
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
EDITORIAL article
Front. Cardiovasc. Med. , 20 May 2024
Sec. Cardiovascular Pharmacology and Drug Discovery
Volume 11 - 2024 | https://doi.org/10.3389/fcvm.2024.1420293
This article is part of the Research Topic Sex Differences and Cardiovascular Therapeutics View all 13 articles
Editorial on the Research Topic
Sex differences and cardiovascular therapeutics
Cardiovascular diseases (CVDs) remain a leading cause of morbidity and mortality worldwide (1). Sex and gender as a biological variable, are crucial factors that impact every aspect of clinical and public health practice and research (2–4). In recent times, research investigating sex differences has gained more attention, partly benefit from federal agencies emphasizing the importance of considering sex as a significant biological factor (5). Within cardiovascular medicine, sex and gender affect disease presentation, pathophysiology, diagnostic assessment, responses to treatments, and overall health outcomes (6, 7). Historically, CVD has been perceived as primarily affecting men; however, it is increasingly recognized as a leading cause of morbidity and mortality in women as well (8). While men tend to develop CVD earlier in life, CVD prevalence increases significantly in postmenopausal women, narrowing the gap between the sexes (9). Men have traditionally experienced higher rates of CVD-related events, but women are more likely to die following an acute cardiovascular event (10). The existence of these gender disparities has prompted significant attention, highlighting the crucial significance of considering gender variations in the prevention, diagnosis, treatment, and overall management of CVD (11).
Traditional risk factors such as hypertension, diabetes, dyslipidemia, and smoking affect both sexes, but their impacts can vary between men and women (12–14). Additionally, women may experience unique risk factors including pregnancy-related complications such as gestational diabetes and preeclampsia, as well as endocrine disorders in reproductive age such as polycystic ovary syndrome (PCOS) and early menopause, which are associated with accelerated development of CVD and impaired CVD-free survival (15–17). Biological differences include genetic differences, variation in sex hormonal status, vascular anatomy, endothelial function, and plaque composition, which contribute to differences in the pathophysiology of CVD between men and women (18, 19). Women showed less plaque inflammatory infiltration compared to plaques from age-matched men (20–22). In addition, women often undergo fewer diagnostic tests and experience delays in diagnosis compared to men, leading to disparities in timely intervention and treatment (23). Despite accumulating evidence, the precise roles of biological sex and the sociocultural aspect of gender in the development and consequences of CVDs have not been fully explained. The interplay between sex-specific disparities in genetic and hormonal mechanisms and the intricate nature of gender, including its various components and influencing factors, which give rise to different disease patterns in men and women, requires further investigation.
The extents to which biological factors, such as genes and hormones, contribute to cardiovascular traits and outcomes are still not fully grasped. Heightened recognition of gender's impact has prompted endeavors to assess gender in both retrospective and prospective clinical studies, leading to the creation of gender scores. Yet, the combined or conflicting influences of sex and gender on cardiovascular characteristics, as well as on the mechanisms underlying CVDs, have not been systematically elucidated. The majority of medication are withdrawn after FDA approval due to unexpected adverse effects in women (24). Additionally, there are differences in the effectiveness and side effects of cardiovascular medications between men and women (25). Current guidelines do not provide sex-specific recommendations on the use of antithrombotic drugs in patients with coronary artery disease. Nevertheless, the effectiveness of antithrombotic medications might be impacted by genetic and biological factors associated to sex (26). Women generally exhibit greater platelet reactivity at baseline and in response to low-dose aspirin treatment in comparison to men (27). Despite receiving high-dose statin therapy following acute coronary syndrome, women showed a smaller absolute reduction in low-density lipoprotein cholesterol (LDL) cholesterol levels compared to men (28). Understanding these sex differences is crucial for providing personalized and effective cardiovascular care. It requires including more women in clinical trials, analyzing data by sex, and considering sex-specific factors in treatment decisions. By doing so, healthcare providers can optimize outcomes and reduce disparities in cardiovascular care between men and women.
Sex hormones, including estrogen, progesterone, and testosterone, play significant roles in cardiovascular health and disease (29, 30). Estrogen, primarily found in premenopausal women, exerts cardioprotective effects (8, 29, 31). It helps maintain healthy blood vessel function by promoting vasodilation, reducing inflammation, and inhibiting the formation of atherosclerotic plaques. Estrogen also influences lipid metabolism, favoring higher levels of high-density lipoprotein (HDL) cholesterol and lower levels of LDL cholesterol, contributing to a reduced risk of CVDs such as heart attacks and strokes (32, 33).
The differences in estrogen levels between men and women, as well as the changes that occur during menopause, contribute to the variation in CVD occurrence between the sexes. Before menopause, women generally have higher levels of estrogen, potentially explaining their lower risk of CVD compared to men of the same age. However, after menopause, when estrogen levels decline, women's risk of CVD increases and may approach that of men (34). Progesterone, another female sex hormone, also plays a role in cardiovascular health, though its effects are less well understood compared to estrogen. Some research suggests that progesterone may have protective effects on the cardiovascular system, such as promoting vasodilation and inhibiting smooth muscle cell proliferation in blood vessels (35, 36).
Androgens, including testosterone and other male sex hormones, can influence cardiovascular health in both men and women. Low levels of testosterone in men have been associated with an increased risk of CVD, including coronary artery disease and heart failure (18). Testosterone influences factors such as blood pressure regulation, lipid metabolism, and the development of atherosclerosis. However, the relationship between testosterone levels and cardiovascular risk is complex, and both low and high levels of testosterone have been implicated in various cardiovascular conditions (33). In addition to testosterone, other androgens such as dehydroepiandrosterone (DHEA) and its sulfate (DHEAS) may also impact cardiovascular risk factors (18).
Overall, sex hormones play intricate roles in cardiovascular physiology and pathology. Understanding the interplay between sex hormones and cardiovascular health is essential for developing personalized approaches to preventing and managing CVDs.
Genetic factors play a significant role in cardiovascular characteristics, with some of these factors being specific to each sex (37). The presence of sex chromosomes (XX in females and XY in males) not only determines primary sexual characteristics but also influences cardiovascular health (38, 39). For instance, genes on the Y chromosome may impact cardiac function (40). Moreover, genetic variations in lipoprotein metabolism can influence the metabolism of lipoproteins differently in men and women (41, 42). For example, certain genetic variants may have a more pronounced effect on the levels of HDL cholesterol in women compared to men, or vice versa (43). Additionally, genes involved in blood pressure regulation may exhibit sex-specific effects. For instance, variations in genes related to the renin-angiotensin-aldosterone system (RAAS) may influence blood pressure in varying ways between men and women (44). Understanding these sex-specific genetic factors is crucial for developing personalized approaches to cardiovascular disease prevention, diagnosis, and treatment. It underscores the importance of considering sex as a biological variable in cardiovascular research and clinical practice.
Our Research Topic: “Sex Differences and Cardiovascular Therapeutics,” featured twelve papers comprising original research papers and reviews (Table 1). These highlights offer a comprehensive perspective on gender-related differences in various CVDs, potential factors contributing to these distinctions, and management strategies. Collectively, these papers contribute to our understanding of sex differences in cardiovascular therapeutics and emphasize the importance of tailored approaches to prevention, diagnosis, and treatment based on gender-specific considerations.
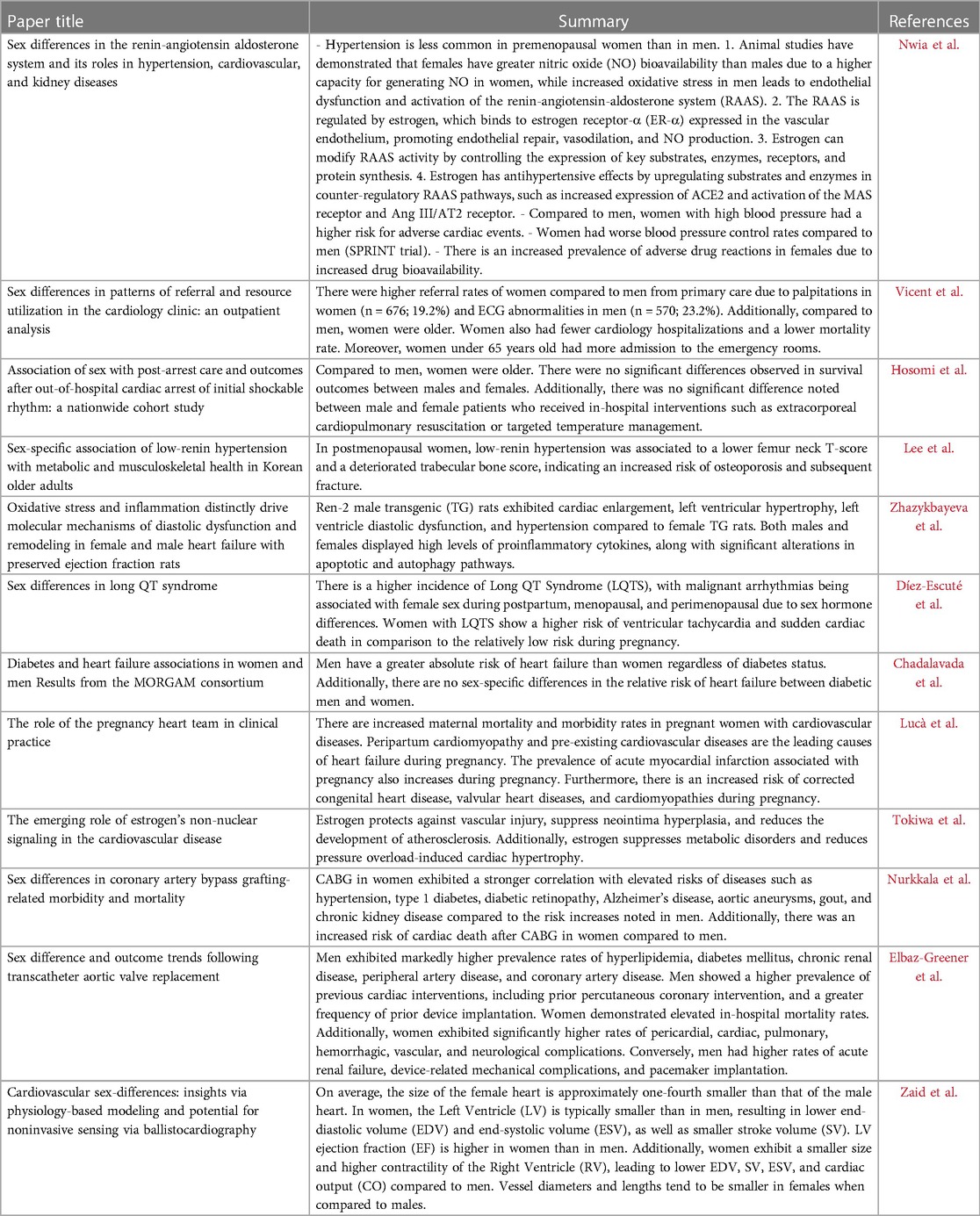
Table 1. Twelve highly viewed research papers, published in our special topic entitled “Sex differences and cardiovascular therapeutics”, are summarized.
Sex differences play a significant role in the epidemiology, pathophysiology, clinical presentation, diagnosis, management, and outcomes of cardiovascular diseases. Recognizing these differences and implementing sex-specific approaches in research, clinical practice, and public health initiatives are essential for reducing disparities and improving cardiovascular outcomes for both men and women. While the differences between sexes in the occurrence and complications of CVDs are widely acknowledged, there are relatively limited data in both clinical and pre-clinical studies that adequately explore the underlying mechanisms regarding sex as a biological variable in CVDs.
FS: Conceptualization, Data curation, Formal Analysis, Investigation, Methodology, Validation, Writing – original draft. KX: Conceptualization, Writing – review & editing. YL: Conceptualization, Writing – review & editing. YS: Conceptualization, Writing – review & editing. XJ: Conceptualization, Writing – review & editing. HW: Conceptualization, Writing – review & editing. XY: Conceptualization, Funding acquisition, Supervision, Formal Analysis, Visualization, Writing – review & editing.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article.
XY is funded by NIH grants (R01 HL163570-01A1 and 1R01HL147565-01).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Roth G, Abat D, Abat K, Abay S, Abbafati C, Abbasi N, et al. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980–2017: a systematic analysis for the global burden of disease study 2017. Lancet. (2018) 392(10159):1736–88. doi: 10.1016/S0140-6736(18)32203-7
2. Clayton JA, Tannenbaum C. Reporting sex, gender, or both in clinical research? JAMA. (2016) 316(18):1863–4. doi: 10.1001/jama.2016.16405
3. Schiebinger L, Stefanick ML. Gender matters in biological research and medical practice. J Am Coll Cardiol. (2016) 67(2):136–8. doi: 10.1016/j.jacc.2015.11.029
4. Mauvais-Jarvis F, Bairey Merz N, Barnes P, Brinton R, Carrero JJ, DeMeo D, et al. Sex and gender: modifiers of health, disease, and medicine. Lancet. (2020) 396(10250):565–82. doi: 10.1016/S0140-6736(20)31561-0
5. Clayton JA. Applying the new SABV (sex as a biological variable) policy to research and clinical care. Physiol Behav. (2018) 187:2–5. doi: 10.1016/j.physbeh.2017.08.012
6. Spence JD, Pilote L. Importance of sex and gender in atherosclerosis and cardiovascular disease. Atherosclerosis. (2015) 241(1):208–10. doi: 10.1016/j.atherosclerosis.2015.04.806
7. Miller L, Marks C, Becker J, Hurn P, Chen WJ, Woodruff T, et al. Considering sex as a biological variable in preclinical research. Faseb J. (2017) 31(1):29–34. doi: 10.1096/fj.201600781r
8. Connelly PJ, Jandeleit-Dahm KAM, Delles C. Sex and gender aspects in vascular pathophysiology. Clin Sci (Lond). (2020) 134(16):2203–7. doi: 10.1042/CS20200876
9. den Ruijter HM, Haitjema S, Asselbergs FW, Pasterkamp G. Sex matters to the heart: a special issue dedicated to the impact of sex related differences of cardiovascular diseases. Atherosclerosis. (2015) 241(1):205–7. doi: 10.1016/j.atherosclerosis.2015.05.003
10. Yu Y, Chen J, Li D, Wang L, Wang W, Liu H. Systematic analysis of adverse event reports for sex differences in adverse drug events. Sci Rep. (2016) 6: 24955. doi: 10.1038/srep24955
11. Seeland U, Regitz-Zagrosek V. Sex and gender differences in cardiovascular drug therapy. Handb Exp Pharmacol. (2012) 214:211–36. doi: 10.1007/978-3-642-30726-3_11
12. Dawber TR, Moore FE, Mann GV. Coronary heart disease in the framingham study. Am J Public Health Nations Health. (1957) 47(4 Pt 2):4–24. doi: 10.2105/AJPH.47.4_Pt_2.4
13. Mahmood SS, Levy D, Vasan RS, Wang TJ. The Framingham heart study and the epidemiology of cardiovascular disease: a historical perspective. Lancet. (2014) 383(9921):999–1008. doi: 10.1016/S0140-6736(13)61752-3
14. Feldman RD. Sex-specific determinants of coronary artery disease and atherosclerotic risk factors: estrogen and beyond. Can J Cardiol. (2020) 36(5):706–11. doi: 10.1016/j.cjca.2020.03.002
15. Veltman-Verhulst SM, van Rijn BB, Westerveld HE, Franx A, Bruinse HW, Fauser BC, et al. Polycystic ovary syndrome and early-onset preeclampsia: reproductive manifestations of increased cardiovascular risk. Menopause. (2010) 17(5):990–6. doi: 10.1097/gme.0b013e3181ddf705
16. Sattar N, Greer IA. Pregnancy complications and maternal cardiovascular risk: opportunities for intervention and screening? Br Med J. (2002) 325(7356):157–60. doi: 10.1136/bmj.325.7356.157
17. Ray JG, Vermeulen MJ, Schull MJ, Redelmeier DA. Cardiovascular health after maternal placental syndromes (CHAMPS): population-based retrospective cohort study. Lancet. (2005) 366(9499):1797–803. doi: 10.1016/S0140-6736(05)67726-4
18. Zhao D, Guallar E, Ballantyne CM, Post WS, Ouyang P, Vaidya D, et al. Sex hormones and incident heart failure in men and postmenopausal women: the atherosclerosis risk in communities study. J Clin Endocrinol Metab. (2020) 105(10):e3798–807. doi: 10.1210/clinem/dgaa500
19. Ventura-Clapier R, Piquereau J, Garnier A, Mericskay M, Lemaire C, Crozatier B. Gender issues in cardiovascular diseases. Focus on energy metabolism. Biochim Biophys Acta Mol Basis Dis. (2020) 1866(6):165722. doi: 10.1016/j.bbadis.2020.165722
20. Wendorff C, Wendorff H, Pelisek J, Tsantilas P, Zimmermann A, Zernecke A, et al. Carotid plaque morphology is significantly associated with sex, age, and history of neurological symptoms. Stroke. (2015) 46(11):3213–9. doi: 10.1161/STROKEAHA.115.010558
21. Sangiorgi G, Roversi S, Biondi Zoccai G, Modena MG, Servadei F, Ippoliti A, et al. Sex-related differences in carotid plaque features and inflammation. J Vasc Surg. (2013) 57(2):338–44. doi: 10.1016/j.jvs.2012.07.052
22. Yuan XM, Ward LJ, Forssell C, Siraj N, Li W. Carotid atheroma from men has significantly higher levels of inflammation and iron metabolism enabled by macrophages. Stroke. (2018) 49(2):419–25. doi: 10.1161/STROKEAHA.117.018724
23. Bugiardini R, Ricci B, Cenko E, Vasiljevic Z, Kedev S, Davidovic G, et al. Delayed care and mortality among women and men with myocardial infarction. J Am Heart Assoc. (2017) 6(8):e005968. doi: 10.1161/JAHA.117.005968
24. Domecq C, Naranjo CA, Ruiz I, Busto U. Sex-related variations in the frequency and characteristics of adverse drug reactions. Int J Clin Pharmacol Ther Toxicol. (1980) 18(8):362–6.7409941
25. Bairey Merz CN, Mark S, Boyan BD, Jacobs AK, Shah PK, Shaw LJ, et al. Proceedings from the scientific symposium: sex differences in cardiovascular disease and implications for therapies. J Womens Health (Larchmt). (2010) 19(6):1059–72. doi: 10.1089/jwh.2009.1695
26. Levin RI. The puzzle of aspirin and sex. N Engl J Med. (2005) 352(13):1366–8. doi: 10.1056/NEJMe058051
27. Price MJ, Nayak KR, Barker CM, Kandzari DE, Teirstein PS. Predictors of heightened platelet reactivity despite dual-antiplatelet therapy in patients undergoing percutaneous coronary intervention. Am J Cardiol. (2009) 103(10):1339–43. doi: 10.1016/j.amjcard.2009.01.341
28. Truong QA, Murphy SA, McCabe CH, Armani A, Cannon CP, TIMI Study Group. Benefit of intensive statin therapy in women: results from PROVE IT-TIMI 22. Circ Cardiovasc Qual Outcomes. (2011) 4(3):328–36. doi: 10.1161/CIRCOUTCOMES.110.957720
29. Clegg D, Hevener AL, Moreau KL, Morselli E, Criollo A, Van Pelt RE, et al. Sex hormones and cardiometabolic health: role of estrogen and estrogen receptors. Endocrinology. (2017) 158(5):1095–105. doi: 10.1210/en.2016-1677
30. Morselli E, Santos RS, Criollo A, Nelson MD, Palmer BF, Clegg DJ. The effects of oestrogens and their receptors on cardiometabolic health. Nat Rev Endocrinol. (2017) 13(6):352–64. doi: 10.1038/nrendo.2017.12
31. Regitz-Zagrosek V, Kararigas G. Mechanistic pathways of sex differences in cardiovascular disease. Physiol Rev. (2017) 97(1):1–37. doi: 10.1152/physrev.00021.2015
32. Pabbidi MR, Kuppusamy M, Didion SP, Sanapureddy P, Reed JT, Sontakke SP. Sex differences in the vascular function and related mechanisms: role of 17β-estradiol. Am J Physiol Heart Circ Physiol. (2018) 315(6):H1499–518. doi: 10.1152/ajpheart.00194.2018
33. dos Santos RL, da Silva FB, Ribeiro RF Jr, Stefanon I. Sex hormones in the cardiovascular system. Horm Mol Biol Clin Investig. (2014) 18(2):89–103. doi: 10.1515/hmbci-2013-0048
34. Garcia M, Mulvagh SL, Merz CN, Buring JE, Manson JE. Cardiovascular disease in women: clinical perspectives. Circ Res. (2016) 118(8):1273–93. doi: 10.1161/CIRCRESAHA.116.307547
35. Bernstein P, Pohost G. Progesterone, progestins, and the heart. Rev Cardiovasc Med. (2010) 11(3):e141–9. doi: 10.3909/ricm0557
36. Prior JC, Elliott TG, Norman E, Stajic V, Hitchcock CL. Progesterone therapy, endothelial function and cardiovascular risk factors: a 3-month randomized, placebo-controlled trial in healthy early postmenopausal women. PLoS One. (2014) 9(1):e84698. doi: 10.1371/journal.pone.0084698
37. Hajar R. Genetics in cardiovascular disease. Heart Views. (2020) 21(1):55–6. doi: 10.4103/HEARTVIEWS.HEARTVIEWS_140_19
38. Abramowitz LK, Olivier-Van Stichelen S, Hanover JA. Chromosome imbalance as a driver of sex disparity in disease. J Genomics. (2014) 2:77–88. doi: 10.7150/jgen.8123
39. Reue K, Wiese CB. Illuminating the mechanisms underlying sex differences in cardiovascular disease. Circ Res. (2022) 130(12):1747–62. doi: 10.1161/CIRCRESAHA.122.320259
40. Praktiknjo SD, Picard S, Deschepper CF. Comparisons of chromosome Y-substituted mouse strains reveal that the male-specific chromosome modulates the effects of androgens on cardiac functions. Biol Sex Differ. (2016) 7:61. doi: 10.1186/s13293-016-0116-4
41. Holven KB, van Lennep JR. Sex differences in lipids: a life course approach. Atherosclerosis. (2023) 384:117270. doi: 10.1016/j.atherosclerosis.2023.117270
42. Tabassum R, Widén E, Ripatti S. Effect of biological sex on human circulating lipidome: an overview of the literature. Atherosclerosis. (2023) 384:117274. doi: 10.1016/j.atherosclerosis.2023.117274
43. Link JC, Chen X, Prien C, Borja MS, Hammerson B, Oda MN, et al. Increased high-density lipoprotein cholesterol levels in mice with XX versus XY sex chromosomes. Arterioscler Thromb Vasc Biol. (2015) 35(8):1778–86. doi: 10.1161/ATVBAHA.115.305460
44. Sampson AK, Andrews KL, Graham D, McBride MW, Head GA, Thomas MC, et al. Origin of the Y chromosome influences intrarenal vascular responsiveness to angiotensin I and angiotensin (1–7) in stroke-prone spontaneously hypertensive rats. Hypertension. (2014) 64(6):1376–83. doi: 10.1161/HYPERTENSIONAHA.114.03756
Keywords: cardiovascular diseases, sex difference, sex hormones, genetic factors, therapeutics
Citation: Saaoud F, Xu K, Lu Y, Shao Y, Jiang X, Wang H and Yang X (2024) Editorial: Sex differences and cardiovascular therapeutics. Front. Cardiovasc. Med. 11:1420293. doi: 10.3389/fcvm.2024.1420293
Received: 19 April 2024; Accepted: 3 May 2024;
Published: 20 May 2024.
Edited and Reviewed by: Masanori Aikawa, Harvard Medical School, United States
© 2024 Saaoud, Xu, Lu, Shao, Jiang, Wang and Yang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xiaofeng Yang, eGZ5YW5nQHRlbXBsZS5lZHU=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.