- Department of Anesthesiology, North Jiangsu people's Hospital Affiliated to Yangzhou University, Yangzhou, Jiangsu, China
Background: To identify the risk factors for postoperative delirium (POD) after cardiac surgery in frail elderly patients and develop a receiver operating characteristic (ROC) prediction model to confirm the effectiveness.
Methods: This was a prospective observational study, patients were assessed preoperatively according to the frailty index (FI) scale. Cerebral (SctO2) was assessed at different time points using near-infrared spectroscopy (NIRS). On the basis of the occurrence of POD within 7 days after surgery, patients were divided into POD and non-POD groups. Risk factors were analyzed using logistic regression analysis, while their predictive values were evaluated using the receiver operating characteristic curve analysis.
Results: POD was significantly associated with frailty, lower preoperative MMSE scores, hyperlipidemia, diabetes, cerebrovascular disease, lower hemoglobin level, lower albumin level, longer operation time, longer CPB time, lower SctO2 at T5, and lower SctO2baseline (P < 0.05). SrtO2 and SmtO2 did not differ significantly between groups. FI, preoperative MMSE score, and operation time as independent risk factors (P < 0.05). Significant predictive value was demonstrated in all 3 variables (P < 0.001; respectively). Among them, high sensitivity and specificity were observed with the FI (cut-off value 0.27, sensitivity 75%, specificity 73.5%) and operation time (cut-off value 237.5, sensitivity 62.5%, specificity 78.6%).
Conclusions: The FI, preoperative MMSE score, and operation time were independent risk factors for POD in elderly patients after cardiac surgery, with high predictive value observed with the FI and operation time. Cerebral oxygen saturation was associated with POD but was not an independent risk factor.
Clinical Trial Registration: Chinese Clinical Trail Registry, No: chictr2200056038.
Introduction
Frailty is an age-related state of diminished physiological reserve and function that results in increased vulnerability to endogenous and exogenous stressors (1–3). With the increasing prevalence of cardiovascular diseases among elderly patients, the incidence of frailty has been increasing among cardiac surgical patients of these age groups (4–6). Limitations in withstanding surgical stressors (7) are associated with an increased risk of adverse health outcomes such as surgery-related complications, falls, disability, hospitalization, and mortality (8, 9).
Postoperative delirium (POD) represents an acute neurocognitive complication characterized by fluctuating levels of consciousness (10, 11). It mainly occurs within 2–3 days after surgery (12), and has been considered the most common surgical complication among elderly patients (13). Besides the negative impacts of POD on postoperative recovery, it often results in prolonged hospital stay, increased medical costs, as well as increased risk of patient morbidity and mortality (14). The incidence of POD varies across different types of surgeries. In China, the overall incidence of POD in hospitalized patients older than 65 years of age is 17.1% (15), with cardiac surgery having a 46% incidence of POD due to the intraoperative effects of extracorporeal circulation (16). The etiology of POD is multifactorial (17), and may involve both intrinsic and extrinsic factors such as age, cognitive dysfunction, comorbidities, visual and hearing status, and alcohol use, among others (18, 19).
The aim of the study is to explore the risk factors for POD in frail elderly patients undergoing on-pump cardiac surgery, to further improve the clinical prevention and treatment of POD among such patients.
Methods
Study design
This study was approved by the Institutional Committee for Medical Ethics (2022ky002), and has been registered on the Chinese Clinical Trial Registry (https://www.chictr.org.cn/ChiCTR2200056038).
Patients undergoing elective on-pump cardiac surgery at Northern Jiangsu People's Hospital (Yangzhou City, Jiangsu province, China) between November 2021 and May 2022 were prospectively enrolled. Inclusion criteria included age ≥65 years. Exclusion criteria included (1) hepatic or renal insufficiency; (2) not capable of self-care; (3) visual and hearing impairment; (4) history of severe neuropsychiatric illness; (5) recent sedatives or antidepressant use; (6) cerebrovascular diseases such as intracranial aneurysm, head and neck artery stenosis or occlusion, and vascular cognitive impairment, (7) hemorrhagic stroke or traumatic brain injury with sequelae, (8) inability to cooperate with study protocol, (9) preoperative Mini-Mental State Examination (MMSE) score <20, and (10) emergency surgeries.
Perioperative management
Baseline frailty status was assessed using the FI scale. Patients were assessed preoperatively according to the FI, and frailty was defined as FI ≥0.25; pre-frailty was defined as FI 0.09–0.25. Cerebral oxygen saturation was monitored using the FORE-SIGHT oximeter (CASMED, Branford, CT, USA). Renal and brachioradialis muscle oxygen saturations were monitored using the INVOS5100C device (Medtronic, Minneapolis, MN).
Study protocol
A single blinded anesthetist was involved in the study, and anesthetic management was not influenced by the oxygen saturation monitoring values. Induction was performed with a single injection of midazolam (0.1–0.5 mg/kg), etomidate (0.1–0.4 mg/kg), sufentanil (0.5 ug/kg), and cisatracurium (0.2 mg/kg). The pressure-controlled ventilation volume-guaranteed (PCV-VG) mode was used with the following parameters: fraction of inspired oxygen (FiO2), 0.6–0.8; tidal volume, 6–8 ml/kg (employing ideal body weight); PEEP, 5 cmH2O; and partial carbon dioxide pressure (PaCO2), 40 mmHg, as measured using an arterial blood gas analyzer (Gem 3500, Instrumentation Laboratory, Bedford, MA, USA). Maintenance was achieved with dexmedetomidine (0.2–0.5 ug/kg/h), cisatracurium (0.05–0.1 mg/kg/h), and sevoflurane (1%–2.5%). Sufentanil was administered as necessary throughout the procedure. Noradrenaline, dopamine, dobutamine, and nitroglycerin were used to maintain hemodynamic balance. MAP was maintained within 20% of baseline.
Extracorporeal circulation was performed using a heart-lung machine (MAQUET, Rastatt, Germany) and a membrane oxygenator (TERUMO Corporation, Tokyo, Japan). Heparin (300 U/kg) was administered to achieve an activated coagulation time (ACT) of ≥480 s. Antegrade hyperkalemic cardioplegia was instituted, and moderate hypothermia was applied (32–35°C). Perfusion flow rate (2.0–2.4 L/min/m2) was adjusted to maintain a perfusion pressure of 60–80 mmHg. Blood pH and hematocrit were maintained at 7.35–7.45 and 25%–30%, respectively. ACT was monitored dynamically, and heparin was added as necessary. Upon completion of the procedure, slow infusion of protamine was administered via the ascending aorta for neutralization.
The FI scale we used assessed 50 items, including mental status, self-care ability, motor coordination, adverse living habits, head and neck diseases, cardiovascular diseases, pulmonary diseases, abdominal diseases, cerebrovascular disease, hypertension, hyperlipidemia, diabetes, skin diseases, musculoskeletal diseases, sleep quality, physiological and mental illness, cognitive disorders, standing and walking posture, and history of falls. The patient FI was defined as the ratio of the number of items showing defects to the total number of assessed items. The total score was 1. Frailty, pre-frailty, and non-frailty were defined as FI ≥0.25, FI 0.09–0.25, and FI ≤0.08, respectively.
Baseline demographic and clinical data included sex, age, body mass index (BMI), noninvasive and invasive blood pressure, the American Society of Anesthesiologist (ASA) score, New York Heart Association (NYHA) classification, MMSE score, presence of comorbidities such as hypertension, diabetes, hyperlipidemia, cerebrovascular disease, intraoperative vasoactive drug doses, hemoglobin, white cell count, albumin, N-terminal pro-B-type natriuretic peptide, S100β calcium binding protein, left ventricular ejection fraction, left atrium diameter, left ventricle diameter, and surgery type.
Intraoperative data included doses of the vasoactive drugs, operation time, mechanical ventilation time, CPB time, aortic cross clamp time, and tissue oxygen saturation. Cerebral (SctO2), renal (SrtO2), and brachioradialis muscle oxygen saturation (SmtO2) were recorded at the following time points: 1 day pre-surgery (T0), 5 min post-admission (T1), pre-tracheal intubation (T2), 5 min post-tracheal intubation (T3), pre-CPB (T4), at aortic clamp (T5), at aortic clamp opening (T6), the end of CPB (T7), post-surgery (T8), followed by post-surgery day 1 (T9), 3 (T10), 5 (T11), and 7 (T12). The baseline (SctO2 baseline, SrtO2 baseline, SmtO2 baseline), lowest (SctO2 lowest, SrtO2 lowest, SmtO2 lowest), and greatest (SctO2 decrease, SrtO2 decrease, SmtO2 decrease) oxygen saturation values were recorded.
Postoperative data included complications, as well as cardiac intensive care unit (ICU) and hospital length of stay. The postoperative complications included postoperative pulmonary complications (pneumonia, atelectasis, pulmonary embolism, pulmonary insufficiency), postoperative nausea and vomiting, and sternal wound infections (both deep and superficial infections).
Statistical analysis
All statistical analyses were performed using SPSS version 25. Normality of distribution was assessed using the Kolmogorov-Smirnov test. Normally distributed data are expressed as mean ± standard deviation (SD), with intra- and inter-group comparisons made using Student t-test, respectively. Non-normally distributed data were compared using Mann-Whitney U-test. Numerical data were compared using the chi-square test. Risk factors for POD were analyzed using logistic regression, and their predictive values were assessed using the receiver operating characteristic (ROC) curve analysis.
Sample size estimation
The sample size was calculated with reference to the preliminary study and based on the sample size calculation formula. Since the probability of postoperative delirium was p = 0.6 for group A and p = 0.3 for group B, then for equal N in each group, α = 0.05, and (1-β) = 0.90, the required sample size was N = 112.
Results
Patient characteristics
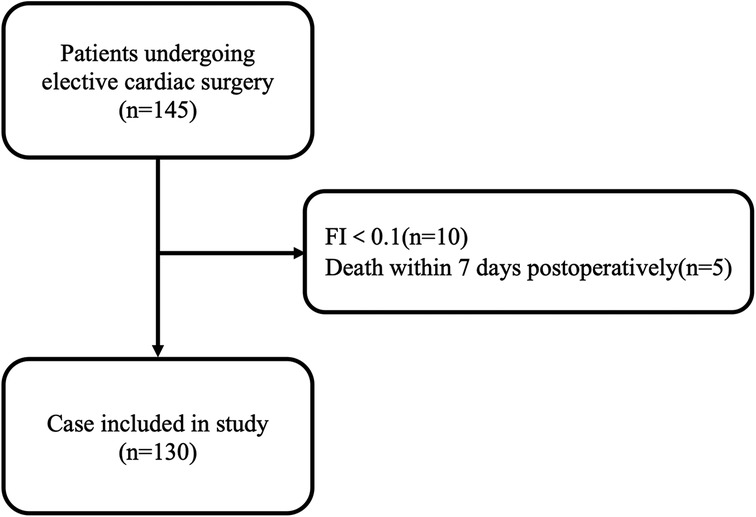
A total of 145 patients were scheduled for on-pump cardiac surgery during the study period (Figure 1). Among them, 15 were excluded due to FI <0.1 (n = 10), and death within 7 days of surgery (n = 5). As such, 130 patients were eventually included for data analysis.
Univariate logistic regression analysis results of potential clinical and demographic risk factors
A total of 32 patients (24.6%) demonstrated POD. The clinical data of the POD and Non-POD groups are summarized in Table 1. Based on univariate analysis, the FI, preoperative MMSE score, hyperlipidemia, diabetes mellitus, cerebrovascular disease, hemoglobin and albumin levels, operation time and CPB time were found as significant risk factors for POD (Table 1).
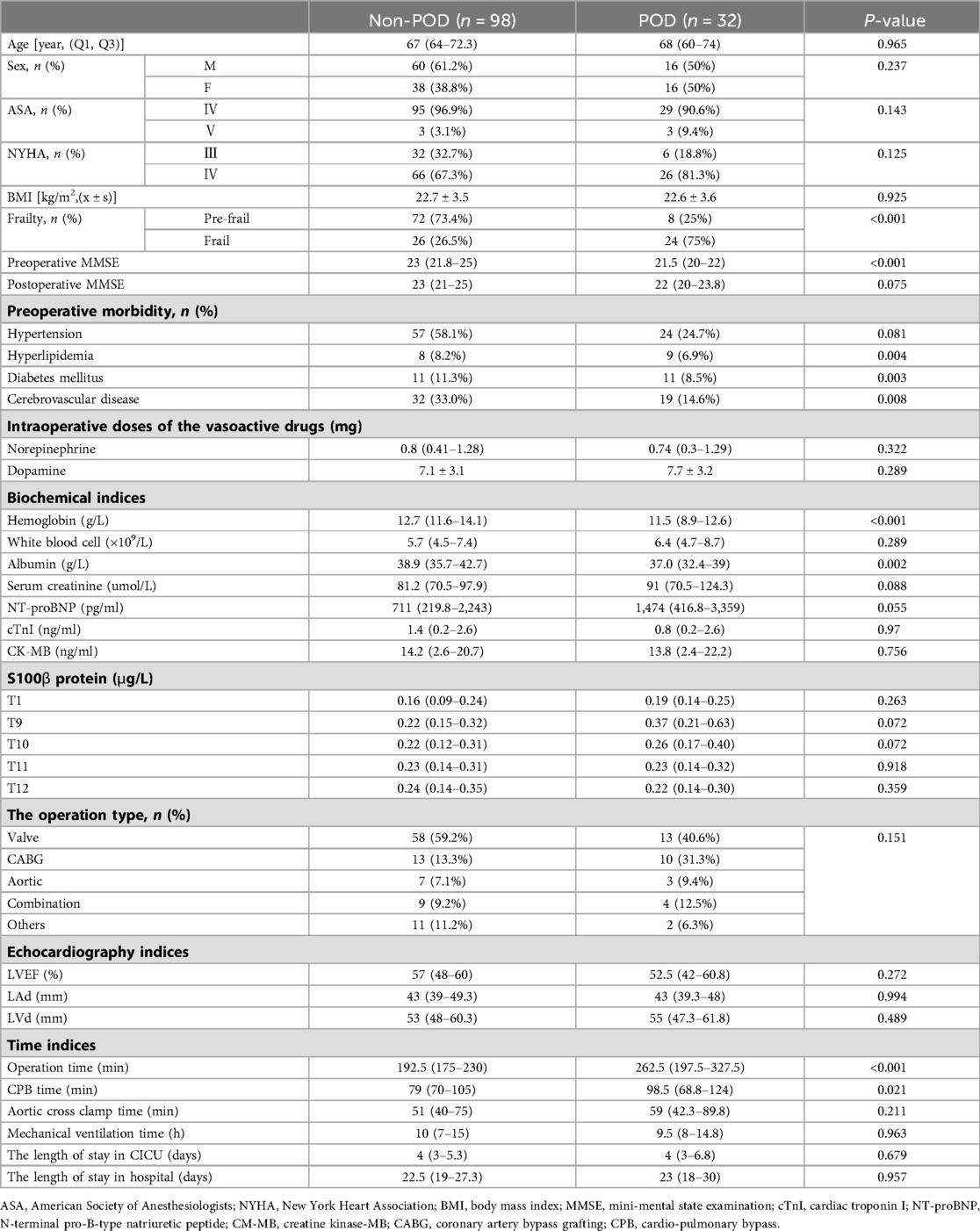
Table 1. Univariate logistic regression analysis results of potential clinical and demographic risk factors.
Tissue oxygen saturation
SctO2 (T2), and SctO2lowest were found as significant risk factors for POD. The two groups showed no statistically significant difference in SrtO2 and SmtO2 (Table 2).
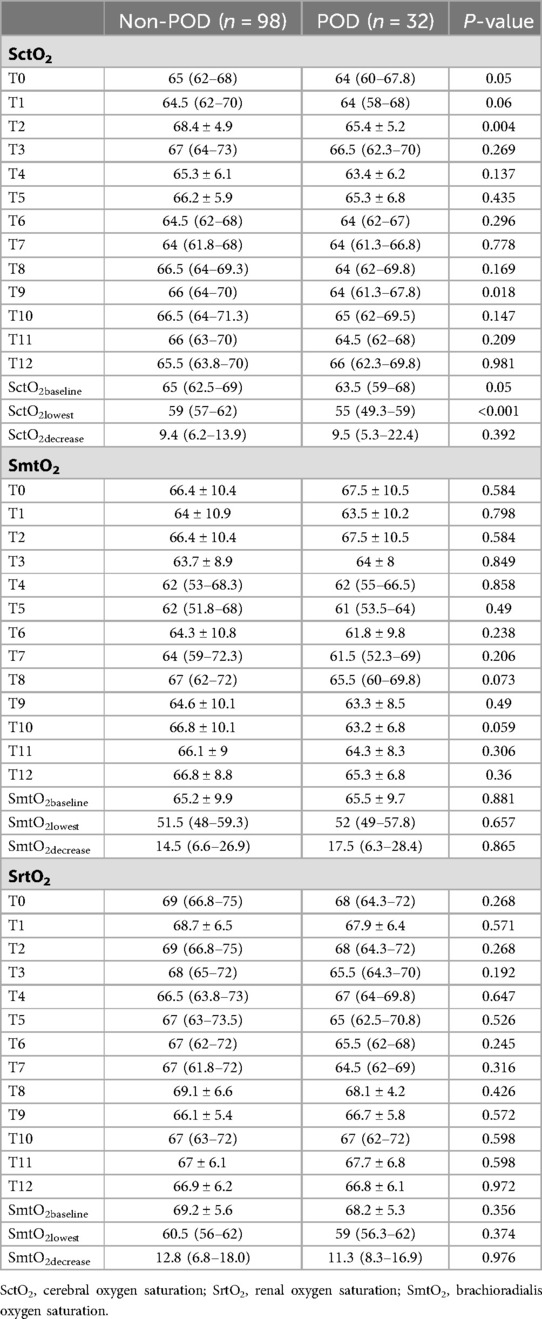
Table 2. Results of univariate logistic regression analysis of potential tissue oxygen saturation risk factors.
Multivariate logistic regression analysis
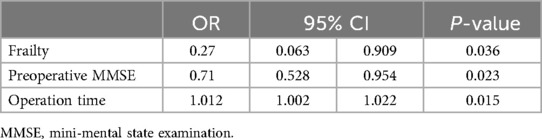
Only the FI (OR 0.27, 95% CI 0.063–0.909), preoperative MMSE score (OR 0.71, 95% CI 0.528–0.954), and operation time (OR 1.012, 95% CI 1.002–1.022) remained significant in the multivariate analysis (P < 0.05) (Table 3).
The FI (AUC 0.742, 95% CI 0.642–0.843, P < 0.001), preoperative MMSE score (AUC 0.281, 95% CI 0.184–0.378, P < 0.001), and operation time (AUC 0.751, 95% CI 0.652–0.849, P < 0.001) were found as significant predictive factors for POD (Figure 2). Both sensitivity and specificity were high for the FI (cut-off value, 0.27; sensitivity, 75%; specificity, 73.5%) and operation time (cut-off value, 237.5; sensitivity, 62.5%; specificity, 78.6%). However, while the sensitivity for the preoperative MMSE score was high, the specificity was found to be 0% (cut-off value, 19; sensitivity, 100%, specificity, 0%).
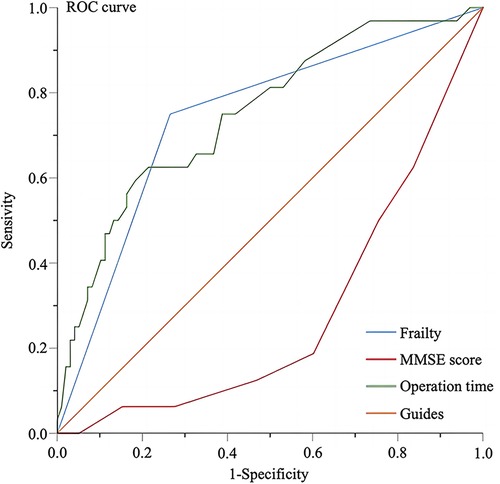
Figure 2. ROC curves on the predictive value of relevant factors for POD. ROC, receiver operating characteristic; MMSE, minimum mental state examination.
Discussion
Among the elderly patients undergoing elective on-pump cardiac surgery, 50 (38.5%) were considered frail at baseline, and demonstrated a POD incidence of 46%. This is in contrast with the 80 (61.5%) pre-frailty patients, who demonstrated a POD incidence of 11.3%, which was significantly lower. The pathogenesis of frailty is multifactorial, and can be the result of chronic diseases, unhealthy lifestyles, and activity limitation. The reduced physiological reserve, coupled with the impaired resistance to surgical stress, thereby render a poor prognosis inevitable among frail patients (20, 21). In line with this, patients of the frailty group demonstrated greater comorbidities at baseline. Such patients further associated with lower cardiac function grades, which corroborated with the need for significantly higher doses of intraoperative dopamine compared to their counterparts. In addition, the rate of postoperative pulmonary complications was significantly higher among frail patients. Frail patients also reported longer length of hospital stay. Although statistically insignificant, this implied a longer recovery duration among such patients.
Frailty was demonstrated to significantly associate with POD in our study. Frailty was assessed in terms of FI, which employs a cumulative deficits approach, and has been considered an effective predictor of adverse outcome (22). As reported in the meta-analysis by Kojima et al., every 0.1 increase in FI was associated with a 28% increase in mortality risk (23). Importantly, our study found frailty as both an independent risk factor and a predictive factor for POD following cardiac surgery. In general, our findings fit with those of prior research. Although our study did not explore the association of frailty with postoperative mortality, both the operation time and postoperative pulmonary complication rate were higher in patients of the frailty group than those of the pre-frailty group, which may also be predictive of poor outcomes in patients with frailty.
The exposure of blood to foreign material during extracorporeal circulation may precipitate widespread inflammatory responses which can lead to postoperative neurocognitive decompensation (24). Hemodynamic fluctuations involved during CPB may further disrupt the perfusion of brain tissues and result in cerebral ischemia, one of the risk factors of POD (25). Conventional arterial pressure monitoring techniques such as MAP have been considered inadequate for the accurate reflection of cerebral perfusion (26, 27). Near-infrared spectroscopy (NIRS) is an emerging noninvasive brain imaging technology that is portable, mobile, and low-cost (28). It utilizes near-infrared light from 650 to 900 nm to determine cerebral oxygenation, blood flow, and metabolic status of localized regions of the brain. NIRS enables the continuous monitoring of rSO2, which allows for timely detection of cerebral hypoxia, and thereby plays an essential role in the protection against POD (29). In the observational study by Eertmans et al. (30) involving the continuous monitoring of rSO2 until 72 h after cardiac surgery, higher EuroSCORE II, lower preoperative MMSE score, and greater decrease in absolute postoperative rSO2 independently associated with POD. Our findings were partly in line with this, with frailty and the preoperative MMSE score identified as significant risk factors for POD, in addition to operation time. In contrast, SctO2 (T2) and SctO2lowest did not demonstrate significant association to POD on multivariate analysis. This may be due to the small sample size of our study, which rendered insufficient statistical power, and the relatively short duration of monitoring. Renal oxygen saturation (SrtO2) has been often used to monitor the renal tissue blood perfusion to determine the presence of renal ischemia and hypoxia and to prevent the occurrence of acute renal injury (31). Simultaneously, other studies have described the monitoring the oxygen saturation of muscle tissue to assess the level of lactic acid in patients and thereby predict the body perfusion of patients (32). These results suggest that the oxygen saturation of renal and muscle tissue can reflect the blood perfusion level and oxygen-carrying capacity of the body to a certain extent. Our study show that the two groups showed no statistically significant difference in SrtO2 and SmtO2. SrtO2 and SmtO2 were not significant risk factors for POD.
Several studies have similarly identified operation time as a risk factor for cognitive dysfunction following surgery (33, 34). Prolonged duration of surgery not only increases the dosage of anesthetic drugs, but also increases the risk of cerebral ischemia and hypoxia (35). Our findings of an operation time of >237.5 min as an independent risk factor highlighted the importance of establishing a reasonable surgical plan to minimize the duration of surgery for the prevention of POD among frail elderly patients undergoing cardiac surgery.
There were several other limitations to this study. First, our results were limited by the single-center observational design. Second, as only cardiac surgeries involving extracorporeal circulation were considered, procedures such as off-pump coronary artery bypass grafting and aortic dissection were overlooked, thereby limiting the applicability of our results. Multi-center large-sample studies evaluating the association of frailty with POD following a wider range of cardiac surgeries are therefore warranted.
In summary, the FI, preoperative MMSE score, and operation time were independent risk factors for POD in elderly patients after cardiac surgery, with the FI and operation time showing a high predictive value, Cerebral oxygen saturation was associated with POD but was not an independent risk factor. Renal oxygen saturation and muscle oxygen saturation were not significant risk factors for POD.
Data availability statement
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found in the article/Supplementary Material.
Ethics statement
The studies involving humans were approved by the Ethics Committee of Northern Jiangsu People's Hospital. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
YD: Software, Writing – original draft. JG: Conceptualization, Funding acquisition, Investigation, Writing – review & editing. YG: Data curation, Writing – review & editing. TH: Project administration, Writing – review & editing. YZ: Funding acquisition, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article.
This research was supported by The National Natural Science Fund, China (82172190 and 82101299).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Cloney MB, Ordon M, Tecle NE, Sprau A, Kemeny H, Dahdaleh NS. Frailty predicts readmission, reoperation, and infection after posterior spinal fusion: an institutional series of 3,965 patients. Clin Neurol Neurosurg. (2022) 222:107426. doi: 10.1016/j.clineuro.2022.107426
2. Beier F, Loffler M, Nees F, Hausner L, Frolich L, Flor H. Sensory and motor correlates of frailty: dissociation between frailty phenotype and frailty index. BMC Geriatr. (2022) 22(1):755. doi: 10.1186/s12877-022-03416-6
3. Fowler AJ, Stephens TJ, Partridge J, Dhesi J. Surgery in older patients: learning from shared decision-making in intensive care. Br J Anaesth. (2022) 129(5):652–5. doi: 10.1016/j.bja.2022.08.002
4. Sun LY, Jabagi H, Fang J, Lee DS. Comparison of multidimensional frailty instruments for estimation of long-term patient-centered outcomes after cardiac surgery. JAMA Netw Open. (2022) 5(9):e2230959. doi: 10.1001/jamanetworkopen.2022.30959
5. Miguelena-Hycka J, Lopez-Menendez J, Prada PC, Garcia MM, Vigil-Escalera C, Harmand MG, et al. Changes in frailty status after cardiac surgery. A prospective cohort study. Arch Gerontol Geriatr. (2022) 98:104568. doi: 10.1016/j.archger.2021.104568
6. Bielecka-Dabrowa A, Ebner N, Dos Santos MR, Ishida J, Hasenfuss G, von Haehling S. Cachexia, muscle wasting, and frailty in cardiovascular disease. Eur J Heart Fail. (2020) 22(12):2314–26. doi: 10.1002/ejhf.2011
7. Miura Y, Nishio K, Kitamura Y, Goto T, Yano M, Matsui S. Surgical risk assessment for super-elderly patients. Geriatr Gerontol Int. (2022) 22(4):271–7. doi: 10.1111/ggi.14340
8. Emmert DA, Arcario MJ, Maranhao B, Reidy AB. Frailty and cardiac surgery: to operate or not? Curr Opin Anaesthesiol. (2022) 35(1):53–9. doi: 10.1097/ACO.0000000000001075
9. Lal S, Gray A, Kim E, Bunton RW, Davis P, Galvin IF, et al. Frailty in elderly patients undergoing cardiac surgery increases hospital stay and 12-month readmission rate. Heart Lung Circ. (2020) 29(8):1187–94. doi: 10.1016/j.hlc.2019.10.007
10. Mossello E, Baroncini C, Pecorella L, Giulietti C, Chiti M, Caldi F, et al. Predictors and prognosis of delirium among older subjects in cardiac intensive care unit: focus on potentially preventable forms. Eur Heart J Acute Cardiovasc Care. (2020) 9(7):771–8. doi: 10.1177/2048872619882359
11. Tsai CY, Liu KH, Lai CC, Hsu JT, Hsueh SW, Hung CY, et al. Association of preoperative frailty and postoperative delirium in older cancer patients undergoing elective abdominal surgery: a prospective observational study in Taiwan. Biomed J. (2022) 46(4):100557. doi: 10.1016/j.bj.2022.08.003
12. Fong TG, Inouye SK. The inter-relationship between delirium and dementia: the importance of delirium prevention. Nat Rev Neurol. (2022) 18(10):579–96. doi: 10.1038/s41582-022-00698-7
13. Liu H, Zhao Q, Liu X, Hu X, Wang L, Zhou F. Incidence and interaction factors of delirium as an independent risk of mortality in elderly patients in the intensive units: a retrospective analysis from MIMIC-IV database. Aging Clin Exp Res. (2022) 34(11):2865–72. doi: 10.1007/s40520-022-02215-8
14. Sato K, Kubota K, Oda H, Taniguchi T. The impact of delirium on outcomes in acute, non-intubated cardiac patients. Eur Heart J Acute Cardiovasc Care. (2017) 6(6):553–9. doi: 10.1177/2048872615624239
15. Zhang M, Zhang X, Gao L, Yue J, Jiang X. Incidence, predictors and health outcomes of delirium in very old hospitalized patients: a prospective cohort study. BMC Geriatr. (2022) 22(1):262. doi: 10.1186/s12877-022-02932-9
16. Inouye SK, Westendorp RG, Saczynski JS. Delirium in elderly people. Lancet. (2014) 383(9920):911–22, doi: 10.1016/S0140-6736(13)60688-1
17. Wilcox ME, Girard TD, Hough CL. Delirium and long term cognition in critically ill patients. Br Med J. (2021) 373:n1007. doi: 10.1136/bmj.n1007
18. Gravante F, Giannarelli D, Pucci A, Gagliardi AM, Mitello L, Montagna A, et al. Prevalence and risk factors of delirium in the intensive care unit: an observational study. Nurs Crit Care. (2021) 26(3):156–65. doi: 10.1111/nicc.12526
19. Kazmierski J, Miler P, Pawlak A, Jerczynska H, Nowakowska K, Walkiewicz G, et al. Increased postoperative myeloperoxidase concentration associated with low baseline antioxidant capacity as the risk factor of delirium after cardiac surgery. Ann Med. (2022) 54(1):610–6. doi: 10.1080/07853890.2022.2039405
20. Kjelsnes AA, Feiring E. Models of integrated care for older people with frailty: a horizon scanning review. BMJ Open. (2022) 12(4):e060142. doi: 10.1136/bmjopen-2021-060142
21. Kalyanasundaram A, Li N, Gardner ML, Artiga EJ, Hansen BJ, Webb A, et al. Fibroblast-specific proteotranscriptomes reveal distinct fibrotic signatures of human sinoatrial node in nonfailing and failing hearts. Circulation. (2021) 144(2):126–43. doi: 10.1161/CIRCULATIONAHA.120.051583
22. Barker FJ, Davies JI, Gomez-Olive FX, Kahn K, Matthews FE, Payne CF, et al. Developing and evaluating a frailty index for older South Africans-findings from the HAALSI study. Age Ageing. (2021) 50(6):2167–73. doi: 10.1093/ageing/afab111
23. Khalafallah AM, Huq S, Jimenez AE, Brem H, Mukherjee D. The 5-factor modified frailty index: an effective predictor of mortality in brain tumor patients. J Neurosurg. (2020) 135(1):78–86. doi: 10.3171/2020.5.JNS20766
24. Hatami S, Hefler J, Freed DH. Inflammation and oxidative stress in the context of extracorporeal cardiac and pulmonary support. Front Immunol. (2022) 13:831930. doi: 10.3389/fimmu.2022.831930
25. Qin XW, Chen XL, Yao L. The value of intraoperative monitoring of cerebral oxygen saturation on postoperative cognitive function in elderly patients undergoing cardiac surgery. Zhonghua Yi Xue Za Zhi. (2021) 101(5):345–9. doi: 10.3760/cma.j.cn112137-20200527-01681
26. Christie IN, Windsor R, Mutsaerts HJ, Tillin T, Sudre CH, Hughes AD, et al. Cerebral perfusion in untreated, controlled, and uncontrolled hypertension. J Cereb Blood Flow Metab. (2022) 42(12):2188–90. doi: 10.1177/0271678X221124644
27. Liu X, Nakano M, Yamaguchi A, Bush B, Akiyoshi K, Lee JK, et al. The association of bispectral index values and metrics of cerebral perfusion during cardiopulmonary bypass. J Clin Anesth. (2021) 74:110395. doi: 10.1016/j.jclinane.2021.110395
28. Mihara M, Miyai I. Review of functional near-infrared spectroscopy in neurorehabilitation. Neurophotonics. (2016) 3(3):031414. doi: 10.1117/1.NPh.3.3.031414
29. Tribuddharat S, Ngamsaengsirisup K, Mahothorn P, Sathitkarnmanee T. Correlation and agreement of regional cerebral oxygen saturation measured from sensor sites at frontal and temporal areas in adult patients undergoing cardiovascular anesthesia. PeerJ. (2022) 10:e14058. doi: 10.7717/peerj.14058
30. Eertmans W, De Deyne C, Genbrugge C, Marcus B, Bouneb S, Beran M, et al. Association between postoperative delirium and postoperative cerebral oxygen desaturation in older patients after cardiac surgery. Br J Anaesth. (2020) 124(2):146–53. doi: 10.1016/j.bja.2019.09.042
31. Bonsante F, Ramful D, Binquet C, Samperiz S, Daniel S, Gouyon JB, et al. Low renal oxygen saturation at near-infrared spectroscopy on the first day of life is associated with developing acute kidney injury in very preterm infants. Neonatology. (2019) 115(3):198–204. doi: 10.1159/000494462
32. Lee YS, Kim WY, Yoo JW, Jung HD, Min TJ. Correlation between regional tissue perfusion saturation and lactate level during cardiopulmonary bypass. Korean J Anesthesiol. (2018) 71(5):361–7. doi: 10.4097/kja.d.17.00002
33. Kang T, Park SY, Lee JH, Lee SH, Park JH, Kim SK, et al. Incidence & risk factors of postoperative delirium after spinal surgery in older patients. Sci Rep. (2020) 10(1):9232. doi: 10.1038/s41598-020-66276-3
34. Zhang G, Wang Z, Wang D, Jia Q, Zeng Y. A systematic review and meta-analysis of the correlation between operation time and postoperative delirium in total hip arthroplasty. Ann Palliat Med. (2021) 10(10):10459–66. doi: 10.21037/apm-21-2190
Keywords: frailty, cardiopulmonary bypass, tissue oxygen saturation, cardiac surgery, postoperative delirium, near-infrared spectroscopy
Citation: Ding Y, Gao J, Ge Y, Huang T and Zhang Y (2024) Risk factors for postoperative delirium in frail elderly patients undergoing on-pump cardiac surgery and development of a prediction model—a prospective observational study. Front. Cardiovasc. Med. 11:1425621. doi: 10.3389/fcvm.2024.1425621
Received: 30 April 2024; Accepted: 26 July 2024;
Published: 7 August 2024.
Edited by:
Leonard Y. Lee, The State University of New Jersey, United StatesReviewed by:
Nikoletta Rachel Czobor, György Gottsegen Hungarian Institute of Cardiology, HungaryDeane Smith, New York University, United States
© 2024 Ding, Gao, Ge, Huang and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yang Zhang, emhhbmd5YW5nOTAxMjI5QGZveG1haWwuY29t
†These authors have contributed equally to this work
 Yinyin Ding
Yinyin Ding Ju Gao†
Ju Gao† Yang Zhang
Yang Zhang