
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Digit. Health, 03 September 2021
Sec. Connected Health
Volume 3 - 2021 | https://doi.org/10.3389/fdgth.2021.683034
This article is part of the Research TopicDigital Health Solutions to HPV VaccinationView all 10 articles
 David B. Buller1*
David B. Buller1* Sherry Pagoto2
Sherry Pagoto2 Kimberly Henry3
Kimberly Henry3 Julia Berteletti1
Julia Berteletti1 Barbara J. Walkosz1
Barbara J. Walkosz1 Jessica Bibeau2
Jessica Bibeau2 Katie Baker4
Katie Baker4 Joel Hillhouse4
Joel Hillhouse4 Kelsey M. Arroyo5
Kelsey M. Arroyo5Introduction: Parents acquire information about human papillomavirus (HPV) vaccines online and encounter vaccine-critical content, especially on social media, which may depress vaccine uptake. Secondary analysis in a randomized trial of a Facebook-delivered adolescent health campaign targeting mothers with posts on HPV vaccination was undertaken with the aims of (a) determining whether the pre–post-change occurred in self-reports of the mothers on HPV vaccination of their adolescent daughters; (b) describing the comments and reactions to vaccine posts; (c) exploring the relationship of campaign engagement of the mothers assessed by their comments and reactions to posts to change in the self-reports of the mothers of HPV vaccination.
Materials and Methods: Mothers of daughters aged 14–17 were recruited from 34 states of the US (n = 869). A social media campaign was delivered in two Facebook private groups that differed in that 16% of posts in one were focused on indoor tanning (IT) and 16% in the other, on prescription drug misuse, assigned by randomization. In both groups, posts promoted HPV vaccination (n = 38 posts; no randomization) and vaccination for other disease (e.g., influenza, n = 49). HPV and other vaccination posts covered the need for a vaccine, the number of adolescents vaccinated, how vaccines are decreasing the infection rates, and stories of positive benefits of being vaccinated or harms from not vaccinating. Guided by social cognitive theory and diffusion of innovations theory, posts were intended to increase knowledge, perceived risk, response efficacy (i.e., a relative advantage over not vaccinated daughters), and norms for vaccination. Some vaccination posts linked to stories to capitalize on identification effects in narratives, as explained in transportation theory. All mothers received the posts on vaccination (i.e., there was no randomization). Mothers completed surveys at baseline and 12- and 18-month follow-up to assess HPV vaccine uptake by self-report measures. Reactions (such as sad, angry) and comments to each HPV-related post were counted and coded.
Results: Initiation of HPV vaccination (1 dose) was reported by 63.4% of mothers at baseline, 71.3% at 12-month posttest (pre/post p < 0.001), and 73.3% at 18-month posttest (pre/post p < 0.001). Completion of HPV vaccination (two or three doses) was conveyed by 50.2% of mothers at baseline, 62.5% at 12-month posttest (pre/post p < 0.001), and 65.9% at 18-month posttest (pre/post p < 0.001). For posts on HPV vaccines, 8.1% of mothers reacted (n = 162 total), and 68.4% of posts received a reaction (63.2% like; 13.2% love, 7.9% sad). In addition, 7.6% of mothers commented (n = 122; 51 unfavorable, 68 favorable, 1 neutral), and 50.0% of these posts received a comment. There were no differences in pre–post change in vaccine status by the count of reactions or comments to HPV vaccine posts (Ps > 0.05). Baseline vaccination was associated with the valence of comments to HPV vaccine posts (7.2% of mothers whose daughters had completed the HPV series at baseline made a favorable comment but 7.6% of mothers whose daughters were unvaccinated made an unfavorable comment).
Conclusion: Effective strategies are needed in social media to promote HPV vaccines and counter misinformation about and resistance to them. Mothers whose daughters complete the HPV vaccine course might be recruited as influencers on HPV vaccines, as they may be predisposed to talk favorably about the vaccine. Comments from mothers who have not been vaccinated should be monitored to ensure that they do not spread vaccine-critical misinformation. Study limitations included lack of randomization and control group, relatively small number of messages on HPV vaccines, long measurement intervals, inability to measure views of vaccination posts, reduced generalizability related to ethnicity and social media use, and use of self-reported vaccine status.
Clinical Trial Registration: www.clinicaltrials.gov, identifier NCT02835807.
Despite the recommendation of the Advisory Committee on Immunization Practices (ACIP), (1) only 54% of adolescents aged 13–17 were up-to-date for the human papillomavirus (HPV) vaccine in 2019 (women 57%; men: 52%) (2), far below the healthy people 2030 target of 80%. Vaccine initiation and completion are affected by health beliefs (e.g., vaccine knowledge; the importance of preventive vaccinations; side effects concerns) (3–6) which are amenable to change through health education interventions. Identifying effective strategies to improve HPV vaccination rates is a national and international priority (7, 8).
Parents frequently use the Internet as a reliable source of information on child health (9–11), and online interventions may reach large proportions of parents whose children are not up-to-date on the HPV vaccine. Parents acquire information about HPV vaccines online (12–15), but unfortunately, inaccurate, misleading, unsupported, and harmful information can be circulated online (16, 17), including about vaccines (12, 18–22). False claims are made that HPV vaccines increase teen sexual activity; a low prevalence of HPV-related diseases exists; other modes of prevention are available; HPV vaccines are unsafe due to insufficient testing; HPV vaccines have severe side effects or cause death; HPV vaccine regulations are a product of corruption or conspiracies; and HPV vaccines violate civil liberties (15, 22–27). HPV vaccination decisions of the parents are affected by this online content (12, 28–31) which can depress vaccine uptake (12, 28–31). For instance, in one survey, parents who heard stories about only harms (e.g., mild side effects and death) were unlikely to vaccinate children for HPV even if they also heard stories about disease prevention (12).
Social media, in particular, spread information on HPV vaccines and transmit vaccine-critical content (12, 32–34). Growing research on social media, particularly related to vaccines, finds widespread misinformation and unsubstantiated claims about corruption, conspiracies, and distrust in vaccine regulations, especially of drug companies, government agencies, and physicians (35). Parents have reported receiving stories about the harms of HPV vaccines on social media and news media, while stories on the prevention of HPV disease occurred in conversations (12). In one study, mothers who first learned about HPV vaccines through social media tended not to vaccinate daughters, while those first hearing about it from their general practitioner vaccinated them (36). There have been calls for efforts to improve accurate HPV content on social media and correct misinformation (37–41) to improve clinical encounters on HPV vaccines (32).
Much of the past research on HPV vaccine content in social media has been descriptive and correlational (21, 26, 42), with few studies examining the impact of HPV vaccine messages prospectively (43, 44). The authors recently completed a randomized trial on a 12-month social media adolescent health campaign delivered to mothers of daughters aged 14–17, which contained posts promoting HPV vaccination. A unique feature of social media is the presence of user-generated content (e.g., comments and reactions), and an analysis of the first 10 posts on HPV vaccination in the campaign (45) revealed that about 10% of mothers reacted/commented on HPV vaccine posts. Mothers posting supportive comments were more likely to have vaccinated daughters at baseline, as had those remaining silent, while mothers posting critical comments were less likely to have vaccinated daughters. In this study, we present analyses of pre-post change in reports of the mothers on vaccination of their adolescent daughters after the entire year-long social media campaign, a description of comments and reactions to all vaccine posts, and the relationship of campaign engagement of the mothers to comments and reactions.
Mothers with teenage daughters were enrolled in a randomized controlled trial with the primary purpose of evaluating the effect of social media posts on their permissiveness toward indoor tanning (IT) by daughters. After a baseline survey, mothers were randomly assigned to one of two Facebook private groups. Randomization was accomplished by the project biostatistician, using permuted-block randomization (block size = 2). All mothers received a Facebook feed of posts on adolescent health topics, mother–daughter communication and current events, which differed on whether the feed included posts on IT (intervention) or prescription drug misuse (control). Both feeds contained posts on HPV vaccination and vaccination for other diseases (e.g., influenza) as there was no randomization on the presence of the HPV vaccination messages. A community manager added mothers to the groups, scheduled posts, and monitored and responded to comments during the 12-month campaign, after which mothers completed posttest surveys at 12- and 18-months post-randomization. To retain participants, any mothers who left the private groups were contacted and asked to re-join and mothers were alerted to upcoming posttests and compensated ($40 for baseline, $20 for 12-month posttest, and $40 for 18-month posttest). Daughters were invited to complete the baseline survey and both posttests (compensation = $20, $15, and $25, respectively) but were not enrolled in the social media feed. Study staff other than the community manager and project coordinator were blinded. The Western Institutional Review Board (IRB) and the IRBs at East Tennessee State University and the University of Connecticut approved study protocols.
Between May 2017 and June 2018, mothers were enrolled who met inclusion criteria: (1) having a daughter aged 14–17; (2) living in one of 34 U.S. states without a complete ban on IT by minors; (3) reading English; (4) having a Facebook account and logging in at least once per week; and (5) willing to “friend” the community manager of the project to join a private Facebook group. Mothers were excluded if they were unable to read English or did not consent and “friend” the community manager. Initially, mothers were recruited in Tennessee through community-based methods (e.g., working with Coordinated School Health coordinators, presentations at community events, and outcalls from a survey center). When these methods did not yield a sufficient number of mothers, Qualtrics was contracted and recruited mothers from its survey panel in 33 other states. All mothers were blind to treatment because they received a social media feed whose purpose was described as providing information on adolescent health and mother-daughter communication. Statistical power calculations provided a target sample size of 860 that would achieve 80% power for small to moderate effects. Mothers provided email addresses for daughters and parental consent, and daughters were invited to complete assessments, providing informed assent. To avoid a major recruitment barrier, the participation of the daughter was not required. When mothers had more than one daughter, the one with the nearest birthday was selected.
The research team developed a social media intervention, named Health Chat, using principles of social cognitive theory (SCT) (46), transportation theory (TT) (47), and diffusion of innovations theory (DIT) (48). The campaign also covered skills for communicating with teens (i.e., active listening, self-disclosure, empathy, and conflict management). Posts sought to create transportation into and identification with stories by linking to narratives from mothers and daughters about health risks, not giving permission for risky behaviors, and avoiding engaging in risky behaviors oneself (47, 49). Posts referenced current events and public figures to heighten the engagement of the mothers and encouraged mothers to react to (e.g., like) and comment on posts to evoke social comparison processes that can build norms (50, 51). Posts included social norms-based appeals, appearance-based messaging, and health-risk messaging.
Messages were created by investigators and reviewed by the entire team for acceptability and readability. Initial messages were pretested in a pilot feed with mothers (n = 90) not in the trial and changes were made to enhance aesthetics, message clarity, and engagement based on the results. Messages addressing current events were created during the intervention. Approximately 84% of posts addressed adolescent health topics and mother–daughter communication. Topics included vaccinations (e.g., influenza and human papillomavirus), mental health (e.g., stress and bullying), substance use (e.g., alcohol, cannabis, and tobacco), healthy lifestyles (e.g., physical activity and nutrition), media literacy, and general parenting (e.g., college preparation). They were selected based on formative research with mothers, engagement of the mothers during pilot testing, or emerging issues in comments of the mothers during the campaign. About 16% of posts focused on preventing IT (intervention group) or prescription drug misuse (control group). The two private Facebook groups received the same feed of posts except for the manipulated posts on IT or prescription drug misuse.
Several techniques were used in an attempt to increase engagement by mothers with the social media feed. Almost all posts included an image or infographic, along with the text. Some included links to outside sources. Many posts included a question or conversation starter, such as “Do you know if your daughters is up-to-date on her vaccines?” to invite mothers to react to and comment on posts. Finally, posts on topics of high human interest but not tied to any of the specific health topics were included periodically in the feed, such as soliciting favorite recipes or book recommendations.
A group of posts promoted vaccination for HPV (n = 38 posts) and general vaccine information, including influenza vaccination (n = 49 posts). Regarding HPV, posts covered the need for the vaccine (perceived risk), percent of adolescents vaccinated, the proportion of parents choosing to vaccinate children against HPV (descriptive norms), how HPV vaccines are decreasing infection rates (response efficacy), and stories of women who died from cervical cancer (perceived severity) or parents who decided to vaccinate their children (identification). Posts on vaccination for other diseases addressed misinformation surrounding vaccines, the need for annual influenza shots (risk), vaccine safety and efficacy (response efficacy), adolescent vaccine schedules (how-to knowledge), and reducing barriers to vaccination. Posts were in didactic (e.g., providing facts about rates of HPV) and narrative (e.g., sharing a story about someone who died from cervical cancer) format. Narratives were intended to influence through a process of identification with the characters in the stories. The primary focus on communicating with mothers was appropriate as they drive decisions about HPV vaccines (52–54) although HPV vaccination may be one of the first opportunities to engage adolescent daughters in healthcare decision-making (55). The posts on HPV and other vaccinations were not randomly assigned; the feeds in both Facebook groups included these posts.
The social media campaign was run in two private Facebook groups. In these groups, posts, comments, reactions, and membership were only viewable to participants and they could not share group content with Facebook users outside the group. This prevented contamination. Messages were posted two times a day to each group over 12 months (~710 total posts). This rate was designed to be sufficient to influence but avoid message fatigue. A community manager scheduled posts, monitored reactions/comments, and replied to misinformation. In addition, mothers received a bi-weekly email newsletter highlighting the most popular recent posts.
The primary outcome measures in the baseline and 12- and 18-month posttest surveys in this analysis were self-reports of HPV vaccination by mothers. Mothers were asked if the daughter had been vaccinated for HPV and if so, how many shots had she received. Initiation of vaccination was defined as receipt of one-shot of HPV vaccine and completion was defined as two or three shots (two shots are recommended for girls under age 15 while three shots are recommended for girls aged 15–17). Daughters were asked these same questions for themselves.
Demographic characteristics were collected, namely, mother and daughter age and skin phenotype (e.g., eye color and hair color) (56). Mothers also reported on personal and family history of skin cancer and political ideology.
The engagement of the mothers with the HPV vaccination posts was measured by counting the number of reactions (i.e., like, love, and sad buttons) and comments to each post. Comments and reactions to posts on HPV and other vaccines were extracted by a trained research assistant at the end of the social media campaign, using Grytics software. The content of reactions was recorded (i.e., like, angry, love, haha, wow). Further, the content in the comments was coded by trained research staff. The comments were coded as favorable (i.e., positive discussion of HPV vaccine or statement daughter was vaccinated), unfavorable (i.e., critical of HPV vaccine or statement of hesitancy or refusal to vaccinate daughter), or neutral (i.e., part of general group dialogue but not related to HPV vaccination specifically). Each comment was coded by one research assistant and 60% were coded by a second coder to check inter-rater reliability (Krippendorff's alpha = 0.76). Emergent themes were then identified based on content codes.
Descriptive statistics were computed using SAS, Version 9.3. F-tests were utilized to determine if increases in HPV vaccination rates were statistically significant. Correlation coefficients were computed to compare mother and daughter reports. Multinomial logistic regression was fit to identify predictors of vaccine uptake from pre- to post-intervention. Alpha criterion level of 0.05 was set for all tests.
Demographic characteristics of the 869 mothers and 469 daughters enrolled in the study have been reported elsewhere (57). Briefly, mothers had a mean age of 43.1 years (SD = 6.6) and were 82.4% non-Hispanic white, 57.8% had a college education, and 51.1% had household incomes over $80,000. They were diverse on political ideology, with 24.5% conservative and 23.8% liberal, with the remaining half (51.7%), middle of the road. The daughters had a mean age of 15.3 years, 74.7% were non-Hispanic whites, and 24.8% had a high-risk skin type.
At baseline, 63.4% of mothers reported that their daughters had received at least one dose of the HPV vaccine, with 50.2% saying they had received two or three doses (i.e., possibly completed series, depending on the age of the daughter). At the 12-month posttest, 71.3% of mothers reported that daughters had received at least one dose of the HPV vaccine (pre/post comparison F = 14.05, p < 0.001) and 62.5% reported that daughters had received two or three vaccine doses (pre/post comparison F = 21.31, p < 0.001). Looking just at mothers whose daughters had not completed the HPV vaccine series at baseline (n = 293, 227 with no shots and 66 with one shot), 18.5% of daughters with no shots at baseline and 53.0% of those who had received one shot at baseline had completed the series at the 12-month follow-up (χ2 = 31.46, p < 0.001). At the 18-month posttest, 73.3% of mothers reported that daughters had received at least one dose of the HPV vaccine (pre/post comparison F = 20.15, p < 0.001), and 65.9% reported that daughters had received two or three vaccine doses (pre/post comparison F = 38.05, p < 0.001). Again, subsetting mothers whose daughters had not completed the HPV vaccine series at pretest (n = 328, 248 with no shots and 80 with one-shot), 22.2% of daughters with no shots at baseline, and 70.0% of those who had received one shot at baseline had completed the series at the 18-month follow-up (χ2 = 61.79, p < 0.001). Reports of the mothers of HPV vaccine uptake were corroborated by daughters (82.1–88.4% correspondence, r = 0.65–0.76, p < 0.001).
For social media posts on HPV vaccines (n = 38), 8.1% of mothers reacted to a post (n = 162 reactions total), and 68.4% of all HPV vaccine posts received a reaction (63.2% like; 13.2% love, 7.9% sad). In addition, 7.6% of mothers commented on an HPV vaccine post (n = 123 comments total; 54 unfavorable, 68 favorable, 1 neutral), and 50.0% of all HPV vaccine posts received a comment. Similarly, for posts on other vaccines, 5.4% of mothers reacted to a post (n = 97 reactions total) and 71.4% of the posts on other vaccines received a reaction (59.2% like; 0.0% love; 12.2% sad). In addition, 4.6% of mothers commented on posts on other vaccines (n = 67 comments total; 14 unfavorable, 48 favorable, 5 neutral), and 42.9% of these posts on other vaccines received a comment. Looking at all posts in the feed, 55.8% of mothers reacted to a post and 68.2% of posts received a reaction. In addition, 58.5% of mothers commented on a post and 53.8% of posts received a comment.
Content analysis of all vaccination comments was done to explore themes for both favorable and unfavorable comments (Table 1). Favorable themes included the daughters were vaccinated, boys, as well as girls, should be vaccinated, benefits of vaccines outweigh the risks, vaccines reduced rates of disease, and physician supported vaccination. Unfavorable themes included daughter received certain vaccines but not others; lack of efficacy, safety concerns, or fear of unknown long-term side effects; negative stories or vague unfavorable “issues” regarding vaccination; mistrust in sources promoting vaccines; and lack of physician support for vaccination. In addition, 4.9% of comments on HPV posts mentioned sexual activity related to decision-making about getting daughters vaccinated.
We explored the relationship between the engagement of the mothers with HPV and other vaccine posts and the status of the vaccine of their daughters. Specifically, we explored whether reactions and comments were associated with pre/post-change in vaccine status. We fit three multinomial logistic regressions, subsetting to include only mothers who reported that their daughters had not completed the HPV vaccine series at baseline. Counts of reactions and comments to HPV vaccine posts (zero vs. 2/3 doses: estimate = −0.24, t = 0.59, p = 0.56; 1 vs. 2/3 doses: estimate = −0.26, t = −0.37, p = 0.71) and other vaccine posts (estimate = −117, t = −1.08, p = 0.28; estimate = 0.04, t = 0.08, p = 0.93) did not differ by vaccine status at 18-month posttest.
Instead, baseline vaccine status was associated with the valence of comments to HPV vaccine posts (Table 2). More vaccine-favorable comments to HPV vaccine posts were made by mothers whose daughters had completed the HPV series at baseline. A few mothers whose daughters were unvaccinated also made favorable comments but mothers whose daughters had initiated but not completed the series made very few favorable comments. By contrast, vaccine-unfavorable comments were made primarily by mothers whose daughters were not vaccinated at baseline. Mothers whose daughters had completed the HPV series at baseline or had initiated but not completed the series made almost no unfavorable comments to the HPV vaccination posts. Although mothers made fewer comments to posts on other vaccines, this same pattern emerged among mothers based on the status of the baseline vaccination of the daughters.
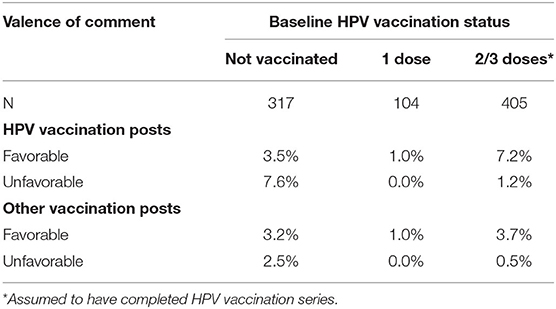
Table 2. Valence of comments to HPV and other vaccination posts by HPV vaccine status of daughter at baseline.
Human papillomavirus vaccine uptake for daughters increased during the 12-month period of the social media campaign. The largest increase appeared in the completion of the series, with smaller changes in the initiation of the series. It is not clear in the pre–post comparison whether these changes were due to the social media campaign, especially since engagement with posts was not related to the pre–post increase in HPV vaccine uptake. Unfortunately, Facebook stopped reporting whether participants viewed posts during the study, so we were limited to counting comments and reactions as indicators of engagement. However, mothers could have viewed posts without commenting on or reacting to them. Other research has shown that users following social media pages who view but do not comment may still be engaged with the content but may be concerned about privacy or have stronger information needs than social interaction needs (58–61). These users can be affected by the posts and pass the information along to others (61, 62). Thus, the number of comments and reactions may have under-estimated actual engagement with the posts in this study.
The effect of the campaign on the completion of the HPV vaccine series may have been slightly greater than on initiation of it for daughters. These mothers may be more inclined to vaccinate daughters than those who had not initiated the series in general, although some remained incomplete at the posttests. The campaign may have nudged some mothers who had started the HPV vaccine series for their daughters prior to the study to take steps to complete the series during the campaign or in the 6 months after it ended, as 70% of mothers whose daughters had received only one shot at baseline reported they had completed the series by the 18-month posttest. A much smaller proportion (18% at 12 months and 22% at 18 months) of those who had not yet vaccinated their daughters at the beginning of the trial had completed the HPV vaccine series at either posttest than those whose daughters who had already had one dose at baseline (53% and 70%).
A sizable group of mothers (27%) had daughters who remained unvaccinated throughout the trial and this group was more likely to post unfavorable comments, suggesting that some of these mothers with unvaccinated daughters were actively resistant to HPV posts. Vaccine-critical comments might be used to identify mothers who are resistant to HPV vaccines and tailor posts to respond to reasons for vaccine hesitancy expressed in their comments. By contrast, mothers who had initiated but not completed HPV vaccination did not comment much either favorably or unfavorably on posts about it. This latter group may have been uncertain about whether to complete it or had barriers to completion, but they were also not strongly resistant to the vaccine. The social media campaign may have nudged some of them to get the HPV vaccine series completed.
Less than 10% of mothers engaged with the posts on HPV vaccination (i.e., reacted or commented) but the number of posts that received a reaction or comment was similar in rate to all posts in the feed. The most common comment in response to HPV vaccine posts was a mother sharing that she had her daughter vaccinated. For this reason, mothers who complete the HPV vaccine series for their daughters might be recruited as influencers on HPV vaccines in future vaccine-promotion programs, as some appear predisposed to talk favorably about the vaccine. However, they may need to be instructed on how to make comments that are likely to influence other mothers because many just simply commented that they had vaccinated their daughters without providing other information that might be influential such as noting the benefits of disease prevention or that physicians recommended it. This same tendency, seen in an early analysis of comments to initial posts (45), continued throughout the social media campaign. Simple statements may help increase perceived descriptive norms for HPV vaccination, which might influence some mothers to vaccinate their daughters (63, 64). But, for many hesitant or resistant mothers, simply providing more information or fact-checking misinformation may not be sufficient. Additional strategies, such as counter-narratives, peer correction, factual elaboration, coherence/credibility appeals, and developing media and e-Health literacy skills (45, 65–71), may be needed to dispel the concerns about lack of efficacy, safety and harmful side-effects, and mistrust of organizations and agencies promoting HPV vaccines. These same vaccine-critical comments about safety and efficacy have been documented in other studies of social media content on HPV vaccines (72–79) and seem to have resonated with some mothers. Sharing stories about why mothers vaccinated daughters for HPV may help correct misinformation and overcome mistrust as stories can influence through identifying with characters, shifting social norms, and reducing counter-arguments by being transported into the stories (49, 80–82). Some mothers shared stories in unfavorable comments in this study and others (22, 23), and they may have had a strong negative impact. Comments and reactions from mothers who have not vaccinated daughters for HPV should also be monitored for misinformation on vaccines, which should be addressed quickly to help forestall it from going viral (65).
The comments that physicians did not support HPV vaccination need to be countered as medical professionals can be important, credible, and influential sources of information on HPV vaccination (14, 83–85). Mistrust in organizations and agencies promoting the HPV vaccine has been observed in other analyses (72, 74, 76, 86) and may be instrumental for hesitant or resistant mothers. Derogating the source is one way to reduce the perceived risk for not vaccinating their daughters when they have decided not to use it and rely instead on less effective prevention methods (87, 88).
The study had several limitations. The lack of randomization and absence of a control group undermined conclusions about whether the social media campaign produced the observed change in HPV vaccination rates at posttest. The number of messages specifically on HPV vaccination was small (about 5% of all posts) but they were supplemented by nearly 50 posts on other vaccinations (e.g., influenza) which should have improved vaccination intentions in general. The measurement times at 12- and 18-months post-randomization were long and risk history effects, where secular events (changes in personal health history; visits to physician offices, and other media coverage on HPV, vaccines, or health topics) could have occurred after the HPV vaccination messages that influenced decisions of the parents to vaccinate daughters. Once again, the lack of randomization meant the design could not control for this threat to internal validity. The inability to collect data on views from the Facebook feed meant we could not determine whether mothers saw the HPV and other vaccination posts. The decision by Facebook to eliminate reports on views of posts in the private groups was out of our control and occurred after the study was launched. We contacted Facebook and requested access to the views data but they were unable to provide it. Instead, we decided to use counts of reactions and comments to the vaccination posts, which were still reported by Facebook, as indicators of viewership, but as noted above these likely under-estimated actual engagement with the vaccination posts. It is worth noting that the lack of an objective measure of exposure to campaign messages by individual respondents often is limited in community-based evaluations of public health campaigns that rely on other media such as television, radio, print, and billboards. While the sample was large and included mothers from 34 states of the US, it may have limited generalizability because mothers were predominately non-Hispanic white and had regular social media use, the Qualtrics survey panel tends toward participants with higher socioeconomic status, mothers who chose to participate were interested in their health of the daughters, mothers lived in states that may be less socially progressive as they did not have bans on indoor tanning by minors, and daughters were older than the first age at which HPV vaccination is recommended. Self-reports of vaccine status of the mothers also may be biased but these measures have shown good specificity and sensitivity in past surveys (89–91) and produced estimates similar to government immunization records (92). Further, they were corroborated by reports of the daughters. The limitations were offset somewhat by strengths in the study: mothers were enrolled and pretested prior to the social media campaign and a pre-post change was observed, rather than inferring pre-existing vaccination beliefs and actions of the mothers.
Human papillomavirus vaccination rates in the United States continue to lag national health goals. Social media is a major source of health information and supportive and critical information on HPV vaccination. Effective strategies are needed in social media to promote HPV vaccines and counter misinformation about them to move mothers who are resisting vaccination. Interspersing vaccine messages in a feed for parents may be effective, as it can expose them to a large number of messages. Even if social media messaging does not change the minds of highly resistant mothers who contribute unfavorable comments, carefully crafted messages may convince mothers who are uninformed, uncertain, or not currently taking action to vaccine their daughters to ignore or resist the false claims and misinformation about the HPV vaccine and complete the series for their daughters.
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
The studies involving human participants were reviewed and approved by The Western Institutional Review Board and the IRBs at East Tennessee State University and University of Connecticut. Written informed consent to participate in this study was provided by the participants' legal guardian/next of kin.
DB: conceptualization, methodology, verification, investigation, writing—original draft, visualization, supervision, project administration, and funding acquisition. SP: conceptualization, methodology, verification, investigation, resources, writing—review and editing, supervision, project administration, and funding acquisition. KH: conceptualization, methodology, formal analysis, writing—review and editing, and funding acquisition. JBe: verification, validation, investigation, resources, data curation, writing—review and editing, and supervision. BW: conceptualization, methodology, investigation, writing—review and editing, resources, and funding acquisition. JBi: verification, validation, investigation, resources, data curation, writing—review and editing, and supervision. KB: conceptualization, methodology, investigation, writing—review and editing, supervision, project administration, and funding acquisition. JH: conceptualization, methodology, investigation, writing—review and editing, and funding acquisition. KA: verification, validation, investigation, data curation, and writing—review and editing. All authors contributed to the article and approved the submitted version.
This research was funded by the National Cancer Institute (CA192652), which had no role in study design, collection, analysis, or interpretation of data, report preparation, or decision to submit the report for publication.
DB's spouse is an owner of Klein Buendel, Inc. and he receives a salary from Klein Buendel. JBe and BW receive a salary from Klein Buendel, Inc.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Meites E, Szilagyi PG, Chesson HW, Unger ER, Romero JR, Markowitz LE. Human papillomavirus vaccination for adults: updated recommendations of the Advisory Committee on Immunization Practices. MMWR Morb Mortal Wkly Rep. (2019) 68:698–702. doi: 10.15585/mmwr.mm6832a3
2. Elam-Evans LD, Yankey D, Singleton JA, Sterrett N, Markowitz LE, Williams CL, et al. National, regional, state, and selected local area vaccination coverage among adolescents aged 13–17 years — United States, 2019. Morb Mortal Weekly Rep. (2020) 69:1109–16. doi: 10.15585/mmwr.mm6933a1
3. Fiks AG, Grundmeier RW, Mayne S, Song L, Feemster K, Karavite D, et al. Effectiveness of decision support for families, clinicians, or both on HPV vaccine receipt. Pediatrics. (2013) 131:1114–24. doi: 10.1542/peds.2012-3122
4. Zimet GD, Perkins SM, Winston Y, Kee R. Predictors of first and second dose acceptance of hepatitis B vaccine among STD clinic patients. Int J STD AIDS. (2008) 19:246–50. doi: 10.1258/ijsa.2007.007136
5. Chao C, Preciado M, Slezak J, Xu L. A randomized intervention of reminder letter for human papillomavirus vaccine series completion. J Adolesc Health. (2015) 56:85–90. doi: 10.1016/j.jadohealth.2014.08.014
6. Wilson AR, Hashibe M, Bodson J, Gren LH, Taylor BA, Greenwood J, et al. Factors related to HPV vaccine uptake and 3-dose completion among women in a low vaccination region of the USA: an observational study. BMC Womens Health. (2016) 16:41. doi: 10.1186/s12905-016-0323-5
7. World Health Organization. Ten Threats to Global Health in 2019 Geneva, Switzerland. Available online at: https://www.who.int/emergencies/ten-threats-to-global-health-in-2019 (accessed March 18, 2021).
8. Division of Cancer Prevention and Control Centers for Disease Control and Prevention. National Comprehensive Cancer Control Program. Avaialble online at: https://www.cdc.gov/cancer/ncccp/priorities/index.htm (accessed March 18, 2021).
9. Cohall AT, Cohall R, Dye B, Dini S, Vaughan RD. Parents of urban adolescents in Harlem, New York, and the Internet: a cross-sectional survey on preferred resources for health information. J Med Internet Res. (2004) 6:e43. doi: 10.2196/jmir.6.4.e43
10. Khoo K, Bolt P, Babl FE, Jury S, Goldman RD. Health information seeking by parents in the Internet age. J Paediatr Child Health. (2008) 44:419–23. doi: 10.1111/j.1440-1754.2008.01322.x
11. Tuffrey C, Finlay F. Use of the internet by parents of paediatric outpatients. Arch Dis Child. (2002) 87:534–6. doi: 10.1136/adc.87.6.534
12. Margolis MA, Brewer NT, Shah PD, Calo WA, Gilkey MB. Stories about HPV vaccine in social media, traditional media, and conversations. Prev Med. (2019) 118:251–6. doi: 10.1016/j.ypmed.2018.11.005
13. Hughes J, Cates JR, Liddon N, Smith JS, Gottlieb SL, Brewer NT. Disparities in how parents are learning about the human papillomavirus vaccine. Cancer Epidemiol Biomarkers Prev. (2009) 18:363–72. doi: 10.1158/1055-9965.EPI-08-0418
14. Brunson EK. The impact of social networks on parents' vaccination decisions. Pediatrics. (2013) 131:e1397–404. doi: 10.1542/peds.2012-2452
15. Penta MA, Baban A. Dangerous agent or saviour? HPV vaccine representations on online discussion forums in Romania. Int J Behav Med. (2014) 21:20–8. doi: 10.1007/s12529-013-9340-z
16. Sutton J. Health communication trolls and bots versus public health agencies' trusted voices. Am J Public Health. (2018) 108:1281–2. doi: 10.2105/AJPH.2018.304661
17. Broniatowski DA, Jamison AM, Qi S, AlKulaib L, Chen T, Benton A, et al. Weaponized health communication: twitter bots and Russian trolls amplify the vaccine debate. Am J Public Health. (2018) 108:1378–84. doi: 10.2105/AJPH.2018.304567
18. Kata A. Anti-vaccine activists, Web 2.0, and the postmodern paradigm–an overview of tactics and tropes used online by the anti-vaccination movement. Vaccine. (2012) 30:3778–89. doi: 10.1016/j.vaccine.2011.11.112
19. Witteman HO, Zikmund-Fisher BJ. The defining characteristics of Web 2.0 and their potential influence in the online vaccination debate. Vaccine. (2012) 30:3734–40. doi: 10.1016/j.vaccine.2011.12.039
20. Betsch C, Brewer NT, Brocard P, Davies P, Gaissmaier W, Haase N, et al. Opportunities and challenges of Web 2.0 for vaccination decisions. Vaccine. (2012) 30:3727–33. doi: 10.1016/j.vaccine.2012.02.025
21. Luisi MLR. From bad to worse: the representation of the HPV vaccine Facebook. Vaccine. (2020) 38:4564–73. doi: 10.1016/j.vaccine.2020.05.016
22. Fu LY, Zook K, Spoehr-Labutta Z, Hu P, Joseph JG. Search engine ranking, quality, and content of web pages that are critical versus noncritical of human papillomavirus vaccine. J Adolesc Health. (2016) 58:33–9. doi: 10.1016/j.jadohealth.2015.09.016
23. Madden K, Nan X, Briones R, Waks L. Sorting through search results: a content analysis of HPV vaccine information online. Vaccine. (2012) 30:3741–6. doi: 10.1016/j.vaccine.2011.10.025
24. Okuhara T, Ishikawa H, Okada M, Kato M, Kiuchi T. Amount of narratives used on Japanese pro- and anti-HPV vaccination websites: a content analysis. Asian Pac J Cancer Prev. (2018) 19:2691–4. doi: 10.22034/APJCP.2018.19.10.2691
25. Bonnevie E, Goldbarg J, Gallegos-Jeffrey AK, Rosenberg SD, Wartella E, Smyser J. Content themes and influential voices within vaccine opposition on Twitter, 2019. Am J Public Health. (2020) 110:S326–S30. doi: 10.2105/AJPH.2020.305901
26. Jamison A, Broniatowski DA, Smith MC, Parikh KS, Malik A, Dredze M, et al. Adapting and extending a typology to identify vaccine misinformation on Twitter. Am J Public Health. (2020) 110:S331–S9. doi: 10.2105/AJPH.2020.305940
27. Lama Y, Hu D, Jamison A, Quinn SC, Broniatowski DA. Characterizing trends in human papillomavirus vaccine discourse on Reddit (2007-2015): an observational study. JMIR Public Health Surveill. (2019) 5:e12480. doi: 10.2196/12480
28. Nan X, Madden K. HPV vaccine information in the blogosphere: how positive and negative blogs influence vaccine-related risk perceptions, attitudes, and behavioral intentions. Health Commun. (2012) 27:829–36. doi: 10.1080/10410236.2012.661348
29. Betsch C, Renkewitz F, Betsch T, Ulshofer C. The influence of vaccine-critical websites on perceiving vaccination risks. J Health Psychol. (2010) 15:446–55. doi: 10.1177/1359105309353647
30. Betsch C, Renkewitz F, Haase N. Effect of narrative reports about vaccine adverse events and bias-awareness disclaimers on vaccine decisions: a simulation of an online patient social network. Med Decis Makin. (2013) 33:14–25. doi: 10.1177/0272989X12452342
31. McRee AL, Reiter PL, Brewer NT. Parents' Internet use for information about HPV vaccine. Vaccine. (2012) 30:3757–62. doi: 10.1016/j.vaccine.2011.11.113
32. Ernst K, Shelby A. Social media in the exam room: stories of human papillomavirus disease and prevention. Acad Pediatr. (2018) 18:S19–S20. doi: 10.1016/j.acap.2017.05.002
33. Shapiro GK, Surian D, Dunn AG, Perry R, Kelaher M. Comparing human papillomavirus vaccine concerns on Twitter: a cross-sectional study of users in Australia, Canada and the UK. BMJ Open. (2017) 7:e016869. doi: 10.1136/bmjopen-2017-016869
34. Du J, Xu J, Song H, Liu X, Tao C. Optimization on machine learning based approaches for sentiment analysis on HPV vaccines related tweets. J Biomed Semant. (2017) 8:9. doi: 10.1186/s13326-017-0120-6
35. Wang Y, McKee M, Torbica A, Stuckler D. Systematic literature review on the spread of health-related misinformation on social media. Soc Sci Med. (2019) 240:112552. doi: 10.1016/j.socscimed.2019.112552
36. Baumann A, Andersen B, Østergaard L, Larsen MB. Sense and sensibility: decision-making and sources of information in mothers who decline HPV vaccination of their adolescent daughters. Vaccine: X. (2019) 2:100020. doi: 10.1016/j.jvacx.2019.100020
37. Chou WYS, Prestin A, Lyons C, Wen KY. Web 2.0 for health promotion: reviewing the current evidence. Am J Public Health. (2013) 103:e9–e18. doi: 10.2105/AJPH.2012.301071
38. Vaccine Safety Communication in the Digital Age. 2018 Meeting Report, Veyrier-du-Lac, Francy, 4-5 June 2018. Geneva: WHO/MVP/EMP/SAV/2019.02 (2019).
39. Chou W-YS, Oh A, Klein WMP. Addressing health-related misinformation on social media. JAMA. (2018) 320:2417–8. doi: 10.1001/jama.2018.16865
40. Yang YT, Broniatowski DA, Reiss DR. Government role in regulating vaccine misinformation on social media platforms. JAMA Pediatrics. (2019) 73:1011–12. doi: 10.1001/jamapediatrics.2019.2838
41. Chou W-YS, Gaysynsky A, Cappella JN. Where we go from here: health misinformation on social media. Am J Public Health. (2020) 110:S273–S5. doi: 10.2105/AJPH.2020.305905
42. Dunn AG, Surian D, Leask J, Dey A, Mandl KD, Coiera E. Mapping information exposure on social media to explain differences in HPV vaccine coverage in the United States. Vaccine. (2017) 35:3033–40. doi: 10.1016/j.vaccine.2017.04.060
43. Glanz JM, Wagner NM, Narwaney KJ, Kraus CR, Shoup JA, Xu S, et al. Web-based social media intervention to increase vaccine acceptance: a randomized controlled trial. Pediatrics. (2017) 140:e20171117. doi: 10.1542/peds.2017-1117
44. Ortiz RR, Shafer A, Cates J, Coyne-Beasley T. Development and evaluation of a social media health intervention to improve adolescents' knowledge about and vaccination against the human papillomavirus. Glob Pediatr Health. (2018) 5:2333794X18777918. doi: 10.1177/2333794X18777918
45. Buller D, Walkosz B, Berteletti J, Pagoto SL, Bibeau J, Baker K, et al. Insights on HPV vaccination in the United States from mothers' comments on Facebook posts in a randomized trial. Hum Vaccin Immunother. (2019) 15:1479–87. doi: 10.1080/21645515.2019.1581555
46. Bandura A. Health promotion by social cognitive means. Health Educ Behav. (2004) 31:143–64. doi: 10.1177/1090198104263660
47. Green MC. Narratives and cancer communication. J Commun. (2006) 56:S163℃S83. doi: 10.1111/j.1460-2466.2006.00288.x
49. Slater MD, Buller DB, Waters E, Archibeque M, LeBlanc M. A test of conversational and testimonial messages versus didactic presentations of nutrition information. J Nutr Educ Behav. (2003) 35:255–9. doi: 10.1016/S1499-4046(06)60056-0
52. Zawistowski CA, Frader JE. Ethical problems in pediatric critical care: consent. Crit Care Med. (2003) 31:S407–S10. doi: 10.1097/01.CCM.0000065274.46402.DB
53. Fost N. Parents as decision makers for children. Primary Care. (1986) 13:285–93. doi: 10.1016/S0095-4543(21)00979-9
54. Woodall WG, Starling R, Buller D, Donohew L, Zimmerman R, Helme D. DA018575: Web-Based Substance Abuse and STD/HIV Prevention. (2009). Available online at: http://projectreporter.nih.gov/project_info_description.cfm?aid=7914379&icde=23322944&ddparam=&ddvalue=&ddsub=&cr=8&csb=default&cs=ASC (accessed March 18, 2021).
55. Alexander AB, Stupiansky NW, Ott MA, Herbenick D, Reece M, Zimet GD. Parent-son decision-making about human papillomavirus vaccination: a qualitative analysis. BMC Pediatr. (2012) 12:192. doi: 10.1186/1471-2431-12-192
56. Berwick M, Armstrong BK, Ben-Porat L, Fine J, Kricker A, Eberle C, et al. Sun exposure and mortality from melanoma. J Natl Cancer Inst. (2005) 97:195–9. doi: 10.1093/jnci/dji019
57. Buller DB, Pagoto S, Baker K, Walkosz BJ, Hillhouse J, Henry KL, et al. Results of a social media campaign to prevent indoor tanning by teens: a randomized controlled trial. Prev Med Rep. (2021) 22:101382. doi: 10.1016/j.pmedr.2021.101382
58. Osatuyi B. Is lurking an anxiety-masking strategy on social media sites? The effects of lurking and computer anxiety on explaining information privacy concern on social media platforms. Comput Human Behav. (2015) 49:324–32. doi: 10.1016/j.chb.2015.02.062
59. Muntinga DG, Moorman M, Smit EG. Introducing COBRAs. Int J Advert. (2011) 30:13–46. doi: 10.2501/IJA-30-1-013-046
60. Khan ML. Social media engagement: what motivates user participation and consumption on YouTube? Comput Human Behav. (2017) 66:236–47. doi: 10.1016/j.chb.2016.09.024
61. Fernandes T, Castro A. Understanding drivers and outcomes of lurking vs. posting engagement behaviours in social media-based brand communities. J Market Manage. (2020) 36:660–81. doi: 10.1080/0267257X.2020.1724179
62. Chen X, Li X, Yao D, Zhou Z. Seeking the support of the silent majority: are lurking users valuable to UGC platforms? J Acad Market Sci. (2019) 47:986–1004. doi: 10.1007/s11747-018-00624-8
63. Lapinski MK, Rimal RN. An explication of social norms. Commun Theory. (2005) 15:127–47. doi: 10.1111/j.1468-2885.2005.tb00329.x
64. Rimal RN, Real K. Understanding the influence of perceived norms on behaviors. Commun Theory. (2003) 13:184–203. doi: 10.1111/j.1468-2885.2003.tb00288.x
65. Bode L, Vraga EK. See something, say something: correction of global health misinformation on social media. Health Commun. (2018) 33:1131–40. doi: 10.1080/10410236.2017.1331312
66. Vraga EK, Bode L. I do not believe you: how providing a source corrects health misperceptions across social media platforms. Inform Commun Soc. (2018) 21:1337–53. doi: 10.1080/1369118X.2017.1313883
67. van der Meer TGLA, Jin Y. Seeking formula for misinformation treatment in public health crises: The effects of corrective information type and source. Health Commun. (2020) 35:560–75. doi: 10.1080/10410236.2019.1573295
68. Walter N, Murphy ST. How to unring the bell: a meta-analytic approach to correction of misinformation. Commun Monogr. (2018) 85:423–41. doi: 10.1080/03637751.2018.1467564
69. Jacobs L, Kattumana T, Konnova A, Obasa M, Smlatic E, Vandendriessche V, et al. How storytelling can combat vaccine hesitancy: a transdisciplinary approach. Transdisciplin Insights. (2018) 2:92–103. doi: 10.11116/TDI2018.2.4
70. Vraga EK, Bode L. Correction as a solution for health misinformation on social media. Am J Public Health. (2020) 110:S278–S80. doi: 10.2105/AJPH.2020.305916
71. Tangcharoensathien V, Calleja N, Nguyen T, Purnat T, D'Agostino M, Garcia-Saiso S, et al. Framework for managing the COVID-19 infodemic: methods and results of an online, crowdsourced WHO technical consultation. J Med Internet Res. (2020) 22:e19659. doi: 10.2196/19659
72. Allen JD, de Jesus M, Mars D, Tom L, Cloutier L, Shelton RC. Decision-making about the HPV vaccine among ethnically diverse parents: implications for health communications. J Oncol. (2012) 2012:401979. doi: 10.1155/2012/401979
73. Beavis AL, Krakow M, Levinson K, Rositch AF. Reasons for persistent suboptimal rates of HPV vaccination in the US: shifting the focus from sexuality to education and awareness. Gynecol Oncol. (2017) 142:4. doi: 10.1016/j.ygyno.2017.03.032
74. Dempsey AF, Abraham LM, Dalton V, Ruffin M. Understanding the reasons why mothers do or do not have their adolescent daughters vaccinated against human papillomavirus. Ann Epidemiol. (2009) 19:531–8. doi: 10.1016/j.annepidem.2009.03.011
75. Dilley SE, Peral S, Straughn JM Jr, Scarinci IC. The challenge of HPV vaccination uptake and opportunities for solutions: lessons learned from Alabama. Prev Med. (2018) 113:124–31. doi: 10.1016/j.ypmed.2018.05.021
76. Ferrer HB, Trotter C, Hickman M, Audrey S. Barriers and facilitators to HPV vaccination of young women in high-income countries: a qualitative systematic review and evidence synthesis. BMC Public Health. (2014) 14:700. doi: 10.1186/1471-2458-14-700
77. Gerend MA, Shepherd MA, Shepherd JE. The multidimensional nature of perceived barriers: global versus practical barriers to HPV vaccination. Health Psychol. (2013) 32:361–9. doi: 10.1037/a0026248
78. Kester LM, Zimet GD, Fortenberry JD, Kahn JA, Shew ML. A national study of HPV vaccination of adolescent girls: rates, predictors, and reasons for non-vaccination. Matern Child Health J. (2013) 17:879–85. doi: 10.1007/s10995-012-1066-z
79. Zimet GD, Rosberger Z, Fisher WA, Perez S, Stupiansky NW. Beliefs, behaviors and HPV vaccine: correcting the myths and the misinformation. Prev Med. (2013) 57:414–8. doi: 10.1016/j.ypmed.2013.05.013
80. Green MC, Brock TC. The role of transportation in the persuasiveness of public narratives. J Pers Soc Psychol. (2000) 79:701–21. doi: 10.1037/0022-3514.79.5.701
81. Green MC, Brock TC. In the mind's eye: transportation-imagery model of narrative persuasion. In: Green MC, Strange JJ, Brock TC, editors. Narrative Impact: Social and Cognitive Foundations. Mahwah, NJ: Erlbaum (2002). p. 315–41.
82. Cohen J. Defining identification: a theoretical look at identification of audiences with media characters. Mass Commun Soc. (2001) 4:245–64. doi: 10.1207/S15327825MCS0403_01
83. Baldwin AS, Bruce CM, Tiro JA. Understanding how mothers of adolescent girls obtain information about the human papillomavirus vaccine: associations between mothers' health beliefs, information seeking, and vaccination intentions in an ethnically diverse sample. J Health Psychol. (2013) 18:926–38. doi: 10.1177/1359105312445078
84. Cates JR, Shafer A, Carpentier FD, Reiter PL, Brewer NT, McRee AL, et al. How parents hear about human papillomavirus vaccine: implications for uptake. J Adolesc Health. (2010) 47:305–8. doi: 10.1016/j.jadohealth.2010.04.003
85. Lai D, Bodson J, Davis FA, Lee D, Tavake-Pasi F, Napia E, et al. Diverse families' experiences with HPV vaccine information sources: a community-based participatory approach. J Community Health. (2017) 42:400–12. doi: 10.1007/s10900-016-0269-4
86. Hendry M, Lewis R, Clements A, Damery S, Wilkinson C. “HPV? Never heard of it!”: a systematic review of girls' and parents' information needs, views and preferences about human papillomavirus vaccination. Vaccine. (2013) 31:5152–67. doi: 10.1016/j.vaccine.2013.08.091
87. Witte K. Putting the fear back into fear appeals: the extended parallel process model. Commun Monogr. (1992) 59:329–49. doi: 10.1080/03637759209376276
88. Witte K, Meyer G, Martell D. Effective Health Risk Messages: A Step-By-Step Guide. Thousand Oaks, CA: Sage Publications (2001).
89. Boakye EA, Tobo BB, Osazuwa-Peters N, Mohammed KA, Geneus CJ, Schootman M. A comparison of parent-and provider-reported human papillomavirus vaccination of adolescents. Am J Prev Med. (2017) 52:742–52. doi: 10.1016/j.amepre.2016.10.016
90. Attanasio L, McAlpine D. Accuracy of parental reports of children's HPV vaccine status: implications for estimates of disparities, 2009–2010. Public Health Rep. (2014) 129:237–44. doi: 10.1177/003335491412900305
91. Ojha RP, Tota JE, Offutt-Powell TN, Klosky JL, Ashokkumar R, Gurney JG. The accuracy of human papillomavirus vaccination status based on adult proxy recall or household immunization records for adolescent females in the United States: results from the National Immunization Survey-Teen. Ann Epidemiol. (2013) 23:281–5. doi: 10.1016/j.annepidem.2013.02.002
92. Ogilvie G, Anderson M, Marra F, McNeil S, Pielak K, Dawar M, et al. A population-based evaluation of a publicly funded, school-based HPV vaccine program in British Columbia, Canada: parental factors associated with HPV vaccine receipt. PLoS Med. (2010) 7:e1000270. doi: 10.1371/journal.pmed.1000270
Keywords: human papillomavirus, vaccine, social media, mothers, adolescents
Citation: Buller DB, Pagoto S, Henry K, Berteletti J, Walkosz BJ, Bibeau J, Baker K, Hillhouse J and Arroyo KM (2021) Human Papillomavirus Vaccination and Social Media: Results in a Trial With Mothers of Daughters Aged 14–17. Front. Digit. Health 3:683034. doi: 10.3389/fdgth.2021.683034
Received: 19 March 2021; Accepted: 28 July 2021;
Published: 03 September 2021.
Edited by:
Heather M. Brandt, St. Jude Children's Research Hospital, United StatesReviewed by:
Parisis Gallos, National and Kapodistrian University of Athens, GreeceCopyright © 2021 Buller, Pagoto, Henry, Berteletti, Walkosz, Bibeau, Baker, Hillhouse and Arroyo. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: David B. Buller, ZGJ1bGxlckBrbGVpbmJ1ZW5kZWwuY29t
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.