
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Digit. Health , 31 October 2022
Sec. Connected Health
Volume 4 - 2022 | https://doi.org/10.3389/fdgth.2022.1010779
This article is part of the Research Topic Highlights in Connected Health 2021/22 View all 7 articles
Background and objectives: Video animations are used increasingly as patient information tools; however, we do not know their value compared to other formats of delivery, such as printed materials, verbal consultations or static images.
Methods: This review compares the effectiveness of video animations as information tools vs. other formats of delivery on patient knowledge, attitudes and cognitions, and behaviours. Included studies had the following features: controlled design with random or quasi-random allocation; patients being informed about any health condition or members of the public being informed about a public health topic; comparing video animation with another delivery format. Multiple digital databases were searched from 1996-June 2021. We also undertook citation searching. We used dual, independent decision-making for inclusion assessment, data extraction and quality appraisal. Included studies were appraised using the Cochrane ROB2 tool. Findings were reported using narrative synthesis.
Results: We included 38 trials, focussed on: explaining medical or surgical procedures (n = 17); management of long-term conditions (n = 11); public health, health-promotion or illness-prevention (n = 10). Studies evaluated cartoon animations (n = 29), 3D animations (n = 6), or 2D animations, “white-board” animations or avatars (n = 1 each). Knowledge was assessed in 30 studies, showing greater knowledge from animations in 19 studies, compared to a range of comparators. Attitudes and cognitions were assessed in 21 studies, and animations resulted in positive outcomes in six studies, null effects in 14 studies, and less positive outcomes than standard care in one study. Patient behaviours were assessed in nine studies, with animations resulting in positive outcomes in four and null effects in the remainder. Overall risk of bias was “high” (n = 18), “some concerns” (n = 16) or “low” (n = 4). Common reasons for increased risk of bias were randomisation processes, small sample size or lack of sample size calculation, missing outcome data, and lack of protocol publication.
Discussion: The overall evidence base is highly variable, with mostly small trials. Video animations show promise as patient information tools, particularly for effects on knowledge, but further evaluation is needed in higher quality studies.
Systematic Review Registration: https://www.crd.york.ac.uk/prospero/display_record.php?, identifier: CRD42021236296.
Easy access to the internet has made online and digital health communication both possible and attractive, and many people consider the internet a valuable tool for finding health information (1–3). This in turn has generated opportunities for the use of multimedia in delivering health information to patients, which may provide benefits both for patients and healthcare providers.
Traditionally, information has been provided to patients through face-to-face clinical consultation, information leaflet (with or without images) or, in the case of some public health issues, short TV film. However, patients do not always understand what is being explained to them, perhaps due to cultural and educational gaps between clinicians and patients (4). This problem is especially relevant for people with low health literacy. This group of people find some health-related information difficult to understand and research suggests that a “high information burden” could actually discourage them from taking part in assessments of their health, such as screening (5).
The application of new technologies to patient communication has provided alternative methods for bringing information to patients and their families, with potential advantages. For example, the Scientific Animations Without Borders (SAWBO) organisation has generated dozens of short animation films, available in multiple languages, on a range of public health topics (6). There is growing evidence for the benefits of multimedia information in enhancing patients' satisfaction with information and improving knowledge retention (4, 7). Use of multimedia, such as video, animations and static images in delivering health information can help patients understand their condition better than words alone. There is evidence that graphics and animations enhance knowledge and the recall of facts related to specific healthcare interventions (8, 9).
Research using non-randomisedstudy designs has shown that animations are better at communicating a complex biological process to patients than a graphic with a figure legend (10), and they can be more effective than static sequential images for teaching dynamic events (11, 12). Animations can also highlight important content better than a photographic video (13), and edited animations may be more acceptable to patients who do not want to see realistic portrayals of medical interventions (13, 14). Animations can also help to overcome language barriers and educate patients with limited literacy skills (15). Outside healthcare settings a meta-analysis of controlled experiments found that animations improved learning (either knowledge or procedural skills) more than static images (16). However, there are also concerns that animations may encourage only surface learning, and that patients' attention to animations may be time-limited.
Considering the potential advantages and disadvantages of animations as patient information tools, we do not know their comparative value against other forms of information delivery in healthcare. This systematic review seeks to address this gap by evaluating the effectiveness of video animations as information tools on patients' knowledge, attitudes and cognitions, and behaviours.
The review protocol was registered with PROSPERO in February 2021 under ID CRD42020084714 (Available from: https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42021236296).
Participants were either patients in a healthcare setting or members of the public being informed about a topic relevant to public health, health promotion or illness prevention. Studies were eligible for inclusion if they used a randomised or quasi-randomised controlled design, and compared a video animation (e.g., cartoons, avatars, “white board” animation, or animated 2D or 3D models) with another format of information delivery (e.g., print, audio recording, “talking head” video, video of a procedure, spoken information) either as an alternative or additional format. Video animations of any length, with or without voiceover were eligible. Animations were eligible if they were part of a multi-component information package as long as the effect of the animation could be isolated. We excluded studies if: they did not include a control arm; or reported a hypothetical scenario; or the animation was compared with no information intervention.
The primary outcome was knowledge, and secondary outcomes were attitudes and cognitions (that is, feelings or thoughts, such as satisfaction with information, self-confidence) and behaviours (that is, actions or intended actions, such as condition self-management skills, appointment attendance, or behavioural intentions).
Relevant studies were identified by searching the following electronic databases: MEDLINE, EMBASE, Cumulative Index to Nursing and Allied Health Literature (CINAHL), PsycINFO and the Cochrane Central Register of Controlled Trials (CENTRAL) published from January 1996 onwards. Additional searches were undertaken on Open Grey (opengrey.eu). Forwards- and backwards-citation searching was also undertaken through Google Scholar and the reference lists of all included articles (See Supplementary S1: Full search strategy). We did not apply any language restrictions. The searches were conducted in June 2021 and were supported by a specialist information scientist from the Centre for Reviews and Dissemination (CRD) at the University of York.
The studies retrieved from the searches were exported into EndNote and de-duplicated. Two reviewers (EE, NB) independently screened titles and abstracts of all records identified in the search using pre-defined criteria, and then by full text article. Disagreements were resolved through consensus or by consultation with a third reviewer (PK) (See Figure 1 for PRISMA flowchart).
We used a piloted data extraction form to extract the following data: basic study information; details of participants; type of intervention and control arms(s); details of the intervention; outcome data. Data extraction was conducted by one reviewer (NB, TMB or PK) and checked by a second reviewer. Any disagreements were resolved through consensus, and if necessary, a third reviewer was consulted.
We used the Cochrane Risk of Bias Tool-2 (RoB 2) (17) to assess the methodological quality of all included trials on the following five criteria: randomisation process; deviation from intended interventions; missing outcome data; outcome measurement; and selection of the reported result. Risk of bias assessment was conducted by one reviewer (NB, TMB or PK) and checked by a second reviewer. Discrepancies were resolved by discussion, with involvement of a third reviewer if necessary.
Due to the degree of heterogeneity among the included trials, formal meta-analysis was not feasible. Therefore, a narrative approach was used, summarising the findings according to three pre-identified outcome categories (knowledge; attitudes and cognitions; behaviours) and de novo the intended purpose of the interventions. We have taken reports of differences between trials arms of p < .05 as indicators of effect.
The database searches produced 3,458 unique hits (see Figure 1). Sifting by title and abstract and then by full text, resulted in 36 eligible studies. A further two studies were added following citation searches, producing a total of 38 included studies.
The 38 studies comprised 35 trials using random allocation and 3 using quasi-random methods. All but two of the trials used individual participant allocation; in two trials allocation had been clustered.
Study samples ranged from 30 to 843 participants (median 101); the included trials recruited a total of 5,646 participants. There was a wide spread of geographical locations, with the studies being undertaken in 19 different countries: eight from the USA; four from Australia; three each from Thailand and New Zealand; two each from Austria, Indonesia, Korea, Netherlands and the United Kingdom; and one each from Belgium, Canada, China, France, India, Iran, Japan, Tanzania, Turkey and Singapore. All but two of the studies were reported in English language journals; the exceptions were studies reported in German (18) and Korean (19). (See Tables 1–3 for summary of study features).
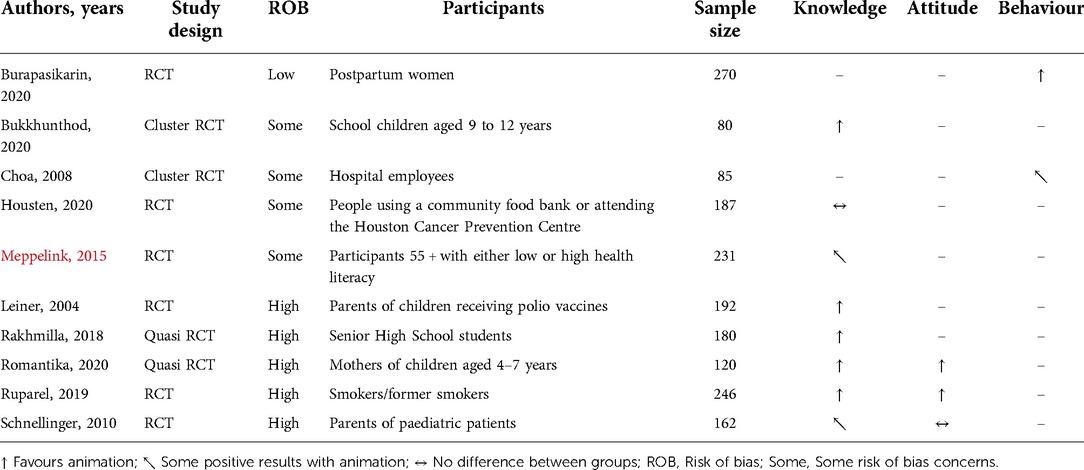
Table 3. Category 3 finding (topics related to public health, health promotion or illness prevention).
Cartoon animations were used in 29 studies, on the subject of: kidney donation (20); post-surgery rehabilitation (21); contraception (22); Type 2 diabetes (23); use of opioids (24); acute coronary syndrome and maintaining heart health (25); polio vaccination (9); thyroid surgery (26) in one arm; chronic constipation (27); liver fluke (28); cardio-pulmonary resuscitation (CPR) (29); consent to CT scanning (19); colorectal cancer screening (30, 31); preparation for preparation for surgery (13, 32), or skin surgery (33, 34), or angiography (35); sputum testing (36); prevention of thalassemia (37); early medical abortion (38); lung cancer screening (39); medicines for epilepsy (40); preventive dental care (41); stem cell transplantation (42); appropriate antibiotic use (8); consent for cystoscopy (43); lumbar puncture (44).
3D animated models were used in six studies to portray: periodontitis (45); maintaining post-operative health (18, 46); dental extraction (47); angiography (48); and cataract surgery (49).
2D animated video was used in one trial with mothers of children with behavioural problems (50).
A “white board” animation was used in one trial to explain angiography (51), and an avatar was used in one trial to explain living well with heart failure (52).
The duration of the animations ranged from 1.25 to 31 min, although in three study reports the animation duration was not stated (29, 49, 52).
Thirteen of the 38 articles (34%) included a link to the tested animation; in 25 articles no link was provided.
In 14 trials the animation was provided in addition to control group interventions, which were:
• standard care (22, 25, 44, 46, 48, 52);
• consultation with surgeon, anaesthetist or other doctor (i.e. spoken information) (13, 34, 40);
• standard written and spoken information (42, 49);
• nurse education audio-recording (20).
In 23 trials the animation was provided as an alternative to control group interventions, which were:
• spoken information (19, 21, 33);
• easy-to-read written information (24, 53);
• either diagram or 3D model, according to allocation (26);
• written booklet (8, 18, 27, 47, 48); printed information (9, 50); booklets, posters and spoken information (28);
• live instructions provided by phone (29);
• audio-booklet or static images, according to allocation (30);
• peer education or conventional lecture, according to allocation (37);
• Tell-Show-Do technique (41);
• verbal consent following provision of spoken information (43).
In one trial (51) the animation was provided as an alternative to the standard physician-patient consent conversation in one trial arm, and in addition to it in another trial arm.
The level of access that participants had to the animations was stated in 22 of the 38 trial reports. In 14 studies they viewed the animation only once (8, 18–20, 22, 27, 30, 36, 38, 40–42, 48, 50) and in one study only once or twice as they preferred (39). In two studies they viewed the animation exactly twice (21) or three times (28). In four studies animation viewing was unlimited (25, 52) or unlimited during the clinic visit (45). In one 3-arm trial, patients were allowed to watch it only once if they were in the clinic (clinic viewing arm) or had unlimited viewing if they were at home (home viewing arm) (44).
In 16 studies level of access was not stated (9, 13, 23, 24, 29, 31–35, 37, 43, 46, 47, 49, 51).
Knowledge was the most commonly reported outcome in 30 trials (8, 9, 13, 18–21, 23–25, 27, 28, 30–33, 35, 37–40, 43–45, 47–52).
Attitudes and cognitions were reported in 20 trials, reporting self-efficacy (20); information satisfaction (18, 32, 33, 38, 42–44, 47–49, 51); illness perceptions (25); perceptions of surgery, quality of recovery (46); information satisfaction, unmet information needs (26); information satisfaction, familiarity with topic (19); desire for information (34); self-care confidence (52); attitude to information (50); subjective knowledge, decisional certainty (39); information satisfaction, having learned from information (8).
Nine trials reported behaviour outcomes, including willingness to give consent and undergo the procedure (20); physical activity (21); contraception use (22); return to work, physical activity and medication adherence (25); CPR skills, time taken to initiate CPR (29); self-care behaviours (52); quality of sputum sample (36); medication adherence (40); patient co-operation (41).
Only two trials reported all three categories of outcome (25, 52).
In 35 studies outcomes were assessed shortly after delivery of the information intervention. However, in five of these studies there was an additional assessment of outcomes (at the second dental appointment (41); 1 day later (32); 2 weeks later (45); 7 weeks later (25); 3 months later (40); or 4 weeks later (8)).
In two studies outcome assessment was only made some time after intervention delivery (30 and 90 days later (52); 6–8 weeks later (22)), and in one study (29) outcomes were assessed at the same time as participants were receiving the intervention.
For the purpose of quality assessment and outcome reporting, we categorised de novo the 38 studies into three groups, according to the intended purpose or setting of the information:
• Category 1: Explaining medical or surgical procedures (17 studies);
• Category 2: Management of long-term conditions (11 studies);
• Category 3: Topics related to public health, health promotion or illness prevention (10 studies).
Figure 2 and Table 1 summarise the risk of bias judgements and findings across the studies in category 1 (17 studies, n = 2,655, sample range 30–843) (13, 18, 19, 26, 32–36, 38, 41–43, 47–49, 51).
Nine of the 17 studies were assessed as having a high risk of bias, most commonly due to the randomisation process. The other studies were rated as at low risk of bias (3 studies) (36, 43, 48) or having “some concerns” (5 studies), due to small sample sizes or a lack of protocol registration (33, 38, 41, 42, 49).
Knowledge was assessed in twelve studies and provision of an animation resulted in positive outcomes in eight of them (13, 19, 33, 35, 43, 48, 49, 51). From the eight studies in which outcomes favoured animation, four were related to informed consent (19, 33, 43, 49). In the remaining studies one study showed some benefits from the animation (i.e., favoured animation at one recruitment site and showed no difference between arms at the other two sites) (38)) and three studies showed no differences between the intervention and control arms (18, 32, 47). It is notable that knowledge outcomes favoured the animation in almost all studies (7/8) when the comparator was standard care or spoken information, but only in a minority of studies (1/4) when the comparator was a work of written information or static images.
No Category 1 study reported better knowledge outcomes in the control group (See Supplementary S2: Table 4 for a detailed summary).
Attitudes and cognitions were assessed in thirteen studies (18, 19, 26, 32–34, 38, 42, 43, 47–49, 51) and only two studies reported statistically significant differences in favour of the animation (19, 48).
Six studies reported no statistically significant differences between arms (32–34, 43, 49, 51), of which three were related to informed consent (33, 43, 49).
Four studies showed some benefits with animation (i.e., outcomes favoured animation in some items or sub-scores, but found no differences between arms with the remainder) (18, 26, 42, 47).
One study (38) showed mixed results: one recruitment site (out of three sites) reported in favour of standard care on the information being “very helpful” and the other two recruitment sites reported no difference between arms. All three sites reported no difference on information they received being “very clear”. Only one out of three recruitment sites reported in favour of animation on “information utility” (38).
Behaviours and skills were assessed in two studies (36, 41) and both studies reported in favour of the animation. One study reported that patients who watched the animation produced better quality sputum samples (36) and the other study the animation was more effective for preparing children for dental treatment (41).
Figure 3 and Table 2 summarise the risk of bias judgements and findings across studies in Category 2 (11 studies, n = 1238, range 36–240) (20, 21, 23–25, 27, 40, 44–46, 54).
Just over half of the studies (7/11) in this category were rated as having “some concerns” of bias due to unclear randomisation, small sample size or lack of protocol registration (20, 21, 24, 27, 44–46).
Four studies were rated as having a high risk of bias due to the randomisation process, missing data or being underpowered (through being unable to recruit the target sample size) (23, 25, 40, 54).
None of the studies in this category were rated as low risk of bias overall.
Knowledge was assessed in ten studies and provision of an animation resulted in positive outcomes in six of them (20, 21, 24, 40, 44, 45) and no difference between arms in one study (27).
The other three studies reported some benefits from the animation (i.e., favoured animation at 90 days but not at 30 days follow-up (54); favoured animations on only one of eight measures (25); and favoured animation in participants with inadequate functional health literacy but not in participants with marginal or adequate functional health literacy (23)).
No Category 2 study reported better knowledge outcomes in the control group (See Supplementary S3: Table 5 for a detailed summary).
Attitudes and cognitions were assessed in five studies (20, 25, 44, 46, 52) and three of the studies reported no significant differences between arms (20, 44, 52). One study reported some improvement with animation on aspects of outcome measures: four out of 18 illness perception items; two out of four medication beliefs items, and cardiac anxiety items (25). The other study reported a positive effect of animation on the quality of recovery but no differences on: perceptions of surgery, recovery, mobilization and oral nutrition, or on traditional beliefs about recovery after surgery (46).
No Category 2 study reported better attitudes and cognitions outcomes in the control group.
Behaviours and skills were assessed in five studies (20, 21, 25, 40, 52) and only one of the five studies (into children with epilepsy) reported in favour of animation in terms of improved drug adherence (40). Two studies reported some benefits with animation (i.e., favoured animation on 1 out of 4 measures (25); favoured animation for IRD willingness only (20)). In the other two studies there was no reported difference between the intervention and control arms in terms of compliance and self-care behaviour (21, 52).
No Category 2 study reported better behaviour outcomes in the control group.
Figure 4 and Table 3 summarise the risk of bias judgements and findings across the studies (10 studies, n = 1,753, sample range 80–270).
Five out of ten studies were rated as having a high risk of bias (8, 9, 37, 39, 50). The most common reasons were the randomisation process and missing outcome data. Four studies were rated as having some concerns, due to lack of protocol or sample size calculation (28–31). Only one study was rated as having low risk of bias (22).
Knowledge was assessed in eight studies (8, 9, 28, 30, 31, 37, 39, 50) and provision of an animation resulted in positive outcomes in five of them (9, 28, 37, 39, 50). The participants in those four out of five studies were either school children or mothers of young children (9, 28, 37, 50). Two studies showed some benefits from animations (i.e., favoured animation at 4 weeks follow-up but not immediately after the intervention (8); favoured animation in the low health literacy spoken text + animation group but not in the high health literacy group or the low health literacy written information + animation group (31)). One study reported no differences between arms regardless of participants’ level of health literacy (30).
No Category 3 study reported better knowledge outcomes in the control group (See Supplementary S4: Table 6 for a detailed summary).
Attitudes and cognitions were assessed in three studies (8, 39, 50) and two studies reported significant differences in favour of animation (39, 50). In one study mothers of young children did not think they had learnt something new about the use of antibiotics by watching the animation when compared to those provided with a pamphlet. They also did not think the animation was more interesting or useful (8).
Behaviours and skills were assessed in two studies (22, 29). One study assessing use of long-acting reversible contraception (LARC) in postpartum women, reported in favour of video animation (22). The other study comparing live CPR instructions from a dispatcher over the phone and video animation reported better scores in checklist assessment and time interval compliance with the animation. However, differences were not apparent for the psychomotor skill measures (29).
This systematic review of trials of video animations as information tools for patients and the general public included 38 studies. Data pooling was not possible due to significant variation across aspects of the trials. Most trials assessed the effect of cartoons or 3D animations. Knowledge was the outcome most often assessed, usually very soon after participants had accessed information. There were consistently positive effects of animations on knowledge, particularly when compared to standard care or spoken information, but also when compared to easy-to-read information, standard printed information, real-time or static images, and audio-recorded information. Participants’ attitudes and cognitions were evaluated less frequently, showing benefits of animations in some studies but no clear benefits in as many studies. Patient behaviours were assessed least frequently, reporting animation benefits in half of relevant studies and no differences in the remainder. Across the 38 studies, only one reported statistically significant benefits of the control intervention over animation (38).
A number of processes were used in the systematic review to reduce potential for bias, including: protocol registration; multiple database searches; entry criteria; inclusion of non-English articles; citation searching; and dual decision-making on study inclusion, data extraction and risk of bias assessment. One strength of the findings was the breadth of health settings and country of origin: although most of the trials were undertaken in high income countries, there was a significant geographical spread.
The included studies were all real world, pragmatic evaluations of outcome effectiveness. However, they did not collect process data (such as attention monitoring or eye tracking), which could indicate patient engagement with the animations and provide insights into patterns of effectiveness. Furthermore, few trials assessed knowledge in the longer-term. In some settings, for example, management of long-term conditions or preventive health behaviours, longer-term knowledge increases would be a more important indicator of intervention success. However, in other settings, such as the preparation of patients for surgery or CT scanning, shorter-term knowledge gains would be valid indicators of effect.
Individual trials were often small and with substantial variation across a number of different study elements. Furthermore, the quality of the 38 trials was mixed, with only four trials rated as having low risk of bias. Frequent sources of risk of bias were randomisation processes, small sample size or lack of sample size calculation, missing outcome data, and lack of protocol publication. Half of the trials recruited fewer than 100 participants and most of these had no stated sample size calculation, which raises two legitimate concerns: (i) possible Type 2 statistical error in studies reporting null effects, and (ii) possible publication bias associated with studies reporting beneficial effects of animations.
Only a minority of articles provided a link to the tested animation. No doubt copyright restrictions were influential in several trials but the inability to play the evaluated animations does restrict the conclusions that can be drawn. For example, it makes it impossible to assess the content, tone, accessibility or quality of animations. Furthermore, it prevents study replication or the ability of build on effective interventions, both of which are crucial elements of scientific methods.
Overall, the findings were similar to those seen in uncontrolled studies (10–14). While the findings of this review suggest there is a potential role for animations as information tools, there remains a lack of good quality evidence on their effectiveness, as well as a lack of clarity on which types of animations and which animation elements are associated with optimal use, acceptability and effectiveness. This implies the need for three types of research:
• First, larger trials that are less susceptible to bias. It should be possible for trials to use allocation concealment when recruiting participants, even if blinding of outcome assessment is not possible. Trials using cluster allocation may be the solution to the inherent problems with intervention blinding in information research, although cluster trial design decisions are not straightforward. Sample size calculation is also essential, although it may be a lesser priority in feasibility or pilot trials. Also important are an adjustment for statistical multiplicity when multiple outcome measures are being assessed, and health economic analyses, particularly when animations are being provided instead of a lower cost information intervention.
• Second, implementation research, evaluating the use of animations in practice to assess the impact of context (particularly health setting and delivery) on uptake and effectiveness. For example, one advantage of animations over static images (in print or online) is that they can be dynamic, having potential to illustrate procedures, interventions and pathology in ways that other formats may not be able to do, which may make them particularly well suited to explaining complex procedures or treatment processes.
• Third, fine-grained process studies may be needed to assess the effects of animation length as well as various design elements on users' attention and knowledge acquisition. One concern is that animations may lead to, or even encourage surface level learning, rather than more meaningful or conceptual learning. Furthermore, users' attention to video and video animations may be limited; this has implications for more complex or detailed topics, when the useful function of animations could be limited to an introduction or overview.
It is vital that reports of future animation studies allow access to the evaluated animations, or it is impossible to discern quality or the effects of mediators (and so understand patterns of effectiveness and ineffectiveness) (16). Furthermore, reports should make clear the extent of patients' access to animations. In some healthcare settings, such as preparation for CT scanning, access will necessarily be time-limited. However, in many settings animations may be available online and with unlimited patient access. This situation can create a mismatch with access limits imposed within a controlled study environment; at the very least, this issue needs acknowledgment in study reports.
The included trials were a mix of studies of animations used in addition to other provision and those in which animations were a replacement. This is an important distinction and one that needs clarification in future studies, given the possible implications of healthcare services having to develop and deliver information in more than one format. Finally, animations may be most beneficial (in relative terms) for children and population groups with lower levels of education or health literacy, but currently the evidence base does not permit such an indication of relative effectiveness.
This is the first systematic review of the effectiveness of video animations as patient information tools, when evaluated in controlled studies. Our findings indicate mostly positive effects on knowledge, particularly in the short-term, and some positive effects on attitudes and cognitions. They also indicate mostly positive effects on behaviour, although this outcome was evaluated in only nine trials. There is almost no evidence of worse patient outcomes from animations.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
The study idea was conceived by PK, and the methods were developed in collaboration with TMB, ND and EE. ND and EE undertook most of the work in sifting database search results. All authors undertook data extraction and quality appraisal. TMB wrote the first draft of the manuscript, which was then refined by all authors. All authors contributed to the article and approved the submitted version.
The research received support from the Hull York Medical School INSPIRE scheme.
We thank Helen Fulbright of the Centre for Reviews & Dissemination, University of York for developing the database searches, which were funded through the Department of Health Sciences, University of York. We thank our colleagues Jana Heinz and Iyn-Hyang Lee for article translation, and Professors Joy Adamson, Peter Gardner and Lina Gega for providing comments on earlier drafts of this work.
We also thank the following study authors for providing links to the evaluated animations: Annie Jones, John Reynolds-Wright, Saskia Tipotsch-Maca, Liise Kayler, Professor Robert Volk and Professor Marie Leiner.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fdgth.2022.1010779/full#supplementary-material.
1. Fiksdal AS, Kumbamu A, Jadhav AS, Cocos C, Nelsen LA, Pathak J, et al. Evaluating the process of online health information searching: a qualitative approach to exploring consumer perspectives. J Med Internet Res. (2014) 16(10):e3341. doi: 10.2196/jmir.3341
2. Perez SL, Kravitz RL, Bell RA, Chan MS, Paterniti DA. Characterizing internet health information seeking strategies by socioeconomic status: a mixed methods approach. BMC Med Inform Decis Mak. (2016) 16:107. doi: 10.1186/s12911-016-0344-x
3. Jia X, Pang Y, Liu LS. Online health information seeking behavior: a systematic review. Healthcare (Basel). (2021) 9(12):1740. doi: 10.3390/healthcare9121740
4. Beranova E, Sykes C. A systematic review of computer-based softwares for educating patients with coronary heart disease. Patient Educ Couns. (2007) 66(1):21–8. doi: 10.1016/j.pec.2006.09.006
5. von Wagner C, Semmler C, Good A, Wardle J. Health literacy and self-efficacy for participating in colorectal cancer screening: the role of information processing. Patient Educ Couns. (2009) 75(3):352–7. doi: 10.1016/j.pec.2009.03.015
6. Bello-Bravo J, Pittendrigh BR. SAWBO- Home 2022 [cited 2022 September 2]. Available from: https://sawbo-animations.org/home/
7. Fox MP. A systematic review of the literature reporting on studies that examined the impact of interactive, computer-based patient education programs. Patient Educ Couns. (2009) 77(1):6–13. doi: 10.1016/j.pec.2009.02.011
8. Schnellinger M, Finkelstein M, Thygeson MV, Vander Velden H, Karpas A, Madhok M. Animated video vs pamphlet: comparing the success of educating parents about proper antibiotic use. Pediatrics. (2010) 125(5):990–6. doi: 10.1542/peds.2009-2916
9. Leiner M, Handal G, Williams D. Patient communication: a multidisciplinary approach using animated cartoons. Health Educ Res. (2004) 19(5):591–5. doi: 10.1093/her/cyg079
10. O’Day DH. The value of animations in biology teaching: a study of long-term memory retention. CBE Life Sci Educ. (2007) 6(3):217–23. doi: 10.1187/cbe.07-01-0002
11. Tversky B, Morrison JB, Betrancourt M. Animation: can it facilitate? Int J Hum Comput Stud. (2002) 57(4):247–62. doi: 10.1006/ijhc.2002.1017
12. Pollock E, Chandler P, Sweller J. Assimilating complex information. Learn Instr. (2002) 12(1):61–86. doi: 10.1016/S0959-4752(01)00016-0
13. Kakinuma A, Nagatani H, Otake H, Mizuno J, Nakata Y. The effects of short interactive animation video information on preanesthetic anxiety, knowledge, and interview time: a randomized controlled trial. Anesth Analg. (2011) 112(6):1314–8. doi: 10.1213/ANE.0b013e31820f8c18
14. Salzwedel C, Petersen C, Blanc I, Koch U, Goetz AE, Schuster M. The effect of detailed, video-assisted anesthesia risk education on patient anxiety and the duration of the preanesthetic interview: a randomized controlled trial. Anesth Analg. (2008) 106(1):202–9. doi: 10.1213/01.ane.0000287665.96156.72
15. Newton JT, Thorogood N, Bhavnani V, Pitt J, Gibbons DE, Gelbier S. Barriers to the use of dental services by individuals from minority ethnic communities living in the United Kingdom: findings from focus groups. Prim Dent Care. (2001) os8(4):157–61. doi: 10.1308/135576101322462228
16. Hoffler TN, Leutner D. Instructional animation versus static pictures: a meta-analysis. Learn Instr. (2007) 17:722–38. doi: 10.1016/j.learninstruc.2007.09.013
17. Sterne JAC, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. Rob 2: a revised tool for assessing risk of bias in randomised trials. BMJ. (2019) 366:l4898. doi: 10.1136/bmj.l4898
18. Hermann M. 3-dimensional Computer animation–a new medium for supporting patient education before surgery. Acceptance and assessment of patients based on a prospective randomized study–picture versus text. [German] Dreidimensionale Computeranimation–neues Medium zur Unterstutzung des Aufklarungsgesprachs vor Operationen. Akzeptanz und Bewertung der Patienten anhand einer prospektiv randomisierten Studie–Bild versus Text. Chirurg. (2002) 73(5):500–7. doi: 10.1007/s00104-001-0416-y
19. Hong JY, Kim CW, Noh H, Lee DH, Kim SE, Lee SJ. The effect of animation-assisted informed consent using tablet personal computer for contrast-enhanced computed-tomography in emergency department. Hong Kong J Emerg Med. (2012) 19(4):257–63. doi: 10.1177/102490791201900404
20. Kayler LK, Dolph BA, Cleveland CN, Keller MM, Feeley TH. Educational animations to inform transplant candidates about deceased donor kidney options: an efficacy randomized trial. Transplant Direct. (2020) 6(7):e575. doi: 10.1097/TXD.0000000000001026
21. Li J, Davies M, Ye M, Li Y, Huang L, Li L. Impact of an animation education program on promoting compliance with active respiratory rehabilitation in postsurgical lung cancer patients: a randomized clinical trial. Cancer Nurs. (2021) 44(2):106–15. doi: 10.1097/NCC.0000000000000758
22. Burapasikarin C, Manonai J, Wattanayingcharoenchai R. The effect of an educational video on long-acting reversible contraception (LARC) utilization at 6–8 weeks postpartum period: a randomized controlled trial. Arch Gynecol Obstet. (2020) 302(6):1503–9. doi: 10.1007/s00404-020-05710-3
23. Calderon JL, Shaheen M, Hays RD, Fleming ES, Norris KC, Baker RS. Improving diabetes health literacy by animation. Diabetes Educ. (2014) 40(3):361–72. doi: 10.1177/0145721714527518
24. Chakravarthy B, Somasundaram S, Mogi J, Burns R, Hoonpongsimanont W, Wiechmann W, et al. Randomized pilot trial measuring knowledge acquisition of opioid education in emergency department patients using a novel media platform. Subst Abuse. (2018) 39(1):27–31. doi: 10.1080/08897077.2017.1375061
25. Jones AS, Ellis CJ, Nash M, Stanfield B, Broadbent E. Using animation to improve recovery from acute coronary syndrome: a randomized trial. Ann Behav Med. (2016) 50(1):108–18. doi: 10.1007/s12160-015-9736-x
26. Mayilvaganan S, Shivaprasad C. Comparison of the efficacy of three different methods of explaining the surgical procedure of hemithyroidectomy. Indian J Endocrinol Metab. (2018) 22(4):520–4. doi: 10.4103/ijem.IJEM_609_17
27. Baker J, editor. Improving chronic constipation health literacy proficiency: animation versus traditional written pamphlets (2018).
28. Bukkhunthod P, Meererksom T, Pechdee P, Ponphimai S, Khiaowichit J, Kaewpitoon N, et al. Animation as supplementary learning material about carcinogenic liver fluke in classes for primary schoolchildren. J Cancer Educ. (2020) 35(1):14–21. doi: 10.1007/s13187-018-1434-5
29. Choa M, Park I, Chung HS, Yoo SK, Shim H, Kim S. The effectiveness of cardiopulmonary resuscitation instruction: animation versus dispatcher through a cellular phone. Resuscitation. (2008) 77(1):87–94. doi: 10.1016/j.resuscitation.2007.10.023
30. Housten AJ, Kamath GR, Bevers TB, Cantor SB, Dixon N, Hite A, et al. Does animation improve comprehension of risk information in patients with low health literacy? A randomized trial. Med Decis Making. (2020) 40(1):17–28. doi: 10.1177/0272989X19890296
31. Meppelink CS, van WJC, Haven CJ, Smit EG. The effectiveness of health animations in audiences with different health literacy levels: an experimental study. J Med Internet Res. (2015) 17(1):e11. doi: 10.2196/jmir.3979
32. Tou S, Tou W, Mah D, Karatassas A, Hewett P. Effect of preoperative two-dimensional animation information on perioperative anxiety and knowledge retention in patients undergoing bowel surgery: a randomized pilot study. Colorectal Dis. (2013) 15(5):e256–65. doi: 10.1111/codi.12152
33. Miao Y, Venning VL, Mallitt K-A, Rhodes JEJ, Isserman NJ, Moreno G, et al. A randomized controlled trial comparing video-assisted informed consent with standard consent for Mohs micrographic surgery. JAAD International. (2020) 1(1):13–20. doi: 10.1016/j.jdin.2020.03.005
34. Platto JF, Maarouf M, Hendricks A, Kurtzman DJ, Shi VY. Animated video consultation for reducing pre-operative anxiety in dermatologic surgery. Dermatol Online J. (2019) 25(3):15. doi: 10.5070/D3253043328
35. Yap J, Teo TY, Foong P, Binte Hussin N, Wang H, Shen T, et al. A randomized controlled trial on the effectiveness of a portable patient education video prior to coronary angiography and angioplasty. Catheter Cardiovasc Interv. (2020) 96(7):1409–14. doi: 10.1002/ccd.28655
36. Mhalu G, Hella J, Doulla B, Mhimbira F, Mtutu H, Hiza H, et al. Do instructional videos on sputum submission result in increased tuberculosis case detection? A randomized controlled trial. PLoS One. (2015) 10(9):e0138413. doi: 10.1371/journal.pone.0138413
37. Rakhmilla LE, Susanah S, Rohmawaty E, Effendi SH. Effectiveness of an educational intervention in providing knowledge about the prevention of thalassemia: an effort to reduce new thalassemia cases. Asian J Epidemiol. (2018) 11(2):59–64. doi: 10.3923/aje.2018.59.64
38. Reynolds-Wright JJ, Belleuvre F, Daberius A, Faucher P, Gemzell-Danielsson K, Cameron ST. Information on early medical abortion for women using an audiovisual animation vs face-to-face consultation: a consortium randomized and quasi-randomized trial. Acta Obstet Gynecol Scand. (2020) 99(12):1611–7. doi: 10.1111/aogs.13944
39. Ruparel M, Quaife SL, Ghimire B, Dickson JL, Bhowmik A, Navani N, et al. Impact of a lung cancer screening information film on informed decision-making: a randomized trial. Ann Am Thorac Soc. (2019) 16(6):744–51. doi: 10.1513/AnnalsATS.201811-841OC
40. Saengow VE, Chancharoenchai P, Saartying W, Pimpa W, Chotichanon N, Lewsirirat T, et al. Epilepsy video animation: impact on knowledge and drug adherence in pediatric epilepsy patients and caregivers. Clin Neurol Neurosurg. (2018) 172:59–61. doi: 10.1016/j.clineuro.2018.06.031
41. Sahebalam R, Rafieinezhad R, Boskabad M. Comparison of the efficacy of Jilo animation approach versus conventional tell-show-do (TSD) technique on cooperation and anxiety levels of children during dental practice: a randomized controlled clinical trials. J Dent. (2020) 21(4):284–91. doi: 10.30476/dentjods.2020.81897.1001
42. Sariturk C, Gereklioglu C, Korur A, Asma S, Yeral M, Solmaz S, et al. Effectiveness of visual methods in information procedures for stem cell recipients and donors. Turk J Haematol. (2017) 34(4):321–7. doi: 10.4274/tjh.2016.0118
43. Winter M, Kam J, Hardy E, Nalavenkata S, Handmer M, Ainsworth H, et al. The use of portable video media versus standard verbal communication in the urological consent process: a randomised controlled clinical trial. J Urol. (2016) 1:e239. doi: 10.1111/bju.13595
44. Babapour Mofrad R, Fruijtier AD, Visser LNC, Hoogland N, van Dijk M, van Rossum F, et al. Lumbar puncture patient video increases knowledge and reduces uncertainty: an RCT. Alzheimer’s Dementia. (2021) 7(1):e12127. doi: 10.1002/trc2.12127
45. Cleeren G, Quirynen M, Ozcelik O, Teughels W. Role of 3D animation in periodontal patient education: a randomized controlled trial. J Clin Periodontol. (2014) 41(1):38–45. doi: 10.1111/jcpe.12170
46. Jones ASK, Kleinstauber M, Akroyd A, Mittendorf A, Bognuda P, Merrie AEH, et al. Using animated visualization to improve postoperative mobilization: a randomized controlled trial. Health Psychol. (2019) 38(8):748–58. doi: 10.1037/hea0000761
47. Mladenovski A, Kieser JA. The efficacy of multimedia pre-operative information for patients: a pilot study. N Z Dent J. (2008) 104(2):36–43. PMID: 1867282718672827
48. Lattuca B, Barber-Chamoux N, Alos B, Sfaxi A, Mulliez A, Miton N, et al. Impact of video on the understanding and satisfaction of patients receiving informed consent before elective inpatient coronary angiography: a randomized trial. Am Heart J. (2018) 200:67–74. doi: 10.1016/j.ahj.2018.03.006
49. Tipotsch-Maca SM, Varsits RM, Ginzel C, Vecsei-Marlovits PV. Effect of a multimedia-assisted informed consent procedure on the information gain, satisfaction, and anxiety of cataract surgery patients. J Cataract Refract Surg. (2016) 42(1):110–6. doi: 10.1016/j.jcrs.2015.08.019
50. Romantika IW, Lusmilasari L, Prabandari YS, Syahrul S. Application of video-based health education in improving mother's Knowledge and attitudes about behavioral problems among preschool children. Enferm Clin. (2020) 30(Suppl 2):172–6. doi: 10.1016/j.enfcli.2019.07.071
51. Mednick Z, Irrcher I, Hopman WM, Sharma S. Assessing a narrated white board animation as part of the consent process for intravenous fluorescein angiography: a randomized educational study. Can J Ophthalmol. (2016) 51(6):471–5. doi: 10.1016/j.jcjo.2016.04.023
52. Wonggom P, Nolan P, Clark RA, Barry T, Burdeniuk C, Nesbitt K, et al. Effectiveness of an avatar educational application for improving heart failure patients’ knowledge and self-care behaviors: a pragmatic randomized controlled trial. J Adv Nurs. (2020) 76(9):2401–15. doi: 10.1111/jan.14414
53. Calderon JL, Bazargan M, Sangasubana N, Hays RD, Hardigan P, Baker RS. A comparison of two educational methods on immigrant Latinas breast cancer knowledge and screening behaviors. J Health Care Poor Underserved. (2010) 21(3 Suppl):76–90. doi: 10.1353/hpu.0.0364
Keywords: video animations, information tools, patients, knowledge, attitudes and cognition, behaviors
Citation: Moe-Byrne T, Evans E, Benhebil N and Knapp P (2022) The effectiveness of video animations as information tools for patients and the general public: A systematic review. Front. Digit. Health 4:1010779. doi: 10.3389/fdgth.2022.1010779
Received: 3 August 2022; Accepted: 6 October 2022;
Published: 31 October 2022.
Edited by:
Pradeep Nair, Central University of Himachal Pradesh, IndiaReviewed by:
Julia Bello-Bravo, State of Michigan, United States© 2022 Moe-Byrne, Evans, Benhebil and Knapp. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Thirimon Moe-Byrne bW9lLmJ5cm5lQHlvcmsuYWMudWs=
Specialty Section: This article was submitted to Connected Health, a section of the journal Frontiers Frontiers in Digital Health
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.