- 1Department of Cardiothoracic Surgery, Harefield Hospital, Guy’s and St Thomas’ NHS Foundation Trust, London, United Kingdom
- 2Department of Cardiothoracic and Vascular Surgery, Jay Prabha Medanta Super Specialty Hospital, Patna, India
- 3Faculty of Medicine, King Abdulaziz University, Jeddah, Saudi Arabia
- 4Department of Cardiothoracic Surgery, Royal Brompton Hospital, Guy’s and St Thomas’ NHS Foundation Trust, London, United Kingdom
- 5Department of Radiology, Shaukat Khanum Memorial Cancer Hospital, Lahore, Pakistan
- 6Department of Surgery, Khyber Medical College, Peshawar, Pakistan
- 7Lister Hospital, Stevenage, United Kingdom
- 8Department of Cardiology, King Edward Medical University, Lahore, Pakistan
- 9Hamad Medical Corporation, Doha, Qatar
- 10Department of Cardiothoracic Surgery, Rush University Medical Center, Chicago, IL, United States
- 11Department of Cardiac Surgery, Yale University School of Medicine, New Haven, CT, United States
- 12Department of Clinical Biochemistry, King’s College Hospital NHS Foundation Trust, London, United Kingdom
- 13Faculty of Life Sciences & Medicine, King’s College London, London, United Kingdom
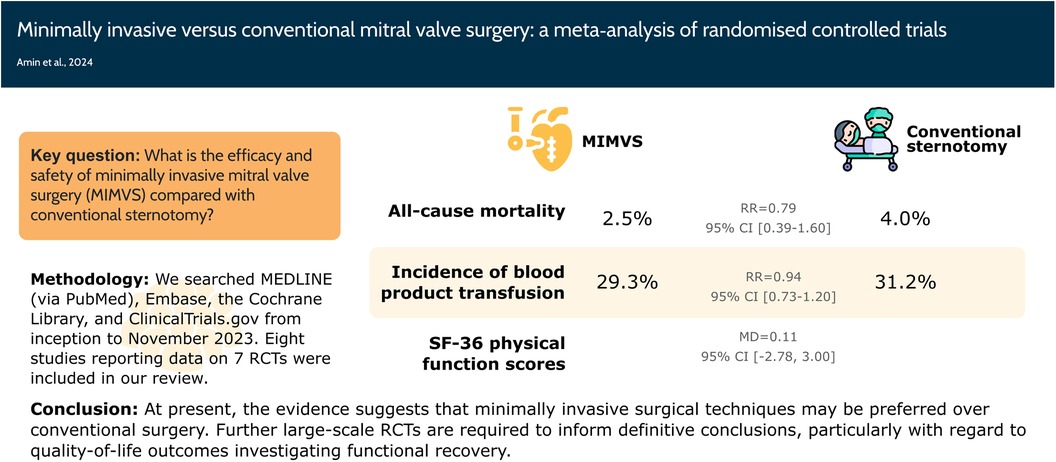
Objective: The evidence underlying the efficacy and safety of minimally invasive mitral valve surgery (MIMVS) is inconclusive. We conducted a meta-analysis to evaluate whether MIMVS improves clinical outcomes compared with conventional sternotomy.
Methods: We searched MEDLINE (via PubMed), Embase, the Cochrane Library, and ClinicalTrials.gov from inception to January 2024 for all randomised controlled trials (RCTs), comparing MIMVS with conventional mitral valve surgery. RevMan 5.4 was used to analyse the data with risk ratio (RR) and mean difference (MD) as the effect measures.
Results: Eight studies reporting data on 7 RCTs were included in our review. There was no significant difference in all-cause mortality, the number of patients requiring blood product transfusion, and the change from baseline in the SF-36 physical function scores between the MIMVS and conventional sternotomy groups. MIMVS reduced the length of hospital stay (MD −2.02 days, 95% CI: −3.66, −0.39) but did not affect the length of ICU stay, re-operation for bleeding, and the incidence of renal injury, wound infection, neurological events, and postoperative moderate or severe mitral regurgitation. MIMVS was associated with a trend toward lower postoperative pain scores (MD −1.06; 95% CI: −3.96 to 0.75).
Conclusions: MIMVS reduced the number of days spent in the hospital and showed a trend toward lower postoperative pain scores, but it did not decrease the risk of all-cause mortality or the number of patients needing blood product transfusions. Further large-scale RCTs are required to inform definitive conclusions, particularly with regard to quality-of-life outcomes investigating functional recovery.
Systematic Review Registration: PROSPERO (CRD42023482122).
Introduction
First pioneered in the 1990s (1, 2), minimally invasive mitral valve surgery (MIMVS) is a dynamic approach that continues to garner broader acceptance in modern cardiac surgery (3–5). However, it is limited to highly specialised centres across the world that employ a multitude of surgical techniques to minimise operative trauma, including right mini-thoracotomy, partial sternotomy, video-assisted port-access surgery, and even robotic approaches (6–11). Surgeons undergo a variably protracted learning curve to achieve the required competencies despite good mentoring and high-fidelity simulation training (12–14).
Compared with conventional sternotomy, the reported benefits of MIMVS include shorter length of hospital stay, less post-operative pain, less incidence of deep wound infections, use of fewer blood products, and better wound cosmesis (15–18). However, these benefits need to be carefully weighed against a prolonged intraoperative period with increased cross-clamp time and cardiopulmonary bypass time and a reportedly elevated risk of adverse effects such as transient ischaemic attack (TIA), stroke, groin infections, femoral artery injury, and pseudoaneurysm (15, 19, 20).
Despite its ever-growing popularity, the evidence underlying the efficacy and safety of MIMVS is indeterminate as previous systematic reviews on the subject have included non-randomized observational and propensity score matched studies, thus carrying a risk of confounding bias and poor internal validity (18, 21–26). Furthermore, the recent availability of data from a large randomised controlled trial (RCT) has strengthened the evidence base, thus necessitating a systematic re-appraisal of all available data (27).
Therefore, we aimed to conduct a meta-analysis of RCTs to deliberate superior evidence in evaluating whether MIMVS improves clinical outcomes compared with conventional sternotomy in adults requiring surgical intervention for mitral valve disease.
Methods
This review has been registered in PROSPERO (CRD42023482122). The procedures for conducting this review adhered to the guidelines outlined in the Cochrane Handbook for Systematic Reviews of Interventions (28). Furthermore, the study was reported following the recommendations of the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) statement (29).
Data sources & search strategy
We comprehensively searched MEDLINE (via PubMed), Embase (via Ovid), Cochrane Central Register of Controlled Trials (CENTRAL, via The Cochrane Library), and ClinicalTrials.gov using a search strategy consisting of relevant keywords and Medical Subject Headings (MeSH) from inception till January 2024. The detailed search strategy is presented in Supplementary Table S1. The search process involved no specific filters or limits. Additionally, we screened the reference lists of the included articles for other relevant studies. A partial search of Google Scholar was also conducted to retrieve any relevant grey literature.
Eligibility criteria
We included RCTs that compared MIMVS to conventional sternotomy in adults requiring surgery for mitral valve disease. We excluded studies that employed robotic surgery or enhancement, observational studies, quasi-randomized studies, and reviews.
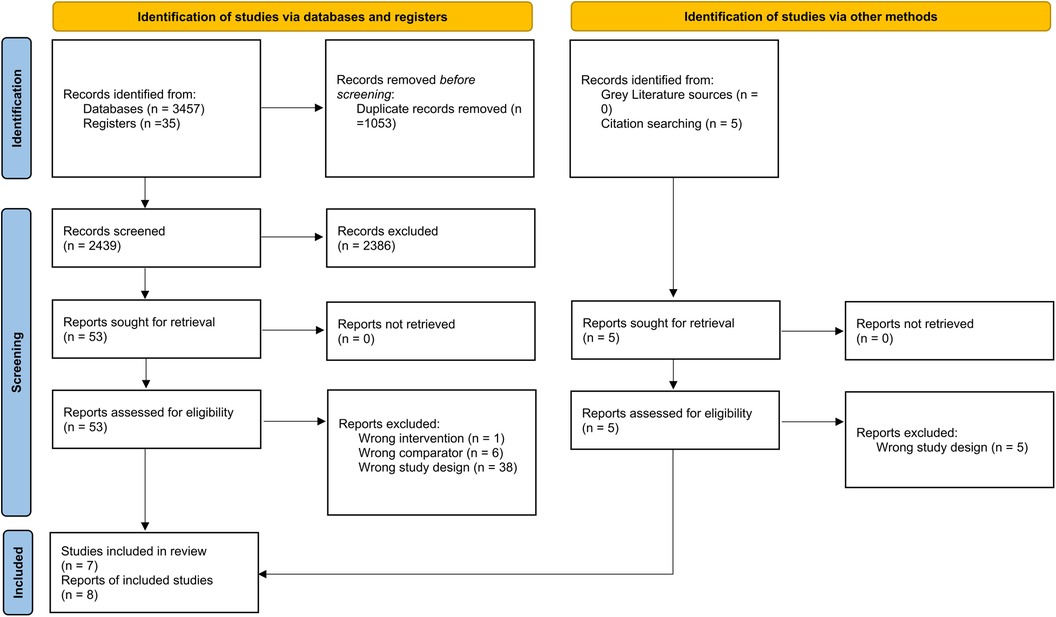
Study selection
All studies obtained from our online search were imported into Mendeley Desktop 1.19.8, and then duplicates were removed. Two authors independently screened the titles and abstracts, followed by the full texts. A third author was assigned to resolve any conflicts.
Data extraction
The following data were extracted into a pre-piloted Excel sheet: (1) summary of the included studies (study ID, location, sample size); (2) baseline characteristics of the patients; (3) outcome data of the outcomes. Our primary outcomes were all-cause mortality, number of patients requiring blood product transfusion, and change from baseline in the 36-Item Short Form Health Survey (SF-36) physical functioning percentage scores. Our secondary outcomes were the ICU length of stay, hospital length of stay, post-operative pain scores on the 3rd or 4th day, re-operation for bleeding, renal injury, wound infection, neurological events, and post-operative moderate or severe mitral regurgitation (MR). The extracted data were cross-checked, and any errors were rectified. If two or more reports of the same RCT were found, data from the report with longer follow-up was preferred.
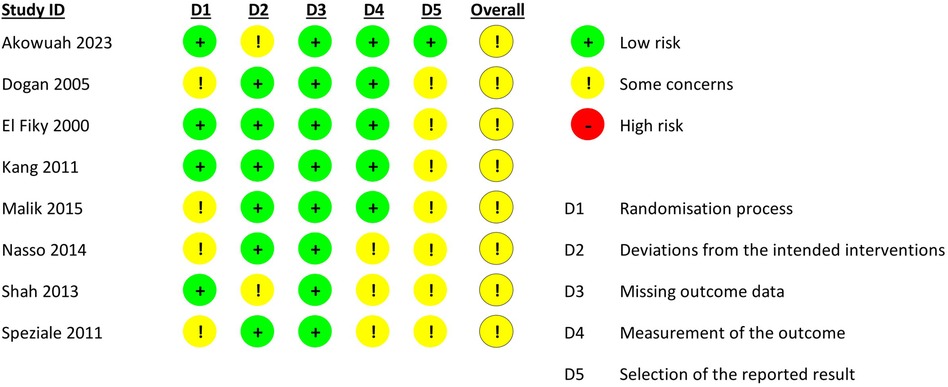
Risk of bias assessment
Two authors independently assessed the quality of the included studies using the revised Cochrane Risk of Bias tool (RoB 2.0). RoB 2.0 investigates the risk of bias according to five domains: (1) randomisation process; (2) deviations from intended interventions; (3) missing outcome data; (4) outcome measurement; and (5) selection of the reported result.
Statistical analysis
The meta-analysis was performed using the Review Manager (RevMan) software version 5.4. We used risk ratios (RRs) and mean differences (MDs) along with their corresponding 95% confidence intervals (CIs) to evaluate our outcomes. The random-effects model was employed to pool data using the Mantel-Haenszel approach for dichotomous outcomes and the Inverse Variance approach for continuous outcomes. Heterogeneity was assessed using the I2 and Chi-square tests; the Chi-square test determined substantial heterogeneity for an alpha level below 0.1, while the I2 test was interpreted according to the guidance presented in the Cochrane Handbook for Systematic Reviews of Intervention (28). We could not investigate publication bias as the number of included studies was less than 10.
Results
Study selection and characteristics
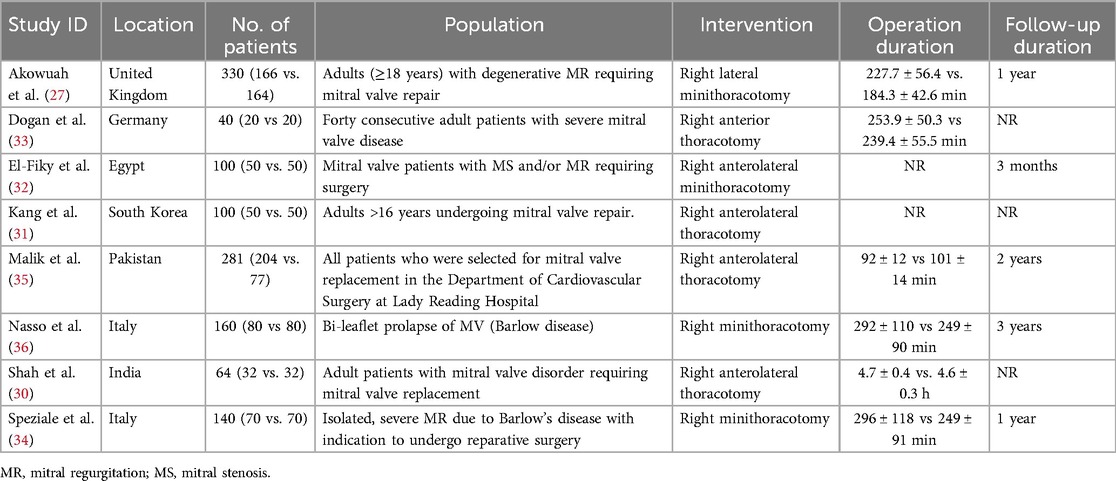
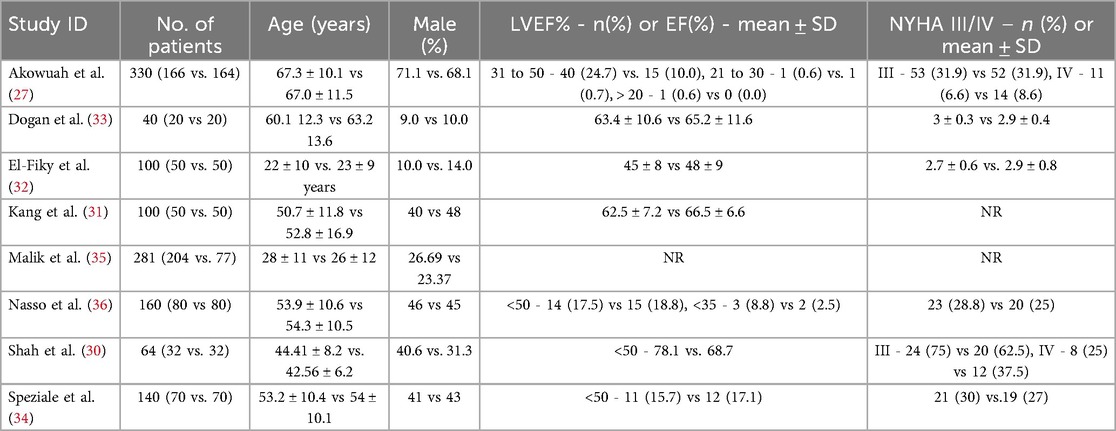
Our meta-analysis included eight reports providing data on 7 RCTs (Figure 1) (27, 30–36). Two reports of the same RCT were obtained, one reporting short- and mid-term results (34) and the other reporting long-term results at 3 years of follow-up (36). All were conducted in different countries, with sample sizes ranging from 40 to 330 patients. The duration of operation was higher in the MIMVS group. Table 1 shows the characteristics of the included RCTs in detail, and Table 2 shows the baseline characteristics of patients in these RCTs.
Risk of bias assessment
All trials had some concerns of bias, primarily due to the absence of a publicly available protocol and/or issues in the randomisation process or measurement of the outcome domain. Figure 2 illustrates the risk of bias assessment.
Results of the meta-analysis
Primary outcomes
There was no significant difference between the MIMVS and the conventional mitral valve surgery groups in the risk of all-cause mortality (RR 0.79; 95% CI: 0.39–1.60, I2 = 0%; Figure 3A) and the number of patients needing blood product transfusion (RR 0.94; 95% CI: 0.73–1.20, I2 = 0%, Figure 3B).
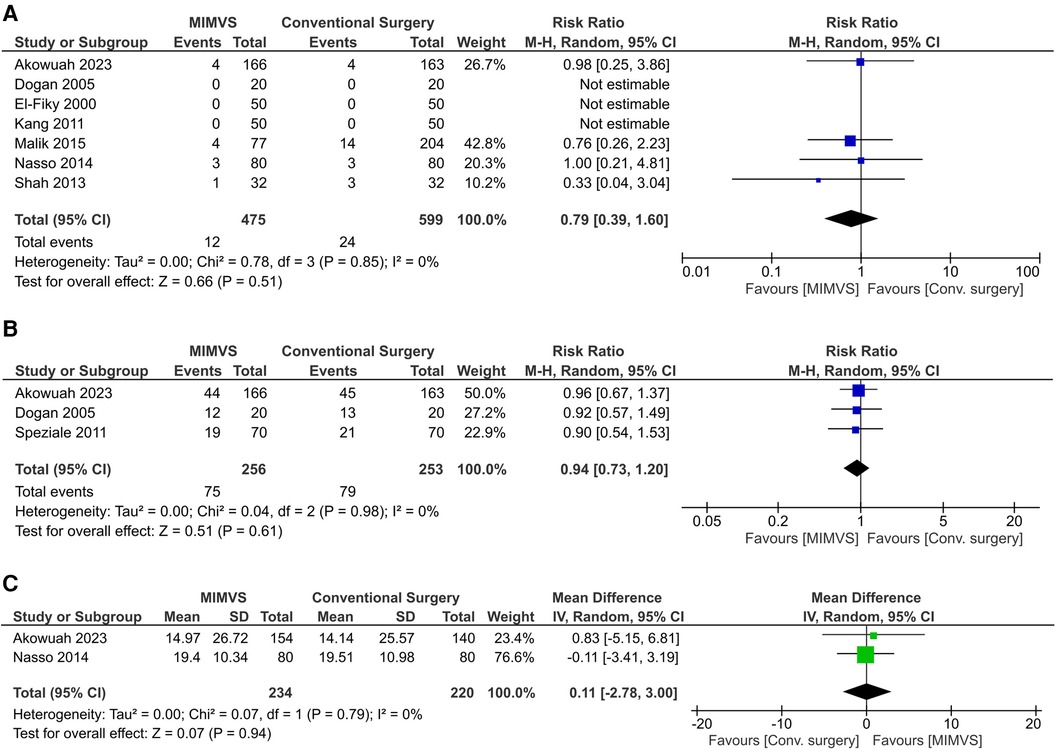
Figure 3. Effect of minimally invasive mitral valve surgery compared to conventional sternotomy on: A) all-cause mortality; B) the number of patients requiring blood product transfusion; and C) the change from baseline in the 36-item short form health survey (SF-36) physical function percentage scores.
MIMVS was not associated with statistically significant improvement in the SF-36 physical functioning percentage score from baseline (MD 0.11; 95% CI: −2.78 to 3.00, I2 = 0%; Figure 3C).
Secondary outcomes
MIMVS had no significant effect on the ICU length of stay (MD −0.87 days; 95% CI: −2.06 to 0.33 days, I2 = 99%; Supplementary Figure S1) but reduced the hospital length of stay (MD −2.02 days; 95% CI: −2.02 to −0.39 days, I2 = 95%; Supplementary Figure S2).
There was no significant difference between the MIMVS and conventional surgery groups in the number of patients who needed re-operation for bleeding (RR 0.52; 95% CI: 0.16–1.65, I2 = 12%; Supplementary Figure S3). There was a trend towards lower post-operative pain scores on the 3rd or 4th day with MIMVS (MD −1.06; 95% CI: −3.96 to 0.75, I2 = 98%; Supplementary Figure S4).
There were no significant differences between the two groups in the incidence of renal injury (RR 1.17; 95% CI: 0.44–3.11, I2 = 0%; Supplementary Figure S5), wound infection (RR 1.21; 95% CI: 0.63- 2.31, I2 = 0%; Supplementary Figure S6), neurological events (RR 0.99; 95% CI: 0.44–2.22, I2 = 0%; Supplementary Figure S7), and postoperative moderate or severe MR (RR 0.95; 95% CI: 0.46–1.97, I2 = 0%; Supplementary Figure S8).
Discussion
To the best of our knowledge, this is the most comprehensive systematic review and meta-analysis to date that evaluates minimally invasive techniques compared with conventional sternotomy for mitral valve surgery using data from RCTs only. Our analysis showed that the two procedures had similar all-cause mortality and blood product transfusion rates. Compared to conventional sternotomy, MIMVS did not improve physical functioning as assessed by SF-36. MIMVS reduced the length of hospital stay but did not affect the ICU length of stay, re-operation for bleeding, and the incidence of renal injury, wound infection, neurological events, and postoperative moderate or severe MR. There was a trend towards lower postoperative pain scores with MIMVS.
Our findings contrast with several prior reviews, which have demonstrated that MIMVS improves postoperative clinical outcomes, including mortality, need for blood transfusions, and/or renal failure (22, 25). Conversely, our meta-analysis reaffirms the findings of other recent systematic appraisals, which have shown similar outcomes with the two surgical techniques apart from a shorter hospital stay in the MIMVS group (23, 26). However, the past reviews suffered from many shortcomings, with the primary one being the reliance on data from primarily observational and single-armed studies, thus incurring a high risk of confounding bias. One previous meta-analysis focused on RCTs but provided low-quality evidence due to the availability of only a few small trials (37). There is a paucity of randomised controlled data, but the recently published UK Mini Mitral Trial, the largest trial on this topic to date (27), has made significant strides toward addressing this knowledge gap. A recent large meta-analysis included 8 RCTs in its analysis, but out of those, one was an observational study mistakenly classified as an RCT (38), and two were different reports of the same RCT (34, 36); the inclusion of multiple reports of a single RCT in a single analysis duplicates patient data and may lead to erroneous and skewed results (28). Our systematic review addresses many of the limitations of previous analyses by including only RCTs, data from one report of an RCT out of multiple ones in each analysis as recommended by the Cochrane guidelines, and data from the UK Mini Mitral Trial (27), which has not been collated in a systematic appraisal thus far. Consequently, our meta-analysis provides more reliable results and a clearer and more robust understanding of this topic.
One of the concerns about MIMVS has been a greater postoperative risk of stroke based on data from observational studies (18, 39, 40); however, we did not find an elevated rate of neurological events in our analysis, thus corroborating the results of the UK Mini Mitral Trial (27). Additionally, there was no increase in any of the other evaluated adverse events, including wound infection, renal injury, and postoperative MR, further allaying any safety and quality of repair concerns. MIMVS has reportedly been associated with aortic dissection; however, we could not assess this postoperative complication due to a scarcity of data. Future RCTs should also evaluate the occurrence of aortic dissection to provide conclusive proof.
The primary benefits of minimally invasive surgery are usually seen with faster functional recovery and lesser postoperative pain. However, surprisingly, very few studies and, subsequently, systematic reviews based on these studies have attempted to assess the quality-of-life outcome measures. In our review, we sought to address this issue and pool relevant data from RCTs. We found no improvement in physical functioning according to SF-36, but we did observe a trend toward lower pain scores in the MIMVS group. Given that data from only two trials was available for these outcomes, and the SF-36 is a generic health survey questionnaire not specific for any surgical technique, new large-scale RCTs focusing on quality of life and patient-reported outcomes assessed through specific tools might reveal the expected benefits of MIMVS.
The evidence from our meta-analysis, taken as a whole, suggests that MIMVS might be preferred over conventional sternotomy due to shorter hospital stays and a possible benefit in functional recovery. Nevertheless, the similar rates of blood transfusion and postoperative complications, such as wound infection, between the two approaches should be highlighted because these have historically been associated with sternotomy access. Therefore, our findings should be interpreted cautiously, and the need for further large-scale RCTs comparing these two techniques should be emphasized before drawing any definitive conclusions.
Some limitations of our meta-analysis need to be stated. Despite the robust analysis, inherent biases were observed across studies, particularly regarding the lack of a registered protocol. Most trials had small sample sizes; therefore, our analysis is likely underpowered for some outcomes, hindering the ability to draw definitive conclusions, especially for the important quality-of-life measures such as the SF-36 physical functioning and postoperative pain scores. Moreover, differences between the trials regarding surgical procedures and postoperative care protocols contribute to heterogeneity. This is an aggregate-level meta-analysis, and we did not have access to individual patient data, limiting our ability to explore any potential effect modifiers. Finally, the short follow-up times of the RCTs preclude evaluation of the longer-term surgical success of the two approaches.
Conclusions
In our meta-analysis, MIMVS and conventional sternotomy had similar mortality and blood product transfusion rates. MIMVS was associated with a shorter hospital stay and did not increase the risk of any postoperative complications, including re-operation for bleeding and the incidence of renal injury, wound infection, neurological events, and postoperative moderate or severe MR. MIMVS did not improve SF-36 physical functioning scores but was associated with a trend toward lower postoperative pain scores. At present, the evidence suggests that minimally invasive surgical techniques may be preferred over conventional surgery due to their potential short-term benefits for patients and lack of significant drawbacks from a clinical perspective; however, further large-scale RCTs, particularly investigating meaningful patient-reported and quality-of-life outcomes are needed to consolidate the evidence base and provide definitive conclusions.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Author contributions
AA: Conceptualization, Data curation, Formal Analysis, Investigation, Methodology, Software, Writing – original draft. RK: Conceptualization, Data curation, Formal Analysis, Investigation, Methodology, Software, Writing – original draft. SM: Investigation, Methodology, Writing – original draft, Data curation. AA: Data curation, Formal Analysis, Methodology, Writing – original draft. AO: Formal Analysis, Investigation, Methodology, Writing – original draft. MK: Investigation, Methodology, Resources, Writing – original draft. SL: Investigation, Validation, Visualization, Writing – review & editing. ZD: Data curation, Formal Analysis, Investigation, Methodology, Writing – original draft. PA: Data curation, Writing – review & editing. HC: Conceptualization, Data curation, Formal Analysis, Investigation, Methodology, Project administration, Resources, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. AN: Project administration, Resources, Supervision, Writing – review & editing. AK: Methodology, Resources, Supervision, Writing – review & editing. AH: Investigation, Resources, Supervision, Writing – review & editing. SB: Investigation, Methodology, Project administration, Resources, Supervision, Validation, Visualization, Writing – review & editing. RV: Supervision, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcvm.2024.1437524/full#supplementary-material
References
1. Navia JL, Cosgrove DM. Minimally invasive mitral valve operations. Ann Thorac Surg. (1996) 62:1542–4. doi: 10.1016/0003-4975(96)00779-5
2. Cohn LH, Adams DH, Couper GS, Bichell DP, Rosborough DM, Sears SP, et al. Minimally invasive cardiac valve surgery improves patient satisfaction while reducing costs of cardiac valve replacement and repair. Ann Surg. (1997) 226:421–6; discussion 427–428. doi: 10.1097/00000658-199710000-00003
3. Falk V, Cheng DCH, Martin J, Diegeler A, Folliguet TA, Nifong LW, et al. Minimally invasive versus open mitral valve surgery: a consensus statement of the international society of minimally invasive coronary surgery (ISMICS) 2010. Innov Phila Pa. (2011) 6:66–76. doi: 10.1097/IMI.0b013e318216be5c
4. Ritwick B, Chaudhuri K, Crouch G, Edwards JRM, Worthington M, Stuklis RG. Minimally invasive mitral valve procedures: the current state. Minim Invasive Surg. (2013) 2013:679276. doi: 10.1155/2013/679276
5. Lucà F, van Garsse L, Rao CM, Parise O, La Meir M, Puntrello C, et al. Minimally invasive mitral valve surgery: a systematic review. Minim Invasive Surg. (2013) 2013:179569. doi: 10.1155/2013/179569
6. Schwartz DS, Ribakove GH, Grossi EA, Buttenheim PM, Schwartz JD, Applebaum RM, et al. Minimally invasive mitral valve replacement: port-access technique, feasibility, and myocardial functional preservation. J Thorac Cardiovasc Surg. (1997) 113:1022–30; discussion 1030–1031. doi: 10.1016/S0022-5223(97)70287-3
7. Mohr FW, Falk V, Diegeler A, Walther T, van Son JA, Autschbach R. Minimally invasive port-access mitral valve surgery. J Thorac Cardiovasc Surg. (1998) 115:567–74; discussion 574–576. doi: 10.1016/S0022-5223(98)70320-4
8. Mishra YK, Malhotra R, Mehta Y, Sharma KK, Kasliwal RR, Trehan N. Minimally invasive mitral valve surgery through right anterolateral minithoracotomy. Ann Thorac Surg. (1999) 68:1520–4. doi: 10.1016/S0003-4975(99)00963-7
9. Greelish JP, Cohn LH, Leacche M, Mitchell M, Karavas A, Fox J, et al. Minimally invasive mitral valve repair suggests earlier operations for mitral valve disease. J Thorac Cardiovasc Surg. (2003) 126:365–71; discussion 371–373. doi: 10.1016/s0022-5223(03)00078-3
10. Angouras DC, Michler RE. An alternative surgical approach to facilitate minimally invasive mitral valve surgery. Ann Thorac Surg. (2002) 73:673–4. doi: 10.1016/S0003-4975(01)03175-7
11. Chen Q, Yu L-L, Zhang Q-L, Cao H, Chen L-W, Huang Z-Y. Minimally invasive video-assisted mitral valve replacement with a right chest small incision in patients aged over 65 years. Braz J Cardiovasc Surg. (2019) 34:428–35. doi: 10.21470/1678-9741-2018-0409
12. Holzhey DM, Seeburger J, Misfeld M, Borger MA, Mohr FW. Learning minimally invasive mitral valve surgery: a cumulative sum sequential probability analysis of 3895 operations from a single high-volume center. Circulation. (2013) 128:483–91. doi: 10.1161/CIRCULATIONAHA.112.001402
13. Sardari Nia P, Daemen JHT, Maessen JG. Development of a high-fidelity minimally invasive mitral valve surgery simulator. J Thorac Cardiovasc Surg. (2019) 157:1567–74. doi: 10.1016/j.jtcvs.2018.09.014
14. Aerts L, Sardari Nia P. Mastering the learning curve of endoscopic mitral valve surgery. Front Cardiovasc Med. (2023) 10:1162330. doi: 10.3389/fcvm.2023.1162330
15. Aklog L, Adams DH, Couper GS, Gobezie R, Sears S, Cohn LH. Techniques and results of direct-access minimally invasive mitral valve surgery: a paradigm for the future. J Thorac Cardiovasc Surg. (1998) 116:705–15. doi: 10.1016/S0022-5223(98)00448-6
16. Gillinov AM, Banbury MK, Cosgrove DM. Hemisternotomy approach for aortic and mitral valve surgery. J Card Surg. (2000) 15:15–20. doi: 10.1111/j.1540-8191.2000.tb00440.x
17. Svensson LG, Atik FA, Cosgrove DM, Blackstone EH, Rajeswaran J, Krishnaswamy G, et al. Minimally invasive versus conventional mitral valve surgery: a propensity-matched comparison. J Thorac Cardiovasc Surg. (2010) 139:926–32.e1–2. doi: 10.1016/j.jtcvs.2009.09.038
18. Cheng DCH, Martin J, Lal A, Diegeler A, Folliguet TA, Nifong LW, et al. Minimally invasive versus conventional open mitral valve surgery: a meta-analysis and systematic review. Innov Phila Pa. (2011) 6:84–103. doi: 10.1097/IMI.0b013e3182167feb
19. Chitwood WR, Wixon CL, Elbeery JR, Moran JF, Chapman WH, Lust RM. Video-assisted minimally invasive mitral valve surgery. J Thorac Cardiovasc Surg. (1997) 114:773–80; discussion 780–782. doi: 10.1016/S0022-5223(97)70081-3
20. Chaney MA, Durazo-Arvizu RA, Fluder EM, Sawicki KJ, Nikolov MP, Blakeman BP, et al. Port-access minimally invasive cardiac surgery increases surgical complexity, increases operating room time, and facilitates early postoperative hospital discharge. Anesthesiology. (2000) 92:1637–45. doi: 10.1097/00000542-200006000-00022
21. Cao C, Gupta S, Chandrakumar D, Nienaber TA, Indraratna P, Ang SC, et al. A meta-analysis of minimally invasive versus conventional mitral valve repair for patients with degenerative mitral disease. Ann Cardiothorac Surg. (2013) 2:69303–703. doi: 10.3978/j.issn.2225-319X.2013.11.08
22. Sündermann SH, Sromicki J, Rodriguez Cetina Biefer H, Seifert B, Holubec T, Falk V, et al. Mitral valve surgery: right lateral minithoracotomy or sternotomy? A systematic review and meta-analysis. J Thorac Cardiovasc Surg. (2014) 148:1989–95.e4. doi: 10.1016/j.jtcvs.2014.01.046
23. Eqbal AJ, Gupta S, Basha A, Qiu Y, Wu N, Rega F, et al. Minimally invasive mitral valve surgery versus conventional sternotomy mitral valve surgery: a systematic review and meta-analysis of 119 studies. J Card Surg. (2022) 37:1319–27. doi: 10.1111/jocs.16314
24. Williams ML, Eranki A, Mamo A, Wilson-Smith A, Hwang B, Sugunesegran R, et al. Systematic review and meta-analysis of mid-term survival, reoperation, and recurrent mitral regurgitation for robotic-assisted mitral valve repair. Ann Cardiothorac Surg. (2022) 11:553–63. doi: 10.21037/acs-2022-rmvs-22
25. Al Shamry A, Jegaden M, Ashafy S, Eker A, Jegaden O. Minithoracotomy versus sternotomy in mitral valve surgery: meta-analysis from recent matched and randomized studies. J Cardiothorac Surg. (2023) 18:101. doi: 10.1186/s13019-023-02229-x
26. Moscarelli M, Fattouch K, Gaudino M, Nasso G, Paparella D, Punjabi P, et al. Minimal access versus sternotomy for Complex mitral valve repair: a meta-analysis. Ann Thorac Surg. (2020) 109:737–44. doi: 10.1016/j.athoracsur.2019.07.034
27. Akowuah EF, Maier RH, Hancock HC, Kharatikoopaei E, Vale L, Fernandez-Garcia C, et al. Minithoracotomy vs conventional sternotomy for mitral valve repair: a randomized clinical trial. JAMA. (2023) 329:1957–66. doi: 10.1001/jama.2023.7800
28. Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al. Cochrane Handbook for Systematic Reviews of Interventions. 2nd ed. Hoboken, NJ: Wiley Blackwell (2019). doi: 10.1002/9781119536604
29. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Br Med J. (2021) 372:n71–n71. doi: 10.1136/bmj.n71
30. Shah ZA, Ahangar AG, Ganie FA, Wani ML, Lone H, Wani NUD, et al. Comparison of right anterolateral thorocotomy with standard median steronotomy for mitral valve replacement. Int Cardiovasc Res J. (2013) 7:15–20. Available online at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3987419/24757613
31. Kang W-S, Yoon T-G, Kim T-Y, Kim S-H. Comparison of the PaO2/FiO2 ratio in sternotomy vs. thoracotomy in mitral valve repair: a randomised controlled trial. Eur J Anaesthesiol EJA. (2011) 28. doi: 10.1097/EJA.0b013e32834ad993
32. El-Fiky MM, El-Sayegh T, El-Beishry AS, Abdul Aziz M, Aboul Enein H, Waheid S, et al. Limited right anterolateral thoracotomy for mitral valve surgery. Eur J Cardiothorac Surg. (2000) 17:710–3. doi: 10.1016/S1010-7940(00)00429-2
33. Dogan S, Aybek T, Risteski PS, Detho F, Rapp A, Wimmer-Greinecker G, et al. Minimally invasive port access versus conventional mitral valve surgery: prospective randomized study. Ann Thorac Surg. (2005) 79:492–8. doi: 10.1016/j.athoracsur.2004.08.066
34. Speziale G, Nasso G, Esposito G, Conte M, Greco E, Fattouch K, et al. Results of mitral valve repair for barlow disease (bileaflet prolapse) via right minithoracotomy versus conventional median sternotomy: a randomized trial. J Thorac Cardiovasc Surg. (2011) 142:77–83. doi: 10.1016/j.jtcvs.2010.08.033
35. Malik A, Asghar M, Laiq N, Shah SMA, Khan RA, Farman MT. Standard median sternotomy versus right anterolateral thoracotomy for mitral valve replacement. J Med Sci. (2015) 23:42–5. Available online at: https://jmedsci.com/index.php/Jmedsci/article/view/293 (Accessed November 3, 2023).
36. Nasso G, Bonifazi R, Romano V, Bartolomucci F, Rosano G, Massari F, et al. Three-year results of repaired barlow mitral valves via right minithoracotomy versus median sternotomy in a randomized trial. Cardiology. (2014) 128:97–105. doi: 10.1159/000357263
37. Al Otaibi A, Gupta S, Belley-Cote EP, Alsagheir A, Spence J, Parry D, et al. Mini-thoracotomy vs. conventional sternotomy mitral valve surgery: a systematic review and meta-analysis. J Cardiovasc Surg (Torino). (2017) 58:489–96. doi: 10.23736/S0021-9509.16.09603-8
38. El Ashkar AM, Khallaf AN. Video-assisted minimally invasive mitral valve surgery: early experience. J Egypt Soc Cardio-Thorac Surg. (2016) 24:223–7. doi: 10.1016/j.jescts.2016.08.005
39. Gammie JS, Zhao Y, Peterson ED, O’Brien SM, Rankin JS, Griffith BP. J. Maxwell chamberlain memorial paper for adult cardiac surgery. Less-invasive mitral valve operations: trends and outcomes from the Society of Thoracic Surgeons adult cardiac surgery database. Ann Thorac Surg. (2010) 90:1401–8, 1410.e1; discussion 1408–1410. doi: 10.1016/j.athoracsur.2010.05.055
Keywords: minimally invasive, minithoracotomy, sternotomy, mitral valve surgery, MIMVS
Citation: Amin A, Kumar R, Mokhtassi SS, Alassiri AK, Odaman A, Khan MAR, Lakshmana S, Din ZU, Acharya P, Cheema HA, Nashwan AJ, Khan AA, Hussain A, Bhudia S and Vincent RP (2024) Minimally invasive vs. conventional mitral valve surgery: a meta-analysis of randomised controlled trials. Front. Cardiovasc. Med. 11:1437524. doi: 10.3389/fcvm.2024.1437524
Received: 23 May 2024; Accepted: 23 July 2024;
Published: 12 August 2024.
Edited by:
Enyi Shi, China Medical University, ChinaReviewed by:
Michael Hofmann, University of Zurich, SwitzerlandMassimo Baudo, Lankenau Institute for Medical Research, United States
© 2024 Amin, Kumar, Mokhtassi, Alassiri, Odaman, Khan, Lakshmana, Din, Acharya, Cheema, Nashwan, Khan, Hussain, Bhudia and Vincent. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Royce P. Vincent, cm95Y2UudmluY2VudEBuaHMubmV0; Huzaifa Ahmad Cheema, aHV6YWlmYWFobWFkY2hlZW1hQGdtYWlsLmNvbQ==
 Aamir Amin
Aamir Amin Rajanikant Kumar
Rajanikant Kumar Shiva Seyed Mokhtassi1
Shiva Seyed Mokhtassi1 Abdullah K. Alassiri
Abdullah K. Alassiri Shashi Lakshmana
Shashi Lakshmana Zahir Ud Din
Zahir Ud Din Huzaifa Ahmad Cheema
Huzaifa Ahmad Cheema Abdulqadir J. Nashwan
Abdulqadir J. Nashwan Arsalan Ali Khan
Arsalan Ali Khan Sunil Bhudia
Sunil Bhudia Royce P. Vincent
Royce P. Vincent