
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Cardiovasc. Med. , 25 February 2025
Sec. General Cardiovascular Medicine
Volume 12 - 2025 | https://doi.org/10.3389/fcvm.2025.1452802
Objective: This study aimed to evaluate the correlation between aerobic exercise intensity based on the 6 min walk test (6MWT) and the anaerobic threshold (AT)-based equivalent in patients with acute myocardial infarction (AMI). The feasibility of using the 6MWT for exercise prescription in primary care settings was also investigated.
Methods: A retrospective analysis was conducted on data from AMI patients, including statistics on all values of the cardiopulmonary exercise test and 6MWT parameters.
Results: Regression analysis showed that the regression equation based on 6MWD exercise intensity (EI6MWD) could predict AT-based exercise intensity (EIAT). Moreover, EI6MWD correlated with EIAT in 91.9%–93.0% of patients' EI6MWD, with AMI equivalent to the EIAT model.
Conclusions: The findings suggest that the anaerobic threshold in AMI patients corresponds to 91.9%–93.0% of the distance covered during the 6MWT. Thus, the 6MWT is a feasible tool for developing exercise prescriptions in primary care hospitals.
Acute myocardial infarction (AMI) is a leading cause of mortality and a major threat to human health (1), with the number of cases rising annually (2). Advances in coronary interventional techniques and clinical management have increased post-surgical survival rates. However, disability and hospitalization rates have also significantly increased (3). Therefore, facilitating early recovery after discharge and reducing readmissions remain critical public health challenges.
Cardiac rehabilitation plays a vital role in improving vascular endothelial and cardiac function, promoting collateral circulation, and preventing the onset and progression of heart failure after AMI. It has been shown to enhance quality of life while reducing the risks of morbidity and mortality associated with cardiovascular disease (4–8). Hence, implementing safe and effective individualized exercise prescriptions as early as possible is essential for optimizing recovery, treatment, and prognosis in AMI patients. The anaerobic threshold (AT) is currently recoginized as a reliable criterion for determining exercise intensity in cardiac rehabilitation for AMI patients (4, 5).
A key factor in effective rehabilitation is selecting an appropriate aerobic exercise intensity for each patient. The cardiopulmonary exercise test (CPET) is considered the gold standard for assessing aerobic capacity with previous studies using it to calculate peak oxygen uptake (peak VO2) and AT (9). Nevertheless, the specialized equipment and high costs associated with CPET limit its widespread clinical application. The 6MWT, a submaximal functional capacity test commonly used in cardiac rehabilitation, offers a practical alternative due to its simplicity, low cost, and ease of operation in all hospitals, especially primary hospitals (10–12). However, AT and peak VO2 cannot be directly or accurately measured using the 6MWT (13, 14). Consequently, no validated method currently exists to develop an exercise prescription equivalent to AT intensity from 6MWT results for guiding exercise rehabilitation in post-AMI patients.
This study aimed to establish an aerobic exercise intensity equivalent to AT for AMI patients based on the 6 min walk distance (6MWD), facilitating the development of cardiac rehabilitation in primary care settings in China.
The data for this study were obtained from a retrospective observational analysis of AMI patients who completed both CPET and 6MWT between December 2016 and December 2022 at the Department of Cardiac Rehabilitation, Daqing Oilfield General Hospital. Inclusion criteria were: (1) age 18–75 years, (2) stable symptoms and signs of myocardial infarction for over 2 weeks, and (3) within 12 months of AMI surgery (15). Patients were excluded if they (1) did not complete the 6MWT with a cardiac ultrasound within 1 day before or after CPET, (2) had mobility problems, uncontrolled hypertension, severe cardiopulmonary failure, malignant ventricular arrhythmias, severe combined hepatic or renal failure, severe cerebrovascular pathology or psychiatric illness, or severe valvular heart disease or cardiomyopathy, or (3) were more than 12 months postoperative AMI (15, 16). Patients were grouped into ST-segment elevation myocardial infarction (STEMI) and non-ST-segment elevation myocardial infarction (N-STEMI) groups according to their electrocardiogram (ECG) changes. All procedures were conducted by a comprehensive cardiac rehabilitation team consisting of 1–2 cardiologists and 1–2 physical therapists.
This study adhered to the Declaration of Helsinki (as revised in 2013) and was approved by the Daqing Oilfield General Hospital Ethics Committee (ZYAF/SC-07/02.0). Informed consent was obtained from all patients.
The 6MWT was performed on a 30-meter flat ground marked at 3-meter intervals. Patients were instructed to walk back and forth along the prescribed test path at their own pace without running. Tests followed uniform standards (17), and the following parameters were recorded: heart rate (HR), peripheral oxygen saturation (SpO2), blood pressure (BP), and symptoms of dyspnea and dizziness, assessed using the Rate of Perceived Exertion (RPE) scale (6–20). The total walk distance was measured, and the average of two test rounds was taken as the final 6MWT result. The intensity of aerobic exercise was determined which based on the patients' average walking speed, termed EI6MWD, calculated as: EI6MWD = 6MWD × 10/1,000 (km/h). For instance, a patient covering 350 meters in the 6MWT would achieve an EI6MWD of 3.5 km/h.
All patients underwent CPET at the Daqing Oilfield Cardiac Rehabilitation Department, following the American College of Cardiology's standard of care and the standard continuous incremental power program used at the Harbor-UCLA Medical Center (4, 18). Testing was conducted using a pulmonary function test system, an exercise test system, and an electric bicycle (CS200, Schiller, Switzerland). The CPET protocol included a 3 min rest period, a 3 min unloaded cycling phase, followed by an incremental workload increase from 0 W/s, with increments of 10–30 W/min based on the patient's age, sex, and estimated functional status. Patients exercised to their symptom-limited maximal effort within 6–10 min, followed by a 5–10 min recovery periode. Patients' resting and peak heart rates, blood pressure, and expiratory breaths were recorded during the CPET. The anaerobic metabolic thresholds were determined using the V-slope method (19). Aerobic exercise intensity, termed EIAT, was determined using AT. The value of EIAT was calculated using the following formula based on metabolic equivalents (METs): EIAT = (METs@AT-1) × 3.5 × 60/100 (km/h). The metabolic equivalent (MET) values were determined by the conversion of aerobic exercise oxygen consumption (1 MET = 3.5 ml/kg/min) (20, 21).
Normally distributed data are shown as mean ± standard deviation (SD), and Pearson's cumulative correlation was used to analyze relationships. Non-normally distributed measures are presented as medians (M) with interquartile spacing (P25, P75), and their relationships were analyzed using Spearman's correlation. Count variables are expressed as composition ratios (%). Correlations between unordered variables (sex) and the measurement data were analyzed using the independent samples t-test, while associations between unordered categorical variables (sex) were assessed using the chi-square test. Multiple linear regression analysis included variables that were significant in univariate analysis and clinically significant. Data were analyzed using SPSS 22.00, with two-tailed testing, and statistical significance was set at P < 0.05.
A total of 467 patients with AMI, aged between 18 and 75 years, underwent CPET at the Daqing Oilfield General Hospital from December 2016 to December 2022. Of these, 429 completed the 6MWT within 24 h before or after CPET. After further refinement, 342 patients who had also undergone echocardiography within the day preceding their CPET were identified. Among them, 142 patients who had undergone AMI surgery more than 12 months earlier were excluded. Ultimately, 200 patients with AMI within the past 12 months were selected based on medical record review and ECG data. Of these, 128 had STEMI and 72 had N-STEMI (Figure 1). Their electronic medical records were analyzed to extract detailed diagnostic information, ancillary test results, body mass index (BMI), and medication history.
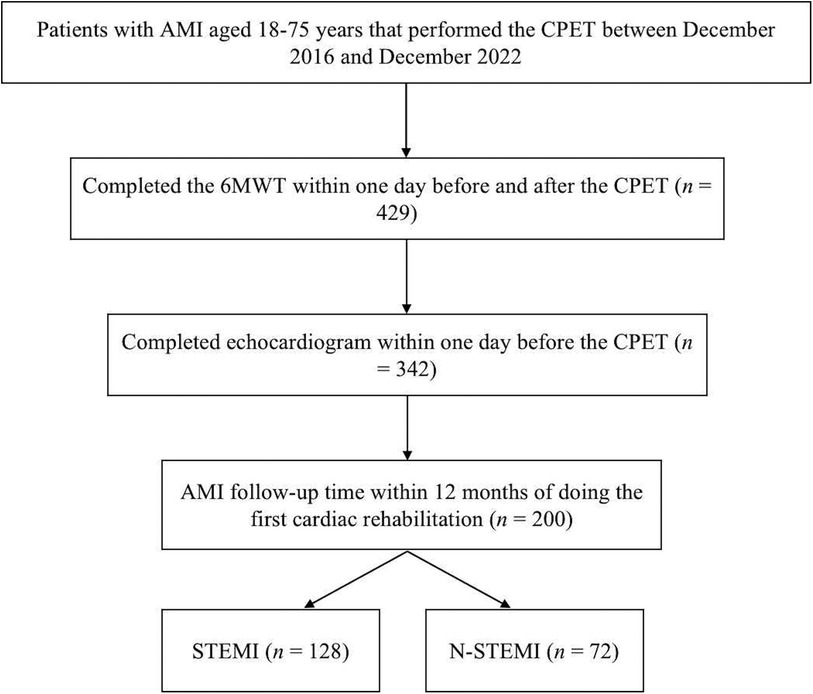
Figure 1. Study flowchart. AMI, acute myocardial infarction; CPET, cardiopulmonary exercise test; 6MWT, 6 min walk test; STEMI, ST-segment elevation myocardial infarction; N-STEMI, non-ST-segment elevation myocardial infarction.
Table 1 shows the characteristics of these 200 AMI patients who completed the CPET, 6MWT, and ECG within 12 months of their AMI. This cohort included 188 males (93.00%), with a median age of 53 years (IQR: 46.00–61.00) and a median BMI of 25.70 kg/m2 (IQR: 24.22–28.40). Infarction classification included 128 patients with STEMI and 72 patients with N-STEMI.
Table 2 presents the study results. A significant difference in left ventricular ejection fraction (LVEF) was observed between the STEMI and N-STEMI groups (P < 0.01). However, there were no significant differences between the two groups in ventilation-to-carbon dioxide output slope (VE/VCO2 slope), AT, or peak VO2 according to the CPET (P > 0.05). In the 6MWT results, no significant differences were found in the correlations between the 6WMD and EI6WMD between the two groups (P > 0.05).
Figure 2 shows the results of the univariate analyses of AT and 6MWD, as well as their correlations with other variables. A strong correlation was observed between age, AT, and 6MWD (Figure 2A–C). Additionally, a significant positive correlation was found between the AT and 6MWD in the AMI group (r = 0.498, P < 0.001) (Figure 2D). The same results were observed in the STEMI group (r = 0.499, P < 0.001) and the N-STEMI group (r = 0.503, P < 0.001).
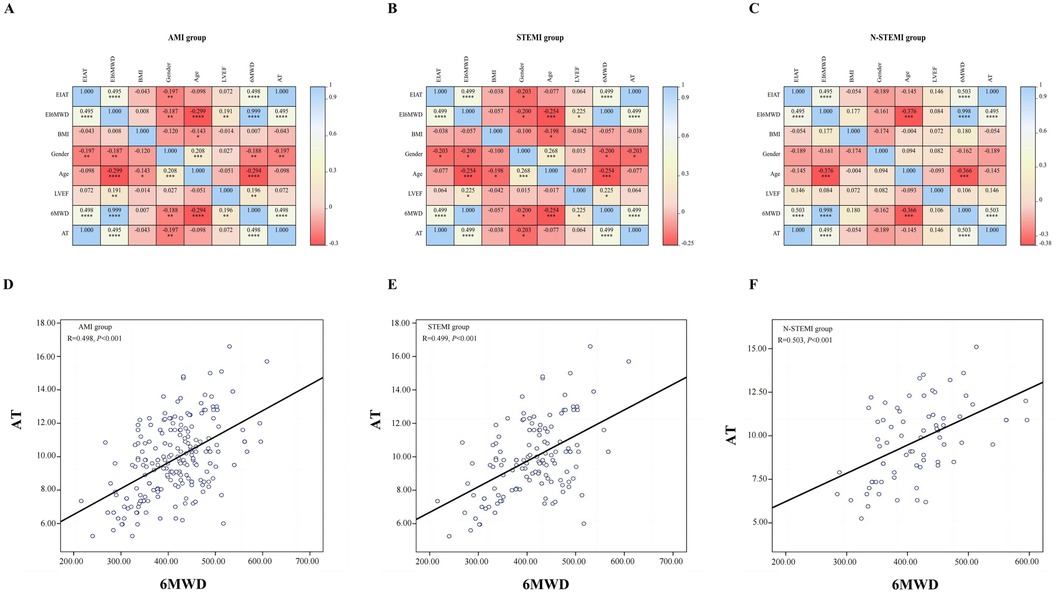
Figure 2. Correlation analysis results with 6MWD and AT. *, P < 0.05; **, P < 0.01; ***, P < 0.005; ****, P < 0.001; 6MWD, 6 min walk distance; AT, anaerobic threshold; AMI, acute myocardial infarction; STEMI, ST-segment elevation myocardial infarction; N-STEMI, non-ST-segment elevation myocardial infarction; (A–C): the correlation between the EIAT, EI6MWD, BMI, Gender, Age, LVEF, 6MWD and AT in the three groups; (D–F): the correlation between 6MWD and AT in the three groups.
We analyzed the AMI group and its subgroups using multiple linear regression (Table 3). The results revealed a positive correlation between EI6MWD and EIAT in the AMI group (P < 0.001). Moreover, this positive correlation was consistently observed across all subgroups in both the STEMI and N-STEMI groups (P < 0.001). The regression equations derived from the multiple regression analysis were as follows: for the AMI group, EIAT = 0.919 × EI6MWD; for the STEMI group, EIAT = 0.93 × EI6MWD; and for the N-STEMI group, EIAT = 0.923 × EI6MWD (Table 3).
The standardized regression coefficients between the EI6MWD and EIAT were compared using the U-test (Table 4). The results demonstrated that the 6MWD and AT had a moderate positive correlation in the AMI group; however, no significant differences were observed between the AMI subgroups (P > 0.05).
This study identified a positive correlation between EI6MWD and EIAT in a retrospective analysis of patients who participated in cardiac rehabilitation exercises within 12 months following AMI surgery. Previous studies have used CPET to measure exercise intensity; however, this method is often unavailable in primary hospitals due to the hight cost of the required equipment (22). In contrast, many studies investigating the relationship between 6MWD and peak VO2 mostly used indirect conversion methods. For instance, Linpkin (23) and Lawrence (24) utilized treadmill tests or bicycle–ergometer tests to determine cardiopulmonary function. However, the results cannot be used universally because the test platforms for the 6MWT and treadmill tests differ significantly (17). Aditionally, previous research has shown that peak VO2 can be estimated from 6MWD. For example, Burr et al. proposed the following equation: peak VO2 = 70.161 + 0.023 × 6MWD (m)—0.276 × body weight (kg)—6.79 × sex (Male = 0; Female = 1)—0.193 × resting heart rate (b.p.m.)—0.191 × age (years) (21). Therefore, the 6MWT, which is applied internationally, could be used to assess exercise capacity in cardiac patients (25, 26). Furthermore, the AT value is commonly employed as an index to quantify cardiac function (27).
Our results suggest that EI6MWD and EIAT are correlated in AMI patients, indicating that 91.9%–93.0% of EI6MWD in AMI patients was equivalent to EIAT. There were no significant differences in AT, peak VO2, or VE/VCO2 slopes among the AMI subgroups at baseline (P > 0.05), indicating no difference in exercise tolerance or ventilation efficiency between the two groups. Furthermore, linear regression analysis demonstrated a positive correlation between 6MWD and AT to varying extents within the AMI group and its subgroups. In a further analysis, the regression equations were as follows: for the AMI group, EIAT = 0.919 × EI6MWD; for the STEMI group, EIAT = 0.93 × EI6MWD; and for the N-STEMI group, EIAT = 0.923 × EI6MWD. These results demonstrated that EIAT can be predicted using EI6MWD, suggesting that aerobic exercise intensity in AMI patients can be estimated using the 6MWT. However, compared to the New York Classification of Cardiac Function, the 6MWT, as a submaximal exercise test for cardiac rehabilitation, provides a more objective representation of patient mobility and cardiac reserve function. In addition, it has been shown to predict long-term mortality and hospitalization rates (28), a consideration widely acknowledged by international researchers. In this study, we concluded that the 6MWT can be used to measure aerobic exercise intensity in AMI patients based on the correlation between exercise intensity as assessed by 6MWT and CPET.
This study has several limitations. Despite spanning an extended period, the sample size—particularly the number of N-STEMI subgroups—was relatively small, which may have affected the fit of the 6MWD to the AT simulation equation in the subgroup analysis. Future studies with larger patient populations are needed. Second, because blood gas and lactate levels were not measured, it remains unclear whether the 6MWT reached the AT. Future studies should incorporate these two indicators. In addition, various factors, such as walking speed and the number of trials performed may affect 6MWT results (18, 19), potentially introducing bias. Since the patients participated in the 6MWT for the first time, further standardization is necessary to improve its accuracy and reproducibility.
This study pioneeringly established an assessment model for anaerobic threshold equivalent exercise intensity (EIAT) based on the 6 min walk test distance (EI6MWD), filling a critical gap in exercise rehabilitation assessment for AMI patients in primary care settings. The results demonstrated that 91.9%–93.0% of AMI patients had EI6MWD values equivalent to EIAT, indicating that the 6 min walk test effectively assesses exercise capacity and provides a foundation for personalized exercise rehabilitation plans. This assessment model is simple, cost-effective, and easy to implement in primary care settings, with the potential to significantly improve exercise rehabilitation rates and prognoses for AMI patients while promoting equitable development in cardiac rehabilitation.
Moreover, this study presents a novel solution for cardiac rehabilitation in community hospitals lacking CPET equipment, which has the potential to enhance its accessibility in developing countries and primary care settings.
However, further validation in larger populations is still needed, and the model's applicability across diverse patient groups should be explored.
The raw data supporting the conclusions of this article will be made available by the corresponding authors, without undue reservation.
The studies involving humans were approved by Daqing Oilfield General Hospital Ethics Committee (ZYAF/SC-07/02.0). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
YF: Formal analysis, Visualization, Writing – original draft, Writing – review & editing. XS: Investigation, Writing – original draft. GL: Investigation, Writing – original draft. XW: Investigation, Writing – original draft. QL: Writing – review & editing. LW: Supervision, Writing – review & editing. YS: Supervision, Writing – review & editing. ZF: Supervision, Conceptualization, Writing – review & editing.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. The study was supported by the Shanghai Health Commission, Key Supporting Disciplines of Shanghai Municipal Health System (Grant No. 2023ZDFC0302).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declare that no Generative AI was used in the creation of this manuscript.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Ades PA. Cardiac rehabilitation and secondary prevention of coronary heart disease. N Engl J Med. (2001) 345(12):892–902. doi: 10.1056/NEJMra001529
2. Liyuan MA, Zengwu WANG, Jing FAN, Shengshou HU. Epidemiology and management of hypertension in China: an analysis using data from the annual report on cardiovascular health and diseases in China (2021). Chin Gen Pract. (2022) 25(30):3715–20. doi: 10.12114/j.issn.1007-9572.2022.0502
3. Song J, Murugiah K, Hu S, Gao Y, Li X, Krumholz HM, et al. Incidence, predictors, and prognostic impact of recurrent acute myocardial infarction in China. Heart. (2021) 107(4):313–8. doi: 10.1136/heartjnl-2020-317165
4. Ibanez B, James S, Agewall S, Antunes MJ, Bucciarelli-Ducci C, Bueno H, et al. 2017 ESC guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: the task force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. (2018) 39(2):119–77. doi: 10.1093/eurheartj/ehx393
5. Dibben G, Faulkner J, Oldridge N, Rees K, Thompson DR, Zwisler AD, et al. Exercise-based cardiac rehabilitation for coronary heart disease. Cochrane Database Syst Rev. (2021) 2021(11):CD001800. doi: 10.1002/14651858.CD001800.pub4
6. Thomas RJ, Balady G, Banka G, Beckie TM, Chiu J, Gokak S, et al. 2018 ACC/AHA clinical performance and quality measures for cardiac rehabilitation: a report of the American College of Cardiology/American Heart Association task force on performance measures. J Am Coll Cardiol. (2018) 71(16):1814–37. doi: 10.1016/j.jacc.2018.01.004
7. Thompson PD, Franklin BA, Balady GJ, Blair SN, Corrado D, Estes NA 3rd, et al. Exercise and acute cardiovascular events placing the risks into perspective: a scientific statement from the American Heart Association council on nutrition, physical activity, and metabolism and the council on clinical cardiology. Circulation. (2007) 115(17):2358–68. doi: 10.1161/CIRCULATIONAHA.107.181485
8. Mediano MFF, Leifer ES, Cooper LS, Keteyian SJ, Kraus WE, Mentz RJ, et al. Influence of baseline physical activity level on exercise training response and clinical outcomes in heart failure: the HF-ACTION trial. JACC Heart Fail. (2018) 6(12):1011–9. doi: 10.1016/j.jchf.2018.09.012
9. Guazzi M, Myers J, Abella J, Peberdy MA, Bensimhon D, Chase P, et al. The added prognostic value of ventilatory efficiency to the Weber classification system in patients with heart failure. Int J Cardiol. (2008) 129(1):86–92. doi: 10.1016/j.ijcard.2007.05.028
10. Pepera GK, Sandercock GR, Sloan R, Cleland JJ, Ingle L, Clark AL. Influence of step length on 6-minute walk test performance in patients with chronic heart failure. Physiotherapy. (2012) 98(4):325–9. doi: 10.1016/j.physio.2011.08.005
11. Coulshed A, Coulshed D, Pathan F. Systematic review of the use of the 6-minute walk test in measuring and improving prognosis in patients with ischemic heart disease. CJC Open. (2023) 5(11):816–25. doi: 10.1016/j.cjco.2023.08.003
12. Enright PL, Sherrill DL. Reference equations for the six-minute walk in healthy adults. Am J Respir Crit Care Med. (1998) 158(5 Pt 1):1384–7. doi: 10.1164/ajrccm.158.5.9710086
13. Pepera G, Ingle L, Sandercock GR. Predictors of the 6-minute walk test in patients with chronic heart failure. Br J Cardiac Nurs. (2015) 10:454–9. doi: 10.12968/bjca.2015.10.9.454
14. Rostagno C, Olivo G, Comeglio M, Boddi V, Banchelli M, Galanti G, et al. Prognostic value of 6-minute walk corridor test in patients with mild to moderate heart failure: comparison with other methods of functional evaluation. Eur J Heart Fail. (2003) 5(3):247–52. doi: 10.1016/s1388-9842(02)00244-1
15. He X. Effect of cardiac rehabilitation on percutaneous coronary intervention in patients with acute myocardial infarction. Cardiovasc Dis J Integr Trad Chin West Med. (2017) 5(18):33–4. doi: 10.16282/j.cnki.cn11-9336/r.2017.18.025
16. American College of Sports Medicine. American College of Sports Medicine’s Guidelines for Exercise Testing and Prescription. 10th edn Phliadephia: Wolters Kluwer Health (2018).
17. ATS Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories. ATS Statement: guidelines for the six-minute walk test. Am J Respir Crit Care Med. (2002) 166(1):111–7. doi: 10.1164/ajrccm.166.1.at1102
18. Sun XG, Hansen JE, Beshai JF, Wasserman K. Oscillatory breathing and exercise gas exchange abnormalities prognosticate early mortality and morbidity in heart failure. J Am Coll Cardiol. (2010) 55(17):1814–23. doi: 10.1016/j.jacc.2009.10.075
19. Beaver WL, Wasserman K, Whipp BJ. A new method for detecting anaerobic threshold by gas exchange. J Appl Physiol. (1986) 60(6):2020–7. doi: 10.1152/jappl.1986.60.6.2020
20. Pescatello LS. ACSM’s Guidelines for Exercise Testing and Prescription. 9th edn Philadelphia: Wolters Kluwer/Lippincott Williams & Wilkins Health (2014). p. 456.
21. Luo Q, Li C, Zhuang B, Li G, Luo L, Ni Y, et al. Establishment of exercise intensity for patients with chronic heart failure equivalent to anaerobic threshold based on 6-minute walking test. Ann Palliat Med. (2020) 9(5):2766–75. doi: 10.21037/apm-20-265
22. Burr JF, Bredin SS, Faktor MD, Warburton DE. The 6-minute walk test as a predictor of objectively measured aerobic fitness in healthy working-aged adults. Phys Sportsmed. (2011) 39(2):133–9. doi: 10.3810/psm.2011.05.1904
23. Lipkin DP. The role of exercise testing in chronic heart failure. Br Heart J. (1987) 58(6):559–66. doi: 10.1136/hrt.58.6.559
24. Cahalin L, Pappagianopoulos P, Prevost S, Wain J, Ginns L. The relationship of the 6-min walk test to maximal oxygen consumption in transplant candidates with end-stage lung disease. Chest. (1995) 108(2):452–9. doi: 10.1378/chest.108.2.452
25. Quittan M, Wiesinger GF, Crevenna R, Nuhr MJ, Posch M, Hülsmann M, et al. Cross-cultural adaptation of the Minnesota living with heart failure questionnaire for German-speaking patients. J Rehabil Med. (2001) 33(4):182–6. doi: 10.1080/165019701750300654
26. Cahalin LP, Mathier MA, Semigran MJ, Dec GW, DiSalvo TG. The six-minute walk test predicts peak oxygen uptake and survival in patients with advanced heart failure. Chest. (1996) 110(2):325–32. doi: 10.1378/chest.110.2.325
27. Arena R, Myers J, Abella J, Pinkstaff S, Brubaker P, Kitzman D, et al. Defining the optimal prognostic window for cardiopulmonary exercise testing in patients with heart failure. Circ Heart Fail. (2010) 3(3):405–11. doi: 10.1161/CIRCHEARTFAILURE.109.906446
Keywords: exercise rehabilitation, acute myocardial infarction, 6-minute walk test, anaerobic threshold, exercise intensity
Citation: Fan Y, Sun X, Li G, Wang X, Luo Q, Wang L, Shen Y and Fan Z (2025) Exploring the exercise intensity equivalent to the anaerobic threshold in patients with acute myocardial infarction based on the 6-minute walk test distance. Front. Cardiovasc. Med. 12:1452802. doi: 10.3389/fcvm.2025.1452802
Received: 12 November 2024; Accepted: 12 February 2025;
Published: 25 February 2025.
Edited by:
Nicola Mumoli, ASST Ovest Milanese, ItalyReviewed by:
Garyfallia Pepera, University of Thessaly, GreeceCopyright: © 2025 Fan, Sun, Li, Wang, Luo, Wang, Shen and Fan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yuqin Shen, c3lfMTk2M0AxMjYuY29t; Zhiqing Fan, emhpcWluZ2ZhbkAxMjYuY29t
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.