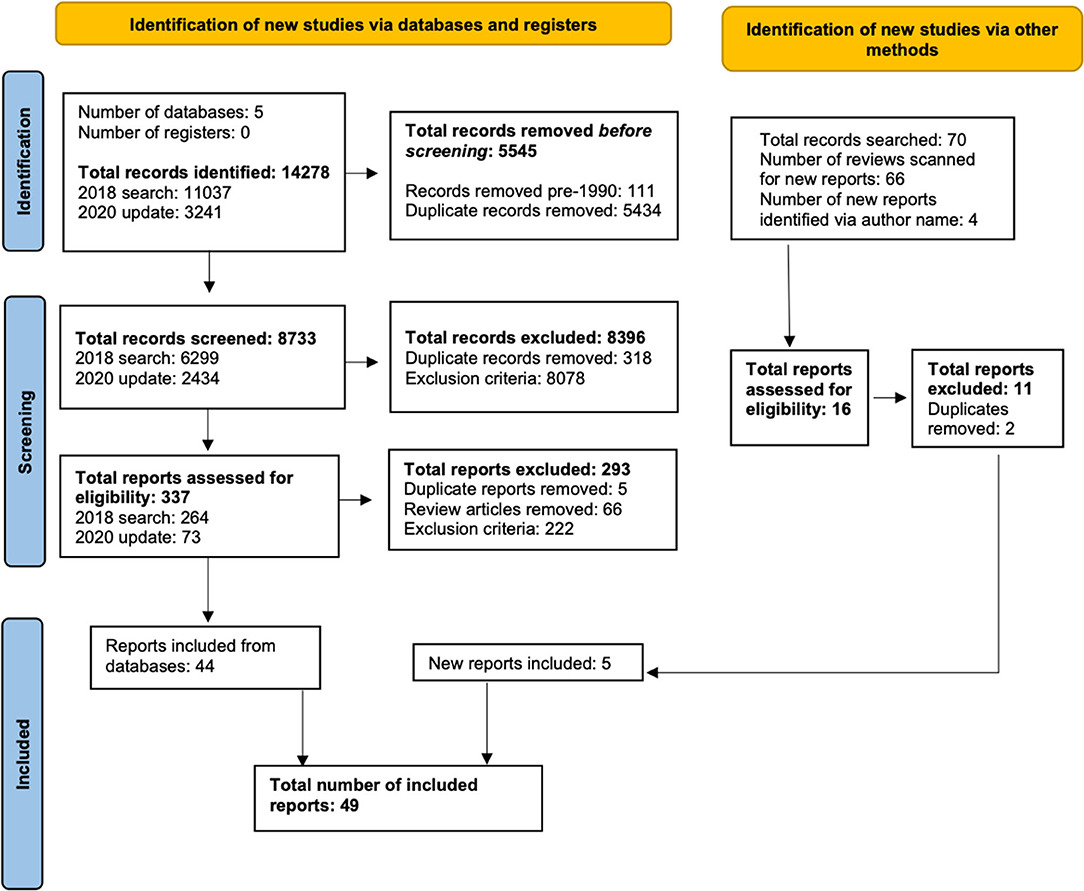
Figure 1. PRISMA 2020 flow diagram for updated systematic reviews which included searches of databases, registers, and other sources.
The 49 studies included 6,592 participants in total. Of the 40 studies with more than one participant and that provided data on gender, 57% (n = 2,199) of participants were female and 43% (n = 1,680) male. Most studies (n = 30) focused on “youth” 19 years or younger. The mean age was 14.4 years for youth and 22.4 years for young adults. Of the 49 studies, 39 tested games for 15 different diagnoses, while 10 studies focused on mental wellness for undiagnosed youth. Depression/depressive symptoms ranked first as the focus of 13 studies (26.5%) followed by studies for depression/anxiety or multiple forms of anxiety (six studies: 12.2%); substance use disorder, and alcohol use disorder or hazardous drinking accounted for three studies each, while complex trauma and obsessive-compulsive disorder had two studies each. The remaining diagnoses, with one study each, were ADHD, bulimia nervosa, specific phobia, PTSD, first episode psychosis, self-identified, and mental health problems (see Study Data file, Appendix 2 in Supplementary Material).
The Stepped Care Model for Videogame Interventions (see Figure 2), developed for this study, distributes the 32 games identified in the review across four steps: Step 0 describing population studies for mental health prevention, promotion, and education with undiagnosed youth, while Steps 1, 2-3, and 4 described ascending severity levels for mental illness, from at-risk or suspected mental health problems, to mild-moderate mental health conditions, to severe and complex mental health conditions. SPARX, the game most studied (74–83), was played by youth at all three levels of illness severity (Steps 1, 2-3, 4) and Dojo (84–86) was played at Steps 2-3 and 4, which brings the total game count to 35 taking these repetitions into account. Other games tested in more than one study were: Recovery Warrior (87, 88) (Step 4), SmartCAT (89, 90) (Steps 2-3), Pesky gNATs (91, 92) (Steps 2-3), and REThink (93–96) (Step 0). The remaining games were evaluated in single studies. Table 1 provides a general overview of characteristics for each digital game intervention (e.g., language, genre, duration, game customization, storyline, and goals).
The new Model provides a comprehensive overview of the state of knowledge in youth digital game technologies, showing how games have been implemented, their outcomes and evidence of capacity for potential use in youth mental health services, based on seven key constructs:
• Processes: study methodologies, including implementation barriers and facilitators (research question (RQ) 1).
• Impact: identification of games with significant improvement on main variable(s) of interest (e.g., symptom reduction for specific or multiple mental health conditions, improved protective factors), and positive results on secondary variables (e.g., life satisfaction, quality of life, psychological functioning, stigma, etc.) (RQ2).
• Effectiveness: statistical ratings/magnitudes of effect or descriptions of effectiveness based on specific outcomes that met study objectives, or study conditions, game designs, delivery platforms, etc. described as “effective”; user satisfaction and acceptability ratings/descriptions (RQ2).
• Sustainability: maintenance of gains from baseline to post-intervention/follow-up periods; intervention scalability (RQ2).
• Equity: reach of game to underserved populations (e.g., sexual, cultural/ethnic minorities; youth from socially and economically disadvantaged and/or remote areas) (RQ2).
• Engagement: types of stakeholder participation (youth, families, service providers, outside experts) in game development, evaluation, and levels of involvement (RQ3, RQ4).
• Ethical Practices: specific measures taken to insure player privacy, confidentiality, and safety; harm reduction measures including attention to potential risks for gaming disorder (RQ5).
The data on these constructs are presented in Supplementary Table 1: Data for 49 studies using the Stepped Care Model for Videogame Interventions as a conceptual framework (see Appendix 3 in Supplementary Material). The findings under Engagement were described in study narratives but were also included in the results on user satisfaction and acceptability. Thus, the complete data on stakeholder participation in developing, evaluating, and testing the videogame interventions, and involvement scores for each game, are presented separately in Table 2 as well as definitions for the four levels of participation and scoring procedures. The complete study results are described below, from no mental health diagnosis (Step 0) to the three levels of mental illness severity (Steps 1-4).
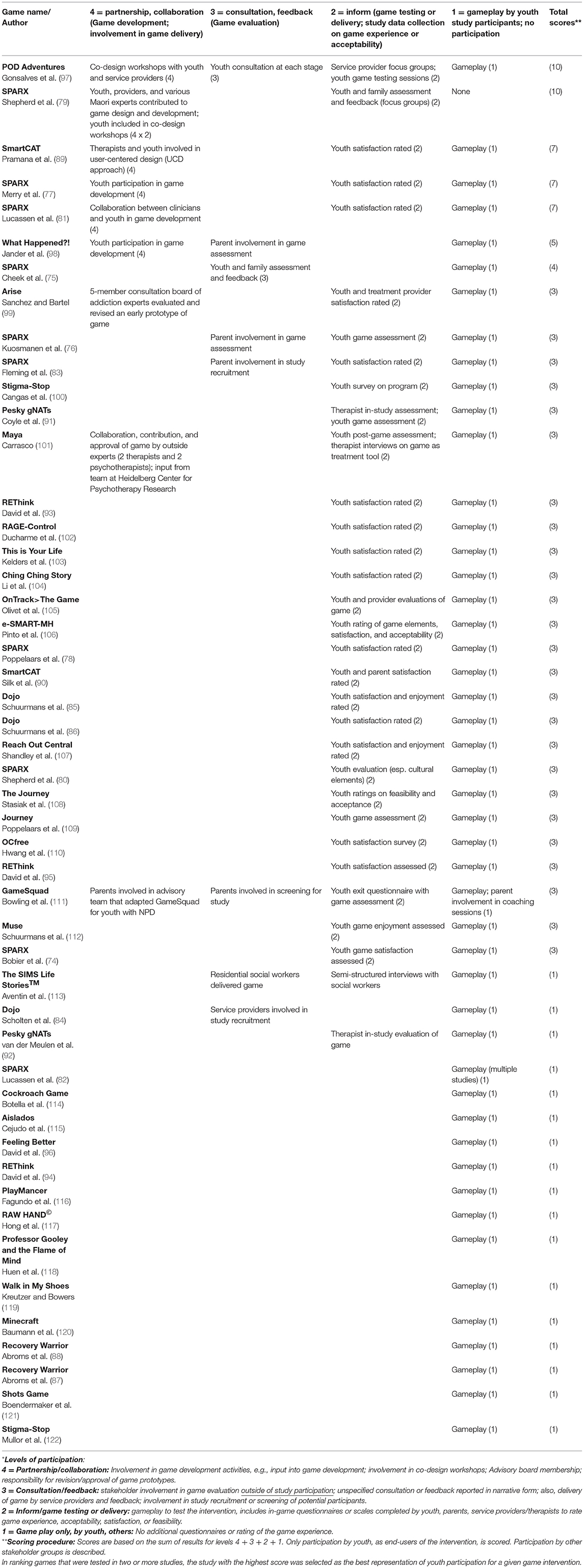
Table 2. Participation data and scores on stakeholder involvement in developing, evaluating, and testing 32 videogame interventions*.
The 10 studies (20.4% of the total 49) at Step 0 targeted young people without mental health diagnoses and included seven games focused on wellness through mental health promotion, prevention, and education. The five youth games involved mental health promotion and prevention: Aislados (115), REThink (93–95), Professor Gooley and the Flame of Mind (118), Stigma-Stop (100) for mental health education, and Feeling Better (96) on emotion regulation. The two games for young adults included a mental health prevention game, This is Your Life (103), and Ching Ching Story (104) for mental health education. Sigma-Stop (122), a third, was the same game as played by youth at Step 0.
Processes (RQ1) included two randomized clinical trials (93, 94), three pre-post game assessments (95, 100, 115), a pilot sequential game assessment (96) and a structural equation model (118). Barriers related to game design involved insufficient game duration and intensity in Feeling Better (96), viewed as a possible reason for results that did not meet expectations, and high attrition rates in Professor Gooley and the Flame of Mind (118) attributed to the self-help format. One study design/research issue in a pilot study concerned small sample size and lack of a control group (96).
Outcomes (RQ2) related to Impact showed significant improvement on the main variables of interest for all five games: for depressive mood in Feeling Better (96), health-related quality of life and mental health in Aislados (115), reduced stigma around mental illness in Stigma-Stop (100), improved functional emotion in REThink (93, 94) and user learning/psychological wellbeing in Professor Gooley and the Flame of Mind (118). Effectiveness was further demonstrated for REThink (93, 95), with a moderate effect on emotional symptoms but large effect on depressive mood. Regarding secondary measures, Aislados (115) promoted positive affect and better mental health. On user satisfaction/acceptability, Stigma-Stop (100) scored high on game usefulness, with 75% of players also recommending the game. Satisfaction scores at mid-intervention favored REThink (93) over controls. Study retention was reported for three games: Feeling Better, 88.0% (96); REThink, 86% (93, 94); and Professor Gooley and the Flame of Mind, 38.6% (118). However, on Sustainability, results were not sustained for REThink after three trials and game satisfaction faded by post-test (93, 96). Equity was promoted especially in Professor Gooley and the Flame of Mind (118), as all secondary students in Hong Kong were invited to the study.
Regarding Engagement (see Table 2), two youth games, REThink (93, 95) and Stigma-Stop (100) reported user satisfaction ratings, while these and the remaining youth studies, Aislados (115), Professor Gooley and the Flame of Mind (118), Feeling Better (96) and the other REThink study (94) included gameplay but no participation. The involvement ratings for these studies were: Stigma-Stop (100) and REThink (93, 95): 3 and for the games with no assessment: Aislados, Professor Gooley and the Flame of Mind, Feeling Better: 1 and a score of 1 for the remaining REThink study (94). Concerning Ethical Practices (RQ5), no results were reported.
Processes (RQ1) for these three studies included one experimental design (103) and two pre-post game assessments (104, 122). The one reported barrier involved a study design/research issue where lack of clarity in definitions of key concepts adversely affected the measures chosen for the study (103).
Outcomes (RQ2) on Impact showed significant improvement on the main variables of interest for all three studies: on game involvement and flow in the gamified vs. non-gamified condition in This is Your Life (103), mental health literacy in Ching Ching Story (104) and on all measures in Stigma-Stop (122): dangerousness, avoidance, segregation and anger. Effectiveness for the gamified version of This is Your Life (103) was equivalent to the non-gamified version on cognitive and affective engagement; while the Ching Ching Story (104) was most effective in enhancing mental health literacy. Stigma-Stop (122) demonstrated similar effectiveness as face-to-face contact or a talk by a professional in reducing stigma. Regarding user satisfaction, scores were high (average 7.8/10) for This is Your Life (103) and for Ching Ching Story (104), suggesting that participants were confident in their acquisition of mental health knowledge. Study adherence rates were reported for Stigma-Stop, 76.4% (122) and Ching Ching Story, 53.7% (104).
Regarding Engagement (see Table 2), no stakeholder involvement was reported on game development for the three adult games (RQ3), although two of them, This is Your Life (103) and the Ching Ching Story (104) had user satisfaction ratings, while Stigma-Stop (122) reported gameplay only (RQ4). Involvement scores were 3 for This is Your Life and the Ching Ching Story, and 1 for Stigma-Stop (122) (see Supplementary Table 1, Appendix 3 in Supplementary Material). Concerning Ethical Practices (RQ5), no findings emerged beyond descriptions of standard ethical procedures.
Step one included five games, three for youth and two for young adults, described in six of the 49 (12.2%) studies. Youth games included a therapeutic game, SPARX (75, 79) for depression risk, an educational game, POD Adventures (97), for self-identified mental health needs and GameSquad (111), a series of exergames with coaching to increase physical activity and counter obesity among youth with co-occurring mental health problems. The two young adult games were an educational/mental health prevention game, Reach Out Central (107) for alcohol use, and the Shots Game (121) for alcohol use.
Regarding Processes (RQ1), three youth studies used qualitative methods (75, 79, 97), while the fourth was an RCT (111). In one SPARX (75) study, participants received information and a 5-min trailer on SPARX, but did not play the game. Regarding barriers to implementation, a game design issue concerning limited game selection in GameSquad (111) was viewed as a possible explanation for drop-off from gameplay over time. Two SPARX studies (75, 97) reported barriers to implementation concerning equity issues around a lack of local internet infrastructure that reduced access to digital games. Resources were also lacking for promoting SPARX with indigenous (Maori) families (79). Maori designs with appeal for indigenous youth and families were identified as a facilitator for reducing cultural barriers and providing support (79). Remote telehealth counseling was viewed in GameSquad (111) as a facilitator for program engagement.
Outcomes (RQ2) in terms of Impact and Effectiveness were largely anecdotal for this group of studies, except for GameSquad (111), an RCT that showed significant improvement in physical activity among participants. User satisfaction reflected positive reactions to the games, while recommendations highlighted the importance of personalization and reflected user preferences for home use of games (75). SPARX showed good face validity, effectiveness, and cultural relevance (79). Program adherence rates were not reported for any youth studies in Step 1. GameSquad (111) showed evidence of Sustainability, with 67% of participants reporting intentions to continue using the program. Regarding Equity, three youth studies were geared toward the needs of youth in rural, underserved areas of Australia (75) and New Zealand (79) (SPARX), while POD Adventures focused on help-seeking among students attending under-resourced schools in rural India (97). Both games included culturally relevant characters with different genders and body shapes, and representations of different social classes and languages. Translations of POD Adventures are available in English, Hindi and Konkani, a local language in Goa. A rating scale with smiley faces was used to assist comprehension.
On Engagement (see Table 2), stakeholder participation by youth, family, service providers and outside experts was considerable in Step 1 studies. Concerning game development (RQ3), youth, service providers and Maori, including a Maori game co-creator, Maori computer company and cultural experts, contributed to the design and development of SPARX (79) and co-design workshops that included youth were held. Youth and service provider participation in developing the POD Adventures (97) app was also provided through co-design workshops. Concerning game assessment (RQ4), youth and family provided evaluation and feedback for SPARX (75, 79), while service providers participated in focus groups for POD Adventures (97) where they expressed positive reactions to the narrative format, use of quizzes and rewards, game interactivity and real-life relatability. Testing sessions by youth for POD Adventures were also held, and both games included gameplay. Participation was also very robust for GameSquad (111), where parents served on an advisory team responsible for adapting the intervention (RQ3), in screening study participants as well as participating in gameplay and in coaching sessions with their children (RQ4). A youth exit questionnaire with game assessment was also offered. Involvement ratings in these youth studies were the highest in the review for POD Adventures and SPARX, which both scored 10, a study on Rainbow SPARX scoring 7, while GameSquad scored 3 on user engagement.
Enhanced Ethical Practices (RQ5) were reported for POD Adventures (97) and GameSquad (111). POD Adventures included a risk assessment question for low mood and a plain-language privacy/confidentiality statement for youth participants, while in GameSquad researchers withheld demographic data to protect against inferred identification of the 23 participants with a host of diagnoses.
Processes used in the two young adult games (RQ1) included a randomized clinical trial (121) and a pre-post game assessment (107). Implementation barriers concerned a game design issue affecting the Shots Game (121), in which limited game elements, personalization and a somewhat simplistic storyline resulted in a disappointing game experience. A similar critique about a storyline that did not sustain interest, particularly for males, was directed at Reach Out Central (107), and downloading requirements were also reportedly complicated. Study design/research issues included leaving game “dosage” to player discretion, resulting in a single playthrough for most participants and a shortened intervention period, both of which may have undermined results in Reach Out Central. Authors also expressed reservations about their decision to eliminate the 16-18-year age group, thereby avoiding the requirement for parental consent, after realizing that Reach Out Central had more appeal for younger players.
In terms of Impact (RQ2), players of Reach Out Central (107) showed positive improvement on alcohol use, psychological distress, and coping. Mental health literacy also improved for both sexes. Program satisfaction reached 90% in Reach Out Central (107), whereas in the case of the Shots Game (121), motivation to change (drink less) decreased among players using gamified visual probe training (VPT-G) while increasing among players of the non-gamified version (VTP-R) and the placebo (VPT-P) conditions. Adherence rates were 93.9% for the Shots Game (121) and 57.9% in Reach Out Central (107).
Regarding Engagement (see Table 2), no findings were reported related to stakeholder participation in game development for the young adult games (RQ3). On game assessment (RQ4), Reach Out Central (107) rated youth satisfaction and enjoyment, and both games were played by youth. Involvement ratings for these two studies were Reach Out Central: 3 and the Shots Game: 1, for gameplay only. No findings emerged on Equity or Ethical Practices (RQ5) in the young adult studies.
This largest category of games for mild to moderate mental health conditions included 16 games evaluated in 24/49 studies (49.0%). Five of the eight youth games were therapeutic games: SPARX (76–78, 80–83) for depression or depression/anxiety, SmartCAT (89, 90) for separation, social and general anxiety, Dojo (84) for anxiety/emotion regulation, Minecraft (120) for ADHD and What Happened?! (98) for binge drinking/alcohol use disorder, while two therapeutic games were labeled as adjunct to therapy: Maya (101) for depressive symptomatology and Pesky gNATs (91, 92) [originally called gNATs Island (91)], for low mood, depression or anxiety. There was one educational game, The Journey (108), for depression. The eight games for young adults included six therapeutic games: On Track>The Game (105) for first episode psychosis, PlayMancer (116) for bulimia nervosa, RAW HAND (117) for OCD, Walk in My Shoes (119) for PTSD, e-SMART-MH (106) for depression and OCfree (110) for OCD. One treatment facilitation game, the Cockroach Game (114), addressed specific phobia and a commercial game, Journey (109), depressive symptomatology.
Processes (RQ1) for the 16 youth studies included: seven RCTs (76–78, 83, 84, 98, 108), two open trials (81, 89), one pre-post game assessment (90), two qualitative studies (80, 101), one multiple case study (91), one mixed-method study (92) one study with sequential recall testing (120) and one secondary data analysis (82). Barriers to implementation reflected game design issues, including unspecified technical problems in The Journey (108), lack of personalization in Pesky gNATs (91) and a suspected lack of cultural fit for SPARX (76), delivered in a Dutch intervention study. Study design/research issues included inadequate sample size and high dropout (76), intervention/control games with similar aims that contributed to weaker results (84) and lack of time/resources to include parent participation (80). Regarding staff issues, some therapists reported fears of being “sidelined” by high client interest in the game intervention (91). Offering interventions on class time was a facilitator (76), as were opportunities for game playing alongside therapists in support of therapeutic elements (92).
Study outcomes (impact, effectiveness, sustainability, and equity: RQ2) included, in terms of Impact, significant improvement on key variables in four of the nine games: on depressive symptoms in SPARX (77, 83), depression in The Journey (108), lower anxiety in SmartCAT (89, 90) and memory consolidation in novel environments for ADHD in Minecraft (120). Effectiveness was further demonstrated for SPARX (83), What Happened?! (98) and for SmartCAT (90), which demonstrated significantly higher effectiveness in the gamified vs. non-gamified version of the app (89). On secondary measures, results were equal or better for SPARX vs. treatment as usual on quality of life measures, and in results of the Mood and Feelings scale and Enjoyment and Satisfaction scale (77). User satisfaction scores were high and commentary positive for six games, including SPARX (76–78, 83) and the Rainbow SPARX adaptation for LGB youth (81). The game designs and characters in SPARX enhanced Maori cultural identity, quality of life and hope (80). Among youth who played The Journey (108), 89% liked the game and would recommend it, while similar reactions occurred for users of Pesky gNATs (91). In addition to a 97% satisfaction rating by parents on SmartCAT (90), therapists also weighed in, giving SmartCAT an A+ rating on usability of the clinician portal, and praising Pesky gNATs for promoting therapeutic relationships and helping to transmit CBT concepts (91). One third of therapists endorsed Maya (101), evaluating the game as a sound treatment approach for externalizing emotions and preventing depression as well as a good fit with their therapeutic work. Therapists using Pesky gNATs (92) stated that the children enjoyed the game and responded well to exercises introduced by the characters. Program adherence was reported for 11 studies on the following six games: Minecraft, 94.4% (120); The Journey, 94% (108); Dojo, 93.5% (84); SmartCAT, 88.2% (90) and 85.7% (89); SPARX, 76.4% (78), 70.4% (81), 60% (77) and 30% (76), although adherence decreased gradually to 0% in What Happened?! (98), despite multiple reminders to keep players struggling with binge drinking engaged. Lucassen et al. (82) reported average completion of 4+ modules (“adequate dose”) for only 6% of intersex participants in a 5-year review of SPARX data.
Sustainability (RQ2) was positive in three of the five studies with measurable impact. Remission from depression persisted at follow-up for SPARX (77, 83); 30-day binge drinking was lower at 4-month follow-up for What Happened?! (98) and symptom improvement persisted at 2-month post-treatment for SmartCAT (90). Equity issues were addressed in SPARX, through game adaptations for sexual minority youth (81, 82), indigenous Maori youth in New Zealand (80) and socio-economically disadvantaged youth in rural areas of New Zealand and Australia (76, 83). Researchers also provided equity testing for internet access in What Happened?! (98).
Results on Engagement (see Table 2) reflected considerable stakeholder participation. Youth involvement in game development (RQ3) occurred for SPARX (77), What Happened?! (98), and for youth in conjunction with therapists in SmartCAT (89). Service providers contributed to game development for SPARX (81), while a range of outside experts in psychiatry collaborated in game development and approval of Maya (101). Parents were involved in game assessment (RQ4) for What Happened?!, and in two SPARX studies (76, 83), while service providers assisted with study recruitment for a Dojo study (84). In-study assessments of youth satisfaction or enjoyment were conducted for Pesky gNATs (91), SPARX (76–78, 80, 81, 83), Maya (101), The Journey (108) and SmartCAT (89), while therapists completed in-study game assessments for Pesky gNATs (91, 92) and Maya (101), and parents did the same for SmartCAT (90). All studies involved youth in gameplay, with the exception of one SPARX study with indigenous Maori participants (79). Involvement ratings for games in this group of studies were: SPARX (7 studies, with scores of 10, 7, four studies scored 3, and one study scored 1); SmartCAT (2 studies, scored 7 and 3, respectively); What Happened?!: 5; the following games had scores of 3: Maya, The Journey, Dojo and one of the two studies on Pesky gNATs; while the other scored 1, as did Minecraft.
Regarding Ethical Practices (RQ5), four studies, three of them SPARX interventions (76, 77, 81) and the other for The Journey (108), implemented safety measures and protections in the form of mood-monitoring questions, safety checks and referrals for high depression/anxiety or risk of self-harm, while two studies involving Dojo (84) and What Happened?! (98) provided written assurance that participant data would not be shared. In a SPARX trial, all students in one setting played the game so that study participants could not be singled out (83).
Processes (RQ1) used in these eight studies included two RCTs (106, 109), one clinical trial (110), two pre-post game assessments (117, 119), one mixed method study (105) and two single case studies (114, 116). The one barrier to study implementation involved a study design/research issue around burdensome travel requirements to the study site that affected recruitment and study feasibility (106).
Outcomes on young adult games for mild-moderate conditions (RQ2) included Impact, with five interventions showing significant improvement on their main variables: attitudes toward recovery in On Track>The Game (105), game feasibility (vs. controls) in e-SMART-MH (106), less binge eating in PlayMancer (116), on reaction scores and video game self-efficacy and attitudes toward the game for Walk in My Shoes (119) and on fear/avoidance in the Cockroach Game (114) for which Effectiveness was also demonstrated. The mobile CBT intervention, OCfree (110), demonstrated equal effectiveness as offline CBT for treating OCD, whereas the commercial game, Journey (109), had no effect on depressive symptoms, which persisted for 50.2% of players at follow-up. No results on secondary variables were reported. User satisfaction scores were 3.5/5 for OCfree, with 70% of participants recommending the game. The Cockroach Game (114) and On Track>The Game (105) for first episode psychosis were rated as very helpful, the latter praised for enhancing recovery, hope and treatment confidence, and for game interactivity and customization. Design elements eliciting user dissatisfaction were lack of self-tailoring in e-SMART-MH (106). Adherence rates were reported for two games only: OCfree, 91.4% (110) and e-SMART-MH, 46.7% (106). The single patient using the Cockroach Game was able to play daily with decreasing anxiety (114). Regarding Sustainability, two single case studies, the Cockroach Game (114) and PlayMancer (116), showed that gains were maintained or improved at 12-month follow-up. Two other studies noted a willingness of participants to continue using digital games post-trial (106, 110). Regarding Equity, two US studies prioritized recruitment of ethnic minorities (African American, Hispanic, mixed-race individuals) (105, 106).
Regarding Engagement (see Table 2), no young adult studies at Steps 2-3 reported on stakeholder involvement in game development (RQ3), whereas four studies reported on in-study user satisfaction, acceptability or other game assessments (RQ 4): On Track>The Game (105), e-SMART-MH (106), OCfree (110), and Journey (109). There was no participation in the other four young adult studies, but gameplay was recorded for the Cockroach Game (114), PlayMancer (116), RAW HAND (117), and Walk in My Shoes (119). Based on the criteria given in Table 2, involvement ratings for five of these studies were evaluated as 3: On Track>The Game, e-SMART-MH, Dojo, Journey, and OCfree, while the remaining four studies counted gameplay but no participation and were each rated 1. Only one study commented on Ethical Practices (RQ5). Virtual reality exposure to phobia, as described in the Cockroach Game, was considered more ethical than in vivo exposure which purposefully evokes distress in patients (114).
Seven games (9/49 studies: 18.4%) were played by youth with severe mental illness in residential institutions or inpatient/outpatient psychiatry units. They included four therapeutic games: The SIMS Life StoriesTM (113) for trauma, SPARX (74) for depression, Muse (112) for trauma and RAGE-Control for anger management (102); two relapse prevention games: Arise (99) for substance use disorder and Recovery Warrior (87, 88) for substance use disorder including opioid or marijuana use disorder, and a biofeedback game, Dojo (85, 86), that was used as adjunct to therapy.
Processes (RQ1) involved a full range of methodologies: three RCTs (86, 87, 112), one open trial (74), two pre-post game assessments (85, 88), one pilot survey (99), one qualitative study (113), and one single case study (102). Barriers to implementation included study design/research issues, e.g., lack of time and space in research settings, competing house/ward activities and illness acuity among participants (74, 113). Recruitment of patients with addiction was especially challenging due to a short time frame that did not allow for rolling enrollment and the inability to reach out directly to a small subpopulation of potential participants. They had to be recruited through providers, whose support was crucial, due to the sensitive nature of data being collected. Participants were later contacted through anonymous email accounts and phone (99). Implementation issues also emerged, as time constraints precluded some residential staff from involvement in research (113).
Study outcomes (RQ2) included game impact, effectiveness, sustainability, and equity. On Impact, significant positive associations were identified on key variables for three of the seven games: abstinence from drugs in Recovery Warrior (88), anxiety and externalizing behavior in Dojo (86) and post-traumatic symptoms and stress, anxiety, aggression and depression in Muse (112). Effectiveness was demonstrated for Dojo and Muse in youth residential settings (85, 86, 112), as well as strong acceptability ratings by youth and providers for SPARX (74) and Arise (99); strong four-week, self-efficacy scores on resistance to marijuana and 44.4% abstinence with Recovery Warrior (88), and lower pre-post scores on anxiety and aggressive behavior with Dojo (85, 86). On user satisfaction, acceptability and enjoyment, also part of Effectiveness, all nine studies reported positive results: social workers viewed The SIMS Life StoriesTM (113) as a good tool for engaging residents in therapeutic work and building therapeutic relationships, while several games were viewed by players as especially useful or helpful: SPARX (74), RAGE-Control (102), Arise (99), and Dojo (85, 86). Muse was enjoyed more and had a stronger treatment effect for male vs. female players (112). Moreover, study adherence, measured as program completion rates, was reported for seven studies that tested six games, as follows: Arise, 100% (99); Dojo, 90% (86), Recovery Warrior, 80% (87) and 66.7% (88); Muse, 77.7% (112), The SIMS Life StoriesTM, 36.7% (113) and SPARX 10.0% (74). Regarding Sustainability, of the studies showing positive results, gains were not sustained at follow-up for Recovery Warrior (87), Muse (112) or for one study with Dojo (86). Equity, the final outcome measure, was largely neglected in Step 4 studies, although one study noted the need to personalize videogames for race, different socioeconomic contexts and literacy issues (99).
Regarding Engagement data for Step 4 (see Table 2), neither youth nor family involvement in game development occurred, but a five-member consultation board of addiction experts evaluated and revised an early prototype of Arise (99) (RQ3). On game evaluation (RQ4), residential social workers who delivered the The SIMS Life Stories™ (113) intervention completed semi-structured interviews, while Arise (99) included service provider and youth satisfaction ratings, the latter also rated for several other games: RAGE-Control (102), Dojo (85, 86), Muse (112), and SPARX (74). Ratings of 3 for youth involvement were calculated for six of the seven games, as follows: Arise, The SIMS Life StoriesTM, RAGE-Control, Muse, SPARX and both studies on Dojo; Recovery Warrior scored 1.
Finally, on Ethical Practices, potential harms related to gaming disorder (RQ5) and mitigation strategies were not specifically addressed in Step 4 studies. However, rules against playing games without a defined mental health benefit in one institution for youth with complex trauma seemed to reflect this concern, obliging researchers to provide both TAU and Muse (112) to the intervention group. Study ethics protocols did include some important protections for vulnerable participants, however, like restricting data-sharing with parents and clinicians (99), private data storage and reinstatement of trauma therapy for vulnerable youth prior to the follow-up period (112). Authors of the RAGE-Control intervention cited an opinion that digital game interventions could potentially substitute for seclusion practices or use of restraints to control aggressive behavior (102).
There were no games for young adults at Step 4.
All studies in the review were primary studies, representing substantial methodological variation (e.g., RCTs and clinical trials, pre-post game assessments, mixed methods, qualitative studies, and a number of single studies using other methods). The quality assessment was limited to RCTs, of which five were rated as “fair” (77, 78, 108, 109, 111) and the remainder “poor.” Methodological issues included lack of blinding of participants and outcome assessors, lack of treatment allocation concealment, small sample sizes, low adherence, loss to follow-up and lack of avoidance of other treatments. For most studies, the randomization methods used, power calculations, reasons for loss to follow-up and low adherence were underreported (see Quality Rating Table, Appendix 4 in Supplementary Material).
This “gaming my way to recovery” review aimed to identify the existing literature on digital game interventions targeting young people with a full range of mental health and substance use problems. According to an international 2021 review on digital games (123), game-based interventions exist for most of the disorders identified in psychiatry, but in various experimental stages. We identified and undertook an exhaustive review of 49 studies concerned with 32 relevant games and, using the new Stepped Care Model for Videogame Interventions, mapped the evidence on the overall aims of game interventions, how they have been implemented, evaluated, and supported through stakeholder participation, and whether using gamified interventions in youth mental health services revealed any harms.
The distribution of the 49 studies across the Model reveals that nearly half, 24 studies (49.0%) evaluated games for mild-moderate mental health problems (Steps 2-3: 16 games), followed by 10 studies (20.4%) for games promoting mental health wellness and education among undiagnosed youth (Step 0: 7 games); nine studies (18.4%) on youth games for severe mental illness or substance use disorder (Step 4: 7 games) and six studies (12.2%) for at-risk groups or suspected mental health problems (Step 1: 5 games). Recent international interest in developing digital games for youth is reflected in the broad geographic scope of this literature across 12 countries. Games are being developed to address rising rates of mental health problems among young people, particularly since the pandemic (7, 10, 124–126) as well as low service use (17, 18). Nearly twice as many games in this review targeted youth, compared with games for young adults (65.7 vs. 34.3%). Authors of 11 games made specific efforts to promote equity and inclusiveness, most focusing on ethnic, racial, and sexual minority youth and those living poor, rural, or underserved areas who receive little help or mental health treatment. Such efforts may extend the reach of mental health interventions, while enhancing the “appealing potential” of videogames as a treatment delivery vehicle (34). As noted, SPARX was by far the most studied (10 studies) and disseminated intervention, reaching three countries beyond New Zealand, as well as the only game implemented across all levels of illness severity (Steps 1, 2-3, and 4).
Digital game interventions are effective and may have added value for youth followed in mental health services. The overall strength of the evidence in this review is suggested by the number of studies with measurable outcomes (n = 38: 77.6%). They include 18 (36.7%) randomized studies with control/comparison groups (13 RCTs, four randomized clinical trials and a between-groups experimental design) and 20 (40.8%) uncontrolled quantitative or mixed method studies (11 pre-post game assessments, three open trials, one structural equation model, one mixed method study, two pilot surveys and two studies using sequential recall testing). The remaining 11 studies (22.4%), consisting of six qualitative studies, three single case and one multiple case study, and a five-year, secondary data analysis, amplified the findings especially in terms of user satisfaction and acceptability and in describing barriers and facilitators related to implementation of the games.
Regarding specific outcomes, two-thirds of the 38 quantitative studies reported significant improvement on one or more key variables, and 12 studies described effectiveness on some or all comparisons. Further positive results emerged on secondary variables for SPARX (Steps 2-3) on quality of life, life satisfaction and mood, and for Aislados (Step 0) on improved affect and mental health among participants. Regarding sustainability, the reported gains carried over to the follow-up period in eight studies: Arise, The SIMS Life StoriesTM, and Dojo (Step 4) and for SPARX, What Happened?!, SmartCAT, PlayMancer and the Cockroach Game (Steps 2-3). As well, 18 studies (36.7%) measured or described user satisfaction, with better than average ratings on all studies and positive results from the qualitative data. Program adherence, another possible indicator of user satisfaction, was reported for 28/49 (57.1%) of studies in the review. While previous research reported low study adherence for digital mental health interventions (29, 127–129), average study retention for videogame interventions in this review was 64.5%. Our results compared favorably with a meta-analysis on adherence in gamified interventions for 61 interventions reported as 54.0% (SD: 24.6%) and where considerable variation was identified based on a number of specific gaming features (130).
Another promising aspect of these 32 games for possible adaptation to mental health settings and further testing was that nearly all were serious games. Steps 1-4 for young people with mental illness or symptomatology included 15 therapeutic games and two described as treatment facilitation games, two relapse prevention games, one cognitive retraining game, five games specifically developed as adjunct to therapy including four using biofeedback, and three educational games. Previous research suggested that the game environment itself may promote engagement, as players have access to a stimulating learning environment that facilitates knowledge acquisition, behavior change through repeated rehearsal of new behaviors, emotional control, and social learning (131–133). Moreover, the addition of a Step 0 in the new Stepped Care Model for Videogame Interventions recognizes the contribution of studies geared toward mental wellness and education for undiagnosed young people at large, with 10 studies carried out in schools or university settings, or at home.
Unfortunately, not all videogame interventions offered a rich and interactive game experience, which seems to have impacted on the effective implementation of certain interventions. Game-related issues ranged from disappointing game experiences due to limited game elements, storylines or game menus and lack of personalization or cultural fit, to the quality of therapeutic relationships or lack of therapist support (i.e., self-help formats), to technical glitches. Such problems may have provoked drop-off from gameplay or affected study results. Barriers to implementation also included issues around study design/research and equity, the former related to recruitment of hard-to-reach participants, e.g., those who used drugs, insufficient doses of the game, or active control groups with aims comparable to those of the intervention, which weakened study results. When intensity of gameplay (number of sessions) was left to player discretion in one study (107), most played the game only once providing insufficient data for analysis. Other barriers concerned staff (Step 4) for whom time constraints prevented active involvement in research, and certain therapists who feared being “sidelined” by patient interest in videogames (91). Finally, material resources were sometimes lacking, such as local internet infrastructure in remote or poor areas, limiting game use.
The identified barriers in these studies suggest possible improvements for building game capacity. Use of the Collaboration on Maximizing the impact of E-therapy and Serious Gaming (COMETS) framework (132) could help improve videogame interventions, the player's experience and overall impact of the mental health intervention in naturalistic settings. The COMETS framework is based on four pillars for change: (1) user-centered approaches, including both user-centered program designs and individualization within programs; (2) engagement of the player using processes such as gaming and gamification; (3) active collaboration in program development, testing, and data sharing across both the mental health and industry sectors in order to achieve higher quality, more sustainable outcomes with greater reach and decreased costs of developing interventions to be shared across sectors; and (4) rapid testing and implementation, including rapid research designs and implementation planning as well as measurements for reach, engagement, effectiveness and timeliness of game implementation, to ensure that interventions ready for use will retain their appeal.
The Engagement construct in the Stepped Care Model for Videogame Interventions brought together results for participation by youth, family, and service providers, as well as outside experts who were involved in various aspects of game development, evaluation, study implementation and testing. Studies in the review presented these results both in narrative form and as measurable results, leading to the development of Table 2, which synthesizes these findings across four levels, based on the adapted Ladder of Children's Participation (70). While engagement by all stakeholder groups is described in Table 2, the “involvement” score calculated for each game was based on the cumulative scores for youth engagement only, recognizing their predominant role as primary end-users of the games. While gameplay may not be viewed as “engagement,” the scores for gameplay by youth in the context of study participation were included as a key element of their involvement. In the seven studies reporting on the four highest scoring games: SPARX, POD Adventures, SmartCAT, and What Happened?!, the elevated scores on youth participation reflected greater inclusion of youth in game design and development (score: 4) and in consultation activities (score: 3). Four of these studies tested the SPARX intervention, revealing scale-up of the game through adaptations for indigenous Maori, sexual minority, and socioeconomically deprived youth, as well as diffusion of the game beyond New Zealand. The next group of 25 studies evaluated 17 new games (8 repeats) with a score of 3, as these games were informed by data on youth experience, acceptability, or user satisfaction. Finally, 17 studies that tested 11 games (six repeats) found no evidence of youth participation, but were rated 1 each for gameplay (see also Study Data file, Appendix 2 in Supplementary Material).
With nearly one third of games in the review (see Table 2 for full results) showing no evidence of any youth participation and only four with intense engagement by youth in initial stages of game design and development, awareness about the importance of youth participation in videogame creation is clearly lacking. Research on therapeutic games in mental health has shown that involving young service users early in the design process through participatory and user-centered approaches produces better game mechanics and enhances user engagement in both games and the treatments they support (45). As well, several frameworks and models are available to guide and monitor patient engagement in treatment and research (134–138). Promoting patient engagement in treatment is essential, helping them to develop greater awareness of their mental health conditions, activate self-management behaviors and gain greater control over their treatment and recovery journeys. Moreover, patient engagement in research, including videogame implementation studies, promotes the development of better interventions tailored to the needs of service users.
All the articles reviewed met standard ethical requirements and were screened by institutional research ethics boards. More than 25% featured enhanced ethical practices, including safeguards against risks of high depression/anxiety or self-harm. Other benefits included providing written assurance to youth participants that their data would not be shared or inviting all students in school settings to participate in research so that study participants with depressive symptoms would not be singled out. One study noted that digital games could substitute for use of seclusion and restraints to control aggressive behavior (102), while another promoted virtual reality exposure to specific phobia as less distressing and more ethical than in vivo exposure (114).
Remarkably, the literature under review was almost completely silent on the pivotal question of whether digital game interventions may be associated with gaming disorder or related harms. In a qualitative study, one therapist cautioned against allowing youth already addicted to videogames to use videogame interventions in therapy (101), while another study described an injunction against gameplay with no defined mental health benefit in an institution for traumatized youth, seemingly to prevent overuse of games by residents (112). A partial explanation for the lack of attention to possible addiction in applied games for mental health may relate to their serious therapeutic purposes, as described above, such as symptom reduction, treatment facilitation or support, education or cognitive retraining. As well, digital games have been used effectively to treat symptoms in a variety of mental health conditions ranging from depression and anxiety, PTSD, autism spectrum disorder and ADHD to alcohol use disorder (34, 38, 139). Yet another explanation may be that digital games have become such an integral part of everyday life that therapists no longer consider them to be any more addictive than other daily activities and hobbies such as exercising, watching tv shows, reading, etc. Nor did the two commercial games in this review suggest a particular risk of overuse or addiction. Journey (109) showed no effectiveness in preventing depression and player engagement was low (109). The other, a therapeutic adaptation of a commercially available game, The SIMS Life StoriesTM (113), was viewed by residential social workers as a potentially useful tool in individual therapy with youth affected by complex trauma. As such, use of these commercial games, where user engagement in therapeutic work was low or challenging, suggested little, if any, risk of gaming addiction.
Several limitations of this study should be acknowledged. Regarding the research process, some relevant studies may have been overlooked, particularly non-English studies, despite a thorough database search and screening by two teams of two reviewers. Second, while the methodological procedures were thorough and results included mainly positive outcomes, some findings like those on study effectiveness were based mainly on descriptive rather than statistical data. User satisfaction, the other measure suggesting effectiveness and assessed with both quantitative scales and open questions, was high. Third, regarding study retention, it should be acknowledged that other factors may have affected program adherence or attrition in this review, including participant issues external to the research. Finally, and most important, were limitations associated with the stepped care framework. While the new Stepped Care Model for Videogame Interventions seeks to establish a comprehensive, rigorous, and consistent process for describing and evaluating studies, a lack of detail in the selected studies forced a merger of “mild” and “moderate” mental health conditions into a Step 2-3 and prevented us from adapting elements from a staging model in developing this model. Moreover, stepped care models are often based on intervention levels, not severity levels, in mental health and the criteria for “stepping up/down” are not clearly established. As well, a “Step 0,” or “no-diagnosis” level had to be created to account for studies focused on mental wellness and education. Moreover, data gathered from published articles does not provide a comprehensive view of the intervention, nor is the information provided by authors on their research process always complete. Studies in this review may have contained important data not captured by the model or inadvertently omitted, for example, information on levels of service, integrated services, or continuity of care. Not least, authors may possibly disagree with how data from their studies were categorized or interpreted.
What could be viewed potentially as exceptions to the study inclusion criteria should be explained: two studies using commercial games were included in the review, as they were both used for therapeutic purposes (one game for depression management and the other as adjunct to emotion regulation treatment); five youth studies were included even though the lower participant age limit was <12 because the mean ages met the inclusion criteria set for this study. The exceptions were two studies of the same game (SmartCAT) where the mean age (11.19) was slightly lower. For the other three cases the mean ages were within the prescribed age range of the review. Finally, the GameSquad study, a series of exergames promoting wellness among youth, was retained as more than half of participants had ADHD, and 26% had anxiety disorders and/or depression.
This review provides an initial categorization of digital game interventions for youth and young adults appropriate to different levels of severity (Steps) and a broad range of diagnoses in mental health and substance use disorder. The benefits and limitations of various interventions for specific diagnoses need to be better understood and further testing is required. Future research should include a meta-analysis comparing the efficacy of digital game interventions as well as analyses of game effectiveness in relation to stakeholder engagement and other outcomes, based on well-controlled studies. Moreover, research needs to focus more on participation by young users to improve engagement with the games, and, crucially, on eliciting participation by service providers and family to promote the transformation of stand-alone digital game interventions into standard tools for mental health treatment in clinical and community settings (schools and home) for youth. Opportunities for blending digital and face-to-face treatment should also be explored (140). Potential harms in the therapeutic use of digital games need to be better understood and more research is needed to unpack the complexity of gaming disorder, deeply rooted in the relationship between the user and the digital technology, and to find a proper framework that promotes safety in the use of digital interventions, particularly videogame interventions (51). The evidence on safety and effectiveness of games destined for clinical practice needs to be clearly established and the persuasive components of games, both ethical and transparent, with full control given to the user. Frameworks like COMETS that prioritize patient engagement in treatment and research can offer valuable tools to overcome multiple barriers related to the uptake of digital game interventions.
The original contributions presented in the study are included in the article/Supplementary Material. Further inquiries can be directed to the corresponding author.
MF, JS, SM, SF, and SMHS completed screening and data extraction. MF, JS, and SM analyzed the data. MF and JS wrote the first draft of the manuscript. All authors designed the study. All authors contributed to the interpretation and subsequent edits of the manuscript.
This study was supported by a combination of grants from Frayme, International Knowledge Translation Platform, Ottawa, Ontario, Canada, the Healthy Brains, Healthy Lives (HBHL) New Recruit Start-Up Supplements Award (MF), and the Fonds de Recherche du Québec–chercheurs-boursiers Junior 1 Award (grant no. 283375) (MF).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fdgth.2022.814248/full#supplementary-material
ADHD, Attention-deficit/hyperactivity disorder; CBT, Cognitive behavioral therapy; OCD, Obsessive compulsive disorder; PRISMA, Preferred Reporting Items for Systematic Reviews; PTSD, Post-traumatic stress disorder; RCT, Randomized controlled trial; RQ, research question.
1. Burns JM, Birrell E, Bismark M, Pirkis J, Davenport TA, Hickie IB, et al. The role of technology in Australian youth mental health reform. Aust Health Rev. (2016) 40:584–90. doi: 10.1071/AH15115
2. Dalsgaard S, Thorsteinsson E, Trabjerg BB, Schullehner J, Plana-Ripoll O, Brikell I, et al. Incidence rates and cumulative incidences of the full spectrum of diagnosed mental disorders in childhood and adolescence. JAMA Psychiatry. (2020) 77:155–64. doi: 10.1001/jamapsychiatry.2019.3523
3. McGrath JJ, Saha S, Al-Hamzawi AO, Alonso J, Andrade L, Borges G, et al. Age of onset and lifetime projected risk of psychotic experiences: cross-national data from the world mental health survey. Schizophr Bull. (2016) 42:933-41. doi: 10.1093/schbul/sbw011
4. Miche M, Hofer PD, Voss C, Meyer AH, Gloster AT, Beesdo-Baum K, et al. Mental disorders and the risk for the subsequent first suicide attempt: results of a community study on adolescents and young adults. Eur Child Adolesc Psychiatry. (2018) 27:839-48. doi: 10.1007/s00787-017-1060-5
5. Sullivan SA, Kounali D, Cannon M, David AS, Fletcher PC, Holmans P, et al. A population-based cohort study examining the incidence and impact of psychotic experiences from childhood to adulthood, and prediction of psychotic disorder. Am J Psychiatry. (2020) 177:308-17. doi: 10.1176/appi.ajp.2019.19060654
6. World Economic Forum. A Global Framework for Youth Mental Health: Investing in Future Mental Capital for Individuals, Communities and Economies. Geneva: World Economic Forum (2020).
7. Hawke LD, Barbic SP, Voineskos A, Szatmari P, Cleverley K, Hayes E, et al. Impacts of COVID-19 on youth mental health, substance use, and well-being: a rapid survey of clinical and community samples: répercussions de la COVID-19 sur la santé mentale, l'utilisation de substances et le bien-être des adolescents : un sondage rapide d'échantillons cliniques et communautaires. Can J Psychiatry. (2020) 65:701-9. doi: 10.1177/0706743720940562
8. Merry SN, Cargo T, Christie G, Donkin L, Hetrick S, Fleming T, et al. Debate: Supporting the mental health of school students in the COVID-19 pandemic in New Zealand - a digital ecosystem approach. Child Adolesc Ment Health. (2020) 25:267-9. doi: 10.1111/camh.12429
9. O'Reilly A, Tibbs M, Booth A, Doyle E, McKeague B, Moore J. A rapid review investigating the potential impact of a pandemic on the mental health of young people aged 12-25 years. Ir J Psychol Med. (2020) 2020:1-16. doi: 10.1017/ipm.2020.106
10. Schmitz N, Holley P, Meng X, Fish L, Jedwab J. COVID-19 and depressive symptoms: a community-based study in Quebec, Canada. Can J Psychiatry. (2020) 65:733-5. doi: 10.1177/0706743720943812
11. MacDonald K, Fainman-Adelman N, Anderson KK, Iyer SN. Pathways to mental health services for young people: a systematic review. Soc Psychiatry Psychiatr Epidemiol. (2018) 53:1005-38. doi: 10.1007/s00127-018-1578-y
12. Gulliver A, Griffiths KM, Christensen H. Perceived barriers and facilitators to mental health help-seeking in young people: a systematic review. BMC Psychiatry. (2010) 10:113. doi: 10.1186/1471-244X-10-113
13. Aguirre Velasco A, Cruz ISS, Billings J, Jimenez M, Rowe S. What are the barriers, facilitators and interventions targeting help-seeking behaviours for common mental health problems in adolescents? A systematic review. BMC Psychiatry. (2020) 20:293. doi: 10.1186/s12888-020-02659-0
14. Heflinger CA, Hinshaw SP. Stigma in child and adolescent mental health services research: understanding professional and institutional stigmatization of youth with mental health problems and their families. Adm Policy Ment Health. (2010) 37:61-70. doi: 10.1007/s10488-010-0294-z
15. Nearchou FA, Bird N, Costello A, Duggan S, Gilroy J, Long R, et al. Personal and perceived public mental-health stigma as predictors of help-seeking intentions in adolescents. J Adolesc. (2018) 66:83-90. doi: 10.1016/j.adolescence.2018.05.003
16. Reardon T, Harvey K, Baranowska M, O'Brien D, Smith L, Creswell C. What do parents perceive are the barriers and facilitators to accessing psychological treatment for mental health problems in children and adolescents? A systematic review of qualitative and quantitative studies. Eur Child Adolesc Psychiatry. (2017) 26:623-47. doi: 10.1007/s00787-016-0930-6
17. Auerbach RP, Alonso J, Axinn WG, Cuijpers P, Ebert DD, Green JG, et al. Mental disorders among college students in the World Health Organization World Mental Health Surveys. Psychol Med. (2016) 46:2955-70. doi: 10.1017/S0033291716001665
18. Werlen L, Puhan MA, Landolt MA, Mohler-Kuo M. Mind the treatment gap: the prevalence of common mental disorder symptoms, risky substance use and service utilization among young Swiss adults. BMC Public Health. (2020) 20:1470. doi: 10.1186/s12889-020-09577-6
19. Leech T, Dorstyn DS, Li W. eMental health service use among Australian youth: a cross-sectional survey framed by Andersen's model. Aust Health Rev. (2019) 44:891-7. doi: 10.1071/AH19095
20. Van Meter AR, Birnbaum ML, Rizvi A, Kane JM. Online help-seeking prior to diagnosis: can web-based resources reduce the duration of untreated mood disorders in young people? J Affect Disord. (2019) 252:130-4. doi: 10.1016/j.jad.2019.04.019
21. Pretorius C, Chambers D, Coyle D. Young people's online help-seeking and mental health difficulties: systematic narrative review. J Med Internet Res. (2019) 21:e13873. doi: 10.2196/13873
22. Birnbaum ML, Rizvi AF, Faber K, Addington J, Correll CU, Gerber C, et al. Digital trajectories to care in first-episode psychosis. Psychiatr Serv. (2018) 69:1259-63. doi: 10.1176/appi.ps.201800180
23. Kaess M, Moessner M, Koenig J, Lustig S, Bonnet S, Becker K, et al. A plea for the sustained implementation of digital interventions for young people with mental health problems in the light of the COVID-19 pandemic. J Child Psychol Psychiatry. (2020) 2020: 916-8. doi: 10.1111/jcpp.13317
24. Hollis C, Falconer CJ, Martin JL, Whittington C, Stockton S, Glazebrook C, et al. Annual research review: digital health interventions for children and young people with mental health problems - a systematic and meta-review. J Child Psychol Psychiatry. (2017) 58:474-503. doi: 10.1111/jcpp.12663
25. Lal S, Adair CE. E-mental health: a rapid review of the literature. Psychiatr Serv. (2014) 65:24-32. doi: 10.1176/appi.ps.201300009
26. Lattie EG, Adkins EC, Winquist N, Stiles-Shields C, Wafford QE, Graham AK. Digital mental health interventions for depression, anxiety, and enhancement of psychological well-being among college students: systematic review. J Med Internet Res. (2019) 21:e12869. doi: 10.2196/12869
27. Wozney L, McGrath PJ, Newton AS, Hartling L, Curran J, Huguet A. RE-AIMing e-Mental Health: A Rapid Review of Current Research. Ottawa, ON: Mental Health Commission of Canada (2017).
28. Alvarez-Jimenez M, Alcazar-Corcoles MA, Gonzalez-Blanch C, Bendall S, McGorry PD, Gleeson JF. Online, social media and mobile technologies for psychosis treatment: a systematic review on novel user-led interventions. Schizophr Res. (2014) 156:96-106. doi: 10.1016/j.schres.2014.03.021
29. Garrido S, Millington C, Cheers D, Boydell K, Schubert E, Meade T, et al. What works and what doesn't work? a systematic review of digital mental health interventions for depression and anxiety in young people. Front Psychiatry. (2019) 10:759. doi: 10.3389/fpsyt.2019.00759
30. Grist R, Croker A, Denne M, Stallard P. Technology delivered interventions for depression and anxiety in children and adolescents: a systematic review and meta-analysis. Clin Child Fam Psychol Rev. (2019) 22:147-71. doi: 10.1007/s10567-018-0271-8
31. Pennant ME, Loucas CE, Whittington C, Creswell C, Fonagy P, Fuggle P, et al. Computerised therapies for anxiety and depression in children and young people: a systematic review and meta-analysis. Behav Res Ther. (2015) 67:1-18. doi: 10.1016/j.brat.2015.01.009
32. Abdel-Baki A, Lal S, D-Charron O, Stip E, Kara N. Understanding access and use of technology among youth with first-episode psychosis to inform the development of technology-enabled therapeutic interventions. Early Interv Psychiatry. (2017) 11:72-6. doi: 10.1111/eip.12250
33. Christie GI, Shepherd M, Merry SN, Hopkins S, Knightly S, Stasiak K. Gamifying CBT to deliver emotional health treatment to young people on smartphones. Internet Interv. (2019) 18:100286. doi: 10.1016/j.invent.2019.100286
34. Fleming TM, Bavin L, Stasiak K, Hermansson-Webb E, Merry SN, Cheek C, et al. Serious games and gamification for mental health: current status and promising directions. Front Psychiatry. (2017) 7:215. doi: 10.3389/fpsyt.2016.00215
35. Barnes S, Prescott J. Empirical evidence for the outcomes of therapeutic video games for adolescents with anxiety disorders: systematic review. JMIR Serious Games. (2018) 6:e3. doi: 10.2196/games.9530
36. Cheng VWS, Davenport T, Johnson D, Vella K, Hickie IB. Gamification in apps and technologies for improving mental health and well-being: systematic review. JMIR Ment Health. (2019) 6:e13717. doi: 10.2196/13717
37. Dias LSP, Barbosa JLV, Vianna HD. Gamification and serious games in depression care: A systematic mapping study. Telematics Informat. (2018) 35:213-24. doi: 10.1016/j.tele.2017.11.002
38. Lau HM, Smit JH, Fleming TM, Riper H. Serious games for mental health: are they accessible, feasible, and effective? A systematic review and meta-analysis. Front Psychiatry. (2017) 7:209. doi: 10.3389/fpsyt.2016.00209
39. Li J, Theng YL, Foo S. Game-based digital interventions for depression therapy: a systematic review and meta-analysis. Cyberpsychol Behav Soc Netw. (2014) 17:519-27. doi: 10.1089/cyber.2013.0481
40. Li J, Theng YL, Foo S. Effect of exergames on depression: a systematic review and meta-analysis. Cyberpsychol Behav Soc Netw. (2016) 19:34-42. doi: 10.1089/cyber.2015.0366
41. Granic I, Lobel A, Engels RC. The benefits of playing video games. Am Psychol. (2014) 69:66-78. doi: 10.1037/a0034857
42. Boot WR, Blakely DP, Simons DJ. Do action video games improve perception and cognition? Front Psychol. (2011) 2:226. doi: 10.3389/fpsyg.2011.00226
43. Jackson M. Making visible: using simulation and game environments across disciplines. On Horiz. (2004) 12:22-5. doi: 10.1108/10748120410540463
44. Read JL, Shortell SM. Interactive games to promote behavior change in prevention and treatment. JAMA. (2011) 305:1704-5. doi: 10.1001/jama.2011.408
45. Fitzgerald M, Ratcliffe G. Serious games, gamification, and serious mental illness: a scoping review. Psychiatr Serv. (2020) 71:170-83. doi: 10.1176/appi.ps.201800567
46. Anderson CA, Bushman BJ. Effects of violent video games on aggressive behavior, aggressive cognition, aggressive affect, physiological arousal, and prosocial behavior: a meta-analytic review of the scientific literature. Psychol Sci. (2001) 12:353-9. doi: 10.1111/1467-9280.00366
47. Gentile D, Pathological video-game use among youth ages 8 to 18. Psychol Sci. (2009) 20:594-602. doi: 10.1111/j.1467-9280.2009.02340.x
48. Singh S, Roy D, Sinha K, Parveen S, Sharma G, Joshi G. Impact of COVID-19 and lockdown on mental health of children and adolescents: a narrative review with recommendations. Psychiatry Res. (2020) 293:113429. doi: 10.1016/j.psychres.2020.113429
49. King DL, Delfabbro PH. The concept of “harm” in Internet gaming disorder. J Behav Addict. (2018) 7:562-4. doi: 10.1016/B978-0-12-812924-1.09996-2
50. Saunders JB, Hao W, Long J, King DL, Mann K, Fauth-Buhler M, et al. Gaming disorder: its delineation as an important condition for diagnosis, management, and prevention. J Behav Addict. (2017) 6:271-9. doi: 10.1556/2006.6.2017.039
51. Ferrari M, Schick A. Teenagers, screens and social media: a commentary on Orben's narrative review. Soc Psychiatry Psychiatr Epidemiol. (2020) 55:973-5. doi: 10.1007/s00127-020-01858-0
52. Aarseth E, Bean AM, Boonen H, Colder Carras M, Coulson M, Das D, et al. Scholars' open debate paper on the World Health Organization ICD-11 Gaming Disorder proposal. J Behav Addict. (2017) 6:267-70. doi: 10.1556/2006.5.2016.088
53. Bean A, Neilsen RKL, van Rooij AI, Ferguson CJ. Video game addiction: the push to pathologize video games. Profession Psychol Res Pract. (2017) 48:378-89. doi: 10.1037/pro0000150
54. Malla A, Iyer S, McGorry P, Cannon M, Coughlan H, Singh S, et al. From early intervention in psychosis to youth mental health reform: a review of the evolution and transformation of mental health services for young people. Soc Psychiatry Psychiatr Epidemiol. (2016) 51:319-26. doi: 10.1007/s00127-015-1165-4
55. Malla A, Shah J, Iyer S, Boska P, Joober R, Andersson N, et al. Youth mental health should be a top priority for health care in Canada. Can J Psychiatry. (2018) 63:216-22. doi: 10.1177/0706743718758968
56. McGorry P, Bates T, Birchwood M. Designing youth mental health services for the 21st century: examples from Australia, Ireland and the UK. Br J Psychiatry. (2013) 202:s30-5. doi: 10.1192/bjp.bp.112.119214
57. Power E, Hughes S, Cotter D, Cannon M. Youth mental health in the time of COVID-19. Ir J Psychol Med. (2020) 37:301-5. doi: 10.1017/ipm.2020.84
58. Alvarez-Jimenez M, Rice S, D'Alfonso S, Leicester S, Bendall S, Pryor I, et al. A novel multimodal digital service (moderated online social therapy+) for help-seeking young people experiencing mental ill-health: pilot evaluation within a national youth e-mental health service. J Med Internet Res. (2020) 22:e17155. doi: 10.2196/17155
59. Lee SY, Lee HK, Choo H. Typology of Internet gaming disorder and its clinical implications. Psychiatry Clin Neurosci. (2017) 71:479-91. doi: 10.1111/pcn.12457
60. Rho MJ, Lee H, Lee TH, Cho H, Jung DJ, Kim DJ, et al. Risk factors for internet gaming disorder: psychological factors and internet gaming characteristics. Int J Environ Res Public Health. (2017) 15:40. doi: 10.3390/ijerph15010040
61. Paulus FW, Ohmann S, Von Gontard A, Popow C. Internet gaming disorder in children and adolescents: a systematic review. Dev Med Child Neurol. (2018) 60:645-59. doi: 10.1111/dmcn.13754
62. Butler-Jones D. The Chief Public Health Officer's Report on the State of Public Health in Canada, 2011: Youth and Young Adults - Life in Transition. Ottawa, ON: The Public Health Agency of Canada (2011).
63. Arksey H, O'Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. (2005) 8:19-32. doi: 10.1080/1364557032000119616
64. Ferrari M, McIlwaine SV, Reynolds JA, Archie S, Boydell K, Lal S, et al. Digital game interventions for youth mental health services (gaming my way to recovery): protocol for a scoping review. JMIR Res Protoc. (2020) 9:e13834. doi: 10.2196/13834
65. Levac D, Colquhoun H, O'Brien KK. Scoping studies: advancing the methodology. Implement Sci. (2010) 5:69. doi: 10.1186/1748-5908-5-69
66. Tricco AC, Lillie E, Zarin W, O'Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. (2018) 169:467-73. doi: 10.7326/M18-0850
67. Berger M, Fernando S, Churchill A, Cornish P, Henderson J, Shah J, et al. Scoping review of stepped care interventions for mental health and substance use service delivery to youth and young adults. Early Interv Psychiatry. (2021). doi: 10.1111/eip.13180. [Epub ahead of print].
68. Boyd L, Baker E, Reilly J. Impact of a progressive stepped care approach in an improving access to psychological therapies service: an observational study. PLoS ONE. (2019) 14:e0214715. doi: 10.1371/journal.pone.0214715
69. Wuthrich VM, Rapee RM, McLellan L, Wignall A, Jagiello T, Norberg M, et al. Psychological stepped care for anxious adolescents in community mental health services: a pilot effectiveness trial. Psychiatry Res. (2021) 303:114066. doi: 10.1016/j.psychres.2021.114066
70. Hart RA. Stepping back from “the ladder”: reflections on a model of participatory work with children. In: Reid A, Jensen B, Nikel J, Simovska V, editors. Participation and Learning: Perspectives on Education and the Environment, Health and Sustainability. Heidelberg: Springer. (2008). p. 19-31.
71. McGowan J, Sampson M, Salzwedel DM, Cogo E, Foerster V, Lefebvre C. PRESS peer review of electronic search strategies: 2015 guideline statement. J Clin Epidemiol. (2016) 75:40-6. doi: 10.1016/j.jclinepi.2016.01.021
72. Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan-a web and mobile app for systematic reviews. Syst Rev. (2016) 5:210. doi: 10.1186/s13643-016-0384-4
73. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. (2021) 372:n71. doi: 10.1136/bmj.n71
74. Bobier C, Stasiak K, Mountford H, Merry S, Moor S. When “e” therapy enters the hospital: Examination of the feasibility and acceptability of SPARX (a cCBT programme) in an adolescent inpatient unit. Adv Mental Health. (2013) 11:286-92. doi: 10.5172/jamh.2013.11.3.286
75. Cheek C, Bridgman H, Fleming T, Cummings E, Ellis L, Lucassen MF, et al. Views of young people in rural Australia on SPARX, a fantasy world developed for New Zealand youth with depression. JMIR Serious Games. (2014) 2:e3. doi: 10.2196/games.3183
76. Kuosmanen T, Fleming TM, Newell J, Barry MM. A pilot evaluation of the SPARX-R gaming intervention for preventing depression and improving wellbeing among adolescents in alternative education. Internet Interv. (2017) 8:40-7. doi: 10.1016/j.invent.2017.03.004
77. Merry SN, Stasiak K, Shepherd M, Frampton C, Fleming T, Lucassen MFG. The effectiveness of SPARX, a computerised self-help intervention for adolescents seeking help for depression: randomised controlled non-inferiority trial. BMJ. (2012) 344:e2598. doi: 10.1136/bmj.e2598
78. Poppelaars M, Tak YR, Lichtwarck-Aschoff A, Engels RC, Lobel A, Merry SN, et al. A randomized controlled trial comparing two cognitive-behavioral programs for adolescent girls with subclinical depression: a school-based program (Op Volle Kracht) and a computerized program (SPARX). Behav Res Ther. (2016) 80:33-42. doi: 10.1016/j.brat.2016.03.005
79. Shepherd M, Fleming T, Lucassen M, Stasiak K, Lambie I, Merry SN. The design and relevance of a computerized gamified depression therapy program for indigenous māori adolescents. JMIR Serious Games. (2015) 3:e1. doi: 10.2196/games.3804
80. Shepherd M, Merry S, Lambie I, Thompson A. Indigenous adolescents' perception of an Emental health program (SPARX): exploratory qualitative assessment. JMIR Serious Games. (2018) 6:e13. doi: 10.2196/games.8752
81. Lucassen MF, Hatcher S, Fleming TM, Stasiak K, Shepherd MJ, Merry SN. A qualitative study of sexual minority young people's experiences of computerised therapy for depression. Australas Psychiatry. (2015) 23:268-73. doi: 10.1177/1039856215579542
82. Lucassen MFG, Perry Y, Frampton C, Fleming T, Merry SN, Shepherd M, et al. Intersex adolescents seeking help for their depression: the case study of SPARX in New Zealand. Australas Psychiatry. (2021) 2021:1039856221992642. doi: 10.26686/wgtn.14399240.v1
83. Fleming T, Dixon R, Frampton C, Merry S. A pragmatic randomized controlled trial of computerized CBT (SPARX) for symptoms of depression among adolescents excluded from mainstream education. Behav Cogn Psychother. (2011) 40:529-41. doi: 10.1017/S1352465811000695
84. Scholten H, Malmberg M, Lobel A, Engels RC, Granic I. A Randomized controlled trial to test the effectiveness of an immersive 3D video game for anxiety prevention among adolescents. PLoS ONE. (2016) 11:e0147763. doi: 10.1371/journal.pone.0147763
85. Schuurmans AA, Nijhof KS, Vermaes IP, Engels RC, Granic I. A pilot study evaluating “Dojo,” a videogame intervention for youths with externalizing and anxiety problems. Games Health J. (2015) 4:401-8. doi: 10.1089/g4h.2014.0138
86. Schuurmans AAT, Nijhof KS, Engels R, Granic I. Using a videogame intervention to reduce anxiety and externalizing problems among youths in residential care: an initial randomized controlled Trial. J Psychopathol Behav Assess. (2018) 40:344-54. doi: 10.1007/s10862-017-9638-2
87. Abroms LC, Fishman M, Vo H, Chiang SC, Somerville V, Rakhmanov L, et al. A motion-activated video game for prevention of substance use disorder relapse in youth: pilot randomized controlled trial. JMIR Serious Games. (2019) 7:e11716. doi: 10.2196/11716
88. Abroms LC, Leavitt LE, Van Alstyne JM, Schindler-Ruwisch JM, Fishman MJ, Greenberg D. A motion videogame for opioid relapse prevention. Games Health J. (2015) 4:494-501. doi: 10.1089/g4h.2014.0100
89. Pramana G, Parmanto B, Lomas J, Lindhiem O, Kendall PC, Silk J. Using mobile health gamification to facilitate cognitive behavioral therapy skills practice in child anxiety treatment: open clinical trial. JMIR Serious Games. (2018) 6:e9. doi: 10.2196/games.8902
90. Silk JS, Pramana G, Sequeira SL, Lindhiem O, Kendall PC, Rosen D, et al. Using a smartphone app and clinician portal to enhance brief cognitive behavioral therapy for childhood anxiety disorders. Behav Ther. (2020) 51:69-84. doi: 10.1016/j.beth.2019.05.002
91. Coyle D, McGlade N, Doherty G, O'Reilly G. Exploratory evaluations of a computer game supporting cognitive behavioural therapy for adolescents. ACM CHI. (2011) 2011:2937-46. doi: 10.1145/1978942.1979378
92. van der Meulen H, McCashin D, O'Reilly G, Coyle D. Using computer games to support mental health interventions: naturalistic deployment study. JMIR Ment Health. (2019) 6:e12430. doi: 10.2196/12430
93. David OA, Cardos RAI, Matu S. Is REThink therapeutic game effective in preventing emotional disorders in children and adolescents? Outcomes of a randomized clinical trial. Eur Child Adolesc Psychiatry. (2019) 28:111-22. doi: 10.1007/s00787-018-1192-2
94. David OA, Cardos RAI, Matu S. Changes in irrational beliefs are responsible for the efficacy of the REThink therapeutic game in preventing emotional disorders in children and adolescents: mechanisms of change analysis of a randomized clinical trial. Eur Child Adolesc Psychiatry. (2019) 28:307-18. doi: 10.1007/s00787-018-1195-z
95. David OA, Predatu R, Cardos RAI. Effectiveness of the REThink therapeutic online video game in promoting mental health in children and adolescents. Internet Interv. (2021) 25:100391. doi: 10.1016/j.invent.2021.100391
96. David OA, Predatu RM, Cardo RA-I. A pilot study of the REThink online video game applied for coaching emotional understanding in children and adolescents in the therapeutic video game environment: the feeling better resources game. J Eviden Based Psychother. (2018) 18:57–68. doi: 10.24193/jebp.2018.1.5
97. Gonsalves PP, Hodgson ES, Kumar A, Aurora T, Chandak Y, Sharma R, et al. Design and development of the “POD Adventures” smartphone game: a blended problem-solving intervention for adolescent mental health in India. Front Public Health. (2019) 7:238. doi: 10.3389/fpubh.2019.00238
98. Jander A, Crutzen R, Mercken L, Candel M, de Vries H. Effects of a web-based computer-tailored game to reduce binge drinking among dutch adolescents: a cluster randomized controlled trial. J Med Internet Res. (2016) 18:e29. doi: 10.2196/jmir.4708
99. Sanchez RP, Bartel CM. The feasibility and acceptability of “Arise”: an online substance abuse relapse prevention program. Games Health J. (2015) 4:136-44. doi: 10.1089/g4h.2014.0015
100. Cangas AJ, Navarro N, Parra JMA, Ojeda JJ, Cangas D, Piedra JA, et al. Stigma-stop: a serious game against the stigma toward mental health in educational settings. Front Psychol. (2017) 8:1385. doi: 10.3389/fpsyg.2017.01385
101. Carrasco AE. Acceptability of an adventure video game in the treatment of female adolescents with symptoms of depression. Res Psychother. (2016) 19:10-8. doi: 10.4081/ripppo.2016.182
102. Ducharme P, Wharff E, Hutchinson E, Kahn J, Logan G, Gonzalez-Heydrich J. Videogame assisted emotional regulation training: an ACT with RAGE-control case illustration. Clin Soc Work J. (2012) 40:75-84. doi: 10.1007/s10615-011-0363-0
103. Kelders SM, Sommers-Spijkerman M, Goldberg J. Investigating the direct impact of a gamified versus nongamified well-being intervention: an exploratory experiment. J Med Internet Res. (2018) 20:e247. doi: 10.2196/jmir.9923
104. Li TM, Chau M, Wong PW, Lai ES, Yip PS. Evaluation of a web-based social network electronic game in enhancing mental health literacy for young people. J Med Internet Res. (2013) 15:e80. doi: 10.2196/jmir.2316
105. Olivet J, Haselden M, Piscitelli S, Kenney R, Shulman A, Medoff D, et al. Results from a pilot study of a computer-based role-playing game for young people with psychosis. Early Interv Psychiatry. (2019) 13:767-72. doi: 10.1111/eip.12556
106. Pinto MD, Greenblatt AM, Hickman RL, Rice HM, Thomas TL, Clochesy JM. Assessing the critical parameters of eSMART-MH: a promising avatar-based digital therapeutic intervention to reduce depressive symptoms. Perspect Psychiatr Care. (2016) 52:157-68. doi: 10.1111/ppc.12112
107. Shandley K, Austin D, Klein B, Kyrios M. An evaluation of 'Reach Out Central': an online gaming program for supporting the mental health of young people. Health Educ Res. (2010) 25:563-74. doi: 10.1093/her/cyq002
108. Stasiak K, Hatcher S, Frampton C, Merry SN. A pilot double blind randomized placebo controlled trial of a prototype computer-based cognitive behavioural therapy program for adolescents with symptoms of depression. Behav Cogn Psychother. (2014) 42:385-401. doi: 10.1017/S1352465812001087
109. Poppelaars M, Lichtwarck-Aschoff A, Otten R, Granic I. Can a commercial video game prevent depression? null results and whole sample action mechanisms in a randomized controlled trial. Front Psychol. (2021) 11:575962. doi: 10.3389/fpsyg.2020.575962
110. Hwang H, Bae S, Hong JS, Han DH. Comparing effectiveness between a mobile app program and traditional cognitive behavior therapy in obsessive-compulsive disorder: evaluation study. JMIR Ment Health. (2021) 8:e23778. doi: 10.2196/23778
111. Bowling AB, Slavet J, Hendrick C, Beyl R, Nauta P, Augustyn M, et al. The adaptive gamesquad xbox-based physical activity and health coaching intervention for youth with neurodevelopmental and psychiatric diagnoses: pilot feasibility study. JMIR Form Res. (2021) 5:e24566. doi: 10.2196/24566
112. Schuurmans AAT, Nijhof KS, Scholte R, Popma A, Otten R. Effectiveness of game-based meditation therapy on neurobiological stress systems in adolescents with posttraumatic symptoms: a randomized controlled trial. Stress. (2021) 2021:1-8. doi: 10.1080/10253890.2021.1998444
113. Aventin Á, Houston S, Macdonald G. Utilising a computer game as a therapeutic intervention for youth in residential care: Some preliminary findings on use and acceptability. Children Youth Serv Rev. (2014) 47:362-9. doi: 10.1016/j.childyouth.2014.10.012
114. Botella C, Breton-López J, Quero S, Baños RM, García-Palacios A, Zaragoza I, et al. Treating cockroach phobia using a serious game on a mobile phone and augmented reality exposure: a single case study. Comput Hum Behav. (2011) 27:217-27. doi: 10.1016/j.chb.2010.07.043
115. Cejudo J, Losada L, Feltrero R. Promoting social and emotional learning and subjective well-being: impact of the “Aislados” intervention program in adolescents. Int J Environ Res Public Health. (2020) 17:609. doi: 10.3390/ijerph17020609
116. Fagundo AB, Via E, Sanchez I, Jimenez-Murcia S, Forcano L, Soriano-Mas C, et al. Physiological and brain activity after a combined cognitive behavioral treatment plus video game therapy for emotional regulation in bulimia nervosa: a case report. J Med Internet Res. (2014) 16:e183. doi: 10.2196/jmir.3243
117. Hong JS, Kim SM, Aboujaoude E, Han DH. Investigation of a mobile “serious game” in the treatment of obsessive-compulsive disorder: a pilot study. Games Health J. (2018) 7:317-26. doi: 10.1089/g4h.2017.0158
118. Huen JM, Lai ES, Shum AK, So SW, Chan MK, Wong PW, et al. Evaluation of a digital game-based learning program for enhancing youth mental health: a structural equation modeling of the program effectiveness. JMIR Ment Health. (2016) 3:e46. doi: 10.2196/mental.5656
119. Kreutzer CP, Bowers CA. Attitudes toward a game-based approach to mental health. Cyberpsychol Behav Soc Netw. (2015) 18:20-4. doi: 10.1089/cyber.2014.0382
120. Baumann V, Birnbaum T, Breitling-Ziegler C, Tegelbeckers J, Dambacher J, Edelmann E, et al. Exploration of a novel virtual environment improves memory consolidation in ADHD. Sci Rep. (2020) 10:21453. doi: 10.1038/s41598-020-78222-4
121. Boendermaker WJ, Sanchez Maceiras S, Boffo M, Wiers RW. Attentional bias modification with serious game elements: evaluating the shots game. JMIR Serious Games. (2016) 4:e20. doi: 10.2196/games.6464
122. Mullor D, Sayans-Jimenez P, Cangas AJ, Navarro N. Effect of a serious game (stigma-stop) on reducing stigma among psychology students: a controlled study. Cyberpsychol Behav Soc Netw. (2019) 22:205-11. doi: 10.1089/cyber.2018.0172
123. Vajawat B, Varshney P, Banerjee D. Digital gaming interventions in psychiatry: evidence, applications and challenges. Psychiatry Res. (2021) 295:113585. doi: 10.1016/j.psychres.2020.113585
124. Racine N, Cooke JE, Eirich R, Korczak DJ, McArthur B, Madigan S. Child and adolescent mental illness during COVID-19: a rapid review. Psychiatry Res. (2020) 292:113307. doi: 10.1016/j.psychres.2020.113307
125. Wiens K, Bhattarai A, Pedram P, Dores A, Williams J, Bulloch A, et al. A growing need for youth mental health services in Canada: examining trends in youth mental health from 2011 to 2018. Epidemiol Psychiatr Sci. (2020) 29:e115. doi: 10.1017/S2045796020000281
126. Leeb RT, Bitsko RH, Radhakrishnan L, Martinez P, Njai R, Holland KM. Mental health-related emergency department visits among children aged <18 years during the COVID-19 pandemic - United States, January 1-October 17, 2020. Morb Mortal Week Rep. (2020) 69:1675-80. doi: 10.15585/mmwr.mm6945a3
127. Wozney L, Huguet A, Bennett K, Radomski AD, Hartling L, Dyson M, et al. How do eHealth programs for adolescents with depression work? A realist review of persuasive system design components in internet-based psychological therapies. J Med Internet Res. (2017) 19:e266. doi: 10.2196/jmir.7573
128. Fleming T, Bavin L, Lucassen M, Stasiak K, Hopkins S, Merry S. Beyond the trial: systematic review of real-world uptake and engagement with digital self-help interventions for depression, low mood, or anxiety. J Med Internet Res. (2018) 20:e199. doi: 10.2196/jmir.9275
129. Valimaki M, Anttila K, Anttila M, Lahti M. Web-based interventions supporting adolescents and young people with depressive symptoms: systematic review and meta-analysis. JMIR Mhealth Uhealth. (2017) 5:e180. doi: 10.2196/mhealth.8624
130. Brown M, O'Neill N, van Woerden H, Eslambolchilar P, Jones M, John A. Gamification and adherence to web-based mental health interventions: a systematic review. JMIR Ment Health. (2016) 3:e39. doi: 10.2196/mental.5710
131. Cheek C, Fleming T, Lucassen MF, Bridgman H, Stasiak K, Shepherd M, et al. Integrating health behavior theory and design elements in serious games. JMIR Ment Health. (2015) 2:e11. doi: 10.2196/mental.4133
132. Fleming TM, de Beurs D, Khazaal Y, Gaggioli A, Riva G, Botella C, et al. Maximizing the impact of e-therapy and serious gaming: time for a paradigm shift. Front Psychiatry. (2016) 7:65. doi: 10.3389/fpsyt.2016.00065
133. Oulasvirta A, Rattenbury T, Ma L, Raita E. Habits make smartphone use more pervasive. Pers Ubiquitous Comput. (2012) 16:105-14. doi: 10.1007/s00779-011-0412-2
134. Graffigna G, Barello S, Bonanomi A, Lozza E. Measuring patient engagement: development and psychometric properties of the Patient Health Engagement (PHE) Scale. Front Psychol. (2015) 6:274. doi: 10.3389/fpsyg.2015.00274
135. NHS Department of Health. Equity and Excellence: Liberating the NHS. London: NHS Department of Health (2010).
136. Brett J, Staniszewska S, Mockford C, Herron-Marx S, Hughes J, Tysall C, et al. A systematic review of the impact and outcomes of patient and public involvement on service users, researchers and communities. Patient. (2014) 7:387-95. doi: 10.1007/s40271-014-0065-0
137. Mockford C, Staniszewska S, Griffiths F, Herron-Marx S. The impact of patient and public involvement on UK NHS health care: a systematic review. Int J Qual Health Care. (2012) 24:28-38. doi: 10.1093/intqhc/mzr066
138. Oliver S, Clarke-Jones L, Rees R, Milne R, Buchanan P, Gabbay J, et al. Involving consumers in research and development agenda setting for the NHS: developing an evidence-based approach. Health Technol Assessment. (2004) 8:1-148, III-IV. doi: 10.3310/hta8150
139. Johnson D, Deterding S, Kuhn KA, Staneva A, Stoyanov S, Hides L. Gamification for health and wellbeing: a systematic review of the literature. Internet Interv. (2016) 6:89-106. doi: 10.1016/j.invent.2016.10.002
Keywords: digital games, digital mental health interventions, video games, e-interventions, youth, youth and young adults, scoping review, stepped care
Citation: Ferrari M, Sabetti J, McIlwaine SV, Fazeli S, Sadati SMH, Shah JL, Archie S, Boydell KM, Lal S, Henderson J, Alvarez-Jimenez M, Andersson N, Nielsen RKL, Reynolds JA and Iyer SN (2022) Gaming My Way to Recovery: A Systematic Scoping Review of Digital Game Interventions for Young People's Mental Health Treatment and Promotion. Front. Digit. Health 4:814248. doi: 10.3389/fdgth.2022.814248
Received: 13 November 2021; Accepted: 26 January 2022;
Published: 07 April 2022.
Edited by:
Max V. Birk, Eindhoven University of Technology, NetherlandsReviewed by:
Eduardo L. Bunge, Palo Alto University, United StatesCopyright © 2022 Ferrari, Sabetti, McIlwaine, Fazeli, Sadati, Shah, Archie, Boydell, Lal, Henderson, Alvarez-Jimenez, Andersson, Nielsen, Reynolds and Iyer. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Manuela Ferrari, bWFudWVsYS5mZXJyYXJpQG1jZ2lsbC5jYQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.