- 1Colorado School of Public Health, University of Colorado, Anschutz Medical Campus, Aurora, CO, United States
- 2School of Medicine, University of Colorado, Anschutz Medical Campus, Aurora, CO, United States
Digital health remains a growing and challenging niche in public health practice. Academic-industry collaboration (AIC) offers a mechanism to bring disparate sectors together to alleviate digital health challenges of engagement, reach, sustainability, dissemination, evaluation, and equity. Despite the ongoing endorsements for AIC in digital health, limited understanding exists of successful AIC exists. Most published research highlights the barriers of collaboration rather than efficacy, leaving collaborators asking: What are the benefits and facilitators of AIC and do they apply in digital health? As an initial effort to fill the gap in the literature, the purpose of this mini review outlines the benefits and facilitators from previous AIC and offers recommendations specific to digital health.
Introduction
Digital health remains a growing and challenging niche in public health practice, particularly given the COVID-19 pandemic (1–5). Increasingly, the use of digital technology to deploy health programs are often thwarted by challenges of engagement, reach, sustainability, dissemination, evaluation, and equity (6, 7). Such digital health challenges persist in the business, technology, and health-care literature. Lagging research methods limit meaningful evidence, thus restricting understanding of efficacy and quality of digital health solutions (8). Digital health end-user engagement remains complex, demanding personalization and adaptive interventions that meet the needs for diverse populations (9). Health-care reimbursement complicates adoption and implementation, determining scale, and sustainability. Privacy and security issues raise warranted ethical discussions, thus demanding regulatory bodies to intervene with policy (10). Oftentimes, academic-industry collaboration (AIC) is endorsed as a mechanism to mitigate these barriers in digital health (11, 12). In response to the global COVID-19 pandemic, many digital health AIC emerged bringing cross-disciplinary sectors together (13–16).
Historically, diverse industries (e.g., semi-conductor, agriculture, space) leveraged AIC for scientific discovery and economic growth (17, 18). AIC has been observed in many clinical applications, yielding breakthroughs in biotechnology (biotech) and biomedicine (19, 20). More recently, in response to COVID-19, the company WHOOP partnered with universities and health system partners to clinical evaluate and deploy their digital respiratory wearable device (16). Similarly, companies like Apple and Fitbit collaborated with Duke University to monitor COVID-19 symptoms during sleep (21).
Many modern models of collaboration exist in digital health, reflecting traditional research and development (R&D) and innovative collaborative approaches [e.g., digital health ecosystems (22), competitions (23), cross-sector consortiums (24, 25), and industry partnerships with academic medical centers] (26–28). Despite AIC advocacy, hesitation remains due to the commonly reported misalignment between academia and industry. In the digital health field partnerships remain challenging due to conflicting priorities (29), values (30), approaches (31, 32), and expectations (33). Among ethical skepticism toward collaboration (34–37), barriers for collaboration include the initiation, maintenance, and sustainment of AICs (38–40).
The literature adequately reports challenges for AIC; however, it lacks a synthesis of benefits (e.g., outcomes) of partnerships and facilitators that guide such collaborations specific to digital health. With ongoing endorsement for AIC in digital health (11, 12, 27, 41, 42), initial investigation is needed to build consensus on best practices and approaches. The purpose of this mini review describes the benefits and facilitators of historical AIC and offers potential AIC recommendations specific to the digital health context.
Methods of Mini Review
The mini review informed a larger, more robust scoping review on the topic (43). Using the PRISMA Extension for Scoping Reviews (PRISMA-ScR) (44) as a guide, the mini review formatively examined benefits, barriers, and facilitators of collaborations between academic and industry in digital health. During May 2019–December 2019, the researchers searched an online database (i.e., Ovid MEDLINE) to identify published papers that examined AIC in digital health settings. Eligibility criteria included both qualitative and quantitative studies, published or translated in the English language, and mention controlled keywords and MeSH subject headings. Example search terms included: digital health (e.g., mHealth, eHealth, innovation, technology, mobile applications, telemedicine, electronic mail, technology, text messaging, information technology, virtual reality); AIC (e.g., public or private, academic, University, industry, startup, cross-sector, collaboration, partnership, cooperation, linkage); recommendations, barriers, and/or facilitators. No date range was included in the eligibility criteria due to the formative nature of the mini review. Search results were exported using software application (i.e., Endnote) for screening and full-text review. Abstracted data included: benefits of collaboration, barriers, facilitators, and recommendations for collaborations. The abstracted data synthesized a range of evidence where sources were thematically grouped and analyzed based on extracted data.
Benefits of Collaboration
Historically, AICs generate public health and economic benefits (i.e., outcomes of partnerships) (45). The literature reiterates that creativity and innovation emerge from heterogeneous perspectives (46, 47), and AICs serve as an intersection to advance that mission. (48) As economic drivers, AICs typically support businesses while leveraging University knowledge and insights (48, 49). Integrating academia and digital health industry improves translational medicine (50), particularly by creating business models that scale interventions to relevant populations. Such cross-sector alignment have reported helping health-care settings achieve the triple aim: (51) improving population health, care experiences, and reducing costs (52). As evidence accumulates, such comprehensive benefits of collaboration are projected to support the digital health field.
AIC cultivates innovation, benefiting both industry and academia. Both sectors may leverage partnership to maintain competitive advantage and advance science. The products from AIC allows industry to differentiate from competitors with scientific claims (39, 53). AIC better positions industry to profit when aligning with subject matter experts (54), improving regulatory appeals (55) and accessing innovative human capital (56, 57). Academic collaborators value from additional funding streams (39, 58, 59) and access to relevant innovations, inspiring new research directions (58). In addition, academic researchers benefit from the ability to extend evidence-based strategies to market for improved health outcomes (60), thus exploring commercialization as a sustainable form of dissemination (61). Such evidence suggests the outcomes of AIC are not unique to each respective field. Positive implications of AIC remain a standard product of interdisciplinary collaboration. Despite the reported benefits of AIC, initiating and executing partnerships in the real world proves challenging. The understanding of such partnerships remains limited (48, 62), particularly how these collaborations play out in the real world (63). While the literature adequately addresses barriers of collaboration, there lacks understanding of what facilitates digital health AIC, specifically the drivers that help guide the initiation and implementation of these partnerships in the real world.
Academic-Industry Collaboration Facilitators
Many sources describe high-level lessons learned that facilitate partnerships among academic and industry collaborators. Such facilitators may be applied to digital health, particularly how they relate to interpersonal dynamics, context, and understanding of success. The importance of collaboration engagement relies heavily on the ability to establish and maintain authentic relationships with all stakeholders (64). Shared expectations, co-creation, awareness of diverse values, and flexibility are commonly described in the literature as facilitators to AIC (18, 48, 65–67). Collaborators should remain reflexive, anticipating, reframing, and negotiating interests (48, 65). Such interpersonal attributes reiterate the importance of trust (48, 68, 69) and interdependency (11, 69), adopting a shared mutually understood language to promote productivity (7). Most sources report establishing a reciprocally beneficial relationship rooted in transparency of each collaborators' values and motivations (52, 70). The acknowledgment and appreciation of interpersonal factors facilitate AIC (18, 20, 48, 52, 56, 68–72).
Beyond a general awareness of strengths and weaknesses facilitating AIC, collaboration climate remains a key facilitator for partnership. Models of collaboration vary; however, intentionally initiated (34, 48, 65, 73), co-created (66, 74–76), well-defined workflows enhance collaboration and improve the quality of deliverables. Many facilitators of AIC rely on a joint structure (66, 71) to leverage strengths of each discipline, encouraging flexibility when possible. (65, 77) Many authors underscore role clarity, communication, iterative project management style, and phase of project or partnership impacted the AIC (18, 32, 48, 52, 56, 64, 71–73, 78–81). A reoccurring cadence of communication promotes partnership, specifically by creating structure around coordination and collaboration management (75, 82, 83). Understanding unique strengths, institutional factors, available infrastructure support, capacity, organizational climate, and overall readiness are reported facilitators of AIC (11, 52). Any gaps in understanding could be addressed early (32) and continually to better manage expectations throughout the collaboration (33).
To fully establish shared expectations, AICs recommend alignment of outputs and deliverables as an early facilitator of collaboration. Many outputs for AIC exist, such as patents, intellectual property, data ownership, and publications. Academic and industry collaborators report prioritizing deliverables differently; thus, a facilitator of partnerships ensures each collaborator obtains an equitable value from collaboration or end goal (32, 65). Similarly, the value for the partnership may differ; therefore, aligning on adoption (52) objectives and scientific advancements (84) prove beneficial for AIC. Determining scientific, economic, and social impact was a reported challenge for AIC; however, some sources recommended using system thinking principles to determine socioecological levels worth investigating in the real world (32, 79, 85). Many sources recommended evaluating and documenting learnings from partnerships (65), particularly to better inform future AIC in practice (40). Establishing evaluation expectations (e.g., results and performance metrics) is important for goal alignment but also determining the success of collaboration. “Successful” AIC varies, but many sources report metrics around balance, mutual benefit, partnership sustainability, and co-development and defined dissemination strategy to facilitate collaboration (32, 52, 56, 72). Such shared expectations and acknowledgments of diverse goals facilitate AIC across disciplines and may offer promise in the digital health field.
Recommendations for Digital Health Academic-Industry Collaboration
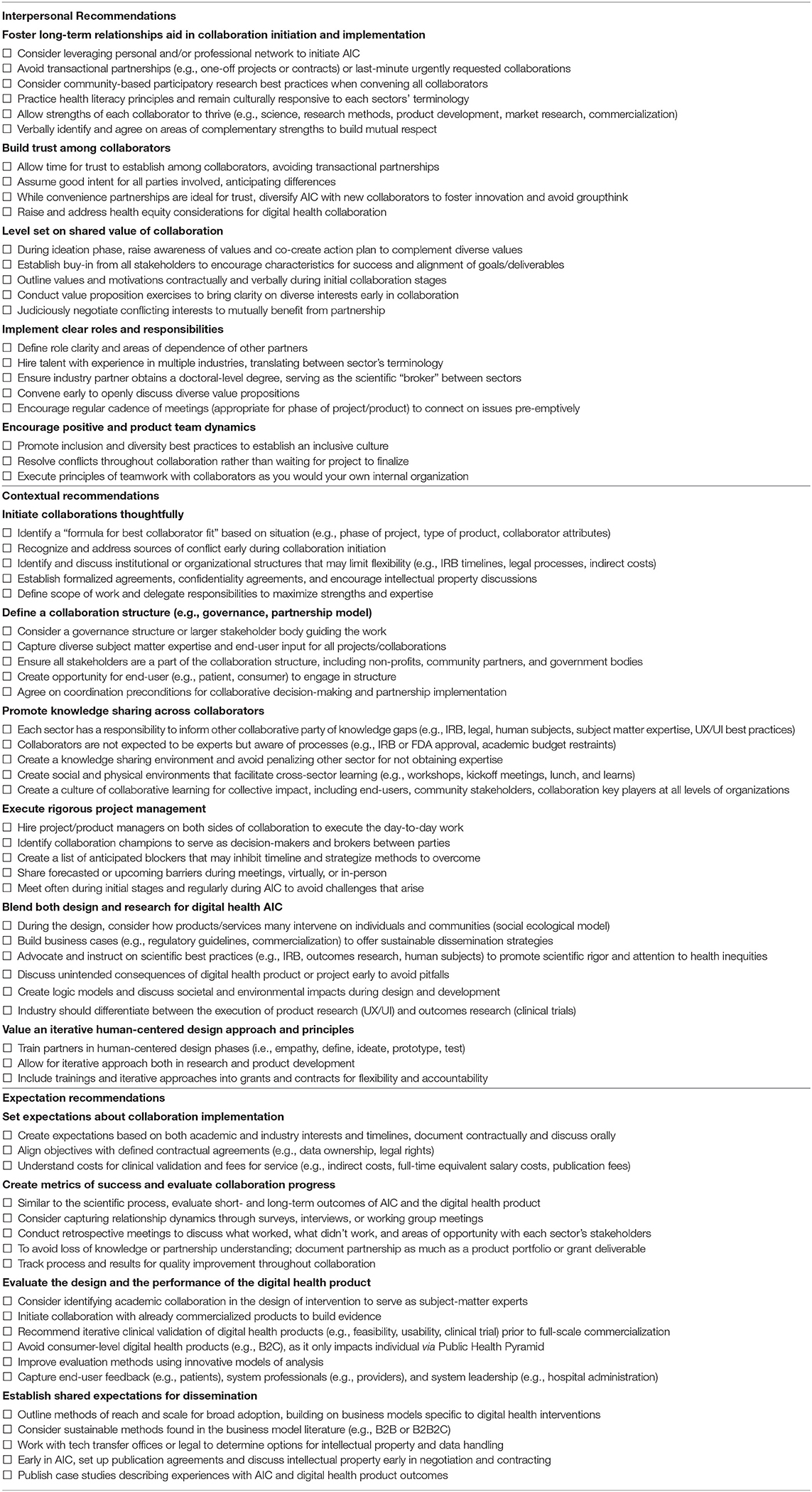
The mini review highlights the reported facilitators of AIC across many disciplines. First, on an interpersonal level, partnerships might consider initiating and implementing collaborations with trusted long-term relationships due to the historical differences between academia and industry. Leveraging trusted partners may improve shared values, clear roles and responsibilities, and encourage better team dynamics. Second, digital health AIC may consider thoughtful consideration of collaboration structure and knowledge sharing to promote understanding of business and market needs and scientific rigor. Given the nuances of technology and health interventions, project management that balances both design and research may promote flexibility, speed, and science. Third, while measuring success proves challenging, digital health AIC may consider setting clear expectations on the dissemination, implementation, partnership, and performance of the digital health product to avoid common conflict around evaluation and ownership.
Due to the barriers reported in the digital health field, such facilitators serve as an initial roadmap to guide both researchers and digital health companies looking to advance their technologies. Currently, there lacks consensus on models of collaboration relevant to digital health (18, 48, 86). Table 1 offers practical solutions, in the form of a check list for initiating and maintaining AIC in the digital health field.
Discussion
This mini review offers valuable insight for the wider scientific and digital health community, underscoring the opportunity in collaboration for public health purposes, serving as a blueprint for digital health researchers seeking industry collaboration. As the use of digital health continues to grow, it challenges practitioners, researchers, and technologists to explore ways to advance technologies for health-care delivery, disease prevention, and public health. Public-health efforts such as education, policy, research, and service implementation remain critical for advancing public health initiatives, however underscore the importance of collaborative practices (87). The collaboration literature echoes this philosophy, illustrating the benefits of heterogenous perspectives when solving for complex situations (47). Stakeholder engagement remains a responsibility of public health, engaging government, nonprofit organizations, and diverse community partners. Industry, particularly the digital health industry, is an additional key stakeholder for disease prevention and health promotion efforts.
In the last few years, researchers and policy makers endorsed interdisciplinary collaboration and future efforts to advance digital health technologies (11, 88, 89). This cross-sector collaboration sentiment is shared by top global health officials in response to the COVID-19 pandemic. The World Health Organization (WHO) presented a call to action for “a global collaboration to accelerate the development, production, and equitable access to new COVID-19 health technologies.” (15) Various innovative diagnostics, therapeutics, and digital tools offer promise in mitigating the social and economic consequences of the COVID-19. Global WHO leaders recognize the alignment, urging community stakeholders and political leaders to commit to a shared aim of equitable global access to innovative tools for COVID-19 for all, emphasizing collective problem-solving, establishing mutual benefit where all stakeholders can share their expertise and knowledge in a productive and meaningful way (15). With such advocacy, AIC remains an emerging frontier to navigate in the digital health industry for both academia and industry.
While the mini review obtains limitations, it offers initial snapshot and recommendations based on historical success of AIC in other industries. The work warrants a scoping or systematic review to fully understand the scope of the collaborative practices in digital health. Findings of the mini review informed a more robust literature search on the topic with clearly defined boundaries and search criteria. The findings of this mini review offer actionable collaboration insights for academia and industry to respond to this call to action. Alignment and partnership with diverse stakeholders prove challenging, however, historically demonstrates rewarding. Many high-functioning AICs have been operating for years and evolved together over time. Processes and extent of collaboration varies; however, acknowledging and appreciating differences may bolster these partnerships and shorten the learning curve among collaborators.
WHO's call to action reiterates the importance of AIC and balancing strengths to create global change by both advancing science and supporting the economy. It remains insufficient for research produce evidence and fails at scale and implementation. Commercial products on the market must be evidence-based and obtain real-world value. Academia and industry are operating in a highly complex adaptive system, where its critical to work together to translate evidence in the real world at scale. Digital health AIC may be an important synergy to answer WHO's call to action.
Despite the growing interest in digital health as a solution for public health problems, challenges persist. While AIC is continually endorsed to alleviate some of these challenges, limited knowledge is known on partnership best practices specific to digital health. To fully realize the potential the digital health industry obtains, stakeholders must be willing to recognize and leverage the strengths of each discipline to drive the industry and public health forward.
Author Contributions
Under the supervision of SB, SM, and KF designed the review and conducted the investigation as a part of a larger body of research. KF and JP developed and synthesized recommendations. KF initiated the manuscript with JP. SZ, XZ, and SG contributed iterations and manuscript edits for final submission. All authors agree and are accountable for the content of the work.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. Torous J, Myrick KJ, Rauseo-Ricupero N, Firth J. Digital mental health and COVID-19: using technology today to accelerate the curve on access and quality tomorrow. JMIR Mental Health. (2020) 7:e18848. doi: 10.2196/18848
2. Fagherazzi G, Goetzinger C, Rashid MA, Aguayo GA, Huiart L. Digital health strategies to fight COVID-19 worldwide: challenges, recommendations, and a call for papers. J Med Internet Res. (2020) 22:e19284. doi: 10.2196/19284
3. Whitelaw S, Mamas MA, Topol E, Van Spall HG. Applications of digital technology in COVID-19 pandemic planning and response. Lancet Digital Health. (2020) 2:e435–40. doi: 10.1016/S2589-7500(20)30142-4
4. Alwashmi MF. The use of digital health in the detection and management of COVID-19. Int J Environ Res Public Health. (2020) 17:2906. doi: 10.3390/ijerph17082906
5. Blandford A, Wesson J, Amalberti R, AlHazme R, Allwihan R. Opportunities and challenges for telehealth within, and beyond, a pandemic. Lancet Global Health. (2020) 8:e1364–5. doi: 10.1016/S2214-109X(20)30362-4
6. Kostkova P. Grand challenges in digital health. Front Public Health. (2015) 3:134. doi: 10.3389/fpubh.2015.00134
7. Patrick K, Hekler EB, Estrin D, Mohr DC, Riper H, Crane D, et al. The pace of technologic change: implications for digital health behavior intervention research. Am J Prev Med. (2016) 51:816–24. doi: 10.1016/j.amepre.2016.05.001
8. Yardley L, Choudhury T, Patrick K, Michie S. Current issues and future directions for research into digital behavior change interventions. Am J Prev Med. (2016) 51:814–5. doi: 10.1016/j.amepre.2016.07.019
9. Yardley L, Spring BJ, Riper H, Morrison LG, Crane DH, Curtis K, et al. Understanding and promoting effective engagement with digital behavior change interventions. Am J Prev Med. (2016) 51:833–42. doi: 10.1016/j.amepre.2016.06.015
10. Weibel N, Unertl K, Boll S, Assoc Comp M. Symposium: WISH - Workgroup on Interactive Systems in Healthcare. New York, NY: Assoc Computing Machinery (2019).
11. Hingle M, Patrick H, Sacher PM, Sweet CC. The intersection of behavioral science and digital health: the case for academic-industry partnerships. Health Educ Behav. (2019) 46:5–9. doi: 10.1177/1090198118788600
12. Moore C, Werner L, BenDor AP, Bailey M, Khan N. Accelerating harmonization in digital health. World Health Population. (2017) 17:43–54. doi: 10.12927/whp.2017.25306
13. Horgan D, Hackett J, Westphalen CB, Kalra D, Richer E, Romao M, et al. Digitalisation and COVID-19: the perfect storm. Biomedicine Hub. (2020) 5:1–23. doi: 10.1159/000511232
14. Seshadri DR, Davies EV, Harlow ER, Hsu JJ, Knighton SC, Walker TA, et al. Wearable sensors for COVID-19: a call to action to harness our digital infrastructure for remote patient monitoring and virtual assessments. Front Dig Health. (2020) 2:8. doi: 10.3389/fdgth.2020.00008
15. World Health Organization. Commitment and Call to Action: Global Collaboration to Accelerate New COVID-19 Health Technologies. Geneva: World Health Organization. (2020). Available online at: https://www.who.int/news-room/detail/24-04-2020-commitment-and-call-to-action-global-collaboration-to-accelerate-new-covid-19-health-technologies (accessed July 09, 2020).
16. Qermane K, Mancha R. WHOOP, Inc.: digital entrepreneurship during the Covid-19 pandemic. Entrepreneur Educ Pedag. (2020) 2515127420975181. doi: 10.1177/2515127420975181
17. Arora A, Belenzon S, Patacconi A, Suh J. The Changing Structure of American Innovation: Some Cautionary Remarks for Economic Growth. National Bureau of Economic Research (2019).
18. Rybnicek R, Königsgruber R. What makes industry–University collaboration succeed? A systematic review of the literature. J Bus Econ. (2019) 89:221–250. doi: 10.1007/s11573-018-0916-6
19. Sartipy P, Björquist P. Employment of the Triple Helix concept for development of regenerative medicine applications based on human pluripotent stem cells. Clin Transl Med. (2014) 3:9. doi: 10.1186/2001-1326-3-9
20. Perkmann M, Tartari V, McKelvey M, Autio E, Broström A, D'este P, et al. Academic engagement and commercialisation: a review of the literature on University–industry relations. Res Policy. (2013) 42:423–442. doi: 10.1016/j.respol.2012.09.007
21. ‘CovIdentify’ Pits Smartphones and Wearable Tech Against the Coronavirus. Duke Pratt School of Engineering (2020).
22. Iyawa GE, Herselman M, Botha A. Digital health innovation ecosystems: from systematic literature review to conceptual framework. Proc Comp Sci. (2016) 100:244–52. doi: 10.1016/j.procs.2016.09.149
23. Walker A, Ko N. Bringing medicine to the digital age via hackathons and beyond. J Med Syst. (2016) 40:1–3. doi: 10.1007/s10916-016-0461-1
24. Tseng J, Samagh S, Fraser D, Landman AB. Catalyzing healthcare transformation with digital health: performance indicators and lessons learned from a Digital Health Innovation Group. Healthcare. (2018) 6:150–5. doi: 10.1016/j.hjdsi.2017.09.003
25. Horowitz CR, Shameer K, Gabrilove J, Atreja A, Shepard P, Goytia CN, et al. Accelerators: sparking innovation and transdisciplinary team science in disparities research. Int J Environ Res Public Health. (2017) 14:225. doi: 10.3390/ijerph14030225
26. Silva PJ, Ramos KS. Academic medical centers as innovation ecosystems: evolution of industry partnership models beyond the bayh-dole act. Acad Med. (2018) 93:1135–1141. doi: 10.1097/ACM.0000000000002259
27. Ford KL, Moore SL, Zhou S, Gore MO, Portz J, Zhang X, et al. Advancing evidence-based digital health through an innovative research environment: an academic-industry collaboration case report. mHealth. (2019) 5:37. doi: 10.21037/mhealth.2019.08.08
28. Depasse JW, Chen CE, Sawyer A, Jethwani K, Sim I. Academic medical centers as digital health catalysts. Healthcare. (2014) 2:173–6. doi: 10.1016/j.hjdsi.2014.05.006
29. Ioannidis JPA. Stealth research: is biomedical innovation happening outside the peer-reviewed literature? JAMA. (2015) 313:663–4. doi: 10.1001/jama.2014.17662
30. Bern BG. From theory to practice: experiences of industry-academia collaboration from a practitioner. In: 2018 IEEE/ACM 5th International Workshop on Software Engineering Research and Industrial Practice (SER&IP). IEEE (2018). p. 22–3.
31. Peiris D, Miranda JJ, Mohr DC. Going beyond killer apps: building a better mHealth evidence base. BMJ Global Health. (2018) 3:e000676. doi: 10.1136/bmjgh-2017-000676
32. Garousi V, Petersen K, Ozkan B. Challenges and best practices in industry-academia collaborations in software engineering: a systematic literature review. Inf Softw Technol. (2016) 79:106–27. doi: 10.1016/j.infsof.2016.07.006
33. Borup M, Brown N, Konrad K, Van Lente H. The sociology of expectations in science and technology. Technol Anal Strat Manag. (2006) 18:285–98. doi: 10.1080/09537320600777002
34. Hochman M, Bedard R. Academic–industry research partnerships: an emerging opportunity or just smoke and mirrors? J Gen Intern Med. (2016) 31:149–50. doi: 10.1007/s11606-015-3527-8
35. Desmond-Hellmann S. Improving health with partnerships between academia and industry. JAMA Int Med. (2013) 173:1051. doi: 10.1001/jamainternmed.2013.826
36. Bodenheimer T. Uneasy alliance. N Engl J Med. (2000) 342:1539–44. doi: 10.1056/NEJM200005183422024
37. Johns MME, Barnes M, Florencio PS. Restoring balance to industry-academia relationships in an era of institutional financial conflicts of interest: promoting research while maintaining trust. JAMA. (2003) 289:741. doi: 10.1001/jama.289.6.741
38. Giuliani E, Arza V. What drives the formation of ‘valuable’University–industry linkages?: Insights from the wine industry. Res Policy. (2009) 38:906–21. doi: 10.1016/j.respol.2009.02.006
39. Barnes T, Pashby I, Gibbons A. Effective University–industry interaction:: a multi-case evaluation of collaborative r&d projects. Eur Manag J. (2002) 20:272–85. doi: 10.1016/S0263-2373(02)00044-0
40. Kaklauskas A, Banaitis A, Ferreira FA, Ferreira JJ, Amaratunga D, Lepkova N, et al. An evaluation system for University–industry partnership sustainability: enhancing options for entrepreneurial universities. Sustainability. (2018) 10:119. doi: 10.3390/su10010119
41. Liu C, Shao S, Liu C, Bennett GG, Prvu Bettger J, Yan LL. Academia–industry digital health collaborations: a cross-cultural analysis of barriers and facilitators. Dig Health. (2019) 5:2055207619878627. doi: 10.1177/2055207619878627
42. Sucala M, Cole-Lewis H, Arigo D, Oser M, Goldstein S, Hekler EB, et al. Behavior science in the evolving world of digital health: considerations on anticipated opportunities and challenges. Transl Behav Med. (2020) 11:495–503. doi: 10.1093/tbm/ibaa034
43. Ford KL. An Exploration of Digital Health Academic-Industry Collaboration. University of Colorado at Denver (Denver, Colorado) (2020).
44. Tricco AC, Lillie E, Zarin W, O'Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. (2018) 169:467. doi: 10.7326/M18-0850
45. Gelijns AC, Thier SO. Medical innovation and institutional interdependence: rethinking University-industry connections. JAMA. (2002) 287:72–7. doi: 10.1001/jama.287.1.72
46. Kirton M. Adaptors and innovators: a description and measure. J Appl Psychol. (1976) 61:622. doi: 10.1037/0021-9010.61.5.622
47. Senge PM. The fifth discipline, the art and practice of the learning organization. Perform Instruct. (1991) 30:37. doi: 10.1002/pfi.4170300510
48. Rajalo S, Vadi M. University-industry innovation collaboration: reconceptualization. Technovation. (2017) 62–3:42–54. doi: 10.1016/j.technovation.2017.04.003
49. Huang M-H, Chen D-Z. How can academic innovation performance in University–industry collaboration be improved? Technol Forecast Soc Change. (2017) 123:210–5. doi: 10.1016/j.techfore.2016.03.024
50. Bornstein SR, Licinio J. Improving the efficacy of translational medicine by optimally integrating health care, academia and industry. Nat Med. (2011) 17:1567. doi: 10.1038/nm.2583
51. Berwick DM, Nolan TW, Whittington J. The triple aim: care, health, and cost. Health Aff. (2008) 27:759–69. doi: 10.1377/hlthaff.27.3.759
53. Mian S, Lamine W, Fayolle A. Technology business incubation: an overview of the state of knowledge. Technovation. (2016) 50:1–12. doi: 10.1016/j.technovation.2016.02.005
54. Myoken Y. The role of geographical proximity in University and industry collaboration: case study of Japanese companies in the UK. Int J Technol Transfer Commercial. (2013) 12:43–61. doi: 10.1504/IJTTC.2013.064170
55. Shuren J, Patel B, Gottlieb S. FDA regulation of mobile medical apps. JAMA. (2018) 320:337–8. doi: 10.1001/jama.2018.8832
56. Perkmann M, Walsh K. University–industry relationships and open innovation: towards a research agenda. Int J Manag Rev. (2007) 9:259–80. doi: 10.1111/j.1468-2370.2007.00225.x
57. Shane SA. Economic Development Through Entrepreneurship: Government, University and Business Linkages. Edward Elgar Publishing (2007).
58. D'Este P, Perkmann M. Why do academics engage with industry? The entrepreneurial University and individual motivations. J Technol Transf. (2011) 36:316–39. doi: 10.1007/s10961-010-9153-z
59. Organization for Economic Co-operation Development Directorate for Science Technology Industry. OECD Science, Technology and Industry Scoreboard 2015: Innovation for Growth and Society. OECD (2015).
60. Brownson RC, Jacobs JA, Tabak RG, Hoehner CM, Stamatakis KA. Designing for dissemination among public health researchers: findings from a national survey in the United States. Am J Public Health. (2013) 103:1693–9. doi: 10.2105/AJPH.2012.301165
61. Brownson RC, Colditz GA, Proctor EK. Dissemination and Implementation Research in Health : Translating Science to Practice. Oxford; New York, NY: Oxford University Press (2012).
62. Steinmo M, Rasmussen E. How firms collaborate with public research organizations: the evolution of proximity dimensions in successful innovation projects. J Bus Res. (2016) 69:1250–9. doi: 10.1016/j.jbusres.2015.09.006
63. Morandi V. The management of industry–University joint research projects: how do partners coordinate and control R&D activities? J Technol Transf. (2013) 38:69–92. doi: 10.1007/s10961-011-9228-5
64. Perkmann M, Schildt H. Open data partnerships between firms and universities: the role of boundary organizations. Res Policy. (2015) 44:1133–43. doi: 10.1016/j.respol.2014.12.006
65. Melese T, Lin SM, Chang JL, Cohen NH. Open innovation networks between academia and industry: an imperative for breakthrough therapies. Nat Med. (2009) 15:502. doi: 10.1038/nm0509-502
66. Hekler EB, Klasnja P, Riley WT, Buman MP, Huberty J, Rivera DE, et al. Agile science: creating useful products for behavior change in the real world. Transl Behav Med. (2016) 6:317–28. doi: 10.1007/s13142-016-0395-7
67. Sharma A, Harrington RA, McClellan MB, Turakhia MP, Eapen ZJ, Steinhubl S, et al. Using digital health technology to better generate evidence and deliver evidence-based care. J Am Coll Cardiol. (2018) 71:2680–90. doi: 10.1016/j.jacc.2018.03.523
68. Hemmert M, Bstieler L, Okamuro H. Bridging the cultural divide: trust formation in University–industry research collaborations in the US, Japan, and South Korea. Technovation. (2014) 34:605–16. doi: 10.1016/j.technovation.2014.04.006
69. D'Amour D, Ferrada-Videla M, San Martin Rodriguez L, Beaulieu M-D. The conceptual basis for interprofessional collaboration: core concepts and theoretical frameworks. J Interprof Care. (2005) 19(Suppl. 1):116–31. doi: 10.1080/13561820500082529
70. Proulx EK, Hager AM, Klein CK. Models of collaboration between nonprofit organizations. Int J Prod Perform Manag. (2014) 63:746–65. doi: 10.1108/IJPPM-06-2013-0121
71. Rau C, Neyer A-K, Möslein KM. Innovation practices and their boundary-crossing mechanisms: a review and proposals for the future. Technol Anal Strat Manag. (2012) 24:181–217. doi: 10.1080/09537325.2012.647647
72. Bruneel J, d'Este P, Salter A. Investigating the factors that diminish the barriers to University–industry collaboration. Res Policy. (2010) 39:858–68. doi: 10.1016/j.respol.2010.03.006
73. Tierney WM, Meslin EM, Kroenke K. Industry support of medical research: important opportunity or treacherous pitfall? J Gen Intern Med. (2016) 31:228–33. doi: 10.1007/s11606-015-3495-z
74. Flood J, Minkler M, Hennessey Lavery S, Estrada J, Falbe J. The collective impact model and its potential for health promotion: overview and case study of a healthy retail initiative in San Francisco. Health Educ Behav. (2015) 42:654–68. doi: 10.1177/1090198115577372
75. Arsenyan J, Büyüközkan G, Feyzioglu O. Modeling collaboration formation with a game theory approach. Exp Syst Appl. (2015) 42:2073–85. doi: 10.1016/j.eswa.2014.10.010
76. Beck K, Beedle M, Van Bennekum A, Cockburn A, Cunningham W, Fowler M, et al. Manifesto for Agile Software Development (2001)
77. Beck K, Beedle M, Van Bennekum A, Cockburn A, Cunningham W, Fowler M, et al. Manifesto for Agile Software Development. (2001).
78. Collins S, Wakoh H. Universities and technology transfer in Japan: recent reforms in historical perspective. J Technol Transf. (2000) 25:213–22. doi: 10.1023/A:1007884925676
79. Ankrah S, Al-Tabbaa O. Universities–industry collaboration: a systematic review. Scand J Manag. (2015) 31:387–408. doi: 10.1016/j.scaman.2015.02.003
80. Roig-Tierno N, Alcazar J, Ribeiro-Navarrete S. Use of infrastructures to support innovative entrepreneurship and business growth. J Bus Res. (2015) 68:2290–4. doi: 10.1016/j.jbusres.2015.06.013
81. Sherman S, Hadar I, Luria G. Leveraging organizational climate theory for understanding industry-academia collaboration. Inf Softw Technol. (2018) 98:148–60. doi: 10.1016/j.infsof.2017.12.006
82. Bedwell WL, Wildman JL, DiazGranados D, Salazar M, Kramer WS, Salas E. Collaboration at work: an integrative multilevel conceptualization. Hum Resour Manag Rev. (2012) 22:128–45. doi: 10.1016/j.hrmr.2011.11.007
83. Salleh MS, Omar MZ. University-industry collaboration models in Malaysia. Proc Soc Behav Sci. (2013) 102:654–64. doi: 10.1016/j.sbspro.2013.10.784
84. Arigo D, Jake-Schoffman DE, Wolin K, Beckjord E, Hekler EB, Pagoto SL. The history and future of digital health in the field of behavioral medicine. J Behav Med. (2019) 42:67–83. doi: 10.1007/s10865-018-9966-z
85. Stroh DP. Systems Thinking for Social Change: A Practical Guide to Solving Complex Problems, Avoiding Unintended Consequences, and Achieving Lasting Results. Chelsea Green Publishing (2015).
86. Miller K, McAdam R, McAdam M. A systematic literature review of University technology transfer from a quadruple helix perspective: toward a research agenda. R&D Manag. (2018) 48:7–24. doi: 10.1111/radm.12228
87. Minkler M, Wallerstein N. Community-Based Participatory Research for Health: From Process to Outcomes. John Wiley & Sons (2011).
88. World Health Organization. WHO Guideline: Recommendations on Digital Interventions for Health System Strengthening (2019).
Keywords: academic industry collaboration, digital health, innovation, partnership, intersector collaboration
Citation: Ford KL, Portz JD, Zhou S, Gornail S, Moore SL, Zhang X and Bull S (2021) Benefits, Facilitators, and Recommendations for Digital Health Academic-Industry Collaboration: A Mini Review. Front. Digit. Health 3:616278. doi: 10.3389/fdgth.2021.616278
Received: 11 October 2020; Accepted: 24 February 2021;
Published: 15 April 2021.
Edited by:
Harry Scarbrough, City University of London, United KingdomReviewed by:
Tijs Van Den Broek, Vrije Universiteit Amsterdam, NetherlandsYaru Chen, City University of London, United Kingdom
Copyright © 2021 Ford, Portz, Zhou, Gornail, Moore, Zhang and Bull. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Kelsey L. Ford, a2Vsc2V5LmZvcmRAY3VhbnNjaHV0ei5lZHU=
 Kelsey L. Ford
Kelsey L. Ford Jennifer D. Portz1,2
Jennifer D. Portz1,2 Shuo Zhou
Shuo Zhou Susan L. Moore
Susan L. Moore