
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Cardiovasc. Med., 21 March 2025
Sec. Coronary Artery Disease
Volume 12 - 2025 | https://doi.org/10.3389/fcvm.2025.1502964
Background: Neutrophil-to-lymphocyte ratio (NLR) has been presented as a possible indicator associated with the outcomes of growing patients and an available predictor of inflammation. Nevertheless, just a handful of researches shed light on the association between NLR and the consequences of critical patients with coronary artery disease (CAD). The study aimed to investigate the correlation between NLR and all-cause mortality of short-term and long-term in patients with CAD.
Methods: We obtained objective data from the Medical Information Mart for Intensive Care (MIMIC)-IV version 2.2, a comprehensive and large-scale single-center database. NLR was calculated separately. Patients were categorized by quartiles of NLR: Q1 group (NLR < 3.56), Q2 (NLR 3.56–5.54), Q3 group (NLR 5.54–9.05), Q4 group (NLR > 9.05). Kaplan–Meier survival curves based on NLR quartiles were created to compare all-cause mortality rates, and the log-rank test evaluated the differences between groups. The hazard ratio (HR) of NLR as a risk factor for outcome events was assessed using the Cox proportional risk model with the Q1 group serving as the reference group and restricted cubic spline (RCS) with the infection points of 5.54.
Results: A total of 3,692 patients were included in this study. The 30-day mortality rate among the patients was 8.85%, while the 365-day mortality rate was 16.98%. High NLR (NLR > 5.54) was significantly associated with 30-day mortality [HR, 3.99,95% confident interval (CI), (3.03–5.24); P < 0.001] and 365-day mortality [HR, 5.72, 95% CI (3.83–8.54); P < 0.001] in patients with critical CAD in the completely adjusted Cox proportional risk model. RCS analysis revealed a U-shaped relationship between NLR and outcome events.
Conclusion: In patients diagnosed with critical CAD, a significant correlation was observed between NLR and all-cause mortality, particularly among individuals exhibiting elevated NLR levels. These findings suggest that NLR may serve as a valuable prognostic marker for evaluating both short-term and long-term mortality risk in this patient population.
Coronary artery disease (CAD) remains a significant global public health challenge, despite advances in prevention and treatment. Critically ill patients admitted to the intensive care unit (ICU) following cardiac surgery often have CAD, requiring specialized ICU care. Additionally, acute exacerbations of chronic cardiovascular diseases contribute to a notable mortality rate, making cardiovascular issues the second leading cause of death globally within a year (1–5). Evaluating the prognosis of patients with critical CAD is a priority due to limited current research in this area.
Inflammation plays a crucial role in the development of severe cardiovascular diseases. Inflammatory markers like white blood cell (WBC), C-reactive protein (CRP), and interleukin-6 (IL-6) are strongly linked to cardiovascular disease. Recently, anti-inflammatory drugs have emerged as potential treatments for these patients (6, 7). The ratio of leukocyte subtypes serves as an indicator of inflammatory onset, with NLR emerging as a novel biomarker. Neutrophils signify non-specific inflammatory responses, while lymphocytes reflect stress levels or compromised immune function (8). Severe inflammation adversely affects patients in coronary care units (CCUs) (9), and the NLR has been shown to predict poor outcomes across various diseases. For patients with advanced heart failure, a higher NLR (indicative of a reduced lymphocyte ratio) correlates with poorer long-term outcomes (10). Studies also associate elevated NLR with adverse prognoses in acute coronary syndrome (ACS) and patients undergoing percutaneous coronary treatments (11, 12). However, whether NLR predicts short-term, long-term, or both forms of mortality in CAD patients remains unclear. This study investigates the relationship between NLR and outcomes in CAD patients, aiming to clarify its predictive value.
This study involved a retrospective analysis of coronary artery disease patient data from the MIMIC-IV database, managed by MIT's (Massachusetts Institute of Technology) Laboratory of Computational Physiology. The research database received approval from the review committee at the Massachusetts Institute of Technology and Beth Israel Deaconess Medical Center, along with a waiver of informed consent. We have completed the online course and passed the online exams (No. 12892471) to gain access to the database. In this investigation, we enrolled 13,968 patients with critical coronary artery disease who were first admitted to ICU from 2008 to 2019. A total of 10,276 patients were initially excluded due to missing data on their neutrophil and lymphocytes count level. Ultimately, a total of 3,692 patients with critical CAD met the inclusion criteria for the study (Figure 1).
The extraction of information was facilitated by the utilization of PostgresSQL (version 13.7.2) and Navicate Premium (version 16) software, employing the execution of Structured Query Language (SQL). Potential confounding variables were extracted as follows: (1). baseline demographic information: age, gender, body mass index (BMI), (2). comorbidities: hypertension, diabetes, atrial fibrillation (AF), acute myocardial infarction (AMI), acute heart failure (AHF), (3). interventions: coronary artery bypass grafting (CABG), percutaneous transluminal coronary angioplasty (PTCA), invasive ventilation, (4). laboratory parameters: white blood cells (WBC), red blood cells(RBC), hemoglobin(HGB), platelets(PLT), Hematocrit (Hct), Sodium, Potassium, calcium, glucose and Red cell distribution (RDW), (5). Scoring system: Acute Physiology Score III (APSIII), and Sepsis-Organ Failure Assessment Score (SOFA). Simplified Acute Physiology Score (SAPS II), Oxford Acute Severity of Illness Score (OASIS) and Charlson comorbidity index. All variables were complete except for serologic indicators. The missing serological values are mainly concentrated in the following variables(missing data and percent): Platelet count: 2(0.05%), hemoglobin:1(0.03%), potassium: 9(0.24%), fasting plasma glucose:48(1.3%). We used the random forest method to impute missing serologic values, as they were less than 5%.
The baseline NLR was calculated by dividing the absolute neutrophil count by the absolute lymphocyte count using the initial laboratory parameters following admission to the ICU. Subsequent assessments of NLR were conducted with the maximum value within the first week of ICU admission, with measurements taken at irregular intervals. The main outcome measure in this study was all-cause mortality occurring within 365 days following patient admission, with the secondary outcome defined as all-cause mortality within 30 days post-admission.
NLR quartiles were used to categorize the study population into four groups: Q1 (n = 923, NLR ≤ 3.56), Q2 (n = 923, 3.56 < NLR ≤ 5.54), Q3 (n = 923, 5.54 < NLR ≤ 9.05), and Q4 (n = 923, NLR > 9.05), with the highest two quartiles classified as high group and the lower two quartiles classified as low group. Categorical variables were represented as percentages and compared using the chi-square test, while continuous numerical variables were expressed as medians (quartiles) following a normality test and compared using the nonparametric rank-sum test. The HR of NLR as a risk factor for outcome events was evaluated using a Cox proportional risk model with the Q1 group as the reference. Age, gender, BMI, PTCA, CABG, AMI, AHF, AF, hypertension, diabetes and invasive ventilation therapy were considered as confounders in the multivariate Cox regression model. Kaplan–Meier survival analysis based on NLR quartiles and the log-rank test were used to compare groups. Restricted cubic spline (RCS) curves were utilized to investigate the relationship between NLR and outcome events. Subgroup analysis were conducted to validate the reliability of the findings. Receiver operating characteristic curves were used to assess the prognostic value of NLR for 30-day and 365-day mortality. Statistical analysis was carried out using R studio (version R4.2.3) and EmpowerStats (version 4.1), with a two-sided P value < 0.05 considered statistically significant.
This study encompassed a cohort of 3,692 patients diagnosed with critical coronary artery disease, consisting of 2,748 male patients (74.4%) and 944 female patients (25.6%,), among whom 627 patients encountered a fatal event within the 365-day observational period. The baseline information based on the NLR quartiles is shown in Table 1. In comparison to the low-NLR group, the high-NLR group exhibited a lower proportion of young male patients, and elevated percentages of CABG procedures, PLT count, and creatinine levels. Conversely, the low-NLR group demonstrated higher percentages of patients with AMI, AHF, AF and elevated hemoglobin levels. Furthermore, the high NLR group displayed higher disease severity scores (SOFA score, APSIII score, SAPSII score, OASIS and Charlson) and WBC counts compared to the low NLR group. Baseline characteristics difference between survivors and non-survivors during the hospital stay are shown in Supplementary Table S1.
We conducted a comparison of the incidence of the primary outcome among groups using KM survival analysis curves based on the NLR quartiles, as depicted in Figure 2. The rate of mortality within 30 days was significantly higher in the Q4 group compared to the other groups (log-rank P < 0.001) (Figure 2a). Further KM survival analysis were performed between every two groups (Supplementary Figure S1). Additionally, the one-year mortality rate was significantly higher in Group Q4 compared to other groups, with a significant difference between the groups (log-rank P < 0.001) (Figure 2b). These findings suggest that high NLR levels have a detrimental impact on the long-term survival of patients with CAD.
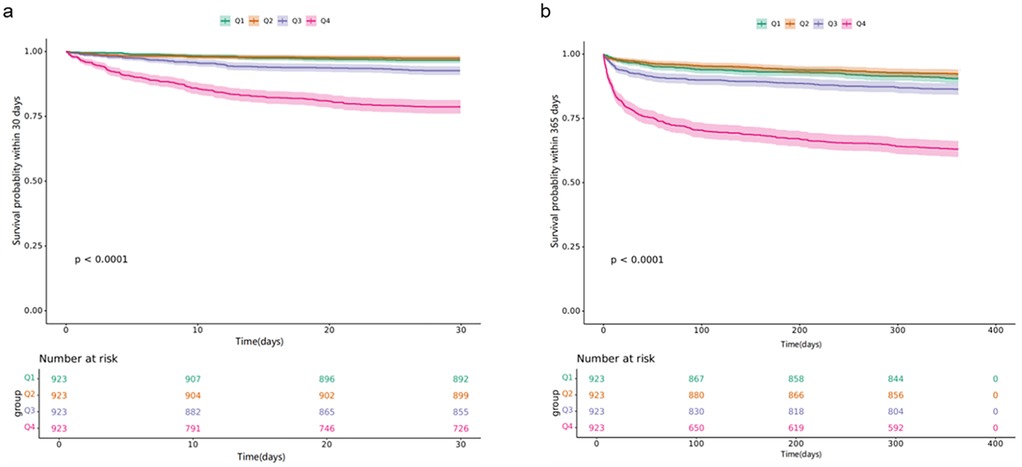
Figure 2. Kaplan–meier all-cause mortality survival analysis curve: (a) showing comparison of mortality within 30 days between groups, (b) showing comparison of mortality within 365 days between groups.
In the analysis of patients' baseline characteristics, it was observed that the Q1 group (NLR < 3.56) exhibited the lowest mortality rate in comparison to the other groups. Subsequently, a correlation between NLR and the primary outcome was examined through the development of Cox proportional risk models, with the Q1 group serving as the reference category. The findings revealed that the Q3 and Q4 group (NLR > 9.05) demonstrated a significant association with both the primary outcome event [Q4 vs. Q1: HR, 8.11 [5.49, 11.99], P < 0.001; Q3 vs. Q1: HR, 2.32 [1.51, 3.59]] and the secondary outcome [Q4 vs. Q1: HR, 5.56 [4.30, 7.19], P < 0.001; Q3 vs. Q1: HR, 1.51 [1.13, 2.02], P = 0.005] in the Cox proportional risk model unadjusted for confounders. We observed a significant association between NLR and increased 365-day mortality [Q4 vs. Q1: HR, 5.72 (3.83, 8.54) P < 0.001] and 30-day mortality [Q4 vs. Q1: HR, 3.99(3.03, 5.24) P < 0.001] in fully adjusted models. Furthermore, we observed a correlation between Q3 group with 5.54 < NLR ≤ 9.05 and 30-day mortality [Q3 vs. Q1: HR, 1.40 (1.04, 1.90) P = 0.028], as well with 365-day mortality [Q3 vs. Q1: HR, 2013 (1.37, 3.32) P < 0.001], in the fully adjusted model. Moreover, the risk of cardiovascular events was not significant between quartiles 1 and 2 groups both in the unadjusted and fully adjusted model (Table 2).
The data presented in Figure 3a indicates that the Q4 group exhibited the highest mortality rate, with the Q3 group following closely behind. Consequently, it can be inferred that elevated levels of high NLR are associated with increased risk for patients diagnosed with critical coronary heart disease. Following this, we conducted a model of RCS, which revealed a significant “U” shaped relationship between NLR and the risk ratio of mortality in individuals diagnosed with severe coronary artery disease, and we found that NLR infection points of 5.54 for both the primary and secondary outcomes.
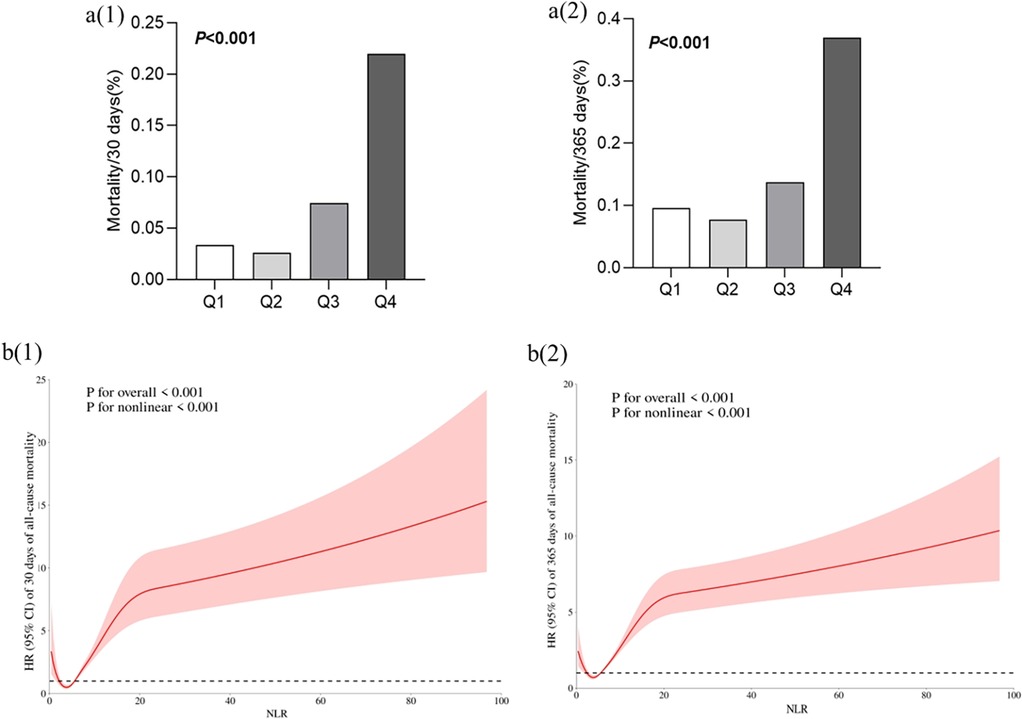
Figure 3. Correlation between NLR and outcome events. (a) Comparison of all-cause mortality between groups based on NLR quartiles. (b) Restricted cubic spline curve for the NLR index hazard ratio. Heavy central lines represent the estimated fully adjusted hazard ratios for covariates as in Table 2, with shaded ribbons denoting 95% confidence intervals. The horizontal dotted lines represent the hazard ratio of 1.0. (b) (1): Restricted Cubic Spline Curve for the mortality rate of patients within 30 days, (b) (2): Restricted Cubic Spline Curve for the mortality rate of patients within 365 days.
Furthermore, we conducted subgroup analyses of patient outcome events based on various risk factors including age, gender, BMI, AMI, AHF, hypertension, and diabetes. Based on the subgroup analysis examining 30-day mortality as the primary outcome event, a high NLR (Q3 + Q4 NLR > 5.54) in the subgroups demonstrated a significant association with primary 30-day mortality in patients diagnosed with critical CAD (Figure 4). Furthermore, the correlation between NLR and 365-day mortality was constant across all subgroups in our analysis, regardless of age (<65 and >65 years), sex, or BMI (Figure 5). Higher NLR levels are related to an increased risk of death, and the results were consistent in different subgroups according to comorbidities like hypertension, heart failure, and diabetes.
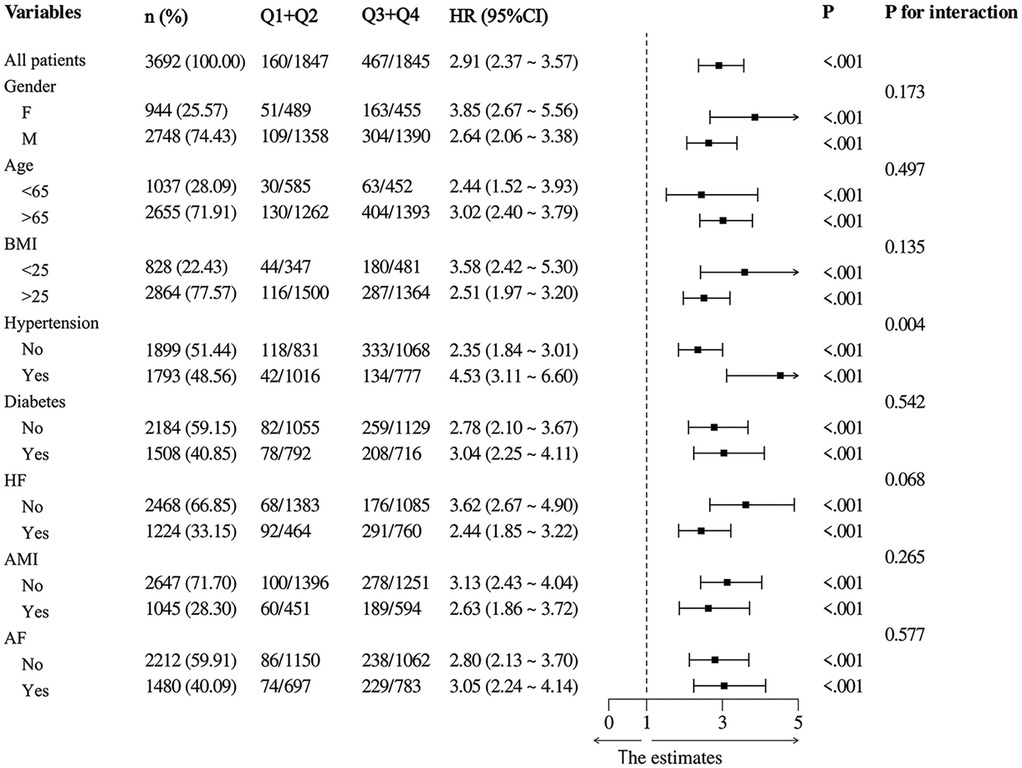
Figure 4. Subgroup analysis with 30-mortality as the outcome event in low and high NLR group (Q1 + Q2 vs. Q3 + Q4).
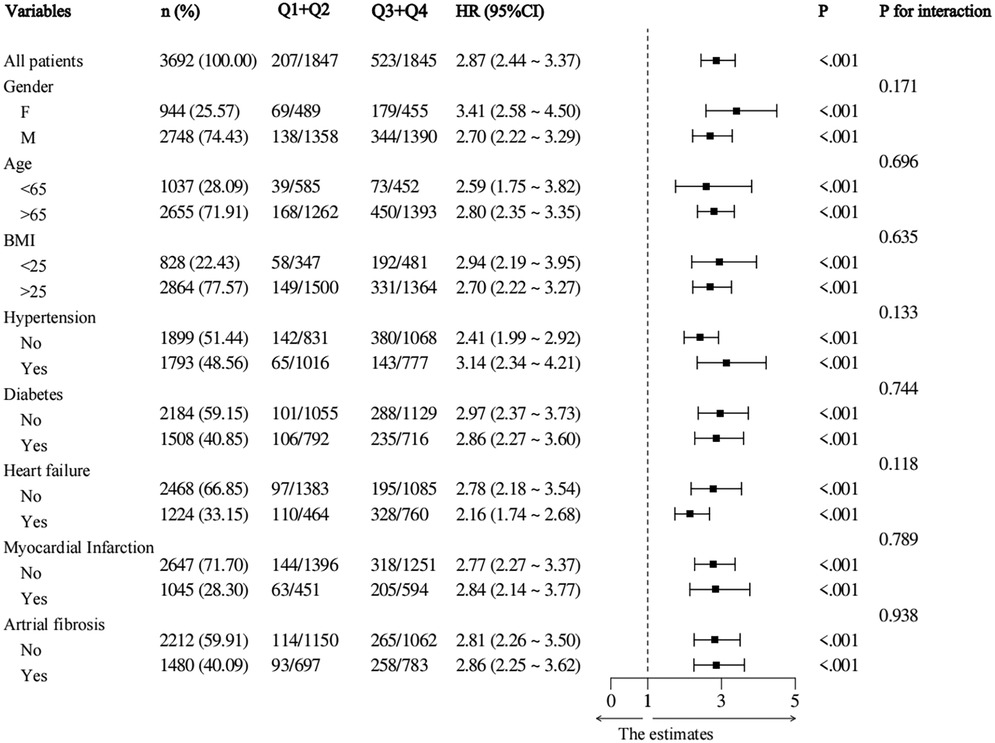
Figure 5. Subgroup analysis with 365-mortality as the outcome event in low and high NLR group (Q1 + Q2 vs. Q3 + Q4).
The Receiver Operating Characteristic (ROC) analysis was employed to assess the discriminative capacity of NLR for detecting CAD in individuals. The findings indicated that the Area Under the ROC Curve (AUROC) for the NLR predicting 30-day mortality, when combined with various demographic and clinical variables, was 0.75 (95% CI: 0.72–0.79), with a sensitivity of 0.75 and a specificity of 0.68 (Figure 6b). Meanwhile, the AUROC for NLR predicting 365-day mortality, also combined with demographic and clinical variables, was 0.71 (95% CI: 0.68–0.73), with a sensitivity of 0.79 (Figure 6b). The result suggested NLR performed better in predicting short-term mortality than long-term mortality.
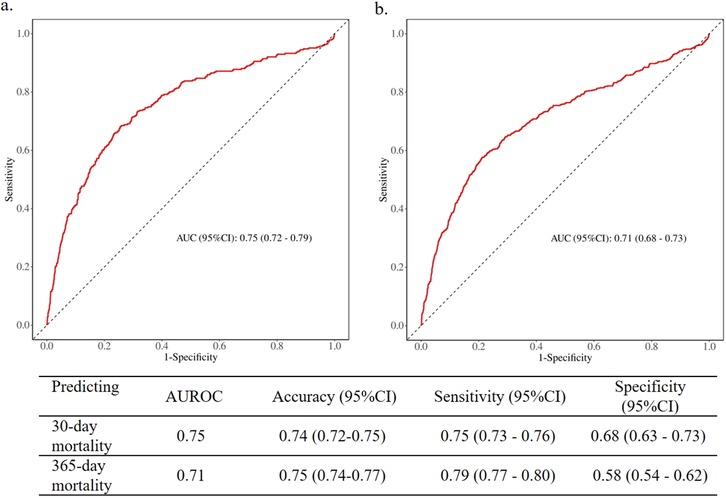
Figure 6. Receiver operating characteristic curves of NLR predicting 30-day and 365-day mortality. (a) 30-day mortality; (b) 365-day mortality.
In this retrospective cohort study, we have demonstrated the presence of a statistically significant positive association between baseline NLR and short-term and long-term mortality among patients diagnosed with coronary artery disease. High NLR at ICU admission was associated with higher 30-day and 365-day mortality. We found a “U” relationship between NLR and the hazard ratio of outcome events in the RCS-based analyses, which is consistent with the results of the analyses described above. The stability of the relationship persisted following adjustments for demographic and clinical confounders, indicating a potential association between an early rise in NLR and unfavorable short-term and long-term outcomes in patients with CAD.
Inflammation plays a crucial role in the development and progression of CAD (13, 14). Modern research not only enhances interest in traditional inflammatory biomarkers such as hsCRP, but also raises awareness of a readily accessible and widely available simple biomarker within the clinical community (15, 16). One such biomarker is NLR, which is derived from the complete blood count. The NLR incorporates data from both the innate immune system, primarily mediated by neutrophils, and the adaptive immune response, facilitated by lymphocytes. Previous studies have shown that a high NLR is linked to atrial fibrillation, heart failure, and cardiac death in patients with cardiovascular diseases (17–19). Furthermore, studies have demonstrated the stability of NLR over time and its responsiveness to anti-inflammatory treatments, suggesting its potential utility as an alternative or adjunct inflammatory biomarker in clinical settings. Previous research has demonstrated that elevated NLR is correlated with a poor short-term and long-term prognosis in several conditions, such as tumors, sepsis, and ARDS (20). In the study, NLR levels were independently associated with an increased risk of all-cause mortality in the population. A recent meta-analysis comprising 23 studies involving patients with ACS revealed that an elevated NLR upon admission was significantly correlated with increased mortality rates and a higher incidence of major adverse clinical outcomes (21). In our study, relatively more abundant data was analyzed and indicated that the risk of cardiovascular events was not significant between quartiles 1 and 2 groups. This study conclusively illustrated that individual with high NLR (NLR > 5.54) exhibit increased cardiovascular risk and all-cause mortality compared to those with low NLR (NLR < 5.54), which varies from the knots implied in other studies. Timely risk stratification is crucial in the treatment of patients with coronary artery disease, and adherence to strict guideline-recommended therapies should be considered for this subset of higher-risk patients. While there is limited research on interventions for patients with high NLR and CAD, such treatments have the potential to mitigate their adverse cardiovascular outcomes.
The link between high NLR and cardiovascular events can be explained by various mechanisms. Both high neutrophil count and low lymphocyte count can impact the clinical outcomes of CAD patients. Neutrophils release substantial quantities of inflammatory mediators and modulate the inflammatory response (22). Moreover, neutrophils have been shown to increase the vulnerability of atherosclerotic plaques through the release of protective enzymes such as myeloperoxidase and superoxide radicals (3, 23). On the other hand, lymphocytes serve as a key regulatory component of the immune system, with studies indicating that inflammatory activation can induce apoptosis in these cells (24, 25). Additionally, a reduction in lymphocyte count has been identified as an early indicator of physiological stress and multivisceral failure resulting from myocardial ischemia, which is facilitated by the release of cortisol (26). Other studies have also found that certain components of white blood cells or platelets can indicate inflammation (27, 28). NLR levels may be a more accurate predictor of cardiovascular events compared to neutrophil levels alone, as neutrophils are linked to inflammation and cardiovascular diseases.
In conclusion, the findings of this study demonstrate a significant association between NLR and all-cause mortality in patients diagnosed with critical CAD. It is recommended that it is crucial to pay closer attention to neutrophil and lymphocytes fluctuations in patients during their ICU stay. Furthermore, due to the presence of numerous confounding variables in ICU patients, a comprehensive prospective study is warranted to further elucidate the relationship between NLR and adverse outcomes in individuals with critical CAD.
In this research, pertinent clinical data regarding patients diagnosed with CAD was obtained from the MIMIC-IV database. It should be noted that the complete clinical diagnostic information of the patients may not have been extracted, and there are potential confounding variables that could impact the overall mortality rates. Additionally, the potential relationship between NLR and adverse outcomes other than all-cause mortality was not explored in this study. Furthermore, the patient's lipid level was identified as an independent risk factor for an unfavorable prognosis; nevertheless, due to a substantial quantity of absent lipid data, these levels were not incorporated into the present study. Ejection fraction (EF) is indeed a crucial prognostic parameter in cardiovascular research. In our study, EF was not included in the baseline characteristics due to the missing of a significant proportion of patients. Moreover, the COX regression Model for NLR was computed utilizing the specific study cohort and may not be universally applicable to other populations. It is our contention that regression models should be developed using data sourced from diverse extensive databases to determine the NLR for distinct population subsets.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
YL: Conceptualization, Data curation, Formal analysis, Methodology, Resources, Software, Visualization, Writing – original draft. DC: Formal analysis, Software, Visualization, Writing – original draft. YF: Validation, Writing – review & editing. QZ: Validation, Writing – review & editing. HD: Investigation, Writing – review & editing. XC: Project administration, Supervision, Writing – review & editing.
The author(s) declare that no financial support was received for the research and/or publication of this article.
We appreciate all the authors for their assistance in this article.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declare that no Generative AI was used in the creation of this manuscript.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcvm.2025.1502964/full#supplementary-material
ACS, acute coronary syndrome; AF, atrial fibrillation; AMI, acute myocardial infarction; AHF, acute heart failure; APSIII, acute physiology score III; BMI, body mass index; CAD, coronary artery disease; CABG, coronary artery bypass grafting; CI, confidence interval; CRP, C-reactive protein; FPG, fasting plasma glucose; Hct, Hematocrit; HGB, hemoglobin; HR, hazard ratio; ICU, intensive care unit; IL-6, interleukin-6; MIMIC-IV, medical information mart for intensive care IV; OASIS, Oxford acute severity of illness score; PLT, platelets; PTCA, percutaneous transluminal coronary angioplasty; RBC, red blood cells; RCS, restricted cubic spline; RDW, Red cell distribution; SAPSII, simplified acute physiology score; SOFA, sepsis-organ failure assessment score; WBC, white blood cell count.
1. Luo F, Das A, Chen J, Wu P, Li X, Fang Z. Metformin in patients with and without diabetes: a paradigm shift in cardiovascular disease management. Cardiovasc Diabetol. (2019) 18(1):54. doi: 10.1186/s12933-019-0860-y
2. Pavasini R, Biscaglia S, Kunadian V, Hakeem A, Campo G. Coronary artery disease management in older adults: revascularization and exercise training. Eur Heart J. (2024) 45(31):2811–23. doi: 10.1093/eurheartj/ehae435
3. Weber C, Noels H. Atherosclerosis: current pathogenesis and therapeutic options. Nat Med. (2011) 17(11):1410–22. doi: 10.1038/nm.2538
4. Luo W, Cao L, Wang C. Low body temperature and mortality in critically ill patients with coronary heart disease: a retrospective analysis from MIMIC-IV database. Eur J Med Res. (2023) 28(1):614. doi: 10.1186/s40001-023-01584-8
5. Mayr VD, Dünser MW, Greil V, Jochberger S, Luckner G, Ulmer H, et al. Causes of death and determinants of outcome in critically ill patients. Crit Care. (2006) 10(6):R154. doi: 10.1186/cc5086
6. Golia E, Limongelli G, Natale F, Fimiani F, Maddaloni V, Pariggiano I, et al. Inflammation and cardiovascular disease: from pathogenesis to therapeutic target. Curr Atheroscler Rep. (2014) 16(9):435. doi: 10.1007/s11883-014-0435-z
7. Fearon WF, Fearon DT. Inflammation and cardiovascular disease: role of the interleukin-1 receptor antagonist. Circulation. (2008) 117(20):2577–9. doi: 10.1161/CIRCULATIONAHA.108.772491
8. Adamstein NH, MacFadyen JG, Rose LM, Glynn RJ, Dey AK, Libby P, et al. The neutrophil-lymphocyte ratio and incident atherosclerotic events: analyses from five contemporary randomized trials. Eur Heart J. (2021) 42(9):896–903. doi: 10.1093/eurheartj/ehaa1034
9. Sun H, Que J, Peng Y, Ye H, Xiang H, Han Y, et al. The neutrophil-lymphocyte ratio: a promising predictor of mortality in coronary care unit patients—a cohort study. Int Immunopharmacol. (2019) 74:105692. doi: 10.1016/j.intimp.2019.105692
10. Curran FM, Bhalraam U, Mohan M, Singh JS, Anker SD, Dickstein K, et al. Neutrophil-to-lymphocyte ratio and outcomes in patients with new-onset or worsening heart failure with reduced and preserved ejection fraction. ESC Heart Fail. (2021) 8(4):3168–79. doi: 10.1002/ehf2.13424
11. Li Y, Chen X, Huang L, Lu J. Association between neutrophil-lymphocyte ratio and arterial stiffness in patients with acute coronary syndrome. Biosci Rep. (2019) 39(5):BSR20190015. doi: 10.1042/BSR20190015
12. Pruc M, Kubica J, Banach M, Swieczkowski D, Rafique Z, Peacock WF, et al. Diagnostic and prognostic performance of the neutrophil-to-lymphocyte ratio in acute coronary syndromes: a meta-analysis of 90 studies including 45 990 patients. Kardiol Pol. (2024) 82(3):276–84. doi: 10.33963/v.phj.99554
13. Ridker PM. Clinician’s guide to reducing inflammation to reduce atherothrombotic risk: JACC review topic of the week. J Am Coll Cardiol. (2018) 72(25):3320–31. doi: 10.1016/j.jacc.2018.06.082
14. Ridker PM, Everett BM, Thuren T, MacFadyen JG, Chang WH, Ballantyne C, et al. Antiinflammatory therapy with canakinumab for atherosclerotic disease. N Engl J Med. (2017) 377(12):1119–31. doi: 10.1056/NEJMoa1707914
15. Wada H, Dohi T, Miyauchi K, Shitara J, Endo H, Doi S, et al. Preprocedural high-sensitivity C-reactive protein predicts long-term outcome of percutaneous coronary intervention. Circ J. (2016) 81(1):90–5. doi: 10.1253/circj.CJ-16-0790
16. Wada H, Dohi T, Miyauchi K, Nishio R, Takeuchi M, Takahashi N, et al. Neutrophil to lymphocyte ratio and long-term cardiovascular outcomes in coronary artery disease patients with low high-sensitivity C-reactive protein level. Int Heart J. (2020) 61(3):447–53. doi: 10.1536/ihj.19-543
17. Berkovitch A, Younis A, Grossman Y, Segev S, Kivity S, Sidi Y, et al. Relation of neutrophil to lymphocyte ratio to risk of incident atrial fibrillation. Am J Cardiol. (2019) 123(3):396–401. doi: 10.1016/j.amjcard.2018.10.036
18. Kim S, Eliot M, Koestler DC, WuK W-C, Kelsey T. Association of neutrophil-to-lymphocyte ratio with mortality and cardiovascular disease in the Jackson heart study and modification by the duffy antigen variant. JAMA Cardiol. (2018) 3(6):455–62. doi: 10.1001/jamacardio.2018.1042
19. Fest J, Ruiter TR, Groot Koerkamp B, Rizopoulos D, Ikram MA, van Eijck CHJ, et al. The neutrophil-to-lymphocyte ratio is associated with mortality in the general population: the rotterdam study. Eur J Epidemiol. (2019) 34(5):463–70. doi: 10.1007/s10654-018-0472-y
20. Zhang W, Wang Y, Li W, Wang G. The association between the baseline and the change in neutrophil-to-lymphocyte ratio and short-term mortality in patients with acute respiratory distress syndrome. Front Med. (2021) 8:636869. doi: 10.3389/fmed.2021.636869
21. Dentali F, Nigro O, Squizzato A, Gianni M, Zuretti F, Grandi AM, et al. Impact of neutrophils to lymphocytes ratio on major clinical outcomes in patients with acute coronary syndromes: a systematic review and meta-analysis of the literature. Int J Cardiol. (2018) 266:31–7. doi: 10.1016/j.ijcard.2018.02.116
22. Dogan I, Karaman K, Sonmez B, Celik S, Turker O. Relationship between serum neutrophil count and infarct size in patients with acute myocardial infarction. Nucl Med Commun. (2009) 30(10):797–801. doi: 10.1097/MNM.0b013e32832e3a16
23. Eriksson EE, Xie X, Werr J, Thoren P, Lindbom L. Direct viewing of atherosclerosis in vivo: plaque invasion by leukocytes is initiated by the endothelial selectins. FASEB J. (2001) 15(7):1149–57. doi: 10.1096/fj.00-0537com
24. Hotchkiss RS, Karl IE. The pathophysiology and treatment of sepsis. N Engl J Med. (2003) 348(2):138–50. doi: 10.1056/NEJMra021333
25. Yang M, Lin S-Q, Liu X-Y, Tang M, Hu C-L, Wang Z-W, et al. Association between C-reactive protein-albumin-lymphocyte (CALLY) index and overall survival in patients with colorectal cancer: from the investigation on nutrition status and clinical outcome of common cancers study. Front Immunol. (2023) 14:1131496. doi: 10.3389/fimmu.2023.1131496
26. Zouridakis EG, Garcia-Moll X, Kaski JC. Usefulness of the blood lymphocyte count in predicting recurrent instability and death in patients with unstable angina pectoris. Am J Cardiol. (2000) 86(4):449–51. doi: 10.1016/S0002-9149(00)00963-2
27. Yamamoto E, Sugiyama S, Hirata Y, Tokitsu T, Tabata N, Fujisue K, et al. Prognostic significance of circulating leukocyte subtype counts in patients with coronary artery disease. Atherosclerosis. (2016) 255:210–6. doi: 10.1016/j.atherosclerosis.2016.08.033
Keywords: coronary artery disease, neutrophil-to-lymphocyte ratio (NLR), MIMIC-IV, all-cause mortality, ICU
Citation: Li Y, Chen D, Fan Y, Zhu Q, Deng H and Chai X (2025) Association between neutrophil to lymphocyte ratio and all-cause mortality in critical patients with coronary artery disease - a study based on the MIMIC-IV database. Front. Cardiovasc. Med. 12:1502964. doi: 10.3389/fcvm.2025.1502964
Received: 3 October 2024; Accepted: 5 March 2025;
Published: 21 March 2025.
Edited by:
Tommaso Gori, Johannes Gutenberg University Mainz, GermanyReviewed by:
Chenggang Li, Xuzhou Medical University, ChinaCopyright: © 2025 Li, Chen, Fan, Zhu, Deng and Chai. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xin Chai, YW5lc3RoZXRpc3RjaGFpQGFsaXl1bi5jb20=
†These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.