- 1Cardiovascular and Thoracic Surgery Unit, Department of Surgery, Lampang Hospital, Lampang, Thailand
- 2Department of Cardiac Surgery, Asahikawa Medical University, Asahikawa, Japan
- 3Department of Emergency Medicine, Lampang Hospital, Lampang, Thailand
- 4Center for Clinical Epidemiology and Clinical Statistics, Faculty of Medicine, Chiang Mai University, Chiang Mai, Thailand
- 5Chaiprakarn Hospital, Chiang Mai, Thailand
Introduction: At our institution, we perform off-pump coronary artery bypass (OPCAB) as a standard procedure. Moreover, patients with favorable coronary anatomy and condition are selected for minimally invasive cardiac surgery (MICS)-OPCAB. We retrospectively compared early outcomes, focusing on safety, between MICS-OPCAB and conventional off-pump techniques for multivessel coronary artery bypass grafting (CABG).
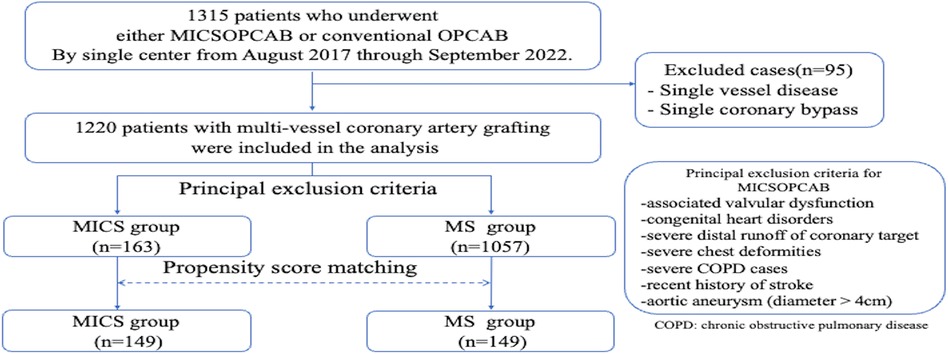
Methods: From August 2017 to September 2022, 1,220 patients underwent multivessel coronary artery grafting at our institution. They were divided into the MICS-OPCAB group (MICS group = 163 patients) and the conventional OPCAB group (MS group = 1057 patients). Propensity score matching (1 : 1 ratio) was applied to the MICS-OPCAB and MS groups (149 patients per group) based on 23 preoperative clinical characteristics.
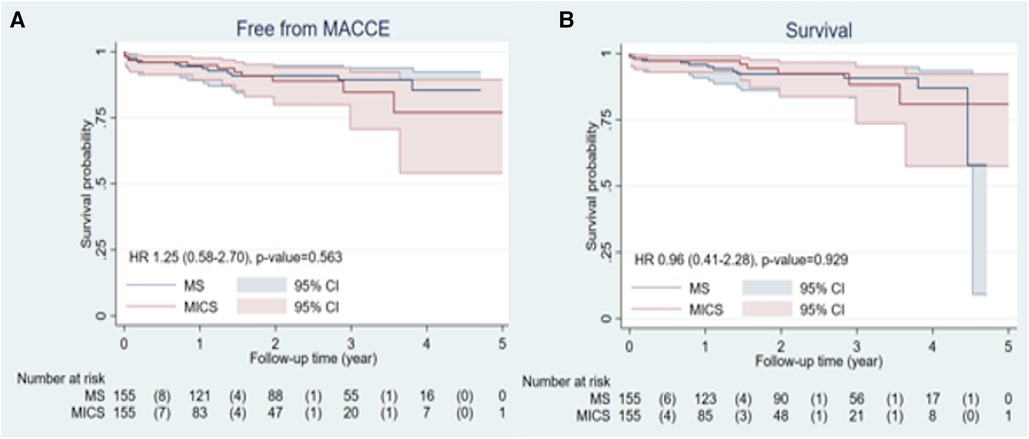
Results: After matching, there were no significant differences in preoperative characteristics between the groups. The MICS group had a lower total graft number (2.3 ± 0.6 vs. 2.9 ± 0.8, p < 0.001) and fewer distal anastomoses (2.7 ± 0.8 vs. 3.2 ± 0.9, p < 0.001). There were no significant differences in hospital stay, intensive care unit stay, postoperative complications, and 30-day mortality. The MICS group had less drain output (MICS 350 ml [250–500], MS 450 ml [300–550]; p = 0.013). Kaplan–Meier analysis revealed no significant differences in postoperative MACCE (major adverse cardiac or cerebrovascular events)-free and survival rates between the groups (MACCE-free rate p = 0.945, survival rate p = 0.374).
Conclusion: With proper patient selection, MICS-OPCAB can provide good short to mid-term results, similar to those of conventional OPCAB.
1 Introduction
Minimally invasive direct coronary artery bypass grafting (MIDCAB) (1) was popularized in the 1990s. Nowadays, multivessel coronary artery bypass grafting (CABG) via a left small thoracotomy has developed as a minimally invasive cardiac surgery coronary artery bypass (MICS-CABG) and maintained gaining attention (2, 3). In our institution, we have performed off-pump coronary artery bypass (OPCAB) as a standard procedure, and patients with favorable coronary anatomy and condition are selected for MICS-OPCAB. This study retrospectively compared the early outcomes of MICS-OPCAB and conventional off-pump techniques regarding the safety of treating multivessel coronary disease.
2 Patients and methods
We retrospectively analyzed 1,315 patients who underwent CABG between August 2017 and September 2022 at our single center (Figure 1). After excluding patients with single-vessel disease, or single coronary bypass (n = 95), a total of 1,220 patients who underwent multivessel CABG were included in this analysis. Patients were divided into the MICS-OPCAB (MICS group = 163 patients) and conventional OPCAB (MS group = 1,057 patients) groups. The MICS-OPCAB group was propensity score-matched (PSM) with the OPCAB group in a 1 : 1 ratio (MICS = 149, MS = 149), where matching was performed based on 23 covariates of preoperative clinical characteristics.
Within one week post operation, coronary computed tomography angiography (CTA) was performed on all MICS-OPCAB patients with creatinine levels of <1.5 ng/dl; while in the MS group, CTA was only considered for complex bypass cases or discharged patients who developed clinical symptoms indicative of postoperative cardiac ischemia.
2.1 Inclusion and exclusion criteria
Our institution has five surgeons total, where one senior surgeon performed all MICS-OPCAB, and the other surgeons performed conventional OPCAB. The principal exclusion criteria for MICS-OPCAB were: comorbid valvular dysfunction, congenital heart disorders, severe distal runoff of coronary target, severe chest deformities, severe chronic obstructive pulmonary disease (COPD), stroke within four weeks prior to surgery, and aortic aneurysm (diameter >4 cm). Relative contraindications included current smokers, tuberculosis, interstitial lung disease history, morbid obesity, and previous cardiac surgery. Acute myocardial infarction within seven days, poor left ventricular ejection fraction (LVEF) < 20%, or cardiomegaly (left ventricular end-diastolic diameter >6.0 cm) were only precautionary, and included in our study.
2.2 Surgical technique
Conventional OPCAB was performed via median sternotomy. Technical details of our MICS-OPCAB techniques were described in our previous report (4). Shortly, patients were positioned with the left chest elevated 30 to 40 degrees to widen intercostal space (ICS). All procedures were performed under differential ventilation, through an 8–10 cm left mini-thoracotomy (with 1/3 of the incision medial to the mid-clavicular line) in the fourth or fifth ICS to expose both internal thoracic arteries. The left internal thoracic artery (LITA) and right internal thoracic artery were harvested full length in a skeletonized fashion under direct vision. The saphenous vein graft was harvested non-touch or skeletonized by skip incision. Usual sequence of anastomosis was the left anterior descending artery (LAD), obtuse marginal branch, and the last posterior descending artery or posterior-lateral artery. Two deep pericardial stitches were routinely fixed in order to expose the lateral and inferior walls of the heart. On-pump conversion was considered in cases with unstable hemodynamics or multiple ventricular arrhythmias.
2.3 Follow-up
Patients were followed up every six months at our outpatient clinic. Information on all causes of death and cardiac complications during the follow-up period was obtained from Lampang Hospital's database. We achieved a 100% follow-up rate by contacting both the patients and their families for any missing data.
2.4 Statistical analysis
Group assignments were not random because the operative approach was a matter of subjective choice. Therefore, we calculated standardized mean differences before and after PSM to assess the balance of variables between the groups. The propensity score (PS) was obtained from a logistic regression model, including 23 covariables presented in Table 1 without European System for Cardiac Operative Risk Evaluation (Euro SCORE) Ⅱ, Society of Thoracic Surgeons (STS) score, and Emergent case (Table 2). Patients were matched 1:1 using the nearest neighbor matching method without replacement and a caliper width of 0.2 of the standard deviation of the logit of the estimated PS. A double adjustment was performed in case of remaining imbalance that standardized differences over 0.10. For double adjustment in the matched sample, we utilized Cox PH regression. Continuous variables exhibiting a normal distribution were tested using the t-test, and continuous variables exhibiting a non-normal distribution were tested using the Mann–Whitney U-test. For categorical variables, chi-squared or Fisher's test was used. In the final analysis, the categorical endpoint was tested using McNemar's exact test to incorporate the correlation after matching. Statistical significance was set at p < 0.05. The Kaplan–Meier method was used to demonstrate survival rate and freedom from major adverse cardiac or cerebrovascular events (MACCE). In addition, Cox PH regression analysis was used to evaluate the treatment effect to free MACCE and survival rate, which was presented as the hazard ratio (HR) with 95% CI. The STATA Software/MP, Version 17.0 (Stata Corporation, College Station, Texas, USA) was used for the statistical analyses.
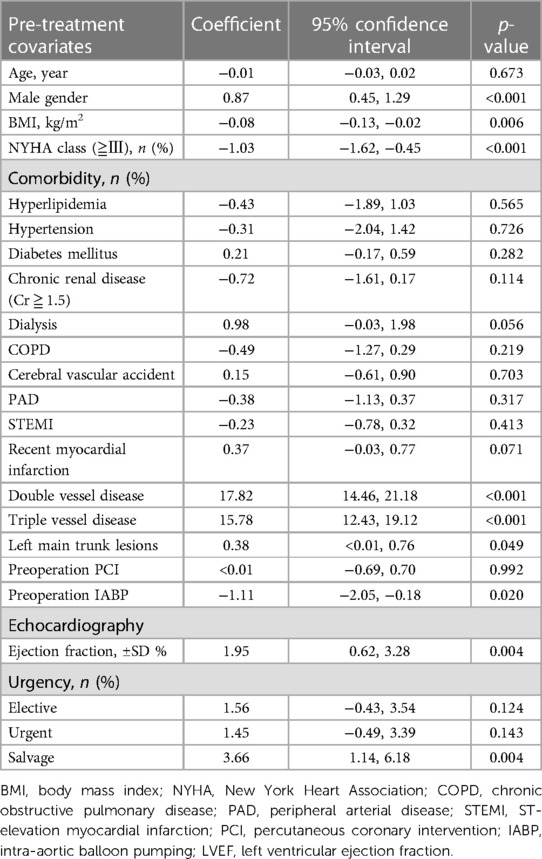
Table 2. Derivation of propensity score equation from pre-treatment covariates under multivariable binary logistic regression.
3 Results
3.1 Preoperative characteristics
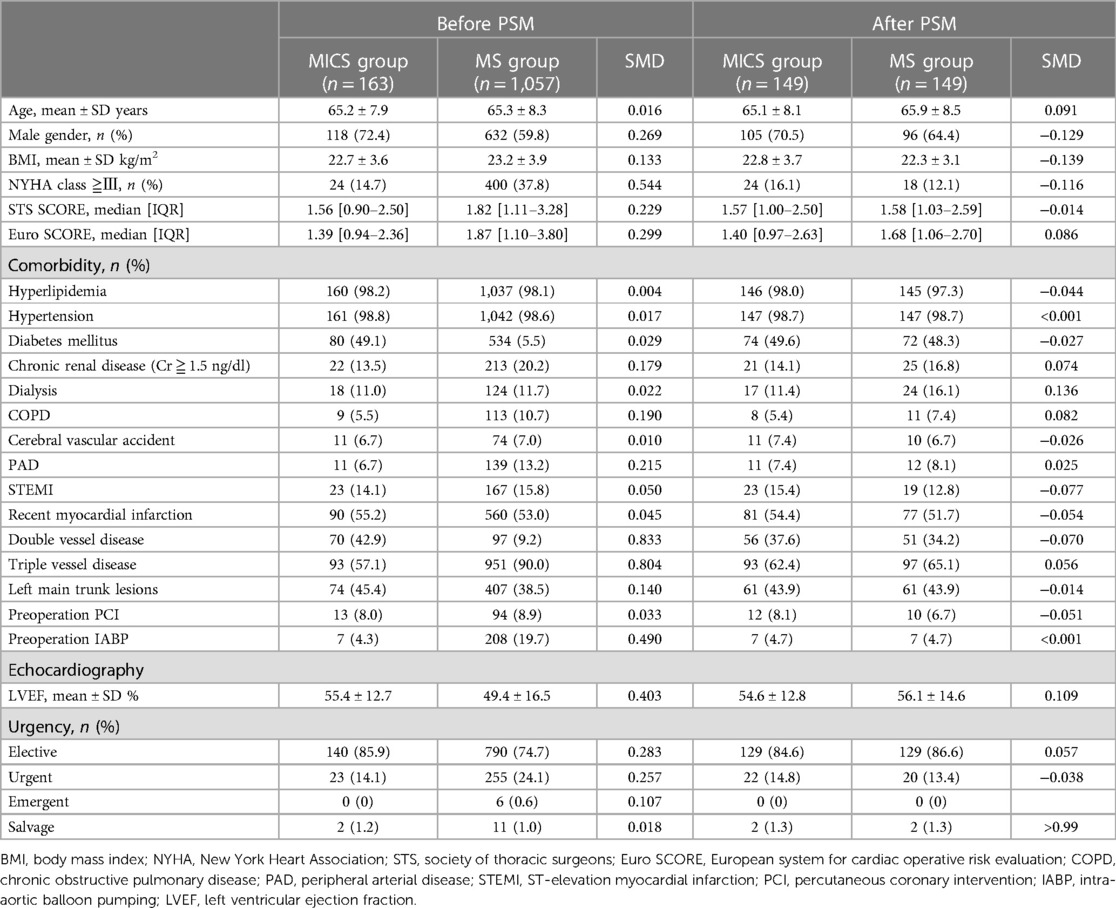
Preoperative characteristics are summarized in Table 1. Before PSM, preoperative conditions were worse in the MS group than the MICS group; the STS SCORE (p = 0.005), Euro SCORE II (p < 0.001), and number of urgent cases (p = 0.005) were higher in the MS group. There were no significant differences in data after PSM. However, for variables (male, body mass index, NYHA class over 3, dialysis, and LVEF) with standardized mean difference values over 10% post matching, a double adjustment was performed above five items to generate Tables 3, 4.
3.2 Operative data
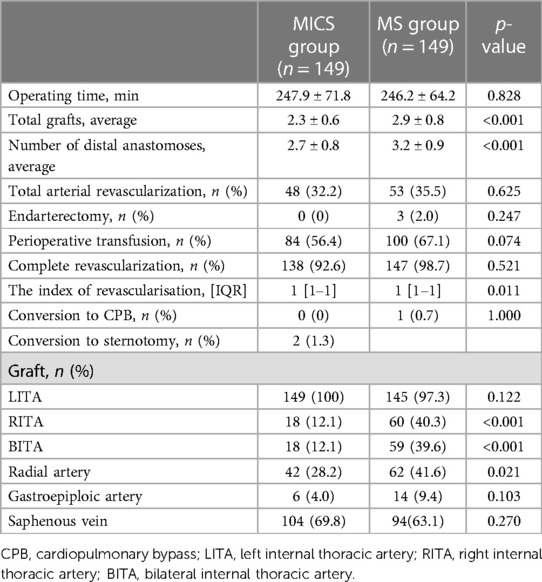
Operative data of the groups are shown in Table 3. There were no differences in operative time, number of complete revascularizations, nor perioperative transfusion rate, but the total graft number (MICS group 2.3 ± 0.6, MS 2.9 ± 0.8; p < 0.001), mean number of distal anastomoses (MICS 2.7 ± 0.8, MS 3.2 ± 0.9; p < 0.001), bilateral internal thoracic artery (BITA) usage rate (MICS 11.5%, MS 36.7%; p < 0.001) were higher in the MS group.
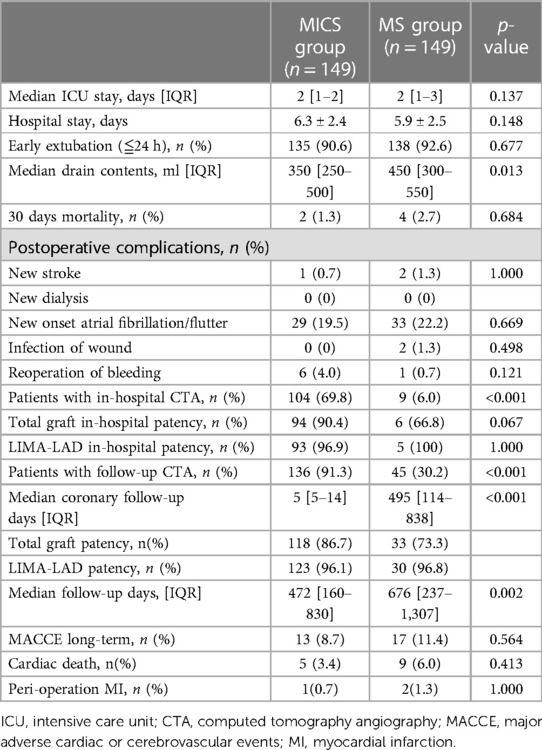
3.3 Short-term outcomes
Short-term outcomes are shown in Table 4. There were no differences in hospital stay, intensive care unit (ICU) stay, postoperative complications, nor 30-day mortality, but the MICS group had less drainage (MICS 350 (250–500) ml, MS 450 (300–550) ml; p = 0.013).
3.4 Postoperative freedom from MACCE and survival rates
The Kaplan–Meier curve of the postoperative MACCE-free rates and survival rates are shown in Figure 2, where there were no differences between the two groups (MACCE-free rate: HR = 1.25, 95% CI: 0.58–2.70, p = 0.945; Survival rate: HR = 0.96, 95% CI: 0.41–2.28, p = 0.374).
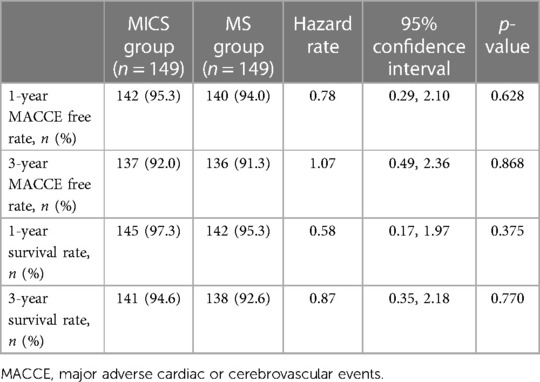
Additionally, there were no differences in the MACCE-free rate and survival rate at 1 and 3 years as shown in Table 5.
4 Discussion
These results demonstrate that MICS-OPCAB is a safe and practical procedure with acceptable short and mid-term outcomes, similar to those of conventional OPCAB. The only statistically significant advantage of MICS-OPCAB was the amount of postoperative drainage.
4.1 Is MICS-OPCAB less invasive compared to conventional OPCAB with median sternotomy?
Previous studies report that MICS-OPCAB could lead to early extubation, less wound infections, less transfusion, faster postoperative recovery, and shorter ICU stay and hospitalization, while maintaining safety and effectiveness compared to median sternotomy (5–7). Another study (8) comparing clinical outcomes of MICS-CABG and OPCAB found that MICS-CABG led to a significantly shorter hospital stay (MICS-CABG = 4 days vs. OPCAB = 5 days) and earlier extubation (MICS-CABG = 70.0% vs. OPCAB = 12.7%) than OPCAB. However, the present study showed multivessel MICS-OPCAB to have a significant advantage only in postoperative drainage; MICS-OPCAB did not improve duration of ICU and hospital stay, perioperative transfusion amount, nor complication rates. Our perioperative transfusion rate is higher compared to rates reported for OPCAB (MICS-CABG = 56.4% vs. OPCAB = 67.1%), likely because we did not specifically focus on minimizing transfusions. Additionally, the introduction of MICS-OPCAB at our hospital in 2017 may have influenced the transfusion rates, as there could have been a higher utilization of transfusions in the MICS-CABG group to prevent conversions to median sternotomy or on-pump procedures. While MICS OPCAB may indeed offer potential improvements in post-operative quality of life for patients, as highlighted by ongoing research such as the Minimally Invasive coronary surgery compared to STernotomy coronary artery bypass grafting (MIST) trial (9), it's important to note that factors such as time to ambulation and pain assessment were not investigated in our study. Furthermore, the durations of early extubation, ICU stay, and hospitalization in the median sternotomy group were already sufficiently short in our study, which may have contributed to the lack of significant differences observed between groups. Therefore, MICS-OPCAB may truly be a less invasive procedure that does not compromise patients’ clinical outcomes.
4.2 Concern about the number of distal anastomoses and complete revascularization rate in MICS-OPCAB
Generally, the number of grafts and distal anastomoses in MICS-OPCAB is fewer, while operative time is longer than conventional OPCAB. Rogers et al. compared OPCAB by left anterolateral thoracotomy (ThoraCAB) and OPCAB by conventional median sternotomy (MS group) at two centers in an RCT trial, where they found the operative time was longer in the ThoraCAB group (4.1 h) than in the MS group (3.3 h) (10). Also, less patients in the ThoraCAB group had more than three grafts (2%), compared to the MS group (17%). This could be attributed to limited range of anastomosis within a constrained space, which isa disadvantage of MICS-OPCAB. Similarly, in our study, the total graft and mean number of distal anastomoses were significantly higher in the MS group, without significant differences in operative time between the two groups. While the numbers of anastomoses and grafts are generally smaller, complete revascularization can be achieved even with the MICS approach. Oleksandr et al. achieved complete revascularization by MICS-CABG on non-selected consecutive patients, using a Chitwood clamp and blood cardioplegia (11). They concluded that complete revascularization in MICS-CABG is possible without patient selection based on graft number, coronary artery quality, location, left ventricular function, age, sex, nor body mass index.
At our institution, we have consistently prioritized comprehensive revascularization with MICS-OPCAB, and our analysis showed that the complete revascularization rate was similar to that of conventional OPCAB (MICS group = 92.6% vs. MS group = 98.7%, p = 0.521). Although Oleksandr et al. found patient selection for MICS-CABG to be more arbitrary, we think that the critical factor for a successful MICS-OPCAB lies in the careful selection of patients for complete revascularization with minimal anastomoses and grafts.
4.3 Long-term outcome of MICS-OPCAB
Although it is widely accepted that MICS-OPCAB yields similar short to mid-term results to MS, the long-term outcome remains uncertain. Barsoum and colleagues reported that patients aged ≥75 years have a significantly lower 5-year all-cause mortality with MICS-CABG than with MS (12). Florisson and colleagues concluded from 12 reports from 1999 to 2017 that MIDCAB is associated with greater morbidity and reintervention rates than OPCAB by MS, due to MIDCAB having a lower rate of complete revascularization (13). However, these studies were conducted approximately 10 years ago, and with technical improvements in recent years, the clinical outcomes have also improved. In our study, there were no significant differences in the MACCE-free and survival rates after 1 year and 3 years between MICS-OPCAB and conventional OPCAB. We have interpreted these results as follows: MICS-OPCAB can provide similar long-term outcomes to conventional OPCAB if complete revascularization can be achieved.
4.4 Grafting strategies in MICS-OPCAB
The concept of surgical revascularization through a left thoracic minimal incision stepped up from single bypasses to multiple bypasses with total arterial grafting using BITA (3, 14, 15). Kikuchi and colleagues analyzed short-term outcomes of MICS-OPCAB using BITA and a single internal thoracic artery (SITA) at a single Japanese medical center between February 2012 and December 2015 (15). Although mean operation time was longer in the BITA group (SITA 265 ± 104 min, BITA 336 ± 73 min), all BITA grafts were harvested without major complications and patent on one-week postoperative CTAs, concluding BITA harvest to be safe in MICS-OPCAB. Based on such findings and improved long-term results with BITA (16), we have been proactively using BITA in MICS-OPCAB for young patients. However, the MICS BITA rate was lower than that of the OPCAB group in our study, because harvesting the right internal thoracic artery (RITA) in the MICS group was often difficult due to cardiac enlargement or concaved thorax (MICS 12.1%, MS 39.6%; p < 0.001).
In MICS-OPCAB cases where harvesting RITA is challenging, LITA Y-composite grafts or the left subclavian artery (Figure 3) are good options for conduits. The Y-composite from LITA as the inflow has shown satisfactory clinical results, when the gold standard configuration of LITA-LAD is preserved (17, 18). CABG using the left axillary artery as a conduit is reported to have a 1-year patency rate of 80%–90% (19), but longer term patency rates remain uncertain. Nonetheless, we believe that the left subclavian artery is a viable option for elderly patients with severe calcification and atheroma in the ascending aorta; At our institution, we have performed >20 MICS-OPCAB with left subclavian artery grafting for such cases. In this way, MICS-OPCAB creates opportunity for more novel graft designs.

Figure 3. Central anastomosis made on the left subclavian artery. (A) Y-composite graft (saphenous vein—radial artery), and (B) postoperative CTA.
4.5 Proper patient selection for MICS-OPCAB
While exclusion criteria for MICS-OPCAB at our institution have already been discussed, the final decision is based on a comprehensive evaluation of the patient's condition, cardiac anatomy, and surgeon experience. Surgeons’ first few cases of MICS-OPCAB can be challenging and time consuming. To overcome this learning curve, we advise beginning with single LITA-LAD bypasses, and selecting simpler cases (such as patients with stable preoperative condition, normal heart size, and preserved LVEF) during early stages of performing multivessel MICS-OPCAB to quickly improve operation time (2, 20). With an established surgical technique, MICS-OPCAB can yield similar results to MS, even in cases with complex graft designs. Contrarily, MS may be a more suitable approach for patients with severely calcified coronary arteries that may require endarterectomy, because extensive exfoliating manipulation is not ideal for MICS. Endarterectomy was not performed in any MICS cases in our study.
4.6 Study limitations
Our study is a retrospective, nonrandomized analysis from a single medical center, where all MICS-OPCAB were performed by one surgeon. PSM was based on preoperational patient characteristics, with several unmeasured confounders. Assessing post-operation outcomes was limited, especially after discharge, because follow-up CTA is generally not done due to a lack of insurance reimbursement in Thailand. That's why our mid-term follow-up data primarily focused on the rates of MACCE and survival. Clinical examinations were conducted for outpatients, with coronary evaluation pursued for patients presenting with symptoms of cardiac ischemia. However, long-term follow-up data for coronary CTA of MICS-OPCAB were lacking. Further research on mid to long-term results is necessary. Furthermore, a simple comparison of patency rates couldn't be made because the median CTA follow-up dates of the MICS and MS groups were quite different and varied.
5 Conclusion
Provided that there is proper patient selection, MICS-OPCAB can provide good short to mid-term results similar to those of conventional OPCAB.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by Kanoksri Samintharapanya, M.D., Chairman of Lampang Human Ethics Research Subcommittee. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
RU: Conceptualization, Data curation, Writing – original draft. AH: Data curation, Writing – review & editing. DY: Resources, Writing – review & editing. BS: Resources, Writing – review & editing. JC: Resources, Writing – review & editing. TL: Formal Analysis, Writing – review & editing. JP: Formal Analysis, Writing – review & editing. SL: Formal Analysis, Writing – review & editing. HK: Methodology, Project administration, Writing – review & editing. NA: Conceptualization, Project administration, Resources, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
We would like to express our sincere gratitude to the faculty and team of Chiang Mai University and Lampang Hospital for their valuable assistance in the statistical analysis of this research. Their expertise and support played a crucial role in ensuring the accuracy of our data analysis.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Subramanian VA. Less invasive arterial CABG on a beating heart. Ann Thorac Surg. (1997) 63(6 Suppl):S68–71. doi: 10.1016/s0003-4975(97)00417-7
2. Rajput NK, Kalangi TKV, Andappan A, Swain AK. MICS CABG: a single-center experience of the first 100 cases. Indian J Thorac Cardiovasc Surg. (2021) 37(1):16–26. doi: 10.1007/s12055-020-01048-2
3. Yang D, Zhang K, Li J, Wei D, Ma J, Wang Y, et al. Ninety-seven cases of experiences with the left thoracotomy approach for off-pump conventional revascularization: a retrospective cohort study. J Thorac Dis. (2022) 14(10):3915–23. doi: 10.21037/jtd-22-1162
4. Ushioda R, Hirofuji A, Yoongtong D, Sakboon B, Cheewinmethasiri J, Kamiya H, et al. Off-pump minimally invasive coronary artery bypass grafting in patients with left ventricular dysfunction: the lampang experience. Front Surg. (2024) 11:1324343. doi: 10.3389/fsurg.2024.1324343
5. Xu ZF, Ling YP, Cui ZQ, Zhao H, Gong YC, Fu YH, et al. Feasibility and safety of minimally invasive cardiac coronary artery bypass grafting surgery for patients with multivessel coronary artery disease: early outcome and short-mid-term follow up results. Beijing Da Xue Xue Bao Yi Xue Ban. (2020) 52(5):863–9. (Chinese). doi: 10.19723/j.issn.1671-167X.2020.05.011
6. Liang L, Liu JJ, Kong QY, You B, Ma XL, Chi LQ, et al. Comparison of early outcomes associated with coronary artery bypass grafting for multi-vessel disease conducted using minimally invasive or conventional off-pump techniques: a propensity-matched study based on SYNTAX score. J Cardiothorac Surg. (2022) 17(1):144. doi: 10.1186/s13019-022-01905-8
7. Lapierre H, Chan V, Sohmer B, Mesana TG, Ruel M. Minimally invasive coronary artery bypass grafting via a small thoracotomy versus off-pump: a case-matched study. Eur J Cardiothorac Surg. (2011) 40(4):804–10. doi: 10.1016/j.ejcts.2011.01.066
8. Rabindranauth P, Burns JG, Vessey TT, Mathiason MA, Kallies KJ, Paramesh V. Minimally invasive coronary artery bypass grafting is associated with improved clinical outcomes. Innovations (Phila). (2014) 9(6):421–6. doi: 10.1177/155698451400900605
9. Guo MH, Wells GA, Glineur D, Fortier J, Davierwala PM, Kikuchi K, et al. Minimally invasive coronary surgery compared to STernotomy coronary artery bypass grafting: the MIST trial. Contemp Clin Trials. (2019) 78:140–5. doi: 10.1016/j.cct.2019.01.006
10. Rogers CA, Pike K, Angelini GD, Reeves BC, Glauber M, Ferrarini M, et al. An open randomized controlled trial of median sternotomy versus anterolateral left thoracotomy on morbidity and health care resource use in patients having off-pump coronary artery bypass surgery: the sternotomy versus thoracotomy (STET) trial. J Thorac Cardiovasc Surg. (2013) 146(2):306–16.e1-9. doi: 10.1016/j.jtcvs.2012.04.020
11. Babliak O, Demianenko V, Melnyk Y, Revenko K, Pidgayna L, Stohov O. Complete coronary revascularization via left anterior thoracotomy. Innovations (Phila. (2019) 14(4):330–41. doi: 10.1177/1556984519849126
12. Barsoum EA, Azab B, Shah N, Patel N, Shariff MA, Lafferty J, et al. Long-term mortality in minimally invasive compared with sternotomy coronary artery bypass surgery in the geriatric population (75 years and older patients). Eur J Cardiothorac Surg. (2015) 47(5):862–7. doi: 10.1093/ejcts/ezu267
13. Florisson DS, DeBono JA, Davies RA, Newcomb AE. Does minimally invasive coronary artery bypass improve outcomes compared to off-pump coronary bypass via sternotomy in patients undergoing coronary artery bypass grafting? Interact Cardiovasc Thorac Surg. (2018) 27(3):357–64. doi: 10.1093/icvts/ivy071
14. Kikuchi K, Une D, Kurata A, Ruel M. Off-pump minimally invasive coronary artery bypass grafting using the bilateral internal thoracic arteries and the right gastroepiproic artery. Eur J Cardiothorac Surg. (2016) 49(4):1285–6. doi: 10.1093/ejcts/ezv281
15. Kikuchi K, Chen X, Mori M, Kurata A, Tao L. Perioperative outcomes of off-pump minimally invasive coronary artery bypass grafting with bilateral internal thoracic arteries under direct vision†. Interact Cardiovasc Thorac Surg. (2017) 24(5):696–701. doi: 10.1093/icvts/ivw431
16. Dorman MJ, Kurlansky PA, Traad EA, Galbut DL, Zucker M, Ebra G. Bilateral internal mammary artery grafting enhances survival in diabetic patients: a 30-year follow-up of propensity score-matched cohorts. Circulation. (2012) 126(25):2935–42. doi: 10.1161/CIRCULATIONAHA.112.117606
17. Wendler O, Hennen B, Markwirth T, König J, Tscholl D, Huang Q, et al. T grafts with the right internal thoracic artery to left internal thoracic artery versus the left internal thoracic artery and radial artery: flow dynamics in the internal thoracic artery main stem. J Thorac Cardiovasc Surg. (1999) 118(5):841–8. doi: 10.1016/s0022-5223(99)70053-x
18. Nakajima H, Kobayashi J, Tagusari O, Bando K, Niwaya K, Kitamura S. Competitive flow in arterial composite grafts and effect of graft arrangement in off-pump coronary revascularization. Ann Thorac Surg. (2004) 78(2):481–6. doi: 10.1016/j.athoracsur.2004.03.003
19. Athanasiou T, Kapetanakis EI, Rao C, Salvador L, Darzi A. Axillary artery to left anterior descending coronary artery bypass with an externally stented graft: a technical report. J Cardiothorac Surg. (2008) 3:6. doi: 10.1186/1749-8090-3-6
Keywords: intercostal space, left small thoracotomy, median sternotomy, minimally invasive direct coronary artery bypass grafting, surgical revascularization
Citation: Ushioda R, Hirofuji A, Yoongtong D, Sakboon B, Cheewinmethasiri J, Lokeskrawee T, Patumanond J, Lawanaskol S, Kamiya H and Arayawudhikul N (2024) Multi-vessel coronary artery grafting: analyzing the minimally invasive approach and its safety. Front. Cardiovasc. Med. 11:1391881. doi: 10.3389/fcvm.2024.1391881
Received: 26 February 2024; Accepted: 18 April 2024;
Published: 7 May 2024.
Edited by:
Francesco Formica, University of Parma, ItalyReviewed by:
Daniel P. Fudulu, University of Bristol, United KingdomPhilemon Gukop, St George’s University Hospitals NHS Foundation Trust, United Kingdom
Alan Gallingani, University Hospital of Parma, Italy
© 2024 Ushioda, Hirofuji, Yoongtong, Sakboon, Cheewinmethasiri, Lokeskrawee, Patumanond, Lawanaskol, Kamiya and Arayawudhikul. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Aina Hirofuji bmVvbGVub3JlNzhAZ21haWwuY29t
 Ryohei Ushioda
Ryohei Ushioda Aina Hirofuji2*
Aina Hirofuji2* Hiroyuki Kamiya
Hiroyuki Kamiya Nuttapon Arayawudhikul
Nuttapon Arayawudhikul