- 1Department of Nursing, Taicang TCM Hospital Affiliated to Nanjing University of Chinese Medicine, Suzhou, China
- 2Department of Gastroenterology, Taicang TCM Hospital Affiliated to Nanjing University of Chinese Medicine, Suzhou, China
- 3Department of Cardiovascular Medicine, Taicang TCM Hospital Affiliated to Nanjing University of Chinese Medicine, Suzhou, China
- 4Department of Cardiovascular Medicine, First Affiliated Hospital of Soochow University, Suzhou, China
Background: Improving medication compliance and self-efficacy in hypertensive patients is of significant importance for their prognosis. This meta-analysis aimed to assess the role of motivational interviewing in reducing systolic and diastolic blood pressure, self-efficacy, quality of life and medication adherence in hypertensive patients.
Methods: Two authors searched PubMed, Cochrane Library, Clinicaltrials, Embase, Web of Science, China National Knowledge Infrastructure (CNKI), Chinese Biomedical Literature Database, Weipu and Wanfang Database up to May 28, 2024 for randomized controlled trials (RCTs) evaluating the role of motivational interviewing on hypertensive patients. The search was restricted to articles published in English and Chinese languages. RevMan 5.4 software was used for meta-analysis.
Results: A total of 16 RCTs were included. The meta-analysis findings demonstrate that motivational interviewing could reduce both systolic pressure [MD = −3.26, 95% CI (−5.16, −1.36), P < 0.001] and diastolic blood pressure [MD = −1.78, 95% CI (−3.48, −0.08), P < 0.001] levels in hypertensive patients, while simultaneously enhancing their self-efficacy [MD = 2.92, 95% CI (1.84, 4.00), P = 0.001], quality of life [MD = 6.99, 95% CI (3.25, 10.74), P = 0.003], and medication compliance [OR = 4.30, 95% CI (1.53, 12.10), P = 0.003]. No significant publication bias across the synthesized outcomes were found by Egger regression analyses (all P > 0.05).
Conclusions: Motivational interviewing has been shown to effectively reduce blood pressure in the short term among individuals with hypertension, while simultaneously enhancing their self-efficacy, quality of life, and adherence to medication regimens.
Introduction
Hypertension is one of the most common chronic diseases worldwide and is also one of the major public health issues globally (1). The prevalence of hypertension among people over 18 years old in our country has exceeded 30%, and the population with hypertension exhibits the following characteristics: high incidence, high mortality, high disability rate, low awareness, low control rate, and low medication compliance rate (2–4). It is reported that the medication compliance rate of hypertension patients in China is only 42.5% (5). In recent years, although the awareness, treatment rate, and control rate of hypertension patients have improved, they are still at a relatively low level, which is related to the lack of disease knowledge and weak self-management ability among hypertension patients (6, 7). Studies (8, 9) have shown that unhealthy lifestyle behaviors can increase the incidence of cardiovascular complications in patients. By intervening in patients’ behavior and disease cognition, patients' initiative can be improved, self-management ability can be enhanced, and the quality of life can be improved (10, 11). Therefore, helping individuals establish healthy behavioral patterns is particularly important in hypertension prevention and management.
Motivational Interviewing, a counseling approach developed by William R. Miller (12, 13) and Stephen Rollnick (14), is a scientifically validated method that has been recognized for its efficacy in addressing lifestyle-related issues and disease management. It is regarded as a valuable intervention strategy, leveraging motivation enhancement techniques to foster behavior change (15). Its appeal lies in its accessibility and economic viability, which has endeared it to patients and their kin (16). The robust theoretical framework of motivational interviewing has garnered significant attention from clinical nursing professionals and scholars within the field. Characterized by its client-centered and directive methodology, motivational interviewing is specifically tailored to address and clarify the client's ambivalence during the process of behavioral change. This approach emphasizes the importance of understanding and navigating the complexities of ambivalence, thereby enhancing the effectiveness of the intervention (17). Motivational interviewing is instrumental in fostering the adoption and sustenance of healthy behaviors among hypertensive patients (18). It also aids in the effective management of blood pressure and holds potential for bolstering patients' self-efficacy (19). While the findings are encouraging, the majority of the studies are limited by their small sample sizes. This limitation restricts the generalizability of the conclusions and weakens the evidence supporting the efficacy of motivational interviewing in the management of hypertension. To address this gap, the objective of this study is to evaluate the efficacy of motivational interviewing in reducing systolic and diastolic blood pressure, enhancing self-efficacy, improving quality of life, and promoting medication adherence among patients with hypertension.
Methods
This meta-analysis was conducted and reported according to the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) statement (20). The requirement for ethical approval and written informed consent was deemed unnecessary for this meta-analysis, as it does not involve the collection, analysis, or reporting of individual participant data.
Literature search strategies
In this study, a comprehensive computer-assisted literature search was performed across multiple databases, including PubMed, Cochrane Library, Clinicaltrials, Embase, Web of Science, China National Knowledge Infrastructure (CNKI), Chinese Biomedical Literature Database, Weipu and Wanfang Database. The search encompassed records from the inception of these databases up to May 28, 2024, employing a strategic combination of Medical Subject Headings (MeSH) and key textual terms. The search strategy for this study was formulated as follows: (“motivational interviewing” OR “motivation interview” OR “MI” OR “motivational counseling”) AND (“hypertension” OR “high blood pressure”).
Inclusion and exclusion criteria
The inclusion criteria for this meta-analysis were as follows: The inclusion criteria for this meta-analysis, as determined in the past and reorganized according to the PICOS framework, were as follows: Population (P): Adults (age ≥18years old) who had been diagnosed with hypertension, according to the “Guidelines for the Diagnosis and Treatment of Hypertension” established jointly by the World Health Organization (WHO) and the International Society of Hypertension. Hypertension was identified by a systolic blood pressure of ≥140 mmHg and/or a diastolic blood pressure of ≥90 mmHg. Intervention (I): The studies had to involve an intervention group that utilized motivational interviewing as part of the treatment approach. Comparison (C): There had to be a control group receiving standard care, which could include routine medical treatment without the addition of motivational interviewing. Outcomes (O): The studies had to report on outcome measures relevant to the impact of motivational interviewing on hypertensive patients. These outcomes included blood pressure levels, self-efficacy, quality of life, and medication compliance. Study Design (S): Only RCTs that investigated the impact of motivational interviewing on hypertensive patients were considered for inclusion in the meta-analysis.
The exclusion criteria for this meta-analysis were as follows: Review articles and case studies; literature with incomplete data; and duplicate publications.
Literature screening and data extraction
In the process of literature screening and data extraction, two independent reviewers meticulously assessed the literature in accordance with pre-established inclusion and exclusion criteria, followed by a thorough cross-verification. Any discrepancies were resolved through collaborative deliberation or by seeking the guidance of subject matter experts. Utilizing a custom-designed form, we systematically extracted pertinent data, encompassing the following elements: authorship, year of publication, geographical context, duration of study, nature of interventions, temporal aspects of intervention delivery, frequency of intervention application, identity of intervention facilitators, and the pertinent outcome measures.
Assessment of literature quality
Two researchers independently utilized the Cochrane Risk of Bias tool (21) to evaluate the studies, with any disagreements resolved through consultation with a third-party expert. The evaluation encompasses several aspects including the generation of random sequences, allocation concealment, implementation of blinding, incomplete reporting of data, selective reporting, and other potential biases. Each component can be rated as having a “low, medium, or high risk of bias”.
Statistical analysis
In this investigation, we utilized the RevMan 5.4 software to conduct a meta-analysis. The assessment of heterogeneity across the study outcomes was performed through a heterogeneity test. The absence or minimal presence of heterogeneity was inferred when the P-value was greater than or equal to 0.1 and the I2 statistic was below 50%, thereby justifying the application of a fixed-effects model. Conversely, when the P-value was less than 0.1 and the I2 statistic exceeded 50%, substantial heterogeneity was identified, prompting the execution of subgroup analyses or sensitivity analyses to elucidate the underlying causes. In these instances, a random-effects model was employed. For the analysis of continuous variables, the mean difference (MD) was selected as the metric for effect size, while the odds ratio (OR) was utilized for categorical data to quantify the effect size. The results for all effect sizes were reported alongside a 95% confidence interval (CI) to provide a measure of precision and statistical confidence. The threshold for statistical significance in this meta-analysis was set at a P-value of less than 0.05.
Results
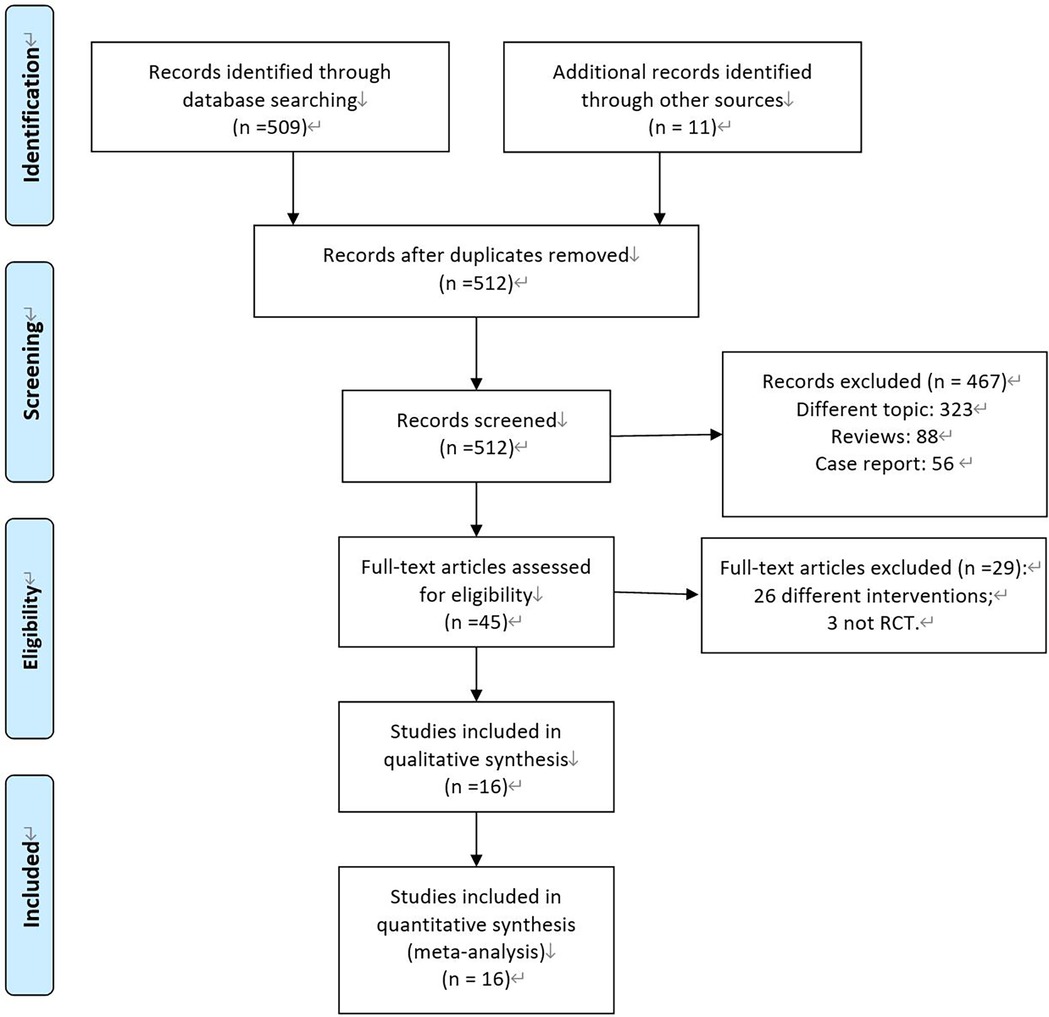
As shown in Figure 1, the study initially retrieved a total of 520 relevant literatures. After excluding duplicate records using EndNote software, 512 remained. After an initial screening based on titles and abstracts, 467 articles were excluded. After reading 45 full texts in detail, 16 RCTs (22–37) were finally included based on the inclusion and exclusion criteria.
Characteristics of included RCTs
As shown in Table 1, the 16 included studies originated from China, the United States, Ireland, and Denmark. All studies included in the review used motivational interviewing as the intervention method. The duration of the intervention ranged from one month to 18 months, with each session lasting between 10 and 40 min. The most commonly reported study outcomes were the levels of systolic and diastolic blood pressure after the intervention.
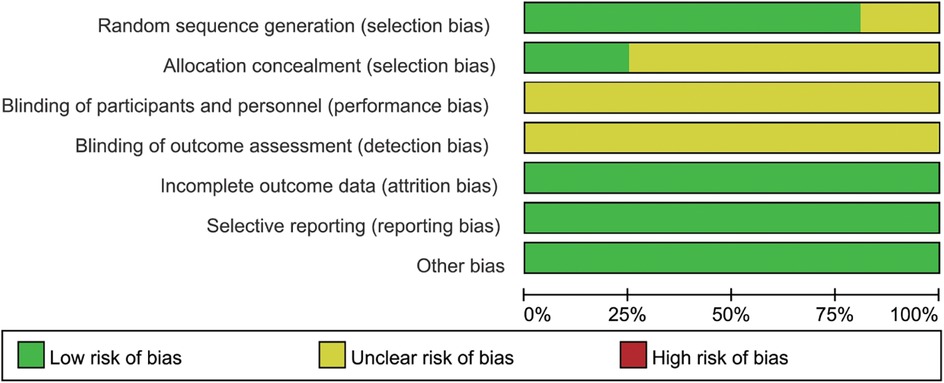
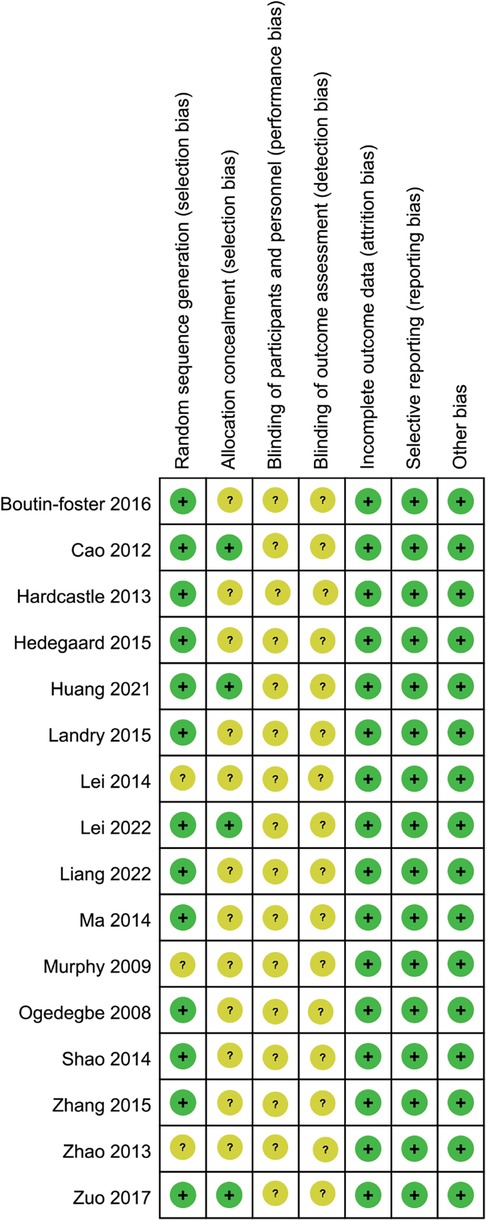
As depicted in Figures 2, 3, while RCTs discussed in this analysis had explicitly stated the adoption of a random study design, it was noteworthy that three of these studies had failed to provide details regarding the specific techniques employed for generating the randomization sequence. This lack of transparency could have potentially impacted the reliability of the study outcomes. Additionally, four studies had been found to have implemented measures for allocation concealment, a critical component in ensuring the integrity of the randomization process. Given the intrinsic nature of the motivational interviewing intervention, it had been deemed impractical to blind both the participants and the interventionists to the study conditions. This was a common challenge in trials involving psychological interventions, where the interactive nature of the therapy made blinding difficult. Despite this limitation, it was reassuring to observe that all studies included in the analysis had reported comparable baseline data across all groups, which helped to mitigate concerns regarding selection bias. Furthermore, each study had diligently documented patient attrition and dropout rates, which was essential for assessing the overall integrity of the study and the generalizability of its findings. Upon thorough examination, no other potential sources of bias had been identified within the studies reviewed.
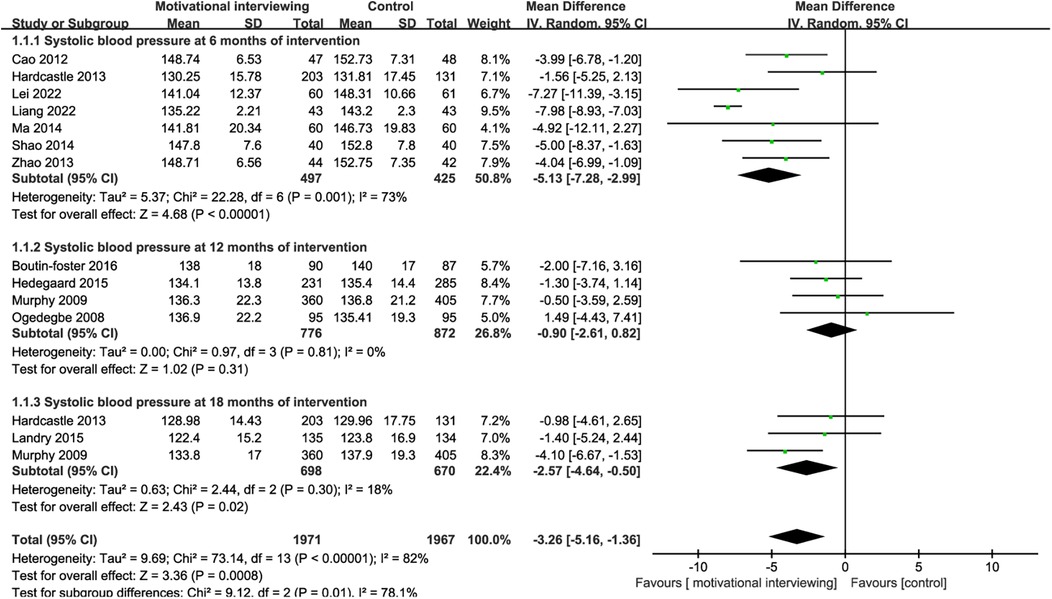
12 RCTs reported the impact of motivational interviewing on the systolic blood pressure of hypertensive patients. There was significant heterogeneity among the studies (I2 = 82%, P < 0.001), leading to the use of a random-effects model for the meta-analysis. The results indicated that motivational interviewing intervention was effective in reducing the systolic blood pressure of hypertension patients [MD = −3.26, 95% CI (−5.16, −1.36), P < 0.001, Figure 4]. Due to the varying intervention durations across the included studies, we conducted subgroup analyses based on the intervention times. Subgroup analysis indicated that motivational interviewing intervention was effective in reducing the systolic blood pressure of hypertension patients at 6 months[MD = −5.13, 95% CI (−7.28, −2.99), P < 0.001] and 18 months[MD = −2.57, 95% CI (−4.64, −0.50), P = 0.02, Figure 4C] of intervention, no significant effects on the systolic blood pressure at 12 months [MD = −0.90, 95% CI (−2.61, 0.82), P = 0.31] were found.
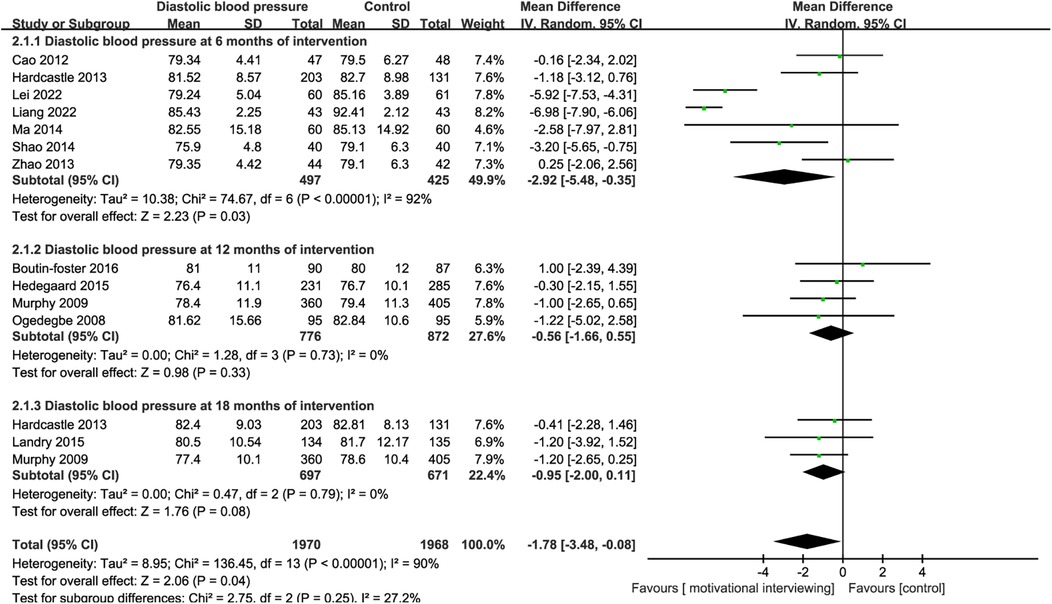
10 RCTs reported the impact of motivational interviewing on the diastolic blood pressure of hypertensive patients. There was significant heterogeneity among the studies (I2 = 90%, P < 0.001), leading to the use of a random-effects model for the meta-analysis. The results indicated that motivational interviewing intervention was effective in reducing the diastolic blood pressure of hypertension patients [MD = −1.78, 95% CI (−3.48, −0.08), P < 0.001, Figure 5]. Due to the varying intervention durations across the included studies, we conducted subgroup analyses based on the intervention times. Subgroup analysis indicated that motivational interviewing intervention was effective in reducing the diastolic blood pressure of hypertension patients at 6 months[MD = −2.92, 95% CI (−5.48, −0.35), P < 0.001] of intervention, no significant effects on the diastolic blood pressure at 12 months[MD = −0.56, 95% CI (−1.66, 0.55), P = 0.33, Figure 5B] and 18 months [MD = −0.95, 95% CI (−2.00, 0.11), P = 0.08] were found.
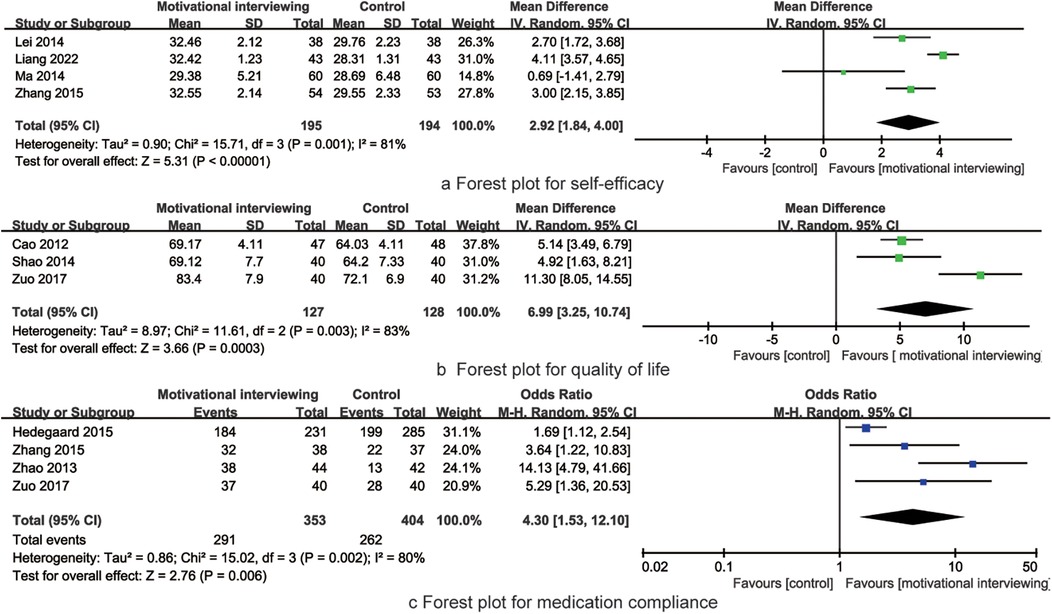
4 RCTs reported the impact of motivational interviewing on the self-efficacy of hypertensive patients. There was significant heterogeneity among the studies (I2 = 81%, P = 0.001), leading to the use of a random-effects model for the meta-analysis. The results indicated that motivational interviewing intervention was effective in improving the self-efficacy of hypertension patients [MD = 2.92, 95% CI (1.84, 4.00), P = 0.001, Figure 6A].
3 RCTs reported the impact of motivational interviewing on the quality of life of hypertensive patients. There was significant heterogeneity among the studies (I2 = 83%, P = 0.003), leading to the use of a random-effects model for the meta-analysis. The results indicated that motivational interviewing intervention was effective in improving the quality of life of hypertension patients [MD = 6.99, 95% CI (3.25, 10.74), P = 0.003, Figure 6B].
4 RCTs reported the impact of motivational interviewing on the medication compliance of hypertensive patients. There was significant heterogeneity among the studies (I2 = 80%, P = 0.002), leading to the use of a random-effects model for the meta-analysis. The results indicated that motivational interviewing intervention was effective in improving the medication compliance of hypertension patients [OR = 4.30, 95% CI (1.53, 12.10), P = 0.003, Figure 6C].
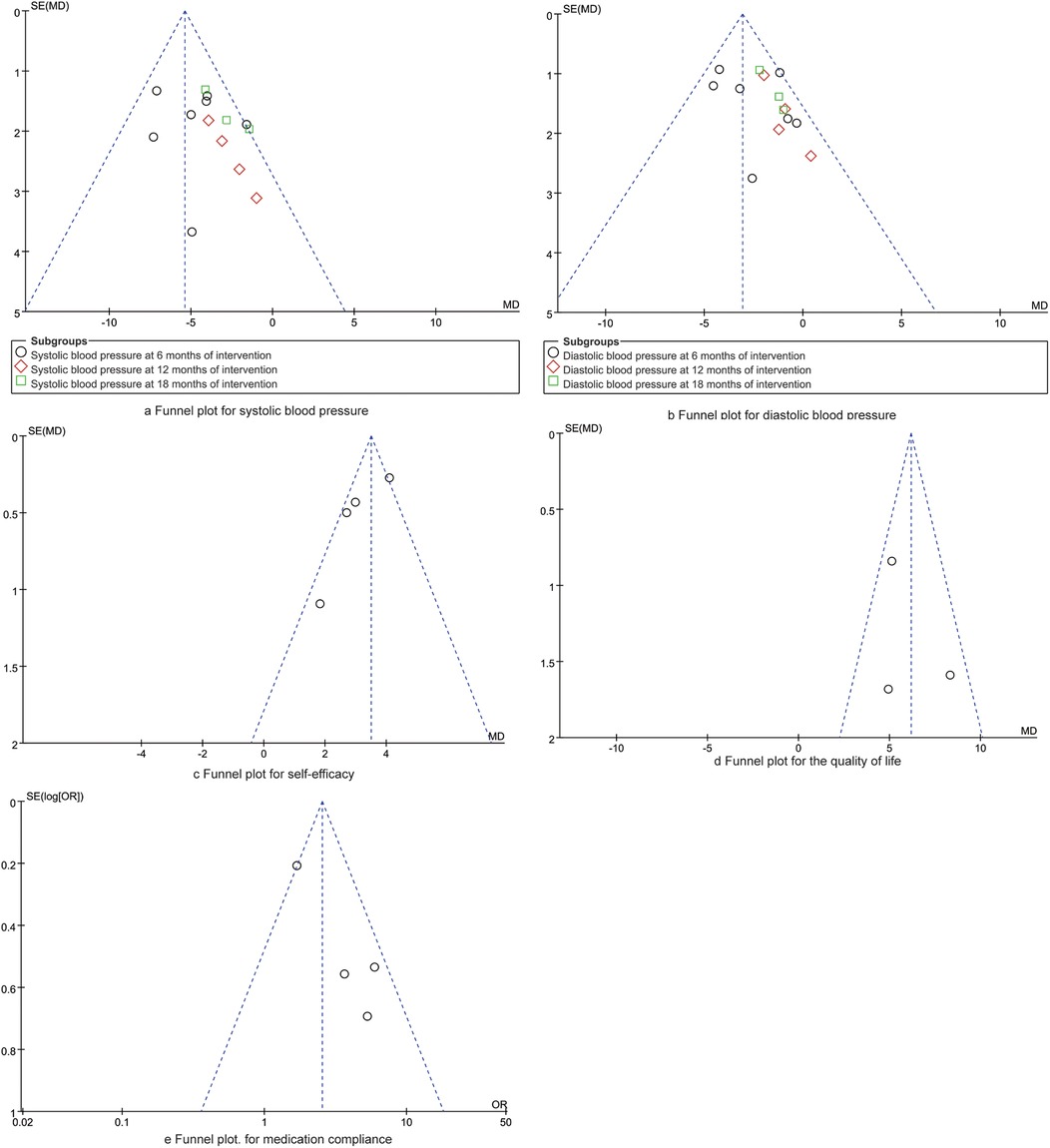
As presented in Figure 7, the symmetrical distribution of dots within the funnel plot suggests a balanced and comprehensive representation of the studies included in the analysis. Furthermore, the Egger regression analysis yielded results indicating no significant publication bias across the synthesized outcomes (P > 0.05).
Discussion
Hypertension is a chronic disease that often goes unnoticed until it leads to severe health complications (38, 39). When hypertension symptoms are mild or not noticeable, patients might not realize how serious their condition is and could unintentionally neglect its management. This unawareness can result in poor self-care and self-management, which are key to regulating blood pressure and stopping the disease from getting worse (40, 41). Research (42) has indicated that although basic health education can boost a patient's comprehension of their illness, it doesn't always lead to better self-management practices. This indicates a significant challenge in chronic disease management, such as hypertension, where there's a disconnect between knowing what to do and actually doing it. The meta-analysis indicates that motivational interviewing is effective at reducing blood pressure in patients with hypertension. By boosting patients' self-efficacy—their confidence in managing their condition—this method can lead to better medication adherence, healthier lifestyle decisions, and an enhanced quality of life.
The results of this meta-analysis suggest that motivational interviewing is associated with a reduction in blood pressure levels among patients. However, it is important to note that there were variations in the control of blood pressure at various time points throughout the study. In the early stages of motivational interviewing intervention, patients become aware of the importance of blood pressure control. After being provided with personalized and gradual guidance by the interviewer on issues related to blood pressure control, patients' cognition of hypertension is enhanced, and their intrinsic motivation is stimulated, leading to behavioral changes (43). Patients increasingly recognize the importance of blood pressure monitoring and adopt healthier lifestyle practices, which consequently lead to a significant reduction in their blood pressure levels. Following the commencement of the motivational interviewing intervention, it has been observed that within six months, patients' self-awareness may wane into a state of complacency, leading to intermittent fluctuations in blood pressure control. Nevertheless, as time elapses, with the ongoing support of the motivational interviewing practitioner, patients' behaviors and lifestyle choices evolve into more consistent patterns. This development, coupled with an enhanced sense of self-efficacy, enables them to effectively manage their blood pressure levels over the long term (44). Furthermore, motivational interviewing strengthens supervision and guidance on patients' execution of behavior change plans, affirms their successes, and helps patients address difficulties encountered during the behavior change process, thus playing a motivational and reinforcing role (45).
Previous research (46) suggests that improving self-efficacy is crucial for enhancing patient behavior and health outcomes, with the enhancement of self-efficacy and self-management considered an ideal model for the control of hypertension. Motivational Interviewing has been shown to increase self-efficacy and medication adherence among hypertensive patients (47). The principal factors contributing to suboptimal medication adherence among hypertensive patients include the belief that long-term medication regimens are excessively challenging and a deficiency in self-confidence regarding their capacity to maintain adherence over time (48). Therefore, a strong belief in medication adherence is vital for patients. Motivational interviewing, based on respect for the patient's thoughts and emotions, employs a range of communication skills to encourage patients to explore their inner conflicting emotions in a harmonious atmosphere and therapeutic environment, identifying areas of weak self-efficacy (49). Motivational interviewing tailors its approach to individual differences, instilling confidence in patients to address their own issues; it guides patients in self-encouragement and self-motivation, thereby stimulating their inner potential and enhancing self-efficacy, which in turn strengthens the patient's medication compliance (50). The main factors affecting the quality of life in hypertensive patients are medication adherence, psychological status, sleep quality, self-efficacy, lifestyle, and the level of knowledge about hypertension (51, 52). Upon a multifaceted assessment of these determinants by the motivational interviewing practitioner, a viable and holistic intervention strategy can be delineated. Through systematic guidance, patients are enlightened about the criticality of punctual medication adherence, lifestyle modifications, emotional regulation, and the incorporation of appropriate physical activity for the management of blood pressure. This approach underscores the significance of self-management in disease control, culminating in lowered blood pressure and an enhanced quality of life for the patients (53, 54).
This meta-analysis has several limitations that warrant consideration. Firstly, a limitation of this study is that the protocol was not registered with the PROSPERO database, which could have offered a transparent and publicly accessible record of our research methodology and outcomes. This omission may impact the generalizability of our findings and the feasibility for other researchers to replicate our study. We acknowledge this shortcoming and recommend that future studies should prioritize registration in PROSPERO to enhance the credibility and transparency of their research. Secondly, the current study only searched for literature in Chinese and English, and due to language factors, there may be an incomplete collection of documents. Thirdly, several of the RCTs incorporated in the analysis did not delineate the precise methodology for generating the random sequence and concealing allocation, which introduces an elevated risk of bias into the study's findings. Finally, although this meta-analysis established strict criteria for the inclusion and exclusion of literature, the lack of a standardized motivational interviewing intervention protocol, variations in the training received by researchers in motivational interviewing, and differences in patient education levels, as well as the duration and frequency of motivational interviewing interventions, may be one of the reasons for the clinical heterogeneity observed. In current clinical practice, the frequency and duration of motivational interviewing interventions vary, as does the content of the interventions. The interviewers' skills also show a wide range of proficiency, and these factors may all exert some influence on the study outcomes. Thus, future studies should aim to refine the content of motivational interviewing interventions, determine the optimal frequency and duration of sessions, and develop a standardized system for conducting these interviews. It would also be beneficial for research to incorporate both quantitative and qualitative methods. Timely documentation of patients’ internal feelings during the motivational interviewing process is crucial. Post-intervention, patient interviews should be conducted to gather their subjective experiences.
Conclusions
In conclusion, the results of this meta-analytic investigation highlight the effectiveness of motivational interviewing in reducing blood pressure levels in the short term (up to six months) among individuals with hypertension. Concurrently, this approach has been shown to enhance patients' self-efficacy, quality of life, and adherence to medication regimens. Given its economic feasibility and practical applicability, motivational interviewing should be considered for integration and adoption within clinical practice. Nevertheless, the limited evidence on the optimal timing and frequency for achieving the best outcomes from motivational interviewing highlights a need for further research. Future studies should focus on refining these methods, establishing standardized interview protocols, and developing thorough training programs for healthcare providers. These efforts are crucial to adapt motivational interviewing to the varying educational levels and disease stages of the hypertensive patients.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Author contributions
JX: Investigation, Writing – original draft. XG: Investigation, Methodology, Writing – original draft. JG: Investigation, Writing – original draft. LZ: Investigation, Writing – original draft. ML: Investigation, Writing – original draft. CH: Investigation, Writing – original draft.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
CNKI, China National Knowledge Infrastructure; PRISMA: preferred reporting items for systematic reviews and meta-analyses; MeSH: medical subject headings; WHO: World Health Organization; RCTs: randomized controlled trials; MD: mean difference; OR: odds ratio; CI: confidence interval.
References
1. Bludorn J, Railey K. Hypertension guidelines and interventions. Prim Care. (2024) 51(1):41–52. doi: 10.1016/j.pop.2023.07.002
2. Hisamatsu T, Miura K. Epidemiology and control of hypertension in Japan: a comparison with western countries. J Hum Hypertens. (2024) 38(6):469–76. doi: 10.1038/s41371-021-00534-3
3. Abalos JB, Saito Y, Ramos MA Jr., Cruz GT. Prevalence, awareness, treatment, and control of hypertension among older adults in the Philippines. J Gerontol A Biol Sci Med Sci. (2024) 79(2):14–8. doi: 10.1093/gerona/glad155
4. Egan BM, Mattix-Kramer HJ, Basile JN, Sutherland SE. Managing hypertension in older adults. Curr Hypertens Rep. (2024) 26(4):157–67. doi: 10.1007/s11906-023-01289-7
5. Yin R, Yin L, Li L, Silva-Nash J, Tan J, Pan Z, et al. Hypertension in China: burdens, guidelines and policy responses: a state-of-the-art review. J Hum Hypertens. (2022) 36(2):126–34. doi: 10.1038/s41371-021-00570-z
6. Zhang M, Shi Y, Zhou B, Huang Z, Zhao Z, Li C, et al. Prevalence, awareness, treatment, and control of hypertension in China, 2004–18: findings from six rounds of a national survey. Br Med J. (2023) 380:e071952.
7. Lu J, Lu Y, Wang X, Li X, Linderman GC, Wu C, et al. Prevalence, awareness, treatment, and control of hypertension in China: data from 1.7 million adults in a population-based screening study (China PEACE million persons project). Lancet. (2017) 390(10112):2549–58. doi: 10.1016/S0140-6736(17)32478-9
8. Redon J, Carmena R. Present and future of drug therapy in hypertension: an overview. Blood Press. (2024) 33(1):2320401. doi: 10.1080/08037051.2024.2320401
9. Zhang Z, Liu Y, Yu W. Effect of online and offline integrated health education on compliance, health behavior and satisfaction of middle-aged hypertensive patients. Qilu J Nurs. (2023) 29(9):100–3.
10. Chen W, Qiu Y, Pan X. Investigation of medication compliance and analysis of influencing factors in patients with hypertension and diabetes mellitus. Chin Gen Med. (2024) 22(4):601–4.
11. Xiao H, Xu J, Lei L. Path analysis of influencing factors of medication compliance in elderly patients with hypertension based on Green’s model. J Pract Cardiac Cerebropulm Vasc Dis. (2024) 32(1):40–4.
12. Hettema J, Steele J, Miller WR. Motivational interviewing. Annu Rev Clin Psychol. (2005) 1:91–111. doi: 10.1146/annurev.clinpsy.1.102803.143833
13. Miller WR. The evolution of motivational interviewing. Behav Cogn Psychother. (2023) 51(6):616–32. doi: 10.1017/S1352465822000431
14. Miller WR, Rollnick S. Ten things that motivational interviewing is not. Behav Cogn Psychother. (2009) 37(2):129–40. doi: 10.1017/S1352465809005128
15. Gagneur A, Gutnick D, Berthiaume P, Diana A, Rollnick S, Saha P. From vaccine hesitancy to vaccine motivation: a motivational interviewing based approach to vaccine counselling. Hum Vaccin Immunother. (2024) 20(1):2391625. doi: 10.1080/21645515.2024.2391625
16. Huang X, Xu N, Wang Y, Sun Y, Guo A. The effects of motivational interviewing on hypertension management: a systematic review and meta-analysis. Patient Educ Couns. (2023) 112:107760. doi: 10.1016/j.pec.2023.107760
17. Steffen PLS, Mendonca CS, Meyer E, Faustino-Silva DD. Motivational interviewing in the management of type 2 diabetes mellitus and arterial hypertension in primary health care: an RCT. Am J Prev Med. (2021) 60(5):e203–12. doi: 10.1016/j.amepre.2020.12.015
18. Mohan A, Majd Z, Johnson ML, Essien EJ, Barner J, Serna O, et al. A motivational interviewing intervention to improve adherence to ACEIs/ARBs among nonadherent older adults with comorbid hypertension and diabetes. Drugs Aging. (2023) 40(4):377–90. doi: 10.1007/s40266-023-01008-6
19. Zabolypour S, Alishapour M, Behnammoghadam M, Abbasi Larki R, Zoladl M. A comparison of the effects of teach-back and motivational interviewing on the adherence to medical regimen in patients with hypertension. Patient Prefer Adherence. (2020) 14:401–10. doi: 10.2147/PPA.S231716
20. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. J Clin Epidemiol. (2021) 134:178–89. doi: 10.1016/j.jclinepi.2021.03.001
21. Sterne JAC, Savovic J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. Rob 2: a revised tool for assessing risk of bias in randomised trials. Br Med J. (2019) 366:l4898. doi: 10.1136/bmj.l4898
22. Boutin-Foster C, Offidani E, Kanna B, Ogedegbe G, Ravenell J, Scott E, et al. Results from the trial using motivational interviewing, positive affect, and self-affirmation in African Americans with hypertension (TRIUMPH). Ethn Dis. (2016) 26(1):51–60. doi: 10.18865/ed.26.1.51
23. Cao X, Wang L, Shao J. Effect of motivational interview intervention on movement changes in elderly patients with hypertension. Chin J Nurs. (2012) 47(1):20–2.
24. Hardcastle SJ, Taylor AH, Bailey MP, Harley RA, Hagger MS. Effectiveness of a motivational interviewing intervention on weight loss, physical activity and cardiovascular disease risk factors: a randomised controlled trial with a 12-month post-intervention follow-up. Int J Behav Nutr Phys Act. (2013) 10:40. doi: 10.1186/1479-5868-10-40
25. Hedegaard U, Kjeldsen LJ, Pottegard A, Henriksen JE, Lambrechtsen J, Hangaard J, et al. Improving medication adherence in patients with hypertension: a randomized trial. Am J Med. (2015) 128(12):1351–61. doi: 10.1016/j.amjmed.2015.08.011
26. Huang H, Pan Z, Cao Y. Effect of motivational interview on middle-aged and elderly female patients with hypertension in community. Chin Mater Child Health. (2021) 36(9):3–6.
27. Landry A, Madson M, Thomson J, Zoellner J, Connell C, Yadrick K. A randomized trial using motivational interviewing for maintenance of blood pressure improvements in a community-engaged lifestyle intervention: HUB city steps. Health Educ Res. (2015) 30(6):910–22. doi: 10.1093/her/cyv058
28. Lei S, Yang L, Hu J. Motivational interview on self-management behavior of elderly patients with hypertension in community. Wisdom Health. (2022) 8(10):172–5.
29. Lei Z, Zhang H, Gao Z. Effect of motivational interview intervention on self-management level of elderly patients with hypertension in community. J Xinxiang Med Coll. (2016) 33(6):541–3.
30. Liang R. Analysis of the effect of motivational interview nursing on hypertension and self-efficacy score. Prevent Treat Cardiovasc Dis. (2022) 32(9):26–8.
31. Ma C, Zhou Y, Zhou W, Huang C. Evaluation of the effect of motivational interviewing counselling on hypertension care. Patient Educ Couns. (2014) 95(2):231–7. doi: 10.1016/j.pec.2014.01.011
32. Murphy AW, Cupples ME, Smith SM, Byrne M, Byrne MC, Newell J, et al. Effect of tailored practice and patient care plans on secondary prevention of heart disease in general practice: cluster randomised controlled trial. Br Med J. (2009) 339:b4220. doi: 10.1136/bmj.b4220
33. Ogedegbe G, Chaplin W, Schoenthaler A, Statman D, Berger D, Richardson T, et al. A practice-based trial of motivational interviewing and adherence in hypertensive African Americans. Am J Hypertens. (2008) 21(10):1137–43. doi: 10.1038/ajh.2008.240
34. Shao Y, Chen Y, Lu H. Effect of motivational interview on blood pressure in elderly patients with hypertension by diet and exercise. Zhejiang J Integr Trad Chin West Med. (2014) 24(11):1032–5.
35. Zhang H, Zhang H, Tang S. Application of motivational interview intervention in elderly patients with hypertension in community. Mod Prevent Med. (2015) 42(18):3332–5.
36. Zhao G. Application of motivational interview in the education of elderly patients with hypertension. Gen Pract Nurs. (2013) 11(31):2963–4.
37. Zuo J, Gu L, Chen Q. Effects of motivational interviews combined with social media tools on quality of life in patients with hypertension. J Nurs Peoples Liberation Army. (2017) 34(10):38–41.
38. Mogi M, Hoshide S, Kario K. Consider hypertension risk factors once again. Hypertens Res. (2024) 47(6):1443–4. doi: 10.1038/s41440-024-01680-0
39. Bakris GL, Weber MA. Overview of the evolution of hypertension: from ancient Chinese emperors to today. Hypertension. (2024) 81(4):717–26. doi: 10.1161/HYPERTENSIONAHA.124.21953
40. Berlowitz DR. Should primary care physicians be managing hypertension? Am J Hypertens. (2024) 37(4):266–7. doi: 10.1093/ajh/hpad119
41. Mitro SD, Wise LA, Waetjen LE, Lee C, Zaritsky E, Harlow SD, et al. Hypertension, cardiovascular risk factors, and uterine fibroid diagnosis in midlife. JAMA Netw Open. (2024) 7(4):e246832. doi: 10.1001/jamanetworkopen.2024.6832
42. Mohan A, Vadhariya A, Majd Z, Esse TW, Serna O, Abughosh SM. Impact of a motivational interviewing intervention targeting statins on adherence to concurrent hypertension or diabetes medications. Patient Educ Couns. (2021) 104(7):1756–64. doi: 10.1016/j.pec.2020.12.009
43. Roldan PC, Ho GY, Ho PM. Updates to adherence to hypertension medications. Curr Hypertens Rep. (2018) 20(4):34. doi: 10.1007/s11906-018-0830-x
44. Boutin-Foster C, Scott E, Rodriguez A, Ramos R, Kanna B, Michelen W, et al. The trial using motivational interviewing and positive affect and self-affirmation in African-Americans with hypertension (TRIUMPH): from theory to clinical trial implementation. Contemp Clin Trials. (2013) 35(1):8–14. doi: 10.1016/j.cct.2013.02.002
45. Khadoura KJ, Shakibazadeh E, Mansournia MA, Aljeesh Y, Fotouhi A. Effectiveness of motivational interviewing on medication adherence among Palestinian hypertensive patients: a clustered randomized controlled trial. Eur J Cardiovasc Nurs. (2021) 20(5):411–20. doi: 10.1093/eurjcn/zvaa015
46. Huang N, Zhou Y, Li L. A qualitative study on the motivation of blood glucose management behavior change in pregnant women with gestational diabetes mellitus. Chin J Nurs. (2022) 57(4):6–9.
47. Chen F, Cheng S, Li Y. Analysis of the effect of motivation interview combined with mindfulness decompression training on postoperative rehabilitation and nursing satisfaction of breast cancer patients with hypertension. Chin Med. (2023) 42(33):142–6.
48. Wang J, Wang L, Zhang Y. Investigation on compliance of prevention and treatment and blood pressure control in patients with essential hypertension. S China Prevent Med. (2022) 48(12):1451–4.
49. Sawyer AT, Wheeler J, Jennelle P, Pepe J. Robinson PS: a randomized controlled trial of a motivational interviewing intervention to improve whole-person lifestyle. J Prim Care Community Health. (2020) 11:2150132720922714. doi: 10.1177/2150132720922714
50. Cook PF, Schmiege SJ, Mansberger SL, Sheppler C, Kammer J, Fitzgerald T, et al. Motivational interviewing or reminders for glaucoma medication adherence: results of a multi-site randomised controlled trial. Psychol Health. (2017) 32(2):145–65. doi: 10.1080/08870446.2016.1244537
51. Majd Z, Mohan A, Johnson ML, Essien EJ, Barner JC, Serna O, et al. Patient-Reported barriers to adherence among ACEI/ARB users from a motivational interviewing telephonic intervention. Patient Prefer Adherence. (2022) 16:2739–48. doi: 10.2147/PPA.S360461
52. Izeogu C, Kalinowski J, Schoenthaler A. Strategies to improve adherence to anti-hypertensive medications: a narrative review. Curr Hypertens Rep. (2020) 22(12):105. doi: 10.1007/s11906-020-01115-4
53. Silveira LCJ, Aliti GB, Da Silva EM, Pimentel RP, Gus M, Rabelo-Silva ER. Effect of motivational interviewing in hypertensive patients (MIdNIgHT): study protocol for a randomized controlled trial. Trials. (2019) 20(1):414. doi: 10.1186/s13063-019-3486-1
Keywords: motivational interviewing, hypertension, care, treatment, management
Citation: Xu J, Gu X, Gu J, Zhao L, Li M and Hong C (2025) Motivational interviewing intervention for the management of hypertension: a meta-analysis. Front. Cardiovasc. Med. 11:1457039. doi: 10.3389/fcvm.2024.1457039
Received: 30 June 2024; Accepted: 26 December 2024;
Published: 20 January 2025.
Edited by:
Izabella Uchmanowicz, Wroclaw Medical Universiy, PolandReviewed by:
Daniel Demetrio Faustino-Silva, Conceição Hospital Group, BrazilAna Luisa Brandão De Carvalho Lira, Federal University of Ceara, Brazil
Copyright: © 2025 Xu, Gu, Gu, Zhao, Li and Hong. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mianxian Li, dGJ6cGg1NUAxNjMuY29t; Cheng Hong, ZmJ4eDIxQHNpbmEuY29t
†These authors have contributed equally to this work
 Ju Xu1,†
Ju Xu1,† Cheng Hong
Cheng Hong